Abstract
Osteoarthritis (OA), the most prevalent form of arthritis, affects up to 15 % of the adult population and is principally characterized by degeneration of the articular cartilage component of the joint. While vital to its function as a weight-bearing tissue, the relatively simple structure and hypocellularity of cartilage severely limits its ability to self-heal. Indeed, treatments of human cartilage injuries are often at odds with the natural progression of OA, resulting in major clinical hurdles. Remarkably, several non-human animal groups are able to regenerate robust cartilage and heal cartilage injuries. This chapter begins with a review of these species to highlight possible clues for improving human cartilage repair. Next, the limitations of human cartilage healing are addressed, as well as current therapies for augmenting cartilage regeneration. Finally, future directions for bridging the gap between cartilage-regenerative responses are discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
4.1 Cartilage Structure and Function
Cartilage is a specialized tissue with several interesting characteristics that highlight a trade-off between function and healing. On the one hand, cartilage is an incredibly robust tissue, with the principal function of providing mechanical support, especially in weight-bearing circumstances. On the other hand, most cartilage exhibits almost a complete lack of intrinsic healing abilities once damaged. These two characteristics, mechanical durability and healing resistance, both stem from the unique structure of cartilage. Adult cartilage tissue is composed of over 90 % of extracellular matrix (ECM) and less than 10 % chondrocytes in total volume [1]. Thus cartilage is considered hypocellular, with few cartilage cells (chondrocytes ) embedded in an abundant ECM. It is the molecular compositions of the cartilage ECM that define its mechano-physical properties: Proteoglycans (PGs) are responsible for the osmotic swelling and the elastic properties of the cartilage tissue. The most abundant cartilage PG, aggrecan , contains a core protein complexed with covalently bound glycosaminoglycan (GAG) side chains of chondroitin sulfate and keratin sulfate . Aggrecan further associates with hyaluronic acid filaments via link proteins. These PGs , which are negatively charged, attract cations and associated water molecules. The charged GAG side chains also repel one another, thereby trapping more water and causing the cartilage tissue to swell in the absence of physical load. In fact, the cartilage ECM contains 65–80 % water in wet weight [2]. Upon application of load, the hydrated GAG side chains allow cartilage to resist compression as water is forced from the tissue. When cyclically loaded, this ebb and flow of liquid through the cartilage tissue enables nutrient transport to chondrocytes [2]. Another important component of the cartilage ECM, the cartilage network , is responsible for the tensile strength of the cartilage matrix [1]. Collagen , the most abundant ECM component in the body, is a triple helical macromolecule with a cross-banded fibrillar structure that also acts as a meshwork that traps large PGs . The main collagen found in cartilage is collagen type II (Col2) , but variations in the amounts of other collagen types and ECM components dictate the precise properties of the cartilage further classified as fibrocartilage , elastic cartilage , and hyaline cartilage [2]. Fibrocartilage is characterized by the inclusion of collagen type I (Col1) in the ECM and is found, for example, in the annulus fibrosus of intervertebral discs, the menisci, the pubic symphysis, and the temporomandibular joint. Elastic cartilage contains high amount of elastin and is found in the outer ear (auricular cartilage), the Eustachian tube, and the epiglottis. Hyaline cartilage matrix contains high amounts of Col2 , chondroitin sulfate and hyaluronan , and is found on the ventral surfaces of ribs, in the larynx, trachea, and bronchi, and on the articular surfaces of bones (articular cartilage), where it is responsible for load bearing and shock absorption. Articular cartilage is the most clinically relevant form of cartilage as it is intimately involved in the pathogenesis of osteoarthritis (OA) , and the last section of this chapter will focus specifically on articular cartilage healing.
While the high matrix-to-cell ratio of cartilage tissue underlies its mechanical properties, it also is responsible for its poor intrinsic healing capacities. In addition to being hypocellular, healthy adult cartilage is also avascular. Thus, injured cartilage has very few reserve chondrocytes available to synthesize new matrix. The chondrocytes that are present are trapped in their lacunae and embedded in dense cartilaginous matrix , making migration to wound sites difficult. Similarly, the lack of blood vessels also presents a barrier for stem cells from other parts of the body to reach the injured cartilage. Once cartilage tissue structure is compromised by a wound, the important nutrient transport environment begins to break down, causing loss of additional chondrocytes and cartilage tissue. Thus, rather than healing, even minor cartilage injuries can result in positive feedback scenarios in which large areas of cartilage are lost and do not regrow. Here we will examine special cases in the animal kingdom where cartilage does, in fact, naturally regenerate, as well as strategies for the therapeutic enhancement of cartilage healing .
4.2 Cartilage Formation During Embryonic Development and Adult Fracture Healing
Cartilage is initially formed in vertebrates during embryonic development of the skeletal system [3]. In fact, the early skeleton is entirely made up of cartilage, and cartilage cell sources vary with body location. For example, cartilage of the head is formed from the neural crest. Cartilage of the neck and trunk forms as part of the axial skeleton from the sclerotome of paraxial mesoderm, while cartilage of the tail skeleton originates from tail bud mesenchyme. Limb cartilage originates with the appendicular skeleton from lateral plate mesoderm. In the earliest stages of chondrogenesis , mesenchymal cells aggregate and condense in response to signaling molecules such as transforming growth factor-β (TGFβ) , sonic hedgehog (SHH) , and bone morphogenetic protein (BMP) . Upon commitment to chondrogenesis , cells express the transcription factor Sox-9 , which drives expression of cartilage-specific genes, including the matrix proteins Col2 and aggrecan . In vertebrates that undergo skeletal ossification , the cartilaginous skeleton acts as a template for the eventual replacement with bone, a process known as endochondral ossification . Chondrocytes cease proliferating and undergo hypertrophy . This critical milestone in the process of endochondral ossification is typified by characteristic changes in chondrocyte morphology , including dramatic increases in cell volume, and a defined gene expression profile. Hypertrophic chondrocytes begin secreting a unique matrix consisting of collagen type X and alkaline phosphatase , which initiates matrix calcification [4–6]. The hypertrophic chondrocytes also begin secreting the protease , matrix metalloproteinase-13 (MMP-13) [7–10], that breaks down cartilage matrix, and growth factors such as vascular endothelial growth factor (VEGF) [11], which induces blood vessels to sprout from the surrounding tissues. The hypertrophic chondrocytes then undergo apoptosis and are replaced by mesenchymal cells and pre-osteoblasts brought into the cartilage template via invading capillaries [12–15]. The remnant cartilage matrix is further cleared by invading osteoclasts and replaced with bone matrix as mesenchymal cells differentiate into osteoblasts . Endochondral ossification concludes when the cartilage template is replaced by bone. Not all embryonic cartilage is replaced by bone, however, and the permanent cartilage that persists following embryonic development make up the fibrocartilage , elastic cartilage , and hyaline cartilage of the adult organism.
Interestingly, many of the same milestones observed in embryonic cartilage and skeletal development are also seen in adult vertebrate fracture healing [16]. Furthermore, the primary morphogenetic pathways that are active during embryonic skeletal development are also expressed in fracture calluses , and a comparison of the transcriptomes has revealed that genes that control appendicular limb development also show increased expression during fracture healing [17]. Fracture healing begins with an initial anabolic phase characterized by an increase in tissue volume related to the de novo recruitment and differentiation of stem cells that form skeletal and vascular tissues. The tissue between broken bones at the fracture site swells as hematomas form. The adjacent periostium also swells, and periosteal stem/progenitor cells proliferate into the fracture. These cells undergo chondrogenesis , forming the cartilage callus. Concurrent with cartilage tissue development, cells that will form the nascent blood vessels that supply the new bone are recruited and differentiate in the surrounding muscle sheath. As chondrocyte differentiation progresses through hypertrophy , the cartilage extracellular matrix undergoes mineralization and the anabolic phase of fracture repair terminates with chondrocyte apoptosis . Just as in endochondral ossification , blood vessels invade in response to VEGF signals, bringing pre-osteoblasts that replace cartilage tissue with bone. The anabolic phase is followed by a prolonged phase in which catabolic activities predominate as the callus is resorbed and remodeled to the bone’s original cortical structure . The recapitulation of these ontological processes is believed to make fracture healing one of the few postnatal processes that is truly regenerative, restoring the damaged skeletal organ to its pre-injury cellular composition, structure and biomechanical function [16]. As discussed in the following section, certain non-mammalian organisms are capable of even more impressive feats of regeneration .
4.3 Cartilage Regeneration During Limb/Tail Regeneration
Several remarkable organisms are able to regenerate amputated limbs and/or tails. In doing so, the tissues of the lost appendage are replaced, including cartilage. In fact, cartilage is the default skeletal tissue for appendage regeneration, and, in these special cases, the regenerated cartilage does not ossify for the lifetime of the regenerate. These feats of regeneration are achieved through processes that meld embryonic development with adult wound healing, and what we learn from them may offer clues for improving mammalian regeneration.
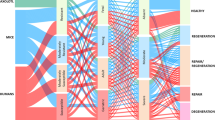
Urodeles (salamanders and newts) and Xenopus frogs are able to regenerate limbs as adults (Table 4.1). While urodeles are able to regenerate both front and back limbs , frogs are able to regenerate front limbs only. Urodeles retain non-ossified, cartilaginous skeletons into adulthood and are able to regenerate fully formed limbs (Fig. 4.1a), with all the cartilaginous skeletal elements of the originals (Fig. 4.1c). Regenerated urodele limbs also recreate the musculature of the amputated arms/legs. Frogs, which do fully develop and exhibit ossified skeleton as adults, regenerate cartilage spikes rather than limbs following amputation (Fig. 4.1b). Cartilage spikes are continuous with the radio-ulna bone of the original limb, and no other skeletal elements are formed, and very little muscle is regenerated (Fig. 4.1d). These differences between urodele and frog limb regeneration are remarkable given that both processes begin very similarly. Following limb loss in both animal groups, limb stump tissues contract and wound epidermis forms to seal the stump. Stump tissues are broken down by secreted proteases, releasing cells into the stump. These cells migrate and proliferate, forming the blastema , the classic indicator of regeneration, and blastema cells reform the majority of tissues of the replacement limb. In frogs , regenerated spike cartilage does not originate from blastema cells. Instead, cartilage spikes originate from severed bones of amputated limbs and are formed similar to cartilage calluses during fracture repair [18]. How this callus-like accumulation of cartilage extends into the spikes of regenerated frog limbs is not known currently, but may provide clues for healing bone fracture gaps that exceed critical size defect lengths. In urodeles, regenerated limb cartilage does originate from blastema cells (Fig. 4.2) [19]. Interestingly, the blastema cells that differentiate into cartilage are derived from both the dermis and cartilage of the original limb stump, but not from muscle. This restriction in differentiation stems from the fact that the urodele limb blastema is a heterogeneous collection of restricted progenitor cells that do not cross developmental origins as they reform lost tissues. For example, both dermis and skeletal tissues originate from the lateral plate mesoderm , and blastema cells originating from either of these tissues are able to differentiate into cartilage, but not muscle, which originates from presomitic mesoderm . Similarly, limb blastema cells derived from muscle do not differentiate into dermis or cartilage.
Examples of limb and tail regeneration in amphibians and lizards . (a, b) Morphological comparison of (a) salamander (Ambystoma mexicanum) and (b) frog (Xenopus laevis) forelimbs before (left) and 8 weeks after (right) amputation. Salamanders regenerate new limbs, while frogs regenerate cartilage spikes. (c, d) Histological analysis (pentachrome) of regenerated (c) salamander and (d) frog limbs. Salamanders regenerate all the skeletal elements of the upper arm and hand,Fig. 4.1 (continued) while frogs regenerate a single cartilage spike. (e, f) Histological (pentachrome) and (e, f Insets) morphological analysis of (e) salamander tail 5-weeks post amputation and (f) lizard (Anolis carolinensis) tail 2 weeks post-amputation. (g) Salamander (top) and lizard (bottom) tails 10 weeks after amputation analyzed by micro-computed tomography. Pentachrome stains cartilage green, bone orange, muscle red, and spinal cord and epidermis purple. Dashed lines denote amputation planes. c carpal, cr cartilage rod, cs cartilage spike, ct cartilage tube, h humerus, m muscle, mc metacarpal, nc notochord, p phalanges, r radius, rm regenerated muscle, rsc regenerated spinal cord, ru radio-ulna, sc spinal cord, u ulna, ve vertebra. Bar = 1 mm. Figure adapted from [31]
Summary of blastema cell differentiation restrictions during salamander limb and tail regeneration. Figure adapted from [19]
The inverse relationship between complexity and regeneration fidelity and the preference for producing cartilage noted for limb regeneration are also observed in tail regeneration. Urodeles and lizards regenerate tails (Table 4.1) [24–26, 32], and both regenerated tail skeletons are almost completely cartilaginous (Fig. 4.1e, f). Salamanders regenerate cartilage rods (CR) ventral to regenerated spinal cords (Fig. 4.1e), while lizards regenerate cartilage tubes (CT) that enclose regenerated spinal cords (Fig. 4.1f). However, regenerated tails of the comparatively primitive salamander segment and develop neural and hemal arches, and mature regenerated salamander tails are almost perfect copies of originals (Fig. 4.1g). The more complex lizards , on the other hand, regrow imperfect regenerated tails, and lizard cartilage tubes never segment and are easily distinguishable from original tail skeletons (Fig. 4.1g). Also unlike salamander cartilage regeneration, a portion of the regenerated lizard cartilage ossifies [24]. The most proximal region of the CT in contact with the original tail skeleton undergoes endochondral ossification in a process similar to what is observed during fracture healing. Proximal CT chondrocytes undergo hypertrophy and are replaced by bone. This proximal ossification event is not observed in the urodele CR, and may reflect the differences in ossification states between adult urodele and lizard skeletons. Interestingly, the perichondrium of the distal lizard CT calcifies without undergoing ossification, while the CT interior remains cartilaginous for the lifetime of the regenerate. Like bone periosteum, the lizard CT perichondrium harbors a stem/progenitor cell population that forms additional cartilage in response to stimulation with TGFβ [24]. Like urodele regenerated cartilage , cartilage formed from lizard CT perichondrium cells does not undergo hypertrophy and endochondral ossification. These observations also indicate a link between original and regenerated cartilage ossification: cartilage formed by cells derived from ossified tissues undergo hypertrophy and ossification, while cartilage derived from cartilaginous tissue elements do not. This topic becomes important during discussion of cell therapies for cartilage healing in humans, which are plagued by unwanted cartilage hypertrophy and ossification.
Tail regeneration also provides an interesting contrast to limb regeneration in terms of cell identity. As with limb regeneration, urodele and lizard tail generation begins with blastemas . Unlike limb blastema cells, whose differentiation is lineage restricted by developmental origin (i.e., mesoderm vs ectoderm) [19], tail blastema cells are able to transition between developmental lineages during differentiation (Fig. 4.2). For example, regenerated tail cartilage is formed from blastema cells that have originated from muscle [20], dermis, or even spinal cord (ependyma) [21]. In fact, tail skeletal tissue contributes only minimally to regenerating tail blastemas and, hence, regenerated cartilage. The reasons for these differences between limb and tail blastema origins are not currently understood, but they may reflect differences involving both development and healing in the appendicular versus axial skeletons .
In summary, appendage regeneration is depended on the formation of wound epithelia and blastemas or blastema-like structures. This encapsulation of proliferating cells by un-differentiated, embryonic-like epithelial tissue provides the necessary environment for tissue differentiation and extension and avoids scar formation. While lizards , urodeles , and frogs provide perhaps the best examples of these structures and the regenerative process, certain mammals are also capable of approximating these healing responses .
4.4 Cartilage Healing and Regeneration in Non-Human Mammals
As a group, mammals exhibit much reduced regenerative abilities compared to amphibians and lizards . For example, no mammal is capable of limb or tail regeneration as adults. While some rodent species, such as African spiny mice (Acomys) and South American spiny rats ( Proechimys) shed tails as strategies for escaping predators (caudal autotomy), lost tails are not regenerated [33, 34]. Perhaps the most impressive naturally-occurring examples of adult regeneration among mammals are observed in species capable of skin autotomy. For example, the skin of Acomys mice is mechanically weak and easily tears and sloughs off [28]. This makes Acomys mice difficult for predators to grab and hold onto, allowing the mice to escape, but often results in large open wounds and skin loss. Acomys mice, but not house mice (Mus), are able to heal these types of skin wounds quickly and without scarring [28]. In the lab, Acomys mice are capable of healing ear hole punches, including auricular cartilage (Table 4.1) [28]. Interestingly, these types of mice appear to generate blastema -like structures during healing, as evidenced by wound epidermis that bears striking similarities to those formed during appendage regeneration in urodeles and lizards . Whether the Acomys blastema follows the same rules in cell fate and differentiation remains to be determined.
While Acomys mice and Proechimys rats may represent the best examples of “natural” cartilage regeneration among mammals, certain mouse strains exhibit enhanced regenerative abilities following selective breeding over many generations. The so-called “super healing ” mouse strains are able to heal a number of tissues better than wild type mice . Collectively known as the Murphy Roths Large (MRL) mice, this groups includes the MRL/MpJ, Murphy Roths Large/lymphoproliferative (lpr) mouse strain (MRL/MpJ-Fas lpr/J) MRL/MpJ-Fas lpr/J, and Large strains [35]. Like Acomys mice, MRL mice are able to heal ear hole punches and regenerate auricular cartilage (Table 4.1) [30]. In addition, MRL mice form a type of wound epidermis faster than other strains, and appear to form blastema -like accumulations of mesenchymal cells in response to certain types of injuries. It is interesting that neither Acomys mice nor MRL strains are able to regenerate limbs, tails, or digit tips as adults [36].
While direct comparisons between Acomys mice and MRL strains have yet to be made, based on their similar abilities to form blastema-like structures and heal hole punch injuries it is possible that similar healing mechanisms are at work in both animals. Unfortunately, the exact underlying mechanisms responsible for the enhanced healing abilities of MRL mice have proven difficult to specify. The “super healer ” phenotype appears to depend most heavily on the inclusion of the Large strain identity, which includes autoimmune anomalies in addition to enhanced healing. For example, the MRL/MpJ-Fas lpr/J strain was established through selective interbreeding of the B6 (0.3 %), C3H (12.1 %), AKR (12.6 %), and Large (75 %) strains [35]. These mice are prone to autoimmune disorders, and these phenotypes were attributed to a mutant Fas gene , which arose spontaneously at generation F12 during selective breeding. However, the link between mutant Fas and healing is confounded by the fact that the MRL /MpJ mice , which have the wild type Fas gene and were maintained as a control strain for the MRL /MpJ-Fas lpr/J mice, also exhibit enhanced healing. Still, since all 3 MRL mouse strains exhibit autoimmune phenotypes, it is natural to suppose a link between regenerative ability and immunity dysfunction. However, a multi-strain wound healing survey offers evidence that they are not genetically linked. It should be noted, however, that mutations in the cell cycle checkpoint gene p21 cause yet another autoimmune disorder similar to lupus, but also enhanced healing phenotypes [37]. Obviously, additional research is needed to work out the mechanisms behind the “super healing ” phenotypes (see comprehensive review by Heydeman [35]).
4.5 Intrinsic Articular Cartilage Repair
While cartilage regeneration activities in response to appendage amputation and ear hole punch injuries are informative in assessing the healing limits of non-human animals, they are admittedly not readily relatable to human cartilage injuries, which predominantly affect the articular cartilage of limb joints. As previously mentioned, highly specialized hyaline cartilage lines the articular surfaces of long bones. Articular cartilage itself is divided into four zones based on chondrocyte morphology, matrix composition and distribution: (1) superficial zone (tangential layer), consisting of two to three layers of small, flattened chondrocytes arranged parallel to the surface; (2) middle or transitional zone, where the chondrocytes are spherical; (3) deep or radial zone, consisting of large chondrocytes that form columns perpendicular to the surface; and (4) calcified zone, where hypertrophic chondrocytes are embedded in the calcified matrix, which is connected to the subchondral bone (Fig. 4.3). Differences in the ECM are seen within the hierarchical structure of articular cartilage. In the surface zone, chondrocytes produce proteoglycans that reduce friction (i.e., lubricin), protect chondrocytes and cartilage surfaces, and inhibit synovial cell overgrowth [39, 40]. In the middle zone, the ECM includes Col2 , aggrecan , and other proteins. Collagen type X and alkaline phosphatase are found in the deep zone and calcified zone, indicating chondrocyte hypotrophy and the calcified matrix environment (Fig. 4.3). Collagen fibrils are oriented mostly parallel to the surface in the superficial zone , obliquely in the middle zone, and perpendicular to the joint surface in the deep zone, which is suited to load transmission (Fig. 4.3) [38].
Schematic view of normal articular cartilage highlighting (a) cell distribution, (b) matrix distribution, and (c) collagen fibril orientation. Figure modified from [38]
In terms of tissue repair ability , cartilage injury is classified on the basis of the depth of defect (Fig. 4.4), and tissue remodeling response differs depending on the type and size of the defect. Partial cartilage defects are limited to the superficial-to-middle zones and do not involve damage to subchondral bone. Full thickness cartilage defects penetrate down to the bone, and are in fact more prone to heal than partial thickness defects if the osteochondral junction is also damaged. In these cases, where full thickness defects penetrate into the bone marrow, bone marrow stromal cells (BMSCs) flow into the lesion site to form a stem-cell rich fibrin clot and stimulate intrinsic repair. While humans are unable to heal both partial and full thickness defects, some of the species discussed above do manage at least some level of articular cartilage healing. MRL mice are able to heal full thickness defects up to 0.5 mm2 in depth, and the regenerated cartilage is robust hyaline cartilage (Table 4.1) [29]. However, even the “super healing ” mouse strains are unable to heal partial thickness defects (Table 4.1). Articular cartilage healing has yet to be studied in Acomys mice and p21 knock-out mice, and such experiments would provide interesting context for the results involving MRL mice. Among non-mammalian animals, lizards are able to regenerate entire articular cartilage surfaces (Table 4.1) [27], but new cartilage tissue appears to undergo hypertrophy and is probably more similar to a fracture cartilage callus than true regenerated articular cartilage [41]. It is currently not known if lizards or other reptiles can heal partial or full thickness cartilage defects. Salamanders can regenerate full thickness cartilage defects that cover approximately 50 % of the joint [23], but it is not yet known if urodeles can regenerate partial thickness defects (Table 4.1). In any case, these experiments not only provide evidence that healing large articular cartilage defects is possible, but they also provide hope that articular cartilage healing may be achieved by humans with the correct therapies .
4.6 Cell-Based Therapies for Human Articular Cartilage Repair
Unlike the cartilage of the special species discussed above, adult human cartilage has limited self-repair ability, and damage to articular cartilage leads directly to the pathogenesis of osteoarthritis (OA) . For example, progressive loss of articular cartilage leads to an increase in subchondral bone formation , as well as new bone formation at joint margins (osteophytes). Unfortunately for the patient, these tissue changes underlie clinical symptoms including joint pain and limited joint movement. Overall, these pathologies manifest as degenerative joint diseases, such as OA, which severely affect the quality of life [42]. OA is one of the most common causes of mobility loss and represents the most prevalent form of musculoskeletal disease worldwide [43, 44]. For example, OA affects 27 million Americans, about 60 % of men and 70 % of women above 65 years of age [45, 46], and directly contributes to disabilities in 9–10 % of the U.S. population [47].
As mentioned above, humans do not spontaneously heal partial or full thickness cartilage defects , OA progresses until the entire affected joint needs to be either fused or replaced. However, there is evidence of incomplete healing in small and deep defects. Osteochondral defects do exhibit limited reparative capacity, and, in clinical practice, this intrinsic reparative property is exploited in the microfracture technique, which involves surgical drilling to the subchondral bone region to treat small size cartilage defects (usually 0.5–2 cm2) [2]. However, the cartilage formed in response to subchondral microfracture consists mainly of fibrocartilage rather than the original hyaline cartilage, and the therapeutic benefits generally last only 2–5 years [48–50]. For larger defects that require more extensive healing, tissue transplantation such as osteochondral auto/allograft (mosaicplasty) has been used; however, tissue source and compatibility present potential complications. Most of the current approaches to treat articular cartilage injuries, therefore, have focused on stimulating intrinsic regeneration and/or replacing diseased or lost tissue. These therapeutic approaches are collectively known as tissue engineering and regenerative medicine , an area that has been developing rapidly since the 1970s. Termed the “next evolution of medical treatments” by the U.S. Department of Health and Human Services , regenerative medicine aims to replace or regenerate human cells , tissues and organs to restore or establish normal function [51]. The basic principle involves the application of cells, biomaterial scaffolds, and signaling molecules to promote endogenous regenerative capacity and/or the replacement of whole tissues with engineered constructs in vitro [52]. Regenerative medicine approaches for healing articular cartilage injuries offer promise for preventing OA .
4.6.1 Autologous Chondrocyte -Based Therapies for Cartilage Defects
The concept of autologous implantations to treat cartilage defects began with studies by O’Driscoll and co-workers, who used periosteal grafting to treat rabbit chondral defects [53]. Further refinement by Grande and Peterson included the use of cultured autologous chondrocytes [54, 55]. Autologous Chondrocyte Implantation/Transplantation (ACI/ACT) was first applied clinically to treat full-thickness chondral defects in knees by Brittberg et al. [56]. Briefly, small amounts of healthy cartilage were harvested from non-load bearing areas under arthroscopy , and the isolated chondrocytes were expanded in vitro for up to 6 weeks . The cultured cells were then injected into the cartilage defect and sealed with a sutured periosteal flap taken from the proximal medial tibia (Fig. 4.5). The overall 0–5 year therapeutic efficacy was generally 70–90 %, as evidenced by relief of symptoms and improvement of joint function [57]. In a 10–20 year (mean 12.8 year) follow-up study, 74 % of the 224 patients that underwent ACI treatment reported their status as good or better than before surgery [58]. ACI/ACT have also been reported to be effective in treating larger cartilage defects [59], with therapeutic benefits lasting longer than those of microfracture marrow-stimulation techniques [60]. Therefore, ACI provides the possibility of regenerating cartilage tissues and restoring normal joint function, criteria which meet the basic clinical definition for functional cartilage repair .
To eliminate the need for secondary surgery sites and to reduce the complexity of the ACI/ACT procedure, biomaterials have been adopted in the next generations of ACI/ACT. Standard procedure of ACI/ACT involves surgical preparation of the defect(s), periosteal harvesting, suturing of periosteum over defect(s), application of fibrin glue sealant, and implantation of chondrocytes with the risks of possible cell leakage from the application sites as well as uneven cell distributions. Furthermore, the harvesting of periosteum increases the operation time and requires a larger surgical exposure field [61]. To address these shortcomings, “second generation” ACI uses biomaterials (e.g., collagen type I/type III membranes) instead of periosteum grafts, thereby reducing open injury sites and shortening operation time. More recently, third generation, or “all in one” grafts, have been developed that make use of combinations of cells and biomaterials, which are delivered directly to defects without either periosteal covers or suture fixation. This technique is referred to as matrix-associated autologous chondrocyte implantation (MACI) . Currently, the most commonly used biomaterials in MACI involve natural ECM materials such as collagen and hyaluronan [62], and there is active, ongoing research to develop more optimal biomaterials [62, 63].
4.6.2 Stem Cell-Based Therapies for Cartilage Regeneration
Despite the promise of ACI and MACI , limitations remain, and current research is aimed at improving therapeutic effectiveness and availability. For example, ACI and MACI are limited by the availability of harvested cell number and quality. In clinical application, chondrocytes directly derived from healthy hyaline cartilage are considered the most appropriate for transplantation [64]. Unfortunately, the numbers of chondrocytes suitable for harvest are very limited. For example, patients in need of ACI often have experienced extensive cartilage degeneration and loss ; in addition, chondrocytes exhibit only limited life span as differentiated cells during culture expansion before cell quality irreversibly suffers. To address the shortage of suitable cell populations, stem cells that may serve as chondroprogenitors are under investigation as new candidate cell sources to replace native chondrocytes for cartilage repair .
Mesenchymal stem cells (MSCs) are the most promising therapeutic cells for cartilage regeneration research, owing to their self-renewal ability, chondrogenic potential, and anti-inflammatory activity [65]. Clinical application of bone marrow-derived MSCs has been reported by several groups [66–68], and a 2 year follow up cohort study showed comparable efficacy of MSCs and native chondrocytes for use in ACI [69]. However, longer term studies are already needed. One of the most important and interesting aspects of using MSCs in ACI is the dependency of MSC chondrogenic potential on cell source since, ultimately, the clinical outcome depends on the ability of the stem cells to form cartilage. A summary of studies evaluating the use of MSCs from various tissue sources in treating ACI in animal studies is presented in Table 4.2. This comparison indicates that bone marrow-derived MSCs produce more hyaline-like cartilage matrix and promote higher functional recovery than MSCs isolated from periosteum, synovium, adipose tissue, and muscle [70], which tend to undergo fibrocartilage differentiation [70, 95]. MSCs isolated from tissues other than bone marrow do offer certain advantages, however. For example, adipose-derived MSCs are easy to obtain, and adipose tissue contains 100-times greater numbers of stem cells per volume than bone marrow aspirates [96]. Unfortunately the chondrogenic potential of adipose-derived MSCs is lower compared to bone marrow MSCs [97], suggesting that more research needs to be done to improve the chondrogenic differentiation of these cells .
Furthermore, given their expanded levels of differentiation potencies, both embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) have the potential for chondrogenesis [94, 98] with the additional options of founding patient-specific cell lines with high self-renewal potential, these cells may be the ideal candidates for cartilage regenerative medicine. Indeed, animal studies have already been conducted [91–93, 99] (Table 4.2). However, several complications have yet to be overcome. For example, not all of the transplanted cells contribute to hyaline cartilage regeneration [93], and not all cell lines differentiate into the target tissue safely [99]. Thus, before ESC and iPSC cells are used in a clinical setting, the topics of differentiation efficiency and tumor formation must be solved.
4.6.3 Future Studies to Enhance Stem Cell-Based Cartilage Regeneration
Both the ACI and MACI techniques for cartilage repair are well-established examples of tissue engineering/regenerative medicine and represent the current best solutions for cartilage injury. However, neither ACI nor MACI can completely regenerate hyaline cartilage for large defects, and there is significant need for further improvements. An important area of current research involves the optimization of differentiation signals and environments for producing robust hyaline cartilage. Clues from embryonic cartilage developmental processes, as well as from cartilage regeneration in non-human animals , could shed light on such studies.
For example, to improve stem cell differentiation efficacy and maintain chondrocyte phenotype, signaling factors such as TGF-βs are required. However, a growing amount of evidence has indicated that treatment with single signaling factors is insufficient for initiating maximal stem cell chondrogenesis and phenotype maintenance. Thus, knowledge gained on embryonic skeletal system development/nonhuman cartilage regeneration should be used a guide.
Embryonic chondrogenesis begins with mesenchymal cell recruitment, proliferation and condensation. Cell condensations are initiated by several growth factors, including TGF-β , FGF, Wnt, and BMPs, acting in concert [3, 100, 101]. Afterwards, several matrix molecules, including fibronectin , hyaluronan and collagens , interact with the cell surface receptors to initiate the transition from chondroprogenitor to chondrocytes [100, 102, 103] and regulation of the chondrogenesis-specific transcription factor Sox-9 [104]. In an example of recreating multi-step differentiation schemes in vitro, ESCs/iPSCs were treated with two-step differentiation strategies . First, ESCs/iPSCs were differentiated into multipotent states (ESC-MSC or iPSC-MSC), which were then differentiated towards the chondrogenic linage [105]. These strategies offer promise for creating significant amounts of healthy cartilage, but additional work is required to fine-tune the differentiation signals. For human MSCs , TGFβ2 and TGFβ3 were shown to be more active than TGFβ1 in promoting chondrogenesis [106]. Interestingly, the effect of TGFβ3 stimulation is enhanced if the growth factor is applied during the initial phase of the culture period and then withdrawn [107, 108]. Adding to the complexity, the effects of growth factor treatments varies with MSC tissue source. For example, BMP6 in addition to TGFβs is required by adipose-derived stem cells for efficient stimulation of chondrogenesis [109, 110]. Again broadening our discussion to non-human animals, TGFβs and Indian hedgehog (Ihh) regulate cartilage formation and maturation during lizard tail regeneration [24]. TGFβ1 and TGFβ3 induce cartilage formation in lizard CT perichondral cells , which express the MSC markers CD90 and CD66, and the CT perichondrium calcifies in response to Ihh. Inhibiting hedgehog signaling in the regenerating lizard tail suppresses cartilage maturation, which may provide clues for preventing similar maturation in cartilage derived from progenitor cells in other species, including human MSCs . Indeed, considering the complex mixture of factors involved in embryonic skeletogenesis and appendage regeneration in vivo, we may surmise that a similarly complex, multifactorial biochemical environment will be required for effective long-term cartilage engineering .
4.7 Conclusion
Cartilage is a tissue that most animals, including humans, are unable to repair. In this chapter we have summarized the cartilage healing abilities of the few species which are able to regenerate cartilage. We have also described the current approaches in therapeutic enhancement of cartilage repair in humans. It is noteworthy that cartilage therapies may be adapted to mimic the pattern and sequence of biological events seen in naturally regenerative tissues. For example, the use of autologous stem cells to augment the resident progenitor cell population represents a strategy that echoes the role of the blastema in appendage regeneration. As future research works out the intricacies of cell differentiation and signaling, similar advancements will help in closing gaps in wound healing capabilities .
Abbreviations
- ACI/ACT:
-
Autologous chondrocyte implantation/transplantation
- BMSC:
-
Bone marrow stromal cell
- BMP:
-
Bone morphogenetic protein
- Col:
-
Collagen type
- CR:
-
Cartilage rod
- CT:
-
Cartilage tube
- ECM:
-
Extracellular matrix
- ESC:
-
Embryonic stem cells
- FGF:
-
Fibroblast growth factor
- GAG:
-
Glycosaminoglycan
- IHH:
-
Indian hedgehog
- iPSC:
-
Induced pluripotent stem cell
- OA:
-
Osteoarthritis
- PG:
-
Proteoglycan
- lpr:
-
Lymphoproliferative
- MACI/MACT:
-
Matrix-associated autologous chondrocyte implantation/transplantation
- MMP:
-
Matrix metalloproteinase
- MSC:
-
Mesenchymal stem cell
- MRL:
-
Murphy Roths Large
- SHH:
-
Sonic hedgehog
- Sox:
-
Sry-related high-mobility-group box
- TGF:
-
Transforming growth factor
- VEGF:
-
Vascular endothelial growth factor
References
Gentili C, Cancedda R (2009) Cartilage and bone extracellular matrix. Curr Pharm Des 15:1334–1348
Williams RJ (2007) Cartilage repair strategies. Humana Press, Totowa
DeLise AM, Fischer L, Tuan RS (2000) Cellular interactions and signaling in cartilage development. Osteoarthr Cartil 8:309–334
Anderson HC, Sipe JB, Hessle L, Dhanyamraju R, Atti E, Camacho NP, Millan JL (2004) Impaired calcification around matrix vesicles of growth plate and bone in alkaline phosphatase-deficient mice. Am J Pathol 164:841–847
Fedde KN, Blair L, Silverstein J, Coburn SP, Ryan LM, Weinstein RS, Waymire K, Narisawa S, Millan JL, MacGregor GR, Whyte MP (1999) Alkaline phosphatase knock-out mice recapitulate the metabolic and skeletal defects of infantile hypophosphatasia. J Bone Miner Res 14:2015–2026
van der Eerden BC, Karperien M, Wit JM (2003) Systemic and local regulation of the growth plate. Endocr Rev 24:782–801
Tchetina EV, Kobayashi M, Yasuda T, Meijers T, Pidoux I, Poole AR (2007) Chondrocyte hypertrophy can be induced by a cryptic sequence of type II collagen and is accompanied by the induction of MMP-13 and collagenase activity: implications for development and arthritis. Matrix Biol 26:247–258
Cawston TE, Wilson AJ (2006) Understanding the role of tissue degrading enzymes and their inhibitors in development and disease. Best Pract Res Clin Rheumatol 20:983–1002
Inada M, Wang Y, Byrne MH, Rahman MU, Miyaura C, Lopez-Otin C, Krane SM (2004) Critical roles for collagenase-3 (Mmp13) in development of growth plate cartilage and in endochondral ossification. Proc Natl Acad Sci U S A 101:17192–17197
Stickens D, Behonick DJ, Ortega N, Heyer B, Hartenstein B, Yu Y, Fosang AJ, Schorpp-Kistner M, Angel P, Werb Z (2004) Altered endochondral bone development in matrix metalloproteinase 13-deficient mice. Development 131:5883–5895
Zelzer E, Glotzer DJ, Hartmann C, Thomas D, Fukai N, Soker S, Olsen BR (2001) Tissue specific regulation of VEGF expression during bone development requires Cbfa1/Runx2. Mech Dev 106:97–106
Mackie EJ, Ahmed YA, Tatarczuch L, Chen KS, Mirams M (2008) Endochondral ossification: how cartilage is converted into bone in the developing skeleton. Int J Biochem Cell Biol 40:46–62
Song F, Li B, Stocum DL (2010) Amphibians as research models for regenerative medicine. Organogenesis 6:141–150
Glowacki J (1998) Angiogenesis in fracture repair. Clin Orthop Relat Res 355:S82–S89
Young HE, Bailey CF, Dalley BK (1983) Gross morphological analysis of limb regeneration in postmetamorphic adult Ambystoma. Anat Rec 206:295–306
Einhorn TA, Gerstenfeld LC (2015) Fracture healing: mechanisms and interventions. Nat Rev Rheumatol 11:45–54
Bais M, McLean J, Sebastiani P, Young M, Wigner N, Smith T, Kotton DN, Einhorn TA, Gerstenfeld LC (2009) Transcriptional analysis of fracture healing and the induction of embryonic stem cell-related genes. PLoS One 4, e5393
Mitogawa K, Makanae A, Satoh A, Satoh A (2015) Comparative analysis of cartilage marker gene expression patterns during axolotl and Xenopus limb regeneration. PLoS One 10, e0133375
Kragl M, Knapp D, Nacu E, Khattak S, Maden M, Epperlein HH, Tanaka EM (2009) Cells keep a memory of their tissue origin during axolotl limb regeneration. Nature 460:60–69
Echeverri K, Clarke JDW, Tanaka EM (2001) In vivo imaging indicates muscle fiber dedifferentiation is a major contributor to the regenerating tail blastema. Dev Biol 236:151–164
Echeverri K, Tanaka EM (2002) Ectoderm to mesoderm lineage switching during axolotl tail regeneration. Science 298:1993–1996
Schnapp E, Kragl M, Rubin L, Tanaka EM (2005) Hedgehog signaling controls dorsoventral patterning, blastema cell proliferation and cartilage induction during axolotl tail regeneration. Development 132:3243–3253
Cosden RS, Lattermann C, Romine S, Gao J, Voss SR, MacLeod JN (2011) Intrinsic repair of full-thickness articular cartilage defects in the axolotl salamander. Osteoarthr Cart 19:200–205
Lozito TP, Tuan RS (2015) Lizard tail regeneration: regulation of two distinct cartilage regions by Indian hedgehog. Dev Biol 399:249–262
Fisher RE, Geiger LA, Stroik LK, Hutchins ED, George RM, Denardo DF, Kusumi K, Rawls JA, Wilson-Rawls J (2012) A histological comparison of the original and regenerated tail in the green anole, Anolis carolinensis. Anat Rec 295:1609–1619
Hutchins ED, Markov GJ, Eckalbar WL, George RM, King JM, Tokuyama MA, Geiger LA, Emmert N, Ammar MJ, Allen AN, Siniard AL, Corneveaux JJ, Fisher RE, Wade J, DeNardo DF, Rawls JA, Huentelman MJ, Wilson-Rawls J, Kusumi K (2014) Transcriptomic analysis of tail regeneration in the lizard Anolis carolinensis reveals activation of conserved vertebrate developmental and repair mechanisms. PLoS One 9, e105004
Alibardi L (2015) Regeneration of articular cartilage in lizard knee from resident stem/progenitor cells. Int J Mol Sci 16:20731–20747
Seifert AW, Kiama SG, Seifert MG, Goheen JR, Palmer TM, Maden M (2012) Skin shedding and tissue regeneration in African spiny mice (Acomys). Nature 489:561–565
Fitzgerald J, Rich C, Burkhardt D, Allen J, Herzka AS, Little CB (2008) Evidence for articular cartilage regeneration in MRL/MpJ mice. Osteoarthr Cart 16:1319–1326
Clark LD, Clark RK, Heber-Katz E (1998) A new murine model for mammalian wound repair and regeneration. Clin Immunol Immunopathol 88:35–45
Lozito TP, Tuan RS (2016) Lizard tail regeneration as an instructive model of enhanced healing capabilities in an adult amniote. Connect Tissue Res 1–10
Angus d’A Bellairs SVB, Darevsky IS, Hubert J, Kupriyanova LA, Pieau C, Raynaud A, Saint Girons H, Shine R, Uzzell T, Yaron Z (1985) The biology of the Reptilia. Wiley, New York
Shargal E, Rath-Wolfson L, Kronfeld N, Dayan T (1999) Ecological and histological aspects of tail loss in spiny mice (Rodentia: Muridae, Acomys) with a review of its occurrence in rodents. J Zool 249:187–193
Dubost G, Gasc JP (1987) The process of total tail autotomy in the South-American rodent, Proechimys. J Zool 212:563–572
Heydemann A (2012) The super super-healing MRL mouse strain. Front Biol 7:522–538
Gourevitch DL, Clark L, Bedelbaeva K, Leferovich J, Heber-Katz E (2009) Dynamic changes after murine digit amputation: the MRL mouse digit shows waves of tissue remodeling, growth, and apoptosis. Wound Repair Regen 17:447–455
Bedelbaeva K, Snyder A, Gourevitch D, Clark L, Zhang XM, Leferovich J, Cheverud JM, Lieberman P, Heber-Katz E (2010) Lack of p21 expression links cell cycle control and appendage regeneration in mice. Proc Natl Acad Sci U S A 107:5845–5850
Johnson DH, Pedowitz RA (2007) Practical orthopaedic sports medicine and arthroscopy [electronic resource]. Wolters Kluwer Health/Lippincott Williams & Wilkins, Philadelphia
Rhee DK, Marcelino J, Baker M, Gong Y, Smits P, Lefebvre V, Jay GD, Stewart M, Wang H, Warman ML, Carpten JD (2005) The secreted glycoprotein lubricin protects cartilage surfaces and inhibits synovial cell overgrowth. J Clin Invest 115:622–631
Waller KA, Zhang LX, Elsaid KA, Fleming BC, Warman ML, Jay GD (2013) Role of lubricin and boundary lubrication in the prevention of chondrocyte apoptosis. Proc Natl Acad Sci U S A 110:5852–5857
Pritchard JJ, Ruzicka AJ (1950) Comparison of fracture repair in the frog, lizard and rat. J Anat 84:236–261
Callaghan JJ (2003) The adult knee, vol 1. Lippincott Williams & Wilkins, Philadelphia, PA
Brooks P (2003) Inflammation as an important feature of osteoarthritis. Bull World Health Organ 81:689–690
World Health Organization (2002) The world health report 2002: reducing risks, promoting healthy life. World Health Organization, Geneva
Goldring MB (2006) Update on the biology of the chondrocyte and new approaches to treating cartilage diseases. Best Pract Res Clin Rheumatol 20:1003–1025
Lethbridge-Cejku M, Helmick CG, Popovic JR (2003) Hospitalizations for arthritis and other rheumatic conditions: data from the 1997 National Hospital Discharge Survey. Med Care 41:1367–1373
Felson DT (2004) An update on the pathogenesis and epidemiology of osteoarthritis. Radiol Clin North Am 42:1–9
Knutsen G, Drogset JO, Engebretsen L, Grontvedt T, Isaksen V, Ludvigsen TC, Roberts S, Solheim E, Strand T, Johansen O (2007) A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am 89:2105–2112
Saris DB, Vanlauwe J, Victor J, Haspl M, Bohnsack M, Fortems Y, Vandekerckhove B, Almqvist KF, Claes T, Handelberg F, Lagae K, van der Bauwhede J, Vandenneucker H, Yang KG, Jelic M, Verdonk R, Veulemans N, Bellemans J, Luyten FP (2008) Characterized chondrocyte implantation results in better structural repair when treating symptomatic cartilage defects of the knee in a randomized controlled trial versus microfracture. Am J Sports Med 36:235–246
Bentley G, Biant LC, Vijayan S, Macmull S, Skinner JA, Carrington RW (2012) Minimum ten-year results of a prospective randomised study of autologous chondrocyte implantation versus mosaicplasty for symptomatic articular cartilage lesions of the knee. J Bone Joint Surg (Br) 94:504–509
Mason C, Dunnill P (2008) A brief definition of regenerative medicine. Regen Med 3:1–5
Kuo CK, Li WJ, Mauck RL, Tuan RS (2006) Cartilage tissue engineering: its potential and uses. Curr Opin Rheumatol 18:64–73
O’Driscoll SW, Keeley FW, Salter RB (1986) The chondrogenic potential of free autogenous periosteal grafts for biological resurfacing of major full-thickness defects in joint surfaces under the influence of continuous passive motion. An experimental investigation in the rabbit. J Bone Joint Surg Am 68:1017–1035
Grande DA, Singh IJ, Pugh J (1987) Healing of experimentally produced lesions in articular cartilage following chondrocyte transplantation. Anat Rec 218:142–148
Grande DA, Pitman MI, Peterson L, Menche D, Klein M (1989) The repair of experimentally produced defects in rabbit articular cartilage by autologous chondrocyte transplantation. J Orthop Res 7:208–218
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331:889–895
Jiang YZ, Zhang SF, Qi YY, Wang LL, Ouyang HW (2011) Cell transplantation for articular cartilage defects: principles of past, present, and future practice. Cell Transplant 20:593–607
Peterson L, Vasiliadis HS, Brittberg M, Lindahl A (2010) Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med 38:1117–1124
Cole BJ, DeBerardino T, Brewster R, Farr J, Levine DW, Nissen C, Roaf P, Zaslav K (2012) Outcomes of autologous chondrocyte implantation in study of the treatment of articular repair (STAR) patients with osteochondritis dissecans. Am J Sports Med 40:2015–2022
Zaslav K, Cole B, Brewster R, DeBerardino T, Farr J, Fowler P, Nissen C (2009) A prospective study of autologous chondrocyte implantation in patients with failed prior treatment for articular cartilage defect of the knee: results of the Study of the Treatment of Articular Repair (STAR) clinical trial. Am J Sports Med 37:42–55
Bartlett W, Skinner JA, Gooding CR, Carrington RW, Flanagan AM, Briggs TW, Bentley G (2005) Autologous chondrocyte implantation versus matrix-induced autologous chondrocyte implantation for osteochondral defects of the knee: a prospective, randomised study. J Bone Joint Surg (Br) 87:640–645
Ahmed TA, Hincke MT (2010) Strategies for articular cartilage lesion repair and functional restoration. Tissue Eng Part B Rev 16:305–329
Filardo G, Kon E, Roffi A, Di Martino A, Marcacci M (2013) Scaffold-based repair for cartilage healing: a systematic review and technical note. Arthroscopy 29:174–186
Vanlauwe JJ, Claes T, Van Assche D, Bellemans J, Luyten FP (2012) Characterized chondrocyte implantation in the patellofemoral joint: an up to 4-year follow-up of a prospective cohort of 38 patients. Am J Sports Med 40:1799–1807
Tuan RS, Boland G, Tuli R (2003) Adult mesenchymal stem cells and cell-based tissue engineering. Arthritis Res Ther 5:32–45
Teo BJ, Buhary K, Tai BC, Hui JH (2013) Cell-based therapy improves function in adolescents and young adults with patellar osteochondritis dissecans. Clin Orthop Relat Res 471:1152–1158
Kasemkijwattana C, Hongeng S, Kesprayura S, Rungsinaporn V, Chaipinyo K, Chansiri K (2011) Autologous bone marrow mesenchymal stem cells implantation for cartilage defects: two cases report. J Med Assoc Thail 94:395–400
Wakitani S, Mitsuoka T, Nakamura N, Toritsuka Y, Nakamura Y, Horibe S (2004) Autologous bone marrow stromal cell transplantation for repair of full-thickness articular cartilage defects in human patellae: two case reports. Cell Transplant 13:595–600
Nejadnik H, Hui JH, Feng Choong EP, Tai BC, Lee EH (2010) Autologous bone marrow-derived mesenchymal stem cells versus autologous chondrocyte implantation: an observational cohort study. Am J Sports Med 38:1110–1116
Li QA, Tang JC, Wang RY, Bei CY, Xin LW, Zeng YJ, Tang XY (2011) Comparing the chondrogenic potential in vivo of autogeneic mesenchymal stem cells derived from different tissues. Artif Cells Blood Substit Immobil Biotechnol 39:31–38
Koga H, Muneta T, Nagase T, Nimura A, Ju YJ, Mochizuki T, Sekiya I (2008) Comparison of mesenchymal tissues-derived stem cells for in vivo chondrogenesis: suitable conditions for cell therapy of cartilage defects in rabbit. Cell Tissue Res 333:207–215
Murphy JM, Fink DJ, Hunziker EB, Barry FP (2003) Stem cell therapy in a caprine model of osteoarthritis. Arthritis Rheum 48:3464–3474
Kayakabe M, Tsutsumi S, Watanabe H, Kato Y, Takagishi K (2006) Transplantation of autologous rabbit BM-derived mesenchymal stromal cells embedded in hyaluronic acid gel sponge into osteochondral defects of the knee. Cytotherapy 8:343–353
Guo X, Park H, Young S, Kretlow JD, van den Beucken JJ, Baggett LS, Tabata Y, Kasper FK, Mikos AG, Jansen JA (2010) Repair of osteochondral defects with biodegradable hydrogel composites encapsulating marrow mesenchymal stem cells in a rabbit model. Acta Biomater 6:39–47
Yan H, Yu CL (2007) Repair of full-thickness cartilage defects with cells of different origin in a rabbit model. Arthroscopy 23:178–187
Im GI, Kim DY, Shin JH, Hyun CW, Cho WH (2001) Repair of cartilage defect in the rabbit with cultured mesenchymal stem cells from bone marrow. J Bone Joint Surg (Br) 83:289–294
Park JS, Yang HN, Woo DG, Chung HM, Park KH (2009) In vitro and in vivo chondrogenesis of rabbit bone marrow-derived stromal cells in fibrin matrix mixed with growth factor loaded in nanoparticles. Tissue Eng Part A 15:2163–2175
Zhou G, Liu W, Cui L, Wang X, Liu T, Cao Y (2006) Repair of porcine articular osteochondral defects in non-weightbearing areas with autologous bone marrow stromal cells. Tissue Eng 12:3209–3221
Sharma B, Williams CG, Khan M, Manson P, Elisseeff JH (2007) In vivo chondrogenesis of mesenchymal stem cells in a photopolymerized hydrogel. Plast Reconstr Surg 119:112–120
Park J, Gelse K, Frank S, von der Mark K, Aigner T, Schneider H (2006) Transgene-activated mesenchymal cells for articular cartilage repair: a comparison of primary bone marrow-, perichondrium/periosteum- and fat-derived cells. J Gene Med 8:112–125
Yoshimura H, Muneta T, Nimura A, Yokoyama A, Koga H, Sekiya I (2007) Comparison of rat mesenchymal stem cells derived from bone marrow, synovium, periosteum, adipose tissue, and muscle. Cell Tissue Res 327:449–462
Xie X, Wang Y, Zhao C, Guo S, Liu S, Jia W, Tuan RS, Zhang C (2012) Comparative evaluation of MSCs from bone marrow and adipose tissue seeded in PRP-derived scaffold for cartilage regeneration. Biomaterials 33:7008–7018
Fernandez FB, Shenoy S, Babu SS, Varma HK, John A (2012) Short-term studies using ceramic scaffolds in lapine model for osteochondral defect amelioration. Biomed Mater 7, 035005
Lee JC, Min HJ, Park HJ, Lee S, Seong SC, Lee MC (2013) Synovial membrane-derived mesenchymal stem cells supported by platelet-rich plasma can repair osteochondral defects in a rabbit model. Arthroscopy 29:1034–1046
Lee JC, Lee SY, Min HJ, Han SA, Jang J, Lee S, Seong SC, Lee MC (2012) Synovium-derived mesenchymal stem cells encapsulated in a novel injectable gel can repair osteochondral defects in a rabbit model. Tissue Eng Part A 18:2173–2186
Suzuki S, Muneta T, Tsuji K, Ichinose S, Makino H, Umezawa A, Sekiya I (2012) Properties and usefulness of aggregates of synovial mesenchymal stem cells as a source for cartilage regeneration. Arthritis Res Ther 14:R136
Pei M, He F, Boyce BM, Kish VL (2009) Repair of full-thickness femoral condyle cartilage defects using allogeneic synovial cell-engineered tissue constructs. Osteoarthritis Cartilage 17:714–722
Pei M, He F, Li J, Tidwell JE, Jones AC, McDonough EB (2013) Repair of large animal partial-thickness cartilage defects through intraarticular injection of matrix-rejuvenated synovium-derived stem cells. Tissue Eng Part A 19:1144–1154
Mifune Y, Matsumoto T, Takayama K, Ota S, Li H, Meszaros LB, Usas A, Nagamune K, Gharaibeh B, Fu FH, Huard J (2013) The effect of platelet-rich plasma on the regenerative therapy of muscle derived stem cells for articular cartilage repair. Osteoarthritis Cartilage 21:175–185
Matsumoto T, Cooper GM, Gharaibeh B, Meszaros LB, Li G, Usas A, Fu FH, Huard J (2009) Cartilage repair in a rat model of osteoarthritis through intraarticular transplantation of muscle-derived stem cells expressing bone morphogenetic protein 4 and soluble Flt-1. Arthritis Rheum 60:1390–1405
Wakitani S, Aoki H, Harada Y, Sonobe M, Morita Y, Mu Y, Tomita N, Nakamura Y, Takeda S, Watanabe TK, Tanigami A (2004) Embryonic stem cells form articular cartilage, not teratomas, in osteochondral defects of rat joints. Cell Transplant 13:331–336
Toh WS, Lee EH, Guo XM, Chan JK, Yeow CH, Choo AB, Cao T (2010) Cartilage repair using hyaluronan hydrogel-encapsulated human embryonic stem cell-derived chondrogenic cells. Biomaterials 31:6968–6980
Dattena M, Pilichi S, Rocca S, Mara L, Casu S, Masala G, Manunta L, Manunta A, Passino ES, Pool RR, Cappai P (2009) Sheep embryonic stem-like cells transplanted in full-thickness cartilage defects. J Tissue Eng Regen Med 3:175–187
Hiramatsu K, Sasagawa S, Outani H, Nakagawa K, Yoshikawa H, Tsumaki N (2011) Generation of hyaline cartilaginous tissue from mouse adult dermal fibroblast culture by defined factors. J Clin Invest 121:640–657
Vinardell T, Sheehy EJ, Buckley CT, Kelly DJ (2012) A comparison of the functionality and in vivo phenotypic stability of cartilaginous tissues engineered from different stem cell sources. Tissue Eng Part A 18:1161–1170
Pendleton C, Li Q, Chesler DA, Yuan K, Guerrero-Cazares H, Quinones-Hinojosa A (2013) Mesenchymal stem cells derived from adipose tissue vs bone marrow: in vitro comparison of their tropism towards gliomas. PLoS One 8, e58198
Hildner F, Albrecht C, Gabriel C, Redl H, van Griensven M (2011) State of the art and future perspectives of articular cartilage regeneration: a focus on adipose-derived stem cells and platelet-derived products. J Tissue Eng Regen Med 5:E36–E51
Yamashita A, Nishikawa S, Rancourt DE (2010) Identification of five developmental processes during chondrogenic differentiation of embryonic stem cells. PLoS One 5, e10998
Yamashita A, Liu S, Woltjen K, Thomas B, Meng G, Hotta A, Takahashi K, Ellis J, Yamanaka S, Rancourt DE (2013) Cartilage tissue engineering identifies abnormal human induced pluripotent stem cells. Sci Rep 3:1978
Goldring MB, Tsuchimochi K, Ijiri K (2006) The control of chondrogenesis. J Cell Biochem 97:33–44
Tuan RS (2003) Cellular signaling in developmental chondrogenesis: N-cadherin, Wnts, and BMP-2. J Bone Joint Surg Am 85-A(Suppl 2):137–141
Shum L, Coleman CM, Hatakeyama Y, Tuan RS (2003) Morphogenesis and dysmorphogenesis of the appendicular skeleton. Birth Defects Res C Embryo Today 69:102–122
Wezeman FH (1998) Morphological foundations of precartilage development in mesenchyme. Microsc Res Tech 43:91–101
Akiyama H, Lefebvre V (2011) Unraveling the transcriptional regulatory machinery in chondrogenesis. J Bone Miner Metab 29:390–395
Hwang NS, Varghese S, Lee HJ, Zhang Z, Ye Z, Bae J, Cheng L, Elisseeff J (2008) In vivo commitment and functional tissue regeneration using human embryonic stem cell-derived mesenchymal cells. Proc Natl Acad Sci U S A 105:20641–20646
Barry F, Boynton RE, Liu B, Murphy JM (2001) Chondrogenic differentiation of mesenchymal stem cells from bone marrow: differentiation-dependent gene expression of matrix components. Exp Cell Res 268:189–200
Byers BA, Mauck RL, Chiang IE, Tuan RS (2008) Transient exposure to transforming growth factor beta 3 under serum-free conditions enhances the biomechanical and biochemical maturation of tissue-engineered cartilage. Tissue Eng Part A 14:1821–1834
Huang AH, Stein A, Tuan RS, Mauck RL (2009) Transient exposure to transforming growth factor beta 3 improves the mechanical properties of mesenchymal stem cell-laden cartilage constructs in a density-dependent manner. Tissue Eng Part A 15:3461–3472
Estes BT, Wu AW, Guilak F (2006) Potent induction of chondrocytic differentiation of human adipose-derived adult stem cells by bone morphogenetic protein 6. Arthritis Rheum 54:1222–1232
Hennig T, Lorenz H, Thiel A, Goetzke K, Dickhut A, Geiger F, Richter W (2007) Reduced chondrogenic potential of adipose tissue derived stromal cells correlates with an altered TGFbeta receptor and BMP profile and is overcome by BMP-6. J Cell Physiol 211:682–691
Acknowledgments
Supported by the Commonwealth of Pennsylvania Department of Health (SAP 4100050913), US Department of Defense (W81XWH-14-2-000, OR130296, W81XWH-15-0104), Arthur J. Rooney, Sr. Endowment, and NIH (R01 GM115444).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Lozito, T.P., Jiang, Y., Tuan, R.S. (2016). Cartilage Healing, Repair, and Regeneration: Natural History to Current Therapies. In: Wilson-Rawls, J., Kusumi, K. (eds) Innovations in Molecular Mechanisms and Tissue Engineering. Stem Cell Biology and Regenerative Medicine. Humana Press, Cham. https://doi.org/10.1007/978-3-319-44996-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-44996-8_4
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-44994-4
Online ISBN: 978-3-319-44996-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)