Abstract
Cardiogenetics faces two major challenges: identifying index cases and making optimal use of sequencing technologies. Nonexpert physicians need to be actively engaged to identify index cases, not only in cardiology and clinical genetics but also in primary care, population screening, at postmortem, and elsewhere in health care. Training, including e-modules, is needed to update knowledge and skills. An active approach to test family members of diagnosed cases may save lives. With decreasing prices of sequencing technologies, the temptation to sequence everything that is possible might lead to many variants of unknown significance. Patients and their families would be better served by targeted analysis of variants of high predictive value and selecting the DNA test based on the phenotype. Data sharing and more detailed and precise phenotyping will help to better understand the current variants of unknown significance.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Health Care Worker
- Familial Hypercholesterolemia
- Familial Hypercholesterolemia
- Brugada Syndrome
- Opportunistic Screening
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Over the last two decades, cardiogenetics has developed as a health service at the interface of cardiology and genetics. The 23 chapters in this book discuss disorders, some of which may be rare, but the sum of which deserves serious attention in health care. Cardiac disorders often follow a well-known pattern (risk associated with age, obesity, smoking, sedentary lifestyle, diabetes) but if the usual pattern does not fit, a cardiogenetic diagnosis may apply, requiring a treatment that is different and often disease-specific. Since many of these conditions are autosomal dominant (with reduced penetrance), presymptomatic diagnosis in family members may provide a platform for early prevention strategies.
In this final chapter, we will discuss challenges for the future. The first challenge is how the increasing body of knowledge can be translated from science to implementation at a population level. To avoid that science is “lost in translation,” an active approach to identify index cases is needed, in cardiology, clinical genetics, primary care, population screening, at postmortem, and elsewhere in health care. Furthermore, a challenge is how new technologies can be implemented in health care in a responsible manner, including genome sequencing technologies and imaging, with the ultimate goal to improve the care of patients and their families with inherited heart diseases.
The First Step
Diagnosis in the Mainstream of Medicine
Translation of cardiogenetic knowledge to health care requires that index cases are recognized. For cardiology and clinical genetics, diagnostic skills and technical support may be relatively well developed. The first contact in health care, however, can be in primary care, in a public health screening program, at the ultrasound unit, or at postmortem. Many stakeholders are involved in these different settings. Therefore, a transdisciplinary collaborative effort is required for a beneficial effect of cardiogenetics in daily medical practice. Current diagnostic workup of suspected ischemic heart disease in primary care often applies a limited set of parameters to assess risk. In daily primary care practice, important subsets of patients at high risk based on a family history of premature heart disease, but otherwise limited conventional risk profile, are withheld further diagnostics.
Current genomic literacy of nongeneticist health care providers is limited. Up-to-date CVD guidelines could be of great value since they are frequently checked in daily practice, could be used in educational activities, and are used to attune between primary and secondary care. While not all (rare) diseases can be recognized, the red flag or gut feeling “this is not a regular cardiovascular problem” should be developed for all health care workers. Electronic health records with integrated ICT tools will help daily practice to register family history, store, and analyze imaging results, and provide decision support. Consequently awareness and information on possibilities for referral to centers with adequate diagnostic facilities can then be provided. The future health care worker can go to online resources to quickly look up which diagnoses should be considered, to whom he can refer, and which tests are available. Postgraduate training will update health care workers on the current status of cardiogenetics. Given the fast developments, not only face-to-face training sessions are needed but also e-learning is needed to enable noncardiogeneticists to update their skills (Houwink et al. [8]).
Population Screening
Apart from recognizing patients who visit a clinic with symptoms of cardiogenetic disorders, it is conceivable that all asymptomatic persons at a certain age (newborn) or in a certain setting (working place, sports) would be offered screening for cardiogenetic risks. Ever increasing genome technological capability will force a discussion of including genetic tests in these screening programs (Henneman et al. [7]). In general, population screening programs are implemented only after careful consideration whether the pros outweigh the cons, a systematic evaluation of which may use the framework developed by Wilson and Jungner in 1968, or frameworks that elaborated these criteria [22]. Criteria include whether the condition screened for is an important health problem, the natural history is adequately understood, treatment is available, good tests are available, and the cost of case finding is economically in balance relative to medical expenditure.
Familial Hypercholesterolemia (FH) as Example
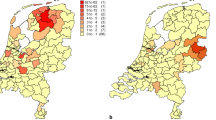
For the field of cardiogenetics, the assessment of cholesterol levels and subsequent DNA testing to recognize familial hypercholesterolemia (FH) may serve as a historical example. Most people with FH are undiagnosed or only diagnosed after their first coronary event. There is a need for earlier detection. The first step should be effective family history taking, the primary care physician would be the first health care worker in most cases where people with (early) disease symptoms could come. Up to 1 in 200–500 individuals carry a mutation in genes associated with FH (LDLR, APOB, PCSK9) (Kassner et al. [12]). Early identification followed by lipid lowering treatment, increasing levels of physical activity and not smoking can substantially reduce mortality and morbidity. A cascade-screening program in the Netherlands identified 28.000 persons affected (Carpay et al. [2]). It has been estimated that this represents 50–71 % of the patients in the country (Carpay et al. [2], Norderstgaard et al. [13]). Other countries have reported lower proportions recognized, even <1 % (Nordestgaard et al. [13]). Several types of FH-screening programs exist, but a recent debate focused on the question whether all 10–12 year old children should be screened. In children, opportunities for CHD prevention are greatest (Wiegman et al. [21]). In the USA in 2003, the CDC began funding integrating genomics into chronic disease programs where possible (St. Pierre [17]). A statewide universal screening of school children would optimize prevention for all FH children. However, in such an endeavor different professional groups come together, each with their own practices, cultures, and structures. Decisions must be made on the type of the test used (first cholesterol, DNA as second tier?). For the future, this primary preventive approach may be suitable for more conditions. Presymptomatic genetic testing of minors is, however, often not encouraged, but it may be acceptable if preventive actions can be initiated before adulthood [3]. In many cardiogenetic conditions indeed, prevention should start before adulthood.
Opportunistic Screening
Sequencing technologies would make it possible to investigate cardiogenes whenever sequencing is performed: opportunistic screening (Green et al. [4]). It has been argued that the ethics of opportunistic screening requires further debate, and informed decision making for the individuals undergoing testing should be facilitated; however, the technical possibilities exist already. Professionals need to develop recommendations for handling genomic findings not related to the initial clinical question, in line with the legal and cultural particularities of individual states (Hehir-Kwa et al. [6]).
Postmortem Cardiogenetic Diagnostics
The first cardiovascular event in a lifetime can lead to sudden death. Pathologists and coroners play an important role to recognize cardiogenetic conditions, particularly in sudden cardiac death in the young aged under 35 years, and thus to contribute to prevention in relatives. Countries differ in their postmortem health services. Protocols should include the possibility of reporting of the results of postmortem investigations to relatives, freezing tissue, or isolating DNA (Semsarian et al. [16], Bagnall et al. [1]). The autopsy rate in young sudden death cases could be increased, and more families should undergo cardiogenetic evaluation to detect inherited cardiac diseases (van der Werf et al. [19]). Presymptomatic diagnosis in healthy relatives will make targeted treatment possible, such as implantable cardioverter defibrillator placement. This can save future lives (Stattin et al. [18]).
New Methods
Pipelines for Multiple Variants in Multiple Genes
Whole genome sequencing techniques have entered diagnostic laboratories, making it possible to investigate simultaneously many potential causes of a specific disorder (Haas et al. [5]). The cost of sequencing has decreased rapidly (https://www.genome.gov/sequencingcosts/), thus making it possible to do the test first and depend less on a differential diagnosis of an expert cardiogeneticist. Many people who lost a family member due to sudden (cardiac?) death did not have access to genomic testing, but with pipelines for hundreds of genes implicated in cardiogenetics, they may qualify for a broad DNA test to confirm or exclude an increased risk for themselves. A major challenge will be the interpretation of variants. Only if the predictive value of a variant is high, a (preventive) treatment should be proposed, but what does this mean for the pipelines to be built? It has been suggested to use a targeted approach first in order to avoid unsolicited findings or findings that cannot be interpreted, and that known genetic variants with limited or no clinical utility should be filtered out (van El et al. [20]).
Interpreting Variants
A major challenge in the current era is determining the pathogenicity of identified variants. Caution is needed as variants of unknown significance (VUS) can be detected in a high percentage of probands (Nunn et al. [14]), with an increase in VUS as more genes are screened. A mutation in genes associated with cardiomyopathies and ion channelopathies is not always a disease causing mutation, and so measures to determine pathogenicity need to be improved as we look ahead at whole exome and genome approaches. Proband genetic testing results in a probabilistic outcome, with the need for accumulating evidence for disease causality (Ingles [10]). Population databases may help to determine whether a variant was frequently seen in healthy persons or only in affected families. Sharing of data is more important than ever not only for research but for clinical purposes as well. Initiatives such as The Global Alliance for Genomics and Health (genomicsandhealth.org) and The Clinical Genome Resource (clinicalgenome.org) call for the establishment of a common framework of harmonized approaches to enable effective and responsible sharing of genomic and clinical data, and by catalyzing data-sharing projects that drive and demonstrate the value of data sharing. Functional data can indicate whether a variant has phenotypical consequences in animal models, or even in in silico tools such as myocytes on-a-chip. Rapid functional assays for determining disease causality of variants are currently lacking and will be an important component of future cardiogenetic evaluation. Newer and faster animal models such as zebrafish, and utility of induced pluripotent stem cells derived from the patient, may be the types of methods which may help to elucidate the functional consequences of the identified genetic variants.
The Choice of the Genetic Test
With the explosion of next-generation sequencing technologies, the temptation will be to screen all genes. The choice of which genetic test is chosen for the individual patient will be more important than ever. Unnecessary screening of genes will likely result in more VUS, more incidental, and secondary findings. As such, the principle of determining the most appropriate genetic tested based on the patient’s phenotype will be essential. Targeted genetic sequencing of the top ten hypertrophic cardiomyopathy genes may be the most appropriate test for someone with classical HCM and a strong family history. In contrast, an unexplained sudden death in a young person may require a genetic testing panel of 50–60 genes covering the main primary arrhythmia disease genes for LQTS, BrS, and CPVT. The clear tradeoff is that in all cardiogenetic diseases, as more disease genes are screened, the greater likelihood of VUS results (Ingles [11]).
Improving Detection of the Cardiac Phenotype: “Deep Phenotyping”
One of the major challenges relating to cardiogenetics in coming years is to match the depth of genetic sequencing with more detailed and precise phenotyping (Semsarian [15]). Most clinicians agree that measuring a QT interval on an ECG or measuring a left ventricular wall thickness on an echocardiogram are very basic and superficial measures for long QT syndrome and HCM respectively. Newer clinical diagnostics will be required to phenotype cardiogenetic patients in more detail. This may include more precise imaging techniques, use of serum biomarkers of disease, and more ambulatory measures such as 12 lead Holter monitoring in Brugada syndrome patients. Such newer approaches will facilitate better definition of the cardiac phenotype, allow better targeting of genetic testing, and may have implications for the choice of therapeutic interventions and overall prognosis.
Imaging
Cardiac magnetic resonance imaging and cardiac computed tomographic angiography are increasingly available for noninvasive diagnosis of cardiovascular disease. Structural anomalies identified while using advanced imaging techniques may help to diagnose hypertrophic cardiomyopathy, FH causing premature coronary disease, and systemic connective tissue diseases. If young high-risk individuals are to profit most from imaging, a strategy is needed to timely recognize these high-risk patients in clinical practice through an increase in genomic literacy of all relevant health care providers (Houwink et al. [9]). An integrated and multidisciplinary strategy is needed for timely detection of cardiovascular disease using advanced imaging and genomics techniques.
Summary/Take Home Message
Cardiogenetics has developed over the last two decades to a very valuable health service. The main challenges ahead are to make this service well known to all who could potentially benefit. A wider circle of health care workers need education and training in cardiogenetics to improve the recognition of index cases. Testing their healthy family members will contribute to save future lives. Technological developments using sequencing technologies currently lead to many VUS. Data-sharing strategies, functional studies, and deep phenotyping are needed to understand their significance. Filtering known variants will be needed. Genetic variants with limited or no clinical utility should be filtered out.
-
The first step to identify index cases requires mainstreaming of cardiogenetics including increased awareness in primary care and with pathologists.
-
Sequencing techniques will make it possible to investigate multiple variants in multiple genes. The filtering of known variants with known predictive value will be a challenge.
-
The choice of which genetic test will continue to rely heavily on the phenotype of the index case and the relevant family history.
-
The complexities of cardiac genetic testing highlight the importance of a specialized multidisciplinary approach to care for patients and their families.
References
Bagnall RD, Weintraub RG, Ingles J, Duflou J, Yeates L, Lam L, et al. A Prospective Study of Sudden Cardiac Death among Children and Young Adults. N Engl J Med. 2016;374:2441–52.
Carpay MEM, van der Horst A, Hoebee B. Eindrapportage bevolkingsonderzoek naar familiaire hypercholesterolemie. Organisatie en opbrengsten. RIVM Briefrapport 2014–0152. 2014. Bilthoven, RIVM.
European Society of Human Genetics. Genetic testing in asymptomatic minors: recommendations of the European Society of Human Genetics. Eur J Hum Genet. 2009;17:720–1.
Green RC, Berg JS, Grody WW, et al. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet Med. 2013;15:565–74.
Haas J, Frese KS, Peil B, Kloos W, Keller A, Nietsch R, et al. Atlas of the clinical genetics of human dilated cardiomyopathy. Eur Heart J. 2015;36:1123–35a.
Hehir-Kwa JY, Claustres M, Hastings RJ, van Ravenswaaij-Arts C, Christenhusz G, Genuardi M, et al. Towards a European consensus for reporting incidental findings during clinical NGS testing. Eur J Hum Genet. 2015;23:1601–6.
Henneman L, McBride CM, Cornel MC, Duquette D, Qureshi N. Screening for familial hypercholesterolemia in children: What can we learn from adult screening programs? Healthcare. 2015;3:1018–30.
Houwink EJ, Muijtjens AM, van Teeffelen SR, Henneman L, Rethans JJ, Jacobi F, et al. Effect of comprehensive oncogenetics training interventions for general practitioners, evaluated at multiple performance levels. PLoS One. 2015;10(4):e0122648.
Houwink EJ, Sollie AW, Numans ME, Cornel MC. Proposed roadmap to stepwise integration of genetics in family medicine and clinical research. Clin Transl Med. 2013;2:5.
Ingles J, Semsarian C. Conveying a probabilistic genetic test result to families with an inherited heart disease. Heart Rhythm. 2014a;11:1073–8.
Ingles J, Semsarian C. The value of cardiac genetic testing. Trends Cardiovasc Med. 2014b;24:217–24.
Kassner U, Wuhle-Demuth M, Missala I, Humphries SE, Steinhagen-Thiessen E, Demuth I. Clinical utility gene card for: Hyperlipoproteinemia, TYPE II. Eur J Hum Genet. 2014. doi:10.1038/ejhg.2013.271.
Nordestgaard BG, Chapman MJ, Humphries SE, Ginsberg HN, Masana L, OS D, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease consensus statement of the European Atherosclerosis Society. Eur Heart J. 2013;34:3478–90.
Nunn LM, Lopes LR, Syrris P, Murphy C, Plagnol V, Firman E, et al. Diagnostic yield of molecular autopsy in patients with sudden arrhythmic death syndrome using targeted exome sequencing. Europace. 2015; pii: euv285.
Semsarian C, Ingles J. Determining pathogenicity in cardiac genetic testing: filling in the blank spaces. Trends Cardiovasc Med. 2015a;25:653–4.
Semsarian C, Ingles J, Wilde AA. Sudden cardiac death in the young: the molecular autopsy and a practical approach to surviving relatives. Eur Heart J. 2015b;36:1290–6.
St. Pierre J, Bach J, Duquette D, Oehlke K, Nystrom R, Silvey K, et al. Strategies, actions, and outcomes of pilot state programs in public health genomics, 2003–2008. Prev Chronic Dis. 2014;11:E97.
Stattin EL, Westin IM, Cederquist K, Jonasson J, Jonsson BA, Mörner S, et al. Genetic screening in sudden cardiac death in the young can save future lives. Int J Legal Med. 2016;130:59–66.
van der Werf C, Hendrix A, Birnie E, Bots ML, Vink A, Bardai A, et al. Improving usual care after sudden death in the young with focus on inherited cardiac diseases (the CAREFUL study): a community-based intervention study. Europace. 2015; pii: euv059.
Van El CG, Cornel MC, Borry P, Hastings RJ, Fellmann F, Hodgson SV, et al. Whole-genome sequencing in health care: recommendations of the European Society of Human Genetics. Eur J Hum Genet. 2013;21:580–4.
Wiegman A, Gidding SS, Watts GF, Chapman MJ, Ginsberg HN, Cuchel M, et al. Familial hypercholesterolaemia in children and adolescents: gaining decades of life by optimizing detection and treatment. Eur Heart J. 2015;36:2425–37.
Wilson JMG, Jungner G. Principles and practice of screening for disease, vol. 68. Geneva: World Health Organization; 1968.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Cornel, M.C., Houwink, I., Semsarian, C. (2016). Future of Cardiogenetics. In: Baars, H., Doevendans, P., Houweling, A., van Tintelen, J. (eds) Clinical Cardiogenetics. Springer, Cham. https://doi.org/10.1007/978-3-319-44203-7_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-44203-7_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-44202-0
Online ISBN: 978-3-319-44203-7
eBook Packages: MedicineMedicine (R0)