Abstract
Swallowing is a complex physiologic process to transport saliva and nutrition from the oral cavity to the stomach, avoiding the threat of food or liquid entering the airway. Complex circuits in the brainstem and in supratentorial areas guarantee sequential and rhythmic patterns of motor neurons controlling the swallowing muscles. Dysphagia is the impairment of these mechanisms, leading to the reduction of swallowing safety with the risk of pulmonary complications and swallowing efficacy with the risk of malnutrition. Different mechanisms related to a wide range of clinical conditions may lead to swallowing safety and efficacy reduction. Appropriate management relies on identification of affected patients through screening programs and clinical and instrumental assessment. Medical management includes the treatment of the underlying diseases, avoidance of drugs that interfere with swallowing, botulinum toxin injection, and in selected cases surgery.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
8.1 Introduction
Swallowing is a series of sequential coordinated events that ensures passage of any substance (food, liquid, saliva, mucus, drugs) from the mouth to the stomach via the pharynx and esophagus, avoiding the passage of the swallowed substance into the airway. Dysphagia is the term used to describe any difficulty in swallowing; therefore, the term dysphagia does not represent a medical diagnosis, but a symptom a patient reports to the physician; in common language and clinical practice, the term dysphagia also refers to any swallowing disorder, reported by the patient or recognized by a clinician through a clinical assessment or an instrumental examination [1]. Different diseases of different origins, neurological and non-neurological, may lead to dysphagia (Table 8.1). The importance in recognizing and managing dysphagia lies in the fact that, irrespective of the original disease, dysphagia can lead to severe complications such as aspiration pneumonia, malnutrition, and dehydration that severely impact patient’s survival, clinical management, and health costs [2]. Adequate management of dysphagia is of pivotal importance for the neurologists as dysphagia complications are often the leading cause of mortality in several neurological diseases such as stroke, Parkinson’s disease, motor neuron disease, and muscular diseases.
In this chapter basic information on swallowing physiology will be reported, so that pathophysiology of dysphagia can be better understood, together with dysphagia complications. Strategies commonly adopted to recognize and assess dysphagia are then analyzed and possible medical treatments outlined.
8.2 Swallowing Physiology
Swallowing physiology is a complex process; for teaching purposes seven stages can be identified in adults’ swallowing (Table 8.2, Fig. 8.1) [3,4,5]. In the oral preparatory stage, the food is taken into the mouth, chewed and insalivated, while the largest concentration and variety of receptors of the whole body analyze taste, odor, texture, and temperature. For mastication chewing muscles elevate the mandible, the anterior neck muscles actively open the mouth, while the tongue moves the food in the molar region and the buccinators push it from the vestibulum oris. This phase is fully voluntary and conscious in normal adults. When the bolus is considered ready to be swallowed by the sensory oral systems, it is placed in the middle of the tongue and pressed against the palate by sequential contraction (oral transport stage). As the bolus reaches the faucial pillars, the so-called swallowing reflex starts, and the pharyngeal phase takes place; its complexity emerges as a consequence of the common shared pathway between the respiratory and gastrointestinal pathways [6]. In order to prevent passage of food into the airway, the pharynx configuration should change from respiratory to digestive, and apnea should be inserted in normal breathing; velopharyngeal closure, laryngeal elevation and anteriorization, laryngeal closure including tilting of the epiglottis, and relaxation of upper esophageal sphincter (UES) are the key points of pharyngeal reconfiguration, while tongue base retraction and pharyngeal peristalsis are the driving force for moving the bolus from the oral cavity into the upper esophagus. Laryngeal elevation is obtained by the contraction of suprahyoid muscles and laryngeal closure relies on intrinsic laryngeal muscles, while epiglottic tilting results as a combination of tongue base retraction, bolus pressure, and laryngeal elevation/anteriorization. UES opening is due to laryngeal anteriorization, cricopharyngeal muscle (CM) relaxation, and bolus pressure [7]. The most common pattern of swallowing/breathing coordination is expiration-swallowing-expiration; only in rare cases, swallowing is followed by inspiration [8]. The pharyngeal phase is automatic and not conscious. Once in the esophagus, the bolus proceeds to the stomach thanks to esophageal peristalsis, a mechanism mainly related to intrinsic nerve plexuses in the esophagus and characterized by the relaxation of the downstream smooth muscles and contraction of the upstream smooth muscles. The passage of the bolus into the stomach is possible thanks to the relaxation of the lower esophageal sphincter (LES); during the gastric phase, the bolus lies in the stomach, and the LES prevents reflux into the esophagus, while the pylorus avoids premature passage into the duodenum.
Schematic representation of the different phases of swallowing. (a) oral phase: the bolus (represented in red) lies in on the midportion of the tongue; (b) end of the oral phase: the bolus has reached the faucial pillar and lies on the tongue base; (c) pharyngeal phase: the bolus is in the valleculae, and the soft palate is elevated; (d) pharyngeal phase: the bolus is in the pharynx, and the epiglottis is inverted; (e) esophageal phase: the bolus is passing through the upper esophageal sphincter; (f) esophageal phase: the bolus is passing in the cervical esophagus
8.2.1 Neurophysiology of Swallowing
Cerebral neuronal activation influences the mechanical behavior of the pharynx and esophagus. Two regions of the central nervous system (CNS) have a role in the control of swallowing: the brain stem and the supramedullary areas. The brain stem is responsible for the reflex part of the swallowing mechanism: both the sensory and motor nuclei of the cranial nerves involved in swallowing as well as the interneurons connecting them lie in this part of the CNS; moreover the sequential and rhythmic patterns of motor neurons controlling the swallowing muscles are generated by a group of neurons of the medulla oblongata, called as the central pattern generator. Afferent inputs from cranial nerves V, IX, and X, of which the superior laryngeal branch, the superior laryngeal nerve, is the most important, represent one possible way to trigger pharyngeal swallowing. The brain stem sequential activity may be triggered or modulated also by the supramedullary regions including the supplementary motor area, the pre- and postcentral gyri, the insula, the anterior cingulate gyrus, the basal ganglia, and the cerebellum [9].
A large number of oral and pharyngeal reflexes are controlled by the neuronal connections of the brain stem and play a vital role in the complex behavior of swallowing (Table 8.3); these reflexes modify motor neurons’ activity, which receive synaptic input from supramedullary regions, and function as supporting networks of neurons assisting in the control of complex motor responses, such as speech, intraoral transport of food, chewing, and swallowing [10]. Supramedullary control of swallowing is an area of active research through animal models as well as different kinds of brain imaging techniques; although definitive understanding is not reached, five functional modules have been suggested: (1) sensorimotor areas and the cingulate cortex, establishing a sensorimotor output for which other areas converge; (2) the inferior frontal gyrus, corpus callosum, basal ganglia, and thalamus, involved in movement planning and implementation of other voluntary motor behaviors; (3) the premotor cortex and posterior parietal cortex, serving to integrate sensory information about the bolus with the internal representation of swallowing movements; (4) the cerebellum, whose role is to facilitate the modulation of the internal representation for swallowing and coordination among the multiple effectors and effector states during swallowing; (5) the insula, recruited for synchronizing the kinematics of the movements [11].
8.3 Pathophysiology of Dysphagia
Different diseases of neurologic and non-neurologic origin may cause dysphagia. For appropriate dysphagia management, disease diagnosis and treatment are often not sufficient, and the mechanism underlying swallowing impairment should be found. The major signs of dysphagia are penetration (Fig. 8.2) and aspiration (Fig. 8.3), residue along the oropharyngoesophageal tract (Fig. 8.4) and regurgitation either from the oropharynx into the rhinopharynx or from the esophagus into the hypopharynx. The term penetration means that part of the bolus enters the laryngeal vestibule, while aspiration means that the bolus passes the vocal folds and reaches the tracheobronchial tree. Penetration and aspiration usually cause reflexive cough, but in cases of laryngeal and/or tracheobronchial sensitivity reduction, cough may be absent (silent penetration/aspiration). Penetration/aspiration may be divided in pre-deglutitive, intra-deglutitive, and post-deglutitive depending whether it occurs respectively before, during, or after the swallowing reflex has started [12]. While dysphagia signs confirm the presence of a swallowing impairment, the underlying mechanism should be identified for appropriate treatment (Table 8.4) [13].
8.4 Complications of Dysphagia
Dysphagia complications include but are not limited to aspiration pneumonia, malnutrition, dehydration, and chronic aspiration; while pulmonary complications are the result of impaired safety of swallowing leading to tracheobronchial aspiration, malnutrition and dehydration are due to impaired efficacy of swallowing with reduced oral intake of nutrients.
8.4.1 Aspiration Pneumonia
Pulmonary complications are probably the most common and severe complications of dysphagia. They are the results of an impaired balance between defense mechanisms of the lower respiratory tract, oropharyngeal bacterial colonization, and impaired efficacy of swallowing with aspiration of the bacteria [14] (Fig. 8.5). The lower respiratory tract is protected by several defense mechanisms: airway clearance, including both cough and mucociliary action, lymphatic clearance, and cellular immune defense by macrophages, lymphocytes, and neutrophils. Several clinical conditions can reduce these defense mechanisms, increasing the risk of pulmonary complications whether food or liquid aspiration occurs. Among pulmonary complications, aspiration pneumonia is defined as the development of an infiltrate in the dependent portions of the lung in people who are at increased risk for aspiration of oropharyngeal contents (microaspiration) containing bacteria with associated symptoms and signs of lung infection [15]. Different papers showed an increased relative risk of developing pneumonia in patients with aspiration; however, the role played by the various risk factors was not equal in the different populations [16,17,18,19,20,21]. Other factors, such as advanced age, medical conditions, mental status, poor nutritional status, and oropharyngeal colonization of pathogenic bacteria appeared as risk factors for developing aspiration pneumonia [22]. The role of oral care has been investigated in a series of studies [23,24,25]; it has been demonstrated that oral care reduces pneumonia and death from pneumonia in both dentate and edentate patients [25].
8.4.2 Dehydration
Dehydration is frequently reported in hospitalized or institutionalized patients. Clinical factors, as undiagnosed dysphagia or cognitive impairment, sociocultural factors, as inability to speak, and institutional factor, as inadequate number of knowledgeable staff, contributed to inadequate fluid intake [26]. When the presence of dysphagia is recognized and aspiration of thin liquids is reported through an instrumental assessment of swallowing, thickened liquids are often recommended [27], in particular when a coexisting language and/or cognitive impairment reduce the possibility to effectively use compensatory strategies (e.g., postures) that may reduce aspiration of thin liquids. Despite the reduction of liquids’ aspiration, different studies report an inadequate liquid intake (<1500 ml/day) in poststroke patients requiring thickened liquids [28,29,30,31], while the positioning of enteral nutrition has a significant and positive impact on dehydration in patients with severe dysphagia [29]. Factors associated with poor fluid intake in poststroke patients with thickened liquids are the presence of functional deficits in cognition reducing the compliance with clinicians’ recommendation, the frequency of beverage offerings and the availability of thickened liquids to patients, and the inaccurate preparation of thickened beverages, often too thick [30]. Therefore, fluid intake in poststroke dysphagic patients could be increased with protocols for the provision and monitoring of thickened liquids’ consumption, through adequate education of nursing staff and caregivers, and by integrating hydration using non-oral supplementary routes.
8.4.3 Malnutrition
Malnourishment is common in hospitalized patients with a prevalence of up to 50% in surgical, medical, geriatric, and stroke patients [32]. This reported high prevalence is related to a number of factors, including sensory losses, chewing or swallowing problems, and anorexia, together with acute or chronic diseases that may compromise dietary intake and lead to nutritional deficiencies and malnutrition [32].
As far as the swallowing problems are concerned, the relationship between dysphagia and malnutrition is debated. A recent systematic review concluded that the odds of malnutrition were increased in elderly, frail and institutionalized persons, in patients with excessive polypharmacy, general health decline, cognitive decline, eating dependencies, and dysphagia [33]. However, only five of the eight studies included in the review reported significant associations between dysphagia and malnutrition, and the pooled analysis revealed a significant effect only for trials conducted several weeks following stroke.
It is possible that malnutrition may develop as a consequence of dysphagia if nutritional intake is substantially reduced in relation to requirements over the course of days or weeks. For those who are able to eat orally, fear of eating and/or choking, unwillingness to eat, and the decreased palatability of texture-modified diets may lead directly to inadequate intake. However, other factors that often accompany dysphagia may also have an impact indirectly on an individual’s desire or ability to eat. This is particularly true in neurologic patients where fatigue, motor impairment, visuospatial perceptual problems, depression, and cognitive deficits may be contributory.
8.4.4 Chronic Aspiration
Chronic aspiration may not cause acute infections within the lungs (aspiration pneumonia) but can lead to diseases such as chronic lipoid pneumonia, obliterative bronchiolitis, and diffuse aspiration bronchiolitis. Typically, the aspiration is silent, and the patient often presents with slowly progressive symptoms of cough, shortness of breath, recurring fevers, and lung opacities on chest radiograph. On CT scan the disease usually presents as diffuse basilar centrilobular nodules and/or tree-in-bud pattern with airway and interstitial thickening. Often the diagnosis is not elucidated until biopsy reveals granulomatous inflammation associated with particulate matter consistent with oral or gastric origin, such as vegetable, lipid, or talc particles. Chronic occult aspiration has been associated with refractory asthma and idiopathic pulmonary fibrosis [34].
8.5 Dysphagia Assessment
Dysphagia assessment is of pivotal importance not for the search of the etiology but also to identify patients with dysphagia, recognize its severity, estimate risk of complications, and provide the most appropriate management.
8.5.1 Screening
The prevalence of dysphagia exceeds 50% in stroke patients, accounts for 10–30% of individuals older than 65 years, and may be as high as 84% in patients with Parkinson’s disease [35]; in many of them, dysphagia is not recognized. Early identification of dysphagia is mandatory since it can reduce the incidence of clinical complications and may improve the outcome in these patients; for these reasons several dysphagia screening tools have been proposed [36]. The large part of them have been developed for stroke population, and only a few screening tools are available for patients with different diagnoses. One of the most promising of them is the Royal Brisbane and Women Hospital (RBWH) dysphagia screening tool [37]. This is a nurse-administered, evidence-based swallow screening tool, based on the triaging concept that can be applied in everyday clinical practice in the management of dysphagia in heterogeneous populations. The RBWH dysphagia screening tool consists of three steps: (1) a two-phase question screen; (2) a water swallow test, as appropriate; and (3) a swallowing management plan. The two-phase question screen reflects the perception that identification of “at-risk” patients should come from a combination of (1) previous medical history/records and (2) specific clinical indicators. The second phase consists of a water swallow test with 90 ml of water. The nurse is prompted to observe for (1) coughing during or between swallows or up to 1 min after swallowing, (2) wet or “gurgly” voice quality post swallow, and (3) increased respiratory rate post swallow [37]. Depending on the results of the screening evaluation, patients with a positive result in the dysphagia screening examination are referred to a swallowing specialist.
8.5.2 Bedside Evaluation (BSE)
The bedside examination (BSE) is the clinical assessment performed by a swallowing expert, usually a speech and language pathologist, without the support of any instrument; the aims are to detect the presence of an alteration of the swallowing process, to decide how to provide nourishment to the patient, to set the rehabilitation goals and program, and to underline the need of an instrumental assessment. The BSE also includes the assessment of aspects different from swallowing, guiding the clinician in the identification of possible barriers, facilitators, and patient’s resources.
The BSE should include:
-
Collection of anamnestic data, i.e., diagnosis, medical history, previous clinical and instrumental assessments of dysphagia, rheological modifications of liquids and foods, and recent modification of nutritional status, respiratory status, alcohol abuse
-
Observation of vigilance, communication efficacy, presence and characteristics of tracheal cannula, sialorrhea, oral hygiene, presence of neglect, auditory and visual defects, and independence
-
Morphodynamic assessment of swallowing structures (the lips, tongue, hard and soft palate, jaw, larynx, and head and trunk control)
-
Oral praxis assessment
-
Sensitivity assessment
-
Normal reflexes assessment (cough, gag, and swallowing reflex)
-
Pathological reflexes assessment
-
Swallowing trials with different consistencies and volumes
Several studies have demonstrated that as nowadays there still exists an inconsistency in the clinical assessment of dysphagia [38, 39]. However, different protocols including all the aspects that should be investigated during the BSE are available in literature. In particular, one of the most widespread protocols is the Mann Assessment of Swallowing Ability (MASA) [40]. After BSE the main pathophysiologic signs of impaired swallowing can be detected; however, pathophysiologic interpretation of signs may be difficult. Moreover, silent aspiration cannot be detected.
8.5.3 Instrumental Assessment of Swallowing
The aim of instrumental assessment of swallowing is to perform a thorough assessment of swallowing in order to understand whether a disorder is present, oral feeding is safe, or rehabilitation is necessary. In order to perform instrumental assessment, specific knowledge and skills are necessary; if the examiner holds only part of the requested knowledge and skills, an incomplete examination will be performed, the information obtained will be misleading, the prescription inadequate, and the clinical decision potentially wrong.
The acronym FEES (fiber-optic endoscopic evaluation of swallowing) is usually applied to mean the assessment of swallowing thanks to a flexible endoscope (Fig. 8.6). FEES may be performed in different settings: at the bedside, in the office, and at home; depending on the circumstances, instrumentation may vary, but a fiberscope and a light source are always needed. The procedure to perform FEES may be divided into five major steps: swallowing structures anatomic assessment; swallowing structures’ sensorimotor assessment, secretion management, bolus transit assessment with foods of different volumes (5 cc, 10 cc, 20 cc), and consistency (thin liquid, nectar, honey, puree, soft solid, solid); response to therapeutic maneuvers; and interventions to improve swallowing. All the swallowing structures should be fully observed including the rhinopharynx, the velum, the oro- and hypopharynx, the larynx, the upper part of the trachea, the pyriform sinuses, and the retro-cricoid region, the tongue base, and the valleculae. The assessment of swallowing structures’ motion is of key importance as it gives information on the neuromotor functionality of the system; it includes specific maneuvers to examine individual movements such as blowing to assess velopharyngeal movements, squeezing maneuver (high-pitch strained voice) to assess pharyngeal wall motion, breathing, voicing to assess laryngeal movement, and Valsalva maneuver to assess laryngeal vestibule closure. In order to assess laryngeal sensibility, the tip of the scope could gently touch the epiglottis, the arytenoids, the laryngeal vestibule, and the vocal folds. In the presence of secretions, its characteristics (serous, mucus), site (oro-/hypopharynx, larynx), and spontaneous or induced management are also of key importance to understand the physiology of swallowing structures. The most important part of the FEES is the assessment of bolus transit: the scope could be positioned just below the velum (high position) or close to the laryngeal vestibule (low position), according to whether the examiner is more interested in a general view of the pharynx and larynx or is more focused on the larynx. At least three food consistencies should be used (liquids, puree, solid), with increasing volumes for each consistency. One of the major advantages of FEES is its versatility as any kind of food could be tested. Finally, the main postures and maneuvers according to their specific rationale (see following chapter) should be tested in case a swallowing impairment is found. In selected cases FEES can also be used for rehabilitation as a biofeedback system.
Schematic representation of a fiber-optic endoscopic examination: the endoscope is passed through the nose and lies just below the soft palate. The numbers show the position; the tip of the endoscope should have to study the soft palate and the velopharyngeal movements (number 1), the oropharynx and the larynx (number 2), the vocal folds and the upper trachea (number 3), and the cricopharyngeal region (number 4)
During bolus transit, FEES does not allow to see the bolus itself. In fact as the bolus enters the oropharynx, the pharyngeal phase of swallowing is triggered, and the pharynx changes its configuration from respiratory to swallowing: the tongue base retracts, the pharyngeal wall is squeezed, and the vision is lost (so-called whiteout phase). As the respiratory configuration of the pharynx is restored, the whiteout phase ends, and the bolus is already in the esophagus. The main abnormal findings include (1) anticipated passage of the bolus from the oral cavity to the oro- and hypopharynx; (2) pooling of the part of the bolus in the oral cavity, in the valleculae (Fig. 8.7) or in the pyriform sinuses (Fig. 8.8); (3) penetration and aspiration (Fig. 8.9); (4) regurgitation from the oropharynx in the rhinopharynx; and (5) regurgitation from the esophagus into the pharynx. The understanding of the underlying mechanism is of key importance for the interpretation of FEES [41].
The videofluoroscopic swallow study (VFSS) is a radiologic technique providing a comprehensive evaluation of the oral, palatal, pharyngeal, pharyngoesophageal, and esophageal segments of swallowing. The patient is positioned upright in an examination chair within the fluoroscopy unit in the lateral position and then in anterior-posterior view. The protocol proceeds in a stepwise fashion. Patients are administered liquid, nectar, honey, and puree barium of precise aliquot of increasing volumes; barium-coated solids are also administered. For each bolus the patient is asked to hold the bolus in the oral cavity and swallow when asked to; the whole process is video-recorded with a frame rate of 25–30 frames per second, in order to interpret the examination after the examination and not while performing it. Frame-by-frame analysis is often necessary for precise interpretation of the VFSS. During VFSS not only the contrast bolus is clearly visible but also the following structures and their movements: the lips, mandible, maxilla, tongue, velum, hyoid bone, vallecula, epiglottis, arytenoid cartilage, false vocal folds, true vocal folds, laryngeal vestibule, pyriform sinuses, pharyngeal muscles, CM, trachea, and cervical spine.
Abnormal findings assessed through VFSS include prolonged oral preparation time, tongue pumping due to difficulty in triggering the pharyngeal phase, and serial swallows also known as piecemeal deglutition due to weakness of the oral and pharyngeal musculature, poor bolus formation, oral stasis, poor mastication, nasal regurgitation, delayed swallowing reflex, penetration/aspiration, reduced hyoid elevation, reduced laryngeal elevation, vallecular or pyriform residue, deviant epiglottic function, reduced laryngeal elevation, cricopharyngeal bar due to a defect in cricopharyngeal opening or closing, pharyngeal diverticula, esophageal diverticula, strictures and rings, and esophageal motor impairment.
FEES and VFSS can be considered the two frontline instrumental examinations to assess a person with a potential or known swallowing impairment; both FEES and VFSS can be used to test treatment strategies (see Chap. 9). These two examinations should not be considered overlapping but rather complementary, as the information they provide are not the same. VFSS allows better assessment of oral phase, allows assessment of esophageal phase, and should be considered the optimal examination, especially for cricopharyngeal dysfunction evaluation; on the other side, FEES allows better definition of residue, penetration, and secretion management; besides, FEES can be prolonged and is a better examination for assessment of fatigue. Finally, FEES can be performed consecutively as needed and in almost any setting, regardless of patient positioning and general conditions [42].
8.5.4 High-Resolution Manometry
High-resolution manometry (HRM) is a diagnostic system that measures intraluminal pressure activity in the gastrointestinal tract from the pharynx to the stomach using a series of closely spaced pressure sensors during 5 ml of liquid swallow. HRM provides a topographic mapping of the space-time patterns of hypopharyngeal pressures by means of colored contour plots emerging from 36 sensors spaced at 1 cm interval. Three-dimensional data are displayed on a two-dimensional planar surface: the pressure levels as color bars (mmHg), the sensor position (cm) on the y-axis, and the time (s) on the x-axis. Mainly developed for esophageal diagnostics, its application in the pharynx is getting an increasing importance. For this purpose the oropharyngeal swallowing process can be viewed as a pressure generation mechanism powered by a two-pump system, the oropharyngeal propulsion pump and the hypopharyngeal suction pump. The oropharyngeal pump reflects the combined activity of the tongue base muscles and the upper pharyngeal constrictor muscles, while the hypopharyngeal suction pump reflects the suction forces in the pharyngeal chamber which are the result of the antero-cephalad movement of the hyoid-laryngeal complex. At that same instant, the CM relaxes, enabling traction forces to open it, while the lower pharyngeal constrictor muscles push the bolus into the esophagus. Various features can be defined, such as the UES resting pressure, duration of UES relaxation, nadir pressure during relaxation, duration and pressure of UES post relaxation contraction, peak pharyngeal pressure, intrabolus pressure, and the coordination of the pharyngeal peak within the UES relaxation period [43].
8.5.5 Other Assessment Tools
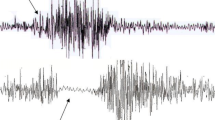
While FEES and VFSS represent the two gold standard techniques, other instrumental tools have been developed. Each of them can have a diagnostic role for specific clinical conditions but may be misleading if not applied after clinical examination and either FEES or VFSS. The two most important instrumental assessment tools besides those previously described are the oropharyngoesophageal scintigraphy (OPES) and the electromyography of swallowing (EMGS). During OPES the patient is given liquid or semisolid with radionuclide technetium-99 and is asked to swallow while placed under a gamma camera. Thanks to the gamma camera, a quantitative picture of radionuclide transit and metabolism can be shown as a plot of radioactivity versus time; while OPES has suboptimal temporal and anatomical resolution, it represents the ideal tool for quantification of residue and aspiration [44]. EMGS allows optimal analysis of muscle contraction duration. Usually EMGS includes surface EMG of submental muscles, needle EMG of the CM, and application of a mechanical transducer on the larynx; simultaneous recording from these three lines allows optimal temporal analysis of submental muscle contractions, laryngeal elevation, and cricopharyngeal relaxation. EMGS is the optimal technique for the identification of CM relaxation impairment that may be treated through botulinum toxin injections [45].
8.6 Medical Management of Dysphagia
8.6.1 Treatment of the Original Disease
As stated in the introduction of this chapter, dysphagia is not a disease, but it is a symptom or a sign of a given disease. Management of dysphagia starts with adequate diagnosis and provision of the best treatment available of the underlying disease. Although dysphagia is often caused by neurological diseases for which no significant treatment is available, as in the case of motor neuron disease, in some other cases, a pharmacological treatment can dramatically improve the clinical condition, as, e.g., in myasthenia gravis. It is therefore imperative to properly treat all neurological diseases, keeping in mind that improvement in neuromuscular function might impact swallowing also; for example, L-DOPA can improve movements in patients with Parkinson’s disease and, if given before mealtime, can improve swallowing too.
8.6.2 Pharmacological Treatment
Swallowing physiology relies on a complex neuromuscular chain of events, regulated by a network of neurons throughout the brain; it is therefore theoretically possible to improve swallowing function by pharmacologic agents that act on the regulation of neurotransmitters involved in these systems. While research is trying to move forward in this direction, especially stimulating the availability of substance P for glossopharyngeal and superior laryngeal nerve, eventually using irritants to the pharynx as capsaicin, there is no evidence in the application of a pharmacological treatment in clinical practice [46].
While no pharmacological treatment to improve swallowing is available, a large number of medications, spanning several classes of pharmacological agents, have undesirable effects on swallowing and should be avoided if possible. One of the most common causes of medication-induced dysphagia is xerostomia; dryness of the mouth impairs bolus transport, increasing the residue in both the oral cavity and the oropharynx. Medicines that depress CNS activity are another large class of medications that interfere with swallowing; decreased arousal and coordination induced by anxiolytics, antihistamines, antipsychotics, and opiates may contribute to dysphagia development. Medications such as theophylline, nitrates, calcium channel blockers, and benzodiazepines reduce LES tone, resulting in gastroesophageal reflux, which injure the mucosa of the upper aerodigestive tract and contribute to dysphagia [47].
8.6.3 Botulinum Toxin
Botulinum toxin is a protease exotoxin produced from Clostridium botulinum. It works by blocking the release of acetylcholine from cholinergic nerve endings causing inactivity of muscles or glands. Its effects are transient and may be graded by varying the dose and frequency of administration [48]. Botulinum toxin has been also used in the treatment of drooling (excessive pooling and poor control of saliva due to dysphagia). Drooling may occur in many patients with neurogenic dysphagia including those with cerebral palsy, neuromuscular diseases such as myasthenia gravis, amyotrophic lateral sclerosis, and neurodegenerative diseases such as Parkinson’s disease. Local injection of botulinum toxin into the salivary glands under ultrasound guidance results in inhibition of cholinergic parasympathetic and postganglionic sympathetic activity causing a reduction of salivary secretion. The effect starts at 1 week and lasts for approximately 3–5 months after injection [49]. The botulinum toxin has been proposed for the treatment of CM incoordination causing dysphagia. The CM is the major component of the UES between the hypopharynx and the esophagus. It is a ring-shaped muscle with horizontal and oblique fibers. The structure and biochemical properties of the CM maintain constant basal tone and luminal occlusion at rest but allow rapid relaxation and contraction during swallowing. The muscle contraction closes the pharyngoesophageal segment, preventing the esophageal reflux and air from entering the esophagus during inspiration. CM dysfunction may result from a delay or failure of relaxation of the fibers during deglutition. Often the underlying cause is not treatable, or it remains unknown. In these cases, EMG-guided botulinum toxin injections to the muscle can be performed either percutaneously [50] or endoscopically [51] and have been found to be effective in the treatment of this selective kind of dysphagia [52].
8.6.4 Surgical Treatment
Severe dysphagic patients with chronic aspiration and/or recurrent aspiration pneumonia, who failed an extensive nonsurgical swallowing rehabilitation, require a strict tube feeding regimen, either by means of a nasogastric tube or a percutaneous gastrostomy tube. However, this will not always result in a complete abolishment of chronic aspiration, as the production and swallowing of saliva will still continue; in addition, lifetime tube feeding is often considered unacceptable for many patients. For this reason, several surgical procedures aimed to the restoration of oral intake have been proposed [53].
UES myotomy can be useful in patients affected by UES dysfunction, while partial pharyngectomy was found to be effective in patients affected by pharyngeal hemiparesis [54]. However, in patients with severe aspiration, inadequate deglutition coordination and diminished laryngeal sensation, more drastic procedures, such as total laryngectomy or other procedures of tracheoesophageal separations, are required. The result is a permanent anatomic separation of the airway and digestive tract with the invariable loss of normal voice and respiration [55]. A valuable alternative to tracheoesophageal separation procedures is the laryngeal elevation in which the larynx is permanently fixed in the position that would normally be obtained during the pharyngeal phase of swallowing. The suspension of the larynx protects the airways from aspiration since the epiglottis is lowered over the laryngeal vestibule, and the larynx is pulled out of the way of the food bolus’ path. In addition, because the UES is attached to the larynx, anterior and cranial displacement of the larynx results in the opening of the esophageal inlet, thus facilitating the passage of the food bolus. Laryngeal elevation was found to be effective in dysphagic patients with severe aspiration caused by deficient laryngeal elevation, insufficient opening of the UES, and lack of pharyngeal constrictor activity. In these patients laryngeal elevation could be considered a valuable alternative to more drastic procedures [55].
References
Logemann JA (1995) Dysphagia: evaluation and treatment. Folia Phoniatr Logop 47:140–164
Odderson IR, Keaton JC, McKenna BS (1995) Swallow management in patients on an acute stroke pathway: quality is cost effective. Arch Phys Med Rehab 76:1130–1133
Logemann JA (ed) (1983) Evaluation and treatment of swallowing disorders. PRO-ED, Austin
Schindler O, Juliani E (1998) La videofluorografia nella diagnosi e nella terapia di disturbi di deglutizione. Giornale dell’Accademia di Medicina di Torino 161:266–277
Owens RE, Metz DE, Haas A (2000) Introduction to communication disorders. A life perspective. Allyn and Bacon, Needham Heights
Dua KS, Ren J, Barden E, Shaker R (1997) Coordination of deglutitive glottal function and pharyngeal bolus transit during normal eating. Gastroenterology 112:75–83
Dodds W (1989) The physiology of swallowing. Dysphagia 3:171–178
Martin-Harris B, Brodsky MB, Michel Y, Ford CL, Walters B, Heffner J (2005) Breathing and swallowing dynamics across the adult lifespan. Arch Otolaryngol Head Neck Surg 131:762–770
Jean A (2001) Brain stem control of swallowing: neuronal network and cellular mechanism. Physiol Rev 81:929–969
Miller AJ (2002) Oral and pharyngeal reflexes in the mammalian nervous system: their diverse range in complexity and their pivotal role of the tongue. Crit Rev Oral Biol Med 13:409–425
Mosier K, Bereznaya I (2001) Parallel cortical networks for volitional control of swallowing in humans. Exp Brain Res 140:280–289
Perlman AL, Schlze-Delrieu K (1997) Deglutition and its disorders. Singula Publising, San Diego
Ickenstein G (2011) Diagnosis and treatment of neurogenic dysphagia. Unimed, Bremen
Schindler A, Ginocchio D, Ruoppolo G (2008) What we don’t know about dysphagia complications? Rev Laryngol Otol Rhinol 129:75–78
Petroianni A, Ceccarelli D, Conti V, Terzano C (2006) Aspiration pneumonia. Pathophysiological aspects, prevention and management. A review. Panminerva Med 48:231–239
Gordon C, Hewer RL, Wade DT (1987) Dysphagia in acute stroke. BMJ 295:411–414
Lundy DS, Smith C, Colangelo L, Sullivan PA, Logemann JA, Lazarus CL, Newman LA, Murry T, Lombard L, Gaziano J (1999) Aspiration: cause and implications. Otolaryngol Head Neck Surg 120:474–478
Mark PE, Kaplan D (2003) Aspiration pneumonia and dysphagia in the elderly. Chest 124:328–336
Holas MA, Depippo KL, Reding MJ (1994) Aspiration and relative risk of medical complications following stroke. Arch Neurol 51:1051–1053
Hilker R, Poetter C, Findeisen N, Sobesky J, Jacobs A, Neveling M, Heis W (2003) Nosocomial pneumonia after acute stroke. Implications for neurological intensive care medicine. Stroke 34:975–981
Pikus L, Levine MS, Yang Y, Rubesin SE, Katzka DA, Laufer I, Gefter WB (2003) Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. Am J Radiol 180:1613–1616
Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, Loesche WJ (1998) Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia 13:69–81
Loesche WJ, Abrams J, Terpenning MS, Bretz WA, Dominguez BL, Grossman NS, Hildebrandt GH, Langmore SE, Lopatin DE (1995) Dental findings in geriatric populations with diverse medical backgrounds. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 80:43–54
Terpenning MS, Taylor GW, Lopatin DE, Kerr CK, Dominguez BL, Loesche WJ (2001) Aspiration pneumonia: dental and oral risk factors in an older veteran population. J Am Geriatr Soc 49:557–563
Yoneyama T, Yoshida M, Ohrui T, Mukaiyama H, Okamoto H, Hoshiba K, Ihara S, Yanagisawa S, Ariumi S, Morita T, Mizuno Y, Ohssawa T, Akagawa Y, Hasimoto K, Sasaki H (2002) Oral care reduces pneumonia in older patients in nursing homes. J Am Geriatr Soc 50:430–433
Kayser-Jones J, Schell ES, Porter C, Barbaccia JC, Shaw H (1999) Factors contributing to dehydration in nursing homes: inadequate staffing and lack of professional supervision. J Am Geriatr Soc 47:1187–1194
Low J, Wyles C, Wilkinson MB, Sainsbury R (2001) The effect of compliance on clinical outcomes for patients with dysphagia on videofluoroscopy. Dysphagia 16:123–127
Finestone HM, Foley NC, Woodbury MG, Greene-Finestone L (2001) Quantifying fluid intake in dysphagic stroke patients: a preliminary comparison of oral and nonoral strategies. Arch Phys Med Rehab 82:1744–1746
Whealn K (2001) Inadequate fluid intakes in dysphagic acute stroke. Clin Nutr 20:423–428
McGrail A, Kelchner LN (2015) Barriers to oral fluid intake: beyond thickened liquids. Rehabil Nurs 47:58–63
Murray J, Miller M, Doeltgen S, Scholten I (2014) Intake of thickened liquids by hospitalized adults with dysphagia after stroke. Int J Speech Lang Pathol 16:486–494
Rasheed S, Woods RT (2013) Malnutrition and quality of life in older people: a systematic review and meta-analysis. Ageing Res Rev 12:561–566
Foley N, Martin RE, Salter KL, Teasell RW (2009) A review of the relationship between dysphagia and malnutrition following stroke. J Rehabil Med 41:707–713
Prather AD, Smith TR, Poletto DM, Tavora F, Chung JH, Nallamshetty L, Hazelton TR, Rojas CA (2014) Aspiration-related lung diseases. J Thorac Imaging 29:304–309
Coates C, Bakheit AM (1997) Dysphagia in Parkinson’s disease. Eur Neurol 38:49–52
Perry L, Love CP (2001) Screening for dysphagia and aspiration in acute stroke: a systematic review. Dysphagia 16:7–18
Cichero JAY, Heaton S, Bassett L (2009) Triaging dysphagia: nurse screening for dysphagia in an acute hospital. J Clin Nurs 18:1649–1659
Mathers-Schmidt BA, Kurlinski M (2003) Dysphagia evaluation practices: inconsistencies in clinical assessment and instrumental examination decision-making. Dysphagia 18:114–125
Martino R, Pron G, Diamant NE (2004) Oropharyngeal dysphagia: surveying practice patterns of the speech-language pathologist. Dysphagia 19:165–176
Mann G (2002) The Mann assessment of swallowing ability. Singular, Thomson, Delmar Learning, Clifton Park
Langmore SE (2001) Endoscopic evaluation and treatment of swallowing disorders. Thieme, New York
Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, Maxwell R, Blair J (2008) MBS measurement tool for swallow impairment–MBSImp: establishing a standard. Dysphagia 23:392–405
Omari T, Rommel N (2014) Diagnosis of pharyngeal and UES dysphagia using HRM. In: Fox M, Kahrilas P, Pandolfino J, Zerbib F (eds) Manual of high resolution esophageal manometry. Uni-Med Verlag AG, Bremen, pp 77–88
Fattori B, Grosso M, Ursino F, Matteucci F, Mancini V, Rizza E, Mattone V, Mariani G, Nacci A (2007) Clinical applications of oro-pharyngo-oesophageal scintigraphy in the study of dysphagia. Acta Otorhinolaryngol Ital 27:192–199
Alfonsi E, Merlo IM, Ponzio M, Montomoli C, Tassorelli C, Biancardi C, Lozza A, Martignoni E (2010) An electrophysiological approach to the diagnosis of neurogenic dysphagia; implications for botulinum toxin treatment. J Neurol Neurosurg Psychiatry 81:54–60
Ebihara T, Takahashi H, Ebihara S, Okazaki T, Sasaki T, Watando A, Nemoto M, Sasaki H (2005) Capsaicin troche for swallowing dysfunction in older people. J Am Geriatr Soc 53:824–828
Schindler JS, Kelly JH (2002) Swallowing disorders in the elderly. Laryngoscope 112:589–602
Persaud R, Garas G, Silva S, Stamatoglou C, Chatrath P, Patel K (2013) An evidence-based review of botulinum toxin (Botox) applications in non-cosmetic head and neck conditions. J R Soc Med Short Rep 4:10
Srivanitchapoom P, Pandey S, Hallett M (2014) Drooling in Parkinson’s disease: a review. Parkinsonism Relat Disord 20:1109–1118
Masiero S, Briani C, Marchese-Ragona R, Giacometti P, Costantini M, Zaninotto G (2006) Successful treatment of long-standing post-stroke dysphagia with botulinum toxin and rehabilitation. J Rehabil Med 38:201–203
Parameswaran MS, Soliman AM (2002) Endoscopic botulinum toxin injection for cricopharyngeal dysphagia. Ann Otol Rhinol Laryngol 111:871–874
Murry T, Wasserman T, Carrau RL, Castillo B (2005) Injection of botulinum toxin a for the treatment of dysfunction of the upper esophageal sphincter. Am J Otolaryngol 26:157–162
Shin T, Tsuda K, Takagi S (1999) Surgical treatment for dysphagia of neuromuscular origin. Folia Phoniatr Logop 51:213–219
Buchholz DW (1995) Cricopharyngeal myotomy may be effective treatment for selected patients with neurogenic oropharyngeal dysphagia. Dysphagia 10:255–258
Shaker R et al (2013) Principles of deglutition: a multidisciplinary text for swallowing and its disorders. Springer, New York
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Mozzanica, F., Pizzorni, N., Schindler, A. (2017). Pathophysiology, Diagnosis, and Medical Management of Dysphagia. In: Arsava, E. (eds) Nutrition in Neurologic Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-53171-7_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-53171-7_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-53170-0
Online ISBN: 978-3-319-53171-7
eBook Packages: MedicineMedicine (R0)