Abstract
Vascular surgery is a speciality in which diseases of the arteries, veins and lymphatic system are diagnosed and managed. It emerged from general surgery and has been considered a separate surgical speciality in the UK since 2013. Minimally invasive surgery now forms a large part of a vascular surgeon’s workload and endovascular approaches are often used during procedures.
This chapter outlines the core concepts of vascular surgery including: core clinical anatomy, commonly treated conditions and descriptions of five commonly performed procedures.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Vascular surgery
- Vascular anatomy
- Vascular disease
- Endovascular abdominal aortic aneurysm repair (EVAR)
- Carotid endarterectomy
- Critical limb ischaemia
- Student
Introduction
Vascular surgery is a speciality in which diseases of the arteries, veins and lymphatic system are diagnosed and managed. It emerged from general surgery and has been considered a separate surgical speciality in the UK since 2013. Minimally invasive surgery now forms a large part of a vascular surgeon’s workload and endovascular approaches are often used during procedures.
This chapter outlines the core concepts of vascular surgery including: core clinical anatomy, commonly treated conditions and descriptions of five commonly performed procedures.
Clinical Anatomy
This section will summarise the anatomy relevant to this chapter. It is not intended to be comprehensive, and for more information, a dedicated anatomy textbook is recommended.
The Aorta
The aorta originates from the left ventricle of the heart and extends down into the abdomen where it bifurcates into the common iliac arteries at vertebral level L4.
It can be divided into the following sections:
-
The ascending aorta:
-
Gives rise to the right and left coronary arteries.
-
-
The aortic arch which has three major branches:
-
The brachiocephalic trunk (sometimes called the innominate artery), which divides into the right common carotid artery and the right subclavian artery.
-
The left common carotid artery.
-
The left subclavian artery.
-
-
The descending thoracic aorta:
-
Branches include the intercostal arteries.
-
-
The abdominal aorta:
-
Has multiple branches including the renal arteries which arise between L1 and L2.
-
The majority of abdominal aortic aneurysms (AAAs) originate below L1/L2 – the origin of the renal arteries – and above the bifurcation of the abdominal aorta. Although thoracic aortic aneurysms also occur, these are much less common and do not feature in exams as much as AAAs.
The Carotid Arteries
There are two common carotid arteries which provide the majority of the blood supply to the head and neck:
-
The right common carotid artery originates from the brachiocephalic trunk (a branch of the aortic arch).
-
The left common carotid artery originates directly from the aortic arch.
-
Both common carotid arteries divide to form internal and external carotid arteries at vertebral level C4.
The carotid arteries are contained in the carotid sheath and are positioned posterior to the sternocleidomastoid muscles in the neck. They are found in close proximity to three cranial nerves:
-
Cranial nerve IX i.e. the glossopharyngeal nerve
-
Cranial nerve X i.e. the vagus nerve
-
Cranial nerve XII i.e. the hypoglossal nerve
During carotid endarterectomy, these nerves are at risk of damage. Damage may cause:
-
Difficulty swallowing and an absent gag reflex (cranial nerve IX damage).
-
Hoarseness as a result of paralysed vocal cords (cranial nerve X damage).
-
Wasting of the ipsilateral side of the tongue (cranial nerve XII damage).
The Femoral Artery
The femoral artery is the main blood supply to the lower limb, and hence its occlusion can result in gangrene and the need for amputation if untreated. It is a continuation of the external iliac artery (a branch of the common iliac artery).
-
It passes into the lower limb under the inguinal ligament, midway between the anterior superior iliac spine (ASIS) and the pubic symphysis.
-
It descends through the thigh in the femoral sheath, lateral to the femoral vein and medial to the femoral nerve (the nerve is not in the sheath).
-
It gives off several branches, the largest being profunda femoris, which supplies most of the thigh via its circumflex and perforating branches.
-
It passes into the popliteal fossa through the adductor hiatus (an opening in the adductor magnus muscle), becoming the popliteal artery.
The Popliteal Artery
The popliteal artery, a continuation of the femoral artery, runs through the popliteal fossa, ending at the lower border of the popliteus muscle. It divides into the anterior and posterior tibial arteries to supply the leg.
It has five genicular branches, which anastomose with branches of the lateral femoral circumflex artery (from the profunda femoris) and the anterior tibial to supply the knee joint. If the femoral artery must be ligated due to the presence of an aneurysm, this anastomosis ensures that blood will still reach the leg. A femoropopliteal bypass operation is used to ensure limb survival in the case of a popliteal aneurysm.
The Great Saphenous Vein
The great saphenous vein is the longest vein in the body. It originates from the dorsal venous arch of the foot and passes in front of the medial malleolus of the ankle, running medially up the leg and anteriorly up the thigh before passing through the saphenous opening of the fascia lata to join the femoral vein.
The great saphenous vein is the most common vein to be used by vascular surgeons as a conduit in bypass operations.
Core Conditions
Vascular surgeons commonly manage peripheral vascular disease, aneurysms, carotid artery disease and varicose veins. These conditions may have a chronic course (e.g. varicose veins) or they may present as vascular emergencies (e.g. ruptured abdominal aortic aneurysms). Vascular repairs are usually carried out using either an open or endovascular approach.
Peripheral Vascular Disease
Peripheral vascular disease (PVD) is obstruction of the peripheral arterial blood flow. This definition therefore excludes the intracranial and coronary arteries. In some patients PVD may be mild with only asymptomatic plaques present. Others may suffer from moderate disease and present with intermittent claudication (IC). Finally, severe disease is likely to present as critical limb ischaemia (CLI), which may result in amputation. Both the presence and severity of PVD is determined by the ankle-brachial pressure index (ABPI). In health the ABPI is greater than 1 mmHg.
The main risk factors for PVD include:
-
Smoking
-
Hypertension
-
Hyperlipidaemia
-
Diabetes Mellitus
-
A family history of PVD
Considering mild disease is mainly asymptomatic the majority of patients present with IC as a result of moderate lower limb ischaemia. The ABPI is typically 0.5–0.9 mmHg. Patients complain of muscular pain in the calf, although pain may also be felt in the thigh and buttocks. Pain is provoked by exercise, most commonly at a ‘claudication distance’ and relieved by rest. Symptoms often follow a cyclical pattern in which they progress then resolve as ischaemia promotes the development of collateral vessels. PVD can be managed conservatively by risk factor reduction strategies, including smoking cessation and supervised exercise programmes. If conservative measures fail vasoactive drugs can be used. Some patients ultimately require surgical treatment.
Severe Limb Ischaemia
Severe limb ischaemia (SLI) is the end stage of PVD. It presents with severe pain at rest which awakens the patient from sleep and requires opiate analgesics. Patients must have symptoms for more than 2 weeks and may also present with ulceration and/or gangrene. SLI encompasses both subcritical limb ischaemia (SCLI) and CLI. Patients with SCLI have an ABPI of greater than 0.5 mmHg with rest pain only. CLI is defined by an ABPI of less than 0.5 mmHg with the clinical features described above. While CLI is usually due to a single-segment of plaque, SCLI is due to plaques at multiple levels within the vascular tree. SCLI can lead to amputation if untreated. Management includes surgical repair by bypass graft or angioplasty.
Bypass Grafts
A huge variety of bypass grafts are carried out as part of vascular surgical procedures. They provide a better blood supply to a tissue, redirecting blood around a narrowed or blocked blood vessel. Considering the nomenclature of the grafts, the first part of the graft name originates from the artery the graft comes from, and the second part comes from the artery the graft is sewn on to. Examples include femoro-popliteal and axillo-femoral grafts.
Aneurysms
An aneurysm is a localised, abnormal, dilatation of a blood vessel (Gr. aneurusma; widening).
Types of Aneurysm
-
True aneurysms:
-
Involve all three layers of the vessel wall (the tunica intima, tunica media and tunica adventitia).
-
Have a diameter that is greater than 150 % of the original vessel diameter.
-
Usually develop as a result of atherosclerosis.
-
Can be fusiform or saccular:
-
Fusiform aneurysms involve the entire circumference of the artery – often referred to as spindle shaped aneurysms.
-
Saccular aneurysms involve only part of the circumference of the artery – often referred to as saclike aneurysms.
-
-
-
False/pseudo aneurysms:
-
Result from a breach in the vessel allowing blood to leak through. The blood is contained by the adventitia. The haematoma surrounding the artery mimics an aneurysm.
-
A common complication of arterial catheterisation (e.g. coronary angiogram).
-
Can also be caused by trauma and infection.
-
Can be identified on ultrasound by a yin-yang sign (due to turbulent flow).
-
Aortic Aneurysms
-
AAAs are the most common type of aortic aneurysm. The most common site is the infrarenal aorta.
-
The suprarenal aorta and thoracic aorta can also be affected.
-
The ascending aorta is usually spared.
-
Aortic aneurysms are usually asymptomatic until they rupture.
-
Clinical features of rupture include:
-
Shock: hypotension, cyanosis, mottling, tachycardia and confusion
-
Sudden onset pain at the site of rupture
-
A pulsatile abdominal mass
-
-
Rupture of an aortic aneurysm has a high mortality rate.
-
-
Surgical repair can be attempted using both open and endovascular techniques.
AAAs with a diameter >5.5 cm have a risk of rupture of over 3 % per year. Until an AAA has reached 5.5 cm the risks of surgery outweigh the risk of rupture. A diameter of 5.5 cm is therefore an indication for surgical repair. Elective, asymptomatic AAA repair has a 30-day mortality of 5–8 %. Emergency, symptomatic AAA repair has a 30-day mortality of 10–20 % and a rupture repair has a mortality of 50 %.
At present, there is a UK National Screening programme which utilises ultrasound to identify AAAs in all men aged 65 years and over. If the scan reveals an AAA <3 cm in diameter, no further follow up is required. An AAA 3–4.4 cm requires follow up in 1 year and a diameter of 4.5–5.4 cm requires follow up every 3 months. Vascular surgery referral is required in those patients with an AAA diameter of 5.5 cm or greater.
Carotid Artery Disease
Stenosis of the carotid arteries in the neck is caused by atherosclerosis and plaque formation. The plaque(s) may be stable and asymptomatic or be the source of embolization. As the embolus travels into the intracranial vasculature it may cause temporary ischaemia resulting in a transient ischemic attack (TIA) or manifest as a thromboembolic stroke resulting in permanent damage. Carotid artery disease may present as a carotid bruit (‘swooshing’ noise) on auscultation. Colour flow duplex ultrasound is the diagnostic modality of choice.
The main risk factors for carotid artery disease include:
-
Smoking
-
Diabetes Mellitus
-
Hypertension
-
Hyperlipidaemia
If there is a greater than 50 % stenosis of the internal carotid artery on investigation which has resulted in a TIA or stroke, the first line treatment is urgent carotid endarterectomy. This is only indicated within 14 days of the event. The North American Symptomatic Carotid Endarterectomy Trial (NASCET) has reported that carotid endarterectomy provides significant benefit in patients with severe symptomatic stenosis [1]. If the stenosis in the internal carotid artery is found incidentally and is asymptomatic, the evidence for surgery is less clear. The asymptomatic carotid surgery trial (ACST) found that while the procedure reduces stroke risk in asymptomatic patients younger than 75 years, benefit to patients depends on a variety of factors including life expectancy and future surgical risk [2]. Current management options in asymptomatic disease also include medical alternatives.
Varicose Veins
There are both superficial and deep venous systems in the lower limb. They are connected to each other by perforating veins and at the sapheno-femoral and sapheno-popliteal junctions. Venous blood is returned to the heart via the iliac veins and inferior vena cava.
When the calf muscles in the legs contract blood is pumped towards the heart as venous blood drains from superficial to deep veins. When the calf muscles relax the ‘one-way’ valves in the veins close. This closure prevents backflow of venous blood into the superficial venous system.
Valve incompetency will allow blood to flow into the superficial veins, converting them into a high-pressure system and producing the enlarged, tortuous appearance of varicose veins.
The main risk factors for varicose veins include:
-
Old age
-
A family history
-
Female gender
-
Pregnancy
-
Obesity
-
A standing occupation
Thrombus Versus Embolus
An important concept to grasp when trying to understand vascular surgery is the difference between a thrombus and an embolus. Although both can block blood vessels and cause tissue necrosis if untreated, their underlying pathology is different.
-
A thrombus is an abnormal aggregation of platelets creating a clot which is formed within a vessel. Thrombi commonly occur in the deep veins of the legs e.g. Deep vein thrombosis (DVT).
-
An embolism implies movement. It may be thought of as a floating clot that lodges somewhere else in the vasculature. They commonly break off from thrombi e.g. a pulmonary embolism as a result of a DVT. Emboli are not always blood clots. Fat, air and bone marrow are other types of emboli.
Core Operations
Five of the most commonly performed (and asked about in exams!) vascular procedures are outlined below.
AAA Repair
This procedure can be carried out using both open and endovascular approaches.
Endovascular AAA Repair (EVAR)
Indications
-
Aneurysm diameter of greater than 5.5 cm.
-
Rapid aneurysm growth (greater than 0.5 cm in 6 months).
-
Symptomatic aneurysm:
-
Tender to touch.
-
Back pain.
-
Distal embolization.
-
-
Aneurysmal rupture.
Contraindications
-
Less than 1.5 cm of normal aorta below the renal arteries (1.5 cm of normal aorta is required to allow a sufficient healing zone for the stent graft).
-
Calcification or tortuosity of the femoral or iliac arteries.
Presentation
Aneurysms are often asymptomatic, and therefore are often found incidentally by ultrasound scan, CT scan or, rarely, clinical examination.
Symptomatic aneurysms occasionally occur. The patient usually presents with abdominal or back pain, and should be urgently referred to a vascular surgeon for diagnosis and consideration for treatment.
Investigations
-
Ultrasound scan.
-
CT angiogram of aorta.
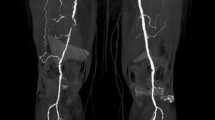
In cases of suspected AAA, it is important to visualise the whole aorta, from the ascending aorta to the femoral arteries. Often, there is co-existent pathology present in the descending thoracic aorta and iliac arteries. A CT angiogram allows the patient’s anatomy to be examined so the most appropriate stent graft can be chosen. It also allows the length of normal aorta below the renal arteries to be assessed, aiding in the decision of whether or not EVAR is the most appropriate procedure.
Step by Step Summary: EVAR
-
1.
Bilateral access to the common femoral artery is obtained via femoral artery cutdown. Alternatively, EVAR can be performed percutaneously.
-
2.
A stiff guidewire is inserted through the incision in the right groin to the aortic arch to allow the surgeon to track the catheters and stent graft into the body.
-
3.
A pigtail catheter is placed at the level of the renal arteries and an aortogram of the abdominal aorta and iliac arteries used to guide the placement of the stent graft. This ensures the renal arteries are not obstructed by the graft.
-
4.
The main body of the stent graft is inserted over the guidewire from the right groin incision and pushed into the correct position with the covered part below the renal arteries. The stent-graft is collapsed during this step.
-
5.
The main body is deployed and the right limb is inserted to complete the procedure on the right side.
-
6.
A guidewire and catheter are used on the left side to allow positioning and deployment of the stent graft on the left side.
-
7.
Ballooning of the stent graft in the aortic neck is carried out to help the stent graft appose to the aortic wall.
-
8.
Ballooning all the stent overlaps is carried out to make sure that no blood can leak between the stent grafts.
-
9.
A “completion aortogram” is carried out to make sure the aneurysm is sealed and there is no endoleak.
-
10.
The arteries are closed either with a percutaneous closure device or direct arterial sutures.
-
11.
The groin incisions are also closed and bandaged.
Complications
-
Bleeding:
-
Most commonly from the artery used for access.
-
Can also occur from accidental rupture of an iliac artery from pushing the device up through narrow calcified vessels.
-
-
Distal embolization.
-
Endoleak:
-
Blood flow outside the lumen of the graft.
-
Occurs if the seal is insufficient.
-
-
Renal failure.
-
Death.
Follow-Up
All patients require follow-up. Most surgeons would advise a CT scan before discharge (or at least in the first 3 months after the procedure) in order to check the position of the stent graft and make sure the aneurysm is sealed with no endoleak. If the CT scan shows no problems, most patients go into an ultrasound surveillance programme for the rest of their lives.
Open AAA Repair (OAR)
Indications
-
As for EVAR.
-
Often used for fit patients who are not suitable for EVAR due to not having a sufficient length of normal aorta below the renal arteries for a stent graft.
Contraindications
-
If the patient is not fit for open surgery.
-
Multiple previous abdominal operations.
-
Presence of stoma (relative contraindication).
Presentation
-
As for EVAR.
Investigations
-
CT angiogram.
-
Assessment of cardiorespiratory fitness:
-
Echocardiography.
-
Stress echocardiogram.
-
Cardiopulmonary exercise test (CPEX).
-
Lung function tests.
-
Step by Step Summary: Open AAA Repair
-
1.
A midline or transverse abdominal incision is made for direct visualisation of the AAA.
-
2.
Dissection of the aneurysm neck and proximal iliac arteries is carried out to allow the aorta to be clamped.
-
3.
The aorta and iliac arteries are clamped.
-
4.
The aneurysm sac is opened and the thrombus is removed.
-
5.
The back bleeding lumbar arteries are oversewn.
-
6.
The top end of the graft is stitched to the aneurysm neck.
-
7.
The bottom end of the graft is stitched to the aortic bifurcation.
-
8.
The graft is flushed to make sure there are no clots that could travel down the vessels supplying the legs.
-
9.
The clamp is released after warning the anaesthetist.
-
10.
The aneurysm sac is closed around the graft to protect the artificial graft from the bowel.
-
11.
The abdominal incision is closed.
Complications
-
Bleeding.
-
Renal failure.
-
Respiratory failure.
-
Cardiac complications.
-
Leg ischaemia:
-
May require amputation.
-
-
Bowel ischaemia.
-
Spinal cord ischaemia.
-
Death.
Follow-Up
Most patients are seen in outpatients 8 weeks after undergoing an open repair, and then discharged.
Carotid Endarterectomy
This procedure can be carried out to relieve stenosis and remove blockages of the carotid arteries in carotid artery disease.
Indications
-
Carotid stenosis of greater than 50 % with symptoms including:
-
TIA within the preceding 14 days affecting the appropriate cerebral hemisphere.
-
Stroke within the preceding 14 days affecting the appropriate cerebral hemisphere.
-
Amaurosis fugax (transient loss of sight in one eye) or central retinal artery occlusion.
-
-
Asymptomatic carotid artery stenosis of greater than 70 %:
-
Controversial in the UK.
-
ACST trial supports carotid surgery for patients <75 years old [2].
-
Contraindications
-
Previous surgery or radiotherapy to the patient’s neck.
-
Patient not fit for open surgery.
Presentation
-
Symptomatic patients are usually referred from stroke physicians:
-
Present with cerebrovascular accidents such as TIAs and strokes, amaurosis fugax or central retinal artery occlusion.
-
-
Asymptomatic patients are referred from a variety of sources:
-
These patients have usually had a carotid duplex scan because of cardiovascular co-morbidities.
-
Investigations
-
Carotid duplex ultrasound scan.
-
CT angiogram.
-
Magnetic resonance angiogram.
-
Transcranial doppler.
Step by Step Summary: Carotid Endarterectomy
-
1.
Local or general anaesthetic may be used.
-
2.
An incision is made along the anterior border of sternocleidomastoid. Incision length is 5–10 cm, depending on the site of the stenosis.
-
3.
The common, internal and external carotid arteries are dissected out. The cranial nerves must be avoided.
-
4.
Slings are placed around the above arteries
-
5.
The arteries are clamped and a longitudinal arteriotomy is made on the distal common carotid and proximal internal carotid artery.
-
6.
Endarterectomy (removal of plaque) is carried out on the insides of the common and internal carotid arteries.
-
7.
The arteriotomy incision is closed with a patch to prevent narrowing. At this point the surgeon must ensure there is no bleeding.
-
8.
Ideally there should be intraoperative assessment of the surgical result with on table duplex or angioscopy.
-
9.
The platysma muscle and skin are closed with dissolvable stitches.
-
10.
Recovery takes place in a High Dependency Unit to monitor any signs of bleeding or new neurological symptoms.
Complications
-
Bleeding.
-
Perioperative stroke.
-
Cranial nerve injury.
-
Numbness of earlobe and angle of the jaw on the side of surgery.
Follow-Up
The carotid duplex ultrasound scan is repeated (as an outpatient procedure) to assess success of the endarterectomy.
Femoro-Popliteal Bypass
Indications
-
Critical limb ischaemia.
-
Short distance claudication.
-
Popliteal artery aneurysm.
Contraindications
-
Patient unfit for open surgery.
-
No autologous vein available for bypass (relative contraindication).
Presentation
-
Rest pain.
-
Tissue loss or gangrene.
-
Claudication upon walking less than 20–30 m (short distance claudication).
-
Popliteal aneurysm greater than 2 cm.
Popliteal aneurysms often occlude suddenly. The patient will suffer acute limb ischaemia, which presents with the 6 P’s:
-
1.
Pain.
-
2.
Paraesthesia.
-
3.
Pallor.
-
4.
Pulselessness.
-
5.
Paralysis.
-
6.
Perishingly cold.
Investigations
-
Arterial duplex ultrasound scan.
-
CT angiogram.
-
Intra-arterial digital subtraction angiogram.
-
Magnetic resonance angiogram.
-
Vein map.
Step by Step Summary: Femoro-Popliteal Bypass
-
1.
General anaesthetic or an epidural is administered.
-
2.
A vertical or transverse incision is made in the groin to allow dissection of the common femoral and proximal superficial and deep femoral arteries.
-
3.
A vertical incision is made behind the tibia to allow dissection of the popliteal artery and harvest of the great saphenous vein.
-
4.
The great saphenous vein is harvested throughout its length.
-
5.
The vein is turned around (reversed) and tunnelled from the femoral artery to the popliteal artery.
-
6.
The vein is joined to the common femoral artery at the top and the popliteal artery at the bottom. The foot should pink up at this point.
-
7.
The wound is closed and bandaged.
Complications
-
Graft occlusion.
-
Wound complications e.g. infection.
-
Reperfusion injury.
-
DVT.
-
Nerve injury.
Follow-Up
Graft surveillance is carried out as an outpatient procedure.
Varicose Vein surgery
This procedure, carried out to repair varicose veins, is commonly asked about in exams!
Indications
-
Absolute indications:
-
Recently healed venous ulcer.
-
Recent superficial thrombophlebitis (inflammation of a vein just under the skin).
-
Bleeding varicose vein.
-
Skin changes related to superficial venous reflux such as lipodermatosclerosis (hard, pigmented skin on the legs due to venous insufficiency).
-
-
Relative indications:
-
Painful varicose veins.
-
To improve cosmetic appearance.
-
Contraindications
-
Previous DVT with elements of deep venous obstruction.
Presentation
-
Described in the ‘Core Knowledge’ section.
Investigations
-
Venous duplex ultrasound scan.
Step by Step Summary: Varicose Vein Surgery
Open Approach:
-
1.
A transverse cut is made 2 cm below and lateral to the pubic tubercle.
-
2.
The superficial femoral vein and its tributaries are dissected. The femoral vein is identified.
-
3.
The superficial femoral vein and its tributaries are ligated.
-
4.
The great saphenous vein is stripped to below the knee.
-
5.
Varicose veins of the calf and thigh are avulsed.
-
6.
The groin wound is closed.
-
7.
The leg is bandaged.
Endovascular ablation:
-
1.
Local anaesthetic is administered.
-
2.
Ultrasound is used to identify the great saphenous and superficial femoral veins.
-
3.
The veins are cannulated using a wire and sheath.
-
4.
A heat ablation catheter is inserted; either laser or radiofrequency ablation is used.
-
5.
The superficial femoral and great saphenous veins are heat ablated throughout their length.
-
6.
There is one small cut which is closed with a piece of surgical tape.
-
7.
The leg is bandaged.
Complications
-
Haematoma formation.
-
Paraesthesia.
-
Phlebitis (endovascular technique).
-
DVT:
-
Rare but catastrophic.
-
Occurs in less than 1 % of patients when the endovascular approach is used.
-
Occurs in approximately 3 % of patients when the open approach is used.
-
Follow-Up
Not required in most patients.
Embolectomy
An embolectomy is the surgical removal of a blood clot blocking an artery. It is often carried out as an emergency operation. This section describes the removal of a clot in the femoral artery.
Indications
-
Acute limb ischaemia.
Contraindications
If ischaemia has been present for too long, it may be too risky to reperfuse the ischaemic limb. Amputation may be required under these circumstances.
Presentation
-
The 6 P’s of acute limb ischaemia (see above).
-
Patients may present with atrial fibrillation.
-
Patients usually present as an emergency.
Investigations
-
CT Angiogram.
Step by Step Summary: Embolectomy
-
1.
Local or general anaesthetic is administered.
-
2.
The common femoral artery is dissected out.
-
3.
A transverse arteriotomy is performed.
-
4.
A Fogarty catheter is passed through the artery to retrieve the clot blocking it.
-
5.
The artery is flushed and back bled to make sure that there is no residual clot.
-
6.
The artery is closed.
-
7.
The limb is reperfused and if successful the foot should at this point pink up.
-
8.
The incision is closed.
Complications
-
Compartment syndrome.
-
Haematoma formation.
-
Amputation may be required.
Follow-Up
Follow-up is usually not required.
Surgeons’ Five Favourite Questions for Students
-
1.
Define what an aneurysm is.
-
2.
What are the indications for surgical repair of an AAA?
-
3.
Which three cranial nerves are at risk during carotid endarterectomy?
-
4.
Name the different sources of emboli
-
5.
What is the difference between an embolus and an in-situ thrombosis?
Student Tips for Placement
A grasp of anatomy, especially the arterial tree, is essential for full understanding of most vascular procedures. When going into theatre, try and find out what procedures you will be observing and read up on them beforehand. Endovascular approaches are common, so read up on the equipment involved. Don’t be afraid to ask questions!
Careers
Vascular surgery is an incredibly varied and exciting specialty. It attracts people who are risk-takers, who like hard work and exciting surgery.
It is technically challenging and requires knowledge of full body anatomy. Vascular on call is unique because it is not possible to tuck a patient with a bleeding aneurysm or acute ischaemic leg up in bed and leave them until the next day – they require operating on as an emergency procedure, which will mean operating on them overnight.
The training pathway for vascular surgery in the UK is the same as for most other surgical specialties. After medical school, you enter foundation training, and then core surgical training before specialising at ST3 level.
Bibliography
Ferguson GG, Eliasziw M, Barr HW, Clagett GP, Barnes RW, Wallace MC, et al. The North American symptomatic carotid endarterectomy trial surgical results in 1415 patients. Stroke. 1999;30:1751–8.
Halliday A, Harrison M, Hayter E, Kong X, Mansfield A, Marro J, et al. 10-year stroke prevention after successful carotid endarterectomy for asymptomatic stenosis (ACST-1): a multicentre randomised trial. Lancet. 2010;376:1074–84.
Sakalihasan N, Limet R, Defawe O. Abdominal aortic aneurysm. Lancet. 2005;365:1577–89.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Ahmad, A.N., Bell, R. (2017). Vascular Surgery. In: Fisher, R., Ahmed, K., Dasgupta, P. (eds) Introduction to Surgery for Students. Springer, Cham. https://doi.org/10.1007/978-3-319-43210-6_18
Download citation
DOI: https://doi.org/10.1007/978-3-319-43210-6_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43209-0
Online ISBN: 978-3-319-43210-6
eBook Packages: MedicineMedicine (R0)