Abstract
30-year-old man with history of cystic fibrosis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Cystic fibrosis
- Fatty replacement
- Shwachman-Diamond syndrome
- Cyst formation (Cystic fibrosis)
- Calcifications (cystic fibrosis).
Clinical History
30-year-old man with history of cystic fibrosis.
Imaging Findings
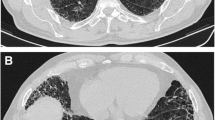
Axial contrast-enhanced CT image demonstrates diffuse fatty attenuation of the pancreatic parenchyma (Fig. 1a, thick white arrow). The pancreatic duct can be appreciated (Fig. 1a, thin arrow). There is heterogeneous appearance of the liver with multiple mass-like areas of low attenuation (Fig. 1a, black arrow). On a non-contrast CT image, the multiple mass-like areas of low attenuation (Fig. 1b, arrows) measure about 1 HU (range, −25–10 HU).

Fig. 1
Differential Diagnosis
Cystic fibrosis, Shwachman-Diamond syndrome, post steroid therapy, Cushing’s syndrome, and Johanson-Blizzard syndrome.
Diagnosis
Diffuse fatty replacement of the pancreas secondary to cystic fibrosis.
Discussion
The pancreas is the most common organ in the abdomen involved in cystic fibrosis, which can present as complete fatty replacement of the organ. Reduced flow in the pancreatic duct caused by inspissated secretions leads to fibrofatty replacement of the organ. Ductal stenosis can also lead to cyst formation [1]. The mean age at which pancreatic fatty replacement is diagnosed is 17 years and correlates with exocrine insufficiency of the organ [2, 3]. Exocrine insufficiency affects about 90% of patients with cystic fibrosis and can, in turn, lead to steatorrhea due to fat malabsorption. Residual pancreatic exocrine function may cause acute recurrent pancreatitis, and acute pancreatitis, on rare occasions, may be the initial presentation of cystic fibrosis [4]. Secretin-stimulated MRI/MRCP has shown high diagnostic accuracy for diagnosing exocrine insufficiency in patients with cystic fibrosis [5]. Endocrine insufficiency is less common, affecting about 30–40% of patients with cystic fibrosis, and can lead to a combination of type 1 and 2 diabetes mellitus [6].
On CT, the attenuation of the pancreas in diffuse fatty replacement of the pancreas secondary to cystic fibrosis is similar that of the mesenteric fat (Fig. 1a). The contour of the pancreas can be appreciated and the pancreatic duct may be visualized within area of lipomatous change (Fig. 1). Cystic change may also occur and when it does the cysts are usually unilocular (Fig. 2). Other imaging findings include partial fatty replacement [7], pancreatic parenchymal calcifications, and diffuse pancreatic atrophy without fatty replacement [8]. The radiographic severity of acute pancreatitis in patients with cystic fibrosis is usually less severe than patients without cystic fibrosis.
Companion case. 42-year-old man with cystic fibrosis. Axial contrast-enhanced CT demonstrates complete fatty replacement of the pancreas (Fig. 2, thick arrow) and a retention cyst in the pancreatic head (Fig. 2, thin arrow)
Hepatic steatosis is seen in about 23–67% of patients with cystic fibrosis and is the most common finding in the liver [9]. Fatty replacement may have a mass-like appearance presenting as multiple pseudomasses in the liver [10] (Fig. 1b).
Similar diffuse fatty replacement of the pancreas is also seen in patients with Shwachman-Diamond syndrome (Fig. 3). However, unlike cystic fibrosis, calcifications and cyst formation do not occur in Shwachman-Diamond syndrome [11]. Other rare causes of fatty infiltration of the pancreas are steroid therapy, Cushing’s syndrome, and Johanson-Blizzard syndrome [12].
Confirmatory test for cystic fibrosis may be made with genetic testing for cystic fibrosis transmembrane conductance regulator (CFTR) gene. The survival of patients with cystic fibrosis has improved over the years with lung transplantation, better nonsurgical therapies, and nutrition supplementation.
Teaching Point
The pancreas is the most common organ involved in cystic fibrosis in the abdomen and presents as complete fatty replacement and cyst formation with or without calcifications.
References
Berrocal T, Pajares MP, Zubillaga AF. Pancreatic cystosis in children and young adults with cystic fibrosis: sonographic, CT, and MRI findings. AJR Am J Roentgenol. 2005;184(4):1305–9. doi:10.2214/ajr.184.4.01841305.
Daneman A, Gaskin K, Martin DJ, Cutz E. Pancreatic changes in cystic fibrosis: CT and sonographic appearances. AJR Am J Roentgenol. 1983;141(4):653–5. doi:10.2214/ajr.141.4.653.
Soyer P, Spelle L, Pelage JP, Dufresne AC, Rondeau Y, Gouhiri M, et al. Cystic fibrosis in adolescents and adults: fatty replacement of the pancreas – CT evaluation and functional correlation. Radiology. 1999;210(3):611–5. doi:10.1148/radiology.210.3.r99mr08611.
De Boeck K, Weren M, Proesmans M, Kerem E. Pancreatitis among patients with cystic fibrosis: correlation with pancreatic status and genotype. Pediatrics. 2005;115(4):e463–9. doi:10.1542/peds.2004-1764.
Madzak A, Engjom T, Wathle GK, Olesen SS, Tjora E, Njolstad PR, et al. Secretin-stimulated MRI assessment of exocrine pancreatic function in patients with cystic fibrosis and healthy controls. Abdom Radiol (NY). 2016; doi:10.1007/s00261-016-0972-8.
Fields TM, Michel SJ, Butler CL, Kriss VM, Albers SL. Abdominal manifestations of cystic fibrosis in older children and adults. AJR Am J Roentgenol. 2006;187(5):1199–203. doi:10.2214/AJR.05.0327.
Carucci LR, Jacobs JE. Focal fatty sparing of the pancreatic head in cystic fibrosis: CT findings. Abdom Imaging. 2003;28(6):853–5.
Lavelle LP, McEvoy SH, Ni Mhurchu E, Gibney RG, McMahon CJ, Heffernan EJ, et al. Cystic fibrosis below the diaphragm: abdominal findings in adult patients. Radiographics. 2015;35(3):680–95. doi:10.1148/rg.2015140110.
Colombo C, Battezzati PM. Liver involvement in cystic fibrosis: primary organ damage or innocent bystander? J Hepatol. 2004;41(6):1041–4. doi:10.1016/j.jhep.2004.10.002.
Akata D, Akhan O, Ozcelik U, Ozmen MN, Oguzkurt L, Haliloglu M, et al. Hepatobiliary manifestations of cystic fibrosis in children: correlation of CT and US findings. Eur J Radiol. 2002;41(1):26–33.
Vaughn DD, Jabra AA, Fishman EK. Pancreatic disease in children and young adults: evaluation with CT. Radiographics. 1998;18(5):1171–87. doi:10.1148/radiographics.18.5.9747614.
Robberecht E, Nachtegaele P, Van Rattinghe R, Afschrift M, Kunnen M, Verhaaren R. Pancreatic lipomatosis in the Shwachman-Diamond syndrome. Identification by sonography and CT-scan. Pediatr Radiol. 1985;15(5):348–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Johnson, S.I. (2017). Case 21: Fatty Infiltration in Cystic Fibrosis. In: Zaheer, A., Fishman, E., Pittman, M., Hruban, R. (eds) Pancreatic Imaging. Springer, Cham. https://doi.org/10.1007/978-3-319-52680-5_21
Download citation
DOI: https://doi.org/10.1007/978-3-319-52680-5_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-52678-2
Online ISBN: 978-3-319-52680-5
eBook Packages: MedicineMedicine (R0)