Abstract
With the advent of long-term mechanical circulatory support devices, the need for improving outcomes in these patients has driven the technological development of percutaneous ventricular assist devices (pVADs). This chapter endeavors to review currently available devices utilized in the advanced heart failure patient population, including patient selection, advantages and disadvantages, technical considerations, and complications.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Percutaneous ventricular assist device (pVAD)
- Intra-aortic balloon pump
- Impella
- Tandem
- ECMO
- Shock
- Temporary support
1 Introduction
Percutaneous ventricular assist devices (pVADs) increasingly are being used in patients with cardiogenic shock (CS) as a bridge to recovery, decision, durable device, or cardiac transplantation [1]. By far the most common cause of CS is myocardial infarction. However, acute regurgitant valve failure, myocarditis, postcardiotomy shock, and acute or chronic heart failure also may present with end-organ dysfunction from hypoperfusion due to cardiac pump failure, the hallmark of this syndrome.
Though fibrinolytics and primary percutaneous coronary intervention (PCI) have improved mortality in patients who experience shock from acute myocardial infarction, little progress in the medical treatment of cardiogenic shock has been made over the last few decades; overall mortality remains greater than 40% [2]. The mainstay of medical treatment continues to be inotropes and vasopressors, but when used to temporize the patient hemodynamically in the short term, it actually contributes to end-organ dysfunction, arrhythmia, increased myocardial oxygen consumption, and increased mortality in the long term [3]. Frequently, they do not provide enough support to maintain adequate perfusion and hemodynamic stability. Unfortunately, once end-organ dysfunction occurs, it not only leads to increased mortality but can prevent the patient from being a candidate for advanced heart failure therapies such as durable ventricular assist devices or cardiac transplantation. In conditions where myocardial recovery is possible, medical therapy may not provide enough support to keep the patient alive and preserve end-organ function until recovery can occur.
While some pVADs have been studied for temporary support during “high-risk” PCI, there has been far less research on the role of these devices in the end-stage heart failure patient. This chapter strives to explain how these devices can be utilized in this patient population.
Currently, there are multiple percutaneous devices available for use in end-stage heart failure patients, and the choice of device or devices is dependent on multiple variables. Is RV failure, LV failure, or biventricular failure present? How much hemodynamic support is needed? Does the patient have respiratory failure, circulatory failure, or both? Does the patient have any absolute or relative contraindications for a particular device? What is the ease and rapidity of device deployment and what is the available operator’s comfort deploying the device? What is the ancillary staff’s level of comfort and experience caring for a patient with the device? What is the next step in management of the patient? The answer to each of these questions is important to determine the most appropriate device for the patient. There is no one-size-fits-all device, and there often is not a single solution to a patient conundrum.
Ultimately, all pVADs serve as a bridge to something, whether it is recovery, decision, durable device, or cardiac transplantation. If the patient has a condition at baseline that precludes them from bridging to advanced therapies or recovery, a pVAD should not be placed. A candid conversation about the possibility of failure to recover or about conditions that disqualify the patient from advanced therapies should take place with the patient and family beforehand whenever possible.
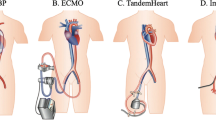
2 Intra-aortic Balloon Pump
The intra-aortic balloon pump (IABP) is the oldest and most widely used pVAD currently in use for left ventricular support. Invented in 1968, it works on the principle of counterpulsation to pressure unload the heart and, to a lesser extent, increase coronary perfusion [4,5,6]. The dual lumen catheter with a balloon at its distal end typically is inserted through the femoral artery and passed retrograde to the proximal descending aorta just distal to the ostium of the subclavian artery (◘ Fig. 29.1). It is then connected to the controller which causes the balloon to inflate and deflate with the timing of the cardiac cycle. One lumen is the channel by which the balloon is inflated, and a second lumen facilitates a guide wire for placement and transduces an aortic pressure tracing when the catheter is in place. Helium is used to inflate and deflate the balloon due to its low viscosity, allowing rapid movement of the gas into and out of the balloon. Helium is able to be more rapidly absorbed by the body in the case of balloon rupture, decreasing the chance of occurrence of a fatal air embolism. Inflation of the balloon during diastole causes both retrograde and antegrade displacement of blood, augmenting diastolic blood flow and pressure. The retrograde flow into the coronary arteries increases coronary blood flow (CBF), and the antegrade displacement increases forward flow to the body, increasing the mean arterial pressure (MAP). Rapid deflation of the balloon at the onset of ventricular systole creates suction, dropping the pressure in the aorta and thus raising forward flow. This decrease in pressure and increase in flow results in a reduction in afterload, decreased LVEDP, rise in stroke volume, and therefore cardiac output. Myocardial ischemia is reduced through multiple mechanisms including decreasing oxygen consumption by lessening ventricular wall tension and coronary microvascular resistance and improving CBF both through a rise in diastolic pressure and a drop in LVEDP. IABP has been shown to increase cardiac output by 0.5 L/min in patients with cardiogenic shock [4].
Technically, the IABP is easy to place. It requires only one arterial access, most commonly 8F, though other sizes are available. A radiopaque tip allows placement under fluoroscopy, but bedside placement with “guestimate distance” is feasible with position later confirmed by the use of a chest X-ray. An experienced operator can insert a balloon in approximately10 min. Insertion via the femoral artery prohibits ambulation, though safety and efficacy have been demonstrated with insertion through the subclavian, axillary, or brachial arteries [7]. These approaches should be performed under fluoroscopic guidance.
The IABP has some limitations. Its performance is dependent on a relatively stable electrical rhythm, intrinsic heart function, vascular tone, correct placement of the balloon in the aorta, and timing of balloon inflation and deflation. It has limited, if any, support in right ventricular failure. It should not be used in patients with more than mild aortic insufficiency as increasing diastolic retrograde flow would raise LVEDP and thus worsen their hemodynamics. Severe atherosclerosis or tortuous vessels can also be a contraindication to IABP placement. Potential complications include bleeding, infection, thrombocytopenia, limb ischemia, embolization to distal vessels including stroke, and compromise of subclavian or renal artery perfusion by forward or backward migration of the balloon. Vascular injury can occur at the entry site or at any point along the aorta including the ostia of the visceral arteries.
Earlier studies on IABP use in patients with myocardial infarction showed improved mortality or a trend toward it. The SHOCK trial demonstrated lower in-hospital mortality of patients with myocardial infarction who received IABP in addition to thrombolytic therapy or early revascularization with PCI or coronary artery bypass graft surgery [8]. GUSTO-I showed a trend toward improved 30 day and 1 year mortality in early IABP and thrombolytic therapy, although this improved mortality comes with an increased risk in bleeding [9]. Subsequent analysis of registry data showed this mortality benefit only held in patients undergoing thrombolytic therapy and not in cases of primary PCI [10]. Meta-analyses of IABP use in infarct-related cardiogenic shock cases not only showed no improvement in mortality but also demonstrated an increased risk of complications including stroke [11]. In spite of the current data, IABP is still widely used and has some class II indications in the current guidelines [12].
The challenge arises with patient selection. With its limited CO augmentation of 0.5 lpm, IABP provides little support when end-organ perfusion is impaired. It is more effective in ischemic situations or acute instability, but it rarely provides adequate support for a prolonged period of time. Thus, while helpful in the post-MI patient, it is not a good durable bridge strategy for more than a day or two. Consequently, if the recovery of end-organ function is not significant, which would reflect adequate hemodynamic support, escalation to next stage therapy is often needed. Most evaluations for transplant or LVAD cannot occur in a day, and, more often than not, the next level of support is another pVAD.
3 TandemHeart®
The TandemHeart® (CardiacAssist, Inc., Pittsburgh, PA) is a continuous-flow pVAD that works in parallel with the heart to augment cardiac output and volume unload the heart. It is FDA approved for up to 6 h of support for procedures not requiring full bypass support, though there are reports of it being in excess of 3 weeks. The TandemHeart is a magnetically driven extracorporeal centrifugal pump that indirectly unloads the LV by transferring oxygenated blood from the left atrium to the iliac arteries and perfusing the aorta retrograde. Access to the left atrium is obtained by passing a catheter to the right atrium by femoral vein access and performing a transseptal puncture and dilation to place the 21F inflow cannula (◘ Fig. 29.2). The outflow cannula is placed in the iliac artery via access of the femoral artery with either a 15F or 17F cannula. In patients with smaller femoral vessels or with peripheral vascular disease, two 12F cannulae can be placed bilaterally to decrease the potential for vascular compromise. The amount of flow can range from 2.5 to 4 L/min depending on the size of the cannulae and the speed of the pump.
The TandemHeart decreases LV preload, filling pressures, and wall stress and improves peripheral tissue perfusion. Due to its parallel circuit to the heart and its unloading distally, stroke volume is reduced, and the ventricular afterload is increased. Though myocardial oxygen demand is lowered due to lessened preload and wall stress, this increase in afterload leaves the absolute effect on myocardial oxygen consumption dependent on the hemodynamic severity of the cardiogenic shock [5, 6]. This device must be placed under fluoroscopy or with intracardiac or transesophageal echocardiographic guidance by an operator skilled in transseptal puncture, often limiting this technology to larger, tertiary centers. Aortography with runoff should be performed before placement to evaluate the iliac arteries. Placement of the device takes 30–45 min when done by an experienced operator. Systemic heparinization is required, and the device is FDA approved for the addition of an oxygenator to the circuit for gas exchange.
Contraindications to placement of the TandemHeart include right or left atrial thrombus, moderate or severe aortic insufficiency, ventricular septal defect, bleeding diathesis and coagulopathies, or significant peripheral vascular disease. Possible complications include bleeding at insertion sites, cardiac perforation and tamponade, infection, and embolic events – including stroke, limb ischemia, vascular injury, hemolysis, desaturation from migration of the left atrial cannula, or right to left shunting, paradoxical embolus, arrhythmia, or creation of an ASD from transseptal puncture.
Though studies of its use in cardiogenic shock after AMI show the TandemHeart provides more support and improves hemodynamics to a greater degree than IABP, no mortality benefit has been demonstrated [13]. In studies powered to detect mortality benefit, an increased risk of bleeding and vascular complications has been seen. Small case series demonstrated utility using the TandemHeart as a bridging device to advanced therapies such as durable device [14] and transplant and as bridge to recovery [15].
Moreover, TandemHeart has been used with limited success to provide RV support in certain clinical conditions such as isolated RV failure from RV infarct and pulmonary hypertension, in conjunction with other PVADs for biventricular failure and for temporary RV support after placement of a durable LVAD [16]. For RV support, both the inflow and outflow cannulae are placed by venous access, usually in the bilateral femoral veins. The inflow cannula is placed in the right atrium and the outflow located in the main pulmonary artery to support and offload the RV. When the distance from the femoral vein to the pulmonary artery is too long, the outflow cannula can be put in the pulmonary artery via the internal jugular. With its highly technical insertion needs, only high volume, tertiary centers are capable of maintaining the skill set necessary for proficiency. Its flexibility to potentially provide biventricular support is a plus. It does have a tendency to migrate over time, and, like all pVADs, risks of complications rise with prolonged support.
4 Impella®
The Impella Recover LP (Abiomed Inc., Danvers, MA) devices have become an increasingly popular pVAD option due to their ability to deliver a significant amount of support and their relative ease of deployment requiring only a single arterial access.
The Impella 2.5 and Impella CP are the most commonly used iterations of the Impella family of devices, and they are installed using the same platform [17, 18]. A miniature axial flow pump is mounted on a pigtail catheter, and using standard catheterization techniques, it is passed retrograde across the aortic valve and placed in the left ventricular cavity with TEE or fluoroscopic visualization (◘ Fig. 29.3). Blood is pumped from the left ventricle through the inlet into the proximal ascending aorta by continuous flow. Up to 2.5 and 3.5 L/min of flow can be delivered by the Impella 2.5 and Impella CP, respectively. The amount of flow is dependent on the size of the pump, the speed of the impeller, and the pressure gradient between the ventricle (inflow) and aorta (outflow).
The Impella 2.5 is indicated for up to 6 h of use during high-risk PCI to prevent hemodynamic instability. The Impella CP is indicated for up to 6 h for partial circulatory support in procedures not requiring cardiopulmonary bypass. Studies comparing the Impella 2.5 and Impella CP with IABP in patients in cardiogenic shock associated with AMI showed superior hemodynamics in the Impella group, but to date there is no mortality benefit [17, 18].
The Impella 5.0 operates with the same type of pump as the Impella 2.5 and CP, but due to its large size it requires a surgical cut down for catheter placement. This procedure can be performed by the CV surgeon or a vascular surgeon in conjunction with a cardiologist. The Impella 5.0 generates a larger amount of flow, up to 5 L/min, than the Impella 2.5. Though the Impella 5.0 was developed initially for femoral artery access, placement in the axillary or subclavian artery (◘ Fig. 29.4) is safe and effective in providing support with the added benefit of allowing the patient to sit in a chair, ambulate, and rehabilitate while it is in place [17, 18].
Indications for the use of the Impella 5.0 are circulatory support with no cardiopulmonary bypass or circulatory support using an extracorporeal bypass control unit for up to 6 h, but it can provide adequate support for over 45 days [17, 18]. Case studies demonstrated successful utilization of the Impella 5.0 as bridge from ECMO to durable device [19], as support in acute rejection after orthotopic heart transplantation [20], for LV support in RV failure as a bridge to RV recovery and durable LVAD [21], as bridge to recovery in myocarditis [22], and as bridge to cardiac transplantation [23]. Results from some small case series suggest survival improved in patients with severe and profound shock after ST elevation myocardial infarction with immediate Impella 5.0 treatment compared to Impella 2.5 support alone [24].
Contraindication to placement of any of the Impella LP devices includes moderate or greater aortic insufficiency, the presence of a mechanical aortic valve, aortic stenosis with valve area less than 1.5 cm2, a heart constrictive device, severe PVD that would impair the ability to place the device, or LV thrombus. The potential complications include bleeding, infection, vascular injury, hemolysis, stroke, cardiac perforation or tamponade, damage to the aortic valve, device malfunction, or arrhythmia. Hemolysis from mechanical shearing can also occur in 5–10% of patients but usually responds to device repositioning. If renal failure from persistent hemolysis occurs, the device should be removed.
Development of the Impella device greatly expanded the temporary support world for end-stage heart failure patients. With growing resistance to implanting durable VADs in the INTERMACS 1 patient, the Impella 5.0 allows adequate hemodynamic support for these patients, appropriate end-organ recovery of function, and a higher rate of success for the eventual cardiac replacement option. With the axillary implant option, these patients can also avoid the deconditioning that results from groin access mandatory bed rest restrictions. While the Impella 5.0 does require a mini-surgical approach, the single vessel access, no need to cross cardiac chambers and axillary implantation makes it poised to be the most currently balanced device for intermediate support in this patient population.
5 Extracorporeal Membrane Oxygenation (ECMO)
Extracorporeal membrane oxygenation (ECMO) offers pulmonary or cardiopulmonary support depending on its configuration. With its improved technology, it is having a “comeback” of sorts.
Venoarterial (V-A) ECMO provides both gas exchange and circulatory support through a continuous-flow pump. It is used in the setting of left ventricular or biventricular failure. In the V-A configuration, the inflow cannula is placed via a large central vein. Blood is circulated through the extracorporeal pump but is returned to the body after gas exchange through an arterial cannula. V-A ECMO can provide essentially physiologic flows up to 6 L/min without any intrinsic activity from the heart. It effectively decreases the preload of the right and left ventricles and increases MAP and end-organ perfusion, but it enhances the afterload on the left ventricle resulting in no real net change in myocardial oxygen consumption [5, 6]. The IABP or Impella devices are sometimes used concurrently with V-A ECMO for LV unloading when inotropes cannot produce enough LV contractility.
In pure pulmonary failure, veno-venous (V-V) ECMO circulates blood through an oxygenator outside of the body using a continuous-flow pump when gas exchange in the lung is impaired. The oxygenator not only oxygenates the blood but removes the waste carbon dioxide. In this configuration both the inflow cannula and the outflow cannula are placed through a venous access, sometimes even the same vein if a dual lumen catheter is used. Because blood is being removed from and returned to a vein, it offers no hemodynamic support and functions only for gas exchange in respiratory failure. The one exception to this rule is when the V-V ECMO outflow cannula is placed in the PA to provide ventricular unloading and RV support. In this case the PA cannula requires surgical placement.
V-V or V-A ECMO can be placed at the bedside without fluoroscopic guidance. The amount of flow generated is dependent on the size of the cannulae and the speed of the pump. ECMO also requires that the patient be heparinized. The degree of heparinization needed is determined by the type of oxygenator in the circuit. Management of the ECMO pump and circuit requires an experienced perfusionist, although high volume centers can appropriately train CVICU nurses to cover this responsibility. Contraindications to ECMO include severe PVD, significant aortic regurgitation, and bleeding diathesis. Potential complications include bleeding, vascular injury, limb ischemia, thromboembolic events, and pump failure. The risk of limb ischemia can be ameliorated by placement of a reperfusion cannula to provide additional blood flow to the limb distal to the cannulation site.
ECMO has resurged as a support technology for end-stage heart failure for recovery or bridge to more durable solutions. Yet the percutaneous approach is limited to groin access and all of the issues associated with prolonged bed rest. While upper vessel implantation can be done with limited surgical approaches, the durability is limited, and vascular complication rates are somewhat higher. However, unlike other technologies, it does have the ability to simultaneously support the RV and LV and provide oxygenation. Thus, when these conditions are present, it can be easier than multiple pVADs. ◘ Tables 29.1 and 29.2 summarize the comparative differences among the described devices in hemodynamics and technical issues.
6 Right Ventricular Support
Treatment of right ventricular failure in cardiogenic shock has been predominantly medical in nature. Volume administration to maintain adequate RV preload, vasodilators to reduce RV afterload, and inotropes to improve contractility are techniques that have been used for several decades. The consensus has been that if patients are able to survive their index hospitalization, their overall mortality is good. Though this remains true, the in-hospital mortality is high in patients with RV failure refractory to medical treatment. Previous options have been ECMO, surgical assist device, and atrial septostomy. Though IABP provided some support in RV infarction by increasing coronary blood flow, options for pVAD support had been extremely limited. With the development of the TandemHeart, percutaneous RVAD support has become a reality as discussed above.
More recently the Impella RP® (Right Percutaneous) was approved by the FDA under a Humanitarian Device Exemption for right ventricular failure refractory to medical therapy [25] . The device works using the same miniature axial flow pump mounted on a pigtail catheter as the Impella LP device with a few key differences. Access is obtained, again with standard catheter technique, via the right femoral vein using a series of upsizing dilators to final size of 24 FR tearaway sheath through which the pump is then inserted. It is passed through the right atrium, tricuspid valve, right ventricle, pulmonic valve, and into the pulmonary artery via a clockwise rotation of the entire device from the IVC. Once placed, the insertion sheath is torn off, and a graded smaller sheath is advanced and secured with a mattress suture. Blood travels in the opposite direction in the Impella RP; the inlet being more proximal and the outlet being more distal on the catheter. The inlet sits in the inferior vena cava where blood is aspirated and pumped into the proximal pulmonary artery (◘ Figs. 29.5 and 29.6). It provides up to 4 L/min of flow.
The RECOVER RIGHT trial was a prospective, multicenter single-arm study of patients with RV failure refractory to medical treatment after implantation of a durable LVAD, postcardiotomy or postmyocardial infarction who received RV support with Impella RP [25]. Hemodynamic benefit was observed using the Impella RP with an increase in cardiac index and a decrease in CVP both during support and after. Survival was 73% which suggested some benefit compared to prior studies, although there was no control arm to the study [25].
The Impella RP is indicated for support for up to 14 days in patients with BSA greater than or equal to 1.5 m2 who develop acute right heart failure refractory to medical therapy following LVAD implantation, MI, heart transplant, or open-heart surgery. Contraindications include severe regurgitation, stenosis, or mechanical replacement of the tricuspid or pulmonic valves, anatomic conditions that preclude placement or correct positioning of the pump including disorders of the pulmonary artery, the presence of IVC filter unless there is clear access for a 21F catheter, or the presence of thrombus in IVC/RA.
Potential complications with the use of the Impella RP include arrhythmia, bleeding, tamponade, vascular injury, hemolysis, thrombocytopenia, liver failure, device malfunction, or injury to the pulmonic or tricuspid valves. Insertion of this device requires a comfort level with percutaneous device implantation due to its rigid nature and somewhat technically challenging insertion. It can be limited by anatomy which often is not known until insertion is attempted.
7 Financial
Cost-effectiveness has increasingly become a focus in healthcare. As heart failure becomes more prevalent, the costs of taking care of heart failure patients is also steadily rising [26, 27]. Acute heart failure is one of the leading causes of hospital readmission in the USA making it a significant consumer of healthcare dollars [26]. A subset of these patients will present in cardiogenic shock and require a higher level of support than medical therapy provides. The availability of pVAD to bridge patients to recovery, durable device, transplant, or intervention gives the clinician another option at the expense of higher cost. Higher cost of an intervention over medical therapy is acceptable if it translates into survival benefit and improved quality of life at an acceptable cost-effectiveness ratio. The cost-effectiveness of pVADs is still being explored, but to date there are no randomized controlled trials in the primary PCI era demonstrating a mortality benefit of IABP over medical therapy or of pVAD (Impella 2.5 and TandemHeart) over IABP. There are no clinical trials comparing the benefit of pVADs with a higher level of support, like Impella 5.0, with IABP.
Retrospective analyses of cost comparisons of the use of IABP versus pVAD versus surgical VAD in patients have been made, the cost of IABP being the lowest and that of surgical VAD being the highest. Classification of these patients was based on coding, however, and not clinical assessment making it unknown if these were patients with similar clinical acuity [28, 29]. Large, randomized clinical trials assessing comparative outcomes in patients receiving pVADs for cardiogenic shock are needed before the cost-effectiveness of these therapies can be determined meaningfully. There is an element of common sense that can be applied. A preimplantation assessment of likelihood of recovery to next treatment should be made by the care provider. If the patient is not a candidate for advanced therapies, then implantation of these devices in an acute or chronic heart failure exacerbation may not be advisable unlike an acute event such as an MI.
8 Future
The technology of pVADs is still in its infancy. Research to develop new devices is ongoing as the industry works to make deployment easier, the size of access smaller, and the level of support greater. A potential example of this evolution is the HeartMate Percutaneous Heart Pump (St. Jude) now in clinical trials (NCT02156609). This pVAD is inserted through a single access via a 12F sheath placed in the femoral artery. The catheter is passed retrograde into the left ventricle where the distal end expands to 24F providing 4–5 L/min of flow. The impeller is caged, offering some protection to the surrounding structures. This device is now being trialed in comparison to Impella 2.5 in the high-risk PCI setting, but it has not been investigated as of yet in the more chronic heart failure situation. Additionally, a more durable pVAD that can provide support for a longer period of time allowing more time for recovery is needed.
Conclusion
Patients who present in cardiogenic shock continue to have high mortality. The utilization of pVADs for support in these critically ill patients continues to rise. Selection of an appropriate device should take into consideration the factors unique to each patient including the amount and type of support needed, the experience of the implanting center, and the presence of a potential end point including recovery, durable device, or transplant. Improvement in hemodynamic parameters has clearly been demonstrated though without mortality benefit in the limited studies to date. Early versus late implementation of support may prevent or ameliorate systemic inflammation and end-organ dysfunction in cardiogenic shock syndrome [30]. There is a clear need for randomized, prospective trials to evaluate the effect of these devices on mortality in patients with cardiogenic shock.
References
Khera R, Cram P, Lu X, Vyas A, Gerke A, Rosenthal GE et al (2015) Trends in the use of percutaneous ventricular assist devices: analysis of national inpatient sample data, 2007 through 2012. JAMA Intern Med 175(6):941–950
Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J (2009) Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation 119(9):1211–1219
Overgaard CB, Dzavik V (2008) Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation 118(10):1047–1056
Scheidt S, Wilner G, Mueller H, Summers D, Lesch M, Wolff G et al (1973) Intra-aortic balloon counterpulsation in cardiogenic shock. Report of a co-operative clinical trial. N Engl J Med 288(19):979–984
Ouweneel DM, Henriques JP (2012) Percutaneous cardiac support devices for cardiogenic shock: current indications and recommendations. Heart 98(16):1246–1254
Werdan K, Gielen S, Ebelt H, Hochman JS (2014) Mechanical circulatory support in cardiogenic shock. Eur Heart J 35(3):156–167
Cochran RP, Starkey TD, Panos AL, Kunzelman KS (2002) Ambulatory intraaortic balloon pump use as bridge to heart transplant. Ann Thorac Surg 74(3):746–751 discussion 51-2
Sanborn TA, Sleeper LA, Bates ER, Jacobs AK, Boland J, French JK et al (2000) Impact of thrombolysis, intra-aortic balloon pump counterpulsation, and their combination in cardiogenic shock complicating acute myocardial infarction: a report from the SHOCK Trial Registry. SHould we emergently revascularize Occluded Coronaries for cardiogenic shocK? J Am Coll Cardiol 36(3 Suppl A):1123–1129
Anderson RD, Ohman EM, Holmes DR Jr, Col I, Stebbins AL, Bates ER et al (1997) Use of intraaortic balloon counterpulsation in patients presenting with cardiogenic shock: observations from the GUSTO-I Study. Global Utilization of Streptokinase and TPA for Occluded Coronary Arteries. J Am Coll Cardiol 30(3):708–715
Barron HV, Every NR, Parsons LS, Angeja B, Goldberg RJ, Gore JM et al (2001) The use of intra-aortic balloon counterpulsation in patients with cardiogenic shock complicating acute myocardial infarction: data from the National Registry of Myocardial Infarction 2. Am Heart J 141(6):933–939
Sjauw KD, Engstrom AE, Vis MM, van der Schaaf RJ, Baan J Jr, Koch KT et al (2009) A systematic review and meta-analysis of intra-aortic balloon pump therapy in ST-elevation myocardial infarction: should we change the guidelines? Eur Heart J 30(4):459–468
Rihal CS, Naidu SS, Givertz MM, Szeto WY, Burke JA, Kapur NK et al (2015) 2015 SCAI/ACC/HFSA/STS clinical expert consensus statement on the use of percutaneous mechanical circulatory support devices in cardiovascular care: endorsed by the American Heart Assocation, the Cardiological Society of India, and Sociedad Latino Americana de Cardiologia Intervencion; Affirmation of Value by the Canadian Association of Interventional Cardiology-Association Canadienne de Cardiologie d’intervention. J Am Coll Cardiol 65(19):e7–e26
Burkhoff D, Cohen H, Brunckhorst C, O’Neill WW, TandemHeart IG (2006) A randomized multicenter clinical study to evaluate the safety and efficacy of the TandemHeart percutaneous ventricular assist device versus conventional therapy with intraaortic balloon pumping for treatment of cardiogenic shock. Am Heart J 152(3):469 e1-8
Bruckner BA, Jacob LP, Gregoric ID, Loyalka P, Kar B, Cohn WE et al (2008) Clinical experience with the TandemHeart percutaneous ventricular assist device as a bridge to cardiac transplantation. Tex Heart Inst J 35(4):447–450
Kar B, Adkins LE, Civitello AB, Loyalka P, Palanichamy N, Gemmato CJ et al (2006) Clinical experience with the TandemHeart percutaneous ventricular assist device. Tex Heart Inst J 33(2):111–115
Kapur NK, Paruchuri V, Korabathina R, Al-Mohammdi R, Mudd JO, Prutkin J et al (2011) Effects of a percutaneous mechanical circulatory support device for medically refractory right ventricular failure. J Heart Lung Transplant 30(12):1360–1367
Sassard T, Scalabre A, Bonnefoy E, Sanchez I, Farhat F, Jegaden O (2008) The right axillary artery approach for the Impella Recover LP 5.0 microaxial pump. Ann Thorac Surg 85(4):1468–1470
Bresson D, Sibellas F, Farhat F, Jegaden O, Kirkorian G, Bonnefoy E (2011) Preliminary experience with Impella Recover((R)) LP5.0 in nine patients with cardiogenic shock: a new circulatory support system in the intensive cardiac care unit. Arch Cardiovasc Dis 104(8–9):458–464
Hollander SA, Reinhartz O, Chin C, Yeh J, Maeda K, Mallidi H et al (2012) Use of the Impella 5.0 as a bridge from ECMO to implantation of the HeartMate II left ventricular assist device in a pediatric patient. Pediatr Transplant 16(2):205–206
Samoukovic G, Al-Atassi T, Rosu C, Giannetti N, Cecere R (2009) Successful treatment of heart failure due to acute transplant rejection with the Impella LP 5.0. Ann Thorac Surg 88(1):271–273
Samoukovic G, Rosu C, Giannetti N, Cecere R (2009) The Impella LP 5.0 as a bridge to long-term circulatory support. Interact Cardiovasc Thorac Surg 8(6):682–683
Andrade JG, Al-Saloos H, Jeewa A, Sandor GG, Cheung A (2010) Facilitated cardiac recovery in fulminant myocarditis: pediatric use of the Impella LP 5.0 pump. J Heart Lung Transplant 29(1):96–97
LaRocca GM, Shimbo D, Rodriguez CJ, Stewart A, Naka Y, Weinberger J et al (2006) The Impella Recover LP 5.0 left ventricular assist device: a bridge to coronary artery bypass grafting and cardiac transplantation. J Am Soc Echocardiogr 19(4):468 e5-7
Engstrom AE, Cocchieri R, Driessen AH, Sjauw KD, Vis MM, Baan J et al (2011) The Impella 2.5 and 5.0 devices for ST-elevation myocardial infarction patients presenting with severe and profound cardiogenic shock: the Academic Medical Center intensive care unit experience. Crit Care Med 39(9):2072–2079
Samuels L (2015) The RECOVER RIGHT™ trial: use of the Impella RP percutaneous right ventricular assist device: an Hde study. 5th international conference on clinical & experimental cardiology; April 27–29, 2015. Philadelphia, USA, J Clin Exp Cardiol 6:4
Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC et al (2013) Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 6(3):606–619
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M et al (2015) Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation 131(4):e29–322
Gregory D, Scotti DJ, de Lissovoy G, Palacios I, Dixon S, Maini B et al (2013) A value-based analysis of hemodynamic support strategies for high-risk heart failure patients undergoing a percutaneous coronary intervention. Am Health Drug Benefits 6(2):88–99
Shah AP, Retzer EM, Nathan S, Paul JD, Friant J, Dill KE et al (2015) Clinical and economic effectiveness of percutaneous ventricular assist devices for high-risk patients undergoing percutaneous coronary intervention. J Invasive Cardiol 27(3):148–154
Chen JM, DeRose JJ, Slater JP, Spanier TB, Dewey TM, Catanese KA et al (1999) Improved survival rates support left ventricular assist device implantation early after myocardial infarction. J Am Coll Cardiol 33(7):1903–1908
Acknowledgments
We wish to thank Suneet Flora for her contributions in our literature search.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sherwood, M., Hall, S.A. (2017). Percutaneous Devices: Options. In: Montalto, A., Loforte, A., Musumeci, F., Krabatsch, T., Slaughter, M. (eds) Mechanical Circulatory Support in End-Stage Heart Failure. Springer, Cham. https://doi.org/10.1007/978-3-319-43383-7_29
Download citation
DOI: https://doi.org/10.1007/978-3-319-43383-7_29
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43381-3
Online ISBN: 978-3-319-43383-7
eBook Packages: MedicineMedicine (R0)