Abstract
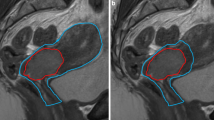
Preoperative radiochemotherapy (RCT) has been successfully adopted to reduce local recurrence rates in locally advanced rectal cancer. This benefit however has to be balanced against the acute and late side effects, of which radiation enteritis due to radiotherapy (RT) induced small bowel injury is the major source. A multitude of factors are influencing the tolerance of small bowel to radiation, including diabetes mellitus, pelvic inflammatory disease, prior abdominal or pelvic surgery, and the administration of concurrent chemotherapy. The major factors however are RT related and include mainly the total radiation dose and the volume of irradiated small bowel. Despite well-accepted and implemented measures such as distention of the urinary bladder, the use of the prone position, and a belly-board technique, the irradiated volume of small bowel can be reduced significantly only by using sophisticated forms of conformal RT such as intensity-modulated RT (IMRT), where geometrically shaped fields and varying intensities within the shaped field create a conformal dose distribution that tightly matches the target volume. Considering the concave shaped form of the planning target volume (PTV) with the small bowel and bladder lying in the middle, preoperative RT of rectal cancer represents a real challenge for IMRT. Dose-volume constraints have been of little relevance for 3D-conformal RT (3D-CRT) as the planner is configuring a variety of beams, wedges, and beamweights to end up in a suitable plan (called “forward planning”). In contrast, the complexity of IMRT requires the inverse and allows clinicians to specify dose-volume constraints to PTV as well as critical organs at risk (OAR) before the optimization is initiated (“inverse planning”). The following section proposes dose-volume constraints for the OARs in preoperative RT of rectal cancer based on available dose-response relationships (Table 24.1).
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Preoperative radiochemotherapy (RCT) has been successfully adopted to reduce local recurrence rates in locally advanced rectal cancer. This benefit however has to be balanced against the acute and late side effects, of which radiation enteritis due to radiotherapy (RT) induced small bowel injury is the major source. A multitude of factors are influencing the tolerance of small bowel to radiation, including diabetes mellitus, pelvic inflammatory disease, prior abdominal or pelvic surgery, and the administration of concurrent chemotherapy. The major factors however are RT related and include mainly the total radiation dose and the volume of irradiated small bowel. Despite well-accepted and implemented measures such as distention of the urinary bladder, the use of the prone position, and a belly-board technique, the irradiated volume of small bowel can be reduced significantly only by using sophisticated forms of conformal RT such as intensity-modulated RT (IMRT), where geometrically shaped fields and varying intensities within the shaped field create a conformal dose distribution that tightly matches the target volume. Considering the concave shaped form of the planning target volume (PTV) with the small bowel and bladder lying in the middle, preoperative RT of rectal cancer represents a real challenge for IMRT. Dose-volume constraints have been of little relevance for 3D-conformal RT (3D-CRT) as the planner is configuring a variety of beams, wedges, and beamweights to end up in a suitable plan (called “forward planning”). In contrast, the complexity of IMRT requires the inverse and allows clinicians to specify dose-volume constraints to PTV as well as critical organs at risk (OAR) before the optimization is initiated (“inverse planning”). The following section proposes dose-volume constraints for the OARs in preoperative RT of rectal cancer based on available dose-response relationships (Table 24.1).
1 Small Bowel
The hypothesis that a critical volume of small bowel has to be irradiated up to a specific dose level before mucosal disruption induces severe diarrhea is supported by the strong association between the frequency of acute gastrointestinal (GI) toxicity and the absolute volume of small bowel irradiated at each dose level in rectal cancer patients undergoing pre- or postoperative radiochemotherapy [1,2,3]. Baglan et al. reported on 40 rectal cancer patients treated with 3D-CRT and found the volume of small bowel receiving a total dose of 15 Gy or more (V15) as an especially predictive factor, with no grade 3+ acute small bowel toxicity in patients receiving 15 Gy to less than 150 cc of small bowel, whereas 50% of the patients receiving 15 Gy to more than 150 cc developed grade 3+ GI toxicity [1]. Similar results have been reported by Gunnlaugsson et al., showing clinically significant diarrhea in 52% of the patients with a V15 > 150 cc, whereas only 11% in patients with a V15 ≤ 150 cc [4]. Robertson et al. also found a significant correlation of the V15 with the incidence of grade 3 diarrhea in a series of 152 rectal cancer patients [5]. Tho et al. noted that the irradiated volume of small bowel correlated strongly with severity of diarrhea at each dose level (p < 0.03) in 41 rectal cancer patients undergoing preoperative RCT, with the greatest correlation at the levels between V5 and V30 [3]. Therefore, the primary aim in the IMRT planning process should be keeping the V15 of the small bowel below 150 cc. On the other hand, high-dose irradiation of small bowel should also be minimized because of correlation of V35, V40, and V45 dose levels with acute diarrhea [3, 6]. In a series of 177 rectal cancer patients, Yang et al. reported the V45 to be the most predictive factor as no grade 2+ diarrhea occurred when V45 was <3% as compared to a ≥ 20% risk for V45 ≥ 27% [6], indicating that acute diarrhea during pelvic RT may be a high-dose effect similar to that observed for cervical or anal cancer [7, 8]. In contrast, Reis et al. suggested to keep the small bowel volume receiving 5 Gy below 300 cc as 82% of the patients with a V5 > 292 cc experienced grade 2–3 diarrhea, as compared to only 29% with a V5 below this cut-off value in a prospective series of 45 rectal cancer patients treated with preoperative multi-agent CRT [9]. Concerning late toxicity, Letschert et al. detected a correlation between the small bowel volume within the radiation field and late occurring small bowel complications by reporting 37% severe late GI toxicity for patients irradiated with opposed anterior and posterior treatment fields with an estimated small bowel volume within the field of 790 ml versus 6% for patients treated with three-field pelvic RT with an estimated in-field volume of 165 ml [10]. The quantitative analysis of normal tissue effects in the clinic (QUANTEC) refined the normal tissue dose/volume tolerance guidelines for small bowel as follows: the V15 should be kept below 120 cc for <10% risk of severe acute toxicity, when delineating individual loops of small bowel [11]. It is indeed of crucial concern how the small bowel is defined when analyzing dose-volume relationships. Yang et al. included the small bowel and sigmoid colon as individual loops in the bowel contour, extending to only 1 cm above the PTV [6]. We consider the small bowel contour as the individual loops from mid L4, or at least 3 cm above the PTV, to the lowest extent in the pelvis [12]. One should notice that the proposed dose-volume constraints are all based on data from patient series treated with 3D-CRT and therefore not immediately applicable to IMRT treatment. Arguably, by keeping the irradiated volumes of small bowel receiving more than 15 Gy below 150 cc in a prospective series of 108 rectal cancer patients treated with IMRT, we recorded only 1% grade 3 acute diarrhea and acceptable rate of 9% grade 3 or more late GI toxicity after a median follow-up of 54 months [13], concluding that IMRT remains an attractive concept in preoperative RT of rectal cancer by its ability to reduce the irradiated volume of surrounding healthy tissues without compromising oncological safety.
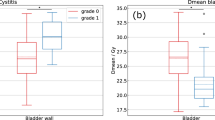
2 Bladder
The bladder is known to be less radiosensitive compared to the small bowel and receives on small volumes often doses ≥70 Gy, e.g., in primary RT of gynecological and urological malignancies, without being harmful. As a consequence of the bladder tolerance, grade 3+ late genitourinary (GU) toxicity was observed in only 2% of the patients undergoing preoperative RCT in the German trial [14]. Appelt et al. demonstrated at first a significant dose-volume relationship for acute urinary toxicity in a large patient cohort of 345 patients undergoing long-course preoperative CRT and reported a dose cut-off of 35 Gy as yielding the closest correlation with the observed urinary toxicity [15]. Keeping the mean bladder dose below 21 Gy, we recorded in an IMRT series 12% grade 2 acute GU toxicity, with no grade 3 acute events [16]. After a median follow-up of 54 months, we reported 4% grade 3 or more chronic urinary toxic effects [13]. One should consider that the recorded late urinary toxicity can be caused by both radiotherapy and/or surgery. No clinically significant benefit is to be expected from IMRT with regard to GU toxicity in preoperative RT of rectal cancer.
3 Pelvic Bone
Several studies investigated pelvic fractures after RT, of which a large retrospective cohort study by Baxter et al. confirmed the association between pelvic irradiation and increased risk of pelvic fractures in elderly women [17]. The most compelling evidence of this association in RT for rectal cancer has been provided by the long-term follow-up data of the Stockholm I and Stockholm II randomized trials. For the irradiated group receiving a total dose of 5 × 5 Gy by using a 2-field or 4-field box technique, they reported 5.3% femoral neck or pelvic fractures with hospitalization, as compared to only 2.4% in the nonirradiated group [18]. Studies establishing the tolerance dose for the head and neck of the femur are lacking, but the risk of fracture could theoretically be altered significantly by the implementation of IMRT by reducing the dose to the bony structures. Pending those data, most radiation oncologist agree to limit the dose to 45–50 Gy.
Sacral insufficiency fractures are rare after preoperative RT, but can cause significant morbidity. Among 562 patients treated with preoperative three-field CRT, Herman et al. reported a 3-year rate of sacral insufficiency fractures of 3.1%, with higher risk for women [19]. Independent risk factors associated with sacral insufficiency fractures are osteoporosis, female gender, and age >60 years according to a retrospective analysis by Kim et al., who recorded a 7.1% incidence of sacral fractures within a median follow-up time of 3.5 years in 582 patients who underwent preoperative CRT [20]. Data on dose-response relationships for sacral insufficiency fractures are awaited in preoperative RT of rectal cancer.
4 Lumbosacral Plexus
Radiation-induced lumbosacral plexopathy is an underestimated and extremely disabling complication of pelvic RT. Tunio et al. evaluated as first the dose distribution to the lumbosacral plexus and its correlation with radiation-induced lumbosacral plexopathy in 50 cervical cancer patients treated with IMRT and high-dose-rate brachytherapy. After a median follow-up of 5 years, they reported 8% grade 2 or more plexopathy and found that a mean dose <45 Gy, V40 < 55%, V50 < 30%, V55 < 5%, and V60 < 0.5% reduced the risk for plexopathy [21]. Larger prospective studies in rectal cancer patients are however warranted before firm conclusions can be draw on the dose-volume relationship, but the lumbosacral plexus should be considered an OAR in rectal cancer patients undergoing preoperative RT.
5 Bone Marrow
As approximately 40% of the total body bone marrow reserves are located in the pelvis, hematological toxicity has been reported in up to 8% of the patients undergoing preoperative CRT with continuous infusion of 5-FU [22]. Mell et al. reported a significant correlation between the volume of bone marrow receiving 10–20 Gy and acute hematological toxicity during CRT for anal cancer, reflecting the high radiosensitivity of bone marrow stem cells [23]. The dosimetric benefit of bone marrow sparing with IMRT has been demonstrated by Mell et al. in the treatment of cervical cancer [24]. IMRT reduced lumbosacral bone marrow irradiation at all dose levels and reduced the volume of pelvic bone marrow irradiated to high doses [24]. In contrast to the low-dose radiation threshold in anal cancer, likely because of the heavily myelosuppressive combination chemotherapy, a higher dose threshold has been reported in rectal cancer RT by Yang et al. [22]. They found the coxal and sacral bone marrow volume receiving at least 45 Gy to be significant predictors for myelosuppression and proposed a dose constraint of sacral V45 < 51% and coxal V45 < 13% [22]. In the setting of minimally myelotoxic chemotherapy such as capecitabine, bone marrow toxicity could theoretically even be lower.
6 General Consideration
IMRT has significantly improved the tolerance of the preoperative RT for rectal cancer, especially with regard to radiation enteritis. The above-discussed DVH parameters were partially obtained using 3D-CRT, without volumetric imaging, and are therefore not strictly applicable to modern IMRT treatments. Considering this and the increasing use of concomitant chemotherapy and new biologicals, we advocate that an individual radiation plan should be accepted only when it is optimized as good as it can get, taking the patient anatomy into account.
References
Baglan KL, Frazier RC, Yan D et al (2002) The dose-volume relationship of acute small bowel toxicity from concurrent 5-FU-based chemotherapy and radiation therapy for rectal cancer. Int J Radiat Oncol Biol Phys 52:176–183
Robertson JM, Lockman D, Yan D et al (2008) The dose-volume relationship of small bowel irradiation and acute grade 3 diarrhea during chemoradiotherapy for rectal cancer. Int J Radiat Oncol Biol Phys 70:413–418
Tho LM, Glegg M, Paterson J et al (2006) Acute small bowel toxicity and preoperative chemoradiotherapy for rectal cancer: investigating dose-volume relationships and role for inverse planning. Int J Radiat Oncol Biol Phys 66:505–513
Gunnlaugsson A, Kjellen E, Nilsson P et al (2007) Dose-volume relationships between enteritis and irradiated bowel volumes during 5-fluorouracil and oxaliplatin based chemoradiotherapy in locally advanced rectal cancer. Acta Oncol 46:937–944
Robertson JM, Söhn M, Yan D (2010) Predicting grade 3 acute diarrhea during radiation therapy for rectal cancer using a cutoff-dose logistic regression normal tissue complication probability model. Int J Radiat Oncol Biol Phys 77:66–72
Yang TJ, Oh JH, Son CH et al (2013) Predictors of acute gastrointestinal toxicity during pelvic chemoradiotherapy in patients with rectal cancer. Gastrointest Cancer Res 6:129–136
Roeske JC, Bonta D, Mell LK et al (2003) A dosimetric analysis of acute gastrointestinal toxicity in women receiving intensity-modulated whole-pelvic radiation therapy. Radiother Oncol 69:201–207
Devisetty K, Mell LK, Salama JK et al (2009) A multi-institutional acute gastrointestinal toxicity analysis of anal cancer patients treated with concurrent intensity-modulated radiation therapy (IMRT) and chemotherapy. Radiother Oncol 93:298–301
Reis T, Khazzaka E, Welzel G et al (2015) Acute small-bowel toxicity during neoadjuvant combined radiochemotherapy in locally advanced rectal cancer: determination of optimal dose-volume cut-off value predicting grade 2–3 diarrhoea. Radiat Oncol 10:30
Letschert JG, Lebesque JV, de Boer RW et al (1990) Dose-volume correlation in radiation-related late small-bowel complications: a clinical study. Radiother Oncol 18:307–320
Marks LB, Yorke ED, Jackson A et al (2010) Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys 76:S10–S19
De Ridder M, Tournel K, Van Nieuwenhove Y et al (2008) Phase II study of preoperative helical tomotherapy for rectal cancer. Int J Radiat Oncol Biol Phys 70:728–734
Engels B, Platteaux N, Van den Begin R et al (2014) Preoperative intensity-modulated and image-guided radiotherapy with a simultaneous integrated boost in locally advanced rectal cancer: report on late toxicity and outcome. Radiother Oncol 110:155–159
Sauer R, Becker H, Hohenberger W et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:1731–1740
Appelt AL, Bentzen SM, Jakobsen A et al (2015) Dose-response of acute urinary toxicity of long-course preoperative chemoradiotherapy for rectal cancer. Acta Oncol 54:179–186
Engels B, Tournel K, Everaert H et al (2012) Phase II study of preoperative helical tomotherapy with a simultaneous integrated boost for rectal cancer. Int J Radiat Oncol Biol Phys 83:142–148
Baxter NN, Habermann EB, Tepper JE et al (2005) Risk of pelvic fractures in older women following pelvic irradiation. JAMA 294:2587–2593
Holm T, Singnomklao T, Rutqvist LE et al (1996) Adjuvant preoperative radiotherapy in patients with rectal carcinoma: adverse effects during long term follow-up of two randomized trials. Cancer 78:968–976
Herman MP, Kopetz S, Bhosale PR et al (2009) Sacral insufficiency fractures after preoperative chemoradiation for rectal cancer: incidence, risk factors, and clinical course. Int J Radiat Oncol Biol Phys 74:818–823
Kim HJ, Boland PJ, Meredith DS et al (2012) Fractures of the sacrum after chemoradiation for rectal carcinoma: incidence, risk factors, and radiographic evaluation. Int J Radiat Oncol Biol Phys 84:694–699
Tunio M, Al Asiri M, Bayoumi Y et al (2014) Lumbosacral plexus delineation, dose distribution, and its correlation with radiation-induced lumbosacral plexopathy in cervical cancer patients. Onco Targets Ther 8:21–27
Yang TJ, Oh JH, Apte A et al (2014) Clinical and dosimetric predictors of acute hematologic toxicity in rectal cancer patients undergoing chemoradiotherapy. Radiother Oncol 113:29–34
Mell LK, Schomas DA, Salama JK et al (2008) Association between bone marrow dosimetric parameters and acute hematologic toxicity in anal cancer patients treated with concurrent chemotherapy and intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 70:1431–1437
Mell LK, Tiryaki H, Ahn KH et al (2008) Dosimetric comparison of bone marrow-sparing intensity-modulated radiotherapy versus conventional techniques for treatment of cervical cancer. Int J Radiat Oncol Biol Phys 71:1504–1510
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Engels, B., De Ridder, M. (2018). What Are the Dose-Volume Constraints for Long-Course Radiochemotherapy to Apply for IMRT?. In: Valentini, V., Schmoll, HJ., van de Velde, C. (eds) Multidisciplinary Management of Rectal Cancer. Springer, Cham. https://doi.org/10.1007/978-3-319-43217-5_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-43217-5_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43215-1
Online ISBN: 978-3-319-43217-5
eBook Packages: MedicineMedicine (R0)