Abstract
Sudden death (SD) is defined as “a nontraumatic, unexpected fatal event occurring within 1 hour after the onset of symptoms in an apparently healthy subject.” “If death is not witnessed, the definition applies when the victim was in good health 24 hours before the event” (Eur Heart J 36(41):2793–2786, 2015). The sudden deaths can be subdivided into noncardiac deaths, sudden cardiac deaths (SCD) and the sudden unexplained deaths (SUD). The latter two categories comprise the cardiac deaths due to inherited diseases and are discussed further in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Sudden Cardiac Deaths (SCD)
- Arrhythmogenic Right Ventricular Dysplasia/cardiomyopathy (ARVD/C)
- Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
- Primary Arrhythmia Syndromes
- Postmortem Investigations
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Sudden death (SD) is defined as “a nontraumatic, unexpected fatal event occurring within 1 hour after the onset of symptoms in an apparently healthy subject.” “If death is not witnessed, the definition applies when the victim was in good health 24 hours before the event” [1]. The sudden deaths can be subdivided into noncardiac deaths, sudden cardiac deaths (SCD) and the sudden unexplained deaths (SUD). The latter two categories comprise the cardiac deaths due to inherited diseases and are discussed further in this chapter.
The sudden death of a young person has an enormous impact on those who are left behind. During the last 10–15 years, it has become clear that in 50–70 % of SCD and SUD victims aged 40 years or younger, potential inherited cardiac disease can be identified as the cause of sudden death [2–4]. Cardiomyopathies (e.g., hypertrophic cardiomyopathy [HCM]) or primary arrhythmia syndromes (e.g., congenital long-QT syndrome [LQTS]) can cause fatal arrhythmias that may lead to sudden death. Premature coronary artery disease, as observed in familial hypercholesterolemia (FH), is another cause of sudden death in the young. Relatives of young SCD victims have an increased risk of carrying the inherited predisposition to develop cardiac disease [5–12]. Furthermore, a family history of sudden death is associated with an increased risk of sudden death among adult family members [13–15]. Increasingly, genetic testing is available for inherited cardiac diseases and new mutations, accounting for specific phenotypes, are being discovered [16–18].
Diagnostic evaluation of first-degree relatives followed by early treatment may reduce the risk of SCD in patients with inherited cardiac diseases [19–22]. However, as sudden cardiac arrest in the young is often the first “symptom” of inherited cardiac disease and early identification is difficult in apparently healthy individuals [23–25], presymptomatic cardiogenetic evaluation has been recommended for first-degree relatives of SCD victims with possible inherited diseases to prevent SCD.
In this chapter, we will present an overview of the epidemiology of SCD in the young and discuss the potential benefits of presymptomatic cardiogenetic evaluation of first-degree relatives. In addition, we will discuss preparticipation screening of young athletes.
Definitions
The terminology that is used to describe SCD is often confusing due to the variety of definitions that are used in the literature. SCD was recently defined as “sudden death due to any cardiac disease or vascular anomaly, or when no extra cardiac cause could be identified at postmortem investigation”. The term sudden unexplained death syndrome (SUDS) is used when the cause of death remains unknown and no postmortem investigation has been performed [1]. In the absence of structural abnormalities on postmortem investigation and with a negative toxicologic screening, the term sudden arrhythmic death syndrome (SADS) is used [1, 5, 8].
The term “sudden death in the young” covers different age categories, but in general comprises victims between 1 and 40 years of age. The general definition of sudden infant death syndrome (SIDS) is “sudden unexpected death of an infant <1 year of age, with onset of the fatal episode apparently occurring during sleep, that remains unexplained after a thorough investigation, including performance of a complete postmortem investigation and review of the circumstances of death and the clinical history” [26]. The distinction between these two age categories (<1 year and >1 year) is based on the differences in incidence and causes. For example, the occurrence of SIDS is strongly associated with sleeping position (after an international public health campaign to place infants on their back while sleeping, the incidence of SIDS decreased with 50–90 %) [27]. Although there is an overlap between the causes of death in SIDS (e.g., the congenital LQTS) and sudden death in the young, we will focus on SCD victims older than 1 year in this chapter.
Incidence
In the general population (over all ages), SCD accounts for approximately 1 death per 1000 person-years. In the young (<40 years), the incidence of SCD is estimated to be 100-fold lower and lies between 0.8 and 3.7 per 100,000 person-years (Fig. 19.1) [11, 28–30]. The population-based incidence of SADS is estimated to be 0.16–0.43/100,000 person-years [31, 32].
Annual incidence of sudden cardiac death among residents of Multnomah County by age-groups, Oregon (population 660,486) (Adapted from Chugh et al. [33])
Incidence estimates vary considerably between studies. The collection of data on this topic is complicated, because most cases of sudden death occur out of hospital and often information needs to be collected retrospectively [34]. In addition, traumatic deaths like car accidents or drownings can initially be caused by a cardiac arrhythmia but are often not taken into account in incidence estimates. As no nationwide registrations of victims of SCD or SUD of 1–40 years exist, present studies are often restricted to regional observations, where socioeconomical status, racial differences, and the presence of founder mutations predisposing to a specific cardiogenetic disorder might influence the occurrence of SCD [35, 36]. From studies based on death certificate diagnosis, absolute numbers of sudden deaths in the young population may be adequately derived, but the proportion of cardiovascular deaths may be unreliable due to misclassification [37, 38].
Causes
SCD in persons older than 40 years is mainly due to coronary artery disease that can result in myocardial ischemia and fatal arrhythmias. It has been estimated that 80 % of the cardiac deaths in victims over 40 years of age are caused by coronary artery disease, 10–15 % by cardiomyopathies, and 5 % by other (less common) causes [39]. However, in the young (1–40 years), inherited cardiac causes are more frequently observed. A review of the literature was performed that included articles from 1980 to 2007 on causes of death in the young. All studies were included in which postmortem investigation was performed in >70 % of the sudden death victims [28]. Seventeen publications were identified, including 3528 cases of SD in the age group of 1–40 years that were collected between 1967 and 2004. The most common causes of SD in persons aged 1–40 years were atherosclerotic coronary artery disease (accounting for 23 % of the cases), followed by the autopsy negative deaths (including the primary arrhythmia syndromes) (16 %) and cardiomyopathies (13 %). In athletes, cardiomyopathies were the most common causes of SD (accounting for 48 % of the cases), followed by (nonatherosclerotic) coronary pathology (e.g., coronary artery aneurysm and vasculitis) (16 %) and atherosclerotic coronary artery disease (CAD) (7 %). A considerable proportion of the sudden deaths remained unexplained, accounting for 16 % of the SCD in the general population and 4 % in the athlete population. This latter group comprises primary arrhythmia syndromes [e.g., LQTS, catecholaminergic polymorphic ventricular tachycardia (CPVT) and the Brugada syndrome (BS)] [40, 41]. The proportion of deaths due to coronary artery disease increases with age. In addition, myocarditis and primary arrhythmia syndromes were relatively more common in the younger sudden death cases (1–25 years) (Table 19.1) [23, 28, 42].
Demographics
Information on regional, racial, and gender differences in SCD in the young is scarce. However, it seems that the incidence and causes of SCD (over all ages) differ among regions and populations [43, 44]. This might be due to several factors including the regional distribution of age and gender and the prevalence of inherited cardiac diseases and coronary artery disease. Several studies reported clustering of inherited diseases in populations (and regions); in southeast Asia for example, especially in Cambodia, Philippines, Thailand, and Japan, the incidence of nocturnal sudden death among young men was estimated to be as high as 26–38 per 100,000 person-years. Cardiogenetic evaluation suggested that a primary arrhythmia syndrome similar to the BS is underlying these sudden deaths [45–48]. Furthermore, SCD occurs more frequently in African Americans than in white Americans [42]. HCM is the most common cause of SCD in the athletes in the United States, while in the Veneto region in Italy, arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C) is accounting for the majority of deaths among athletes [49–51].
Overall, SCD in the young (1–40 years) is more common in men (2.27 per 100,000 person-years) than in women (0.95 per 100,000 person-years) [28]. This difference can partly be explained by the high proportion of deaths due to coronary artery disease which is increasing over age (especially >30 years) [28, 42] and perhaps because women are relatively protected for the development of atherosclerosis in the premenopausal period [52–54].
Postmortem Diagnosis
A dedicated and focused postmortem investigation as compared to a “routine” cardiac postmortem investigation is essential in detecting potential inherited cardiac diseases in sudden death victims. Postmortem investigation includes investigation of the circumstances of death, verification of the victim’s medical history and family history, postmortem investigation, and DNA storage. [55, 56]
Circumstances of Death, Verification of the Victim’s Medical History and Family History
An effort should be made to obtain relevant information from health care professionals (e.g., resuscitation team) and other witnesses of the event regarding the circumstances of death (e.g., occurring during sleep, emotional stress, or exercise), the type and duration of preceding symptoms (e.g., chest pain, dizziness, nausea, fever, or headache), and the location of the fatal event. Relatives and general practitioners can be a useful source of information on medical and family history. Circumstances of death can provide important clues to the underlying causes of death, since triggers of sudden cardiac arrest might be specific for the underlying disease. Arrhythmias may be triggered by exercise in patients with HCM, ARVD/C, LQTS type 1, or CPVT, while in patients with BS or LQTS type 3, fatal arrhythmias more often occur during sleep. Furthermore, information on the victim’s medical history should be collected (e.g., recent infections, surgical operations, or comorbidities (e.g., hypertension, neuromuscular diseases, asthma, or epilepsy). Medication use as well as cigarette exposure, alcohol, and substance abuse should be reported.
Besides, the victim’s family history with respect to sudden death and inherited cardiac or neuromuscular diseases can reveal important additional information. When available, antemortem investigations (e.g., electrocardiogram, echocardiography, results of exercise testing, or CT scan) should be investigated [55, 56].
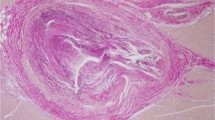
Postmortem Investigation
Recently, international guidelines for postmortem investigation in SCD/SUD in the young have been published [55, 57]. When postmortem investigation is limited to macroscopic examination of the heart without histological sampling of cardiac tissue or toxicological examination, focal cardiac abnormalities or extracardiac causes such as an intoxication may remain undetected. In 79 % of the cases of SCD without macroscopic abnormalities, histopathological examination of the heart revealed local pathology like focal myocarditis or the presence of conduction system abnormalities [58]. Revision of the heart by a cardiac expert pathologist is recommended when no cause of death can be established. A toxicological examination for drugs (e.g., opiates, amphetamine), alcohol, and medication may be considered necessary in cases with no structural abnormalities at autopsy [59, 60].
DNA Storage
Storage of the victim’s DNA enables genetic testing when relatives consult a cardiologist or clinical–geneticist for cardiogenetic evaluation. Postmortem investigation allows tissue to be collected and stored in a tissue bank. Usually, only paraffin-embedded tissue is stored when a SCD victim is autopsied, which is not an optimal source for extensive genetic testing. Guidelines have supported the notion that it is desirable to store EDTA-blood and/or frozen muscle, liver, or spleen tissue that can be obtained during postmortem investigation [1, 58, 61]. When no postmortem investigation is performed, a skin biopsy might be taken (with permission from the victim’s relatives). Prior to the biopsy, the skin needs to be disinfected with alcohol. The obtained tissue can be temporarily stored in a sterile vial with physiological isotonic saline before sending it to a DNA laboratory [62].
Cardiogenetic Evaluation of First-Degree Relatives of Young Sudden Cardiac Death Victims
Cardiogenetic Clinic
When an inherited cardiac disease is suspected or when the cause of death remains unknown, relatives should be referred for cardiogenetic evaluation that comprises cardiological assessment and/or genetic testing [1, 57]. Cardiogenetic evaluation entails several aspects that need careful consideration upfront. These include difficulties in establishing a final diagnosis, the interpretation of genetic test results, and the ethical considerations concerning genetic testing [63]. Relatives should be informed about the advantages and disadvantages of cardiogenetic evaluation (see Chap. 2). Therefore, dedicated cardiogenetic outpatient clinics have been established that provide integrated cardiogenetic care by combining expertise from the fields of ethics, genetics, and cardiology.
Genetic Testing in SCD and SADS Victims
Recent cardiogenetic developments have resulted in the identification of many different mutated genes related to specific cardiac pathology, and consequently lead to a better understanding of the pathophysiology of clinical syndromes such as HCM and LQTS [64]. However, genetic testing does not always reveal a genetic mutation when an inherited cardiac disease is suspected [65–67].
Not all causative mutations have been discovered yet and many clinical syndromes show genetic heterogeneity. In SADS victims, genetic testing revealed a mutation in LQTS-associated genes in 20 % of the victims and a mutation in CPVT-associated genes in 14 % of the victims [40, 41]. Genetic testing in SCD and SADS victims is generally guided by the antemortem and postmortem findings and by the cardiological evaluation of the relatives.
Evaluation of First-Degree Relatives
Because most inherited heart diseases show an autosomal dominant pattern of inheritance, first-degree relatives of SCD victims with genetic disease have a 50 % risk of being a carrier of the same disease [64]. As mentioned earlier, former studies showed that, with thorough clinical assessment of first-degree relatives of SUD victims, a cause of death can be established in 22–53 % of the families [5–8]. A Dutch investigation of 43 families of SUD victims, of whom 22 were autopsied, found an inherited cardiac disease in 17 of the 43 families that explained the sudden death of the victims (Fig. 19.2) [6]. Furthermore, a study executed in the United Kingdom revealed an inherited disease in 53 % of the 57 families of SADS victims aged 4–64 years [8].
Diagnosis after evaluation of families with ≥1 SUD victim FH familiar hypercholesterolemia, HCM hypertrophic cardiomyopathy, ARVC arrythmogenic right ventricular cardiomyopathy, LQTS long-QT syndrome, BS Brugada syndrome, CPVT catecholaminergic polymorphic ventricular tachycardia (Adapted from Tan et al. [6])
The yield of genetic testing in relatives is high when the causative mutation is known [68]. However, it should be realized that a relative carrying the mutation of an inherited cardiac disease will not necessarily develop signs or symptoms of the clinical syndrome that is associated with the mutation. Penetrance of genetic mutations may vary among individuals of the same family and sometimes secondary factors (or genes) can influence the phenotype expression [64, 66].
Three scenarios for the cardiogenetic evaluation of first-degree relatives of young SCD/SUD victims can be distinguished (Fig. 19.3):
-
(a)
The causative mutation in the SCD victim is known.
-
(b)
An inherited cardiac disease is suspected in the victim, but not established by genetic testing.
-
(c)
The cause of the victim’s death is unknown (with or without extensive postmortem investigation).
Scenario (a) allows for a targeted approach by genetic testing of the victim’s relatives. Cascade screening, starting with genetic testing of the (genetically) first-degree relatives (which include the parents, children, brothers, and sisters) of an affected individual will genetically identify the causative mutation in one or more of the relatives. Subsequently, the screening can be extended to the connecting branch of the pedigree [66]. Consequently, the absence of the mutation rules out the presence of the disease, and no further investigation of the pedigree is needed. In case a causative mutation is present in a relative, cardiologic evaluation and/or diagnostic follow-up is usually indicated.
In scenario (b), the cardiogenetic evaluation of relatives is more complicated. The postmortem findings in the victim may raise the suspicion of an inherited cardiac disease. Based on this, targeted cardiologic evaluation of the relatives can be performed. Based on the results of the cardiologic evaluation of relatives, targeted genetic testing can be performed in the victim (if the victim’s DNA is available) or in the clinically affected relative (with cardiac abnormalities).
If a mutation is found, cascade screening in the pedigree is recommended (see scenario a). In case no mutation can be detected, cardiologic evaluation (guided by the findings in the affected relative or postmortem findings in the sudden death victim) of all first-degree relatives may be considered. As the penetrance of a causative mutation may differ among individuals, the absence of abnormalities on cardiologic evaluation does not automatically rule out the presence of an inherited disease. In some diseases, symptoms develop only at older age (e.g., HCM, DCM, and ARVD/C), which may mandate follow-up in these individuals.
In scenario (c), the cause of sudden death is unknown and no clues are available for a specific diagnosis, which makes cardiogenetic evaluation less feasible. A cardiac examination of the relatives may reveal a relevant diagnosis. Examination should include the following aspects; (1) medical history, (2) physical examination, (3) standard resting 12 lead electrocardiogram and 12 lead electrocardiogram with specific right precordial positioning of the leads (leads – V1, V2, 1V1, and 1V2), (4) echocardiography, (5) Holter recording, (6) exercise testing, and (7) measurement of serum lipid levels [69]. If the initial examination raises the possibility of a specific genetic disorder, additional investigations may be indicated, which may include provocation testing (e.g., ajmaline challenging), cardiac MRI, and genetic testing [5–8].
Cost-Effectiveness of Cardiogenetic Evaluation of First-Degree Relatives
A formal evaluation of the above-mentioned scenarios to identify inherited cardiac diseases in relatives of young sudden death victims has not been performed. The cost-effectiveness of cardiogenetic evaluation of relatives of SCD/SUD victims depends on the balance between the probability of identifying the causative mutation and its associated therapeutic (risk reduction through treatment) and prognostic consequences (risk when no treatment is given). This can differ from situation to situation. Since the costs of genetic testing are associated with the number and size of the analyzed genes, a targeted genetic evaluation of relatives (e.g., scenarios a and b) is likely to result in a higher yield of genetic testing and lower costs [70]. When the cause of death is unknown (scenario c), genetic evaluation is less (cost)-effective [71]. Limited analyses of only those genes that are responsible for the major part of the clinical syndromes seem to increase efficiency. To date, no studies on the yield and cost-effectiveness of cardiogenetic evaluation of relatives of SCD/SUD victims have been published. A cost-effectiveness analysis through modeling is necessary to provide additional information on the value of cardiogenetic evaluation of relatives for different diseases and scenarios [28]. Based on these future studies, recommendations can be drafted regarding the cardiogenetic evaluation of relatives of SCD/SUD victims.
Preparticipation Screening of Athletes
Being physically active is generally regarded as the best way to prevent (cardiovascular) disease, but vigorous activity can also acutely and transiently increase the risk of acute cardiac events in susceptible persons [72]. Physical activity can trigger fatal arrhythmias in persons with cardiomyopathies (e.g., HCM or ARVD/C), CPVT, and LQTS or provoke coronary plaque rupture in those with coronary artery disease [72, 73]. The sudden death of an apparently healthy athlete inevitably leads to discussions if death could have been prevented by preparticipation screening.
Approximately 5–14 % of all SCDs in the young occur during physical activity [74–76]. However, it is still largely unclear whether young athletes have an increased risk of SCD compared to nonathletes. An Italian study reported that the risk of SD was 2.5 (CI: 1.8–3.4) times higher in young athletes than in nonathletes [77]. In this study, events not directly associated with physical activity were also taken into account. The physician’s Health Study reported a 16.9 times higher risk of sudden death (CI: 10.5–27.0) during physical activity and the 30 min after physical activity than during episodes of low activity, but an association between the frequency of physical activity and the long-term risk of sudden death could not be established [76]. A moderate to intensive level of physical activity was associated with a significant decrease in SCD in a study of 7735 middle-aged men [72].
In 2015, the European Society of Cardiology issued recommendations for routine preparticipation cardiovascular screening of young competitive athletes [1]. It is recommended that asymptomatic adults who are moderately active, should be evaluated according to a risk assessment scheme. The evaluation consists of a questionnaire, physical examination, an electrocardiogram and a risk SCORE [78]. An electrocardiogram (although recommended for specific subgroups) is not a standard part of the preparticipation screening recommended by the American Heart Association that essentially relies on medical history and physical examination [79]. The European recommendations are largely based on the Italian experience, suggesting that the introduction of a screening program in young athletes led to a decline in the incidence of SCD. In Italy, 55 cases of SCD aged 12–35 years among screened athletes were registered between 1997 and 2004. The incidence of SCD dropped from 4.19 (CI: 1.78–7.59) to 0.87 (CI: 0.46–1.28) per 100,000 athletes per year [29].
The European preparticipation screening recommendations have led to a stream of pro-contra discussions [80, 81]. The main criticisms of the recommendations are the lack of randomized studies to support the recommendations, the absence of validated questionnaires and electrocardiographic criteria, and the potential of false-positive findings among screened athletes, especially given the rare occurrence of SCD in young athletes [80]. The interpretation of the electrocardiogram of athletes is hampered by physiological adaptation to systematic training, known as the athlete’s heart [82]. Up to 40 % of the electrocardiograms taken in athletes demonstrate variations that can be deemed abnormal, such as sinus bradycardia, atrial fibrillation, and ST-segment changes in the right precordial leads [78]. Furthermore, it has been estimated that only a small proportion of the athletes who suddenly died would have been previously identified as being at increased risk of SCD by the preparticipation program [80].
The Netherlands Institute for Public Health and Environment calculated that a randomized study of the effects of preparticipation screening (assuming a 50 % reduction in the rate of SCD from 4 to 2 per 100,000 athletes per year, with 80 % power) would mandate two groups with 1,200,000 person-years of follow-up. Taking this into account, it is unlikely that definitive evidence supporting the use of preparticipation screening will ever be presented.
Raising awareness of the potential consequences of symptoms during exercise (e.g., collapse, chest discomfort), improving the availability of automated external defibrillators, and careful cardiogenetic evaluation of young SCD victims and their relatives may constitute sound alternatives to mandatory preparticipation screening. Given the higher absolute number of acute cardiac arrests in older athletes, in whom coronary artery disease is far more common, this group should not be neglected [83].
Take Home Message
-
The incidence of sudden cardiac death in persons 40 years or younger is approximately 0.8–1.6 per 100,000 person-years.
-
Sudden cardiac death or sudden unexplained death in the young is frequently caused by inherited cardiac diseases.
-
A thorough postmortem investigation of young SCD/SUD victims is desirable to establish the cause of death.
-
Standardization of postmortem investigation is important to compare studies on the causes of sudden cardiac death and sudden unexplained death and to enable pooling of information from various sources.
-
Relatives of sudden cardiac death victims with diagnosed inherited diseases have a high risk of being a carrier of an inherited cardiac disease, because most inherited cardiac diseases show an autosomal dominant pattern of inheritance.
-
If postmortem investigation does not reveal any structural abnormalities in young victims or when no postmortem examination is performed in SUD victims, cardiogenetic evaluation of relatives should be considered.
-
The cost-effectiveness of screening of relatives of sudden cardiac and sudden unexplained death victims needs to be analyzed in future studies.
-
Given the rare occurrence of SCD in young athletes, the preventive effects of routine preparticipation screening is likely to be limited.
-
Raising awareness of the potential consequences of symptoms during exercise (e.g., collaps, chest discomfort), improving the availability of automated external defibrillators, and careful cardiogenetic evaluation of young SCD/SUD victims and their relatives may constitute sound alternatives to mandatory preparticipation screening.
References
Priori SG, Blomstrom-Lundqvist C. Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC) endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36(41):2793–86.
Wilde AA, Bezzina CR. Genetics of cardiac arrhythmias. Heart. 2005;91(10):1352–8.
Wilde AA, van Langen IM, Mannens MM, Waalewijn RA, Maes A. Sudden death at young age and the importance of molecular-pathologic investigation. Ned Tijdschr Geneeskd. 2005;149(29):1601–4.
Vaartjes I, Hendrix A. Sudden death in persons younger than 40 years of age: incidence and causes. Eur J Cardiovasc Prev Rehabil. 2009;16(5):592–6.
Behr E, Wood DA, Wright M, et al. Cardiological assessment of first-degree relatives in sudden arrhythmic death syndrome. Lancet. 2003;362(9394):1457–9.
Tan HL, Hofman N, van Langen IM, van der Wal AC, Wilde AA. Sudden unexplained death: heritability and diagnostic yield of cardiological and genetic examination in surviving relatives. Circulation. 2005;112(2):207–13.
Hofman N, Tan HL, Clur SA, Alders M, van Langen IM, Wilde AA. Contribution of inherited heart disease to sudden cardiac death in childhood. Pediatrics. 2007;120(4):e967–73.
Behr ER, Dalageorgou C, Christiansen M, et al. Sudden arrhythmic death syndrome: familial evaluation identifies inheritable heart disease in the majority of families. Eur Heart J. 2008;29(13):1670–80.
Schwartz K, Carrier L, Guicheney P, Komajda M. Molecular basis of familial cardiomyopathies. Circulation. 1995;91(2):532–40.
Garson Jr A, Dick M, Fournier A, et al. The long QT syndrome in children. An international study of 287 patients. Circulation. 1993;87(6):1866–72.
Vd Werf C, Hendrix A, et al. Improving usual care after sudden death in the young with focus on inherited cardiac diseases (the CAREFUL study): a community-based intervention study. Europace 2015 Apr 1
Cann F, Corbett M et al. Phenotype driven molecular autopsy for sudden cardiac death. Clin Genet. 2016 Mar 22.
Friedlander Y, Siscovick DS, Weinmann S, et al. Family history as a risk factor for primary cardiac arrest. Circulation. 1998;97(2):155–60.
Jouven X, Desnos M, Guerot C, Ducimetiere P. Predicting sudden death in the population: the Paris prospective study I. Circulation. 1999;99(15):1978–83.
Elliott PM, Poloniecki J, Dickie S, et al. Sudden death in hypertrophic cardiomyopathy: identification of high risk patients. J Am Coll Cardiol. 2000;36(7):2212–8.
Alders M, Koopmann TT, Christiaans I, et al. Haplotype-sharing analysis implicates chromosome 7q36 harboring DPP6 in familial idiopathic ventricular fibrillation. Am J Hum Genet. 2009;84(4):468–76.
Lehnart SE, Ackerman MJ, Benson DW, et al. Inherited arrhythmias: a national heart, lung, and blood institute and office of rare diseases workshop consensus report about the diagnosis, phenotyping, molecular mechanisms, and therapeutic approaches for primary cardiomyopathies of gene mutations affecting ion channel function. Circulation. 2007;116(20):2325–45.
Priori SG, Wilde AA, et al. Executive summary: HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. Europace. 2013;15(10):1389–406.
Maron BJ, Spirito P, Shen WK, et al. Implantable cardioverter-defibrillators and prevention of sudden cardiac death in hypertrophic cardiomyopathy. JAMA. 2007;298(4):405–12.
Watanabe H, Chopra N, Laver D, et al. Flecainide prevents catecholaminergic polymorphic ventricular tachycardia in mice and humans. Nat Med. 2009;15(4):380–3.
Hobbs JB, Peterson DR, Moss AJ, et al. Risk of aborted cardiac arrest or sudden cardiac death during adolescence in the long-QT syndrome. JAMA. 2006;296(10):1249–54.
Moss AJ, Zareba W, Hall WJ, et al. Effectiveness and limitations of beta-blocker therapy in congenital long-QT syndrome. Circulation. 2000;101(6):616–23.
Drory Y, Turetz Y, Hiss Y, et al. Sudden unexpected death in persons less than 40 years of age. Am J Cardiol. 1991;68(13):1388–92.
Amital H, Glikson M, Burstein M, et al. Clinical characteristics of unexpected death among young enlisted military personnel: results of a three-decade retrospective surveillance. Chest. 2004;126(2):528–33.
Wisten A, Forsberg H, Krantz P, Messner T. Sudden cardiac death in 15-35-year olds in Sweden during 1992–99. J Intern Med. 2002;252(6):529–36.
Krous HF, Beckwith JB, Byard RW, et al. Sudden infant death syndrome and unclassified sudden infant deaths: a definitional and diagnostic approach. Pediatrics. 2004;114(1):234–8.
Moon RY, Horne RS, Hauck FR. Sudden infant death syndrome. Lancet. 2007;370(9598):1578–87.
Vaartjes I, Hendrix A, Hertogh EM, et al. Sudden death in persons younger than 40 years: causes and incidence. Eur J Cardiovasc Prev and Prehab. 2009;16(5):592–6.
Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006;296(13):1593–601.
Winkel BG, Holst AG. Nationwide study of sudden cardiac death in persons aged 1–35 years. Eur Heart J. 2011;32(8):983–90.
Morentin B, Suarez-Mier MP, Aguilera B. Sudden unexplained death among persons 1-35 years old. Forensic Sci Int. 2003;135(3):213–7.
Behr ER, Casey A, Sheppard M, et al. Sudden arrhythmic death syndrome: a national survey of sudden unexplained cardiac death. Heart. 2007;93(5):601–5.
Chugh SS, Jui J, Gunson K, et al. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44(6):1268–75.
de Vreede-Swagemakers JJ, Gorgels AP, Dubois-Arbouw WI, et al. Out-of-hospital cardiac arrest in the 1990’s: a population-based study in the Maastricht area on incidence, characteristics and survival. J Am Coll Cardiol. 1997;30(6):1500–5.
Corrado D, Basso C, Thiene G. Sudden cardiac death in young people with apparently normal heart. Cardiovasc Res. 2001;50(2):399–408.
Maron BJ. Sudden death in young athletes. N Engl J Med. 2003;349(11):1064–75.
Iribarren C, Crow RS, Hannan PJ, Jacobs Jr DR, Luepker RV. Validation of death certificate diagnosis of out-of-hospital sudden cardiac death. Am J Cardiol. 1998;82(1):50–3.
Fox CS, Evans JC, Larson MG, et al. A comparison of death certificate out-of-hospital coronary heart disease death with physician-adjudicated sudden cardiac death. Am J Cardiol. 2005;95(7):856–9.
Huikuri HV, Castellanos A, Myerburg RJ. Sudden death due to cardiac arrhythmias. N Engl J Med. 2001;345(20):1473–82.
Tester DJ, Ackerman MJ. Post-mortem long QT syndrome genetic testing for sudden unexplained death in the young. J Am Coll Cardiol. 2007;49(2):240–6.
Tester DJ, Spoon DB, Valdivia HH, Makielski JC, Ackerman MJ. Targeted mutational analysis of the RyR2-encoded cardiac ryanodine receptor in sudden unexplained death: a molecular post-mortem investigation of 49 medical examiner/coroner’s cases. Mayo Clin Proc. 2004;79(11):1380–4.
Zheng ZJ, Croft JB, Giles WH, Mensah GA. Out-of-hospital cardiac deaths in adolescents and young adults in the United States, 1989 to 1998. Am J Prev Med. 2005;29(5 Suppl 1):36–41.
Soo L, Huff N, Gray D, Hampton JR. Geographical distribution of cardiac arrest in Nottinghamshire. Resuscitation. 2001;48(2):137–47.
Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–31.
Roberts R, Brugada R. Genetics and arrhythmias. Annu Rev Med. 2003;54:257–67.
Vatta M, Dumaine R, Varghese G, et al. Genetic and biophysical basis of sudden unexplained nocturnal death syndrome (SUNDS), a disease allelic to Brugada syndrome. Hum Mol Genet. 2002;11(3):337–45.
Tungsanga K, Sriboonlue P. Sudden unexplained death syndrome in north-east Thailand. Int J Epidemiol. 1993;22(1):81–7.
Tatsanavivat P, Chiravatkul A, Klungboonkrong V, et al. Sudden and unexplained deaths in sleep
Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119(8):1085–92.
Corrado D, Basso C, Schiavon M, Thiene G. Screening for hypertrophic cardiomyopathy in young athletes. N Engl J Med. 1998;339(6):364–9.
Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA. 1996;27(3):199–204.
Gordon T, Kannel WB, Hjortland MC, McNamara PM. Menopause and coronary heart disease. The Framingham Study. Ann Intern Med. 1978;89(2):157–61.
Atsma F, Bartelink ML, Grobbee DE, van der Schouw YT. Postmenopausal status and early menopause as independent risk factors for cardiovascular disease: a meta-analysis. Menopause. 2006;13(2):265–79.
Colditz GA, Willett WC, Stampfer MJ, Rosner B, Speizer FE, Hennekens CH. Menopause and the risk of coronary heart disease in women. N Engl J Med. 1987;316(18):1105–10.
Basso C, Burke M, Fornes P, et al. Guidelines for post-mortem investigation investigation of sudden cardiac death. Virchows Arch. 2008;452(1):11–8.
de la Grandmaison GL. Is there progress in the post-mortem investigation diagnosis of sudden unexpected death in adults? Forensic Sci Int. 2006;156(2–3):138–44.
Ackerman MJ, Priori SG. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Heart Rhythm. 2011;8(8):1308–39.
Carturan E, Tester DJ, Brost BC, Basso C, Thiene G, Ackerman MJ. Post-mortem genetic testing for conventional post-mortem investigation-negative sudden unexplained death: an evaluation of different DNA extraction protocols and the feasibility of mutational analysis from archival paraffin-embedded heart tissue. Am J Clin Pathol. 2008;129(3):391–7.
Safranek DJ, Eisenberg MS, Larsen MP. The epidemiology of cardiac arrest in young adults. Ann Emerg Med. 1992;21(9):1102–6.
van Ingen G, van Loenen AC, Voortman M, Zweipfenning PG, Meijer CJ. Recommendations for toxicologic studies in sudden, unexpected death. Ned Tijdschr Geneeskd. 1996;140(4):179–81.
Ackerman MJ, Tester DJ, Driscoll DJ. Molecular post-mortem investigation of sudden unexplained death in the young. Am J Forensic Med Pathol. 2001;22(2):105–11.
Christiaans I, Langen IM, Wilde AA. Plotselinge dood op jonge leeftijd, de noodzaak van obductie en erfelijkheidsonderzoek. Medisch Contact. 2009;61:1253–6.
Hendriks KS, Hendriks MM, Birnie E, et al. Familial disease with a risk of sudden death: a longitudinal study of the psychological consequences of predictive testing for long QT syndrome. Heart Rhythm. 2008;5(5):719–24.
Priori SG, Barhanin J, Hauer RN, et al. Genetic and molecular basis of cardiac arrhythmias: impact on clinical management parts I and II. Circulation. 1999;99(4):518–28.
Priori SG, Napolitano C. Role of genetic analyses in cardiology: part I: mendelian diseases: cardiac channelopathies. Circulation. 2006;113(8):1130–5.
Clinical indications for genetic testing in familial sudden cardiac death syndromes: an HRUK position statement. Heart. 2008;94(4):502–7.
Lakdawala NK, Funke BH, Baxter S, et al. Genetic testing for dilated cardiomyopathy in clinical practice. J Card Fail. 2012;18(4):296–303.
Basso C, Calabrese F, Corrado D, Thiene G. Post-mortem diagnosis in sudden cardiac death victims: macroscopic, microscopic and molecular findings. Cardiovasc Res. 2001;50(2):290–300.
Sangwatanaroj S, Prechawat S, Sunsaneewitayakul B, Sitthisook S, Tosukhowong P, Tungsanga K. New electrocardiographic leads and the procainamide test for the detection of the Brugada sign in sudden unexplained death syndrome survivors and their relatives. Eur Heart J. 2001;22(24):2290–6.
Wilde AA, Pinto YM. Cost-effectiveness of genotyping in inherited arrhythmia syndromes, are we getting value for the money? Circ Arrhythmia electrophysiol. 2009;2:1–3.
Bai R, Napolitano C, Bloise R, Monteforte N, Priori SG. Yield of genetic screening in inherited cardiac channelopathies. Circ Arrhythmia Electrophysiol. 2009;2:6–15.
Thompson PD, Franklin BA, Balady GJ, et al. Exercise and acute cardiovascular events placing the risks into perspective: a scientific statement from the American Heart Association Council on nutrition, physical activity, and metabolism and the Council on Clinical Cardiology. Circulation. 2007;115(17):2358–68.
Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329(23):1677–83.
Burke AP, Farb A, Virmani R, Goodin J, Smialek JE. Sports-related and non-sports-related sudden cardiac death in young adults. Am Heart J. 1991;121(2 Pt 1):568–75.
Quigley F, Greene M, O’Connor D, Kelly F. A survey of the causes of sudden cardiac death in the under 35-year-age group. Ir Med J. 2005;98(8):232–5.
Albert CM, Mittleman MA, Chae C, Lee IM, Hennekens CH, Manson JE. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343(19):1355–61.
Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003;42(11):1959–63.
Corrado D, Pelliccia A, Bjornstad HH, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26(5):516–24.
AHA guideline, Maron et al., circulation 2015.
Viskin S. Antagonist: routine screening of all athletes prior to participation in competitive sports should be mandatory to prevent sudden cardiac death. Heart Rhythm. 2007;4(4):525–8.
Corrado D, Thiene G. Protagonist: routine screening of all athletes prior to participation in competitive sports should be mandatory to prevent sudden cardiac death. Heart Rhythm. 2007;4(4):520–4.
Maron BJ, Pelliccia A. The heart of trained athletes: cardiac remodeling and the risks of sports, including sudden death. Circulation. 2006;114(15):1633–44.
Mohlenkamp S, Lehmann N, Breuckmann F, et al. Running: the risk of coronary events: prevalence and prognostic relevance of coronary atherosclerosis in marathon runners. Eur Heart J. 2008;29(15):1903–10.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Hendrix, A., Bots, M.L., Mosterd, A. (2016). Sudden Cardiac Death in the Young; Epidemiology and Cardiogenetic Evaluation of Victims and Their Relatives. In: Baars, H., Doevendans, P., Houweling, A., van Tintelen, J. (eds) Clinical Cardiogenetics. Springer, Cham. https://doi.org/10.1007/978-3-319-44203-7_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-44203-7_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-44202-0
Online ISBN: 978-3-319-44203-7
eBook Packages: MedicineMedicine (R0)