Abstract
Helicobacter pylori is a bacterial pathogen which commonly colonizes the human gastric mucosa from early childhood and persists throughout life. In the vast majority of cases, the infection is asymptomatic. H. pylori is the leading cause of peptic ulcer disease and gastric cancer, however, and these outcomes occur in 10–15% of those infected. Gastric adenocarcinoma is the third most common cause of cancer-associated death, and peptic ulcer disease is a significant cause of morbidity. Disease risk is related to the interplay of numerous bacterial host and environmental factors, many of which influence chronic inflammation and damage to the gastric mucosa. This chapter summarizes what is known about health and disease in H. pylori infection, and highlights the need for additional research in this area.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The bacterial pathogen Helicobacter pylori was discovered by Barry Marshall and Robin Warren in the early 1980s, who first reported its presence on mucosal tissue sections from the stomach of patients with gastritis and peptic ulcers (Marshall and Warren 1984). It is a fastidious and microaerophilic Gram-negative bacterium characterized by a curved rod morphology and positive reactions for catalase, oxidase, and urease, the latter reaction being characteristically rapid and most frequently used for initial identification. In the vast majority of cases, the infection is completely asymptomatic; however, peptic ulcer disease or gastric cancer occurs in 10–15% of those infected. The type and severity of disease depends on several factors including characteristics of the colonizing strain, the host immune response, as well as environmental factors such as smoking, a high-salt diet, and the presence of other concurrent infections (Amieva and Peek 2016). It is important to characterize the effects of these factors in order to understand why disease occurs, and who may be at risk of developing disease in the future.
2 H. pylori Infection and Strategies of Persistence
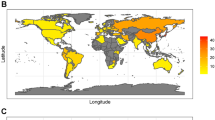
H. pylori usually establishes colonization of the gastric mucosa during early childhood, and it persists life long in the absence of an effective eradication treatment. The organism has co-evolved with humans over at least 60,000 years since their migration from Africa (Atherton and Blaser 2009), and is currently estimated to colonize almost 50% of the world’s population. The prevalence of H. pylori differs greatly around the world, with the highest infection rates in developing countries. The prevalence of H. pylori is declining, with increased urbanization and common use of antibiotics during childhood. H. pylori infection rates in young children from developed countries are now very low and, since it is unusual to acquire the infection as an adult, this creates a birth cohort effect. Of those below 20 years of age residing in the USA, for example, only approximately 10% are H. pylori-positive, compared with 40% amongst the over 60s (Nagy et al. 2016).
H. pylori is almost exclusively found in humans. The presence of other Helicobacter species in the human stomach is comparatively rare, and these are thought to be acquired from domestic pets. The precise routes of transmission of H. pylori are unclear; however, close person-to-person contact is required, and the faecal–oral and oral–oral routes are most likely. Strains of H. pylori are usually isolated from gastric biopsy tissue specimens; however, it is also possible for the bacterium to be recovered from saliva, gastric reflux fluid, diarrhoea, and vomitus. The organism does not typically survive passage through the intestine into normal faeces; however, its isolation and transmission from contaminated water supplies and farm animals has also been reported (Breckan et al. 2016).
H. pylori inhabits the harsh, highly acidic environment of the stomach, and has evolved several mechanisms in order to survive. This bacterium is not an acidophile and can only survive for a short period at pH 2, quickly losing motility in a pH- and pepsin-dependent manner. Whilst the basal acidity in the human stomach lumen is usually below pH 2, this can increase to pH 5.5 following a meal in adults and as high as pH 7 in breast-fed children. Furthermore, pepsin activity is exponentially reduced at higher pH, thus allowing H. pylori a longer survival time in the gastric lumen if infection occurs postprandial and in younger children compared to adults (Schreiber et al. 2005). H. pylori possesses several important enzymes to enable survival under acid shock conditions. 15% of H. pylori’s expressed protein is made up of cytoplasmic urease, made up of two subunits, UreA and UreB. In an environment below pH 6.5, a channel in the cytoplasmic membrane, encoded by the ureI gene, opens to enable entry of host urea. This becomes hydrolysed by urease to produce ammonia and carbon dioxide, buffering the cytoplasm (Weeks et al. 2000). Another important enzyme is α-carbonic anhydrase. This is located within the periplasm and catalyses the reversible hydration of carbon dioxide, diffusing into the periplasm from the action of cytoplasmic urease, to bicarbonate, buffering the periplasm. Both of these enzymes are regulated by the two component acid-responsive signalling system, ArsRS (Pflock et al. 2005; Wen et al. 2007), which also regulates other non-essential enzymes which aid acid tolerance: the amidase AmiE; the formamidase AmiF; and the urea-producing arginase RocF (Pflock et al. 2006).
As well as surviving the acidic environment of the gastric lumen, H. pylori must avoid clearance through frequent gastric emptying. The organism has unipolar flagella, is highly motile, and is able to sense pH and bicarbonate ions. This allows the bacteria to quickly migrate from the highly acidic gastric lumen into the mucus layer overlying the epithelium. The secretion of bicarbonate ions by gastric epithelial cells establishes a pH gradient through the mucus layer, from a near neutral pH close to the epithelial cell surface to the highly acidic stomach lumen. The viscosity of the mucus layer is pH-dependent and ranges from a thick, protective gel near the acidic lumen to a viscous solution near the epithelium. Upon entering the mucus gel from the lumen, H. pylori is able to reduce the viscosity of the mucus gel to aid its motility by increasing the local pH through the urease-catalysed hydrolysis of urea to ammonia (Celli et al. 2009). The bacteria use the pH gradient to orientate themselves in the gastric mucus, moving from the acidic lumen to a more neutral environment deeper in the mucus layer. Histological analysis has shown most of the bacteria to be free-swimming in the mucus close to the epithelium, with some adhering to the surface of the epithelial cells or within the gastric glands. This close proximity allows it to deliver bacterial products to the cells, either in the form of secreted or surface proteins, or in outer membrane vesicles, for its own benefit. One example of this is the loosening of tight junctions and release of interstitial fluid for access to nutrients and urea. H. pylori can sense other important signals such as the essential amino acid arginine, urea, and the quorum-sensing molecule autoinducer 2, and is repelled from conditions which reduce electron transport (Keilberg and Ottemann 2016). Host urea appears to be the main attractant that H. pylori uses to sense the epithelium (Huang et al. 2015). Urea binds strongly to the chemoreceptor, TlpB, and coupled with the hydrolysis of urea within the immediate environment of the bacteria, and H. pylori is able to sense levels of the molecule below the nanomolar range (Huang et al. 2015). Interestingly, H. pylori has been shown to preferentially colonize sites of gastric injury in mice, and this response is both rapid and requires a functional chemotactic system (Aihara et al. 2014). Such areas of damage may be a good source of nutrients for the bacteria. Whilst close interactions with the epithelium protect H. pylori from the harsh environment of the stomach lumen and provide access to nutrients, it comes at a cost: the activation of the immune response and increased induction of bactericidal factors. In order to persist, a careful balance is struck between the bacteria and the host.
H. pylori interacts with the gastric epithelium, stimulating the expression of pro-inflammatory cytokines and chemokines in addition to antimicrobial peptides such as beta-defensin 2 (Fig. 1a). The chemokine response recruits the migration of immune and inflammatory cells. This includes neutrophils, which phagocytose the bacteria. Macrophages also secrete reactive oxygen and nitrogen species to kill bacteria, but also express pro-inflammatory cytokines which can induce epithelial cell apoptosis. Macrophage-derived cytokines also have an important influence on the development and balance of the adaptive immune response (Munari et al. 2014). Dendritic cells (DCs) in a pro-inflammatory cytokine environment stimulate the differentiation of T-helper 1 (Th1), Th17 and Th22 cells, which in turn secrete cytokines to enhance the inflammatory response (Atherton and Blaser 2009).
Pro- and anti-inflammatory responses to H. pylori in the gastric mucosa. a Interactions between gastric epithelial cells and H. pylori result in activation of inflammatory signalling, resulting in the expression of high concentrations of cytokines and chemokines including interleukin-8 (IL-8), CCL20, and CXCL1–3. These chemokines stimulate the migration of immune cells, including dendritic cells (DCs), neutrophils (Nϕ), macrophages, and B and T lymphocytes into the mucosa from capillary blood. Upon arrival, the cells respond to the local cytokine milieu, becoming pro-inflammatory in nature. Macrophages and neutrophils phagocytose bacteria that penetrate the mucosa. Bacterial components and outer membrane vesicles (OMVs) pass through the epithelial barrier and further activate immune and inflammatory cells. DCs secrete IL-12 and IL-23, which stimulate the differentiation of naïve T cells into T-helper 1 (Th1) and Th17 cells, respectively. The cytokines secreted by these Th subsets act on macrophages to stimulate their development into an M1 type, being highly bactericidal, secreting reactive oxygen and nitrogen species (ROS, NO) and expressing inflammatory cytokines including IL-1β, IL-6, and tumour necrosis factor alpha (TNFα). This results in damage to the epithelial barrier and the induction of epithelial cell apoptosis. The presence of inflammatory cytokines also exacerbates the chemokine response of gastric epithelial cells. b Less pathogenic (cagPAI-negative) strains of H. pylori stimulate lower-level expression of cytokines and chemokines from gastric epithelial cells, resulting in reduced recruitment of immune and inflammatory cells into the mucosa. Upon penetration of the mucosal barrier (e.g. via OMVs), some bacterial components such as VacA and GGT have a tolerizing effect on DCs. These DCs promote the differentiation of regulatory T cells (Tregs), which express anti-inflammatory cytokines including IL-10, IL-35, and transforming growth factor beta (TGFβ). Macrophages in this environment express markers of an M2 type, express IL-10 and perform wound-healing rather than inflammatory or bactericidal functions. The presence of IL-10 suppresses chemokine expression from gastric epithelial cells
Despite this potent inflammatory and bactericidal activity, H. pylori has multiple mechanisms for evading immunity and directing the immune system towards a suppressive response. It thereby minimizes damage and enables it to maintain persistent, lifelong colonization of the host (Fig. 1b). Many components of H. pylori are modified so that they do not potently activate recognition receptors such as the toll-like receptors, and its fucosylated ligands for the C-type lectin receptor DC-SIGN stimulate anti-inflammatory cytokine responses including interleukin-10 (IL-10) (Salama et al. 2013). Some components have the ability to induce regulatory immune responses (White et al. 2015) (reviewed in Chapters “Immune Evasion Strategies and Persistence of Helicobacter pylori ” and “ Helicobacter pylori and Extragastric Diseases”), for having a tolerizing effect on DCs and causing them to promote the differentiation of naïve T cells into regulatory T cells (Tregs) (Oertli et al. 2012; Luther et al. 2011). These suppressive cells modulate inflammation by secreting cytokines such as IL-10 and transforming growth factor beta (TGFβ), or they may act via a number of contact-mediated mechanisms (Ai et al. 2014). Such effects result in reduced chemokine expression by gastric epithelial cells, and therefore reduced migration of inflammatory cells into the mucosa and less tissue damage. Macrophages responding to the cytokine milieu of the mucosa may express markers of the M2 type, whose chief role is in wound-healing rather than having a potent bactericidal and inflammatory function, which are attributes of M1 macrophages (Quiding-Jarbrink et al. 2010). H. pylori expresses enzymes such as catalase and arginase to protect against the damaging effects of reactive oxygen and nitrogen species (Ramarao et al. 2000; Gobert et al. 2001), and in addition, the bacterium is known to downregulate the expression of some antimicrobial peptides by gastric epithelial cells, including beta-defensins 1 and 3 (Patel et al. 2013; Bauer et al. 2012). These mechanisms are also thought to contribute to the persistence of the infection.
3 H. pylori Infection in Health and Disease
Chronic H. pylori colonization almost always leads to local inflammation of the gastric mucosa (gastritis), but this does not usually result in any symptoms. The most common disease outcomes of H. pylori infection include gastric and duodenal ulcer disease, distal gastric adenocarcinoma, and primary gastric mucosal-associated lymphoid tissue (MALT) lymphoma. Other conditions associated with H. pylori infection include dyspepsia, atrophic gastritis, iron deficiency anaemia, and idiopathic thrombocytopenia purpura. Pathogenesis is linked with the level of gastric inflammation, and interestingly the pattern of gastritis within the stomach is an important determinant of disease outcome (see Chapters “Human and Helicobacter pylori Interactions Determine the Outcome of Gastric Diseases” and “Pathogenesis of Gastric Cancer: Genetics and Molecular Classification”). What dictates the distribution of gastritis remains unknown; however, antral-predominant gastritis is associated with duodenal ulceration, whereas corpus-predominant or pan-gastritis is associated with the development of gastric ulcers and gastric cancer (Atherton 2006). It has been proposed that the time of development of atrophic gastritis may an important factor in deciding disease outcome. If atrophic gastritis is not acquired early, high gastric acid output may result, with increased risk of duodenal ulcer later in life. An earlier appearance of atrophic gastritis would cause low gastric acid production, and consequently gastric cancer may occur (Ubukata et al. 2011).
Peptic ulcer disease is a fairly modern outcome of H. pylori infection, and the reasons for its emergence are unknown. In the USA, gastric ulcers were described from 1838 and duodenal ulcer disease reported a little later in 1931. Peak prevalence was in the early 1900s (Baron and Sonnenberg 2001). Possible theories for the emergence of peptic ulcer disease include increased strain virulence, and reduced transmission making infection with a single strain more common. Changes in the immune response, due to environmental factors such as cigarette smoking, diet, or exposure to other infections, are also important (Atherton and Blaser 2009). The ancestry and co-evolution of the H. pylori strain and its host population has also been shown to influence gastric cancer risk (Kodaman et al. 2014). Within populations in Africa, Asia, and India, some anomalies in the prevalence of disease have been reported, and these “enigmas” may provide clues about the circumstances of disease development. Much controversy surrounds whether these actually exist however (Graham et al. 2009), and the factors influencing the risk of disease are extremely complex (Table 1).
On the other hand, a protective association between H. pylori infection and disorders such as gastroesophageal reflux disease (GERD), oesophageal adenocarcinoma, inflammatory bowel disease, multiple sclerosis, and asthma has been variously described (Robinson 2015) (described in Chapter “ Helicobacter pylori and Extragastric Diseases”).
3.1 Gastritis
The surface of the gastric mucosa is covered by layers of protective mucus, which H. pylori swims through to avoid damage from gastric acid and digestive enzymes. H. pylori is able to interact with the mucins via major adhesins the blood group antigen-binding adhesin (BabA), sialic acid-binding adhesin (SabA), and the lacdiNAc-specific adhesin, LabA (Ilver et al. 1998; Mahdavi et al. 2002; Rossez et al. 2014). Once in proximity to gastric epithelial cells, H. pylori activates inflammatory gene expression via interactions with pattern recognition receptors, for example Toll-like receptor 2 and NOD1 (Viala et al. 2004), and inflammasomes (Kim et al. 2013; Vanaja et al. 2015). Components of the H. pylori cytotoxin-associated gene pathogenicity island (cagPAI) encoded type IV secretion system (T4SS) activate inflammatory signalling in gastric epithelial cells via a number of different mechanisms (described briefly in Sect. 3.1, and in detail in Chapter “Structural Insights into Helicobacter pylori Cag Protein Interactions with Host Cell Factors”), resulting in the secretion of cytokines and chemokines, including interleukin-8 (IL-8), IL-1β, tumour necrosis factor alpha (TNFα), IL-6, IL-12, CCL2-5, CCL20, and CXCL1-3 (Cook et al. 2014). The presence of chemokines leads to the recruitment of neutrophils, macrophages, mast cells, dendritic cells (DCs), innate lymphoid cells, and lymphocytes, a feature termed gastritis (Atherton and Blaser 2009).
The level and nature of gastritis varies, affecting the risk of disease development (Macarthur et al. 2004). Innate cells including neutrophils, macrophages, and NK cells contribute to gastritis via the secretion of inflammatory and tissue-damaging factors including reactive oxygen and nitrogen species (ROS and RNS) (Italiani and Boraschi 2014), perforin and granzymes (Yun et al. 2005).
It has recently been shown that human gastric epithelial cells and DCs produce retinoic acid (RA), which regulates the level of inflammation. During H. pylori infection, RA production is reduced, which leads to more intense inflammation and mucosal damage (Bimczok et al. 2015). DCs also play an important role in regulating the development of the adaptive immune response. They promote the development of pro-inflammatory Th1 and Th17 cells, the numbers of which correlate with the severity of gastritis (Hitzler et al. 2012). In the H. pylori-infected gastric mucosa however, DCs are thought to be semi-mature and tolerogenic (Rizzuti et al. 2015), stimulating the development of regulatory T cells (Tregs) which suppress inflammation.
Molecular mimicry by H. pylori frequently induces autoreactive antibodies against molecules such as the parietal cell H+, K+-ATPase. It is thought that these antibodies may enhance inflammation and damage in the stomach (Smyk et al. 2014). In addition, Th1 cells secrete the cytokines interferon-gamma (IFNγ) and TNFα, which stimulate macrophages to secrete further pro-inflammatory factors. Th17 cells secrete IL-17A, IL-17F, IL-21, and IL-22, which also stimulate the expression of ROS, RNS, and chemokines, leading to further inflammation and neutrophil recruitment (Hitzler et al. 2012).
3.2 Peptic Ulcer Disease
H. pylori is the leading cause of peptic ulceration, with 95% of duodenal ulcers and 70% gastric ulcers being attributable to the infection (Ford et al. 2016). The presence of these breaks in the lining of the duodenal or gastric mucosa is associated with significant mortality, for example from haemorrhage and perforation.
Chronic inflammation of the antrum resulting from H. pylori infection leads to destruction of delta cells, and subsequent reduction in the level of somatostatin they secrete. As somatostatin inhibits gastrin production from neighbouring G cells, reduced levels of this hormone lead to hypergastrinemia. In the case of antral-predominant gastritis, elevated gastrin levels overstimulate the acid-producing parietal cells of the undamaged corpus resulting in hyperchlorhydria. In some people with antral-predominant gastritis, this increased gastric acid output results in gastric metaplasia of the duodenal epithelium. This permits H. pylori to colonize and cause inflammation, possibly leading to duodenal ulceration. Gastric ulcers may develop in those with corpus-predominant or pan-gastritis, where the acid output is normal or reduced. Low acid output can arise owing to loss of parietal cells resulting from atrophic changes to the corpus mucosa induced by chronic inflammation of this part of the stomach. Despite increased gastrin production from the H. pylori-infected antrum, a state of hypochlorhydria is established. This prevents the development of duodenal ulcers; however, inflammation and damage to the gastric mucosa may result in the development of gastric ulcers. Pre-malignant lesions and gastric adenocarcinoma may also arise as a result of this gastritis pattern (Atherton and Blaser 2009; Malfertheiner 2011).
Peptic ulceration is more frequently found in those with reduced numbers of Tregs in their gastric mucosa, and thus impaired capacity to control inflammation (Cook et al. 2014; Robinson et al. 2008). Gastric Th1 and Th17 cells from the antrum of patients with peptic ulcer disease induce epithelial cells to express higher levels of MHC class II, and exposure to their secreted cytokines leads to activation of mitogen-activated protein (MAP) kinases and transcription factors AP-1 and NF-κB, thereby enhancing the inflammation and damage (Zhou et al. 2007).
3.3 Gastric Adenocarcinoma
Gastric cancer is the fifth most common malignancy worldwide, and there are approximately 100,000 new cases each year (Colquhoun et al. 2015). Most cases are found in Asia, with over two-thirds of those reported in China (Ferlay et al. 2015). It is the third most common cause of cancer-related death, since initial diagnosis is usually at a late stage (Herrero et al. 2014). It can be divided into two subtypes depending on the location: cardia (arising from epithelial cells at the gastroesophageal junction) and non-cardia (arising from the distal stomach). Cardia gastric cancers have similar risk factors to those for oesophageal adenocarcinoma and Barrett’s oesophagus, and are thought to be mostly unrelated to H. pylori infection (Colquhoun et al. 2015). In contrast, non-cardia gastric cancer is strongly associated with H. pylori, with up to 89% of cases attributed to the infection. H. pylori has been classified as a carcinogen, and the risk of gastric cancer development for an infected individual is 1–2% (Plummer et al. 2015).
The two histological types of gastric cancer are classed as intestinal and diffuse. The intestinal type develops along a stepwise progression driven by inflammation. H. pylori infection leads to chronic gastritis which, after several decades, leads to gastric gland atrophy, intestinal metaplasia, dysplasia, and finally adenocarcinoma. H. pylori eradication therapy reduces the incidence of atrophic gastritis, but does not reduce the risk of gastric cancer development unless the eradication is administered prior to pre-malignant changes (Malfertheiner et al. 2006).
Gastric carcinogenesis is associated with ROS/RNS-mediated DNA damage, the silencing of tumour suppressor genes via DNA methylation, histone epigenetic modifications, and epithelial–mesenchymal transition (Na and Woo 2014) (see Chapters “Exploiting the Gastric Epithelial Barrier: Helicobacter pylori’s Attack on Tight and Adherens Junctions” and “ Helicobacter pylori-Mediated Genetic Instability and Gastric Carcinogenesis”). Gene polymorphisms associated with a higher risk of gastric adenocarcinoma tend to result in more severe inflammation, mediated by genetically determined high expression of pro-inflammatory cytokines (IL-6, IL-8, TNFα, IL-1β), low expression of anti-inflammatory cytokines (IL-10, TGFβ), or enhanced responsiveness to bacterial components (Toll-like receptors 1, 2, 4, 5, and 9) (Ramis et al. 2015; El-Omar et al. 2008). High-level Th17 and Th22 responses are associated with increased gastric cancer progression and poor survival, probably because the cytokines that they secrete favour angiogenesis and increased tumour invasiveness (Liu et al. 2012). The Th1 response also contributes to carcinogenesis, but there is evidence that this includes stronger anti-tumour immunity, and thus a better prognosis for gastric cancer patients. Treg responses are important for controlling inflammation; however, as they inhibit anti-tumour immunity, having high levels of these cells is an indication of poor prognosis (Hou et al. 2014).
3.4 MALT Lymphoma
H. pylori infection is present in virtually all patients with gastric MALT lymphoma, but this outcome occurs rarely (approximately 0.8 per 100,000 per year). Around 10% of cases are thought to be independent of H. pylori, but may be due to an undiagnosed H. pylori infection, or perhaps gastric non-pylori Helicobacters. H. pylori-mediated inflammation induces the formation of lymphoid follicles in the gastric mucosa, which are not present in the uninfected stomach (Genta et al. 1993). Uncontrolled expansion of marginal zone B cells in these lymphoid follicles occurs as a consequence of chronic inflammation and continuous antigenic stimulation (Du and Atherton 2006). The tumour cells are commonly disseminated throughout the gastric mucosa and often remain localized to this site. Spread to regional lymph nodes and more distant mucosal sites, however, occurs in approximately 40% of cases. Low-grade MALT lymphomas may transform into more aggressive diffuse large B cell lymphomas (DLBCL). This occurs in around half of gastric lymphoma cases, which have a considerably worse prognosis (Du and Atherton 2006).
Low-grade B cell MALT lymphomas usually regress following H. pylori eradication treatment. Chromosomal translocation t(11; 18), the most common genetic aberration in gastric MALT lymphoma, is found in one-quarter of cases, and more frequently when advanced to stage II or above. This chromosomal breakage and translocation results in fusion between the activator protein-12 (AP-12) and MALT-1 genes, and the product of this stimulates activation of the transcription factor NF-κB, which regulates the expression of anti-apoptotic genes and cell survival (Du and Atherton 2006). The presence of t(11; 18) also predicts the non-responsiveness of gastric MALT lymphoma to H. pylori eradication therapy (Fischbach 2014). Mutations in immunoglobulin heavy chain variable region (IGHV) genes are also frequently present, and there is a bias in the usage of certain IGHV gene families, suggesting that tumour cells have undergone antigen selection in germinal centres (Zucca and Bertoni 2016). Bacterial virulence factors do not seem to greatly influence the risk of developing gastric MALT lymphoma; however, there is growing evidence that host genetic factors play an important role.
4 H. pylori Virulence Factors and their Association with Disease
H. pylori expresses several factors that are strongly associated with increased risk of disease development. These include toxins, adhesins, and chemoattractants. Many are highly polymorphic, phase variable, and have diverse functions. For further information, see Chapters “Human and Helicobacter pylori Interactions Determine the Outcome of Gastric Diseases”, “Immune Evasion Strategies and Persistence of Helicobacter pylori ” and “Structural Insights into Helicobacter pylori Cag Protein Interactions with Host Cell Factors”.
4.1 The cag Pathogenicity Island
As described in detail in Chapter “Structural Insights into Helicobacter pylori Cag Protein Interactions with Host Cell Factors”, the cagPAI is a 40 kB horizontally transmitted segment of DNA. It encodes a type IV secretion system (T4SS), with many of the expressed subunits forming a pilus through which CagA, peptidoglycan peptides, and other components are transferred into the host cell cytoplasm. CagL is found at the tip of the T4SS pilus structure and binds α5β1 integrin on epithelial cells (Kwok et al. 2007). Upon interaction of CagL with the integrin, and transfer of CagA and peptidoglycan peptides into cells via the pilus, the transcription factor NF-κB is activated, enters the nucleus, and induces the expression of pro-inflammatory cytokines and chemokines, most notably IL-8 and CCL20 (Cook et al. 2014; Gorrell et al. 2013). CagA rapidly interacts with signalling molecules in the cell cytoplasm. It is tyrosine-phosphorylated at its EPIYA (Glu-Pro-Ile-Tyr-Ala) motifs by Src kinases and interacts with SHP-2 phosphatase, leading to cytoskeletal changes, NF-κB activation and further pro-inflammatory gene expression (Tegtmeyer et al. 2011; Mueller et al. 2012). Unphosphorylated CagA interacts with the tight junction protein ZO-1, causing disruption of tight junctions between epithelial cells, and with E-cadherin, promoting the α-catenin-mediated upregulation of genes with oncogenic potential (Amieva et al. 2003; Franco et al. 2005).
The cagPAI may be fully complete and functional, or it may be partially present or absent. Strains with a functional cag T4SS are strongly associated with increased gastric cancer risk. The cagA gene is polymorphic, with EPIYA motifs categorized as EPIYA-A, B, C, or D depending on their flanking sequences (Backert et al. 2010). EPIYA-A, EPIYA-B, and EPIYA-C motifs are usually present in Western CagA strain types whilst EPIYA-A, EPIYA-B, and EPIYA-D motifs are commonly found in East Asian CagA (Lind et al. 2014, 2016). A larger number of EPIYA-C motifs or the presence of an EPIYA-D increases the strength of SHP-2 interactions, and is associated with a higher risk of intestinal metaplasia and gastric cancer (Amieva and Peek 2016).
4.2 Vacuolating Cytotoxin (VacA)
VacA is a pore-forming toxin, originally named for its ability to induce vacuolation in gastric epithelial cells in vitro [recently reviewed by Foegeding et al. (2016)]. A wide range of functions have now been identified, including the induction of epithelial cell apoptosis, autophagy, and inhibition of T cell activation, and many of these effects depend on its formation of anion-selective channels (Kim and Blanke 2012; Terebiznik et al. 2009; Gebert et al. 2003). The vacA gene is present in almost all strains, and is highly polymorphic, with two alternative allelic variants for the signal (s1/s2), intermediate (i1/i2), and mid (m1/m2)-regions. The mid-region type is important for binding to epithelial cells, with m1 forms binding to a wider range of cell types than m2 forms of the toxin. s2 and i2 types of VacA also have reduced vacuolating activity compared to the s1 and i1 variants (Atherton et al. 1995; Rhead et al. 2007). All forms of VacA appear to be important in the tolerization of dendritic cells, promoting the differentiation of Treg cells and protecting against asthma in a mouse model (Oertli et al. 2013).
The vacA s1 and i1 alleles are associated with increased risk of peptic ulceration, atrophy, and gastric adenocarcinoma; however, the amount that is expressed is also important. A genetic determinant of increased vacA expression has recently been reported, consisting of a putative stem-loop structure in the 5′ untranslated region of the transcript (Amilon et al. 2015). The presence of this stem-loop region in colonizing strains is associated with more severe inflammation and pre-malignant pathology in the human gastric mucosa (Sinnett et al. 2016).
Genotypic analysis of H. pylori clinical isolates from around the world has shown that the majority of cagPAI-positive strains are vacA s1/i1 type whilst cagPAI-negative strains are usually vacA s2/i2 type. This makes it difficult to definitively determine the contribution of each individual factor to gastric disease. This association is not due to clonality or genetic linkage, and a simple functional dependence is not responsible either, as cagA knockouts still retain vacuolating activity (Tummuru et al. 1994), and a vacA null mutant strain still delivers CagA into AGS cells inducing a hummingbird phenotype and IL-8 secretion (Argent et al. 2008). However, mutagenesis studies suggest that CagA and VacA may downregulate each other’s effect on epithelial cells presumably to avoid excessive damage to host gastric cells during infection (Argent et al., 2008). Both CagA and VacA localize to lipid rafts (Asahi et al.2003; Nakayama et al. 2006), where CagA associates with tyrosine-phosphorylated GIT1/Cat-1 (G protein-coupled receptor kinase-interactor 1/Cool-associated, tyrosine-phosphorylated 1). GIT1 is an important scaffold protein involved in signalling mechanisms that regulate cytoskeletal dynamics and membrane trafficking, processes central to hummingbird formation and vacuolation. GIT1 is phosphorylated by Src and FAK (focal adhesion kinase) kinases, the latter inactivated by phosphorylated CagA (Tsutsumi et al. 2006), and is dephosphorylated by receptor-like protein–tyrosine phosphatase-β (RPTPβ), the receptor for VacA. Studies have shown that CagA decreases the tyrosine phosphorylation of GIT1 (Asahi et al. 2003) whilst VacA binding to RPTPβ increases it (Fujikawa et al. 2003). Thus, functional interaction between CagA and VacA may be acting through GIT1-regulated signalling. There may also be interaction between these two virulence factors acting through NFAT (nuclear factor of activated T cells) signalling. CagA upregulates the expression of NFAT-regulated genes through stimulation of calcineurin (Yokoyama et al. 2005). However, the anion channel properties of VacA interfere with the calcium ion influx required for calcineurin activity, reducing NFAT activation (Boncristiano et al. 2003; Gebert et al. 2003). In addition to differential effects on signalling pathways, CagA inhibits the endocytosis of VacA, reducing the toxin’s ability to induce vacuolation and apoptosis (Akada et al. 2010; Oldani et al. 2009). If VacA channels in the epithelial cell plasma membrane benefit the bacteria by releasing nutrients or urea, there may be a selective advantage in inhibiting its endocytosis. CagA can also increase the uptake of transferrin across the basolateral surface of polarized epithelial cells, whilst VacA redirects the internalized transferrin/transferrin receptor complex to the apical surface of the cell (Tan et al. 2011). In this way, CagA and VacA may work together to modify iron trafficking to support the growth of H. pylori microcolonies on the epithelial surface.
4.3 DupA and tfs4
Duodenal ulcer-promoting gene A, dupA, is present in the tfs4 gene cluster along with other vir gene homologues which are thought to encode a type IV secretion system. As the name indicates, this was initially described as associated with duodenal ulcer disease, and dupA+ strains were reported to induce increased IL-8 expression in the antral gastric mucosa. dupA− clinical isolates and null mutants were also impaired in their ability to stimulate IL-12 production from peripheral blood mononuclear cells and monocytes, compared to dupA+ isolates and wild-type strains (Lu et al. 2005; Hussein et al. 2010). Not all studies have been able to demonstrate an association with duodenal ulcer disease, however. This is probably because an intact tfs4 gene cluster is required for virulence rather than dupA alone.
4.4 NapA
H. pylori neutrophil activating protein (NapA, sometimes also called HP-NAP) is a highly conserved dodecameric 150-kDa protein, which is able to stimulate the activation and production of oxygen radicals by neutrophils. The protein is a neutrophil chemoattractant, stimulating these cells to produce pro-inflammatory cytokines and chemokines, and it has been shown to induce a strong Th1 response. NapA may therefore play a central role in H. pylori pathogenesis (de Bernard and D’Elios 2010).
4.5 Adhesins
H. pylori expresses several major adhesins including BabA, SabA, LabA, OipA, and AlpAB. It is thought that adhesins mediate a closer association of the bacteria with the epithelium, and thus enhances exposure to other virulence factors, resulting in increased inflammation and damage to the gastric mucosa. BabA (blood group antigen-binding adhesin) binds to difucosylated Leb blood group antigens on host epithelial cells and mucins, and is the major adhesin involved in the colonization process (Ilver et al. 1998). The babA genes exist in two allelic forms: babA1, lacking the translational start site and signal peptide, and babA2, encoding the full-length, active protein. Expression of functional BabA protein can be modulated by recombination between babA alleles and a closely related locus babB. The babA2 allele has been associated with increased H. pylori colonization density, higher inflammation, and more severe gastric disease, particularly in combination with other virulence determinants such as cagA and the vacA s1 allele (Yu et al. 2002). The increased adherence of babA2-type H. pylori may enhance the virulent actions of CagA- and VacA s1-type toxin. SabA (sialic acid-binding adhesin), which becomes the predominant adhesin in the chronically inflamed stomach, binds to sialylated Lewis antigens (Mahdavi et al. 2002). The expression of functional SabA adhesin is subject to phase variation owing to the presence of dinucleotide repeats near the start of the gene (Mahdavi et al. 2002). Colonization with SabA-expressing strains is associated with an increased risk of gastric cancer (Yamaoka et al. 2006). LabA (lacdiNAc-binding adhesin) is a recently discovered adhesin, which binds a N,N′-diacetyllactosediamine (lacdiNAc) motif on MUC5AC mucin (Rossez et al. 2014). The expression of OipA (outer membrane inflammatory protein) is also controlled by phase variation. OipA-expressing strains are associated with increased risk of duodenal ulcer and gastric cancer, but these are also likely to be cagPAI-positive (Yamaoka and Graham 2014). oipA was originally identified as a gene required for the induction of IL-8 production by epithelial cells. An oipA null mutant strain failed to induce full phosphorylation and activation of FAK in gastric epithelial cells, preventing H. pylori-induced actin stress fibre formation and changes in cell morphology (Tabassam et al. 2008). Interestingly, the effects of oipA mutagenesis on FAK phosphorylation were greater than those observed for a cagPAI deletion mutant. Two further adhesins encoded by adjacent genes alpA and alpB have been shown to be involved in binding to human gastric tissue, and are required for colonization of animal models. AlpAB adhesins from East Asian and Western H. pylori strains have been found to differ in their ability to modulate pro-inflammatory signalling cascades, which may relate to geographical differences in disease outcome (Lu et al. 2007; Odenbreit et al. 2002).
5 Environmental Factors and their Association with Disease
In epidemiological studies, factors including diet, alcohol consumption, and cigarette smoking have been found to influence the risk of developing peptic ulcer disease and gastric cancer (Fang et al. 2015).
Smoking is well known to increase the risk of morbidity from many diseases and cancers outside the respiratory tract (Ordonez-Mena et al. 2016). Cigarette smoke contains hundreds of toxic and carcinogenic compounds, and within the mucosa of the gastrointestinal tract, these are reported to decrease blood flow, increase gastric acid output, skew immune responses, cause cell death, and inhibit cell turnover (Li et al. 2014). Smokers are more likely to be H. pylori-positive, and to develop peptic ulcer disease with ulcers that are frequently more difficult to heal. There is a strong association between smoking and the development of gastric cardia adenocarcinoma, but the association between smoking and non-cardia adenocarcinoma is less convincing as unfortunately most studies have not investigated H. pylori status (Malfertheiner et al. 2012). Investigations of the mechanisms in vitro have shown that nicotine enhances the proliferation and epithelial–mesenchymal transition of gastric epithelial cells; however, cigarette smoke extract and nicotine exposure is reported to have conflicting pro- or anti-inflammatory effects (Goncalves et al. 2011).
The composition of the human diet has an important influence on disease risk. High-salt diets predispose to gastric cancer (Fang et al. 2015), probably because of an exacerbated inflammatory response, and this has also been demonstrated in H. pylori-infected Mongolian gerbils (Loh et al. 2015). The increased risk of disease may be due to the effects on the bacteria as well as the host, since H. pylori expresses increased levels of CagA and VacA when cultured in the presence of high sodium chloride concentrations (Amilon et al. 2015). On the other hand, diets that are high in fruits and vegetables tend to be inversely associated with gastric cancer risk (Fang et al. 2015; Amieva and Peek 2016). A number of clinical trials have demonstrated some significant protective effects from antioxidants, vitamins, and high dietary fibre [reviewed by den Hoed and Kuipers (2016)].
The human gastric mucosa is colonized by bacterial phyla, predominantly including Actinobacteria, Bacteroidetes, Firmicutes, and Proteobacteria (including Helicobacter). The composition of the gastric microbiota differs markedly according to the presence or absence of H. pylori and gastric pathology, particularly as these changes result in alterations of acid production and mucosal mucin expression [reviewed by He et al. (2016)]. Mouse studies have demonstrated that H. pylori infection influences the microbiome of the intestinal tract as well as the stomach, and that the composition of the gastric microbiota influences disease development (He et al. 2016). The main focus of studies on human gastroduodenal disease has thus far centred on the interaction of H. pylori with host cells and mucosal tissue; however, the contributions of the other components of the gastric microbiota are only just beginning to come to light (see Chapter “Impact of the Microbiota and Gastric Disease Development by Helicobacter pylori ”).
6 Treatment of H. pylori and Prospects for a Vaccine
Patients with persistent dyspeptic symptoms are normally referred for endoscopy, and gastric biopsies routinely taken for H. pylori infection diagnosis by a rapid, commercial CLO (Campylobacter-like organism) test based on urease activity, and/or culture of the organism. Breath tests using 13C-labelled urea, serology, and stool antigen testing are also alternative, non-invasive diagnostic methods employed for determining H. pylori status. H. pylori is sensitive to a variety of antibiotics in vitro, but the efficacy of single-drug therapy is limited by the localization of the bacterium within the low pH, viscous environment of the gastric mucus layer. The standard treatment for H. pylori consists of a triple therapy, with two antibiotics (typically clarithromycin and amoxicillin or metronidazole) and a proton pump inhibitor to suppress gastric acid output. This regimen has been proved effective in healing existing ulcers and preventing their recurrence, and it is recommended in various consensus reports and clinical guidelines (Sugano et al. 2015; Malfertheiner et al. 2012). Unfortunately, resistance to clarithromycin and metronidazole is a growing problem, resulting in more numerous treatment failures. The prevalence of antibiotic resistance varies widely around the world and is linked to the consumption of these drugs in each region. Metronidazole resistance is the most common problem, being present in approximately 75% of strains in Africa, 46% in Asia, and around 30% in Europe and the USA. For treatment regimens to be effective, it is therefore recommended that they should be chosen based on susceptibility testing in that region (Sugano et al. 2015).
With such antibiotic resistance issues, vaccination appears the logical approach to control H. pylori; however, progress in this area has not been straightforward despite using a wide range of approaches over the past 30 years. These include formulations of whole cell lysates, outer membrane vesicles, single or multiple purified antigens (e.g. urease, catalase, NapA, VacA, CagA, and heat–shock proteins) and DNA vaccines, with mucosal or parenteral delivery systems and adjuvants (Blanchard and Nedrud 2010). The search for new vaccine antigens is continuing using genomic and proteomic approaches (Walduck et al. 2015).
Since H. pylori infections are usually acquired in early childhood, it would be difficult to ensure that prophylactic vaccines are administered at an early enough stage. The most practical alternative is therefore to administer a therapeutic vaccine to eradicate the infection in people who are already colonized. In Helicobacter-infected animal models, therapeutic immunization has been shown to reduce the bacterial load as well as protecting against a subsequent reinfection (Ikewaki et al. 2000; Rossi et al. 2004). A commonly identified problem with therapeutic vaccines in particular, however, is the phenomenon of post-immunization gastritis. This has been reported in mice (Garhart et al. 2002; Sutton et al. 2001), rhesus monkeys (Solnick et al. 2000), and gnotobiotic piglets (Krakowka et al. 1991), and seems to result from the inflammatory response to residual colonizing bacteria. In humans, phase 1 trials have been conducted and the vaccine formulations tested appear safe and immunogenic (Michetti et al. 1999; Kotloff et al. 2001). An avirulent H. pylori strain has been developed so that immunization-challenge studies can be carried out in humans (Graham et al. 2004).
Trials in H. pylori-infected adult humans have been rather disappointing [reviewed in Anderl and Gerhard (2014)]. Recently, however, a phase 3 clinical trial of a H. pylori vaccine based on recombinant urease B subunit fused to heat-labile enterotoxin B subunit showed an efficacy of 71.8% in preventing H. pylori infection in H. pylori-naïve children aged 6–15 years within 1 year post-immunization (Zeng et al. 2015). This study demonstrates that continued development of effective vaccines coupled with early immunization of young children could be an effective approach to prevent H. pylori-related disease in future generations.
7 Concluding Remarks
The most common outcome of H. pylori infection is chronic asymptomatic gastritis, and this is probably because the bacteria have adapted to evade and suppress the immune response. Disease outcome is determined by the complex interplay of multiple host, bacterial and environmental factors. The chronic inflammatory response is undoubtedly of extreme importance in disease pathogenesis; however, the mechanisms are not yet completely understood. As research progresses, it may become possible to develop prognostic tests, based on the important risk factors, to predict who might develop gastric cancer in the future. It will be important to ensure that effective antibiotic treatments or vaccines are available for these individuals in particular.
References
Ai TL, Solomon BD, Hsieh CS (2014) T-cell selection and intestinal homeostasis. Immunol Rev 259(1):60–74. doi:10.1111/imr.12171
Aihara E, Closson C, Matthis AL, Schumacher MA, Engevik AC, Zavros Y, Ottemann KM, Montrose MH (2014) Motility and chemotaxis mediate the preferential colonization of gastric injury sites by Helicobacter pylori. PLoS Pathog 10(7):e1004275. doi:10.1371/journal.ppat.1004275
Akada JK, Aoki H, Torigoe Y, Kitagawa T, Kurazono H, Hoshida H, Nishikawa J, Terai S, Matsuzaki M, Hirayama T, Nakazawa T, Akada R, Nakamura K (2010) Helicobacter pylori CagA inhibits endocytosis of cytotoxin VacA in host cells. Disease models & mechanisms 3(9–10):605–617. doi:10.1242/dmm.004879
Amieva M, Peek RM Jr (2016) Pathobiology of Helicobacter pylori-induced gastric cancer. Gastroenterology 150(1):64–78. doi:10.1053/j.gastro.2015.09.004
Amieva MR, Vogelmann R, Covacci A, Tompkins LS, Nelson WJ, Falkow S (2003) Disruption of the epithelial apical-junctional complex by Helicobacter pylori CagA. Science 300(5624):1430–1434
Amilon KR, Letley DP, Winter JA, Robinson K, Atherton JC (2015) Expression of the Helicobacter pylori virulence factor vacuolating cytotoxin A (vacA) is influenced by a potential stem-loop structure in the 5′ untranslated region of the transcript. Mol Microbiol 98(5):831–846. doi:10.1111/mmi.13160
Anderl F, Gerhard M (2014) Helicobacter pylori vaccination: is there a path to protection? World J Gastroenterology : WJG 20(34):11939–11949. doi:10.3748/wjg.v20.i34.11939
Argent RH, Thomas RJ, Letley DP, Rittig MG, Hardie KR, Atherton JC (2008) Functional association between the Helicobacter pylori virulence factors VacA and CagA. J Med Microbiol 57(Pt 2):145–150. doi:10.1099/jmm.0.47465-0
Asahi M, Tanaka Y, Izumi T, Ito Y, Naiki H, Kersulyte D, Tsujikawa K, Saito M, Sada K, Yanagi S, Fujikawa A, Noda M, Itokawa Y (2003) Helicobacter pylori CagA containing ITAM-like sequences localized to lipid rafts negatively regulates VacA-induced signaling in vivo. Helicobacter 8(1):1–14
Atherton JC (2006) The pathogenesis of Helicobacter pylori-induced gastro-duodenal diseases. Ann Rev Pathol 1:63–96. doi:10.1146/annurev.pathol.1.110304.100125
Atherton JC, Blaser MJ (2009) Coadaptation of Helicobacter pylori and humans: ancient history, modern implications. J Clin Invest 119(9):2475–2487. doi:10.1172/JCI38605
Atherton JC, Cao P, Peek RM Jr, Tummuru MK, Blaser MJ, Cover TL (1995) Mosaicism in vacuolating cytotoxin alleles of Helicobacter pylori. Association of specific vacA types with cytotoxin production and peptic ulceration. J Biol Chem 270(30):17771–17777
Backert S, Tegtmeyer N, Selbach M (2010) The versatility of Helicobacter pylori CagA effector protein functions: the master key hypothesis. Helicobacter 15(3):163–176. doi:10.1111/j.1523-5378.2010.00759.x
Baron JH, Sonnenberg A (2001) Period- and cohort-age contours of deaths from gastric and duodenal ulcer in New York 1804–1998. Am J Gastroenterol 96(10):2887–2891. doi:10.1111/j.1572-0241.2001.04243.x
Bauer B, Pang E, Holland C, Kessler M, Bartfeld S, Meyer TF (2012) The Helicobacter pylori virulence effector CagA abrogates human beta-defensin 3 expression via inactivation of EGFR signaling. Cell Host Microbe 11(6):576–586. doi:10.1016/j.chom.2012.04.013
Bimczok D, Kao JY, Zhang M, Cochrun S, Mannon P, Peter S, Wilcox CM, Monkemuller KE, Harris PR, Grams JM, Stahl RD, Smith PD, Smythies LE (2015) Human gastric epithelial cells contribute to gastric immune regulation by providing retinoic acid to dendritic cells. Mucosal Immunol. doi:10.1038/mi.2014.86
Blanchard TG, Nedrud JG (2010) Helicobacter pylori vaccines. In: Sutton P, Mitchell H (eds) Helicobacter pylori in the 21st century. CAB International, Cambridge, pp 167–189
Blaser MJ, Nomura A, Lee J, Stemmerman GN, Perez-Perez GI (2007) Early-life family structure and microbially induced cancer risk. PLoS Med 4(1):e7. doi:10.1371/journal.pmed.0040007
Boncristiano M, Paccani SR, Barone S, Ulivieri C, Patrussi L, Ilver D, Amedei A, D’Elios MM, Telford JL, Baldari CT (2003) The Helicobacter pylori vacuolating toxin inhibits T cell activation by two independent mechanisms. J Exp Med 198(12):1887–1897
Breckan RK, Paulssen EJ, Asfeldt AM, Kvamme JM, Straume B, Florholmen J (2016) The all-age prevalence of Helicobacter pylori infection and potential transmission routes. A population-based study. Helicobacter 21(6):586–595. doi:10.1111/hel.12316
Celli JP, Turner BS, Afdhal NH, Keates S, Ghiran I, Kelly CP, Ewoldt RH, McKinley GH, So P, Erramilli S, Bansil R (2009) Helicobacter pylori moves through mucus by reducing mucin viscoelasticity. Proc Natl Acad Sci U S A 106(34):14321–14326. doi:10.1073/pnas.0903438106
Chen J, Gong TT, Wu QJ (2016) Parity and gastric cancer risk: a systematic review and dose-response meta-analysis of prospective cohort studies. Sci Rep 6:18766. doi:10.1038/srep18766
Colquhoun A, Arnold M, Ferlay J, Goodman KJ, Forman D, Soerjomataram I (2015) Global patterns of cardia and non-cardia gastric cancer incidence in 2012. Gut 64(12):1881–1888. doi:10.1136/gutjnl-2014-308915
Cook KW, Letley DP, Ingram RJ, Staples E, Skjoldmose H, Atherton JC, Robinson K (2014) CCL20/CCR6-mediated migration of regulatory T cells to the Helicobacter pylori-infected human gastric mucosa. Gut 63(10):1550–1559. doi:10.1136/gutjnl-2013-306253
de Bernard M, D’Elios MM (2010) The immune modulating activity of the Helicobacter pylori HP-NAP: friend or foe? Toxicon (Official Journal of the International Society on Toxinology) 56(7):1186–1192. doi:10.1016/j.toxicon.2009.09.020
den Hoed CM, Kuipers EJ (2016) Gastric cancer: how can we reduce the incidence of this disease? Curr Gastroenterol Rep 18(7):34. doi:10.1007/s11894-016-0506-0
Du MQ, Atherton JC (2006) Molecular subtyping of gastric MALT lymphomas: implications for prognosis and management. Gut 55(6):886–893
El-Omar EM, Ng MT, Hold GL (2008) Polymorphisms in toll-like receptor genes and risk of cancer. Oncogene 27(2):244–252
Fang X, Wei J, He X, An P, Wang H, Jiang L, Shao D, Liang H, Li Y, Wang F, Min J (2015) Landscape of dietary factors associated with risk of gastric cancer: a systematic review and dose-response meta-analysis of prospective cohort studies. Eur J Cancer 51(18):2820–2832. doi:10.1016/j.ejca.2015.09.010
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386. doi:10.1002/ijc.29210
Fischbach W (2014) Gastric MALT lymphoma—update on diagnosis and treatment. Best Pract Res Clin Gastroenterol 28(6):1069–1077. doi:10.1016/j.bpg.2014.09.006
Foegeding NJ, Caston RR, McClain MS, Ohi MD, Cover TL (2016) An overview of Helicobacter pylori VacA toxin biology. Toxins 8(6). doi:10.3390/toxins8060173
Ford AC, Gurusamy KS, Delaney B, Forman D, Moayyedi P (2016) Eradication therapy for peptic ulcer disease in Helicobacter pylori-positive people. Cochrane Database Syst Rev 4:CD003840. doi:10.1002/14651858.CD003840.pub5
Franco AT, Israel DA, Washington MK, Krishna U, Fox JG, Rogers AB, Neish AS, Collier-Hyams L, Perez-Perez GI, Hatakeyama M, Whitehead R, Gaus K, O’Brien DP, Romero-Gallo J, Peek RM Jr (2005) Activation of beta-catenin by carcinogenic Helicobacter pylori. Proc Natl Acad Sci U S A 102(30):10646–10651. doi:10.1073/pnas.0504927102 0504927102 [pii]
Fujikawa A, Shirasaka D, Yamamoto S, Ota H, Yahiro K, Fukada M, Shintani T, Wada A, Aoyama N, Hirayama T, Fukamachi H, Noda M (2003) Mice deficient in protein tyrosine phosphatase receptor type Z are resistant to gastric ulcer induction by VacA of Helicobacter pylori. Nature Genetics 33(3):375–381. doi:10.1038/ng1112
Garhart CA, Redline RW, Nedrud JG, Czinn SJ (2002) Clearance of Helicobacter pylori infection and resolution of postimmunization gastritis in a kinetic study of prophylactically immunized mice. Infect Immun 70(7):3529–3538
Gebert B, Fischer W, Weiss E, Hoffmann R, Haas R (2003) Helicobacter pylori vacuolating cytotoxin inhibits T lymphocyte activation. Science 301(5636):1099–1102
Genta RM, Hamner HW, Graham DY (1993) Gastric lymphoid follicles in Helicobacter pylori infection: frequency, distribution, and response to triple therapy. Hum Pathol 24(6):577–583
Global Burden of Disease Cancer C, Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre MF, Allen C, Hansen G, Woodbrook R, Wolfe C, Hamadeh RR, Moore A, Werdecker A, Gessner BD, Te Ao B, McMahon B, Karimkhani C, Yu C, Cooke GS, Schwebel DC, Carpenter DO, Pereira DM, Nash D, Kazi DS, De Leo D, Plass D, Ukwaja KN, Thurston GD, Yun Jin K, Simard EP, Mills E, Park EK, Catala-Lopez F, deVeber G, Gotay C, Khan G, Hosgood HD III, Santos IS, Leasher JL, Singh J, Leigh J, Jonas JB, Sanabria J, Beardsley J, Jacobsen KH, Takahashi K, Franklin RC, Ronfani L, Montico M, Naldi L, Tonelli M, Geleijnse J, Petzold M, Shrime MG, Younis M, Yonemoto N, Breitborde N, Yip P, Pourmalek F, Lotufo PA, Esteghamati A, Hankey GJ, Ali R, Lunevicius R, Malekzadeh R, Dellavalle R, Weintraub R, Lucas R, Hay R, Rojas-Rueda D, Westerman R, Sepanlou SG, Nolte S, Patten S, Weichenthal S, Abera SF, Fereshtehnejad SM, Shiue I, Driscoll T, Vasankari T, Alsharif U, Rahimi-Movaghar V, Vlassov VV, Marcenes WS, Mekonnen W, Melaku YA, Yano Y, Artaman A, Campos I, MacLachlan J, Mueller U, Kim D, Trillini M, Eshrati B, Williams HC, Shibuya K, Dandona R, Murthy K, Cowie B, Amare AT, Antonio CA, Castaneda-Orjuela C, van Gool CH, Violante F, Oh IH, Deribe K, Soreide K, Knibbs L, Kereselidze M, Green M, Cardenas R, Roy N, Tillmann T, Li Y, Krueger H, Monasta L, Dey S, Sheikhbahaei S, Hafezi-Nejad N, Kumar GA, Sreeramareddy CT, Dandona L, Wang H, Vollset SE, Mokdad A, Salomon JA, Lozano R, Vos T, Forouzanfar M, Lopez A, Murray C, Naghavi M (2015) The global burden of cancer 2013. JAMA Oncol 1(4):505–527. doi:10.1001/jamaoncol.2015.0735
Gobert AP, McGee DJ, Akhtar M, Mendz GL, Newton JC, Cheng Y, Mobley HL, Wilson KT (2001) Helicobacter pylori arginase inhibits nitric oxide production by eukaryotic cells: a strategy for bacterial survival. Proc Natl Acad Sci U S A 98(24):13844–13849
Goncalves RB, Coletta RD, Silverio KG, Benevides L, Casati MZ, da Silva JS, Nociti FH Jr (2011) Impact of smoking on inflammation: overview of molecular mechanisms. Inflamm Res (Official Journal of the European Histamine Research Society [et al]) 60(5):409–424. doi:10.1007/s00011-011-0308-7
Gorrell RJ, Guan J, Xin Y, Tafreshi MA, Hutton ML, McGuckin MA, Ferrero RL, Kwok T (2013) A novel NOD1- and CagA-independent pathway of interleukin-8 induction mediated by the Helicobacter pylori type IV secretion system. Cell Microbiol 15(4):554–570. doi:10.1111/cmi.12055
Graham DY, Opekun AR, Osato MS, El-Zimaity HM, Lee CK, Yamaoka Y, Qureshi WA, Cadoz M, Monath TP (2004) Challenge model for Helicobacter pylori infection in human volunteers. Gut 53(9):1235–1243. doi:10.1136/gut.2003.037499
Graham DY, Lu H, Yamaoka Y (2009) African, Asian or Indian enigma, the East Asian Helicobacter pylori: facts or medical myths. J Dig Dis 10(2):77–84. doi:10.1111/j.1751-2980.2009.00368.x
He C, Yang Z, Lu N (2016) Imbalance of gastrointestinal microbiota in the pathogenesis of Helicobacter pylori-associated diseases. Helicobacter 21(5):337–348. doi:10.1111/hel.12297
Herrero R, Park JY, Forman D (2014) The fight against gastric cancer—the IARC Working Group report. Best Pract Res Clin Gastroenterol 28(6):1107–1114. doi:10.1016/j.bpg.2014.10.003
Hitzler I, Kohler E, Engler DB, Yazgan AS, Muller A (2012) The role of Th cell subsets in the control of Helicobacter infections and in T cell-driven gastric immunopathology. Front Immunol 3:142. doi:10.3389/fimmu.2012.00142
Hou J, Yu Z, Xiang R, Li C, Wang L, Chen S, Li Q, Chen M, Wang L (2014) Correlation between infiltration of FOXP3+ regulatory T cells and expression of B7-H1 in the tumor tissues of gastric cancer. Exp Mol Pathol 96(3):284–291. doi:10.1016/j.yexmp.2014.03.005
Huang JY, Sweeney EG, Sigal M, Zhang HC, Remington SJ, Cantrell MA, Kuo CJ, Guillemin K, Amieva MR (2015) Chemodetection and destruction of host urea allows Helicobacter pylori to locate the epithelium. Cell Host Microbe 18(2):147–156. doi:10.1016/j.chom.2015.07.002
Hussein NR, Argent RH, Marx CK, Patel SR, Robinson K, Atherton JC (2010) Helicobacter pylori dupA is polymorphic, and its active form induces proinflammatory cytokine secretion by mononuclear cells. J Infect Dis 202(2):261–269. doi:10.1086/653587
Ikewaki J, Nishizono A, Goto T, Fujioka T, Mifune K (2000) Therapeutic oral vaccination induces mucosal immune response sufficient to eliminate long-term Helicobacter pylori infection. Microbiol Immunol 44(1):29–39
Ilver D, Arnqvist A, Ogren J, Frick IM, Kersulyte D, Incecik ET, Berg DE, Covacci A, Engstrand L, Boren T (1998) Helicobacter pylori adhesin binding fucosylated histo-blood group antigens revealed by retagging. Science 279(5349):373–377
Italiani P, Boraschi D (2014) From monocytes to M1/M2 macrophages: phenotypical vs. functional differentiation. Front Immunol 5:514. doi:10.3389/fimmu.2014.00514
Keilberg D, Ottemann KM (2016) How Helicobacter pylori senses, targets and interacts with the gastric epithelium. Environ Microbiol 18(3):791–806. doi:10.1111/1462-2920.13222
Kim IJ, Blanke SR (2012) Remodeling the host environment: modulation of the gastric epithelium by the Helicobacter pylori vacuolating toxin (VacA). Front Cell Infect Microbiol 2:37. doi:10.3389/fcimb.2012.00037
Kim DJ, Park JH, Franchi L, Backert S, Núñez G (2013) The Cag pathogenicity island and interaction between TLR2/NOD2 and NLRP3 regulate IL-1β production in Helicobacter pylori infected dendritic cells. Eur J Immunol 43(10):2650–2658. doi:10.1002/eji.201243281
Kodaman N, Pazos A, Schneider BG, Piazuelo MB, Mera R, Sobota RS, Sicinschi LA, Shaffer CL, Romero-Gallo J, de Sablet T, Harder RH, Bravo LE, Peek RM Jr, Wilson KT, Cover TL, Williams SM, Correa P (2014) Human and Helicobacter pylori coevolution shapes the risk of gastric disease. Proc Natl Acad Sci U S A 111(4):1455–1460. doi:10.1073/pnas.1318093111
Kotloff KL, Sztein MB, Wasserman SS, Losonsky GA, DiLorenzo SC, Walker RI (2001) Safety and immunogenicity of oral inactivated whole-cell Helicobacter pylori vaccine with adjuvant among volunteers with or without subclinical infection. Infect Immun 69(6):3581–3590
Krakowka S, Eaton KA, Rings DM, Morgan DR (1991) Gastritis induced by Helicobacter pylori in gnotobiotic piglets. Rev Infect Dis 13(Suppl 8):S681–S685
Kwok T, Zabler D, Urman S, Rohde M, Hartig R, Wessler S, Misselwitz R, Berger J, Sewald N, Konig W, Backert S (2007) Helicobacter exploits integrin for type IV secretion and kinase activation. Nature 449(7164):862–866. doi:10.1038/nature06187
Li LF, Chan RL, Lu L, Shen J, Zhang L, Wu WK, Wang L, Hu T, Li MX, Cho CH (2014) Cigarette smoking and gastrointestinal diseases: the causal relationship and underlying molecular mechanisms (review). Int J Mol Med 34(2):372–380. doi:10.3892/ijmm.2014.1786
Lind J, Backert S, Pfleiderer K, Berg DE, Yamaoka Y, Sticht H, Tegtmeyer N (2014) Systematic analysis of phosphotyrosine antibodies recognizing single phosphorylated EPIYA-motifs in CagA of Western-type Helicobacter pylori strains. PLoS ONE 9(5):e96488. doi:10.1371/journal.pone.0096488
Lind J, Backert S, Hoffmann R, Eichler J, Yamaoka Y, Perez-Perez GI, Torres J, Sticht H, Tegtmeyer N (2016) Systematic analysis of phosphotyrosine antibodies recognizing single phosphorylated EPIYA-motifs in CagA of East Asian-type Helicobacter pylori strains. BMC Microbiol 16(1):201. doi:10.1186/s12866-016-0820-6
Liu T, Peng L, Yu P, Zhao Y, Shi Y, Mao X, Chen W, Cheng P, Wang T, Chen N, Zhang J, Liu X, Li N, Guo G, Tong W, Zhuang Y, Zou Q (2012) Increased circulating Th22 and Th17 cells are associated with tumor progression and patient survival in human gastric cancer. J Clin Immunol 32(6):1332–1339. doi:10.1007/s10875-012-9718-8
Loh JT, Gaddy JA, Algood HM, Gaudieri S, Mallal S, Cover TL (2015) Helicobacter pylori adaptation in vivo in response to a high-salt diet. Infect Immun 83(12):4871–4883. doi:10.1128/IAI.00918-15
Lu H, Hsu PI, Graham DY, Yamaoka Y (2005) Duodenal ulcer promoting gene of Helicobacter pylori. Gastroenterology 128(4):833–848
Lu H, Wu JY, Beswick EJ, Ohno T, Odenbreit S, Haas R, Reyes VE, Kita M, Graham DY, Yamaoka Y (2007) Functional and intracellular signaling differences associated with the Helicobacter pylori AlpAB adhesin from Western and East Asian strains. J Biol Chem 282(9):6242–6254. doi:10.1074/jbc.M611178200
Luther J, Owyang SY, Takeuchi T, Cole TS, Zhang M, Liu M, Erb-Downward J, Rubenstein JH, Chen CC, Pierzchala AV, Paul JA, Kao JY (2011) Helicobacter pylori DNA decreases pro-inflammatory cytokine production by dendritic cells and attenuates dextran sodium sulphate-induced colitis. Gut 60(11):1479–1486. doi:10.1136/gut.2010.220087
Macarthur M, Hold GL, El-Omar EM (2004) Inflammation and cancer II. Role of chronic inflammation and cytokine gene polymorphisms in the pathogenesis of gastrointestinal malignancy. Am J Physiol Gastrointest Liver Physiol 286(4):G515–G520
Mahdavi J, Sonden B, Hurtig M, Olfat FO, Forsberg L, Roche N, Angstrom J, Larsson T, Teneberg S, Karlsson KA, Altraja S, Wadstrom T, Kersulyte D, Berg DE, Dubois A, Petersson C, Magnusson KE, Norberg T, Lindh F, Lundskog BB, Arnqvist A, Hammarstrom L, Boren T (2002) Helicobacter pylori SabA adhesin in persistent infection and chronic inflammation. Science 297(5581):573–578. doi:10.1126/science.1069076
Malfertheiner P (2011) The intriguing relationship of Helicobacter pylori infection and acid secretion in peptic ulcer disease and gastric cancer. Dig Dis 29(5):459–464. doi:10.1159/000332213
Malfertheiner P, Fry LC, Monkemuller K (2006) Can gastric cancer be prevented by Helicobacter pylori eradication? Best Pract Res Clin Gastroenterol 20(4):709–719. doi:10.1016/j.bpg.2006.04.005
Malfertheiner P, Megraud F, O’Morain CA, Atherton J, Axon AT, Bazzoli F, Gensini GF, Gisbert JP, Graham DY, Rokkas T, El-Omar EM, Kuipers EJ, European Helicobacter Study G (2012) Management of Helicobacter pylori infection—the Maastricht IV/Florence consensus report. Gut 61(5):646–664. doi:10.1136/gutjnl-2012-302084
Marshall BJ, Warren JR (1984) Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet 1(8390):1311–1315
Michetti P, Kreiss C, Kotloff KL, Porta N, Blanco JL, Bachmann D, Herranz M, Saldinger PF, Corthesy-Theulaz I, Losonsky G, Nichols R, Simon J, Stolte M, Ackerman S, Monath TP, Blum AL (1999) Oral immunization with urease and Escherichia coli heat-labile enterotoxin is safe and immunogenic in Helicobacter pylori-infected adults. Gastroenterology 116(4):804–812
Mueller D, Tegtmeyer N, Brandt S, Yamaoka Y, De Poire E, Sgouras D, Wessler S, Torres J, Smolka A, Backert S (2012) c-Src and c-Abl kinases control hierarchic phosphorylation and function of the CagA effector protein in Western and East Asian Helicobacter pylori strains. J Clin Invest 122(4):1553–1566. doi:10.1172/jci61143
Munari F, Fassan M, Capitani N, Codolo G, Vila-Caballer M, Pizzi M, Rugge M, Della Bella C, Troilo A, D’Elios S, Baldari CT, D’Elios MM, de Bernard M (2014) Cytokine BAFF released by Helicobacter pylori-infected macrophages triggers the Th17 response in human chronic gastritis. J Immunol 193(11):5584–5594. doi:10.4049/jimmunol.1302865
Na HK, Woo JH (2014) Helicobacter pylori induces hypermethylation of CpG islands through upregulation of DNA methyltransferase: possible involvement of reactive oxygen/nitrogen species. J Cancer Prevent 19(4):259–264. doi:10.15430/JCP.2014.19.4.259
Nagy P, Johansson S, Molloy-Bland M (2016) Systematic review of time trends in the prevalence of Helicobacter pylori infection in China and the USA. Gut Pathog 8:8
Nakayama M, Hisatsune J, Yamasaki E, Nishi Y, Wada A, Kurazono H, Sap J, Yahiro K, Moss J, Hirayama T (2006) Clustering of Helicobacter pylori VacA in lipid rafts, mediated by its receptor, receptor-like protein tyrosine phosphatase beta, is required for intoxication in AZ-521 Cells. Infection and Immunity 74 (12):6571–6580. doi:10.1128/IAI.00356-06
Odenbreit S, Kavermann H, Puls J, Haas R (2002) CagA tyrosine phosphorylation and interleukin-8 induction by Helicobacter pylori are independent from alpAB, HopZ and bab group outer membrane proteins. Int J Med Microbiol 292(3–4):257–266
Oertli M, Sundquist M, Hitzler I, Engler DB, Arnold IC, Reuter S, Maxeiner J, Hansson M, Taube C, Quiding-Jarbrink M, Muller A (2012) DC-derived IL-18 drives Treg differentiation, murine Helicobacter pylori-specific immune tolerance, and asthma protection. J Clin Invest 122(3):1082–1096. doi:10.1172/JCI61029 61029 [pii]
Oertli M, Noben M, Engler DB, Semper RP, Reuter S, Maxeiner J, Gerhard M, Taube C, Muller A (2013) Helicobacter pylori gamma-glutamyl transpeptidase and vacuolating cytotoxin promote gastric persistence and immune tolerance. Proc Natl Acad Sci U S A 110(8):3047–3052. doi:10.1073/pnas.1211248110
Oldani A, Cormont M, Hofman V, Chiozzi V, Oregioni O, Canonici A, Sciullo A, Sommi P, Fabbri A, Ricci V, Boquet P (2009) Helicobacter pylori counteracts the apoptotic action of its VacA toxin by injecting the CagA protein into gastric epithelial cells. PLoS Pathogens 5(10):e1000603. doi:10.1371/journal.ppat.1000603
Ordonez-Mena JM, Schottker B, Mons U, Jenab M, Freisling H, Bueno-de-Mesquita B, O’Doherty MG, Scott A, Kee F, Stricker BH, Hofman A, de Keyser CE, Ruiter R, Soderberg S, Jousilahti P, Kuulasmaa K, Freedman ND, Wilsgaard T, de Groot LC, Kampman E, Hakansson N, Orsini N, Wolk A, Nilsson LM, Tjonneland A, Pajak A, Malyutina S, Kubinova R, Tamosiunas A, Bobak M, Katsoulis M, Orfanos P, Boffetta P, Trichopoulou A, Brenner H, Consortium on H, Ageing: Network of Cohorts in E, the United S (2016) Quantification of the smoking-associated cancer risk with rate advancement periods: meta-analysis of individual participant data from cohorts of the CHANCES consortium. BMC Med 14(1):62. doi:10.1186/s12916-016-0607-5
Patel SR, Smith K, Letley DP, Cook KW, Memon AA, Ingram RJ, Staples E, Backert S, Zaitoun AM, Atherton JC, Robinson K (2013) Helicobacter pylori downregulates expression of human beta-defensin 1 in the gastric mucosa in a type IV secretion-dependent fashion. Cell Microbiol 15(12):2080–2092. doi:10.1111/cmi.12174
Pflock M, Kennard S, Delany I, Scarlato V, Beier D (2005) Acid-induced activation of the urease promoters is mediated directly by the ArsRS two-component system of Helicobacter pylori. Infect Immun 73(10):6437–6445. doi:10.1128/IAI.73.10.6437-6445.2005
Pflock M, Finsterer N, Joseph B, Mollenkopf H, Meyer TF, Beier D (2006) Characterization of the ArsRS regulon of Helicobacter pylori, involved in acid adaptation. J Bacteriol 188(10):3449–3462. doi:10.1128/JB.188.10.3449-3462.2006
Plummer M, Franceschi S, Vignat J, Forman D, de Martel C (2015) Global burden of gastric cancer attributable to Helicobacter pylori. Int J Cancer 136(2):487–490. doi:10.1002/ijc.28999
Quiding-Jarbrink M, Raghavan S, Sundquist M (2010) Enhanced M1 macrophage polarization in human Helicobacter pylori-associated atrophic gastritis and in vaccinated mice. PLoS ONE 5(11):e15018. doi:10.1371/journal.pone.0015018
Ramarao N, Gray-Owen SD, Meyer TF (2000) Helicobacter pylori induces but survives the extracellular release of oxygen radicals from professional phagocytes using its catalase activity. Mol Microbiol 38(1):103–113
Ramis IB, Vianna JS, Goncalves CV, von Groll A, Dellagostin OA, da Silva PE (2015) Polymorphisms of the IL-6, IL-8 and IL-10 genes and the risk of gastric pathology in patients infected with Helicobacter pylori. J Microbiol Immunol Infect = Wei mian yu gan ran za zhi. doi:10.1016/j.jmii.2015.03.002
Rhead JL, Letley DP, Mohammadi M, Hussein N, Mohagheghi MA, Eshagh Hosseini M, Atherton JC (2007) A new Helicobacter pylori vacuolating cytotoxin determinant, the intermediate region, is associated with gastric cancer. Gastroenterology 133(3):926–936
Rizzuti D, Ang M, Sokollik C, Wu T, Abdullah M, Greenfield L, Fattouh R, Reardon C, Tang M, Diao J, Schindler C, Cattral M, Jones NL (2015) Helicobacter pylori inhibits dendritic cell maturation via interleukin-10-mediated activation of the signal transducer and activator of transcription 3 pathway. J Innate Immun 7(2):199–211. doi:10.1159/000368232
Robinson K (2015) Helicobacter pylori-mediated protection against extra-gastric immune and inflammatory disorders: the evidence and controversies. Diseases 3(2):34–55. doi:10.3390/diseases3020034
Robinson K, Kenefeck R, Pidgeon EL, Shakib S, Patel S, Polson RJ, Zaitoun AM, Atherton JC (2008) Helicobacter pylori-induced peptic ulcer disease is associated with inadequate regulatory T cell responses. Gut 57(10):1375–1385
Rossez Y, Gosset P, Boneca IG, Magalhaes A, Ecobichon C, Reis CA, Cieniewski-Bernard C, Joncquel Chevalier Curt M, Leonard R, Maes E, Sperandio B, Slomianny C, Sansonetti PJ, Michalski JC, Robbe-Masselot C (2014) The lacdiNAc-specific adhesin LabA mediates adhesion of Helicobacter pylori to human gastric mucosa. J Infect Dis 210(8):1286–1295. doi:10.1093/infdis/jiu239
Rossi G, Ruggiero P, Peppoloni S, Pancotto L, Fortuna D, Lauretti L, Volpini G, Mancianti S, Corazza M, Taccini E, Di Pisa F, Rappuoli R, Del Giudice G (2004) Therapeutic vaccination against Helicobacter pylori in the beagle dog experimental model: safety, immunogenicity, and efficacy. Infect Immun 72(6):3252–3259
Salama NR, Hartung ML, Muller A (2013) Life in the human stomach: persistence strategies of the bacterial pathogen Helicobacter pylori. Nat Rev Microbiol 11(6):385–399. doi:10.1038/nrmicro3016
Schreiber S, Bucker R, Groll C, Azevedo-Vethacke M, Garten D, Scheid P, Friedrich S, Gatermann S, Josenhans C, Suerbaum S (2005) Rapid loss of motility of Helicobacter pylori in the gastric lumen in vivo. Infect Immun 73(3):1584–1589. doi:10.1128/IAI.73.3.1584-1589.2005
Sinnett CG, Letley DP, Narayanan GL, Patel SR, Hussein NR, Zaitoun AM, Robinson K, Atherton JC (2016) Helicobacter pylori vacA transcription is genetically-determined and stratifies the level of human gastric inflammation and atrophy. J Clin Pathol. doi:10.1136/jclinpath-2016-203641
Smyk DS, Koutsoumpas AL, Mytilinaiou MG, Rigopoulou EI, Sakkas LI, Bogdanos DP (2014) Helicobacter pylori and autoimmune disease: cause or bystander. World J Gastroenterol 20(3):613–629. doi:10.3748/wjg.v20.i3.613
Solnick JV, Canfield DR, Hansen LM, Torabian SZ (2000) Immunization with recombinant Helicobacter pylori urease in specific-pathogen-free rhesus monkeys (Macaca mulatta). Infect Immun 68(5):2560–2565
Sugano K, Tack J, Kuipers EJ, Graham DY, El-Omar EM, Miura S, Haruma K, Asaka M, Uemura N, Malfertheiner P, faculty members of Kyoto Global Consensus C (2015) Kyoto global consensus report on Helicobacter pylori gastritis. Gut 64(9):1353–1367. doi:10.1136/gutjnl-2015-309252
Sutton P, Danon SJ, Walker M, Thompson LJ, Wilson J, Kosaka T, Lee A (2001) Post-immunisation gastritis and Helicobacter infection in the mouse: a long term study. Gut 49(4):467–473
Tabassam FH, Graham DY, Yamaoka Y (2008) OipA plays a role in Helicobacter pylori-induced focal adhesion kinase activation and cytoskeletal re-organization. Cell Microbiol 10(4):1008–1020. doi:10.1111/j.1462-5822.2007.01104.x
Tan S, Noto JM, Romero-Gallo J, Peek RM, Jr, Amieva MR (2011) Helicobacter pylori perturbs iron trafficking in the epithelium to grow on the cell surface. PLoS Pathogens 7(5):e1002050. doi:10.1371/journal.ppat.1002050
Tegtmeyer N, Wessler S, Backert S (2011) Role of the cag-pathogenicity island encoded type IV secretion system in Helicobacter pylori pathogenesis. FEBS J 278(8):1190–1202. doi:10.1111/j.1742-4658.2011.08035.x
Terebiznik MR, Raju D, Vazquez CL, Torbricki K, Kulkarni R, Blanke SR, Yoshimori T, Colombo MI, Jones NL (2009) Effect of Helicobacter pylori’s vacuolating cytotoxin on the autophagy pathway in gastric epithelial cells. Autophagy 5(3):370–379
Tsutsumi R, Takahashi A, Azuma T, Higashi H, Hatakeyama M (2006) Focal adhesion kinase is a substrate and downstream effector of SHP-2 complexed with Helicobacter pylori CagA. Molecular and Cellular Biology 26(1):261–276. doi:10.1128/MCB.26.1.261-276.2006
Tummuru MK, Cover TL, Blaser MJ (1994) Mutation of the cytotoxin-associated cagA gene does not affect the vacuolating cytotoxin activity of Helicobacter pylori. Infect Immun 62(6):2609–2613
Ubukata H, Nagata H, Tabuchi T, Konishi S, Kasuga T, Tabuchi T (2011) Why is the coexistence of gastric cancer and duodenal ulcer rare? Examination of factors related to both gastric cancer and duodenal ulcer. Gastric Cancer (Official Journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association) 14(1):4–12. doi:10.1007/s10120-011-0005-9
Vanaja SK, Rathinam VA, Fitzgerald KA (2015) Mechanisms of inflammasome activation: recent advances and novel insights. Trends Cell Biol 25(5):308–315. doi:10.1016/j.tcb.2014.12.009
Viala J, Chaput C, Boneca IG, Cardona A, Girardin SE, Moran AP, Athman R, Memet S, Huerre MR, Coyle AJ, DiStefano PS, Sansonetti PJ, Labigne A, Bertin J, Philpott DJ, Ferrero RL (2004) Nod1 responds to peptidoglycan delivered by the Helicobacter pylori cag pathogenicity island. Nat Immunol 5(11):1166–1174
Walduck A, Andersen LP, Raghavan S (2015) Inflammation, immunity, and vaccines for Helicobacter pylori infection. Helicobacter 20(Suppl 1):17–25. doi:10.1111/hel.12252
Weeks DL, Eskandari S, Scott DR, Sachs G (2000) A H+-gated urea channel: the link between Helicobacter pylori urease and gastric colonization. Science 287(5452):482–485
Wen Y, Feng J, Scott DR, Marcus EA, Sachs G (2007) The HP0165-HP0166 two-component system (ArsRS) regulates acid-induced expression of HP1186 alpha-carbonic anhydrase in Helicobacter pylori by activating the pH-dependent promoter. J Bacteriol 189(6):2426–2434. doi:10.1128/JB.01492-06
White JR, Winter JA, Robinson K (2015) Differential inflammatory response to Helicobacter pylori infection: etiology and clinical outcomes. J Inflamm Res 8:137–147. doi:10.2147/JIR.S64888
Wu CY, Wu MS, Kuo KN, Wang CB, Chen YJ, Lin JT (2010) Effective reduction of gastric cancer risk with regular use of nonsteroidal anti-inflammatory drugs in Helicobacter pylori-infected patients. J Clin Oncol (Official Journal of the American Society of Clinical Oncology) 28(18):2952–2957. doi:10.1200/JCO.2009.26.0695
Yamaoka Y, Graham DY (2014) Helicobacter pylori virulence and cancer pathogenesis. Future Oncol 10(8):1487–1500. doi:10.2217/fon.14.29
Yamaoka Y, Ojo O, Fujimoto S, Odenbreit S, Haas R, Gutierrez O, El-Zimaity HM, Reddy R, Arnqvist A, Graham DY (2006) Helicobacter pylori outer membrane proteins and gastroduodenal disease. Gut 55(6):775–781
Yokoyama K, Higashi H, Ishikawa S, Fujii Y, Kondo S, Kato H, Azuma T, Wada A, Hirayama T, Aburatani H, Hatakeyama M (2005) Functional antagonism between Helicobacter pylori CagA and vacuolating toxin VacA in control of the NFAT signaling pathway in gastric epithelial cells. Proceedings of the National Academy of Sciences of the United States of America 102(27):9661–9666. doi: 10.1073/pnas.0502529102
Yu J, Leung WK, Go MY, Chan MC, To KF, Ng EK, Chan FK, Ling TK, Chung SC, Sung JJ (2002) Relationship between Helicobacter pylori babA2 status with gastric epithelial cell turnover and premalignant gastric lesions. Gut 51(4):480–484
Yun CH, Lundgren A, Azem J, Sjoling A, Holmgren J, Svennerholm AM, Lundin BS (2005) Natural killer cells and Helicobacter pylori infection: bacterial antigens and interleukin-12 act synergistically to induce gamma interferon production. Infect Immun 73(3):1482–1490
Zeng M, Mao XH, Li JX, Tong WD, Wang B, Zhang YJ, Guo G, Zhao ZJ, Li L, Wu DL, Lu DS, Tan ZM, Liang HY, Wu C, Li DH, Luo P, Zeng H, Zhang WJ, Zhang JY, Guo BT, Zhu FC, Zou QM (2015) Efficacy, safety, and immunogenicity of an oral recombinant Helicobacter pylori vaccine in children in China: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 386(10002):1457–1464. doi:10.1016/S0140-6736(15)60310-5
Zhou Y, Toh ML, Zrioual S, Miossec P (2007) IL-17A versus IL-17F induced intracellular signal transduction pathways and modulation by IL-17RA and IL-17RC RNA interference in AGS gastric adenocarcinoma cells. Cytokine 38(3):157–164. doi:10.1016/j.cyto.2007.06.002
Zucca E, Bertoni F (2016) The spectrum of MALT lymphoma at different sites: biological and therapeutic relevance. Blood 127(17):2082–2092. doi:10.1182/blood-2015-12-624304
Acknowledgements
Our research was supported by the National Institute for Health Research (NIHR), through the Biomedical Research Unit in Gastrointestinal and Liver Diseases at Nottingham University Hospitals NHS Trust and the University of Nottingham. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Disclosure Statement
There are no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Robinson, K., Letley, D.P., Kaneko, K. (2017). The Human Stomach in Health and Disease: Infection Strategies by Helicobacter pylori . In: Tegtmeyer, N., Backert, S. (eds) Molecular Pathogenesis and Signal Transduction by Helicobacter pylori. Current Topics in Microbiology and Immunology, vol 400. Springer, Cham. https://doi.org/10.1007/978-3-319-50520-6_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-50520-6_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-50519-0
Online ISBN: 978-3-319-50520-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)