Abstract
“Pain caused by a lesion or disease of the somatosensory nervous system” is a definition for neuropathic pain according to the International Association for the Study of Pain. “Lesion” refers to an abnormality found on a diagnostic test (e.g., evidence of demyelination); “disease” refers to a known process causing a lesion (e.g., Guillain-Barre Syndrome). This lesion or disease-causing neuropathic pain may be in either the central or peripheral nervous system.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Lesion
- Dyesthesias
- Neuropathic Pain Questionnaire
- Symmetric
- Diabetic neuropathy
- Trigeminal neuralgia
- Ligand
- Topical agents
- Opioids
- Spinal cord stimulation
Neuropathic Pain: Definition
“Pain caused by a lesion or disease of the somatosensory nervous system” is a definition for neuropathic pain according to the International Association for the Study of Pain. “Lesion” refers to an abnormality found on a diagnostic test (e.g., evidence of demyelination); “disease” refers to a known process causing a lesion (e.g., Guillain-Barre Syndrome). This lesion or disease-causing neuropathic pain may be in either the central or peripheral nervous system .
Prevalence
A recent systematic review of epidemiological studies has estimated that neuropathic pain has a prevalence of between 6.9 and 10 % in the population .
Evaluation and Diagnosis
The onset and progression of neuropathic pain is often gradual, and symptoms may be spontaneous or evoked. Its hallmark dysesthesias may be described by a range of phrases (e.g., “burning,” “pins and needles,” “shock-like”) and pain may be associated with hyperalgesia and allodynia, as well as motor and autonomic disturbances. Validated questionnaires are available to identify neuropathic elements of pain (e.g., the Neuropathic Pain Questionnaire).
The initial approach to assessing a patient with neuropathic pain is to determine the territory of neuropathic symptoms and signs. A common presentation is of a symmetric , length-dependent pattern of injury that starts in the feet, which are innervated by the longest axons, and progresses upward. Presumably, a systemic stressor (e.g., hyperglycemia) reaches all nerves, but has the greatest impact on those axons furthest from their cell body. In contrast, an asymmetric, non-length-dependent neuropathy affects both proximal and distal territories and is not symmetric (e.g., CIDP).
Next in the evaluation, take note of the affected modalities: sensory, motor, or autonomic axons. Sensory involvement is a predominant component of almost all neuropathies; motor involvement may occur as a late finding of a symmetric, length-dependent process, or early in the disease course when demyelination occurs (e.g., CIDP, Charcot-Marie-Tooth). Autonomic involvement is overall rare, but common in certain conditions (e.g., diabetic neuropathy).
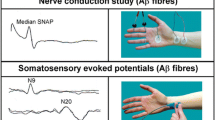
Further in your evaluation, consider whether the pathology is occurring at the axon or myelin sheath. With axonal injury, deep tendon reflexes are preserved and muscles atrophy; with myelin injury, reflexes are lost and muscle bulk is preserved. If in doubt, NCS/EMG can confirm the etiology of the deficit. If a small fiber neuropathy is suspected, a skin punch biopsy may be performed .
While most patients presenting to a pain specialist with a painful neuropathy have an established diagnosis, understanding the basic pathophysiology of neuropathic pain is important as this may guide treatment.
Etiologic Classification
Painful neuropathies can be classified by their etiology.
Symmetric , length-dependent processes can be caused by metabolic (e.g., diabetic neuropathy), infectious (e.g., HCV, HIV), toxic (e.g., heavy metals, chemotherapeutics), nutritional (e.g., thiamine deficits in Beriberi), or genetic abnormalities (e.g., Charcot-Marie-Tooth, Fabry’s). Non-length-dependent processes may be caused by autoimmune demyelinating (e.g., GBS, CIDP) or vasculitic (e.g., polyarteritis nodosa) disorders.
Examples of Common Painful Neuropathies
Diabetic neuropathy is the most common painful neuropathy and is discussed in detail elsewhere in this text, as are CRPS and PHN .
Trigeminal neuralgia typically manifests as paroxysmal, lancinating, unilateral pain in the distribution of the maxillary nerve, although the pain may also be bilateral and involve other branches of cranial nerve V. A common trigger is light touch, as occurs with daily activities such as shaving, tooth brushing, and eating. MRI can be used to evaluate for secondary causes such as vascular compression by the superior cerebellar artery or a demyelinating process such as multiple sclerosis. The clinical diagnosis, however, is made by history and does not require additional tests. An effective pharmacologic treatment is carbamazepine, the use of which requires frequent follow-up to evaluate for the development of agranulocytosis. Acute, severe exacerbations may be treated with IV phenytoin. Microvascular decompression or percutaneous, neuroablative procedures should be reserved for refractory cases.
Treatment Modalities
For patients with neuropathic pain, treatment should be provided for their underlying disease process—avoidance of hyperglycemia will, for example, help slow the progression of diabetic neuropathy .
Much of the research on pharmacologic interventions to treat neuropathic pain has been based on diabetic neuropathy; often, the promising agents from these trials are then applied to other painful neuropathies.
Another consideration is that neuropathic pain is stubbornly difficult to treat and often requires multiple medications to achieve satisfactory pain relief. Furthermore, many of the medications known to effectively treat neuropathic pain, such as tricyclic antidepressants and anticonvulsants, are known to have anti-cholinergic, anti-histaminergic, and other troublesome side effects. Therefore, a less effective agent but one with a better safety profile may be first used, especially in the elderly patient.
Pharmacologic treatment usually begins with an α2δ ligand such as gabapentin. Next, one may consider the addition of an SNRI such as duloxetine, a TCA, or another anti-convulsant. Additional pharmacologic treatments include topical agents (e.g., capscaicin) and, for patients who show benefit, opioids .
Spinal cord stimulation and peripheral nerve stimulation are additional treatment modalities appropriate for some patients with neuropathic pain (e.g., SCS for CRPS). These modalities are discussed elsewhere in this text.
Additional Reading
Heck O, Austin S, Khan R, Smith B, Torrance N. Neuropathic pain in the general population: a systematic review of epidemiological studies. Pain. 2014;155:654–62.
Walk D, Backonja MM. Chapter 24: Painful neuropathies. In: Fishman S, Ballantyne J, Rathmell JP, editors. Bonica’s management of pain. 4th ed. New York: Williams & Wilkins; 2009. p. 304–14.
Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ. 2014;17:348–57.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Abrecht, C.R., Nedeljkovic, S.S. (2017). Neuropathic Pain. In: Yong, R., Nguyen, M., Nelson, E., Urman, R. (eds) Pain Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-43133-8_145
Download citation
DOI: https://doi.org/10.1007/978-3-319-43133-8_145
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43131-4
Online ISBN: 978-3-319-43133-8
eBook Packages: MedicineMedicine (R0)