Abstract
The characteristic effects of ageing observed across the human lifespan are accompanied by a multitude of molecular changes. These age-related changes are a result of the complex interaction between our genetic makeup, lifestyle factors, and unique environments. People are subject to a variety of different exposures; many of these influences have the potential to “mark” our DNA and actually alter our cellular processes. This is a key component of epigenetics: a field that focuses on modifications to DNA and DNA packaging that function without altering the genetic sequence itself. DNA methylation is arguably the most well-characterized epigenetic modification, involving the addition of a methyl group to DNA, which, in an interesting paradox, is both stable long-term as well as plastic and reversible. DNA methylation fluctuates throughout the lifespan of mammalian organisms and has the potential to influence cellular processes through changes in gene expression. An important role of DNA methylation is as a molecular mediator between environmental exposures and physiological changes, which makes it a likely modifier of the immune system. In regards to the ageing process, the actual function of DNA methylation is unknown; however, global trends and site-specific changes in DNA methylation have been strongly correlated with chronological age. Here, we will discuss the particulars of epigenetics, with a focus on DNA methylation and its role in the development, maturation, dysfunction, and ageing of white blood cells of the immune system.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Epigenetics
- DNA methylation
- Epigenetic Drift
- Epigenetic Clock
- Age Acceleration
- Biological Age
- Blood
- Immune system
- Environment
- Ageing
3.1 Introduction
Epigenetics is a rapidly emerging field investigating the interface between our genomes and our environments. Epigenetic mechanisms are responsible for the structural organization of DNA and its packaging proteins; one major function of which is to regulate gene expression by controlling DNA accessibility. While the genetic sequence is unaltered, these structural changes act as a regulatory stratum on the genome, instructing cellular identity and driving important cellular processes. Current characterized epigenetic marks include post-translational modifications to histone proteins, such as acetylation and methylation, histone variants, non-coding RNAs, and chemical modifications covalently bound directly to DNA. The latter include DNA methylation, the most commonly studied epigenetic mark, especially in human populations, which refers to the covalent attachment of a methyl group primarily to the 5′carbon of cytosine bases [1]. This chapter will briefly review DNA methylation, then examine the role of DNA methylation in three important areas: cell type specification, environmental embedding, and disease; using examples from the immune system. We will then discuss the interesting connections between DNA methylation and ageing, and conclude with emerging hypotheses on how this might influence ageing of the immune system.
3.2 DNA Methylation
DNA methylation is found primarily at cytosine bases adjacent to guanine bases, referred to as a cytosine-phosphate-guanine dinucleotides (CpGs ). Non-CpG DNA methylation has also been observed in some tissues, but will not be discussed here in detail [2]. The process of DNA methylation is catalyzed by a family of highly conserved enzymes called DNA methyltransferases (DNMTs) . In mammals, there are three principal DNMTs: the de novo methyltransferases , DNMT3A and DNMT3B , add methyl groups to unmethylated DNA, while DNMT1 is responsible for the maintenance of DNA methylation at hemi-methylated sites during cell division [3]. Until recently, the removal of DNA methylation marks was highly puzzling, as there was evidence for active demethylation, but the enzymes and process responsible remained elusive. In the past few years, new discoveries have shown that DNA demethylation is primarily controlled by 10–11 translocation methylcytosine dioxygenase (TET) enzymes, which catalyze the first step in active demethylation through the base excision repair system [1, 3, 4].
DNA methylation is highly genomic region-specific, partly because CpGs themselves are non-randomly distributed across the genome. CpGs are globally under-represented in genomic sequences, but are enriched in regions called CpG islands: sequences that possess higher than average CpG density and are generally lowly methylated. Interestingly, CpGs are also very dense at many repetitive elements, therefore such high density regions tend to be methylated and silenced to avoid transposition [5, 6]. Nearly 70 % of gene promoters are near a CpG island, and this proximity results in an important relationship between promoter DNA methylation and gene expression [7]. Early models of this relationship posited that high levels of DNA methylation at promoter-associated CpG islands were associated with low levels of expression, and vice versa [8–10] (Fig. 3.1). However, this model is relatively simplistic and we are now beginning to understand that the relationship is much more complex [11–13]. For instance, reverse causation is possible and gene expression levels can influence levels of DNA methylation [12, 14]. In addition, DNA methylation marks in genomic locations other than promoters have equally importance and, in some cases, very different associations with gene expression [12]. For example, both regions of low CpG density directly adjacent to CpG islands, known as “island shores ”, and enhancer regions do not follow the high DNA methylation/low gene expression model. In island shores, higher levels of DNA methylation are often associated with high levels of gene expression, while at enhancers these relationships have been inconsistent and thus far are poorly understood [1, 5–7, 14, 15].
DNA methylation patterns at promoter-associated CpG islands and gene bodies in active (above) and inactive (below) genes. Each gene indicates exons (black), introns (white), CpG islands (dark grey) and shores (light grey). Below each gene the drawing indicates where DNA methylation is high or low across the gene
The underlying genetic sequence can also influence both gene expression and DNA methylation. Reminiscent of earlier work examining the linkage of allelic variation and gene expression, multiple studies have identified SNP/CpG pairs at which genotype is associated with methylation level [8–10, 12, 16–18]. These CpG sites are referred to as methylation quantitative trait loci (mQTLs) , and a number of different mechanisms have been hypothesized for their function. For example, the SNP partner may disrupt genetic elements responsible for creating boundaries between methylated and unmethylated genomic regions [11–13, 19]. Alternatively, sequence changes may alter gene expression levels, which in turn influence DNA methylation levels [14]. Regardless of the mechanism by which this relationship functions, it is very important to consider genetic regulation in the analysis of DNA methylation effects.
Finally, the relationships between DNA methylation, genotype, and gene expression are dynamic and may change over the life span. For example, it appears that genotype-DNA methylation correlations are susceptible to age-related differences. From early to later life, more than half of the associations between genotype and DNA methylation change [20]. Conversely, correlations between DNA methylation and gene expression appear to be more consistent over the ageing process [21]. Continuing research is required to understand the entire complexity of the role of DNA methylation in genetic regulation across the lifespan.
3.2.1 DNA Methylation and Cell Type Specification
DNA methylation plays a central role in embryogenesis, and this importance continues throughout development [1]. In the immune system, for example, maintenance of DNA methylation patterns is required for hematopoietic stem cell self-renewal and differentiation [22]. During hematopoietic stem cell differentiation, DNA methylation gains and losses at specific regions of the genome “lock-in” differentiation marks that allow cells with the same genetic material to express only the specific genes required for their unique cellular processes and identities [23]. This is illustrated by the lineage-specific epigenetic differences that arise when early multipotent progenitors split into myeloerythroid and lymphoid lineages; these patterns become more specific as differentiation progresses, resulting in cell type specific DNA methylation signatures in mature cells [24–28] (Fig. 3.2). Hematopoietic stem cells lacking the maintenance methyltransferase prematurely lose their self-renewal capabilities, and cells lacking de novo methyltransferases show impaired lineage commitment, illustrating that these DNA methylation changes are essential for lineage development [29, 30].
Representation of changes in DNA methylation during hematopoietic stem cell differentiation. Gain and loss of DNA methylation at lineage-specific genomic regions confers cell-type specificity. Methylation patterns become more unique as differentiation progresses. The shaded boxes represent DNA methylation at specific regions of the genome. For example, the black-shaded box in the hematopoietic stem cell represents DNA methylation levels at genes that enable pluripotency. This mark is slowly lost as the cell becomes more differentiated, and marks of specific cell types arise
Because of these cell type specific DNA methylation patterns, cell and tissue types are the largest determinants of DNA methylation variation in healthy individuals [31–33]. It is important to note that these differences in cell type DNA methylation patterns can create at least two major challenges for studies examining the role of DNA methylation in organs or tissues composed of multiple cell types: inter-individual variation in cell types and the concordance between central and surrogate tissues . First, inter-individual cell type differences within a tissue can induce confounding effects that may mask or overwhelm another biological signal with a smaller effect size. In blood, for example, it is essential to control for differences in white blood cell composition between individuals. When cell count information is not available, DNA methylation patterns can be used to predict the underlying cellular composition in order to control for it [28, 34]. This tool is particularly important when studying the relationship between DNA methylation and age in blood tissue, as it has been shown that white blood cell composition changes drastically with age, and that failing to control for these changes can result in white blood cell DNA methylation lineage markers being mistaken for age-associated DNA methylation sites [35]. In regards to tissues other than blood, similar predictive models exist for neurons versus glia in the brain, and other methods exist that can control for cell type differences without specifically predicting underlying cell composition [36–38]. The second challenge presented by cell type specific DNA methylation patterns arises when studying surrogate tissues. In human studies, tissues of interest are often inaccessible or require invasive collection methods. To address this, easily collected surrogate tissues, such as blood or cheek swabs, are substituted. However, given the tissue specificity of DNA methylation, it can be challenging to make biological interpretations of function in the tissue of interest when using these alternatives. Ongoing research into the concordance of DNA methylation between tissues collected post-mortem, such as brain and blood, is making the study of surrogate tissues increasingly more interpretable and valuable [33, 39, 40].
3.2.2 DNA Methylation and Environmental Exposures
Complementing its role in cell type specification, DNA methylation is also emerging as a mechanism by which cells “remember” past exposures. Although DNA methylation is stable in that it is generally faithfully transmitted from mother to daughter cells, paradoxically it also appears to be malleable in response to exposures and experiences [41–43]. Researchers have examined environmentally-induced changes in DNA methylation in both gene-specific contexts as well as genome-wide changes, such as average methylation across repetitive elements [44, 45]. These changes may be transient and revert back to their original state after the exposure ends, but in some cases they can remain associated long after the exposure has passed [46]. It is currently hypothesized that early life is a particularly sensitive time for the long-term embedding of epigenetic signatures of exposures, but in many cases it is not until later in life that health outcomes associated with these exposures are revealed. As such, the environmental exposures that accumulate as a person ages can leave behind a biological residue that might influence long-term health.
Some specific environmental exposures have been associated with long-lasting DNA methylation signatures that persist after the exposure itself. For example, a number of DNA methylation changes are strongly associated with previous and current cigarette smoke exposure[47, 48]. The cigarette smoke-related DNA methylation change in the promoter of a well-characterized tumor suppressor gene , aryl hydrocarbon receptor repressor (AHRR) , is currently the best replicated environmentally induced epigenetic alteration. In the AHRR gene, changes in both DNA methylation and gene expression have been observed upon exposure to firsthand and secondhand cigarette smoke , as well as prenatal exposure to maternal smoking [47]. The AHRR protein regulates an enzyme responsible for binding nicotine, thus supporting a plausible mechanism for a DNA methylation response to cigarette smoke exposure.
Lifestyle and the environment can have important effects on DNA methylation, which in turn, may influence immune function, as described in two recent studies. One study examined DNA methylation in African populations with recent divergence in habitat and lifestyle. The study found that a population which had recently diverged into two different habitats, forest versus urban, showed distinct DNA methylation differences between the groups, which were enriched for genes involved in immune function [49]. Another study examined adolescents raised in the American Midwest and compared those who spent the first few years of their lives in Eastern European orphanages to those who were born and raised in their biological families in the US. A significant difference in the ratio of CD4+ T to CD8+ T cells was found in their blood. As well, a DNA methylation pattern unique to the adopted children was enriched for genes involved in development, gene regulation, and behaviour [50]. Together, these examples suggest that the immune system may use DNA methylation as a way to adapt to the environment.
An equally intriguing example of exposure related DNA methylation changes is the reported epigenetic connection between early life adversity and regulation of the inflammatory response in later life. One study examining the association between DNA methylation and early life socioeconomic status (SES) found that while DNA methylation was associated with early life SES, this association was only visible after correction for white blood cell type, reinforcing the evidence for an interaction between DNA methylation and blood cell lineages [11]. Other studies have shown alterations in gene expression and DNA methylation of immune-related genes in adulthood that are associated with low socioeconomic status in childhood [51, 52]. Further work will determine whether this biological signature from early life influences the trajectories of immune ageing.
It is possible that the establishment of these DNA methylation patterns in response to environmental exposures serve to predict future phenotype, including immune responses. For example, pre-stimulation DNA methylation differences in leukocytes can predict their cytokine responses when stimulated through the TLR pathway [11]. As the variability in these baseline patterns was representative of the differences in lifetime environmental exposures between the cells, DNA methylation may function both as a memory of past exposures as well as a predictor of future immune response.
3.2.3 DNA Methylation and Disease
The etiologies of complex diseases are particularly challenging to decode as they often have both environmental and genetic contributors. As DNA methylation has a role in the interface between the genome and the environment, it has been investigated as a mediator between environmental exposure and disease manifestation. DNA methylation could be associated with current or future disease, either mechanistically or as a biomarker. In terms of mechanism, DNA methylation could influence the development of disease via moderation of a genetic risk or embedding of a past environmental exposure, for example. Concurrent disease-related changes in DNA methylation or patterns that predict future disease that do not have an identified mechanistic link to the disease may be biomarkers that could be used for patient stratification or assessment of intervention. Here, examples from the immune system illustrate some of the recent findings connecting DNA methylation and disease.
A number of immune diseases have recently been investigated for epigenetic mediation of genetic risk, in which DNA methylation of immune-related genes alters the penetrance of a risk allele. Investigations of rheumatoid arthritis and peanut allergy have both shown evidence that DNA methylation of the major histocompatibility complex (MHC) in combination with genetic factors alters risk of disease development [53, 54]. The source of the variation in DNA methylation is not known for either of these diseases, but possibilities include stochastic changes or embedded environmental signatures. Future work on the MHC region will be required to elucidate whether environmental exposures alter DNA methylation in that area, as well as whether these can be mitigated to alter disease trajectory.
One of the first autoimmune diseases predicted to have an epigenetic contribution was systemic lupus erythematosus . Potential environmental contributions have led researchers to examine DNA methylation patterns to determine whether genes involved in the production of anti-nuclear antibodies are differentially methylated in lupus patients [55]. In a study examining multiple white blood cell types, abnormally low DNA methylation was observed near interferon-related genes, in both active and quiescent lupus [56]. This implies that the DNA methylation changes are not associated with disease flare-ups, but rather reflect a basal difference in DNA methylation in patients with lupus regardless of their disease status, which may be indicative of molecular “poising” awaiting a specific trigger. The clinical implications of these findings include potential targets for interventions to reduce the active lupus symptoms, or as biomarkers of those who may be at risk for a flare-up.
Other immune diseases show specific patterns of DNA methylation dysregulation, but the mechanistic contribution of DNA methylation is currently not understood. Differences in DNA methylation and gene expression in leukocytes have recently been found between twins discordant for two autoimmune diseases which show generally low concordance: psoriasis and Type 1 diabetes [57, 58]. DNA methylation dysregulation has also been observed in synovial cells of patients with rheumatoid arthritis [59].
DNA methylation has also been identified as a factor involved in microbial infection with two distinct relationships; in some cases it is associated with immune adaptation and in others it is associated with facilitating intracellular parasitic infection. For example, epigenetic remodeling was observed in monocyte-derived dendritic cells in response to Mycobacterium tuberculosis , the primary cause of tuberculosis in humans. Infected cells showed DNA methylation changes that altered the regulation of immune transcription factors in a way that contributed to a short-term memory of infection in innate immune cells [60]. Another study demonstrated numerous DNA methylation changes in a macrophage cell line were associated with Leishmania donovani infection. Many of these changes were associated with host immune defense pathways such as the AK/STAT signaling pathway and the MAPK signaling pathway [61]. On the other hand, Anaplasma phagocytophilum , a prokaryotic pathogen, has been shown to elicit epigenetic changes in human neutrophils that promote infection by enabling pathogen survival and replication [62]. These results highlight an interesting branch of immune epigenetics, showcasing the complex roles DNA methylation has in the process of microbial infection.
In all of these cases, it is not yet known whether the DNA methylation changes observed are a mechanism of disease development or a concurrent biomarker of disease. Regardless of the origin of these changes, they raise the tantalizing possibility that epigenetics in general and DNA methylation in particular may be a new frontier for research into the development of complex immune diseases and phenotypes.
3.3 DNA Methylation and Ageing
Aside from the aforementioned associations of DNA methylation, recent work has shown that DNA methylation also exhibits strong correlations with age, the function of which is not yet known. Since genetic sequence accounts for less than 30 % of lifespan variation, the major driver of human longevity must be attributed to non-genetic factors such as diet, physical activity, smoking and other exposures [63, 64]. Alterations in DNA methylation may occur as a result of the combination of programmed changes in cell type or function with age, the embedding of lifelong environmental exposures, and possible stochastic events over time. Given the combination of evidence that DNA methylation is involved in the embedding of past environments and the development of disease, and that the human methylome is age-sensitive, it seems likely that DNA methylation may have a functional role in ageing. An emerging possible functional role of these age-related epigenetic changes may, in part, play into the molecular pathway responsible for the decline in immune dysfunction observed with age [65]. Over the past years, work has focused on determining the relative contribution of specific environments and stochastic changes in altering DNA methylation patterns during ageing.
3.3.1 Genome-Wide DNA Methylation Ageing Trends
While the link between DNA methylation and ageing has been studied over a long period of time, recent findings and advances have sharpened the focus on the role of DNA methylation in the ageing process. Early studies began assessing the relationship of age and DNA methylation patterns over 40 years ago, using techniques such as liquid chromatography to assess bulk mean methylation levels in salmon, rodent, cattle, and chicken [66, 67]. A pioneering study showed a significant loss of total DNA methylation over the rodent life course across a number of tissues, a finding that was later validated in blood from a cross sectional human cohort consisting of both newborns and centenarians [68, 69]. These explorations laid the foundation for human DNA methylation ageing studies, and as technology continues to advance, allowing easier access to the entire methylome, we enter an exciting era of epigenetic ageing research.
It is estimated that one-third of the epigenome’s DNA methylation content changes in association with the ageing process, and recent advances have helped further elucidate the context and potential function of these changes. For example, the previously mentioned finding that DNA exhibits a gradual loss of mean methylation over time has recently been shown to occur in a genomic context-specific manner. Loss of methylation preferentially occurs at regions of low CpG density, often located within a gene body [69]. Despite the fact that mean DNA methylation decreases with age, there are specific age-related methylation changes that involve a gain in methylation as well. These tend to be found within CpG islands, or areas of high CpG density [70, 71]. Together, these changes demonstrate a regression to the mean pattern—low CpG density regions, which are normally highly methylated lose DNA methylation with age, while high density regions which tend to have low levels of DNA methylation gain DNA methylation with age. Since most CpGs in the genome are methylated, this translates to a global loss of DNA methylation. An interesting exception to this pattern is repetitive elements, which tend to be highly methylated and lose DNA methylation with age, despite their high CpG density [72].
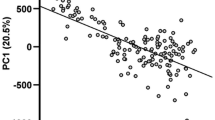
Clearly, the relationship between DNA methylation and age is highly complex, with specific patterns occurring at unique genetic regions. A host of research explorations including animal models, human longitudinal twin studies and age-variable cohorts, have all contributed to identifying DNA methylation patterns with age. From the combination of these research findings, it is evident that two common trends of epigenetic aging have emerged: (1) random changes to DNA methylation that are inconsistent across individuals, and (2) predictable, site-specific DNA methylation changes occurring in a similar way across individuals with age [73, 74] (Fig. 3.3).
Epigenetic drift results in divergent DNA methylation patterns with increasing age. In early life (left), identical twins have highly similar epigenetic patterns (individuals A and B), while individual C is distinct. Later in life (right), all individuals are more discordant, as epigenetic drift has altered lowly-methylated CpGs (lighter) to be more methylated, and higher-methylated CpGs (darker) to be less methylated
3.3.2 Epigenetic Drift
One repeatedly observed feature of age-associated DNA methylation is an increase in variability, resulting from changes in DNA methylation that do not share a common direction (gain or loss) across individuals. These age-related changes are collectively referred to as epigenetic drift, a trend composed of non-directional DNA methylation changes that may be due to stochastic or environmental factors [73–75]. Epigenetic drift accounts for the increasing degree of inter-individual variation across the DNA methylome that occurs with age [76]. This was well-illustrated in an early study of monozygotic twins, which found that at infancy twin pairs possessed almost indistinguishable methylation profiles, while older twin pairs had highly divergent methylomes [77]. The increased inter-individual variability of DNA methylation with age is also reflected in increased variability in transcriptional regulation [78]. Epigenetic drift may not be benign, as variability in DNA methylation has been suggested to increase the risk for diseases such as depression [79]. The source of this increase in variability is still unknown and may represent random DNA methylation events, or an age-associated decline in efficiency of the machinery responsible for maintaining DNA methylation [78, 80]. Others have proposed that an individual’s unique combination of lifelong environments and experiences may create differences in cellular processes that in turn lead to higher variability in DNA methylation over time [81]. Regardless of its cause, the phenomenon of epigenetic drift is interesting, as it may lead to differential cellular functioning and diverse health outcomes possibly reflected in varying ageing rates.
3.3.3 Epigenetic Clock
In contrast to epigenetic drift, there are CpGs in the genome that are highly associated with age across individuals throughout the life course. These sites follow the same age-related trajectories as epigenetic drift, in which sites that are lowly methylated gain DNA methylation and sites that are highly methylated lose DNA methylation with age [78, 82, 83]. The major difference is that the specific sites that change with age and the direction of that change is consistent across individuals [73]. These sites are in current investigation to determine why they show this consistent relationship, and recently have been used to construct multivariate age predictors, giving rise to the concept of the “epigenetic clock ” [78, 82–85] (Fig. 3.4). Several epigenetic clocks have been created to predict biological age within a specific tissue or even across multiple tissues [36, 78, 83, 85]. The current most commonly used age-predictor analyzed over 8000 samples from 51 different cell types to identify 353 sites capable of predicting age with a mean error of 3.6 years [85]. The high correlation between estimated epigenetic age and chronological age supports DNA methylation as a strong biological age predictor.
3.4 Epigenetic Age: A Molecular Marker of Biological Wellbeing?
The widespread application of epigenetic age prediction has shown very high concordance between chronological age and predicted age; however, some individuals show large discrepancies between the two. These efforts have sparked a profusion of studies focused on determining the relationship between lifelong environmental exposures, biological age as measured by the epigenetic clock, and the presence of health and disease during aging.
Recent findings have shown epigenetic age acceleration in a number of diseases and disorders, though few studies have been able to determine whether this acceleration preceded, was concurrent with, or followed disease manifestation in late-onset diseases. For example, neurodegenerative disorders, such as a decline in cognitive function, episodic memory, and working memory, as well as neuropathological measures, such as diffuse and neurotic plaques and amyloid load have been associated with epigenetic age acceleration [86]. In addition, individuals with Down Syndrome , which has been associated with early cognitive decline, have an average epigenetic age 6.6 years older than their chronological age [87]. There have been many other studies showcasing deviations in the relationship between epigenetic age and chronological age in diseases such as Schizophrenia , PTSD , Parkinson’s Disease , and HIV [88–92]. In one case, however, researchers were able to show an association between lung cancer incidence and increased epigenetic age acceleration prior to diagnosis [93]. Together, these studies show there are particular diseases or disorders that associate with increased biological age, a relationship consistent with the toll diseases take on human health.
The connection between accelerated epigenetic age and poor health is further reinforced by work analyzing the association between epigenetic age acceleration and all-cause mortality. A longitudinal study found that an epigenetic age more than 5 years older than one’s chronological age was associated with a 21 % increased mortality rate [94]. The heritability of age acceleration, the degree to which is attributed to genetic composition, was also assessed in a parent-offspring cohort and revealed that approximately 40 % of the variation in age acceleration is due to genetic factors [94]. These results show that although a significant proportion of age-related methylation changes may be under a strong genetic influence, there is an even larger unknown non-genetic contribution to the variation in these events. These findings provided one of the first links between DNA methylation- predicted age and mortality, highlighting the potential clinical relevance of age-related DNA methylation.
More recently, another study investigated associations between epigenetic age and mortality in a cohort of 378 Danish twins, aged 30–82 years old. Upon resampling the 86 oldest twins in a 10-year follow-up, a mean 35 % higher mortality risk was associated with each 5-year increase in epigenetic age. Interestingly, through a separate intra-pair twin analysis, a 3.2 times greater risk for mortality per 5-year epigenetic age difference within twin pairs was observed for the epigenetically older twin, after controlling for familial factors [95]. This highlights, again, the link between mortality and DNA methylation-predicted age, exemplifying the capacity of DNA methylation to discriminate between biologically younger or older individuals independent of genetic sequence.
The described relationships, where the presence of disease is associated with acceleration in DNA methylation age, which in turn is associated with mortality, are highly suggestive that epigenetic age may be an excellent biomarker of human health. Future work will determine whether acceleration in biological ageing is reversible, and what factors might be involved in modifying the progression of ageing.
3.5 Concluding Remarks
The research highlighted throughout this chapter has only briefly summarized an exceptional amount of work that has contributed to our understanding of the roles DNA methylation plays in health and ageing. It is becoming increasingly evident that DNA methylation functions as the interface of genetic sequence, environmental exposures, and phenotypic outcomes. Thus, it is tempting to speculate that this critical epigenetic mark can be extremely useful to our understanding of health, either through functional contributions or as biomarkers of human phenotypes and diseases.
Although there is an indisputable association between DNA methylation and chronological age throughout the entirety of life, even to the point of developing extremely accurate DNA methylation-based age predictors, it is still not clear what functional role DNA methylation plays in the ageing process. One possible scenario is that epigenetic drift may represent embedding of unique environmental exposures across the lifetime, resulting in increased divergence of DNA methylation profiles with age. Under this model, sites that correlate linearly with chronological age, such as those used for epigenetic clocks, may represent markers of biological ageing and give a molecular insight into the ageing process. On the other hand, it is also possible that age-associated DNA methylation changes do not have a functional component. Under this assumption, epigenetic drift may not reflect environments, but random changes with time, and the epigenetic clock may simply represent those regions of the genome which are more susceptible to age-related changes across individuals [96]. However, the finding that epigenetic age acceleration is correlated with mortality and disease suggests a specific role for common epigenetic changes with age, and further research is needed to clarify its functional relevance.
Despite our gaps in understanding the mechanistic function of DNA methylation in immunity and ageing, it is apparent that methylation is associated with events and exposures that shape an individual’s lifelong health. The further we explore these associations, the more it becomes clear that DNA methylation has a significant position in the complex process of ageing and age-related diseases.
References
Jones PA. Functions of DNA methylation: islands, start sites, gene bodies and beyond. Nat Rev Genet. 2012;13(7):484–92.
Ziller MJ, Müller F, Liao J, Zhang Y, Gu H, Bock C, et al. Genomic distribution and inter-sample variation of non-CpG methylation across human cell types. PLoS Genet. 2011;7(12), e1002389.
Smith ZD, Meissner A. DNA methylation: roles in mammalian development. Nat Rev Genet. 2013;14(3):204–20.
He Y-F, Li B-Z, Li Z, Liu P, Wang Y, Tang Q, et al. Tet-mediated formation of 5-carboxylcytosine and its excision by TDG in mammalian DNA. Science. 2011;333(6047):1303–7.
Kochanek S, Renz D, Doerfler W. DNA methylation in the Alu sequences of diploid and haploid primary human cells. EMBO J. 1993;12(3):1141–51.
Alves G, Tatro A, Fanning T. Differential methylation of human LINE-1 retrotransposons in malignant cells. Gene. 1996;176(1-2):39–44.
Weber M, Hellmann I, Stadler MB, Ramos L, Pääbo S, Rebhan M, et al. Distribution, silencing potential and evolutionary impact of promoter DNA methylation in the human genome. Nat Genet. 2007;39(4):457–66.
Kass SU, Landsberger N, Wolffe AP. DNA methylation directs a time dependent repression of transcription initiation. Curr Biol. 1997;7(3):157–65.
Jones PA. The DNA, methylation paradox. Trends Genet. 1999;15(1):34–7.
Bell JT, Pai AA, Pickrell JK, Gaffney DJ, Pique-Regi R, Degner JF, et al. DNA methylation patterns associate with genetic and gene expression variation in HapMap cell lines. Genome Biol. 2011;12(1):R10.
Lam LL, Emberly E, Fraser HB, Neumann SM, Chen E, Miller GE, et al. Factors underlying variable DNA methylation in a human community cohort. Proc Natl Acad Sci U S A. 2012;109 Suppl 2:17253–60.
Gutierrez Arcelus M, Lappalainen T, Montgomery SB, Buil A, Ongen H, Yurovsky A, et al. Passive and active DNA methylation and the interplay with genetic variation in gene regulation. Elife. 2013;2, e00523.
Jones MJ, Fejes AP, Kobor MS. DNA methylation, genotype and gene expression: who is driving and who is along for the ride? Genome Biol. 2013;14(7):126.
Wagner JR, Busche S, Ge B, Kwan T, Pastinen T, Blanchette M. The relationship between DNA methylation, genetic and expression inter-individual variation in untransformed human fibroblasts. Genome Biol. 2014;15(2):R37.
Edgar R, Tan PPC, Portales-Casamar E, Pavlidis P. Meta-analysis of human methylomes reveals stably methylated sequences surrounding CpG islands associated with high gene expression. Epigenetics Chromatin. 2014;7(1):28.
Zhang H, Wang F, Kranzler HR, Yang C, Xu H, Wang Z, et al. Identification of methylation quantitative trait loci (mQTLs) influencing promoter DNA methylation of alcohol dependence risk genes. Hum Genet. 2014;133(9):1093–104.
Banovich NE, Lan X, McVicker G, van de Geijn B, Degner JF, Blischak JD, et al. Methylation QTLs are associated with coordinated changes in transcription factor binding, histone modifications, and gene expression levels. PLoS Genet. 2014;10(9), e1004663.
Fraser HB, Lam LL, Neumann SM, Kobor MS. Population-specificity of human DNA methylation. Genome Biol. 2012;13(2):R8.
Maurano MT, Wang H, John S, Shafer A, Canfield T, Lee K, et al. Role of DNA methylation in modulating transcription factor occupancy. Cell Rep. 2015;12(7):1184–95.
Smith AK, Kilaru V, Kocak M, Almli LM, Mercer KB, Ressler KJ, et al. Methylation quantitative trait loci (meQTLs) are consistently detected across ancestry, developmental stage, and tissue type. BMC Genomics. 2014;15:145.
Peters MJ, Joehanes R, Pilling LC, Schurmann C, Conneely KN, Powell J, et al. The transcriptional landscape of age in human peripheral blood. Nat Commun. 2015;6:8570.
Trowbridge JJ, Snow JW, Kim J, Orkin SH. DNA methyltransferase 1 is essential for and uniquely regulates hematopoietic stem and progenitor cells. Cell Stem Cell. 2009;5(4):442–9.
Meissner A. Epigenetic modifications in pluripotent and differentiated cells. Nat Biotechnol. 2010;28(10):1079–88. doi:10.1038/nbt.1684. http://www.nature.com/doifinder.
Calvanese V, Fernandez AF, Urdinguio RG, Suarez-Alvarez B, Mangas C, Pérez-García V, et al. A promoter DNA demethylation landscape of human hematopoietic differentiation. Nucleic Acids Res. 2012;40(1):116–31.
Suarez-Alvarez B, Rodriguez RM, Fraga MF, López-Larrea C. DNA methylation: a promising landscape for immune system-related diseases. Trends Genet. 2012;28(10):506–14.
Álvarez-Errico D, Vento-Tormo R, Sieweke M, Ballestar E. Epigenetic control of myeloid cell differentiation, identity and function. Nat Rev Immunol. 2014;15(1):7–17.
Reinius LE, Acevedo N, Joerink M, Pershagen G, Dahlen S-E, Greco D, et al. Differential DNA methylation in purified human blood cells: implications for cell lineage and studies on disease susceptibility. PLoS One. 2012;7(7), e41361.
Houseman EA, Accomando WP, Koestler DC, Christensen BC, Marsit CJ, Nelson HH, et al. DNA methylation arrays as surrogate measures of cell mixture distribution. BMC Bioinformatics. 2012;13:86.
Challen GA, Sun D, Mayle A, Jeong M, Luo M, Rodriguez B, et al. Dnmt3a and Dnmt3b have overlapping and distinct functions in hematopoietic stem cells. Cell Stem Cell. 2014;15(3):350–64.
Bröske A-M, Vockentanz L, Kharazi S, Huska MR, Mancini E, Scheller M, et al. DNA methylation protects hematopoietic stem cell multipotency from myeloerythroid restriction. Nat Genet. 2009;41(11):1207–15.
Davies MN, Volta M, Pidsley R, Lunnon K, Dixit A, Lovestone S, et al. Functional annotation of the human brain methylome identifies tissue-specific epigenetic variation across brain and blood. Genome Biol. 2012;13(6):R43.
Ziller MJ, Gu H, Müller F, Donaghey J, Tsai LTY, Kohlbacher O, et al. Charting a dynamic DNA methylation landscape of the human genome. Nature. 2013;500(7463):477–81.
Farré P, Jones MJ, Meaney MJ, Emberly E, Turecki G, Kobor MS. Concordant and discordant DNA methylation signatures of aging in human blood and brain. Epigenetics Chromatin. 2015;8:19.
Koestler DC, Christensen B, Karagas MR, Marsit CJ, Langevin SM, Kelsey KT, et al. Blood-based profiles of DNA methylation predict the underlying distribution of cell types: a validation analysis. Epigenetics. 2013;8(8):816–26.
Jaffe AE, Irizarry RA. Accounting for cellular heterogeneity is critical in epigenome-wide association studies. Genome Biol. 2014;15(2):R31.
Guintivano J, Aryee MJ, Kaminsky ZA. A cell epigenotype specific model for the correction of brain cellular heterogeneity bias and its application to age, brain region and major depression. Epigenetics. 2013;8(3):290–302.
Houseman EA, Molitor J, Marsit CJ. Reference-free cell mixture adjustments in analysis of DNA methylation data. Bioinformatics. 2014;30(10):1431–9.
Zou J, Lippert C, Heckerman D, Aryee M, Listgarten J. Epigenome-wide association studies without the need for cell-type composition. Nat Methods. 2014;11(3):309–11.
Cai C, Langfelder P, Fuller TF, Oldham MC, Luo R, van den Berg LH, et al. Is human blood a good surrogate for brain tissue in transcriptional studies? BMC Genomics. 2010;11(1):589.
Hannon E, Lunnon K, Schalkwyk L, Mill J. Interindividual methylomic variation across blood, cortex, and cerebellum: implications for epigenetic studies of neurological and neuropsychiatric phenotypes. Epigenetics. 2015;10(11):1024–32.
Marsit CJ. Influence of environmental exposure on human epigenetic regulation. J Exp Biol. 2015;218(Pt 1):71–9.
Boyce WT, Kobor MS. Development and the epigenome: the “synapse” of gene-environment interplay. Dev Sci. 2015;18(1):1–23.
Feil R, Fraga MF. Epigenetics and the environment: emerging patterns and implications. Nat Rev Genet. 2012;13(2):97–109.
Baccarelli A, Tarantini L, Wright RO, Bollati V, Litonjua AA, Zanobetti A, et al. Repetitive element DNA methylation and circulating endothelial and inflammation markers in the VA normative aging study. Epigenetics. 2010;5(3):222–8.
Bollati V, Baccarelli A. Environmental epigenetics. Heredity. 2010;105(1):105–12.
Essex MJ, Boyce WT, Hertzman C, Lam LL, Armstrong JM, Neumann SMA, et al. Epigenetic vestiges of early developmental adversity: childhood stress exposure and DNA methylation in adolescence. Child Dev. 2013;84(1):58–75.
Monick MM, Beach SRH, Plume J, Sears R, Gerrard M, Brody GH, et al. Coordinated changes in AHRR methylation in lymphoblasts and pulmonary macrophages from smokers. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(2):141–51.
Shenker NS, Polidoro S, van Veldhoven K, Sacerdote C, Ricceri F, Birrell MA, et al. Epigenome-wide association study in the European Prospective Investigation into Cancer and Nutrition (EPIC-Turin) identifies novel genetic loci associated with smoking. Hum Mol Genet. 2013;22(5):843–51.
Fagny M, Patin E, MacIsaac JL, Rotival M, Flutre T, Jones MJ, et al. The epigenomic landscape of African rainforest hunter-gatherers and farmers. Nat Commun. 2015;6:10047.
Esposito EA, Jones MJ, Doom JR, MacIsaac JL, Gunnar MR, Kobor MS. Differential DNA methylation in peripheral blood mononuclear cells in adolescents exposed to significant early but not later childhood adversity. Dev Psychopathol. 2016:1–15.
Stringhini S, Polidoro S, Sacerdote C, Kelly RS, van Veldhoven K, Agnoli C, et al. Life-course socioeconomic status and DNA methylation of genes regulating inflammation. Int J Epidemiol. 2015;44(4):1320–30.
Miller GE, Chen E, Fok AK, Walker H, Lim A, Nicholls EF, et al. Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proc Natl Acad Sci U S A. 2009;106(34):14716–21.
Hong X, Hao K, Ladd-Acosta C, Hansen KD, Tsai H-J, Liu X, et al. Genome-wide association study identifies peanut allergy-specific loci and evidence of epigenetic mediation in US children. Nat Commun. 2015;6:6304.
Liu Y, Aryee MJ, Padyukov L, Fallin MD, Hesselberg E, Runarsson A, et al. Epigenome-wide association data implicate DNA methylation as an intermediary of genetic risk in rheumatoid arthritis. Nat Biotechnol. 2013;31(2):142–7.
Zhang Y, Zhao M, Sawalha AH, Richardson B, Lu Q. Impaired DNA methylation and its mechanisms in CD4(+)T cells of systemic lupus erythematosus. J Autoimmun. 2013;41:92–9.
Absher DM, Li X, Waite LL, Gibson A, Roberts K, Edberg J, et al. Genome-wide DNA methylation analysis of systemic lupus erythematosus reveals persistent hypomethylation of interferon genes and compositional changes to CD4+ T-cell populations. PLoS Genet. 2013;9(8), e1003678.
Gervin K, Vigeland MD, Mattingsdal M, Hammerø M, Nygård H, Olsen AO, et al. DNA methylation and gene expression changes in monozygotic twins discordant for psoriasis: identification of epigenetically dysregulated genes. PLoS Genet. 2012;8(1), e1002454.
Stefan M, Zhang W, Concepcion E, Yi Z, Tomer Y. DNA methylation profiles in type 1 diabetes twins point to strong epigenetic effects on etiology. J Autoimmun. 2014;50:33–7.
Laricade L, Urquiza JM, Gomez-Cabrero D, Islam ABMMK, López-Bigas N, Tegnér J, et al. Identification of novel markers in rheumatoid arthritis through integrated analysis of DNA methylation and microRNA expression. J Autoimmun. 2013;41:6–16.
Pacis A, Tailleux L, Morin AM, Lambourne J, MacIsaac JL, Yotova V, et al. Bacterial infection remodels the DNA methylation landscape of human dendritic cells. Genome Res. 2015;25(12):1801–11.
Marr AK, MacIsaac JL, Jiang R, Airo AM, Kobor MS, McMaster WR. Leishmania donovani infection causes distinct epigenetic DNA methylation changes in host macrophages. PLoS Pathog. 2014;10(10), e1004419. http://dx.plos.org/10.1371/journal.ppat.1004419.
Sinclair SHG, Yegnasubramanian S, Dumler JS. Global DNA methylation changes and differential gene expression in Anaplasma phagocytophilum-infected human neutrophils. Clin Epigenetics. 2015;7(1):77.
Gebel K, Ding D, Chey T, Stamatakis E, Brown WJ, Bauman AE. Effect of moderate to vigorous physical activity on all-cause mortality in middle-aged and older Australians. Am Medical Assoc. 2015;175(6):970–7.
Christensen K, Johnson TE, Vaupel JW. The quest for genetic determinants of human longevity: challenges and insights. Nat Rev Genet. 2006;7(6):436–48.
Goronzy JJ, Li G, Weyand CM. DNA methylation, age-related immune defects, and autoimmunity. Epigenetics of aging. New York: Springer; 2010. p. 327–44.
Romanov GA, Vanyushin BF. Methylation of reiterated sequences in mammalian DNAs. Effects of the tissue type, age, malignancy and hormonal induction. Biochim Biophys Acta. 1981;653(2):204–18.
Hoal-van Helden EG, van Helden PD. Age-related methylation changes in DNA may reflect the proliferative potential of organs. Mutat Res. 1989;219(5-6):263–6.
Wilson VL, Smith RA, Ma S, Cutler RG. Genomic 5-methyldeoxycytidine decreases with age. J Biol Chem. 1987;262(21):9948–51.
Heyn H, Li N, Ferreira HJ, Moran S, Pisano DG, Gomez A, et al. Distinct DNA methylomes of newborns and centenarians. Proc Natl Acad Sci U S A. 2012;109(26):10522–7.
Johansson A, Enroth S, Gyllensten U. Continuous aging of the human DNA methylome throughout the human lifespan. PLoS One. 2013;8(6), e67378.
Christensen BC, Houseman EA, Marsit CJ, Zheng S, Wrensch MR, Wiemels JL, et al. Aging and environmental exposures alter tissue-specific DNA methylation dependent upon CpG island context. PLoS Genet. 2009;5(8), e1000602.
Bollati V, Schwartz J, Wright R, Litonjua A, Tarantini L, Suh H, et al. Decline in genomic DNA methylation through aging in a cohort of elderly subjects. Mech Ageing Dev. 2009;130(4):234–9.
Jones MJ, Goodman SJ, Kobor MS. DNA methylation and healthy human aging. Aging Cell. 2015;14(6):924–32.
Boks MP, van Mierlo HC, Rutten BPF, Radstake TRDJ, De Witte L, Geuze E, et al. Longitudinal changes of telomere length and epigenetic age related to traumatic stress and post-traumatic stress disorder. Psychoneuroendocrinology. 2015;51:506–12.
Teschendorff AE, West J, Beck S. Age-associated epigenetic drift: implications, and a case of epigenetic thrift? Hum Mol Genet. 2013;22(R1):R7–15.
Martin GM. Epigenetic drift in aging identical twins. Proc Natl Acad Sci U S A. 2005;102(30):10413–4.
Fraga MF, Ballestar E, Paz MF, Ropero S, Setien F, Ballestart ML, et al. Epigenetic differences arise during the lifetime of monozygotic twins. Proc Natl Acad Sci U S A. 2005;102(30):10604–9.
Hannum G, Guinney J, Zhao L, Zhang L, Hughes G, Sadda S, et al. Genome-wide methylation profiles reveal quantitative views of human aging rates. Mol Cell. 2013;49(2):359–67.
Córdova-Palomera A, Fatjó-Vilas M, Gastó C, Navarro V, Krebs M-O, Fañanás L. Genome-wide methylation study on depression: differential methylation and variable methylation in monozygotic twins. Transl Psychiatry. 2015;5, e557.
Winnefeld M, Lyko F. The aging epigenome: DNA methylation from the cradle to the grave. Genome Biol. 2012;13(7):165.
Murgatroyd C, Patchev AV, Wu Y, Micale V, Bockmühl Y, Fischer D, et al. Dynamic DNA methylation programs persistent adverse effects of early-life stress. Nat Neurosci. 2009;12(12):1559–66.
Bocklandt S, Lin W, Sehl ME, Sanchez FJ, Sinsheimer JS, Horvath S, et al. Epigenetic predictor of age. PLoS One. 2011;6(6), e14821.
Weidner CI, Lin Q, Koch CM, Eisele L, Beier F, Ziegler P, et al. Aging of blood can be tracked by DNA methylation changes at just three CpG sites. Genome Biol. 2014;15(2):R24.
Koch CM, Wagner W. Epigenetic-aging-signature to determine age in different tissues. Aging (Albany NY). 2011;3(10):1018–27.
Horvath S. DNA methylation age of human tissues and cell types. Genome Biol. 2013;14(10):R115.
Levine ME, Lu AT, Bennett DA, Horvath S. Epigenetic age of the pre-frontal cortex is associated with neuritic plaques, amyloid load, and Alzheimer’s disease related cognitive functioning. Aging (Albany NY). 2015;7(12):1198–211.
Horvath S, Garagnani P, Bacalini MG, Pirazzini C, Salvioli S, Gentilini D, et al. Accelerated epigenetic aging in Down syndrome. Aging Cell. 2015;14(3):491–5.
van Eijk KR, de Jong S, Strengman E, Buizer-Voskamp JE, Kahn RS, Boks MP, et al. Identification of schizophrenia-associated loci by combining DNA methylation and gene expression data from whole blood. Eur J Hum Genet. 2015;23(8):1106–10.
Wolf EJ, Logue MW, Hayes JP, Sadeh N, Schichman SA, Stone A, et al. Accelerated DNA methylation age: Associations with PTSD and neural integrity. Psychoneuroendocrinology. 2015;63:155–62.
Horvath S, Levine AJ. HIV-1 infection accelerates age according to the epigenetic clock. J Infect Dis. 2015;212(10):1563–73.
Rickabaugh TM, Baxter RM, et al. Acceleration of age-associated methylation patterns in HIV-1-infected adults. PLoS One. 2015;10(3), e0119201. http://dx.plos.org/10.1371/journal.pone.0119201.
Horvath S, Ritz BR. Increased epigenetic age and granulocyte counts in the blood of Parkinson’s disease patients. Aging (Albany NY). 2015;7(12):1130–42.
Levine ME, Hosgood HD, Chen B, Absher D, Assimes T, Horvath S. DNA methylation age of blood predicts future onset of lung cancer in the women’s health initiative. Aging (Albany NY). 2015;7(9):690–700.
Marioni RE, Shah S, McRae AF, Chen BH, Colicino E, Harris SE, et al. DNA methylation age of blood predicts all-cause mortality in later life. Genome Biol. 2015;16(1):25.
Christiansen L, Lenart A, Tan Q, Vaupel JW, Aviv A, McGue M, et al. DNA methylation age is associated with mortality in a longitudinal Danish twin study. Aging Cell. 2015;15(1):149–54.
Reynolds LM, Taylor JR, Ding J, Lohman K, Johnson C, Siscovick D, et al. Age-related variations in the methylome associated with gene expression in human monocytes and T cells. Nat Commun. 2014;5:5366.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
McEwen, L.M., Goodman, S.J., Kobor, M.S., Jones, M.J. (2017). The DNA Methylome: An Interface Between the Environment, Immunity, and Ageing. In: Bueno, V., Lord, J., Jackson, T. (eds) The Ageing Immune System and Health. Springer, Cham. https://doi.org/10.1007/978-3-319-43365-3_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-43365-3_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43363-9
Online ISBN: 978-3-319-43365-3
eBook Packages: MedicineMedicine (R0)