Abstract
Interleukin-2 (IL-2) is a very well-known cytokine that has been studied for the past 35 years. It plays a major role in the growth and proliferation of many immune cells such NK and T cells. It is an important immunotherapy cytokine for the treatment of various diseases including cancer. Systemic delivery of IL-2 has shown clinical benefit in renal cell carcinoma and melanoma patients. However, its use has been limited by the numerous toxicities encountered with the systemic delivery. Intravenous IL-2 causes the well-known “capillary leak syndrome,” or the leakage of fluid from the circulatory system to the interstitial space resulting in hypotension (low blood pressure), edema, and dyspnea that can lead to circulatory shock and eventually cardiopulmonary collapse and multiple organ failure. Due to the toxicities associated with systemic IL-2, an aerosolized delivery approach has been developed, which enables localized delivery and a higher local immune cell activation. Since proteins are absorbed via pulmonary lymphatics, after aerosol deposition in the lung, aerosol delivery provides a means to more specifically target IL-2 to the local immune system in the lungs with less systemic effects. Its benefits have extended to diseases other than cancer. Delivery of IL-2 via aerosol or as nebulized IL-2 liposomes has been previously shown to have less toxicity and higher efficacy against sarcoma lung metastases. Dogs with cancer provided a highly relevant means to determine biodistribution of aerosolized IL-2 and IL-2 liposomes. However, efficacy of single-agent IL-2 is limited. As in general, for most immune-therapies, its effect is more beneficial in the face of minimal residual disease. To overcome this limitation, combination therapies using aerosol IL-2 with adoptive transfer of T cells or NK cells have emerged.
Using a human osteosarcoma (OS) mouse model, we have demonstrated the efficacy of single-agent aerosol IL-2 and combination therapy aerosol IL-2 and NK cells or aerosol IL-2 and interleukin 11 receptor alpha-directed chimeric antigen receptor-T cells (IL-11 receptor α CAR-T cells) against OS pulmonary metastases. Combination therapy resulted in a better therapeutic effect. A Phase-I trial of aerosol IL-2 was done in Europe and proved to be safe. Others and our preclinical studies provided the basis for the development of a Phase-I aerosol IL-2 trial in our institution to include younger patients with lung metastases. OS, our disease of interest, has a peak incidence in the adolescent and young adult years. Our goal is to complete this trial in the next 2 years.
In this chapter, we summarize the different effects of IL-2 and cover the advantages of the aerosol delivery route for diseases of the lung with an emphasis on some of our most recent work using combination therapy aerosol IL-2 and NK cells for the treatment of OS lung metastases.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
2.1 Introduction
Interleukin-2 (IL-2) is primarily one of the first cytokines that has been characterized to stimulate the growth of T cells. IL-2 was discovered in 1976, as a T-cell growth factor (TCGF), that was capable of growing and differentiating T-lymphocytes in vitro from undifferentiated bone marrow extracts [1]. Mier et al. later characterized the molecule and named it as “IL-2”. The introduction of IL-2 as an antitumor agent represented the first successful immunotherapy cancer treatment approach for humans [1]. Purified natural IL-2 formulations were produced by DuPont from the Jurkat T tumor cell line following phytohemagglutinin (PHA) stimulation and used for the treatment of patients with advanced cancer [2, 3]. The IL-2 gene was cloned in 1983, followed by the production of recombinant IL-2 (rIL-2) by E. coli. This stimulated preclinical research in animals and led to various IL-2 clinical trials for the treatment of metastatic disease. Thereafter, several strategies are being utilized to develop novel and more effective IL-2 formulations for cancer immunotherapy [4].
2.2 IL-2 Receptor and Signaling
IL-2 is a 15.5 kDa cytokine, which exerts its activity by binding with the IL-2 receptor. The IL-2 receptor consists of three components: the α chain (IL-2Rα), the β chain (IL-2Rβ), and the γ chain (IL-2Rγ). Different combinations of these three components have different affinities to IL-2, and their heterodimerization may vary according to the cell type and activation. The αβγ heterotrimer, βγ dimer, and α chain monomer have “high,” “intermediate,” and “low” affinities to IL-2, respectively. As depicted in Fig. 2.1, binding of IL-2 with its receptor induces tyrosine phosphorylation of numerous proteins, as kinases bind to the cytoplasmic domains of the receptor subunits. IL-2Rβ and IL-2Rγ heterodimerize to activate Janus kinases (JAK) 1 and 3, which are also associated with β and γ chain, respectively. Either of the Signal Transducers and Activators of Transcription family of Transcription factors 1 (STAT1), 3 (STAT3), and 5 (STAT5) in T cells, or 4 (STAT4) in NK cells, are recruited and bind to the phosphorylated IL-2 receptor, resulting in their dissociation and subsequent dimerization. STAT dimers are then translocated to the nucleus, resulting in the transcription of target genes. The proto-oncogene tyrosine-protein kinase Src may also bind to the phosphorylated receptor leading to activation of the extracellular signal-regulated kinases 1 (Erk-1) and 2 (Erk-2) and cell cycle progression. In addition, IL-2 can activate the phosphatidylinositol-3 (PI3K)—protein kinase B (Akt)-p70S6 kinase pathway, thus promoting cell survival and growth.
IL-2 and IL-2R signaling pathway. Interaction of IL-2 with β and γ receptors causes JAK1 and JAK3 phosphorylation, which in turn activates and dimerizes STAT proteins with subsequent nuclear translocation and transcription of various genes. IL-2 activation may also lead to the activation of PI3K-Akt or MEK-Erk pathway and lead to cell survival and cell cycle progression
IL-2 has been known to be involved in the growth and expansion of immune cells such as T cells, NK cells, and B cells. IL-2 can also stimulate the differentiation of CD4+ cells and CD8+ T cells into memory cells and terminally differentiated lymphocytes. Moreover, IL-2 plays an important role in augmenting the cytolytic activity of NK cells and T-lymphocytes.
2.3 Systemic IL-2 as an Immunotherapeutic Tool to Treat Malignant Diseases
Preliminary studies in animal models demonstrated that rIL-2 caused tumor regression of established pulmonary metastases and subcutaneous sarcoma tumors [5]. The preclinical findings from mice models were translated into clinical trials, where for the first time, 23 patients with various tumors, were treated with different regimens and doses of rIL-2 [2, 3]. Immunological changes such as cytokines and IFN-γ release were found in the serum; however, tumor regression was not seen when IL-2 was given alone perhaps because one of the major limitations of this therapy includes treatment-associated toxicity [6].
However, the ability of IL-2 to sustain the growth of T-lymphocytes encouraged the idea of the high-dose administration of IL-2 as a better immunotherapeutic strategy against cancer. IL-2 was shown to activate a population of lymphocytes, the lymphokine-activated killer cells (LAK), which have the unique property of killing the tumor cells irrespective of their histocompatibility expression status [7]. This phenomenon was further addressed by other investigators where exposure of peripheral blood mononuclear cells (PBMCs) or mouse splenocytes to supernatants containing IL-2 generated by LAK cells enhanced killing of various human cancer cell lines in vitro and primary human tumors in vivo [8,9,10,11]. Furthermore, preclinical studies using adoptive transfer of LAK cells expanded in vitro and given to mice with hepatic and pulmonary tumors caused significant antitumor in vivo activity [12,13,14,15,16]. These studies also showed that IL-2 augmented the in vivo activity of LAK cells in murine models of sarcomas and in one adenocarcinoma model. Therapeutic efficacy of IL-2 was shown to be dose dependent [15, 16].
Preclinical studies in animals prompted the use of high-dose IL-2 delivery in the clinical setting. The first study to discover the efficacy of high-dose IL-2 administration in mediating tumor regression was published in 1985 by Rosenberg et al. in patients with advanced cancer [17]. Twenty five patients with metastatic cancer were treated with escalating doses of IL-2 until toxicity was observed. The initial dose was 60,000 IU/kg followed by 180,000 or 600,000 IU/kg. Objective regression was observed in 11 of 25 patients. Four of seven patients with metastatic melanoma and 3 of 3 patients with renal cancer showed regression of metastatic disease. As the best durable responses were seen in melanoma and renal cell carcinoma, follow-up studies to investigate ways to improve IL-2 efficacy were only focused on these diseases. These initial studies uncovered the unique concept of immune modulation as a way to stimulate the immune system against tumor progression.
2.4 Efficacy of High-Dose IL-2 in Melanoma and Renal Cancer
A significant breakthrough in the IL-2 immunotherapy was highlighted by the Rosenberg et al. study at the National Cancer Institute, where 283 patients with metastatic melanoma or renal cancer were treated with high-dose IL2. High-dose IL-2 was delivered either as a bolus or as a continuous infusion [18]. IL-2 exerted significant antitumor effects, with 7% complete response and 10% partial responses in metastatic melanoma, and 7% complete response and 13% partial responses in metastatic renal carcinoma.
Similar efficacy was observed in further clinical trials using various high-dose IL-2 infusion schedules either alone or in combination with other cytokines or adoptive cell therapy [19,20,21,22,23]. Seven Phase-2 clinical trials of high-dose IL-2 for metastatic renal cancer patients resulted in an overall response of 14% and a complete response of 5% [23]. Due to the durability of responses from multicenter trials, United States Food and Drug administration (US-FDA) approved high-dose bolus IL-2 for the treatment of patients with metastatic renal cancer in 1992. IL-2 was the second immunotherapeutic agent approved for patients with cancer.
Similar multicenter trials were conducted by 22 institutions for the high-dose IL-2 delivery in patients with metastatic melanoma. From 272 patients, 6% had a complete response and 10% had a partial response [19]. Because high-dose IL-2 was shown to induce durable responses associated with disease-free survival in a small percentage of patients, in 1998, high-dose IL-2 was approved by the US-FDA for the treatment of metastatic melanoma.
However, because of the significant toxicities associated with high-dose IL-2, its application was limited to highly selected patients. Further combination regimens containing lower doses of IL-2 were investigated.
2.5 Systemic IL-2 as an Immunotherapeutic Approach for Sarcomas
No effective immunotherapies have thus far been identified for the treatment of sarcomas. However, building on additional immunotherapeutic advances made in other tumors has provided encouraging alternatives. The role of the immune system as a therapeutic approach to target cancer was first described in sarcomas where tumor regression was observed in a patient who developed postoperative infections [6]. This suggested that the ability of the body to respond to infections may also play a role in the antitumor response. As a consequence, few immunotherapy approaches have been investigated which included cytokines such as IL-2 and IFN-γ.
Initial studies using combination of IL-2 and LAK cells by Rosenberg et al. in patients with multiple malignancies demonstrated responses in metastatic renal cell cancer, melanoma, colorectal cancer, and non-Hodgkin’s lymphoma. However, six sarcoma patients in the study showed no response [24]. Another study included ten heavily pretreated pediatric patients with multiple malignancies including four osteosarcoma and two Ewing’s sarcoma patients. Variable responses were noted. Two osteosarcoma patients had durable complete responses with a median follow-up of 28 months and the two other had progressive disease suggesting that IL-2 efficacy was limited to only a subset of patients [25]. Further studies have been developed using combination therapy with IL-2. Nevertheless, no specific benefit of this cytokine alone has been described in sarcomas.
2.6 Limitations and Alternatives to Systemic IL-2 Administration
Systemic IL-2 administration provided high regression rates in patients with various advanced cancers. However, the high doses exerted a variety of serious dose-dependent systemic toxicities. One of the most predominant toxicity of IL-2 is the “capillary leak syndrome,” caused by extravasation of fluid into the organs, causing multi-organ damage. This translates into pulmonary congestion, hypotension, pre-renal azotemia, adult respiratory distress syndrome, and myocardial infarction [26]. These latter biologic effects are the result of IL-2 activation of NK and other immune cells, which in turn stimulate the release of inflammatory cytokines, which eventually leads to the so-called cytokine storm [27]. The cytokine storm is a major driver of the IL-2-mediated side effects, some of which include fever, chills, malaise, diarrhea, nausea, anemia, thrombocytopenia, eosinophilia, elevation of hepatic enzymes, and confusion [28]. An increase in the vascular permeability may be caused by IL-2 and CD-25-dependent endothelial cell damage and indirectly by the release of NK cell-mediated tumor necrosis factor-α (TNF-α) [29, 30].
High-dose IL-2 has also been linked to the development of eosinophilic myocarditis [31]. It can also enhance neutrophil chemotaxis, which makes patients who receive IL-2, more prone to Gram-positive and Gram-negative organism infections [32]. Due to the complexity of IL-2-induced toxicities, appropriate care and management of treated patients is crucial. Patients are initially screened to rule out any cardiac pathology, and those found to have a cardiac abnormality are not favored for IL-2 therapy. Early termination of treatment or interruption is followed when toxicity is noted.
Some other limitations are related to the fact that systemic IL-2 delivery has a very short half-life (15–30 min) and is rapidly excreted through the kidneys upon intravenous administration [30, 33,34,35,36]. Moreover, the route of administration also affects the absorption, biodistribution, and the half-life of IL-2. Intramuscular and subcutaneous IL-2 delivery results in higher systemic absorption as compared to intravenous administration [36].
Other methods of administration such as intraperitoneal, intrapleural, intrathecal, intraventricular, and inhalational delivery routes have emerged as they are more advantageous in providing a better local sustained effect in addition to a greater therapeutic efficacy [36]. Low-dose bolus, continuous infusions or subcutaneous delivery regimens have also been developed as an alternative approach to decrease the serious side effects of IL-2 [37]. However, low-dose IL-2 therapy was shown not to be effective as antitumor therapy. By contrary, it results in the expansion of immunosuppressive T regulatory (T-reg) cells, which can be detrimental to the patients. Lastly, methods to incorporate cytokine proteins into multi-lamellar liposomes have been developed. This methodology has provided an alternative way to maintain more stable and sustained cytokine levels locally within the tumor bed, which has translated in a better local therapeutic benefit [38,39,40].
2.7 Strategies to Enhance the Efficacy of IL-2 Therapy
Several strategies are being studied to enhance the therapeutic efficacy and decrease the systemic side effects elicited by IL-2.
2.7.1 IL-2/Anti-IL-2 Monoclonal Antibody (mAb) Complexes
In this approach, target tumor cell killing is enhanced as the anti-IL-2 mAb is fused with the IL-2 cytokine, which in turn recognizes and binds to the IL-2 receptors on immune cells. The increase in the IL-2/anti-IL-2 mAb conjugate formation allows for a better biological response [41, 42]. IL-2 antibody fusions, has also been used in several mouse models to direct IL-2 to cells expressing CD122 (IL-2-c-x), such as CD8+ T and NK cells [43,44,45,46,47]. Treatment with antibody fusion caused a robust T and NK cell expansion, which resulted in more effective antitumor immune responses [30, 45]. The advantages of antibody fusions compared to high-dose IL-2 administration are prolonged in vivo half-life, preferential stimulation of CD8+ T cells over T-regs and reduction in side effects [30, 45, 48, 49]. Currently, humanized and anti-human IL-2 antibodies (IL-2-c-x) are being developed for clinical testing.
2.7.2 IL-2 Muteins
Another approach was to design mutants of IL-2 to preferentially create binding to the IL-2 receptor chains responsible for cytotoxic T cells proliferation. An IL-2 “superkine” was generated by amino acid substitutions between positions 80 and 92. These modifications caused an enhanced binding to the IL-2Rβ and spare IL-2Rα binding [47]. In addition, the IL-2 “superkine” resulted in a more stable and flexible helix of the IL-2Rβ binding site, which allowed for a sustained phosphorylation and signaling. The end result translated in a greater cytotoxic T-cell production as opposed to T-regs, and a reduction in pulmonary edema in mice treated with the superkine.
An additional mutein, the no-α mutein, was designed to reduce the affinity of IL-2 to CD25, the IL-2 receptor responsible for T-reg proliferation, and maintain normal binding with IL-2Rβγ [50]. No-α mutein inhibited the metastasis of B16 melanoma variant and 3LL-D122 Lewis lung carcinoma in mice. It also increased NK cell activation and exerted less toxicities compared to wild-type IL-2.
As compared to IL-2/Anti-IL-2 mAb complexes, IL-2 muteins have a shorter half-life in vivo and hence require frequent administration. Also, IL-2 muteins contain epitopes that may be immunogenic. Patients could potentially develop antibodies that could inhibit IL-2 muteins biological activity [51].
2.7.3 IL-2 Fusion Proteins
An additional novel alternative to reduce the side effects associated with systemic IL-2 delivery is a fusion protein in which IL-2 is covalently linked to a specific inhibitory binding component separated by a protease cleavage site. The proteases overexpressed in the tumor microenvironment such as matrix metalloproteinases (MMPs), cleave the protease cleavage site of the fusion protein, which in turn allows for a local increase in IL-2 concentration and as a consequence immune cell activation. Immune cells can further produce more cytokines, thus accounting for a better antitumor effect. One example is Selectikine I or NHS-IL2LT, a fully humanized IL-2 fusion protein used for the treatment of solid tumors and B-cell non-Hodgkin’s lymphoma. It caused only mild grade 1 hypotension and vascular leak syndrome compared to wild-type IL-2 [52,53,54]. It is composed of a fully human de-immunized monoclonal antibody, NHS76, which binds free DNA from the dying tumor cells usually released after tumors are exposed to either radiation or chemotherapy. In addition, to decrease the toxicity effects of IL-2, a D20T mutation was introduced to the IL-2 motif. This mutation has little to no effect on the activity of free IL-2, is highly specific for activating the high-affinity IL-2 receptor, and has reduced binding to endothelial cells. In a Phase-I clinical trial in humans, the investigators were able to demonstrate that Selectikine has a favorable safety profile and induced the biological effects typical of IL-2 [54].
Two additional IL-2 fusion proteins, GA504 and GA501, comprise a fusion of the IL-2 mutein with a disrupted binding to CD25 and a humanized antibody targeting either carcinoembryonic antigen (CEA-GA504) or the familial adenomatous polyposis antigen (FAP-GA501). Both GA504 and GA501 were shown to cause strong activation and expansion (about 100-fold) of NK and CD8+ T cells and shift the CD4+:CD8+ ratio towards CD8+ T cells systemically in the peripheral blood and at the tumor site. These fusion proteins showed therapeutic efficacy in the murine colon adenocarcinoma model, MC38-CEA, and in the murine pancreatic carcinoma model, PancO2-CEA, as compared to the wild-type IL-2 [55]. Lastly, another IL-2 fusion protein, hu14.18-IL-2, was created in an effort to improve the antitumor effects of IL-2 or monoclonal antibody, ch14.18. It contains IL-2 molecularly linked to the carboxy terminus of the IgG heavy chains of the humanized hu14.18 monoclonal Ab, which recognizes disialoganglioside (GD2) on neuroblastoma and melanoma tumors [56, 57]. Intra-tumoral injection of hu14.18-IL2 led to increased NK and CD8+ T-cell infiltration and improved antitumor efficacy [57].
In summary, different strategies have provided different alternative benefits. However, the limitations of IL-2 to be considered as single-agent therapy still remain.
2.8 The Aerosol Route: A Novel Approach to Deliver IL-2
Drug concentration in lung tumors is low after systemic administration. This might be one of the major contributors of treatment failure [58]. In humans, drug concentration in the tumors appears to be a key parameter for drug efficacy [59]. The inhalation route discovered in the 1990s offers several advantages over systemic delivery. These include: (1) direct local high-dose concentrations in the lungs and airways with lower doses and fewer side effects and (2) the use of a noninvasive delivery system, which avoids first-pass metabolism of the drug through the liver. Moreover, the alveolar surface also provides a large surface area for fast systemic absorption [60]. Owing to the toxicities of the systemic delivery approach, aerosolized delivery of IL-2 has been studied as an alternative delivery route for the treatment of certain diseases limited to the lung.
A number of studies in renal cell carcinoma and melanoma have used aerosol IL-2 and confirmed that this route of administration can be safely administered and that it has modest efficacy against pulmonary metastases. Bronchoalveolar lavage recovered from patients treated by this approach demonstrated not only an increase in the number of lymphocytes but also an activated phenotype, indicating predominantly localized lymphocyte activation by the aerosol IL-2 treatment in the lung. Further studies demonstrated feasibility of this approach for the treatment of patients with various sarcoma types in addition to patients with immune deficiency diseases [61, 62]. These included patients with osteosarcoma (OS). Lung metastasis is the main cause of death in patients with OS. Aerosolized IL-2 offers an advantage as the target organ of treatment are the lungs. Biodistribution and pharmacokinetics of aerosolized IL-2 and IL-2 liposomes has been demonstrated in dogs with OS. Interestingly, nuclear medicine studies showed that lung retention times were significantly prolonged for both free IL-2 and IL-2 liposomes [38, 39]. Aerosol delivery of IL-2 was proved to be safe in dogs with spontaneous OS lung metastases [38, 39].
Our group has previously published work supporting the rationale and efficacy of aerosol IL-2 for the treatment of OS lung metastases. Using our LM7 OS mouse model, we demonstrated single-agent aerosol IL-2 efficacy against OS lung metastasis [63, 64]. Aerosolized IL-2 treatment given twice a week in the presence of micrometastatic disease, developed 5 weeks after i.v. injection of tumor cells, demonstrated therapeutic benefit. The number of macro- and micro-metastasis significantly decreased after 5 weeks of treatment with aerosol IL-2 at a dose of 2000 U/day twice a week. In addition, there was a significant increase in the number of apoptotic cells in the aerosol IL-2-treated lung metastases as compared to the PBS-treated groups as demonstrated by an increase in terminal deoxynucleotidyl transferase dUTP end labeling (TUNEL) staining (data not shown). Furthermore, aerosol IL2 caused an increase in the migration and activation of local immune cells in the lung. Fig. 2.2a, b shows that there was a significant increase in the number of mouse NK cells in the lung tumors of the aerosol IL-2-treated group compared to the aerosol PBS group as shown by an increase in the NKp46 immunohistochemistry (IHC) staining (p = 0.05). In addition, the number of macrophages was also significantly increased in the lung tumors from the aerosol IL-2-treated group as compared to the PBS control group as demonstrated by an increase in the F4/80 IHC staining (p = 0.05) (Fig. 2.2a, b).
Increase in the number of local NK cells and macrophages in osteosarcoma lung metastases from mice treated with aerosol IL-2. Representative images of (a) Significant increase of NK cells in LM7 OS lung metastases from mice treated with aerosol IL-2 as determined by NKp46 (brown) immunohistochemistry (IHC) staining (left top) and quantification (right top) p < 0.05 as compared to untreated control and; (b) Significant increase of macrophage infiltration in LM7 OS lung metastases from mice treated with aerosol IL-2 as demonstrated by F4/80 (brown) IHC staining (left bottom) and quantification (right bottom) p < 0.05 as compared to untreated control
The effect of aerosolized IL-2 on the local immune system in the lung was also demonstrated using immunocompetent mice. Mice received 2000 U/day of aerosol rhIL-2 or aerosol PBS for a total of 15 days. Single cell isolation from lungs of both treatment groups was performed and compared. Fluorescence-activated cell sorting (FACS) analysis depicted that the number CD3+, CD8+, and CD4+ cells significantly increased on day 13 following aerosol IL-2 treatment compared to aerosol PBS, and persisted for 3 days after terminating the treatment. IHC staining also showed a slight increase in T regulatory cells (T-regs), as demonstrated by forkhead box P3 (Foxp3) staining. However, the increase in Foxp3+ cells was smaller compared to the increase in CD4+ cells, indicating that T-regs do not account for the majority of the CD4+ cells induced by aerosol IL-2. The number of CD4+ and Foxp3+ cells returned back to the original levels, 1 month after terminating aerosol IL-2 treatment (data not shown). CM-Dil-labeled T cells injected intravenously localized and proliferated in the lung after aerosol IL-2 administration [65].
Lastly, survival studies using the human LM7 OS mouse model revealed an improved median survival time of mice treated with aerosol IL-2 as compared with aerosol PBS (89.5 versus 71 days; p = 0.03) [63].
In summary, our preclinical studies using an OS mouse model constitute real evidence of the immunotherapeutic benefit of this approach for the treatment of OS lung metastases and provide a strong rationale for the design of future clinical trials.
2.9 Different Combination Therapy Approaches Using IL-2
2.9.1 IL-2 in Combination with Cytokines and/or Chemotherapy
Several strategies to augment the immunotherapeutic effect of IL-2 have been studied. Combination treatments of IL-2 with IFN-α showed a limited advantage over high-dose IL-2 treatment, but served as a good outpatient management strategy [66, 67]. Furthermore, combination therapy of IL-2 with Cisplatin and Dacarbazine resulted in efficacious outcomes for metastatic melanoma patients [68]. IFN-α and IL-2 along with 5-Fluorouracil therapy resulted in 48% response rate in metastatic renal cancer patients [69]. Patients with metastatic melanoma, who did not respond initially to chemotherapy, showed better responses when high-dose IL-2 was added to the regimen [70].
2.9.2 IL-2 in Combination with Antibody Therapy
Low doses of IL-2 in combination with the anti-vascular endothelial growth factor A (VEGF-A), Bevacizumab, resulted in significant antitumor activity in patients with metastatic renal cell carcinoma [71].
2.9.3 IL-2 in Combination with Vaccines
Phase-III clinical trials using a GP-100 peptide vaccine, based on the ability of melanoma-derived tumor-infiltrating lymphocytes to recognize melanocyte-specific antigen gp-100 in combination with high-dose IL-2 resulted in better clinical activity than high-dose IL-2 alone in metastatic melanoma [72, 73]. In addition, Phase-II clinical trials using combination of modified vaccinia Ankara virus (MVA) expressing 5T4, a non-secreted membrane glycoprotein expressed on clear cell and papillary renal cell carcinoma, and IL-2 resulted in disease stabilization in patients with metastatic renal cell carcinoma [74]. In some instances, studies evaluating the combination of IL-2 as an immune adjuvant for a peptide vaccine against melanoma demonstrated IL-2 to likely be immunosuppressive in this setting, suggesting no additional benefit [75].
2.9.4 IL-2 in Combination with Adoptive T-Cell Therapy
Adoptive T-cell therapy has been described as an effective strategy to target metastases. However, a major barrier in adoptive transfer is the survival and persistence of the T cells in vivo. Combination with cytokines such as IL-2 has helped overcome this barrier. Hence, studies showed that combination of autologous T-cell adoptive transfer with high-dose IL-2 therapy with previous lymphodepletion using cyclophosphamide and fludarabine or total body irradiation, resulted in objective responses from 50 to 70% in metastatic melanoma patients [76, 77]. In these studies, the CD8+ lymphocytes obtained from tumors were clonally expanded using high-dose IL-2 initially for 5–6 weeks. Further expansion was performed using feeder cells and anti-CD3, in addition to high-dose IL-2, for an additional 2 weeks before the cells were reinfused to the patients [76]. Additional Phase-II clinical trials from the NCI showed that combination treatment of adoptive T-cell therapy with high-dose IL-2 resulted in a 50% clinical response rate and 13% durable responses with complete regression lasting more than 5 years in metastatic melanoma patients [78]. Similar clinical responses have also been shown in adoptive T-cell transfer trials in metastatic melanoma conducted at M.D. Anderson Cancer Center and Sheba Medical Center in Tel Hashomer, Israel [79,80,81]. Nevertheless, the widespread application of this treatment is limited by the complex procedure of T-cell expansion and the toxicities elicited by high-dose IL-2. Recently, a pilot trial was conducted by researchers at Danish Translational Research Center, using low-dose subcutaneous IL-2 injection along with adoptive T-cell transfer in melanoma patients. The results showed durable, complete responses with reduced toxicity, suggesting that low-dose IL-2 may be sufficient to prolong the survival of T cells [82].
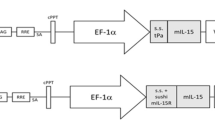
Our laboratory, previously demonstrated that intravenous delivery of genetically modified T cells expressing chimeric antigen receptor (CAR) targeting IL-11Rα, expressed in OS tumors, resulted in regression of OS lung metastasis. IL-11Rα-CAR-T cells were generated by ex vivo expansion in the presence of IL-2 and IL-15 and a feeder system of antigen-presenting cells (APCs) [83]. This therapy was further enhanced when aerosol IL-2 was added. Others’ and our findings suggest that the addition of IL-2 to T-cell therapy offers additional therapeutic benefit for the treatment of many tumors.
2.9.5 IL-2 in Combination with NK Cell Therapy
Although we and others have demonstrated that aerosolized IL-2 alone has therapeutic effect against some tumors, complete control of metastatic spread has not been achieved. In our preclinical studies using a human OS mouse model, complete eradication of OS lung metastasis was not attained with aerosol IL-2 alone as there was evidence of relapsed disease. In order to augment the effect of IL-2, we combined aerosolized IL-2 with adoptive NK cell immunotherapy.
NK cells possess an advantage over T cells as they can target tumor cells without the requirement of tumor-antigen recognition or major histocompatibility complex (MHC) restriction. However, infusion of NK cells also requires culture and ex vivo expansion, as the number of cells that are usually harvested is very small and not enough to lead to a good therapeutic outcome. Several platforms have been used to expand NK cells ex vivo using the feeder cells or APCs. Genetically modified K562 cells, like K562-membrane bound 15-41BBL, have had successful applications to expand allogeneic NK cells from patients treated for acute myelogenous leukemia, gastric cancer, and multiple myeloma [84, 85]. Denman and colleagues showed that membrane bound IL-21-expressing K562 APCs caused high rate of proliferation of NK cells and constitutes an additional successful approach [86]. Either approach is feasible and provides the advantage of not only expanding the NK cells but also enhancing their activity.
The addition of aerosolized IL-2 to the adoptive transfer of NK cells showed additional therapeutic advantage against OS lung metastasis in our human OS mouse model [64]. Aerosolized IL-2 increased the number of human NK cells in the lung. The combination therapy resulted in a greater decrease in the number and size of lung metastases and greater tumor cell apoptosis as compared to aerosol IL-2 or the administration of NK cells alone (Fig. 2.3a, b). Lastly, aerosol IL-2 and NK cells combination therapy led to an improved overall survival as the median survival of mice treated with the combination was 130 days as compared to 71 days for untreated mice. The improved survival demonstrated by the combination therapy was also superior to either IL-2 or NK cell treatment alone confirming the benefit of this approach [63]. Figure 2.4 summarizes our proposed model and expected outcomes.
Therapeutic benefit of the combination therapy aerosol IL-2 and NK cells for the treatment of OS lung metastases. (a, b) Aerosol IL-2 and NK cell combination therapy resulted in a significant decrease in the number of metastatic lung tumor nodules as compared to PBS control (p = 0.01), aerosol IL-2 (p = 0.03), or NK cell (p = 0.01) treatments alone in a human LM7 OS mouse model, (c, d). Aerosol IL-2 and NK cell combination therapy led to a significant increase in tumor cell apoptosis as determined by TUNEL staining (brown) as compared to either treatment alone, (p = 0.009-PBS, p = 0.02-aerosol IL-2 and p = 0.05-NK cells)
Schematic proposed model of the combination therapy aerosol IL-2 and NK cells with expected outcomes. Mice with micrometastatic disease were treated with aerosol IL-2 twice a week, along with infusion of human NK cell therapy (50 million cells). Aerosol IL-2 increased the number of infused NK cells proliferating in the lung leading to enhanced tumor cell apoptosis and improved survival
Additionally, clinical trials of adoptive transfer of in vitro-activated autologous NK cells have not demonstrated any significant clinical benefit in any of the tumors studied perhaps due to the self-tolerance of autologous NK cells [87, 88]. As a consequence, allogeneic NK cell infusions have been generally administered after immunosuppressive chemotherapy or after an HLA-mismatched transplantation.
Adoptively transferred human-mismatched (haploidentical) allogeneic NK cells have been shown to be more effective against AML and solid cancers such as metastatic melanoma, renal cell carcinoma, and Hodgkin’s disease [89,90,91]. A Phase-I trial of adoptive transfer of allogeneic natural killer cells in patients with advanced non-small cell lung cancer has demonstrated some benefit [92]. However, there are so far, no studies to address the benefit of combining IL-2 with the adoptive transfer of NK cells. We have an ongoing Phase-I study at M.D. Anderson Cancer Center, of aerosol IL-2 for the treatment of lung metastases to address the feasibility of this approach in the pediatric population and facilitate a future combination therapy trial using adoptive transfer of NK cells in addition to aerosolized IL-2.
2.10 Summary
IL-2 has been one of the most widely studied cytokines and immunotherapeutic agents for the treatment of various cancers and other diseases. IL-2 has been approved by the US-FDA for the treatment of melanoma and renal cell carcinoma. Due to the serious toxicities and limited efficacy of systemic IL-2, alternative unique approaches have been studied. In this chapter, we summarized all these approaches with a greater emphasis on aerosol IL-2 as a potential safe and feasible method capable of enhancing local and adoptive transfer of immune cells for the treatment of lung metastases. Successful completion of the Phase-I/II clinical trial of aerosol IL-2 will allow for further combination therapy trials using this less invasive and less toxic approach.
References
Taniguchi T, Minami Y. The IL-2/IL-2 receptor system: a current overview. Cell. 1993;73(1):5–8.
Lotze MT, et al. In vivo administration of purified human interleukin 2. I. Half-life and immunologic effects of the Jurkat cell line-derived interleukin 2. J Immunol. 1985;134(1):157–66.
Lotze MT, et al. In vivo administration of purified human interleukin 2. II. Half life, immunologic effects, and expansion of peripheral lymphoid cells in vivo with recombinant IL 2. J Immunol. 1985;135(4):2865–75.
Parkinson DR. Interleukin-2 in cancer therapy. Semin Oncol. 1988;15(6 Suppl 6):10–26.
Rosenberg SA, et al. Regression of established pulmonary metastases and subcutaneous tumor mediated by the systemic administration of high-dose recombinant interleukin 2. J Exp Med. 1985;161(5):1169–88.
D’Angelo SP, et al. Sarcoma immunotherapy: past approaches and future directions. Sarcoma. 2014;2014:391967.
Fagan EA, Eddleston AL. Immunotherapy for cancer: the use of lymphokine activated killer (LAK) cells. Gut. 1987;28(2):113–6.
Grimm EA, et al. Lymphokine-activated killer cell phenomenon. Lysis of natural killer-resistant fresh solid tumor cells by interleukin 2-activated autologous human peripheral blood lymphocytes. J Exp Med. 1982;155(6):1823–41.
Yang SC, et al. Clinical and immunomodulatory effects of combination immunotherapy with low-dose interleukin 2 and tumor necrosis factor alpha in patients with advanced non-small cell lung cancer: a phase I trial. Cancer Res. 1991;51(14):3669–76.
Yang SC, et al. Induction of lymphokine-activated killer cytotoxicity with interleukin-2 and tumor necrosis factor-alpha against primary lung cancer targets. Cancer Immunol Immunother. 1989;29(3):193–8.
Rosenberg SA, et al. Prospective randomized trial of high-dose interleukin-2 alone or in conjunction with lymphokine-activated killer cells for the treatment of patients with advanced cancer. J Natl Cancer Inst. 1993;85(8):622–32.
Mazumder A, Rosenberg SA. Successful immunotherapy of natural killer-resistant established pulmonary melanoma metastases by the intravenous adoptive transfer of syngeneic lymphocytes activated in vitro by interleukin 2. J Exp Med. 1984;159(2):495–507.
Mule JJ, et al. Adoptive immunotherapy of established pulmonary metastases with LAK cells and recombinant interleukin-2. Science. 1984;225(4669):1487–9.
Mule JJ, Shu S, Rosenberg SA. The anti-tumor efficacy of lymphokine-activated killer cells and recombinant interleukin 2 in vivo. J Immunol. 1985;135(1):646–52.
Lafreniere R, Rosenberg SA. Successful immunotherapy of murine experimental hepatic metastases with lymphokine-activated killer cells and recombinant interleukin 2. Cancer Res. 1985;45(8):3735–41.
Lafreniere R, Rosenberg SA. Adoptive immunotherapy of murine hepatic metastases with lymphokine activated killer (LAK) cells and recombinant interleukin 2 (RIL 2) can mediate the regression of both immunogenic and nonimmunogenic sarcomas and an adenocarcinoma. J Immunol. 1985;135(6):4273–80.
Rosenberg SA, et al. Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N Engl J Med. 1985;313(23):1485–92.
Rosenberg SA, et al. Treatment of 283 consecutive patients with metastatic melanoma or renal cell cancer using high-dose bolus interleukin 2. JAMA. 1994;271(12):907–13.
Atkins MB, et al. High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: analysis of 270 patients treated between 1985 and 1993. J Clin Oncol. 1999;17(7):2105–16.
Kruit WH, et al. Dose efficacy study of two schedules of high-dose bolus administration of interleukin 2 and interferon alpha in metastatic melanoma. Br J Cancer. 1996;74(6):951–5.
Keilholz U, et al. Interferon-alpha and interleukin-2 in the treatment of metastatic melanoma. Comparison of two phase II trials. Cancer. 1993;72(2):607–14.
de Gast GC, et al. Phase I trial of combined immunotherapy with subcutaneous granulocyte macrophage colony-stimulating factor, low-dose interleukin 2, and interferon alpha in progressive metastatic melanoma and renal cell carcinoma. Clin Cancer Res. 2000;6(4):1267–72.
Dutcher JP, et al. Interleukin-2-based therapy for metastatic renal cell cancer: the Cytokine Working Group experience, 1989-1997. Cancer J Sci Am. 1997;3(Suppl 1):S73–8.
Rosenberg SA, et al. Experience with the use of high-dose interleukin-2 in the treatment of 652 cancer patients. Ann Surg. 1989; 210(4):474–84; discussion 484–5.
Schwinger W, et al. Feasibility of high-dose interleukin-2 in heavily pretreated pediatric cancer patients. Ann Oncol. 2005;16(7):1199–206.
Rosenstein M, Ettinghausen SE, Rosenberg SA. Extravasation of intravascular fluid mediated by the systemic administration of recombinant interleukin-2. J Immunol. 1986;137(5):1735–42.
Panelli MC, et al. Forecasting the cytokine storm following systemic interleukin (IL)-2 administration. J Transl Med. 2004;2(1):17.
Lotze MT, et al. Clinical effects and toxicity of interleukin-2 in patients with cancer. Cancer. 1986;58(12):2764–72.
Boyman O, Sprent J. The role of interleukin-2 during homeostasis and activation of the immune system. Nat Rev Immunol. 2012;12(3):180–90.
Boyman O, Surh CD, Sprent J. Potential use of IL-2/anti-IL-2 antibody immune complexes for the treatment of cancer and autoimmune disease. Expert Opin Biol Ther. 2006;6(12):1323–31.
Schuchter LM, et al. Eosinophilic myocarditis associated with high-dose interleukin-2 therapy. Am J Med. 1990;88(4):439–40.
Klempner MS, et al. An acquired chemotactic defect in neutrophils from patients receiving interleukin-2 immunotherapy. N Engl J Med. 1990;322(14):959–65.
Donohue JH, Rosenberg SA. The fate of interleukin-2 after in vivo administration. J Immunol. 1983;130(5):2203–8.
Shaker MA, Younes HM. Interleukin-2: evaluation of routes of administration and current delivery systems in cancer therapy. J Pharm Sci. 2009;98(7):2268–98.
Konrad MW, et al. Pharmacokinetics of recombinant interleukin 2 in humans. Cancer Res. 1990;50(7):2009–17.
Anderson PM, Sorenson MA. Effects of route and formulation on clinical pharmacokinetics of interleukin-2. Clin Pharmacokinet. 1994;27(1):19–31.
Kammula US, White DE, Rosenberg SA. Trends in the safety of high dose bolus interleukin-2 administration in patients with metastatic cancer. Cancer. 1998;83(4):797–805.
Khanna C, et al. Interleukin-2 liposome inhalation therapy is safe and effective for dogs with spontaneous pulmonary metastases. Cancer. 1997;79(7):1409–21.
Khanna C, et al. Nebulized interleukin 2 liposomes: aerosol characteristics and biodistribution. J Pharm Pharmacol. 1997;49(10):960–71.
Dow S, et al. Phase I study of liposome-DNA complexes encoding the interleukin-2 gene in dogs with osteosarcoma lung metastases. Hum Gene Ther. 2005;16(8):937–46.
Rabinovitch A, et al. Combination therapy with sirolimus and interleukin-2 prevents spontaneous and recurrent autoimmune diabetes in NOD mice. Diabetes. 2002;51(3):638–45.
Shin JI, Park SJ, Kim JH. A possible role of leptin-associated increase in soluble interleukin-2 receptor diminishing a clinical response to infliximab in rheumatoid arthritis: comment on the article by Klaasen et al. Arthritis Rheum. 2011;63(9):2833–4; author reply 2834.
Tomala J, et al. In vivo expansion of activated naive CD8+ T cells and NK cells driven by complexes of IL-2 and anti-IL-2 monoclonal antibody as novel approach of cancer immunotherapy. J Immunol. 2009;183(8):4904–12.
Votavova P, Tomala J, Kovar M. Increasing the biological activity of IL-2 and IL-15 through complexing with anti-IL-2 mAbs and IL-15Ralpha-Fc chimera. Immunol Lett. 2014;159(1–2):1–10.
Krieg C, et al. Improved IL-2 immunotherapy by selective stimulation of IL-2 receptors on lymphocytes and endothelial cells. Proc Natl Acad Sci U S A. 2010;107(26):11906–11.
Letourneau S, et al. IL-2/anti-IL-2 antibody complexes show strong biological activity by avoiding interaction with IL-2 receptor alpha subunit CD25. Proc Natl Acad Sci U S A. 2010;107(5):2171–6.
Levin AM, et al. Exploiting a natural conformational switch to engineer an interleukin-2 ‘superkine’. Nature. 2012;484(7395):529–33.
Rojas G, et al. Deciphering the molecular bases of the biological effects of antibodies against interleukin-2: a versatile platform for fine epitope mapping. Immunobiology. 2013;218(1):105–13.
Rojas G, et al. Fine epitope specificity of antibodies against interleukin-2 explains their paradoxical immunomodulatory effects. MAbs. 2014;6(1):273–85.
Carmenate T, et al. Human IL-2 mutein with higher antitumor efficacy than wild type IL-2. J Immunol. 2013;190(12):6230–8.
Rotte A, et al. Immunotherapy of melanoma: present options and future promises. Cancer Metastasis Rev. 2015;34(1):115–28.
Gillies SD, et al. A low-toxicity IL-2-based immunocytokine retains antitumor activity despite its high degree of IL-2 receptor selectivity. Clin Cancer Res. 2011;17(11):3673–85.
Gubbels JA, et al. Ab-IL2 fusion proteins mediate NK cell immune synapse formation by polarizing CD25 to the target cell-effector cell interface. Cancer Immunol Immunother. 2011;60(12):1789–800.
Gillessen S, et al. A phase I dose-escalation study of the immunocytokine EMD 521873 (Selectikine) in patients with advanced solid tumours. Eur J Cancer. 2013;49(1):35–44.
Klein C. Novel CEA-targeted IL-2 variant immunocytokine for immunotherapy of cancer. J ImmunoTherapy Cancer. 2014;2(Suppl 2):18.
Hank JA, et al. Immunogenicity of the hu14.18-IL2 immunocytokine molecule in adults with melanoma and children with neuroblastoma. Clin Cancer Res. 2009;15(18):5923–30.
Shusterman S, et al. Antitumor activity of hu14.18-IL2 in patients with relapsed/refractory neuroblastoma: a Children’s Oncology Group (COG) phase II study. J Clin Oncol. 2010;28(33):4969–75.
Sharma S, et al. Development of inhalational agents for oncologic use. J Clin Oncol. 2001;19(6):1839–47.
Minchinton AI, Tannock IF. Drug penetration in solid tumours. Nat Rev Cancer. 2006;6(8):583–92.
Gagnadoux F, et al. Aerosolized chemotherapy. J Aerosol Med Pulm Drug Deliv. 2008;21(1):61–70.
Merimsky O, et al. Targeting pulmonary metastases of renal cell carcinoma by inhalation of interleukin-2. Ann Oncol. 2004;15(4):610–2.
Lorenz J, et al. Phase I trial of inhaled natural interleukin 2 for treatment of pulmonary malignancy: toxicity, pharmacokinetics, and biological effects. Clin Cancer Res. 1996;2(7):1115–22.
Guma SR, et al. Aerosol interleukin-2 induces natural killer cell proliferation in the lung and combination therapy improves the survival of mice with osteosarcoma lung metastasis. Pediatr Blood Cancer. 2014;61(8):1362–8.
Guma SR, et al. Natural killer cell therapy and aerosol interleukin-2 for the treatment of osteosarcoma lung metastasis. Pediatr Blood Cancer. 2014;61(4):618–26.
Huang GX, et al. Genetically modified T cells targeting interleukin-11 receptor alpha-chain kill human osteosarcoma cells and induce the regression of established osteosarcoma lung metastases. Cancer Res. 2012;72(1):271–81.
Atkins MB, et al. Randomized phase II trial of high-dose interleukin-2 either alone or in combination with interferon alfa-2b in advanced renal cell carcinoma. J Clin Oncol. 1993;11(4):661–70.
Sparano JA, et al. Randomized phase III trial of treatment with high-dose interleukin-2 either alone or in combination with interferon alfa-2a in patients with advanced melanoma. J Clin Oncol. 1993;11(10):1969–77.
Keilholz U, et al. Results of interleukin-2-based treatment in advanced melanoma: a case record-based analysis of 631 patients. J Clin Oncol. 1998;16(9):2921–9.
van Herpen CM, et al. Immunochemotherapy with interleukin-2, interferon-alpha and 5-fluorouracil for progressive metastatic renal cell carcinoma: a multicenter phase II study. Dutch Immunotherapy Working Party. Br J Cancer. 2000;82(4):772–6.
Tarhini AA, et al. A phase 2 trial of sequential temozolomide chemotherapy followed by high-dose interleukin 2 immunotherapy for metastatic melanoma. Cancer. 2008;113(7):1632–40.
Panares RL, Garcia AA. Bevacizumab in the management of solid tumors. Expert Rev Anticancer Ther. 2007;7(4):433–45.
Bakker AB, et al. Melanocyte lineage-specific antigen gp100 is recognized by melanoma-derived tumor-infiltrating lymphocytes. J Exp Med. 1994;179(3):1005–9.
Smith FO, et al. Treatment of metastatic melanoma using interleukin-2 alone or in conjunction with vaccines. Clin Cancer Res. 2008;14(17):5610–8.
Kaufman HL, et al. Phase II trial of Modified Vaccinia Ankara (MVA) virus expressing 5T4 and high dose interleukin-2 (IL-2) in patients with metastatic renal cell carcinoma. J Transl Med. 2009;7:2.
Block MS, et al. Pilot study of granulocyte-macrophage colony-stimulating factor and interleukin-2 as immune adjuvants for a melanoma peptide vaccine. Melanoma Res. 2011;21(5):438–45.
Dudley ME, et al. Adoptive cell therapy for patients with metastatic melanoma: evaluation of intensive myeloablative chemoradiation preparative regimens. J Clin Oncol. 2008;26(32):5233–9.
Dudley ME, et al. Cancer regression and autoimmunity in patients after clonal repopulation with antitumor lymphocytes. Science. 2002;298(5594):850–4.
Restifo NP, Dudley ME, Rosenberg SA. Adoptive immunotherapy for cancer: harnessing the T cell response. Nat Rev Immunol. 2012;12(4):269–81.
Radvanyi LG, et al. Specific lymphocyte subsets predict response to adoptive cell therapy using expanded autologous tumor-infiltrating lymphocytes in metastatic melanoma patients. Clin Cancer Res. 2012;18(24):6758–70.
Besser MJ, et al. Minimally cultured or selected autologous tumor-infiltrating lymphocytes after a lympho-depleting chemotherapy regimen in metastatic melanoma patients. J Immunother. 2009;32(4):415–23.
Besser MJ, et al. Clinical responses in a phase II study using adoptive transfer of short-term cultured tumor infiltration lymphocytes in metastatic melanoma patients. Clin Cancer Res. 2010;16(9):2646–55.
Ellebaek E, et al. Adoptive cell therapy with autologous tumor infiltrating lymphocytes and low-dose interleukin-2 in metastatic melanoma patients. J Transl Med. 2012;10:169.
Huang G, et al. Genetically modified T cells targeting interleukin-11 receptor alpha-chain kill human osteosarcoma cells and induce the regression of established osteosarcoma lung metastases. Cancer Res. 2012;72(1):271–81.
Garg TK, et al. Highly activated and expanded natural killer cells for multiple myeloma immunotherapy. Haematologica. 2012;97(9):1348–56.
Fujisaki H, et al. Expansion of highly cytotoxic human natural killer cells for cancer cell therapy. Cancer Res. 2009;69(9):4010–7.
Denman CJ, et al. Membrane-bound IL-21 promotes sustained ex vivo proliferation of human natural killer cells. PLoS One. 2012;7(1):e30264.
Krause SW, et al. Treatment of colon and lung cancer patients with ex vivo heat shock protein 70-peptide-activated, autologous natural killer cells: a clinical phase i trial. Clin Cancer Res. 2004;10(11):3699–707.
Parkhurst MR, et al. Adoptive transfer of autologous natural killer cells leads to high levels of circulating natural killer cells but does not mediate tumor regression. Clin Cancer Res. 2011;17(19):6287–97.
Ruggeri L, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science. 2002;295(5562):2097–100.
Miller JS, et al. Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in patients with cancer. Blood. 2005;105(8):3051–7.
Curti A, et al. Successful transfer of alloreactive haploidentical KIR ligand-mismatched natural killer cells after infusion in elderly high risk acute myeloid leukemia patients. Blood. 2011;118(12):3273–9.
Iliopoulou EG, et al. A phase I trial of adoptive transfer of allogeneic natural killer cells in patients with advanced non-small cell lung cancer. Cancer Immunol Immunother. 2010;59(12):1781–9.
Acknowledgements
The authors would like to acknowledge Dr. Eugenie S. Kleinerman for her continuous mentorship, encouragement, and support and Dr. Sergei R. Guma for allowing us to share some of his studies to further inform the scientific community.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Dhupkar, P., Gordon, N. (2017). Interleukin-2: Old and New Approaches to Enhance Immune-Therapeutic Efficacy. In: Naing, A., Hajjar, J. (eds) Immunotherapy. Advances in Experimental Medicine and Biology, vol 995. Springer, Cham. https://doi.org/10.1007/978-3-319-53156-4_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-53156-4_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-53155-7
Online ISBN: 978-3-319-53156-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)