Abstract
This chapter is dedicated to basic unenhanced, and static enhanced MRI. Distinction is made between imaging for local staging and for tissue characterization purpose, as well as between what is essential, what should be avoided, and what are useful additional techniques. An appropriate choice of imaging planes is suggested, stressing the importance of axial plane imaging for local staging.
For unenhanced MRI SE T1-WI and an optimal fluid-sensitive sequence are mandatory. The added value of fat-suppressed T1-WI for tissue characterization is discussed.
Enhanced MRI is not always mandatory but usually improves the evaluation of the internal structure of a tumor. Nonfat-suppressed-enhanced T1-WI is very useful for surgical planning.
Fat-suppressed-enhanced T1-WI is very popular, although not a routine requirement. Its advantages, disadvantages, and possible misinterpretation of Gd uptake are explained.
Subtraction images might be useful to differentiate between a subacute hematoma and a hemorrhagic tumor. Finally the limitation of static enhanced MRI and the added value of dynamic enhanced MRI are briefly discussed.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Due to its unequaled soft tissue contrast and multiplanar imaging capability, MRI is the modality of choice to image soft tissue tumors. This chapter is dedicated to basic unenhanced and static enhanced MRI. Advanced MRI and posttreatment imaging are discussed in other chapters. Distinction will be made between imaging for local staging and tissue characterization purpose, as well as between what is essential, what should be avoided, and what are useful additional techniques.
MR imaging should be of the highest possible quality to provide all necessary information needed for adequate local staging as well as grading of a soft tissue tumor.
Local Staging
Accurate staging needs precise localization of a tumor within its anatomical compartment and relative to important surrounding landmarks and determination whether a mass is confined to its compartment or whether it is invading or encasing surrounding structures [2]. Imaging should always precede biopsy, as blood and edema that follow a biopsy can be difficult to differentiate from tumor or the peritumoral reactive zone, with or without Gd administration. An appropriate decision whether or not to perform limb-salvaging surgery based on a post-biopsy MR examination may be impossible.
Tissue Characteristics
Although tissue characteristics derived from MRI alone are often insufficient to predict a specific pathological diagnosis, a well-performed MRI helps to narrow down the differential diagnosis, facilitating the clinical management. MRI is essential for the decision whether or not to perform a biopsy and planning of the optimal, most informative biopsy site. Lesions in which the observer is highly confident of a benign diagnosis at MR may not require histologic biopsy [25].
2 Imaging Planes
The strategy in designing the optimal MR examination depends on the location of a lesion, the desired coverage of the region to be examined, the available hardware (field strength, coils), the time constraints, and the local preferences. The MR examination should be supervised, tailored to the individual patient. Careful assessment of the region of clinical concern should precede any imaging to ensure its complete coverage with the most appropriate coil and to avoid waste of time due to repositioning of the patient after the first imaging sequence.
Demarcation of subtle, doubtful, or diffuse lesions with a lipid marker prior to imaging may be helpful. Care should be taken not to compress the mass by this marker. Images should be of sufficiently high spatial resolution to demonstrate relevant morphologic features and anatomic detail. The use of a large field-of-view results in loss of spatial resolution. It is usually not necessary to examine the contralateral side for comparison when an extremity is being evaluated. A wider field-of-view may be used for initial detection or when multiple lesions are suspected, followed by a smaller field-of-view targeted to the lesion.
Imaging usually starts with a sequence in the most appropriate longitudinal plane. Anteriorly or posteriorly located lesions are best imaged in a sagittal plane, medial or lateral localizations in a coronal plane. Care should be taken to respect the anatomical orthogonal planes since with excessive rotation of a limb, inappropriate positioning of longitudinal scan planes results in images which are difficult to interpret and probably useless for surgical planning. Since this sequence should depict the lesion, together with eventually surrounding edema, with the highest conspicuity and over its entire cephalocaudal extent, fat-suppressed fast spin-echo T2-weighted or STIR imaging with a large field-of-view is recommended.
This first sequence in the longitudinal plane is usually followed by imaging in the axial plane. Since most anatomical compartments of the extremities are oriented longitudinally, accurate assessment of localization and extent of a tumor requires imaging in the axial plane, in which the majority of sequences should be obtained. Not only the tumor but also the peritumoral edema at its proximal and distal poles should be covered by these axial sequences. As a rule, the most proximal and distal slices should show no pathology. Usually T1- and T2-weighted acquisitions are obtained in the axial plane at exactly the same location, thus allowing an image-by-image comparison. Contrast-enhanced images have to be acquired at least in the axial and the most useful longitudinal plane and at the same positions as the precontrast images.
The choice of an additional imaging plane depends on the location of the lesion and the clinical questions to be answered. Inclusion of the nearest joint, or another key anatomic landmark, serving as a reference in at least one of the longitudinal imaging planes is essential for surgical planning since especially deeply situated masses can be hard to localize based on clinical examination alone. Oblique planes may also be useful. Typical examples are oblique sagittal images for optimal depiction of a lesion’s relation to the scapula or the iliac wing.
3 Unenhanced MRI
For detection, local staging, and characterization of a mass, the use of conventional spin-echo sequences is recommended. It is the most reproducible technique, the one with which we are most familiar for tumor evaluation, and the most often referenced in tumor imaging literature [19].
3.1 T1-Weighted Imaging (T1-WI)
Local Staging
In delineation of a soft tissue tumor, distinction must be made between tumor-to-muscle and tumor-to-fat contrast. On T1-WI, with exception of fat-containing tumors, soft tissue tumors are generally more or less isointense to muscle, resulting in low tumor-to-muscle but high tumor-to-fat contrast (Figs. 4.1b, 4.2a, 4.3a, and 4.4a). As a consequence T1-WI is essential in the identification of anatomical structures and delineation of a tumor from intermuscular fat planes (Figs. 4.1b and 4.3a), fat surrounding neurovascular structures, subcutaneous fat, and fatty bone marrow. Since identification of anatomical fat planes is essential for surgical planning, nonfat-suppressed T1-WI in the axial plane is mandatory.
(a–c) Myxoid liposarcoma in the distal thigh. (a) Axial STIR sequence. A sharply margined mass lesion with homogeneous high signal intensity is interposed between the vastus lateralis muscle and the distal femur. (b) Axial unenhanced T1-weighted image. A very low tumor-to-muscle contrast is shown with the lesion’s signal intensity slightly lower than muscle. In combination with the high signal intensity on STIR sequence, this lesion could be mistaken for a cyst based on unenhanced sequences alone. Also note the very high tumor-to-fat contrast, typical for unenhanced T1-weighted images. (c) Axial Gd-enhanced T1-weighted image. The lesion shows a definite and heterogeneous enhancement, inconsistent with a cystic origin of the lesion. Although there is a decreased tumor-to-fat contrast, delineation of the tumor from the adjacent fat still is perfectly possible. In addition, due to a clear increase in tumor-to-muscle contrast, this sequence is very suitable for surgical planning. Beside the adequate delineation of the tumor, this enhanced T1-weighted sequence improves the evaluation of the internal structure of the tumor. It helps to differentiate viable tumor from a cyst, with a totally different surgical approach, and helps to select an appropriate biopsy site. Because it mainly consists of less well-vascularized and myxoid or necrotic tissue, a biopsy in de posterior part of the lesion should be avoided
(a, b) Myxoid round cell liposarcoma in the upper arm. (a) Axial unenhanced SE T1-weighted image. Large tumor in the lateral head of the triceps muscle, isointense to muscle, resulting in poor tumor-to-muscle but high tumor-to-fat contrast. In the posterior half of the lesion, a small hyperintense area is visible, consistent with fat or another short-T1 tissue. (b) Axial unenhanced fat-suppressed SE T1-weighted image. Fat suppression clearly decreases the signal intensity of the small area, consistent with fatty tissue, raising the suspicion of a possible liposarcoma
(a, b) B-cell non-Hodgkin lymphoma of the left buttock. (a) Axial unenhanced SE T1-weighted image. Large mass in the left gluteus maximus muscle, slightly hyperintense to muscle. Due to high muscle-to-fat contrast, a fat plane is clearly visible anterior to the mass. In the lateral part, a small hyperintense area is visible, consistent with fat or another short-T1 tissue. (b) Axial unenhanced fat-suppressed SE T1-weighted image. Due to the rescaling effect, the subtle hyperintensity of the mass compared with the surrounding muscle is magnified, hence becoming more obvious. Fat suppression doesn’t decrease the signal intensity of the small lateral area, and rescaling even increases its signal intensity. Hence, it is unlikely that we are dealing with a liposarcoma. Notice fat suppression results in obscuring of anatomical fat planes
(a–c) Malignant peripheral nerve sheath tumor in the distal vastus medialis muscle of the thigh. (a) Axial unenhanced SE T1-weighted image. The signal intensity of the mass is heterogeneous, grossly isointense to muscle with some slightly hyperintense areas. (b) Axial unenhanced fat-suppressed SE T1-weighted image. Fat suppression results in magnification of the signal heterogeneity, increasing the conspicuity of a small hyperintense area in the medial half of the lesion. (c) Axial Gd-enhanced fat-suppressed SE T1-weighted image. After Gd administration two rims of enhancement are visible, one surrounding the lesion and another surrounding a hypointense area in the medial half of the lesion. Since Gd-enhanced blood vessels now are the most hyperintense structures, rescaling occurs resulting in downscaling of the slightly hyperintense area in the medial half of the lesion. Due to the same rescaling, assessment of Gd uptake in the lateral half and posterior part of the lesion is difficult. Most likely the uptake is slight. This would be even more difficult if precontrast fat-suppressed images weren’t available and assessment was based on comparison of a with c. In this case subtraction images, subtracting sequence b from c, and/or nonfat-suppressed Gd-enhanced T1-WI would have been of great value
Because of the low tumor-to-muscle contrast, T1-WI in another than the axial plane usually is not useful. For fatty tumors, with excellent tumor-to-muscle contrast, additional T1-WI in a longitudinal plane might be helpful for local staging.
Tissue Characteristics
Tissue characterization is based on several imaging parameters, some of them related to the signal intensity on T1-WI [4]. Unenhanced T1-WI also is essential as a baseline for contrast-enhanced studies.
3.2 Fat-Suppressed T1-Weighted Imaging (FS T1-WI)
Extra information can be derived from the addition of a fat-suppression technique to a T1-weighted sequence. Chemical shift-based, also known as frequency selective, fat suppression should be used in these cases.
Local Staging
Suppression of the high signal intensity of fat results in loss of tumor-to-fat contrast, obscuring fat planes, which is a major disadvantage in planning of surgery (Figs. 4.2b and 4.3b). For this reason FS T1-WI should never be performed without its non-FS equivalent.
Tissue Characteristics
The added value of FS T1-WI for tissue characterization is threefold : a more efficient use of the dynamic range for display of tissue contrast, differentiation between fat and other short-T1 tissues, and a baseline for comparison with FS contrast-enhanced T1-WI.
Suppression of the high signal intensity of fat induces a rescaling, a redistribution of gray levels, leading to a more efficient use of the dynamic range for display of tissue contrast [12]. Minor differences in signal intensity between tissues on non-FS T1-WI get magnified, and signal inhomogeneity, an important parameter in characterization, is better evaluated [10] (Figs. 4.3a, b and 4.4a, b)
A signal hyperintense to muscle is considered to be hyperintense on T1-WI. Hyperintense substances on T1-WI include fat, methemoglobin, melanin, and proteinaceous fluid [30]. Chemical shift-based FS selectively decreases the signal intensity of fat, while other hyperintense tissues remain hyperintense [18, 22] (Figs. 4.2, 4.3, and 4.5b). FS T1-WI is useful if a lesion shows high signal intensity on the T1-WI [24, 30], e.g., to differentiate fatty tissue from a recent hematoma. It is important to perform the sequence with frequency-selective FS. Inversion-recovery FS is nonspecific and can cause loss of signal of not only fat but also of other short-T1 substances [30].
(a–d) Necrotic, hemorrhagic high-grade pleiomorphic sarcoma of the posterior thigh compartment. (a) Sagittal unenhanced T1-weighted image. The large mass lesion is showing an inhomogeneous high signal intensity, possibly of lipomatous origin. (b) Sagittal fat-suppressed-unenhanced T1-weighted image. Persistence of the high signal intensity despite fat suppression is inconsistent with the hypothesis of a fatty tumor and in favor of the presence of methemoglobin in a large hematoma or hemorrhagic tumor. (c) Sagittal fat-suppressed Gd-enhanced T1-weighted image. Differentiation between hematoma and hemorrhagic tumor needs administration of gadolinium (Gd) contrast. Unfortunately, because of the presence of intralesional methemoglobin, the conspicuity of Gd enhancement doesn’t benefit from the fat-suppression technique. Based on this sequence, it is virtually impossible to differentiate enhancement from methemoglobin. (d) Sagittal subtraction image (b subtracted from c). Subtraction of pre- from post-Gd fat-suppressed T1-weighted images permits to isolate the areas of Gd enhancement, showing a thin rim enhancement and only some small foci of mural enhancement in the upper posterior part of the lesion
As explained in the contrast-enhanced section, it is essential to ensure that a precontrast fat-suppressed sequence is available for comparison if the postcontrast image is intended to be a fat-saturated T1-WI [12]. When time constraints are an issue, performing FS T1-WI frequently is not useful when the lesion is isointense or hypointense to muscle on T1-WI.
3.3 Fluid-Sensitive Sequences
Local Staging
Fluid-sensitive sequences are important for the detection of a tumor and the differentiation of a hyperintense tumor and its surrounding edema from the hypointense surrounding muscles (Fig. 4.6b). The reactive edema around a tumor often contains satellite tumor micronodules and is considered as an integral part of the lesion and therefore is removed en bloc with the tumor [14, 17, 21, 23]. The conspicuity of this peritumoral edema should be as high as possible. The conspicuity with a classic double-echo T2-weighted sequence is acceptable. Its main disadvantage remains the relatively long acquisition times [19], which can be overcome by the use of a FSE T2-weighted sequence. However, since fat appears bright on FSE sequences [2, 13], with subsequent decrease of conspicuity of tumors or edema juxtaposed to fat [19], FSE T2-weighted sequences without fat suppression should not be used in tumor imaging (Fig. 4.6a). For maximal conspicuity of a tumor and its surrounding edema against the background of muscle and fat, a fat-suppressed fluid-sensitive sequence should be used. Usually a chemical shift-based fat-suppression technique is chosen. Its acquisition time is shorter with a higher signal-to-noise ratio compared to STIR imaging [8]. A disadvantage is its susceptibility to magnetic field inhomogeneities. STIR provides more uniform fat suppression but results in longer scan times or lower signal-to-noise ratio [3].
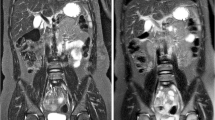
(a, b) Synovial sarcoma of the proximal thigh. (a) Coronal FSE T2-weighted image. A mass consisting of several intermediate to hypointense nodulus and a strongly hyperintense medial area is shown. No clear perilesional edema is visible, although this assessment is difficult due to the artificially high signal intensity of fat, typical for this FSE T2-weighted sequence. (b) Coronal STIR sequence. Signal intensity of the mass is comparable with the previous sequence. However, due to the decreased signal intensity of fat by this inversion recovery type of fat suppression, resulting in a high fluid-to-fat contrast, a reactive zone of perilesional edema at the distal pole of the lesion becomes unequivocally visible. This case illustrates the ineffectiveness of FSE T2-WI for local staging purpose
Tissue Characteristics
Spin-echo T2-WI is essential for tumor characterization [4]. Since fat appears artificially bright on FSE sequences, FSE T2-WI without fat suppression should not be used in tumor characterization [2, 13]. It is important to realize that the signal intensity of a mass can appear quite different on a FS T2-WI, as compared with the corresponding non-FS T2-WI because of the rescaling effect. FS sequences alone cannot be used to reliably describe the signal characteristics of a mass [30].
As with T1-WI chemical shift-based FS T2-WI can be used to confirm the presence of fat in a lesion. In addition it also increases the conspicuity of non-lipomatous components in lipomatous tumors, the latter helping in distinguishing lipoma from well-differentiated liposarcoma [9].
Since its fat suppression is nonspecific, STIR imaging should not be used for tissue characterization. Nonfatty tissues can be suppressed along with fat, and fatty tissues may not be fully suppressed. Knowledge of this pitfall is necessary for correct image interpretation [1].
3.4 T2* Gradient Echo Imaging
Tissue Characteristics
In some selected applications, a T2*-weighted gradient echo sequence can be very useful. In the absence of gas or calcifications on radiographs and computed tomography, a marked signal loss on GRE sequences is almost pathognomonic for hemosiderin (Fig. 4.7) [11]. When present in sufficient quantities, hemosiderin can appear more prominent, the so-called blooming, and therefore useful in the diagnosis of hemangiomas, PVNS, and mature hematomas [16].
(a, b) Giant cell tumor of tendon sheath of the foot. (a) Axial unenhanced SE T1-weighted image. Unsharply demarcated mass along the tibialis posterior insertion, deep to the abductor hallucis muscle, causing an erosion at the medioplantar side of the navicular bone. The lesion shows a heterogeneous signal intensity with strongly hypointense areas, consistent with possible collagen content, calcifications, or hemosiderin. (b) Axial T2*-weighted gradient echo image. On this gradient echo sequence, the whole lesion shows a profound signal loss, the so-called blooming effect, highly suggestive of the presence of hemosiderin, consistent with giant cell tumor of tendon sheath (extra-articular type of PVNS)
4 Contrast-Enhanced MRI
Routine IV Gd administration is not a requirement and unnecessary when the result wouldn’t influence patient care. Characterization and delineation of, e.g., lipomas and some subtypes of vascular malformations are easily performed on unenhanced sequences. However, contrast administration is certainly helpful in staging, characterization, and clinical management of most of the soft tissue tumors. Generally contrast is administered in a nondynamic fashion: after contrast injection a relatively longer acquisition of a high spatial resolution is obtained.
Local Staging
Enhanced T1-WI improves the delineation of a tumor (Figs. 4.1b, c and 4.5), helping to highlight tissue planes to aid in assessing the degree of invasion into surrounding structures [15].
Tissue Characteristics
Enhanced T1-WI improves the evaluation of the internal structure of a tumor (Figs. 4.1b, c and 4.5). It demonstrates the relative vascularity of a tumor and helps to differentiate well-perfused, viable tumor from tumor necrosis, intratumoral hemorrhage from hematoma, cysts from solid tumors (Fig. 4.1), and cystic parts from myxoid parts. Contrast-enhanced MR is essential for the decision whether or not to perform a biopsy and planning of the biopsy site. Since every additional procedure increases the risk of inadvertent tumor cell contamination, the selection of the biopsy site should be well considered. A biopsy containing well-vascularized viable tumor will be of greater value than a nondiagnostic specimen with hemorrhage, edema, or necrotic tissue. If only static enhanced MRI is used, the area showing the most intense enhancement should be selected as biopsy site [26] (Fig. 4.1c).
4.1 Contrast-Enhanced T1-Weighted Imaging
Local Staging
On T1-WI tumor-to-muscle contrast usually increases markedly after contrast administration (Fig. 4.1b, c). Although there is no improvement of this tumor-to-muscle contrast when compared with fluid-sensitive sequences [6, 28], the static enhanced T1-weighted sequence without fat suppression is very useful. As an “almost-all-in-one sequence,” it has the anatomical detail, fat planes inclusive, typical of T1-WI, a tumor-to-muscle contrast equal to that of fluid-sensitive sequences, and it provides useful information on tumor content due to the Gd administration (Fig. 4.1c). Most surgeons use these images for planning their interventions. A disadvantage of enhanced T1-WI is a decreased tumor-to-fat contrast (Fig. 4.8).
(a–c) Hibernoma of the left groin. (a) Axial unenhanced SE T1-weighted image. Mass between the femoral neurovascular bundle and the pectineus muscle, hyperintense to muscle, and hypointense to fat, resulting in an excellent tumor-to-fat contrast. (b) Axial Gd-enhanced SE T1-weighted image. The strong Gd uptake by the lesion causes a complete loss of tumor-to-fat contrast. (c) Axial fat-suppressed Gd-enhanced SE T1-weighted image. Due to suppression of the high signal intensity of fat, the excellent tumor-to-fat contrast is restored, allowing the exclusion of infiltration of the mass into the surrounding fat
Tissue Characteristics
As already mentioned, this sequence provides useful information on tumor content.
4.2 Fat-Suppressed Contrast-Enhanced T1-Weighted Imaging
Chemical shift-based fat suppression may be applied on contrast-enhanced T1-WI. STIR sequences should not be used since not only fat but also enhancing tissue will be shown with a reduced signal intensity [1].
Local Staging
Enhanced T1-WI decreases or even obscures the tumor-to-fat contrast. Applying fat suppression to postcontrast T1-WI restores the optimal tumor-to-fat contrast (Fig. 4.8). Since FS Gd-enhanced T1-WI shows areas of contrast enhancement with a greater conspicuity compared with T1-WI without fat suppression, subsequently resulting in images which are easier to interpret, the use of this sequence became very popular. However, since fat suppression results in obscured fat planes, which is a major disadvantage in planning of surgery, this sequence should never be acquired without its non-FS equivalent. For local staging purpose, it is only recommended when tumor abuts or infiltrates adjacent fat.
Tissue Characteristics
The assessment of Gd uptake usually occurs by comparison of non-FS precontrast T1-WI with postcontrast T1-WI. With these images detection of Gd uptake can be difficult when differences are subtle in case of minor Gd uptake, or when on precontrast images the lesion already shows hyperintense areas (Fig. 4.5).
Conspicuity of Gd uptake increases with the use of FS T1-WI. Suppression of the high signal intensity of fat induces a rescaling, magnifying minor differences in signal intensity between tissues due to subtle Gd uptake. This rescaling effect is responsible for an apparently obvious Gd enhancement of tissue that only shows minimal enhancement on non-FS T1-WI [10, 12].
When on precontrast images, the lesion shows hyperintense areas, the assessment of Gd uptake will only benefit from fat suppression when hyperintensity is due to fat, resulting in suppression of the hypersignal with subsequently increased conspicuity of enhancement along or within these fatty areas. When the precontrast hyperintensity is of nonfatty origin, fat suppression doesn’t decrease the signal, enhancement conspicuity might not increase, and areas that are slightly hyperintense might be rescaled moderately to strongly hyperintense.
One should be aware of the risk of misinterpretation when Gd uptake is evaluated by comparison of FS-enhanced T1-WI with non-FS precontrast T1-WI since a high signal intensity of a lesion on FS-enhanced T1-WI can be the consequence of two variables that have been changed [12]. The change of one variable by applying fat suppression to precontrast T1-WI causes a rescaling effect, leading to an increased signal intensity of tissues, especially those which are hyperintense to muscle on non-FS images. Differences in signal intensity between T1-WI and FS T1-WI are the result of fat suppression and rescaling (Figs. 4.2, 4.3, and 4.4).
IV administration of Gd changes another variable. Differences in signal intensity between pre- and postcontrast T1-WI, or between pre- and postcontrast FS T1-WI, are the result of Gd uptake in vascularized tissues (Figs. 4.1, 4.4, and 4.8). The change of two variables simultaneously by comparison of precontrast T1-WI with postcontrast FS T1-WI might hamper interpretation since differences in signal intensity can be the result of fat suppression, rescaling, or Gd uptake. The rescaling effect might be responsible for apparently obvious Gd enhancement of tissue that only shows minimal enhancement on non-FS T1-WI [10, 12], or even apparently slight or moderate enhancement of tissue which is non-enhancing on non-FS T1-WI (Fig. 4.4).
Gd administration might cause a downscaling effect on FS T1-WI. Hyperintense areas may lose signal intensity when they are not or only minimally enhancing due to rescaling induced by strongly Gd-enhancing tissue (Fig. 4.4). In these cases interpretation might be more difficult. Availability of non-FS pre- and postcontrast T1-WI, or the use of subtraction images, might facilitate interpretation.
As a consequence, reliable interpretation of FS Gd-enhanced T1-WI is only possible if also unenhanced FS T1-WI and enhanced non-FS T1-WI are obtained, resulting in longer examination times. However, the use of FS-enhanced T1-WI certainly is not a routine requirement [12].
4.3 Subtraction Images
With subtraction imaging, an unenhanced T1-WI sequence is digitally subtracted from the identical Gd-enhanced sequence by means of a postprocessing tool. The exact similarity in all imaging parameters between both sequences to be subtracted is required. Any gray scale value other than signal void on subtraction images is consistent with Gd enhancement. To obtain useful subtraction images, the patient should not change position during the examination, and IV access should be acquired before the start of the examination.
Tissue Characteristics
Subtraction images are especially useful in lesions showing hyperintense signal on precontrast T1-WI due to nonfatty content (methemoglobin, melanin, or proteinaceous fluid). Determination of the presence or absence of enhancement in these lesions might be critical, and visual assessment of enhancement is difficult or even impossible [5]. The subtraction technique can adequately determine Gd enhancement on a background of hyperintense signal, which is extremely important in differentiation between a subacute hematoma and a hemorrhagic tumor (Fig. 4.5). When time constraints are a matter, enhancement conspicuity can also be obtained by the use of image subtraction.
4.4 Static Versus Dynamic Enhanced MRI
Static Gd-enhanced MRI is performed in the equilibrium state when the Gd concentration in the interstitium equals that of plasma. Dynamic Gd-enhanced MRI provides physiologic information, such as tissue perfusion and vascularization, capillary permeability, and the volume of the interstitial space, which is not available on static Gd-enhanced MRI (see Chap. 5) [27, 29].
Local Staging
Reliable differentiation between tumor and peritumoral edema cannot be made by means of T2-WI nor by static enhanced T1-WI. Dynamic enhanced MR studies can contribute to the differentiation of tumor from edema, because edema shows a much more gradual increase in signal intensity than the tumor tissue.
Tissue Characteristics
Static enhanced MRI has a limited value in the characterization of soft tissue tumors and the differentiation of benign from malignant lesions. Dynamic enhanced studies improve differentiation between highly vascularized, less well-vascularized, and necrotic tumor areas, which further narrows down the differential diagnosis, helps to increase the suspicion of malignant lesions [25], and is important in the selection of the highest vascularized, highest-grade part of the tumor for the biopsy site [20, 26].
Since dynamic enhanced sequences are obtained with lower spatial resolution, these should be followed by a delayed static enhanced study, which produces higher spatial resolution [7].
Key Points
-
1.
MR imaging should always precede biopsy since tumor staging based on a post-biopsy MR examination may be impossible.
-
2.
Adequate evaluation of tumor extent requires multiplanar imaging, but the axial plane is probably the most important. Meticulous description of the extent of peritumoral edema is mandatory.
-
3.
FSE T2-weighted sequences without fat suppression are far less appropriate for depiction of local tumor extent than fat-suppressed T2-WI.
-
4.
When contrast-enhanced MR is performed, pre- and postcontrast T1-WI without fat suppression is mandatory. Pre- and postcontrast fat-suppressed T1-WI is optional.
The use of fat-suppressed-enhanced T1-WI is only recommended when tumor abuts or infiltrates adjacent fat. Gd-enhancement conspicuity can also be obtained from subtraction images.
-
5.
Don’t use fat-suppressed T1-WI without their nonfat-suppressed equivalent since they obscure surgically important fat planes and because of the risk of misinterpretation of Gd enhancement.
-
6.
Since its fat suppression is nonspecific, STIR imaging should not be used for tissue characterization.
References
Amini B, Jessop AC, Ganeshan DM, Tseng WW, Madewell JE (2015) Contemporary imaging of soft tissue sarcomas. J Surg Oncol 111:496–503
Constable RT, Anderson AW, Zhong J, Gore JC (1992) Factors influencing contrast in fast spin-echo MR imaging. Magn Reson Imaging 10:497–511
Delfaut EM, Beltran J, Johnson G, Rousseau J, Marchandise X, Cotton A (1999) Fat suppression in MR imaging: techniques and pitfalls. Radiographics 19:373–382
De Schepper AM (2006) Grading and characterization of soft tissue tumors. In: De Schepper AM, Vanhoenacker F, Gielen J, Parizel PM (eds) Imaging of soft tissue tumors, 3rd edn. Springer, Berlin/Heidelberg/New York, pp 139–162
Eid M, Abougabal A (2014) Subtraction images: a really helpful tool in non-vascular MRI. Egypt J Radiol Nucl Med 45:909–919
Erlemann R, Reiser MF, Peters PE, Vasallo P, Nommensen B, Kusnierz-Glaz CR, Ritter J, Roessner A (1989) Musculoskeletal neoplasms: static and dynamic Gd-DTPA-enhanced MR imaging. Radiology 171:767–773
Fayad LM, Jacobs MA, Wang X, Carrino JA, Bluemke DA (2012) Musculoskeletal tumors: how to use anatomic, functional, and metabolic MR techniques. Radiology 265(2):340–356
Fleckenstein JL, Archer BT, Barker BA, Vaughan JT, Parkey RW, Peshock RM (1991) Fast short-tau inversion-recovery MR imaging. Radiology 179:499–504
Galant J, Marti-Bonmati L, Saez F, Soler R, Alcala-Santaella R, Navarro M (2003) The value of fat-suppressed T2 or STIR sequences in distinguishing lipoma from well-differentiated liposarcoma. Eur Radiol 13:337–343
Gielen J, De Schepper A, Parizel P, Wang X, Vanhoenacker F (2003) Additional value of magnetic resonance with spin echo T1-weighted imaging with suppression in characterization of soft tissue tumors. J Comput Assist Tomogr 27(3):434–441
Hardy PA, Kucharczyk W, Henkelman RM (1990) Cause of signal loss in MR images of old hemorrhagic lesions. Radiology 174:549–555
Helms CA (1999) The use of fat suppression in gadolinium-enhanced MR imaging of the musculoskeletal system : a potential source of error. AJR Am J Roentgenol 173:234–236
Henkelman RM, Hardy PA, Bishop JE, Poon CS, Piewes DB (1992) Why is fat bright in RARE and fast spin-echo imaging. J Magn Reson Imaging 2:533–540
Kaya M, Wada T, Nagoya S, Sasaki M, Matsumura T, Yamaguchi T, Hasegawa T, Yamashita T (2008) MRI and histological evaluation of the infiltrative growth pattern of myxofibrosarcoma. Skeletal Radiol 37:1085–1090
Kransdorf MJ, Murphey MD (2000) Radiologic evaluation of soft-tissue masses: a current perspective. AJR Am J Roentgenol 175:575–587
Mallinson PI, Chou H, Forster BB, Munk PL (2014) Radiology of soft tissue tumors. Surg Oncol Clin N Am 29:911–936
McDonald DJ (1994) Limb-salvage surgery for treatment of sarcomas of the extremities. AJR Am J Roentgenol 163:509–513
Mirowitz SA, Apicella P, Reinus WR, Hammerman AM (1994) MR imaging of bone marrow lesions: relative conspicuousness on T1-weighted, fat-suppressed T2-weighted, and STIR-images. AJR Am J Roentgenol 162:215–221
Rubin DA, Kneeland JB (1994) MR imaging of the musculoskeletal system: technical considerations for enhancing image quality and diagnostic yield. AJR Am J Roentgenol 163:1155–1163
Shapeero LG, Vanel D, Verstraete KL, Bloem JL (2002) Fast magnetic resonance imaging with contrast for soft tissue sarcoma viability. Clin Orthop Relat Res 397:212–227
Shuman WP, Patten RM, Baron RI, Liddell RM, Conrad EU, Richardson ML (1991) Comparison of STIR and spin-echo MR imaging at 1.5 T in 45 suspected extremity tumors: lesion conspicuity and extent. Radiology 179:247–252
Soulie D, Boyer B, Lescop J, Pujol A, Le Friant G, Cordoliani YS (1995) Liposarcome myxoide. Aspects en IRM. J Radiol 1:29–36
Stark D, Bradley W (1992) Magnetic resonance imaging, 2nd edn. Mosby Year Book, St.Louis
Taïeb S, Penel N, Vanseymortier L, Ceugnart L (2009) Soft tissue sarcomas or intramuscular haematomas ? Eur J Radiol 72:44–49
van Rijswijk CS, Geirnaerdt MJ, Hogendoorn PC, Taminiau AH, van Coevorden F, Zwinderman AH, Pope TL, Bloem JL (2004) Soft tissue tumors: value of static and dynamic Gadopentetate dimeglumine-enhanced MR imaging in prediction of malignancy. Radiology 233:493–502
Verstraete KL, Lang P (2000) Bone and soft tissue tumors: the role of contrast agents for MR imaging. Eur J Radiol 34:229–246
Verstraete KL, De Deene Y, Roels H, Dierick A, Uyttendaele D, Kunnen M (1994) Benign and malignant musculoskeletal lesions: dynamic contrast-enhanced MR imaging – parametric ‘first-pass’ images depict tissue vascularization and perfusion. Radiology 192:835–843
Verstraete KL, Vanzieleghem B, De Deene Y, Palmans H, De Greef D, Kristoffersen DT, Uyttendaele D, Roels H, Hamers J, Kunnen M (1995) Static, dynamic and first-pass MR imaging of musculoskeletal lesions using gadodiamide injection. Acta Radiol 36(1):27–36
Verstraete KL, Van der Woude HJ, Hogendoorn PC, De Deene Y, Kunnen M, Bloem JL (1996) Dynamic contrast-enhanced MR imaging of musculoskeletal tumors: basic principles and clinical applications. J Magn Reson Imaging 6(2):311–321
Wu JS, Hochman MG (2009) Soft-tissue tumors and tumorlike lesions: a systematic imaging approach. Radiology 253(2):297–316
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Brys, P. (2017). Magnetic Resonance Imaging: Basic Concepts. In: Vanhoenacker, F., Parizel, P., Gielen, J. (eds) Imaging of Soft Tissue Tumors. Springer, Cham. https://doi.org/10.1007/978-3-319-46679-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-46679-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-46677-4
Online ISBN: 978-3-319-46679-8
eBook Packages: MedicineMedicine (R0)