Abstract
Amphetamine and cocaine are drugs of abuse worldwide consumed for their stimulant properties in the central nervous system. They mainly potentiate noradrenergic and dopaminergic neurotransmission and induce long-term changes in multiple neuronal circuits, modifying the future responses to pharmacological or non-pharmacological challenges. The altered neuronal connectivity induced by psychostimulants has long been studied in reward processing brain areas and in behavioral responses. Different neurotransmitter systems are involved in these responses, including the neuropeptide angiotensin II. Locally produced brain angiotensin II, acting through AT1 receptors, plays an important role in the modulation of central dopaminergic neurotransmission. Dopamine-innervated areas such as caudate putamen, nucleus accumbens, substantia nigra, hypothalamus, and ventral pallidum express high AT1 receptor density. Our recent studies show the role of angiotensin II AT1 receptors in the development of neuroadaptative behavioral and neurochemical changes induced by amphetamine. Moreover, we found alterations in the components of the renin angiotensin system (RAS) and in the functionality of AT1 receptors after amphetamine exposure. The evidence presented in this chapter highlight the RAS as a neuromodulatory system of superior brain activities, and further validate Angiotensin II involvement in amphetamine-induced alterations through AT1 receptor activation. The AT1 receptor blockers are currently and safely used in clinic for different pathologies, so they would be prominent candidates for pharmacological treatment in pathologies related to altered dopamine neurotransmission, such as drug addiction, schizophrenia, or even depression.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Psychostimulant Pharmacology
D-amphetamine and cocaine are drugs known as psychostimulants. These drugs have a common pharmacological target as indirect catecholaminergic agonists. They produce their stimulant and psychotic effects by increasing synaptic concentrations of dopamine (DA) through inhibition of reuptake and potentiation of presynaptic release. The potency of the psychotogenic effects induced by psychostimulants is associated with the dopaminergic agonist action, although no consistent correlation has been found between symptoms and measures of DA neuronal activity [1,2,3]. However, the physiological actions induced by drug administration extend beyond the transient changes in synaptic concentrations of DA, since a temporal dissociation exists between behavioral response and plasma drug concentrations [1,2,3].
Neuroadaptative Changes Associated with Psychostimulants
Repeated administration of stimulants may produce a supersensitive condition in the central nervous system by upward regulation of postsynaptic DA receptors [4, 5]. This is a consequence of presynaptic DA depletion and lowered tonic basal DA levels after the increased dopaminergic synaptic activation induced by psychostimulants. Furthermore, sustained dopaminergic activation could develop autoreceptor subsensitivity associated with a reduced inhibition of presynaptic DA synthesis and release [6]. These events could lead to increased DA neurotransmission due to dysregulation of presynaptic and postsynaptic mechanisms.
At behavioral level, the supersensitivity induced by psychostimulants is a phenomenon termed behavioral sensitization, characterized by an enhanced response to psychostimulants that relies on neuroplastic changes. These changes are time-dependent and involve the motivational behavior circuitry of the brain [7, 8]. The behavioral sensitization involves changes associated with long-lasting hyperactivity of the mesolimbic dopaminergic pathway [8, 9]. Moreover, considerable evidence indicates that exposure to a drug of abuse does not need to be repeated to induce locomotor sensitization. In this regard, it has been described in mouse and rat studies that a single exposure to psychostimulants (cocaine or amphetamine) induces behavioral sensitization [10, 11]. The sensitization process presents two temporally distinct phases: induction and expression [8, 12]. The mesocorticolimbic dopaminergic projections play a key role in both described phases of amphetamine-induced behavioral sensitization. In this respect, it is known that sensitization can be induced by microinjection of amphetamine into the ventral tegmental area; meanwhile, its expression is associated with time-dependent adaptations in forebrain DA-innervated areas, such as the nucleus accumbens (NAc) and caudate putamen (CPu) [13].
In contrast with observations of enhanced DA neurotransmission within the NAc and CPu in response to the repeated administration of psychostimulants, the DA response in the medial prefrontal cortex (mPFC) has been reported to be decreased in animals sensitized to cocaine [14,15,16]. Moreover, the evidence suggests that the dorsal mPFC, which provides glutamatergic afferents specifically to NAc core, enhances the expression of behavioral sensitization to cocaine by increasing glutamate transmission [17]. Oppositely, lesions in the prelimbic area of the mPFC were shown to affect the development of sensitization to the locomotor activating effects of cocaine [18]. Furthermore, a negative relationship has been described between DA levels in the ventral and dorsal mPFC and locomotor activity in response to the acute systemic administration of cocaine. Meanwhile, in the shell of the NAc a positive relationship between DA levels and locomotor response to cocaine has been described [19]. Based on the available evidence, it seems that DA tone in the mPFC is involved in the balance between hyper- or hypo-stimulation states.
Schizophrenia and Interactions with Psychostimulants
The neurobiological bases of schizophrenia and chronic stimulant drug effects suggest the potential for their interaction. Schizophrenic patients who abuse psychostimulant drugs are susceptible to incur several types of risk because they can present symptom exacerbations that otherwise might not have occurred. Beyond this, given the occurrence of behavioral sensitization and neurotoxic effects, chronic stimulant use could conceivably exacerbate the pathophysiology of the disease, resulting in an acceleration of disease progress and/or an increase in the severity of symptoms. In addition, the antipsychotic treatment response might be altered in an unfavorable direction. However, schizophrenic patients use smaller quantities of drugs of abuse than healthy drug abusers. Even though the dose–response parameters could be different for schizophrenic patients, the concern whether chronic stimulant abuse in healthy persons can induce a schizophrenia-like condition persisting without stimulant abuse is currently unsettled. In this regard, the evidence suggests that the onset of schizophrenia may be precipitated in pre-psychotic or latent schizophrenic patients, but not directly caused by psychostimulant abuse [3, 20].
Role of Angiotensin in Brain Excitability
Currently, it is well established that the brain possesses its own and distinct angiotensin system [21]. The pharmacological manipulation of this system may modulate a number of events coordinated by the central nervous system such as drinking behavior [22], hormone release [23], anxiety [24,25,26], cognition [27,28,29,30], locomotor activity [31, 32], and stereotypy [32, 33]. The pharmacological and molecular evidence indicates the presence of at least two receptors for the octapeptides angiotensin II AT1 and AT2 [34, 35]. These receptor subtypes mediate responses evoked by angiotensin II, although to date the majority of the known physiological responses evoked by angiotensin II appear to be mediated via the AT1 receptor [36, 37].
The immunohistochemical and neuropharmacological evidence suggests that angiotensin II and its derived peptides angiotensin III and/or IV are neurotransmitters or neuromodulators in specific neuronal pathways in the brainstem, forebrain, and hypothalamus. AT1 receptor activation by angiotensin II elicits neuronal depolarization by affecting the permeability of different ion channels. In this regard, AT1 receptor mediates an inhibition of potassium channel [38] or opening of a non-selective sodium-calcium channel [39]. The activation of these different signaling pathways inducing depolarization would reflect the fine tuning level of the overall cellular activation. The electrophysiological evidences show that angiotensin II applied in vitro induces a firing increase in the median preoptic neurons [40], paraventricular nucleus of the hypothalamus [41], basolateral nucleus of amygdala [42], central nucleus of amygdala [43] and the hippocampus [44, 45]. Similarly to Angiotensin II, angiotensin IV exerts stimulating effects on the firing rate and burst discharges in the hippocampus [45]. The different distribution of the co-localized AT1 and AT4 receptors in the same hippocampal neuron could be a reason for the observed difference in excitation produced by either angiotensin II or angiotensin IV respectively. The excitatory effects induced by angiotensin II are due to presynaptic AT1 receptor activation and modulatory effects on classical neurotransmitter release [38], or activation of postsynaptic AT1 receptors that induces membrane depolarization and an inward current [40]. It has been found that angiotensin II and angiotensin IV exert dual effects on the dorsal lateral geniculate nucleus [46], amygdala [42] and hippocampus [44, 45], but the inhibitory role predominates in the locus coeruleus [47], superior colliculus [48], and septum [49].
In many brain areas, there is an interaction between angiotensinergic and glutamatergic systems, and this interaction could explain in part the inhibitory effects induced by angiotensin II. In this regard, angiotensin II modulates the response to glutamate in the superior colliculus acting through AT1 and AT2 receptors, while visual potentials evoked by glutamate receptor agonist have been shown to be attenuated by postsynaptic AT1 receptor activation only [50]. In the locus coeruleus, angiotensin II blocked the excitation evoked by glutamate [47]. Moreover, it has been described that angiotensin inhibited the NMDA- and/or kainate-evoked increase in the firing rate of dorsal lateral geniculate nucleus, and the AT1 receptors may be involved [46]. In-vivo studies show that angiotensin II modulates the baroreceptor reflex response, acting on the area postrema, and in an electrophysiological study, an inhibitory effect was found in this area, induced by angiotensin II. Neurons from the area postrema are in reciprocal connection with the nucleus tractus solitarius, a region involved in integration of baroreceptor reflex response [51]. Moreover, angiotensin II and III inhibit the neurons of nucleus reticularis ventrolateralis, and subsequently the spontaneous baroreceptor reflex response. This action could be reversed by AT2 receptor antagonists [52]. The presented evidence strongly suggests angiotensin II and derived peptides as modulators of neuronal activity.
Relationship Between Dopamine and Angiotensin II
There is a large body of evidence supporting the relationship between brain angiotensin II and catecholamine systems [53, 54]. This interaction could be involved in some central actions of angiotensin II such as cardiovascular control, dipsogenesis, and complex behaviors, supporting the idea that drugs able to modulate brain angiotensin II may be useful in regulating central DA activity. In this respect, high AT1 receptor density has been described in DA-rich regions, in CPu, hypothalamus, NAc, and ventral pallidum [55, 56]. The evidence shows that brain angiotensin II increases the DA release in CPu and NAc [57]. Moreover, it has been found that in CPu the DA release induced by angiotensin II is mediated by AT1 receptors [55], and the stereotype behavior induced by apomorphine (DA receptor agonist) could also be blocked by AT1 receptor antagonists [58].
Given the established role of the nigro-striatal dopamine system in the control of movement, and the fact that angiotensin II enhances the release of dopamine in the rat striatum (that provides a neurochemical mechanism underlying the modulation of locomotor activity and other DA mediated behaviors) we may hypothesize that the angiotensin system could be a useful tool for pharmacological manipulation of the DA system (see above).
The available evidence suggests that DA and angiotensin II systems directly regulate against each other in the striatum and substantia nigra of rodents [59, 60]. In this regard, reserpine-induced DA depletion produced a significant increase in the expression of AT1 and AT2 receptors, which decreased when the dopaminergic function was restored. The same phenomenon was observed after dopaminergic denervation with 6-hydroxydopamine. In this case, the administration of L-Dopa decreased AT1 and increased AT2 receptor density [59]. Moreover, changes in angiotensin II levels may affect angiotensin II receptor density. In this regard, transgenic rats with very low levels of brain angiotensin II showed increased AT1 receptors [61]. The Labandeira-Garcia group found evidence suggesting that AT1 receptors expression is closely related to DA levels through direct (DA and AT1 receptors) and indirect (changes in angiotensin II levels) mechanisms [60].
Brain Angiotensin II and Cocaine
Although it is generally recognized that cocaine has a potentially toxic effect upon the cardiovascular system, the process by which this occurs is extremely complex and is not, at present, fully understood. Acutely, cocaine administration has been associated with a wide range of effects, including increases in heart rate and blood pressure, coronary vasoconstriction, increases in myocardial contractility, and decreases in ejection fraction [62]. Based on the available evidence, it seems that these effects are associated with cocaine-induced increases in sympathetic output subsequent to potentiation of monoamines. Consistent with its local anesthetic properties, mediated by voltage-gated sodium channel blockade, cocaine also may depress heart function. These ‘opposing’ effects may create significant imbalances in oxygen demand and supply, which, particularly in a cocaine-induced prothrombotic context, have the potential to significantly degrade the electrical and mechanical functioning of the heart [63]. Findings in chronic cocaine abusers include hypertension, left ventricular hypertrophy, malignant arrhythmias, myocardial ischemia, and cardiomyopathy [64]. The clinical etiologic context is complex, as it is necessary to disentangle the effects of cocaine from cardiovascular risk factors associated with a drug-abusing lifestyle, including different factors such as poor diet and intravenous drug use [65].
Angiotensin I converting enzyme (ACE), the main angiotensin II generating enzyme, is an essential part of the renin–angiotensin system (RAS) present in the brain. Interestingly, research points to central nervous system effects of ACE-inhibitors that may bear upon their potential utility for the treatment of cocaine addiction. A number of studies in animals point to activation of the hypothalamic–pituitary–adrenal (HPA) axis by drugs of abuse, which may affect the drug’s positive reinforcement properties, as well as mediate anxiogenic-like behavior associated with drug withdrawal [66]. There is evidence suggesting that cocaine withdrawal is associated with activation of corticotropin-releasing factor (CRF) [67]. Extrapolated to a clinical population, CRF release may mediate the abstinence-associated dysphoria, as well as the stress-related relapse to cocaine [68]. It has been found that ACE-inhibitors in cocaine-abusing patients decrease CRF release [69]. Conversely, angiotensin II increases CRF release [70]. Decrease in CRF by ACE-inhibitors could potentially play a role in reducing stress-related relapse to cocaine [65].
As was described above, DA release in the striatum of the rat can be directly affected by angiotensin II [71, 72] or through a metabolite-like angiotensin IV [55, 73, 74]. Angiotensin II increases CRF release [75], an effect also induced by cocaine withdrawal [76]. The available evidence supports the importance and possible implications of the complete RAS in the brain, where it acts to regulate a number of physiological processes (e.g., cardiovascular maintenance, memory, fluid intake, energy balance). ACE-inhibitors are ligands that form a complex with Zn2+ at the active site of ACE. ACE-inhibitors are effective in reducing blood pressure in hypertensive individuals, as they block the conversion of angiotensin I to angiotensin II and reduce the degradation of bradykinin. It has been described that ACE-inhibitors are able to increase dopamine release in the striatum, an effect probably mediated by the opioid system [65]. As they could indirectly block CRF release and directly block angiotensin II production, ACE-inhibitors have been suggested to be used in the treatment of cocaine abuse [65]. Moreover, it has been observed that chronic administration of ACE-inhibitors increased the turnover of dopamine in the striatum of rats [77]. Similarly, it has been found that sodium depletion, known as a treatment that induces RAS activation, is able to induce behavioral cross-sensitization with cocaine, showing the involvement of angiotensin II in the neuroplastic events induced by this psychostimulant [78].
The central nucleus of the amygdala (CeA) plays a critical role in integrating sympathetic and behavioral responses to stress and the stimulation of the CeA produces increases in blood pressure and heart rate [79]. The CeA also contains angiotensin II, ACE, and angiotensin receptors [80]. In addition, CRF-like immunoreactivity exists in the CeA [81, 82]. Moreover, it has been described that microinjection of angiotensin II in the CeA elicits a pressor response, whereas CRF evokes both an increase in plasma catecholamines and arterial pressure [83, 84]. Cocaine and acute stress increase CRF and/or its mRNA in the amygdala [68, 85, 86]. Therefore, multiple studies suggest that angiotensin II and CRF are key neurotransmitters in the CeA involved in regulation of sympathetic and hemodynamic responses to stress [79].
Brain Angiotensin II and Amphetamine
Long-Lasting Changes in Brain Angiotensin II Involved in the Neuroadaptive Responses to Amphetamine
A direct relationship between angiotensin II and behavioral sensitization induced by amphetamine was found in our laboratory. In this regard, it was shown that angiotensin II AT1 receptors are involved in the development of behavioral and neurochemical sensitization induced by a single exposure to amphetamine [87, 88]. Moreover, it was recently reported by our group that amphetamine exposure induces persistent alterations in brain angiotensin II components within CPu and NAc [89]. In this respect, both studied regions, CPu and NAc, presented long-lasting increase in AT1 receptor density after amphetamine exposure but in CPu, a significant decrease in angiotensinogen (angiotensin II precursor) was found. The available evidence suggests a relationship between the AT1 receptors and angiotensinogen in the brain. In this regard, it has been described that the administration of AT1 receptor antagonists induced widespread up-regulation of angiotensinogen mRNA levels with low doses and down-regulation with higher doses [90] (Fig. 15.1). Meanwhile, other authors found a decrease in angiotensinogen, angiotensin II, and angiotensin-converting enzyme mRNA levels in basal ganglia after systemic administration of candesartan, an AT1 receptor antagonist [91]. This evidence supports the view that manipulations of AT1 receptors could induce changes in brain angiotensinogen levels. The results obtained for our group showing amphetamine-induced decrease in angiotensinogen in CPu could be related to an overstimulation of AT1 receptors. In this regard, it was also found that the expression of behavioral sensitization was attenuated by AT1 receptor blockade in CPu [89]. In NAc, no changes were observed in angiotensinogen after amphetamine exposure, and the AT1 receptor antagonists were ineffective in preventing the expression of behavioral sensitization induced by the psychostimulant [89]. Even though the two brain areas evaluated are rich in dopaminergic terminals and are strongly related to psychostimulants neuroadaptive responses, they show differential DA release in response to electrical stimulation. Moreover, the DA release in the CPu is not regulated by dopamine autoreceptor activation, in contrast to NAc [92]. Two mechanisms have been suggested for regulating DA release in the projections of dopaminergic systems: a phasic release regulated by depolarization of dopaminergic nerve cell bodies, and a tonic regulation of DA release independent of electrical activity of these neurons [93]. The tonic influences are more significant in the CPu than in the NAc [92]. This last fact is in agreement with the evidence showing the tonic influence of angiotensin II on DA synthesis and release in CPu through AT1 receptors [55, 94]. However, CPu and NAc seem to have different roles in the neuroadaptive responses to drugs of abuse [95, 96].
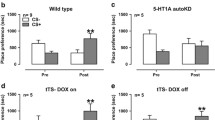
AT1 receptors are involved in the altered neuronal activation induced by amphetamine exposure in response to different challenges. Angiotensin II (400 pmol) was administered intracerebrally and amphetamine (0.5 mg/kg) intraperitoneally. The neuronal activation was measured as Fos expression in the two brain areas from animals exposed to amphetamine 21 days before, pretreated with AT1 receptor antagonist (CV) or vehicle. The values were calculated as percentage respect control group (vehicle-saline animals exposed to saline challenge) and expressed as mean ± SEM. Two-way ANOVA analysis, *p < 0.05, n = 7–10
Repeated Amphetamine Exposure Modifies Brain Angiotensin II AT1 Receptor Functionality
Sodium depletion, which activates RAS, develops cross-sensitization effects leading to enhanced locomotor activity responses to amphetamine [97]. These experiments indicate that treatments implying RAS activation show reciprocal behavioral cross-sensitization with psychostimulants. In relation to these findings, our group, using a protocol of repeated amphetamine, found long-lasting changes affecting brain response to angiotensin II [98]. These alterations were revealed by exogenously intracerebrally injected angiotensin II in conscious rats, known to produce a marked increase in water and sodium intake, as well as an increased natriuresis [98]. All these effects have been previously and exhaustively described [99,100,101,102,103]; however, the results obtained in our study showed that previous exposure to repeated amphetamine administration modified the described effects of angiotensin II i.c.v. on these parameters in a long-term manner (1 week after amphetamine withdrawal) [104]. In this respect, it was found that repeated amphetamine exposure markedly decreased the sodium intake induced by angiotensin II; meanwhile, water intake was unaffected. Sodium intake behavior is likely to reflect the differential regulation of intracellular signaling pathways. In this regard, it has been hypothesized that differential AT1 receptors signaling pathways play separable roles in water and saline intake stimulated by angiotensin II [105, 106]. There are results that support this hypothesis, demonstrating that G protein-dependent pathways appear to be more important for water intake stimulated by angiotensin II, whereas G protein-independent pathways may be more relevant for angiotensin II-stimulated sodium intake [107]. In accordance with this last fact are the results showing that repeated i.c.v. angiotensin II administration reduced the dipsogenic effect without affecting sodium intake [108]. Therefore, a possible explanation for amphetamine exposure effects is the alteration of intracellular signaling pathway involved in the effects of angiotensin II on sodium intake. This altered response obtained in amphetamine-exposed animals may involve the desensitization of AT1 receptors through internalization of these receptors [109]. This last is supported by the evidence showing that angiotensin II i.c.v. induces internalization of AT1 receptors [110]. Accordingly, a decrease in the response to angiotensin II after a persistent or repetitive stimulation of AT1 receptors has been described [111]. Moreover, it has been shown that the early inducible genes, c-fos, c-jun, and delta-fos are involved in the control of transcription factors expression that ultimately mediate the desensitization to the angiotensin II signal [112]. In our laboratory, we found that angiotensin II i.c.v. induced a threefold increase in NAc and CPu neuronal activation; this effect was blunted by repeated amphetamine exposure. This decreased response could demonstrate an AT1 receptor desensitization induced by repeated psychostimulant administration. In this regard, AT1 receptor desensitization-reduced Fos expression has been described as a consequence of repetitive angiotensin II i.c.v. administration in different brain areas that co-expressed AT1 receptors [112]. Interestingly, these results are in agreement with those obtained in regard to the decreased response in sodium intake to angiotensin II i.c.v.
It is known that exogenous i.c.v. angiotensin II administration stimulates oxytocin release from the pituitary gland [113, 114]. It has been found that the increase of sodium intake through sodium deprivation or adrenalectomy decreases basal oxytocin levels; meanwhile, treatments that stimulate oxytocin secretion (e.g., hypertonic saline, lithium chloride, and copper sulfate) inhibit sodium intake in sodium-deprived rats [115,116,117]. Moreover, blockade of central oxytocin receptors before i.c.v. angiotensin II administration resulted in a potentiation of angiotensin II-induced sodium intake, although in the absence of exogenously administered angiotensin II, blockade of oxytocin receptors does not interfere with the dipsogenic properties of angiotensin II, nor does it stimulate sodium intake [115]. In rats, the oxytocin receptor antagonist administration-induced sodium intake is blunted by AT1 receptor antagonist administration [118]. This evidence supports the idea of an inhibitory oxytocinergic tone involved in the activation or disinhibition of AT1 receptors [118].
The results obtained in our study using repeated amphetamine administration reveal a long-lasting effect of amphetamine exposure.
Moreover, it is possible to suggest that the decreased response in sodium intake induced by angiotensin II i.c.v. in amphetamine-exposed animals could be attributed to an increased oxytocin response to angiotensin II as a consequence of AT1 receptors altered functionality. This explanation is supported by our results, showing that amphetamine exposure increased the number of Fos-oxytocin positive neurons in response to angiotensin II. The mechanisms by which angiotensin II i.c.v. induces natriuretic effects could involve brain oxytocin release [119]. It has been shown that angiotensin II i.c.v. activates oxytocin neurons in paraventricular and supraoptic nucleus [113,114,115]. In our study, the repeated amphetamine administration potentiated the activation of oxytocin neurons induced by angiotensin II i.c.v. in different oxytocinergic subnuclei of paraventricular and supraoptic nucleus, possibly showing an increased oxytocin response to angiotensin II because of the reduced AT1 receptor functionality mentioned above. Therefore, the repeated amphetamine exposure could reduce AT1 receptor functionality (desensitization-like) shown as a potentiated oxytocinergic response to i.c.v. angiotensin II that elicits a decrease in sodium intake, an increase in natriuresis, and decreases in plasma renin activity. These results are also supported by the increased number of Fos-oxytocin positive neurons in paraventricular and supraoptic nucleus in response to i.c.v. angiotensin II found in the amphetamine-exposed animals [104].
In conclusion, the results presented here support the view that long-lasting changes in brain RAS could be considered among the psychostimulant-induced neuroadaptations.
References
Angrist B, Corwin J, Bartlik B, Cooper T. Early pharmacokinetics and clinical effects of oral D-amphetamine in normal subjects. Biol Psychiatry. 1987;22(11):1357–68.
Sherer MA. Intravenous cocaine: psychiatric effects, biological mechanisms. Biol Psychiatry. 1988;24(8):865–85.
Lieberman JA, Kinon BJ, Loebel AD. Dopaminergic mechanisms in idiopathic and drug-induced psychoses. Schizophr Bull. 1990;16(1):97–110.
Klawans HL, Margolin DI. Amphetamine-induced dopaminergic hypersensitivity in guinea pigs. Implications in psychosis and human movement disorders. Arch Gen Psychiatry. 1975;32(6):725–32.
Dackis C, Gold MS. Neurotransmitter and neuroendocrine abnormalities associated with cocaine use. Psychiatr Med. 1985;3(4):461–83.
Antelman SM, Chiodo LA. Dopamine autoreceptor subsensitivity: a mechanism common to the treatment of depression and the induction of amphetamine psychosis. Biol Psychiatry. 1981;16(8):717–27.
Kalivas PW, Pierce RC, Cornish J, Sorg BA. A role for sensitization in craving and relapse in cocaine addiction. J Psychopharmacol. 1998;12(1):49–53.
Stewart J, Badiani A. Tolerance and sensitization to the behavioral effects of drugs. Behav Pharmacol. 1993;4(4):289–312.
Pierce RC, Kalivas PW. A circuitry model of the expression of behavioral sensitization to amphetamine-like psychostimulants. Brain Res Brain Res Rev. 1997;25(2):192–216.
Vanderschuren LJ, Schmidt ED, De Vries TJ, Van Moorsel CA, Tilders FJ, Schoffelmeer AN. A single exposure to amphetamine is sufficient to induce long-term behavioral, neuroendocrine, and neurochemical sensitization in rats. J Neurosci. 1999;19(21):9579–86.
Valjent E, Bertran-Gonzalez J, Aubier B, Greengard P, Herve D, Girault JA. Mechanisms of locomotor sensitization to drugs of abuse in a two-injection protocol. Neuropsychopharmacology Off Publ Am Col Neuropsychopharmacology. 2010;35(2):401–15.
Vanderschuren LJ, Kalivas PW. Alterations in dopaminergic and glutamatergic transmission in the induction and expression of behavioral sensitization: a critical review of preclinical studies. Psychopharmacology (Berl). 2000;151(2–3):99–120.
Vezina P. D1 dopamine receptor activation is necessary for the induction of sensitization by amphetamine in the ventral tegmental area. J Neurosci. 1996;16(7):2411–20.
Prasad BM, Hochstatter T, Sorg BA. Expression of cocaine sensitization: regulation by the medial prefrontal cortex. Neuroscience. 1999;88(3):765–74.
Sorg BA, Kalivas PW. Effects of cocaine and footshock stress on extracellular dopamine levels in the medial prefrontal cortex. Neuroscience. 1993;53(3):695–703.
Sorg BA, Davidson DL, Kalivas PW, Prasad BM. Repeated daily cocaine alters subsequent cocaine-induced increase of extracellular dopamine in the medial prefrontal cortex. J Pharmacol Exp Ther. 1997;281(1):54–61.
Pierce RC, Reeder DC, Hicks J, Morgan ZR, Kalivas PW. Ibotenic acid lesions of the dorsal prefrontal cortex disrupt the expression of behavioral sensitization to cocaine. Neuroscience. 1998;82(4):1103–14.
Tzschentke TM, Schmidt WJ. The development of cocaine-induced behavioral sensitization is affected by discrete quinolinic acid lesions of the prelimbic medial prefrontal cortex. Brain Res. 1998;795(1–2):71–6.
Hedou G, Feldon J, Heidbreder CA. Effects of cocaine on dopamine in subregions of the rat prefrontal cortex and their efferents to subterritories of the nucleus accumbens. Eur J Pharmacol. 1999;372(2):143–55.
Richard ML, Liskow BI, Perry PJ. Recent psychostimulant use in hospitalized schizophrenics. J Clin Psychiatry. 1985;46(3):79–83.
Lippoldt A, Paul M, Fuxe K, Ganten D. The brain renin–angiotensin system: molecular mechanisms of cell to cell interactions. Clin Exp Hypertens. 1995;17(1–2):251–66.
Steckelings UM, Bottari SP, Unger T. Angiotensin receptor subtypes in the brain. Trends Pharmacol Sci. 1992;13(9):365–8.
Steele MK, Stephenson KN, Meredith JM, Levine JE. Effects of angiotensin II on LHRH release, as measured by in vivo microdialysis of the anterior pituitary gland of conscious female rats. Neuroendocrinology. 1992;55(3):276–81.
Barnes NM, Costall B, Kelly ME, Murphy DA, Naylor RJ. Anxiolytic-like action of DuP753, a non-peptide angiotensin II receptor antagonist. Neuroreport. 1990;1(1):20–1.
Kaiser FC, Palmer GC, Wallace AV, Carr RD, Fraser-Rae L, Hallam C. Antianxiety properties of the angiotensin II antagonist, DUP 753, in the rat using the elevated plus-maze. Neuroreport. 1992;3(10):922–4.
Georgiev V, Tanaka M, Tsuda A, Koga C, Takeda S, Yokoo H, et al. Effects of angiotensin II on regional brain noradrenaline metabolism in non-stressed and stressed rats. Kurume Med J. 1992;39(4):235–44.
Barnes NM, Costall B, Kelly ME, Murphy DA, Naylor RJ. Cognitive enhancing actions of PD123177 detected in a mouse habituation paradigm. Neuroreport. 1991;2(6):351–3.
Barnes JM, Barnes NM, Costall B, Coughlan J, Kelly ME, Naylor RJ, et al. Angiotensin-converting enzyme inhibition, angiotensin, and cognition. J Cardiovasc Pharmacol. 1992;19(Suppl 6):S63–71.
Dennes RP, Barnes JC. Attenuation of scopolamine-induced spatial memory deficits in the rat by cholinomimetic and non-cholinomimetic drugs using a novel task in the 12-arm radial maze. Psychopharmacology (Berl). 1993;111(4):435–41.
Wayner MJ, Armstrong DL, Polan-Curtain JL, Denny JB. Role of angiotensin II and AT1 receptors in hippocampal LTP. Pharmacol Biochem Behav. 1993;45(2):455–64.
Georgiev V, Kambourova T. Behavioural effects of angiotensin II in the mouse following MPTP administration. Gen Pharmacol. 1991;22(4):625–30.
Banks RJ, Mozley L, Dourish CT. The angiotensin converting enzyme inhibitors captopril and enalapril inhibit apomorphine-induced oral stereotypy in the rat. Neuroscience. 1994;58(4):799–805.
Georgiev V, Getova D, Opitz M. Mechanisms of the angiotensin II effects on exploratory behavior of rats in open field. III. Modulatory role of GABA. Methods Find Exp Clin Pharmacol. 1991;13(1):5–9.
Wong PC, Duncia JV, Santella 3rd JB, Smith RD, Wexler RR, Timmermans PB, et al. EXP597, a nonpeptide angiotensin II receptor antagonist with high affinities for the angiotensin AT1 and AT2 receptor subtypes. Eur J Pharmacol. 1994;260(2–3):261–4.
Inagami T, Iwai N, Sasaki K, Yamano Y, Bardhan S, Chaki S, et al. Cloning, expression and regulation of angiotensin II receptors. Eur Heart J. 1994;15(Suppl D):104–7.
Brown L, Sernia C. Angiotensin receptors in cardiovascular diseases. Clin Exp Pharmacol Physiol. 1994;21(10):811–8.
Dzau VJ, Pratt R, Gibbons GH. Angiotensin as local modulating factor in ventricular dysfunction and failure due to coronary artery disease. Drugs. 1994;47(Suppl 4):1–13.
Allen AM, Moeller I, Jenkins TA, Zhuo J, Aldred GP, Chai SY, et al. Angiotensin receptors in the nervous system. Brain Res Bull. 1998;47(1):17–28.
Yang CR, Phillips MI, Renaud LP. Angiotensin II receptor activation depolarizes rat supraoptic neurons in vitro. Am J Physiol. 1992;263(6 Pt 2):R1333–8.
Bai D, Renaud LP. ANG II AT1 receptors induce depolarization and inward current in rat median preoptic neurons in vitro. Am J Physiol. 1998;275(2 Pt 2):R632–9.
Latchford KJ, Ferguson AV. ANG II-induced excitation of paraventricular nucleus magnocellular neurons: a role for glutamate interneurons. Am J Physiol Regul Integr Comp Physiol. 2004;286(5):R894–902.
Albrecht D, Nitschke T, Von Bohlen Und Halbach O. Various effects of angiotensin II on amygdaloid neuronal activity in normotensive control and hypertensive transgenic [TGR(mREN-2)27] rats. FASEB J Off Publ Federation Am Soc Exp Biol. 2000;14(7):925–31.
Martial FP, Thornton SN, Lienard F, Mousseau MC, Nicolaidis S. Tonic neuronal inhibition by AII revealed by iontophoretic application of Losartan, a specific antagonist of AII type-1 receptors. Brain Res Bull. 1994;34(6):533–9.
Palovcik RA, Phillips MI. Saralasin increases activity of hippocampal neurons inhibited by angiotensin II. Brain Res. 1984;323(2):345–8.
Albrecht D, Broser M, Kruger H. Excitatory action of angiotensins II and IV on hippocampal neuronal activity in urethane anesthetized rats. Regul Pept. 1997;70(2–3):105–9.
Albrecht D, Broser M, Kruger H, Bader M. Effects of angiotensin II and IV on geniculate activity in nontransgenic and transgenic rats. Eur J Pharmacol. 1997;332(1):53–63.
Xiong HG, Marshall KC. Angiotensin II modulation of glutamate excitation of locus coeruleus neurons. Neurosci Lett. 1990;118(2):261–4.
Merabet L, de Gasparo M, Casanova C. Dose-dependent inhibitory effects of angiotensin II on visual responses of the rat superior colliculus: AT1 and AT2 receptor contributions. Neuropeptides. 1997;31(5):469–81.
Simonnet G, Bioulac B, Rodriguez F, Vincent JD. Evidence of a direct action of angiotensin II on neurones in the septum and in the medial preoptic area. Pharmacol Biochem Behav. 1980;13(3):359–63.
Mooney RD, Zhang Y, Rhoades RW. Effects of angiotensin II on visual neurons in the superficial laminae of the hamster's superior colliculus. Vis Neurosci. 1994;11(6):1163–73.
Cai Y, Bishop VS. Effects of arginine vasopressin and angiotensin II on area postrema neurons in rabbit brain slice preparation. Neurosci Lett. 1995;190(2):125–8.
Lin KS, Chan JY, Chan SH. Involvement of AT2 receptors at NRVL in tonic baroreflex suppression by endogenous angiotensins. Am J Physiol. 1997;272(5 Pt 2):H2204–10.
Georgiev V, Gyorgy L, Yonkov D, Getova D, Markovska V, Petkova B. Dopaminergic influence on the effects of angiotensin II in behavioural reactions. Physiol Bohemoslov. 1985;34(Suppl):45–8.
Huang BS, Malvin RL. Dopaminergic modulation of some central actions of angiotensin II in vivo. Proc Soc Exp Biol Med Soc Exp Biol Med. 1988;188(4):405–9.
Brown DC, Steward LJ, Ge J, Barnes NM. Ability of angiotensin II to modulate striatal dopamine release via the AT1 receptor in vitro and in vivo. Br J Pharmacol. 1996;118(2):414–20.
Daubert DL, Meadows GG, Wang JH, Sanchez PJ, Speth RC. Changes in angiotensin II receptors in dopamine-rich regions of the mouse brain with age and ethanol consumption. Brain Res. 1999;816(1):8–16.
Hoebel BG, Rada P, Mark GP, Hernandez L. The power of integrative peptides to reinforce behavior by releasing dopamine. Ann N Y Acad Sci. 1994;739:36–41.
Zhuo J, Moeller I, Jenkins T, Chai SY, Allen AM, Ohishi M, et al. Mapping tissue angiotensin-converting enzyme and angiotensin AT1, AT2 and AT4 receptors. J Hypertens. 1998;16(12 Pt 2):2027–37.
Labandeira-Garcia JL, Rodriguez-Pallares J, Dominguez-Meijide A, Valenzuela R, Villar-Cheda B, Rodriguez-Perez AI. Dopamine–angiotensin interactions in the basal ganglia and their relevance for Parkinson's disease. Mov Disord. 2013;28(10):1337–42.
Labandeira-Garcia JL, Rodriguez-Pallares J, Villar-Cheda B, Rodriguez-Perez AI, Garrido-Gil P, Guerra MJ. Aging, angiotensin system and dopaminergic degeneration in the substantia nigra. Aging Dis. 2011;2(3):257–74.
Villar-Cheda B, Rodriguez-Pallares J, Valenzuela R, Munoz A, Guerra MJ, Baltatu OC, et al. Nigral and striatal regulation of angiotensin receptor expression by dopamine and angiotensin in rodents: implications for progression of Parkinson's disease. Eur J Neurosci. 2010;32(10):1695–706.
Kloner RA, Hale S, Alker K, Rezkalla S. The effects of acute and chronic cocaine use on the heart. Circulation. 1992;85(2):407–19.
Billman GE. Cocaine: a review of its toxic actions on cardiac function. Crit Rev Toxicol. 1995;25(2):113–32.
Mouhaffel AH, Madu EC, Satmary WA, Fraker Jr TD. Cardiovascular complications of cocaine. Chest. 1995;107(5):1426–34.
Margolin A, Avants SK, Setaro JF, Rinder HM, Grupp L. Cocaine, HIV, and their cardiovascular effects: is there a role for ACE-inhibitor therapy? Drug Alcohol Depend. 2000;61(1):35–45.
Goeders NE. A neuroendocrine role in cocaine reinforcement. Psychoneuroendocrinology. 1997;22(4):237–59.
DeVries AC, Taymans SE, Sundstrom JM, Pert A. Conditioned release of corticosterone by contextual stimuli associated with cocaine is mediated by corticotropin-releasing factor. Brain Res. 1998;786(1–2):39–46.
Sarnyai Z. Neurobiology of stress and cocaine addiction. Studies on corticotropin-releasing factor in rats, monkeys, and humans. Ann N Y Acad Sci. 1998;851:371–87.
Zacharieva S, Matrozov P, Stoeva I, Andonova K. The effect of angiotensin-converting enzyme inhibition on ACTH response to corticotropin-releasing hormone (CRH) in normal men. Horm Metab Res. 1991;23(5):245–6.
Aguilera G, Kiss A, Luo X. Increased expression of type 1 angiotensin II receptors in the hypothalamic paraventricular nucleus following stress and glucocorticoid administration. J Neuroendocrinol. 1995;7(10):775–83.
Mendelsohn FA, Jenkins TA, Berkovic SF. Effects of angiotensin II on dopamine and serotonin turnover in the striatum of conscious rats. Brain Res. 1993;613(2):221–9.
Dwoskin LP, Jewell AL, Cassis LA. DuP 753, a nonpeptide angiotensin II-1 receptor antagonist, alters dopaminergic function in rat striatum. Naunyn Schmiedebergs Arch Pharmacol. 1992;345(2):153–9.
Braszko JJ. Participation of D 1-4 dopamine receptors in the pro-cognitive effects of angiotensin IV and des-Phe 6 angiotensin IV. Neurosci Biobehav Rev. 2010;34(3):343–50.
Stragier B, Sarre S, Vanderheyden P, Vauquelin G, Fournie-Zaluski MC, Ebinger G, et al. Metabolism of angiotensin II is required for its in vivo effect on dopamine release in the striatum of the rat. J Neurochem. 2004;90(5):1251–7.
Aguilera G, Young WS, Kiss A, Bathia A. Direct regulation of hypothalamic corticotropin-releasing-hormone neurons by angiotensin II. Neuroendocrinology. 1995;61(4):437–44.
DeVries AC, Pert A. Conditioned increases in anxiogenic-like behavior following exposure to contextual stimuli associated with cocaine are mediated by corticotropin-releasing factor. Psychopharmacology (Berl). 1998;137(4):333–40.
Jenkins TA, Mendelsohn FA, Chai SY. Angiotensin-converting enzyme modulates dopamine turnover in the striatum. J Neurochem. 1997;68(3):1304–11.
Acerbo MJ, Johnson AK. Behavioral cross-sensitization between DOCA-induced sodium appetite and cocaine-induced locomotor behavior. Pharmacol Biochem Behav. 2011;98(3):440–8.
Watanabe MA, Kucenas S, Bowman TA, Ruhlman M, Knuepfer MM. Angiotensin II and CRF receptors in the central nucleus of the amygdala mediate hemodynamic response variability to cocaine in conscious rats. Brain Res. 2010;1309:53–65.
von Bohlen und Halbach O, Albrecht D. Visualization of specific angiotensin II binding sites in the rat limbic system. Neuropeptides. 1998;32(3):241–5.
Sakanaka M, Shibasaki T, Lederis K. Distribution and efferent projections of corticotropin-releasing factor-like immunoreactivity in the rat amygdaloid complex. Brain Res. 1986;382(2):213–38.
Uryu K, Okumura T, Shibasaki T, Sakanaka M. Fine structure and possible origins of nerve fibers with corticotropin-releasing factor-like immunoreactivity in the rat central amygdaloid nucleus. Brain Res. 1992;577(1):175–9.
Brown MR, Gray TS. Peptide injections into the amygdala of conscious rats: effects on blood pressure, heart rate and plasma catecholamines. Regul Pept. 1988;21(1–2):95–106.
Ku YH, Tan L, Li LS, Ding X. Role of corticotropin-releasing factor and substance P in pressor responses of nuclei controlling emotion and stress. Peptides. 1998;19(4):677–82.
Hsu DT, Chen FL, Takahashi LK, Kalin NH. Rapid stress-induced elevations in corticotropin-releasing hormone mRNA in rat central amygdala nucleus and hypothalamic paraventricular nucleus: an in situ hybridization analysis. Brain Res. 1998;788(1–2):305–10.
Gardi J, Biro E, Sarnyai Z, Vecsernyes M, Julesz J, Telegdy G. Time-dependent alterations in corticotropin-releasing factor-like immunoreactivity in different brain regions after acute cocaine administration to rats. Neuropeptides. 1997;31(1):15–8.
Paz MC, Assis MA, Cabrera RJ, Cancela LM, Bregonzio C. The AT(1) angiotensin II receptor blockade attenuates the development of amphetamine-induced behavioral sensitization in a two-injection protocol. Synapse. 2011;65(6):505–12.
Paz MC, Marchese NA, Cancela LM, Bregonzio C. Angiotensin II AT(1) receptors are involved in neuronal activation induced by amphetamine in a two-injection protocol. Biomed Res Int. 2013;2013:534817.
Paz MC, Marchese NA, Stroppa MM, Gerez de Burgos NM, Imboden H, Baiardi G, et al. Involvement of the brain renin–angiotensin system (RAS) in the neuroadaptive responses induced by amphetamine in a two-injection protocol. Behav Brain Res. 2014;272(314):23.
Pediconi D, Martarelli D, Fontanazza A, Pompei P. Effects of losartan and irbesartan administration on brain angiotensinogen mRNA levels. Eur J Pharmacol. 2005;528(1–3):79–87.
Pelisch N, Hosomi N, Ueno M, Masugata H, Murao K, Hitomi H, et al. Systemic candesartan reduces brain angiotensin II via downregulation of brain renin–angiotensin system. Hypertens Res Off J Jpn Soc Hypertens. 2010;33(2):161–4.
Trout SJ, Kruk ZL. Differences in evoked dopamine efflux in rat caudate putamen, nucleus accumbens and tuberculum olfactorium in the absence of uptake inhibition: influence of autoreceptors. Br J Pharmacol. 1992;106(2):452–8.
Grace AA. Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: a hypothesis for the etiology of schizophrenia. Neuroscience. 1991;41(1):1–24.
Mertens B, Vanderheyden P, Michotte Y, Sarre S. Direct angiotensin II type 2 receptor stimulation decreases dopamine synthesis in the rat striatum. Neuropharmacology. 2010;58(7):1038–44.
Vanderschuren LJ, Everitt BJ. Behavioral and neural mechanisms of compulsive drug seeking. Eur J Pharmacol. 2005;526(1–3):77–88.
Wise RA. Drug-activation of brain reward pathways. Drug Alcohol Depend. 1998;51(1–2):13–22.
Clark JJ, Bernstein IL. Reciprocal cross-sensitization between amphetamine and salt appetite. Pharmacol Biochem Behav. 2004;78(4):691–8.
Marchese NA, Artur de laVillarmois E, Basmadjian OM, Perez MF, Baiardi G, Bregonzio C. Brain angiotensin II AT receptors are involved in the acute and long-term amphetamine-induced neurocognitive alterations. Psychopharmacology. 2016;233(5):795–807.
Ferguson AV, Washburn DL, Latchford KJ. Hormonal and neurotransmitter roles for angiotensin in the regulation of central autonomic function. Exp Biol Med (Maywood). 2001;226(2):85–96.
Fitzsimons JT. Angiotensin, thirst, and sodium appetite. Physiol Rev. 1998;78(3):583–686.
Fluharty SJ, Manaker S. Sodium appetite elicited by intracerebroventricular infusion of angiotensin II in the rat: I. Relation to urinary sodium excretion. Behav Neurosci. 1983;97(5):738–45.
Geerling JC, Loewy AD. Central regulation of sodium appetite. Exp Physiol. 2008;93(2):177–209.
Unger T, Horst PJ, Bauer M, Demmert G, Rettig R, Rohmeiss P. Natriuretic action of central angiotensin II in conscious rats. Brain Res. 1989;486(1):33–8.
Casarsa BS, Marinzalda MA, Marchese NA, Paz MC, Vivas L, Baiardi G, et al. A previous history of repeated amphetamine exposure modifies brain angiotensin II AT1 receptor functionality. Neuroscience. 2015;307:1–13.
Daniels D, Yee DK, Faulconbridge LF, Fluharty SJ. Divergent behavioral roles of angiotensin receptor intracellular signaling cascades. Endocrinology. 2005;146(12):5552–60.
Daniels D, Yee DK, Fluharty SJ. Angiotensin II receptor signalling. Exp Physiol. 2007;92(3):523–7.
Daniels D, Mietlicki EG, Nowak EL, Fluharty SJ. Angiotensin II stimulates water and NaCl intake through separate cell signalling pathways in rats. Exp Physiol. 2009;94(1):130–7.
Vento PJ, Daniels D. Repeated administration of angiotensin II reduces its dipsogenic effect without affecting saline intake. Exp Physiol. 2010;95(6):736–45.
Hunyady L, Catt KJ, Clark AJ, Gaborik Z. Mechanisms and functions of AT(1) angiotensin receptor internalization. Regul Pept. 2000;91(1–3):29–44.
Sasamura H, Dzau VJ, Pratt RE. Desensitization of angiotensin receptor function. Kidney Int. 1994;46(6):1499–501.
Tang H, Shirai H, Inagami T. Inhibition of protein kinase C prevents rapid desensitization of type 1B angiotensin II receptor. Circ Res. 1995;77(2):239–48.
Moellenhoff E, Blume A, Culman J, Chatterjee B, Herdegen T, Lebrun CJ, et al. Effect of repetitive icv injections of ANG II on c-Fos and AT(1)-receptor expression in the rat brain. Am J Physiol Regul Integr Comp Physiol. 2001;280(4):R1095–104.
Lang RE, Rascher W, Heil J, Unger T, Wiedemann G, Ganten D. Angiotensin stimulates oxytocin release. Life Sci. 1981;29(14):1425–8.
Ferguson AV, Kasting NW. Angiotensin acts at the subfornical organ to increase plasma oxytocin concentrations in the rat. Regul Pept. 1988;23(3):343–52.
Blackburn RE, Demko AD, Hoffman GE, Stricker EM, Verbalis JG. Central oxytocin inhibition of angiotensin-induced salt appetite in rats. Am J Physiol. 1992;263(6 Pt 2):R1347–53.
Stricker EM, Verbalis JG. Central inhibition of salt appetite by oxytocin in rats. Regul Pept. 1996;66(1–2):83–5.
Stricker EM, Verbalis JG. Central inhibitory control of sodium appetite in rats: correlation with pituitary oxytocin secretion. Behav Neurosci. 1987;101(4):560–7.
Fitts DA, Zierath DK, Wilkins EE, Bassett JE. Losartan blocks drinking and cFos expression induced by central ornithine vasotocin in rats. Physiol Behav. 2005;86(4):573–7.
Verbalis JG, Mangione MP, Stricker EM. Oxytocin produces natriuresis in rats at physiological plasma concentrations. Endocrinology. 1991;128(3):1317–22.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Bregonzio, C., Marchese, N.A., Paz, M.C., de la Villarmois, E.A., Baiardi, G., Pérez, M.F. (2017). The Extent of Neuroadaptive Responses to Psychostimulants: Focus on Brain Angiotensin System. In: Gargiulo, P., Mesones-Arroyo, H. (eds) Psychiatry and Neuroscience Update - Vol. II. Springer, Cham. https://doi.org/10.1007/978-3-319-53126-7_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-53126-7_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-53125-0
Online ISBN: 978-3-319-53126-7
eBook Packages: MedicineMedicine (R0)