Abstract
Cuff-less blood pressure (BP) measurement provides an efficient way to estimate blood pressure and thus prevent cardiovascular disease caused by hypertension. Pulse transit time (PTT) based BP estimation model has attracted much interests but with limited application. The measurement of PTT needs two photoplethysmographic (PPG) sensors or one electrocardiogram (ECG) sensor and one PPG sensor and thus restricted its widespread acceptance. In this study, a novel indicator, Photoplethysmography Acceleration Ratio (PAR), is extracted from the second-order derivative of PPG signal, which is validated as a significant parameter for estimating BP. 120 subjects, aged from 18 to 84, participated in this experiment. The results show that the correlation coefficient between PAR and systolic, diastolic and mean BP are 0.701, 0.331 and 0.629 respectively. Furthermore, the performance of accuracy and precision is good through correlation analysis. Therefore, the proposed PAR is demonstrated to be useful for SB measurement with only one sensor.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Blood pressure (BP) is the major risk factor for predicting cardiovascular events [1]. High BP (hypertension) and low BP (hypotension) reflect the abnormal physiological status of people. Hypertension is becoming more prevalent but poorly controlled due to low awareness, even in young people under 40, and thus creates great burdens on the society. Ubiquitous BP measurement is significant to improve hypertension and pre-hypertension patient management by providing continuous BP monitoring.
Currently, cuffs are used for blood pressure measurement. However, blood pressure machine with cuff for inflation is big in size and inconvenient for use, therefore cannot fulfill the requirement of monitoring BP anytime and anywhere. Recent cuff-less blood pressure estimation approach based on Pulse Transit Time (PTT) has been studied in [2–4] and has achieved reasonable accuracy. However, these approaches are not very straightforward as the measurement of PTT needs two photoplethysmographic (PPG) sensors or one electrocardiogram (ECG) sensor and one PPG sensor. Calibration is also needed in such approaches. By taking this situation into consideration, some studies presented blood pressure estimation method with features extracted from just one PPG sensor [5–7]. Satomi et al. [5] took advantage of several points of acceleration pulse wave to estimate blood pressure based only on photoplethysmogram. In his experiment, the age of volunteers were divided into more than 60 and less than 60. Hayato Fukushima et al. [6, 7] constructed blood pressure model with CO (Cardiac Output) and TPR (Total Peripheral Resistance), both of which were measured by Finometer Pro, a product of Finapres Medical Systems Corp. Although those methods obtained good results that are closed to AAMI requirement, some complex measurement steps may limit their application and promotion. Novel indicators for BP should be further studied to improve accuracy and convenience of cuff-less measurement.
In this paper, we propose a novel BP estimation indicator Photoplethysmography Acceleration Ratio (PAR) extracted from one single PPG signal, which is easy to collect. The normalized waveform of PPG and acceleration PPG (APG) are shown as Fig. 1 and the indicator PAR is extracted from APG signals. With the help of PAR, we can reduce the complexity of the BP measurement and enhance the portability of BP measurement products. Significantly, it provides a promising attempt for constructing a more accurate BP estimation model that can be combined with other techniques.
2 Method
2.1 Subjects and Experiment Protocol
In this study, a total of 120 subjects were recruited for data collection. An informed consent was obtained from each subject and this experiment was approved by institutional ethics committee. The experimental cohorts consisted of healthy groups and high blood pressure groups where participants were engaged in various occupations.
Three-In-One, a portable physiological signal acquisition system designed by Shenzhen Institute of Advanced Technology (SIAT), was used to collect PPG signals of subjects using the sample frequency of 500 Hz. OMRON HEM-1020 electronic sphygmomanometer was used to measure subjects’ blood pressures. The basic data collection procedures contained following steps:
-
Subjects rest for 5 min before data collection.
-
Subjects sit in upright posture. Blood pressure is measured by OMRON HEM-1020, and denoted as \( BP_{1} \).
-
Subjects keep sitting and PPG signal from middle finger is gathered for 1 min by Three-In-One.
-
After finishing PPG signals collection, blood pressure is measured again immediately and denoted as \( BP_{2} \).
During the data collection, the average blood pressure, symbolized as \( BP_{\alpha } \), can be calculated by averaging \( BP_{1} \) and \( BP_{2} \):
\( BP_{a} \) can be approximate to the average blood pressure during this 1 min time. Meanwhile, index finger transmittance PPG signals are recorded and saved.
2.2 Data Preprocessing
Through data collection steps described above, 1 min PPG signals sequences gathered from each subject were saved in computer. As Three-In-One equipment is an integrated and portable physiological signal acquisition circuit board, low complexity is one of its features. Because the raw PPG signals were mixed with noises that include low frequency and high frequency signals, a digit band-pass filter program was designed to eliminate those noises. Moreover, a smoothing algorithm was applied to these signals. This study implemented three-time-seven-point smooth processing using following formula:
where input x represented raw PPG signals and output y is smoothed PPG signals.
2.3 Feature Points Selection and Data Filtration
Numerous features based on electrocardiogram (ECG) and PPG have been proposed by many researchers. However, more features do not necessarily mean better results and it is not enough to utilize these features for accurate blood pressure estimation. More concerns should be focused on appropriate and effective features selection. Changes in blood volume produce PPG, i.e. pulse wave. Through second-order differential, APG can be obtained from PPG and is reported as a more practical waveform that has clear features [8]. These feature points and their combination have been also shown to be meaningful by many studies [3, 5, 6, 10, 11]. Furthermore, APG is associated with some symptomatic risk factors such as systolic blood pressure and diastolic blood pressure [9]. Figure 2 shows some feature points of APG.
The waveform between two waves’ peak points, contains a large amount of undiscovered useful information. These features including peak and valley points a, b, c, d, e, f that have been proposed and used by previous researches [10, 11]. This study employed a new point g, which is located at the end of the current waveform and is close to peak point a of next wave.
As a matter of fact, the positions of peak or valley points c, d, e, f are difficult to capture because of the influence of environment, postures and measuring equipment, especially when portable measurement equipments are used. In addition, for many subjects some of the four clear points cannot be observed clearly. The error rate of feature extraction is quite high. Hence, this study automatically extracted point d and g instead of the entire set of points, as shown in Fig. 3.
Different ages and physical conditions may create variations in the shapes of points. Furthermore, some waveforms of the subjects have inconspicuous standard points d due to individual difference, so the point d does not always appear as a valley point, as shown in Fig. 4(a). In this situation, this study considered the point with minimum slope between point b and e as the correct point d. This type of point d and standard point d are shown in Fig. 4.
2.4 Proposed Feature
After the feature points d and g are extracted, we can get the section of signal waveform between point d and g. We can truncate this section from the whole signal waveform, as shown in Fig. 5. The waveform contains other undefined feature points that influence the shape of this waveform to a great extent.
In this study, we proposed a novel feature θ, which was an angle calculated from the extracted signal waveform. First, we set point d as the initial point, and point g as the end point of a points sequence \( Y = \left\{ {y_{1} ,y_{2} , \ldots ,y_{\text{n}} } \right\} \) with a corresponding discrete time sequence \( X = \left\{ {1,\,2,\, \ldots ,\,n} \right\} \). Second, using these pairs of discrete points, a fitted regression line equation such as (3) was constructed using the least squares fitting method (LSFM). From the gradient of this line the accelerating rate of artery blood flow was calculated. Through LSFM, we can calculate this gradient p using the Eq. (4). Finally, using the transformation function (5), we obtained the angle θ, which is shown in Fig. 6.
The angle θ, that is PAR, can be extracted from each PPG waveform cycle. From a physical point of view, PAR reflects the accelerating ability between point d and g provided by individual APG waveform and the value of PAR changes along with the PPG waveform.
3 Experiment and Result
3.1 Data Description
120 subjects were randomly recruited in this experiment and the age of them ranged from 18 to 84 years old. All of their PPG signals were collected and saved in the computer. The experiment steps are as follows:
-
Through observation, 7 distorted signals were abandoned and 113 signals were picked out.
-
Based on the feature point d, the signals consisted of two groups. Members of Group A (95 signals) had clear valley point d in their waveforms and members of Group B (18 signals) do not.
-
Feature extraction was done on both Group A and Group B separately.
-
Data analysis was executed and blood pressure estimation was made using regression method.
Among the subjects, there were 59 males and 54 females. Table 1 shows the age distribution of these subjects. Their SBP is shown in Table 2 and some of the subjects were hypertension patients.
3.2 Performance of the Proposed Indicator in BP Estimation
Using the indicator PAR, which is proposed to track the BP of subjects, we get equations for systolic blood pressure (SBP), mean artery pressure (MAP) and diastolic blood pressure (DBP) estimation through polynomial regression method. A correlation analysis was first performed between the proposed PAR and SBP, MAP, DBP respectively using Pearson’s correlation in SPSS. The results are shown in Table 3. From Table 3 we can see that PAR shows significant correlation with SBP, MAP and DBP (p < 0.01), especially with the SBP, where the Pearson correlation coefficient is over 0.7. Thus PAR is a potential indicator of SBP.
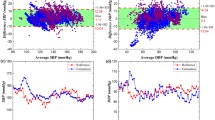
To verify the effectiveness of PAR in estimating BP, univariate linear regression analysis was used for modeling BP. The fitted models and residuals analysis for SBP, MAP and DBP are presented in Figs. 7, 8 and 9 respectively. From the figures we can see that PAR and BP basically conform to a linear model, especially for PAR and SBP. We also evaluate the performance of the fitted model in terms of mean difference (MD) ± standard deviation (SD) and mean absolute difference (MAD) of the estimated BP with the reference blood pressure. The results are presented in Table 4. We can see that even though the mean errors are small, the standard deviations should be further improved to conform to AAMI standard.
4 Discussion and Conclusion
As presented in [11], the PPG patterns are distinctive in different population groups. Due to individual differences and physiological status such as activity and nervous, we also found some APG waveforms have no obvious d point or the d point does not appear in the PPG waveform. To solve this problem, this study presented the minimum slope method to locate the probable position of point d. However, the correct results acquired by this method is probabilistic. In the future, an efficient method to handle this kind of signals should be further studied to gain wider acceptance of the proposed model. However, the development of the PAR indicator represents a new research direction for monitoring BP, and may produce ultimate indicators of BP estimation. Besides, the waveforms of PPG and its transformation forms play an important role in BP monitoring, so more significant features should be further discovered and extracted from them, such as latent parameters of PPG [12]. Hence, more accurate BP estimation equation will be further created through statistical methods and machine learning technologies.
In this study, we proposed a novel indicator PAR for cuff-less BP estimation. The experiment on 113 subjects that included hypertensive patients and health people shows that PAR is high correlated with BP. Therefore, with the help of PAR, we may realize portable, generalized and high precision BP measurement in the future by merging more features into the BP-estimation model.
References
Kannel, W.B.: Elevated systolic blood pressure as a cardiovascular risk factor. Am. J. Cardiol. 85, 251–255 (2000)
Mukkamala, R., Hahn, J.O., Inan, O.T., Mestha, L.K., Kim, C.S., Toreyin, H., Kyal, S.: Toward ubiquitous blood pressure monitoring via pulse transit time: theory and practice. IEEE Trans. Biomed. Eng. 62, 1879–1901 (2015)
Kachuee, M., Kiani, M.M., Mohammadzade, H., Shabany, M.: Cuff-less high-accuracy calibration-free blood pressure estimation using pulse transit time. In: IEEE International Symposium on Circuits and Systems, pp. 1006–1009 (2015)
Gesche, H., Grosskurth, D., Küchler, G., Patzak, A.: Continuous blood pressure measurement by using the pulse transit time: comparison to a cuff-based method. Eur. J. Appl. Physiol. 112, 309–315 (2012)
Suzuki, S., Oguri, K.: Cuff-less and non-invasive systolic blood pressure estimation for aged class by using a photoplethysmograph. In: 30th IEEE International Conference Engineering on Medicine and Biology Society, Vancouver, British Columbia, Canada, pp. 1327–1330 (2008)
Fukushima, H., Kawanaka, H., Bhuiyan, M.S., Oguri, K.: Cuff-less blood pressure estimation using only photoplethysmography based on cardiovascular parameters. In: 35th IEEE International Conference Engineering on Medicine and Biology Society, Osaka, Japan, pp. 2132–2135 (2013)
Hodgson, Y., Choate, J.: Continuous and noninvasive recording of cardiovascular parameters with the Finapres finger cuff enhances undergraduate student understanding of physiology. Adv. Physiol. Educ. 36, 20–26 (2012)
Song, S.H., Cho, J.S., Oh, H.S., Lee, J.S., Kim, I.Y.: Estimation of blood pressure using photoplethysmography on the wrist. In: Computers in Cardiology, pp. 741–744 (2009)
Takada, H., Washino, K., Harrell, J.S., Iwata, H.: Acceleration plethysmography to evaluate aging effect in cardiovascular system. Using new criteria of four wave patterns. Med. Prog. Technol. 21, 205–210 (1995)
Takazawa, K., Tanaka, N., Fujita, M., Matsuoka, O., Saiki, T., Aikawa, M., Tamura, S., Ibukiyama, C.: Assessment of vasoactive agents and vascular aging by the second derivative of photoplethysmogram waveform. Hypertension 32, 365–370 (1998)
Suzuki, A., Ryu, K.: Feature selection method for estimating systolic blood pressure using the Taguchi method. IEEE Trans. Ind. Inform. 10, 1077–1085 (2014)
Datta, S., Banerjee, R., Choudhury, A.D., Sinha, A., Pal, A.: Blood pressure estimation from photoplethysmogram using latent parameters. In: IEEE International Conference on Communications, Kuala Lumpur, Malaysia, pp. 1–7 (2016)
Acknowledgements
This work was supported in part by the National Natural Science Foundation of China (No. 61502472), National 863 project of China (SS2015AA020109) and STS funding from Chinese Academy of Sciences (KFJ-EW-STS-095). Besides, the authors feel grateful to the students and colleagues of Shenzhen Institutes of Advanced Technology for their participation and help.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing AG
About this paper
Cite this paper
Jiang, H. et al. (2016). A Novel Indicator for Cuff-Less Blood Pressure Estimation Based on Photoplethysmography. In: Yin, X., Geller, J., Li, Y., Zhou, R., Wang, H., Zhang, Y. (eds) Health Information Science. HIS 2016. Lecture Notes in Computer Science(), vol 10038. Springer, Cham. https://doi.org/10.1007/978-3-319-48335-1_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-48335-1_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-48334-4
Online ISBN: 978-3-319-48335-1
eBook Packages: Computer ScienceComputer Science (R0)