Abstract
The structurally unrelated antimicrobials, macrolides, lincosamides, and streptogramins are grouped into a single family, called MLS family. This classification is based on a similar, although not identical, mechanism of action. Macrolides are composed of a minimum of two amino and/or neutral sugars attached to a lactone ring of variable size [1] (Fig. 18.1). Erythromycin, produced by a strain of the actinomycete Saccharopolyspora erythraea (formerly Streptomyces erythraeus), is the first macrolide discovered in 1952. It actually corresponds to a mixture of antibiotics that includes erythromycin A, which is the active compound and has a 14-membered lactone ring with two sugars, cladinose and an amino sugar (e.g., desosamine). Other commercially available macrolides derived from erythromycin A include clarithromycin, dirithromycin, roxithromycin, as well as azithromycin that has an enlarged 15-membered ring resulting from a nitrogen insertion. Structural modifications of erythromycin A resulted in improved pharmacokinetic profiles and better tolerance, but cross-resistance between members of this class of antimicrobials was still observed. Some 16-membered ring macrolides are also available in a few countries (spiramycin, josamycin, midecamycin, and miocamycin) or for veterinary use (tylosin). The most recent class of ketolides comprises telithromycin and cethromycin (ABT-773), which are derived from clarithromycin and have two major modifications, replacement of cladinose by a keto-function and an 11-12-carbamate extension with an alkyl-aryl modification in telithromycin. The first fluoroketolide solithromycin (CEM-101), exhibiting a different side chain and a fluorine atom linked to C-2 of the lactone, shows higher in vitro activity and enhanced accumulation in macrophages as compared to telithromycin [2].
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The structurally unrelated antimicrobials–macrolides, lincosamides, and streptogramins–are grouped into a single family, called the MLS family. This classification is based on a similar, although not identical, mechanism of action. Macrolides are composed of a minimum of two amino and/or neutral sugars attached to a lactone ring of variable size [1] (Fig. 18.1). Erythromycin, produced by a strain of the actinomycete Saccharopolyspora erythraea (formerly Streptomyces erythraeus), is the first macrolide discovered in 1952. It actually corresponds to a mixture of antibiotics that includes erythromycin A, which is the active compound and has a 14-membered lactone ring with two sugars, cladinose and an amino sugar (e.g., desosamine). Other commercially available macrolides derived from erythromycin A include clarithromycin, dirithromycin, roxithromycin, as well as azithromycin that has an enlarged 15-membered ring resulting from a nitrogen insertion. Structural modifications of erythromycin A resulted in improved pharmacokinetic profiles and better tolerance, but cross-resistance between members of this class of antimicrobials was still observed. Some 16-membered ring macrolides are also available in a few countries (spiramycin, josamycin, midecamycin, and miocamycin) or for veterinary use (tylosin). The most recent class of ketolides comprises telithromycin and cethromycin (ABT-773), which are derived from clarithromycin and have two major modifications, replacement of cladinose by a keto-function and an 11-12-carbamate extension with an alkyl-aryl modification in telithromycin. The first fluoroketolide solithromycin (CEM-101), exhibiting a different side chain and a fluorine atom linked to C-2 of the lactone, shows higher in vitro activity and enhanced accumulation in macrophages as compared to telithromycin [2].
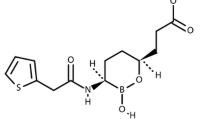
Lincosamides form a small group of antibiotics of naturally occurring compounds or semisynthetic derivatives that contain an amino acid, a proline residue, attached by a peptide bond to a galactoside ring [3] (Fig. 18.1). Lincomycin is produced by the actinomycete Streptomyces lincolnensis. Clindamycin (7-chloro-7-deoxy lincomycin), a semisynthetic derivative of lincomycin in which a hydroxyl group has been replaced by chlorine, is the most important in clinical use. This minor difference in the structure of the molecules results in a noteworthy increase of the molecule affinity for its target [3].
The streptogramin antibiotics are composed of two chemically distinct compounds, namely type A and type B streptogramins [4]. The type A streptogramins are polyunsaturated cyclic macrolactones whereas type B streptogramins are cyclic hepta- or hexadepsipeptides (Fig. 18.1) [4–6]. Originally, streptogramins are natural mixtures produced by different members of Streptomyces or related genera [6, 7]. Every antibiotic producer synthesizes a mixture of various A and B components with a predominant member within each group. For instance, Streptomyces pristinaespiralis produces a mixture of group B compounds called pristinamycins I (pristinamycin IA, pristinamycin IB, and pristinamycin IC with a ratio of 80–90 %, 3–5 %, and 2–5 %, respectively) and a mixture of group A compounds called pristinamycins II (pristinamycin IIA and pristinamycin IIB) [6]. Note that pristinamycin IIA is predominant in the pristinamycin II mixture. Actually, pristinamycin, an oral streptogramin produced by S. pristinaespiralis is essentially a mixture of pristinamycin IA and pristinamycin IIA in a 30:70 ratio by weight [5, 6]. This drug is not commercially available except in some countries such as France and some African countries. Virginiamycin is another oral streptogramin used in livestock in certain countries for growth promotion and prevention of infection. Quinupristin and dalfopristin (hemisynthetic derivatives from pristinamycin IA and pristinamycin IIA, respectively) are combined in an injectable formulation with a 30:70 ratio (w/w) of methane sulfonate salts [5, 6]. More recently, an orally bioavailable combination (NXL 103) composed of linopristin (type B) and flopristin (type A) has been developed by Novexel SA and recently acquired by AstraZeneca [8].
2 Mode of Action
MLS antibiotics are bacteriostatic antibiotics that inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit and ultimately inhibit microbial growth [1–3, 9]. The ribosome is composed of two subunits 30S and 50S built with RNAs and proteins, which assemble to produce a structure functional for protein synthesis. Each part undertakes a specific function. The small subunit 30S decodes mRNA, whereas in the large 50S part, the protein is formed by the polymerization of amino acids according to the genetic code. tRNA molecules carry the amino acids. Ribosomes possess three tRNA-binding sites A, P, and E, hosting the aminoacyl-tRNA, the peptidyl-tRNA, and the exiting tRNA, respectively. Each elongation cycle involves the advancement of the mRNA together with A → P → E site passage of the tRNA molecule driven by GTPase activity [10]. The 50S subunit is formed in part by 23S rRNA, which is organized into six domains. The domain V loop, called peptidyl transferase center (PTC), contains the active site of the peptide bond formation [11, 12]. This PTC loop is positioned at the bottom of a cavity located at the interface of the two subunits, adjacent to the entrance of the peptide tunnel. This tunnel crosses the 50S subunit and emerges on the back of the ribosome. Three-dimensional molecular structure of the ribosome was revealed by electron-cryomicroscopic studies and at atomic level by RX crystallography at high resolution [13]. From three bacterial species (Thermus thermophilus, Haloarcula marismortui, and Deinococcus radiodurans) chosen as a model for the high stability of their ribosomes, much has been learned about the antibiotics that inhibit ribosome function. Although some differences may occur in the ribosomal binding of macrolides and lincosamides according to bacterial species, common features have been found [14, 15].
The binding sites for the MLS antibiotics are located in the PTC or in the near vicinity of PTC at the beginning of the peptide tunnel, before it is constricted by the ribosomal proteins L4 and L22 [16]. The common nucleotide moieties involved in hydrogen bond interactions of the 23S rRNA with macrolides and clindamycin are the nitrogen bases of the nucleotide residues A2058, a crucial MLS-binding site, and A2059 [16]. However, each class of drugs forms its own unique set of interactions with specific additional nucleotides. According to its position, the antibiotic inhibits peptide bond formation or peptide nascent chain progression. All the macrolides attach their lactone ring inside the peptide tunnel at the upper portion, and can protrude their appendage into the PTC cavity [17]. The mechanism of action depends on their size and sugar components [18]. Important contacts are formed between the C5 monosaccharide (desosamine) or disaccharide side chain of 14-15-16-membered macrolides and rRNA [19]. The shape of desosamine sugar of the macrolactone ring in erythromycin fits exactly with that of cavity formed by several nucleotides including A2058, and this interaction is considered to be required for ribosome binding [20].
The telithromycin macrolactone ring had additional hydrogen bond and hydrophobic interactions involving the three keto groups and two nucleotides residues of PTC. Several telithromycin- and erythromycin-binding sites within the 23S RNA overlap exactly. Telithromycin binds 10 times more strongly to ribosomes than the parent macrolide erythromycin, largely because of the alkyl-aryl substituent extending from the macrolactone ring position 11 and 12 that generates a hydrogen bond with nucleotide U2609 [14]. Both macrolides and ketolides act by producing a steric blockage of the ribosome exit tunnel, hence hampering the progression of nascent peptide [16].
Clindamycin binds in an elongated conformation oriented with its long axis roughly parallel to the axis of the exit tunnel. The proline residue occupies the same cleft as the site A substrate puromycin and blocks PTC activity by hampering the binding of transfer RNA to the A site. Clindamycin interacts directly with the A and P sites and blocks the formation of peptide bond by disturbing the positioning of tRNA in A and P sites [14]. The overlapping of some binding sites may explain why macrolides and clindamycin bind competitively to ribosome and why modification of binding sites confers cross-resistance [9].
Type A streptogramins block substrate attachment to both A and P sites of the PTC, competing with the binding of tRNAs to either the A- or P-site, and thus preventing the two early steps of elongation [7, 21]. Type B streptogramins share overlapping binding sites with macrolides and lincosamides (domains II and V), and act similarly by inhibiting translocation, preventing polypeptide extension, and triggering the premature release of incomplete protein chains [7, 21]. In addition, binding of type A streptogramins induces a conformational change in the ribosome near the PTC that subsequently unmasks a high-affinity binding site for streptogramins B leading to an increasing of their activity by ca. 100-fold [4, 7, 21].
3 Spectrum of Activity
MICs of MLS for important pathogenic bacteria are shown in Table 18.1. Macrolides have a spectrum of activity limited to Gram-positive cocci and bacilli, notably staphylococci, β-hemolytic streptococci, and pneumococci, as well as Gram-negative cocci. Gram-negative bacilli are generally resistant with the exception of some clinically important species, such as Bordetella pertussis, Moraxella catarrhalis, Campylobacter spp., and Helicobacter pylori. Macrolides also exhibit in vitro activity against intracellular bacteria, such as chlamydiae, mycoplasmas, and Legionella pneumophila. Note that clarithromycin has a good in vitro and in vivo activity against nontuberculous mycobacteria, especially Mycobacterium avium complex.
Lincosamides have a spectrum of activity closely related to that of macrolides, despite their different structure. Noteworthy, Enterococcus faecalis has an intrinsic resistance to lincosamides and streptogramins A (LSA phenotype) that is shared with other species of enterococci, such as Enterococcus avium, Enterococcus gallinarum, and Enterococcus casseliflavus. By contrast, Enterococcus faecium, Enterococcus hirae, and Enterococcus durans are intrinsically susceptible to lincosamides. A particular feature of clindamycin is its activity against anaerobic bacteria, in particular, Clostridium spp., Peptostreptococcus spp., and Gram-negative rods. However, incidence of acquired resistance is now relatively high in the Bacteroides fragilis group. Also, Clostridium sporogenes, Clostridium tertium, and Clostridium difficile are frequently resistant to clindamycin. Finally, clindamycin has some activity against Toxoplasma gondii and Pneumocystis jirovecii.
Like macrolides and lincosamides, the spectrum of activity of streptogramins includes a broad range of aerobic and anaerobic Gram-positive bacteria, with MIC50 generally ≤1 μg/mL (Table 18.1). Noteworthy, E. faecalis is a gap in the antimicrobial spectrum since this Gram-positive species is intrinsically resistant due to a LSA phenotype (see below).
4 Mechanisms of Resistance and Clinical Implications
Resistance to MLS can be mediated by multiple mechanisms including target modification, enzymatic drug inactivation, and active efflux. Target modification usually encompasses methylation of A2058, which is, as previously mentioned, a key residue with which macrolides, lincosamides, and streptogramins B interact. It also can be due to mutations in 23S rRNA or in conserved regions of ribosomal proteins L4 and L22. In pathogenic microorganisms, the impact of these mechanisms is unequal in terms of incidence and of clinical implications. Modification of the ribosomal target confers broad-spectrum resistance to MLS, whereas enzymatic modification affects only structurally related antibiotics. These mechanisms have been found in antibiotic producers, which often combine several self-protective mechanisms against the antimicrobial that they produce.
4.1 Ribosomal Methylation
4.1.1 erm Genes
Ribosomal modification by methylation was the first mechanism of resistance to macrolides elucidated. This mechanism results from the acquisition of an erm gene (erythromycin ribosome methylase) usually carried by plasmids or transposons in pathogenic bacteria. Biochemical studies indicated that erm genes encode methylases that add one or two methyl groups to a single position (A2058) in bacterial 23S rRNA [22]. As a consequence of methylation, the activity of antibiotics that have the A2058 nucleotide as a key nucleotide for their binding to the ribosome is impaired. The overlapping binding sites in the peptidyl transferase region of 23S ribosomal RNA of macrolides, lincosamides, and streptogramins B account for cross-resistance (the so-called MLSB resistance phenotype).
A wide range of microorganisms that are targets for macrolides and lincosamides express Erm methylases. More than 40 different erm genes have been reported so far (http://faculty.washington.edu/marilynr/), of which six major classes are detected in pathogenic microorganisms: erm(A), erm(B), erm(C), erm(F), erm(G), and erm(X). Both erm(A) and erm(C) typically are staphylococcal gene classes. Genes belonging to the erm(B) class and to a subclass of the erm(A) gene class, previously called erm(TR), are widespread in β-hemolytic streptococci and enterococci. The erm(F) and erm(G) class genes are detected in Bacteroides spp. and other anaerobic bacteria whereas the erm(X) class genes are identified in Gram-positive rods. Although each class is relatively confined to a bacterial genus, it is not strictly genus specific. For instance, erm(B) genes may be found in staphylococci and anaerobes. Although all members of the erm family methylate the adenine of 23S rRNA located at position 2058, they differ by their capacity to monomethylate or dimethylate this nucleotide position. The major Erm methylases detected in pathogens, Erm(A), Erm(B), and Erm(C), generally function as dimethylases that confer a high-level cross-resistance to MLSB drugs (including telithromycin). However, Erm(B) and Erm(A) (formerly ermTR) may function as monomethylases in Streptococcus pneumoniae and Streptococcus pyogenes, respectively [23, 24]. In fact, this makes a difference for ketolides, which are weakly affected by monomethylation, but not for erythromycin and clindamycin that are poorly active whether the ribosome is mono- or dimethylated.
MLSB resistance may be constitutively or inducibly expressed [25, 26]. In inducible resistance, the bacteria produce inactive mRNA that is unable to encode methylase. In the model of the staphylococcal gene erm(C), the inactivity of the mRNA is due to the structure of its 5′ untranslated region (UTR) which has a set of inverted repeats that sequester the initiation sequences (ribosome-binding site and initiation codon) for the methylase by base-pairing in the absence of erythromycin [26]. Thus, the methylase cannot be produced since the initiation motifs for translation of the enzyme are not accessible to the ribosomes. Induction is related to the presence of an open-reading frame encoding a short 14-amino acid peptide upstream of the erm(C) structural gene. In the presence of low concentrations of erythromycin, binding of the antibiotic to a ribosome translating the leader peptide causes the ribosome to stall. Ribosome stalling likely induces destabilization of the pairing and conformational rearrangements in the mRNA that would then unmask the initiation sequences for the methylase, allowing synthesis to proceed by available ribosomes.
The erm(C) regulation model designated as posttranscriptional (or translational) attenuation would also account for the regulation of the erm(A) and erm(B) determinants [26]. For a given attenuator, the inducing capacity of the macrolides depends on the antibiotic structure. Whereas 14-membered macrolides (erythromycin, roxithromycin, and clarithromycin) and 15-membered macrolides (azithromycin) are inducers for the production of most Erm methylases, ketolides and lincosamides are generally not. Mutations in the attenuator may modify the induction pattern. In particular, lincosamides may become inducers in the case of mutation of the attenuator. This feature has been reported in laboratory mutants [27] and rarely for clinical isolates of S. aureus [28]. In staphylococci that typically contain erm(A) or erm(C) genes, inducible resistance leads to dissociated phenotypes of resistance between inducers (erythromycin) that are not active and noninducers (clindamycin) that remain active. The phenotype of MLSB-inducible resistance expressed by staphylococci is characteristic, provided that the strains are tested by the disk-diffusion technique. A blunting of the clindamycin inhibition zone, similar to the shape of the letter D and referred as to a D-shaped zone, can be observed, provided that a disk of erythromycin is placed nearby (Fig. 18.2b). Which holds true for staphylococci is not for streptococci that usually harbor erm(B) genes. Indeed, the inducible erm(B) gene generally confers a cross-resistance to erythromycin and clindamycin, which differs from the dissociated resistance conferred by the staphylococcal erm(A) and erm(C) genes. The particular expression of erm(B) might be related to methylation of various proportions of ribosomes even in the absence of erythromycin [24]. This paradox could be explained by a nonstringent control of the expression of the methylase by the erm(B) attenuator. Fusion of the mutated erm(B) attenuator with a lacZ reporter gene has confirmed that the expression of the methylase can be partly derepressed in some strains [29]. By contrast, the control of methylase expression by the staphylococcal erm(A) and erm(C) methylases appears more strict. Other additional features, such as differences in the promoter strength or in the copy number of the erm(B) gene, may also account for the various levels of ribosomal methylation. The presence of basal levels of methylase appears sufficient to confer resistance to lincosamides, explaining the cross-resistance between macrolides and lincosamides in streptococci containing inducible erm(B) genes [28]. The expression in streptococci of the erm(A) gene (formerly ermTR) resembles that of the staphylococcal erm(A) gene [25].
Phenotypes of resistance to macrolides and clindamycin in S. aureus. (a) S. aureus susceptible to erythromycin and clindamycin; (b) S. aureus containing an erm(C) gene inducibly expressed (a D-shaped zone can be observed for the clindamycin zone of inhibition on the edge closest to the erythromycin zone of inhibition); (c) S. aureus containing an erm(C) gene constitutively expressed; (d) S. aureus containing an lnu(A) gene responsible for inactivation of lincosamides; (e) S. aureus resistant to erythromycin by msr(A)-mediated efflux (note the absence of D-shaped zone). C clindamycin, E erythromycin, L lincomycin
In constitutive expression, active methylase mRNA is produced in the absence of an inducer, and the strains express cross-resistance to MLSB antibiotics, regardless of the nature of the erm gene (Fig. 18.2c). In the laboratory, mutants derived from inducible strains of staphylococci and expressing constitutive MLSB resistance can be selected on agar plates containing inhibitory concentrations of clindamycin at frequencies varying between 10−6 and 10−8, depending on the strain [25, 30]. In addition, clinical isolates constitutively resistant to erythromycin are widespread, especially among methicillin-resistant staphylococci. It has been shown both in laboratory mutants and in clinical isolates that constitutive expression is due to deletions, duplications, or point mutations in the attenuator sequence leading to derepressed production of the methylase [26]. Similarly, in vitro selection by clindamycin of constitutive resistance at a frequency of 10−7 has been reported in a clinical isolate of S. pyogenes inducibly resistant to erythromycin and harboring erm(TR), a subclass of erm(A) genes [31].
The use of clindamycin for the treatment of an infection due to an inducibly resistant strain of S. aureus is not devoid of risk. As previously mentioned, constitutive mutants can be selected in vitro in the presence of clindamycin at a relatively high frequency. Bacterial inocula exceeding 107 cfu can be found in mediastinitis and in certain lower respiratory tract infections. The risk to patients is illustrated by reports of selection of constitutive mutants during the course of clindamycin therapy administered to patients with severe infections due to inducibly erythromycin-resistant S. aureus [30, 32–37]. However, clinical evidence regarding the risk of emergence of clindamycin resistance is based only on a few case reports which are summarized in Table 18.2, and there are also reports of successful use of clindamycin in treating patients with D-test-positive isolates. Although it seems reasonable to discourage the use of clindamycin in deep-seated infections or in infections with heavy bacterial inoculum that increases the risk for selection of constitutive mutants, there are no criteria to confidently predict the success or the failure of clindamycin therapy in infections due to MLSB-inducible staphylococci. Nonetheless, it is worth noting that isolates containing the inducible erm(C) present significantly higher frequencies of mutational resistance than those harboring the erm(A) gene [38]. More prospective studies of cases of staphylococcal or streptococcal infections treated with clindamycin are needed to better define the role of this antimicrobial in infections due to microorganisms with various macrolide resistance phenotypes. Noteworthy, the bactericidal activity of streptogramins against staphylococci expressing (like numerous MRSA isolates) a constitutive MLSB phenotype is generally altered [39].
4.1.2 cfr Gene
Ribosomal methylation, occurring at a different site than the A2058 previously mentioned, may confer resistance to lincosamides but not to macrolides. Initially identified in staphylococcal isolates from animal sources, it has been recently detected in human S. aureus and E. faecalis clinical isolates [40–43]. Interestingly, in a linezolid-resistant MRSA clinical isolate, the cfr gene was located downstream of an erm(B) gene, both genes being co-transcribed [41]. The resistance is due to the production of the Cfr (chloramphenicol florfenicol resistance) protein that specifically methylates the 23S rRNA at the A2503 residue [44]. This still rare mechanism causes cross-resistance to five different antibiotic families: phenicols, lincosamides, oxazolidinones, pleuromutilins, and streptogramins A (the so-called PhLOPSA phenotype) [45]. Although almost exclusively found on plasmids, chromosomal location has also been reported [40, 41].
4.2 Ribosomal Mutations
Studies with mutants obtained in the laboratory and reports of clinical isolates have revealed that several structures participating in the binding of macrolides, particularly domains V and II of 23S rRNA and proteins L4 and L22, can display mutations responsible for macrolide/lincosamide resistance. The resistance phenotype conferred by alterations in the ribosomal target varies according to the nature of the mutated structure, but there is generally cross-resistance to MLS. In addition, since bacteria generally have several copies of the rrl gene coding for the 23S rRNA, susceptibility to macrolides and lincosamides varies according to the number of mutated copies and decreases as the number of the mutated copies increases [46]. Ribosomal mutations are rare in clinical isolates of staphylococci and streptococci [25], but are the main mechanism of resistance to macrolides in some bacterial species, such as Campylobacter spp., H. pylori, P. acnes, and M. avium complex [47].
4.3 Enzymatic Inactivation
Unlike target modification, inactivation of MLS antibiotics only confers resistance to structurally related antibiotics. Different esterases and phosphorylases have been identified in strains resistant to macrolides, almost exclusively in Gram-negative bacteria. Indeed, members of the family Enterobacteriaceae highly resistant to erythromycin due to the presence of these resistance determinants have been reported. Most of the strains were isolated from stool or blood cultures during selective digestive tract decontamination in neutropenic patients [48]. The isolates inactivate the lactone ring of 14-membered ring macrolides by production of erythromycin esterases or macrolide 2′-phosphotransferases that add phosphate to the 2′-hydroxyl group of an amino sugar [49–51]. Two types (I and II) of esterases, encoded by ere(A) and ere(B) (erythromycin esterase) genes, respectively, have been identified so far. Note that the G + C content of ere(B) (36 %), unlike that of ere(A) (50 %), is significantly different from the base composition of the Escherichia coli chromosome (50 %), suggesting that ere(B) is of exogenous origin, possibly a Gram-positive coccus. The ere(B) gene was detected in only 5 of 851 isolates (0.6 %) of erythromycin-resistant MRSA strains collected from 24 European hospitals while no ere(A) gene could be detected [52]. There are two groups of phosphotransferases, MPH(2′)-I (encoded by mph(A) and mph(D) genes) that inactivates 14- and 15-membered ring macrolides more efficiently than 16-membered ones, and MPH(2′)-II (encoded by mph(B) and mph(C) genes) that inactivates both groups of macrolides [53]. mph(A) and mph(B) are the most prevalent genes among Gram-negative bacteria. Notably, the plasmid-borne mph(A) gene conferring resistance to azithromycin has emerged in Shigella sonnei isolates responsible for an outbreak in Paris area while E. coli could constitute a major reservoir for this gene [54, 55]. An mph(C) gene, distinct from mph(A) and mph(B), has been described in a few strains of S. aureus [56].
Specific resistance to lincosamides is due to enzymatic inactivation of those antibiotics. Phosphorylation and nucleotidylation of the hydroxyl group at position 3 or 4 of lincosamides have been detected in several species of Streptomyces. In both animal and human isolates, lincosamide nucleotidyltransferases encoded by lnu genes (formerly lin) were reported. In clinical isolates, five lnu class genes have been described: lnu(A), lnu(B), lnu(C), lnu(D), and lin(F) [57–62]. The O-nucleotidyltransferases encoded by these genes inactivate lincosamides by adenylylation [58]. The lnu(A) genes have been reported in staphylococci and Bacteroides spp. [57, 60]. Initially described in E. faecium, lnu(B) is the most prevalent lnu gene among streptococci of human and animal origin [58]. The lnu(F) gene has been rarely described in E. coli and Salmonella spp. [59]. The lnu(C) gene was first characterized in a Streptococcus agalactiae clinical isolate, being located on a small mobilizable transposon [61, 63]. A second report of lnu(C) was recently published in a Streptococcus anginosus clinical isolate [64]. The lnu(D) gene was first described in a clinical isolate of Streptococcus uberis responsible for a case of bovine mastitis, and was then detected in two other S. uberis veterinary isolates [62, 65, 66]. Mechanistically, LnuA nucleotidyltransferase modifies a hydroxyl group of clindamycin and lincomycin at positions 3 and 4, respectively, whereas LnuB modifies a hydroxyl at position 3 in both clindamycin and lincomycin [58].
Although Lnu(A), Lnu(B), Lnu(C), and Lnu(D) nucleotidyltransferases inactivate in vitro more efficiently clindamycin than lincomycin, the corresponding genes confer resistance to lincomycin (MICs from 16 to 32 μg/mL) but not to clindamycin (MICs from 0.06 to 0.12 μg/mL), the so-called L phenotype [57, 58, 62, 63] (Fig. 18.2d). By contrast, when the lnu(A), lnu(B), lnu(C), and lnu(D) genes were cloned into E. coli, they conferred cross-resistance to lincomycin and clindamycin [57, 58, 62, 63]. A similar phenotype was observed for the lin(F) gene in E. coli [59]. The reason for the difference in phenotypic expression of the resistance determinant in the two backgrounds remains unexplained. Hypothetically, the difference between the two lincosamides might be related to differences in relative affinities of clindamycin and lincomycin for the ribosomes of Gram-positive and Gram-negative organisms and for the Lnu enzymes: clindamycin might have better affinity for the Gram-positive ribosomes than for Lnu(C), explaining why its activity is maintained. Although the activity of clindamycin against the Gram-positive hosts of the lnu gene was only weakly affected by the mechanism of resistance, a 100-fold increase in the bacterial inoculum led to a three-dilution increase in the MIC of clindamycin for S. agalactiae UCN36 containing lnu(C) [61] and the bactericidal activity of clindamycin (already weak against susceptible strains) was totally abolished against a staphylococcal strain with lnu(A) [57].
Inactivation of type A streptogramins is due to 0-acetylation by acetyltransferases encoded by vat genes [5, 7, 67]. These enzymes transfer an acetyl group from acetyl-CoA to the secondary hydroxyl of type A streptogramins. Type B streptogramins can be inactivated by enzymes called lyases or lactonases, which are encoded by vgb genes [5, 7, 67]. They cause a cleavage of the ester linkage leading to a linearization of the molecule.
4.4 Active Efflux
Efflux was reported as responsible for the intrinsic resistance to macrolides and lincosamides of E. coli and other Gram-negative bacteria, and as putatively responsible for the intrinsic resistance of E. faecalis to lincosamides and streptogramins A. In E. coli, inactivation of the tripartite pump AcrAB-TolC renders this organism susceptible to erythromycin and clindamycin [68]. In E. faecalis OG1RF, cross-resistance to lincosamides and streptogramins A (the so-called LSA phenotype) was related to the expression of a species-specific chromosomal lsa gene, renamed lsa(A), coding for an ABC protein [69]. Inactivation of the lsa(A) gene resulted in entire susceptibility to clindamycin, dalfopristin, and quinupristin–dalfopristin, whereas trans-complementation with a recombinant plasmid bearing an intact lsa gene restored resistance to these antibiotics. In Staphylococcus sciuri, a LSA phenotype was demonstrated to be related to the expression of the plasmid-mediated lsa(B) gene coding for a Lsa(A) homolog [70]. A similar LSA phenotype was observed from S. agalactiae clinical isolates from New Zealand, and was due to a Lsa(A)-like protein encoded by the chromosomal lsa(C) gene [71, 72]. The last lsa-like gene, called lsa(E), has been recently identified in MRSA isolates of swine origin [73]. As opposed to E. faecalis, E. faecium is intrinsically susceptible to all macrolides and related compounds, but the LSA phenotype may be selected in vitro and in vivo [74]. The resistance is due to a unique mutation within a gene coding for an ABC homologue showing 66 % amino acid identity with Lsa(A), leading to an amino acid substitution. The wild-type allele was named eat(A) (for Enterococcus ABC transporter) and its mutated resistant variant, eat(A)v [75]. Interestingly, the phenotype conferred by Lsa-like proteins actually comprises lincosamides, streptogramins A, and pleuromutilins (e.g., tiamulin), and is known as LSAP phenotype [72, 75].
Acquired efflux of lincosamides (as a LSA phenotype) has also been detected in staphylococcal isolates. This phenotype, similar to that mediated by Lsa-like proteins, is due to the acquisition of plasmid genes vga(A), vga(A)v, or vga(A)LC, which also code for ABC proteins responsible for a low-level resistance to lincosamides and streptogramins A [76–78].
Active efflux has been reported as an acquired mechanism of resistance to macrolides in clinical isolates of Gram-positive organisms. In particular, the efflux pump msr(A) responsible for the MSB phenotype (resistance to erythromycin and streptogramins B) in staphylococci and the dual efflux pump mef(A)/mel responsible for the M phenotype (resistance to erythromycin) in streptococci [79]. msr(A) and mel belong to the ABC transporter family whereas mef(A) is part of the Major Facilitator Superfamily [80]. Note that these mechanisms that are widely spread do not affect the activity of lincosamides, and that the activity of ketolides is affected by mef(A) only at a very low level, being likely not clinically significant. mef(A)/mel genes are borne by a transposon [81, 82] and have been described in a variety of species, mostly S. pneumoniae and S. pyogenes. The msr(A) gene is usually found in staphylococci but has also been detected in Streptococcus, Enterococcus, Corynebacterium, and Pseudomonas [83]. Different msr(A) homologs have also been described, such as msr(C) in Enterococcus, msr(D) in many genera and linked to mef(A), and msr(E) in some Gram-negative bacteria.
As opposed to Mef(A) that is undoubtedly an efflux pump, the biochemical basis of resistance remains unclear for aforementioned Lsa-, Vga-, and Msr-like proteins. They all belong to the family of ABC systems, of which most of them are involved in import and export, and then called ABC transporters [84]. These “classical” transporters share a common organization with two hydrophobic transmembrane domains (TMDs) and two intracytoplasmic nucleotide-binding domains (NBDs) implicated in ATP hydrolysis. Actually, Lsa-, Vga-, and Msr-like proteins belong to a third group of ABC proteins (named class 2) that lack TMDs consisting of two NBDs fused into a single protein [84]. Even though these class 2 ABC proteins are presumed to function as efflux pumps, the biochemical mechanism of resistance has been poorly elucidated. Only two studies that showed about Msr(A) suggest that Msr(A) and vga(A)LC might be able to hijack the TMDs of ABC transporters to mediate efflux [77, 85], but no membrane partners have been identified so far [86]. A ribosomal-related mechanism of resistance, such as ribosomal protection, might also be hypothesized.
5 Reports of Susceptibility Tests by the Laboratory
5.1 Staphylococci
Both clindamycin and erythromycin have to be tested. As noted above, resistance to both erythromycin and clindamycin relates to constitutive MLSB resistance and is easily recognized. Dissociated susceptibility results for erythromycin and clindamycin require the attention of the clinical microbiology laboratory. The following cases can be discussed.
5.1.1 Strains Resistant to Erythromycin but Susceptible to Clindamycin
When clindamycin is active, the identification of the phenotype is required. The inducible MLSB resistance can be detected only by methods showing induction of clindamycin resistance. As previously mentioned, the disk-diffusion method is an easy method to detect this phenotype by placing an erythromycin disk near a clindamycin disk on an agar growth medium, using a standard disk dispenser [87]. The presence of a D-shape zone is the signature of the MLSB-inducible phenotype (Fig. 18.2b). This approach is recommended by the CLSI susceptibility testing standards. When staphylococci are tested using a broth-based method (including automated instruments), the CLSI recommends placing erythromycin (15 μg) and clindamycin (2 μg) disks nearly 15–26 mm apart (center to center) on the blood agar plate that is used to control the purity of the bacterial inoculum [88, 89]. Isolates displaying a D-shaped zone, therefore inducibly resistant to MLSB antibiotics, should be reported as clindamycin resistant by the laboratory [88]. However, the clinical laboratory may add the following comment: “This isolate is presumed to be resistant based on detection of inducible clindamycin resistance; clindamycin may still be effective in some patients.” Note that certain automated systems also propose a liquid-based induction test. The final decision to treat or not the patient with clindamycin should be based on the analysis of each specific case, and if a clindamycin therapy is started, it requires close follow-up of the patient for failure. In the absence of D-shaped zone, the staphylococcal isolate is presumably resistant to erythromycin by active efflux through acquisition of the msr(A) gene (Fig. 18.2e). Since clindamycin is neither an inducer nor a substrate for this pump, the isolate can safely be reported as susceptible to clindamycin. Strains of S. aureus ATCC strain BAA-977 containing erm(A) and S. aureus ATCC BAA-976 harboring the efflux pump encoded by msr(A) are recommended as positive and negative control organisms, respectively [90].
5.1.2 Strains Susceptible to Erythromycin but Resistant to Lincosamides
This dissociated phenotype of resistance is rare in S. aureus, found in less than 1 % of the strains, but is more frequent in coagulase-negative staphylococci, with frequencies ranging from 1 to 7 % of strains depending on the staphylococcal species [57]. Two phenotypes of resistance should be distinguished: the LSA type of resistance that is detected as a resistance or an intermediate susceptibility to both clindamycin and lincomycin, and the L phenotype resistance that can be identified only if lincomycin is tested since MIC of clindamycin or zone size diameter for the disk of clindamycin remain within the range of those for a susceptible isolate. This phenotype can be easily identified by testing both lincomycin and clindamycin, which display an unusual dissociated susceptibility to clindamycin and resistance to lincomycin. By the disk-diffusion technique, lincosamide inactivation can be easily predicted by observing the appearance of the clindamycin inhibition zone edge. A sharply demarcated edge correlates with the production of lincosamide nucleotidyltransferases (Fig. 18.2d). There is no recommendation for the interpretation of the result for clindamycin and the clinical relevance is unknown.
5.2 Other Organisms
For streptococci, concerns about the activity of clindamycin against isolates susceptible to this antibiotic but with an inducible MLSB phenotype could also be raised. However, routine testing for inducible resistance for pneumococci is not recommended since isolates containing an inducible erm(B) gene usually display cross-resistance between erythromycin and clindamycin, as mentioned above. Only rare isolates with an inducible MLSB phenotype are susceptible to clindamycin and clinical significance has not been established. The same observation can be made for β-hemolytic streptococci containing an inducible erm(B) gene. However, β-hemolytic streptococci might contain an inducible erm(A) gene (formerly ermTR) with a positive D-shaped zone test. In this case, although no clinical failure has been reported, the use of clindamycin does not seem safe. By contrast, isolates of S. pneumoniae or S. pyogenes expressing the efflux pumps MefA/Mel remain fully susceptible to clindamycin. Resistance to clindamycin in Bacteroides fragilis is frequent (generally more than 30 % of isolates) and is mostly due to ribosomal methylation (MLSB phenotype) mostly by erm(F), erm(G), and erm(B) genes. The resistance is often expressed at a high level. C. perfringens is rarely resistant to clindamycin. Again, resistant isolates expressing an MLSB phenotype which, in some cases of inducible expression, can be detected only after 48 h of incubation. For some fastidious organisms (e.g., H. pylori, M. avium complex), molecular detection of 23S rRNA mutations is a good option since the number and the position of mutations conferring macrolide resistance are limited. Many different approaches, particularly real-time PCR assays, have been developed. For instance, it is possible to detect most of mutations conferring clarithromycin resistance in H. pylori, even directly from gastric biopsies [91].
6 Conclusion
Favorable properties of macrolides and clindamycin, in terms of tissue distribution, convenient oral or intravenous dosing, and low cost explain why these antibiotics, available for more than 40 years, remain widely used. However, a multiplicity of mechanisms has emerged in staphylococci, streptococci, enterococci, and anaerobes that confer resistance to this group of antimicrobials and lead to complex resistance phenotypes. Identification of the corresponding resistance mechanisms has a clinical importance as regards to the use of macrolides and clindamycin. The clinical relevance of the inducible MLSB type of resistance for activity of clindamycin still remains to be fully evaluated. Epidemiological aspects of resistance to macrolides and lincosamides have not been discussed in this chapter, since it is highly variable according to the country and even within a single country. The frequencies of resistance to clindamycin cannot be deduced from those to erythromycin since cross-resistance is unpredictable. In particular, efflux mechanisms affect the activity of erythromycin but not that of clindamycin, both in streptococci and staphylococci. The reverse is also true for other mechanisms of resistance. Therefore, specific surveys of macrolide and lincosamide resistance in pathogens are required. Both surveillance of the incidence of resistance and of the respective prevalence of the various resistance mechanisms is justified by the rapid variations in resistance observed in several countries.
References
Takashima H. Structural consideration of macrolide antibiotics in relation to the ribosomal interaction and drug design. Curr Top Med Chem. 2003;3:991–9.
Llano-Sotelo B, Dunkle J, Klepacki D, Zhang W, Fernandes P, Cate JH, Mankin AS. Binding and action of CEM-101, a new fluoroketolide antibiotic that inhibits protein synthesis. Antimicrob Agents Chemother. 2010;54:4961–70.
Spizek J, Novotna J, Rezanka T. Lincosamides: chemical structure, biosynthesis, mechanism of action, resistance, and applications. Adv Appl Microbiol. 2004;56:121–54.
Mukhtar TA, Wright GD. Streptogramins, oxazolidinones, and other inhibitors of bacterial protein synthesis. Chem Rev. 2005;105:529–42.
Canu A, Leclercq R. Overcoming bacterial resistance by dual target inhibition: the case of streptogramins. Curr Drug Targets Infect Disord. 2001;1:215–25.
Barriere JC, Berthaud N, Beyer D, Dutka-Malen S, Paris JM, Desnottes JF. Recent developments in streptogramin research. Curr Pharm Des. 1998;4:155–80.
Johnston NJ, Mukhtar TA, Wright GD. Streptogramin antibiotics: mode of action and resistance. Curr Drug Targets. 2002;3:335–44.
Politano AD, Sawyer RG. NXL-103, a combination of flopristin and linopristin, for the potential treatment of bacterial infections including community-acquired pneumonia and MRSA. Curr Opin Investig Drugs. 2010;11:225–36.
Verdier L, Bertho G, Gharbi-Benarous J, Girault JP. Lincomycin and clindamycin conformations. A fragment shared by macrolides, ketolides and lincosamides determined from TRNOE ribosome-bound conformations. Bioorg Med Chem. 2000;8:1225–43.
Agmon I, Amit M, Auerbach T, Bashan A, Baram D, Bartels H, Berisio R, Greenberg I, Harms J, Hansen HA, Kessler M, Pyetan E, Schluenzen F, Sittner A, Yonath A, Zarivach R. Ribosomal crystallography: a flexible nucleotide anchoring tRNA translocation, facilitates peptide-bond formation, chirality discrimination and antibiotics synergism. FEBS Lett. 2004;567:20–6.
Ban N, Nissen P, Hansen J, Moore PB, Steitz TA. The complete atomic structure of the large ribosomal subunit at 2.4 Å resolution. Science. 2000;289:905–20.
Yonath A. Ribosomal crystallography: peptide bond formation, chaperone assistance and antibiotics activity. Mol Cells. 2005;20:1–16.
Harms J, Schluenzen F, Zarivach R, Bashan A, Gat S, Agmon I, Bartels H, Franceschi F, Yonath A. High resolution structure of the large ribosomal subunit from a mesophilic Eubacterium. Cell. 2001;107:679–88.
Tu D, Blaha G, Moore PB, Steitz TA. Structures of MLSBK antibiotics bound to mutated large ribosomal subunits provide a structural explanation for resistance. Cell. 2005;121:257–70.
Wilson DN, Harms JM, Nierhaus KH, Schlünzen F, Fucini P. Species-specific antibiotic-ribosome interactions: implications for drug development. Biol Chem. 2005;386:1239–52.
Schlünzen F, Zarivach R, Harms J, Bashan A, Tocilj A, Albrecht R, Yonath A, Franceschi F. Structural basis for the interaction of antibiotics with the peptidyl transferase centre in eubacteria. Nature. 2001;413:814–21.
Polacek N, Mankin AS. The ribosomal peptidyl transferase center: structure, function, evolution, inhibition. Crit Rev Biochem Mol Biol. 2005;40:285–311.
Poehlsgaard J, Douthwaite S. The bacterial ribosome as a target for antibiotics. Nat Rev Microbiol. 2005;13:870–81.
Gaynor M, Mankin AS. Macrolide antibiotics: binding site, mechanism of action, resistance. Curr Top Med Chem. 2003;3:949–60.
Yonath A, Bashan A. Ribosomal crystallography: initiation, peptide bond formation, and amino acid polymerization are hampered by antibiotics. Annu Rev Microbiol. 2004;58:233–51.
Cocito C, Di Giambattista M, Nyssen E, Vannuffel P. Inhibition of protein synthesis by streptogramins and related antibiotics. J Antimicrob Chemother. 1997;39(Suppl A):7–13.
Weisblum B. Erythromycin resistance by ribosome modification. Antimicrob Agents Chemother. 1995;39:577–85.
Liu M, Douthwaite S. Activity of the ketolide telithromycin is refractory to Erm monomethylation of bacterial rRNA. Antimicrob Agents Chemother. 2002;46:1629–33.
Douthwaite S, Jalava J, Jakobsen L. Ketolide resistance in Streptococcus pyogenes correlates with the degree of rRNA dimethylation by Erm. Mol Microbiol. 2005;58:613–22.
Leclercq R, Courvalin P. Resistance to macrolides and related antibiotics in Streptococcus pneumoniae. Antimicrob Agents Chemother. 2002;46:2727–34.
Weisblum B. Insights into erythromycin action from studies of its activity as inducer of resistance. Antimicrob Agents Chemother. 1995;39:797–805.
Tanaka T, Weisblum B. Mutant of Staphylococcus aureus with lincomycin- and carbomycin-inducible resistance to erythromycin. Antimicrob Agents Chemother. 1974;5:538–40.
Clarebout G, Nativelle E, Leclercq R. Unusual inducible cross resistance to macrolides, lincosamides, and streptogramins B by methylase production in clinical isolates of Staphylococcus aureus. Microb Drug Resist. 2001;7:317–22.
Rosato A, Vicarini H, Bonnefoy A, Chantot JF, Leclercq R. A new ketolide, HMR 3004, active against streptococci inducibly resistant to erythromycin. Antimicrob Agents Chemother. 1998;42:1392–6.
Lewis II JS, Jorgensen JH. Inducible clindamycin resistance in staphylococci: should clinicians and microbiologists be concerned? Clin Infect Dis. 2005;40:280–5.
Fines M, Gueudin M, Ramon A, Leclercq R. In vitro selection of resistance to clindamycin related to alterations in the attenuator of the erm(TR) gene of Streptococcus pyogenes UCN1 inducibly resistant to erythromycin. J Antimicrob Chemother. 2001;48:411–6.
Rao GG. Should clindamycin be used in treatment of patients with infections caused by erythromycin-resistant staphylococci? J Antimicrob Chemother. 2000;45:715–6.
McGehee RF, Barrett FF, Finland F. Resistance of Staphylococcus aureus to lincomycin, clindamycin, and erythromycin. Antimicrob Agents Chemother. 1968;13:392–7.
Drinkovic D, Fuller ER, Shore KP, Holland DJ, Ellis-Pegler R. Clindamycin treatment of Staphylococcus aureus expressing inducible clindamycin resistance. J Antimicrob Chemother. 2001;48:315–6.
Frank AI, Marcinak JF, Mangat PD, Tjhio JT, Kelkar S, Schreckenberger PC, Quinn JP. Clindamycin treatment of methicillin-resistant Staphylococcus aureus infections in children. Pediatr Infect Dis J. 2002;21:530–4.
Siberry GK, Tekle T, Carroll K, Dick J. Failure of clindamycin treatment of methicillin-resistant Staphylococcus aureus expressing inducible clindamycin resistance in vitro. Clin Infect Dis. 2003;37:1257–60.
Levin TP, Suh B, Axelrod P, Truant AL, Fekete T. Potential clindamycin resistance in clindamycin-susceptible, erythromycin-resistant Staphylococcus aureus: report of a clinical failure. Antimicrob Agents Chemother. 2005;49:1222–4.
Daurel C, Huet C, Dhalluin A, Bes M, Etienne J, Leclercq R. Differences in potential for selection of clindamycin-resistant mutants between inducible erm(A) and erm(C) Staphylococcus aureus genes. J Clin Microbiol. 2008;46:546–50.
Clarebout G, Nativelle E, Bozdogan B, Villers C, Leclercq R. Bactericidal activity of quinupristin-dalfopristin against strains of Staphylococcus aureus with the MLS(B) phenotype of resistance according to the erm gene type. Int J Antimicrob Agents. 2004;24:444–9.
Schwarz S, Werckenthin C, Kehrenberg C. Identification of a plasmid-borne chloramphenicol-florfenicol resistance gene in Staphylococcus sciuri. Antimicrob Agents Chemother. 2000;44:2530–3.
Toh SM, Xiong L, Arias CA, Villegas MV, Lolans K, Quinn J, Mankin AS. Acquisition of a natural resistance gene renders a clinical strain of methicillin-resistant Staphylococcus aureus resistant to the synthetic antibiotic linezolid. Mol Microbiol. 2007;64:1506–14.
Witte W, Cuny C. Emergence and spread of cfr-mediated multiresistance in staphylococci: an interdisciplinary challenge. Future Microbiol. 2011;6:925–31.
Diaz L, Kiratisin P, Mendes RE, Panesso D, Singh KV, Arias CA. Transferable plasmid-mediated resistance to linezolid due to cfr in a human clinical isolate of Enterococcus faecalis. Antimicrob Agents Chemother. 2012;56:3917–22.
Kehrenberg C, Schwarz S, Jacobsen L, Hansen LH, Vester B. A new mechanism for chloramphenicol, florfenicol and clindamycin resistance: methylation of 23S ribosomal RNA at A2503. Mol Microbiol. 2005;57:1064–73.
Long KS, Poehlsgaard J, Kehrenberg C, Schwarz S, Vester B. The Cfr rRNA methyltransferase confers resistance to Phenicols, Lincosamides, Oxazolidinones, Pleuromutilins, and Streptogramin A antibiotics. Antimicrob Agents Chemother. 2006;50:2500–5.
Tait-Kamradt A, Davies T, Cronan M, Jacobs MR, Appelbaum PC, Sutcliffe J. Mutations in 23S rRNA and ribosomal protein L4 account for resistance in pneumococcal strains selected in vitro by macrolide passage. Antimicrob Agents Chemother. 2000;44:2118–25.
Roberts MC. Update on macrolide-lincosamide-streptogramin, ketolide, and oxazolidinone resistance genes. FEMS Microbiol Lett. 2008;282:147–59.
Arthur M, Andremont A, Courvalin P. Distribution of erythromycin esterase and rRNA methylase genes in members of the family Enterobacteriaceae highly resistant to erythromycin. Antimicrob Agents Chemother. 1987;3:404–9.
Barthélémy P, Autissier D, Gerbaud G, Courvalin P. Enzymic hydrolysis of erythromycin by a strain of Escherichia coli. A new mechanism of resistance. J Antibiot. 1984;37:1692–6.
Noguchi N, Emura A, Matsuyama H, O’Hara K, Sasatsu M, Kono M. Nucleotide sequence and characterization of erythromycin resistance determinant that encodes macrolide 2′-phosphotransferase I in Escherichia coli. Antimicrob Agents Chemother. 1995;39:2359–63.
Noguchi N, Katayama J, O’Hara K. Cloning and nucleotide sequence of the mphB gene for macrolide 2′-phosphotransferase II in Escherichia coli. FEMS Microbiol Lett. 1996;144:197–202.
Schmitz FJ, Sadurski R, Kray A, Boos M, Geisel R, Kohrer K, Verhoef J, Fluit AC. Prevalence of macrolide-resistance genes in Staphylococcus aureus and Enterococcus faecium isolates from 24 European university hospitals. J Antimicrob Chemother. 2000;45:891–4.
Chesneau O, Tsvetkova K, Courvalin P. Resistance phenotypes conferred by macrolide phosphotransferases. FEMS Microbiol Lett. 2007;269:317–22.
Boumghar-Bourtchai L, Mariani-Kurkdjian P, Bingen E, Filliol I, Dhalluin A, Ifrane SA, Weill FX, Leclercq R. Macrolide-resistant Shigella sonnei. Emerg Infect Dis. 2008;14:1297–9.
Phuc Nguyen MC, Woerther PL, Bouvet M, Andremont A, Leclercq R, Canu A. Escherichia coli as reservoir for macrolide resistance genes. Emerg Infect Dis. 2009;15:1648–50.
Matsuoka M, Endou K, Kobayashi H, Inoue M, Nakajima Y. A plasmid that encodes three genes for resistance to macrolide antibiotics in Staphylococcus aureus. FEMS Microbiol Lett. 1998;167:221–7.
Leclercq R, Brisson-Noel A, Duval J, Courvalin P. Phenotypic expression and genetic heterogeneity of lincosamides inactivation in Staphylococcus spp. Antimicrob Agents Chemother. 1987;31:1887–91.
Bozdogan B, Berrezouga L, Kuo M, Yurek D, Farley K, Stockman B, Leclercq R. A new resistance gene, linB, conferring resistance to lincosamides by nucleotidylation in Enterococcus faecium HM1025. Antimicrob Agents Chemother. 1999;43:925–9.
Heir E, Lindstedt BA, Leegaard TM, Gjernes E, Kapperud G. Prevalence and characterisation of integrons in blood culture Enterobacteriaceae and gastrointestinal Escherichia coli in Norway and reporting of a novel class I integron-located lincosamide resistance gene. Ann Clin Microbiol Antimicrob. 2004;3:12.
Wang J, Shoemaker N, Wang GR, Salyers A. Characterization of a Bacteroides mobilizable transposon of a functional lincomycin resistance gene. J Bacteriol. 2000;182:3559–71.
Achard A, Villers C, Pichereau V, Leclercq R. New lnu(C) gene conferring resistance to lincomycin by nucleotidylation in Streptococcus agalactiae UCN36. Antimicrob Agents Chemother. 2005;49:2716–9.
Petinaki E, Guérin-Faublée V, Pichereau V, Villers C, Achard A, Malbruny B, Leclercq R. Lincomycin resistance gene lnu(D) in Streptococcus uberis. Antimicrob Agents Chemother. 2008;52:626–30.
Achard A, Leclercq R. Characterization of a small mobilizable transposon, MTnSag1, in Streptococcus agalactiae. J Bacteriol. 2007;189:4328–31.
Gravey F, Galopin S, Grall N, Auzou M, Andremont A, Leclercq R, Cattoir V. Lincosamide resistance mediated by lnu(C) (L phenotype) in a Streptococcus anginosus clinical isolate. J Antimicrob Chemother. 2013;68(11):2464–7.
Haenni M, Saras E, Bertin S, Leblond P, Madec JY, Payot S. Diversity and mobility of integrative and conjugative elements in bovine isolates of Streptococcus agalactiae, S. dysgalactiae subsp. dysgalactiae, and S. uberis. Appl Environ Microbiol. 2010;76:7957–65.
Haenni M, Saras E, Chaussière S, Treilles M, Madec JY. ermB-mediated erythromycin resistance in Streptococcus uberis from bovine mastitis. Vet J. 2011;189:356–8.
Hershberger E, Donabedian S, Konstantinou K, Zervos MJ. Quinupristin-dalfopristin resistance in gram-positive bacteria: mechanism of resistance and epidemiology. Clin Infect Dis. 2004;38:92–8.
Li XZ, Nikaido H. Efflux-mediated drug resistance in bacteria. Drugs. 2004;64:159–204.
Singh KV, Weinstock GM, Murray BE. An Enterococcus faecalis ABC homologue (Lsa) is required for the resistance of this species to clindamycin and quinupristin-dalfopristin. Antimicrob Agents Chemother. 2002;46:1845–50.
Kehrenberg C, Ojo KK, Schwarz S. Nucleotide sequence and organization of the multiresistance plasmid pSCFS1 from Staphylococcus sciuri. J Antimicrob Chemother. 2004;54:936–9.
Malbruny B, Werno AM, Anderson TP, Murdoch DR, Leclercq R. A new phenotype of resistance to lincosamides and streptogramin A-type antibiotics in Streptococcus agalactiae in New Zealand. J Antimicrob Chemother. 2004;54:1040–4.
Malbruny B, Werno AM, Murdoch DR, Leclercq R, Cattoir V. Cross-resistance to lincosamides, streptogramins A, and pleuromutilins due to the lsa(C) gene in Streptococcus agalactiae UCN70. Antimicrob Agents Chemother. 2011;55:1470–4.
Li B, Wendlandt S, Yao J, Liu Y, Zhang Q, Shi Z, Wei J, Shao D, Schwarz S, Wang S, Ma Z. Detection and new genetic environment of the pleuromutilin-lincosamide-streptogramin A resistance gene lsa(E) in methicillin-resistant Staphylococcus aureus of swine origin. J Antimicrob Chemother. 2013;68:1251–5.
Dowzicky M, Talbot GH, Feger C, Prokocimer P, Etienne J, Leclercq R. Characterization of isolates associated with emerging resistance to quinupristin/dalfopristin (Synercid) during a worldwide clinical program. Diagn Microbiol Infect Dis. 2000;37:57–62.
Isnard C, Malbruny B, Leclercq R, Cattoir V. Genetic basis for in vitro and in vivo resistance to lincosamides, streptogramins A and pleuromutilins (LSAP phenotype) in Enterococcus faecium. Antimicrob Agents Chemother. 2013;57(9):4463–9.
Haroche J, Morvan A, Davi M, Allignet J, Bimet F, El Solh N. Clonal diversity among streptogramin A-resistant Staphylococcus aureus isolates collected in French hospitals. J Clin Microbiol. 2003;41:586–91.
Novotna G, Janata J. A new evolutionary variant of the streptogramin A resistance protein, Vga(A)LC, from Staphylococcus haemolyticus with shifted substrate specificity towards lincosamides. Antimicrob Agents Chemother. 2006;50:4070–6.
Tessé S, Trueba F, Berthet N, Hot C, Chesneau O. Resistance genes underlying the LSA phenotype of French staphylococcal isolates. Antimicrob Agents Chemother. 2013;57(9):4543–6.
Ambrose KD, Nisbet R, Stephens DS. Macrolide efflux in Streptococcus pneumoniae is mediated by a dual efflux pump (mel and mef) and is erythromycin inducible. Antimicrob Agents Chemother. 2005;48:4203–9.
Leclercq R. Mechanisms of resistance to macrolides and lincosamides: nature of the resistance elements and their clinical implications. Clin Infect Dis. 2002;34:482–92.
Santagati M, Iannelli F, Oggioni MR, Stefani S, Pozzi G. Characterization of a genetic element carrying the macrolide efflux gene mef(A) in Streptococcus pneumoniae. Antimicrob Agents Chemother. 2000;44:2585–7.
Gay K, Stephens DS. Structure and dissemination of a chromosomal insertion element encoding macrolide efflux in Streptococcus pneumoniae. J Infect Dis. 2001;184:56–65.
Ojo KK, Striplin MJ, Ulep CC, Close NS, Zittle J, Luis H, Bernardo M, Leitao J, Roberts MC. Staphylococcus efflux msr(A) gene characterized in Streptococcus, Enterococcus, Corynebacterium, and Pseudomonas isolates. Antimicrob Agents Chemother. 2006;50:1089–91.
Davidson AL, Dassa E, Orelle C, Chen J. Structure, function, and evolution of bacterial ATP-binding cassette systems. Microbiol Mol Biol Rev. 2008;72:317–64.
Ross JI, Eady EA, Cove JH, Cunliffe WJ, Baumberg S, Wootton JC. Inducible erythromycin resistance in staphylococci is encoded by a member of the ATP-binding transport super-gene family. Mol Microbiol. 1990;4:1207–14.
Reynolds E, Ross JI, Cove JH. Msr(A) and related macrolide/streptogramin resistance determinants: incomplete transporters? Int J Antimicrob Agents. 2003;22:228–36.
Fiebelkorn KR, Crawford SA, McElmeel ML, Jorgensen JH. Practical disk diffusion method for detection of inducible clindamycin resistance in Staphylococcus aureus and coagulase-negative staphylococci. J Clin Microbiol. 2003;41:4740–4.
Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing; 21th informational supplement. M100-S11. Wayne, PA: CLSI; 2011.
Jorgensen JH, Crawford SA, McElmeel ML, Fiebelkorn KR. Detection of inducible clindamycin resistance of staphylococci in conjunction with performance of automated broth susceptibility testing. J Clin Microbiol. 2004;42:1800–2.
Zelazny AM, Ferraro MJ, Glennen A, Hindler JF, Mann LM, Munro S, Murray PR, Reller LB, Tenover FC, Jorgensen JH. Selection of strains for quality assessment of the disk induction method for detection of inducible clindamycin resistance in staphylococci: a CLSI collaborative study. J Clin Microbiol. 2005;43:2613–5.
Burucoa C, Garnier M, Silvain C, Fauchère JL. Quadruplex real-time PCR assay using allele-specific scorpion primers for detection of mutations conferring clarithromycin resistance to Helicobacter pylori. J Clin Microbiol. 2008;46:2320–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Cattoir, V., Leclercq, R. (2017). Resistance to Macrolides, Lincosamides, and Streptogramins. In: Mayers, D., Sobel, J., Ouellette, M., Kaye, K., Marchaim, D. (eds) Antimicrobial Drug Resistance. Springer, Cham. https://doi.org/10.1007/978-3-319-46718-4_18
Download citation
DOI: https://doi.org/10.1007/978-3-319-46718-4_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-46716-0
Online ISBN: 978-3-319-46718-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)