Abstract
Damage-control laparotomy and temporary abdominal closure have become important components of the armamentarium of many surgeons. Although the goal was to achieve delayed primary fascial closure in these patients, the most critically injured patients will require a different management scheme. We apply a 3-staged management algorithm to patients in whom delayed fascial closure is unattainable and will require future abdominal wall reconstruction. We will share lessons that we have learned after studying abdominal wall reconstruction for the past 25 years. We found that the standard component separation technique was insufficient to close the giant abdominal wall defects. For this reason, we developed a modification that we refer to as the Memphis modification for component separation. This modification allows us to reconstruct the abdominal wall using native tissue in a greater number of patients and thus avoids insertion of prosthetics. We will review the preoperative workup for planned ventral hernia repair, give a detailed step-by-step intra-operative description of the Memphis modification, and discuss postoperative complication and long-term results.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Damage-control laparotomy
- Temporary abdominal closure
- Planned ventral hernia
- Abdominal wall reconstruction
- Component separation
Introduction
Temporary abdominal closure has become an important component of the armamentarium of many surgeons. Several scenarios, including abdominal compartment syndrome, damage-control laparotomy for trauma, or repeated laparotomies with intra-abdominal catastrophe, call for surgeons to have an algorithm for the management of open abdomens. Attempts at fascial closure under tension often lead to fascial necrosis and/or abdominal compartment syndrome.
Various techniques have been utilized in the final phase of abdominal wall reconstruction. When prosthetic materials are used for reconstruction, the most severe complications are mesh infection and recurrent hernia. Many of the prosthetic infections occur when the mesh is inserted in conjunction with intestinal contamination such as stomal or fistula closure. Many of the patients that we care for with the planned ventral hernias have stomas that require concurrent reversal of these stomas at the time of abdominal wall reconstruction.
In 1990, Ramirez and associates [1] first described the component separation technique that allows closure of the abdominal wall using the native fascial layers without the use of prosthetics. We found that the standard component separation was insufficient to close the giant defects that represent a large portion of our patient population. For that reason, we developed a modification that we refer to as the Memphis modification for the component separation [2] that allows more extensive mobilization and advancement of autologous tissues. We have found that the modification allows us to close a large portion of giant abdominal wall defects without the use of permanent mesh.
Factors that have been identified which are predictors of failure to achieve native fascial closure of open abdomens during initial hospitalization after trauma include greater number of subsequent explorations, intra-abdominal abscess/sepsis, blood stream infections, acute renal failure, development of enteric fistula, and higher injury severity score [3]. Others have identified that waiting greater than 48 h before the first take back after initial damage-control laparotomy is negatively associated with achieving primary fascial closure. The failure to return to the operating room within 48 h has been found to carry with it a real and increased risk of not achieving fascial closure of 1.1 % per hour of delay [4]. These predictors can help identify patients early in their hospital course that are high risk for needing future abdominal wall reconstruction and can be managed using a staged algorithm.
Staged Management Approach
We apply a 3-staged management algorithm to critically ill patients with abdominal catastrophes that may require future abdominal wall reconstruction. Figure 19.1 demonstrates this management scheme. Stage I is the damage-control laparotomy and temporary abdominal closure. The use of damage control is highly selective at our institution, and only critically ill patients with major physiologic derangements have planned re-exploration. Temporary abdominal closure materials used at our institution include plastic materials such as X-ray cassette covers, blue towels placed to suction, as well as commercially available negative-pressure devices such as the ABThera (KCI). If we are unable to achieve delayed fascial closure with these materials, we then place vicryl mesh. After the placement of vicryl mesh, we continue to attempt to tighten or cinch the mesh at bedside. The patients that are not amendable to fascial closure at this point, despite aggressive attempts, progress to the next stage. This group of patients comprises the patients that will have future abdominal wall reconstruction. Stage II occurs approximately 2 weeks after granulation tissue has developed under the temporary closure. The temporary closure is removed, and a split-thickness skin graft is placed over the viscera. Stage III is the definitive reconstruction of the abdominal wall and is usually performed 8 months later. The assessment of the readiness to remove the skin graft is determined by “pinching” the graft to see whether it can be easily lifted from the underlying viscera as seen in Fig. 19.2. Occasionally, this can occur as early as 6 months. If definitive reconstruction is attempted too early, the adhesions are very dense, and this leads to unwanted enterotomies and deserosalization of the bowel, which can lead to subsequent intra-abdominal abscesses and/or enteric fistulas. The reason to proceed with the reconstruction no later than 12 months is that further delay can lead to fascial retraction laterally and loss of domain that makes reconstruction more difficult and carries a high chance of needing to use prosthetic mesh.
Flow diagram representing the 3-staged approach to abdominal closure. Reproduced with permission from Dicocco et al. [7]
Lessons Learned from Previous Studies
We would like to share some practical lessons that we have learned after studying abdominal wall reconstruction for the past 25 years. In our initial years of planned ventral hernia management, the choice of temporary abdominal closure prosthetic was a decision that was left to the operating surgeon, and the prosthetics included polypropylene mesh, woven vicryl mesh, expanded PTFE soft tissue patch, and plastic (intravenous fluid bag or X-ray cassette cover). The application of a variety of prosthetic materials in our institution in the past has provided a perspective on merits and drawbacks of each material. The removal of polypropylene mesh is not a simple procedure and is very time consuming and carries a higher risk of injury to bowel. The cost and difficulty of removal of expanded PTFE were made evident in the past studies, and the lack of durability of plastic material used for coverage has led to a change in our practice. These factors have been responsible for the gradual switch to absorbable mesh with woven vicryl being chosen most frequently at our institution [5].
Another lesson that we have learned over the past decade is that it is best to immediately place the skin graft at the time of vicryl mesh removal. In our early experience, we performed dressing changes for a couple of days to diminish nosocomial bacterial colonization of the granulated wounds before applying the skin graft. However, we had patients during those few days that eviscerated and had resulting derserosalization that resulted in difficult to management enteric fistula [2]. This has led to our change in practice, and now all patients receive immediate STSG at the time of mesh removal.
We have also determined that it is best to remove the mesh and place the skin graft no later than 3 weeks after mesh placement [2]. Those patients who had mesh retention beyond 3 weeks were found to have a significant increased risk of intestinal fistula. For this reason, we strive to remove the vicryl mesh and place STSG on these patients approximately 2 weeks after placement of the vicryl mesh.
There have also been many proponents of vacuum-assisted closure (VAC) to aid in the delayed primary fascial closure rates. We performed a prospective randomized trial to address the rates of delayed fasical closure and fistula rates comparing temporary closure with vicryl mesh versus VAC in patients with open abdomens [6]. Our results indicated that the VAC group trended toward increased morbidity. There was an increase in fistula rates in the VAC group, and we believe this was due to the need for repeated vacuum changes that are not required with vicryl mesh. We also found that enteral gastrostomy and jejunostomy tubes that were placed had a higher rate of becoming dislodged with the repeated vacuum dressing changes. We also had patients with loss of domain and massive visceral edema that experienced evisceration with VAC closure. The study found that neither method was superior in regard to the rates of delayed fascial closure. For these reasons, we have adopted absorbable vicryl mesh followed by skin grafting for those patients in whom delayed fascial closure seems unlikely.
We have also found that delaying definitive abdominal wall reconstruction beyond 1 year directly contributes to the need for prosthetic mesh as well as increases the rate of hernia recurrence [2]. Delay beyond 1 year leads to loss of domain and decreased fascial compliance due to contraction and consequent retraction of the abdominal wall fascia laterally. For this reason, we carefully follow all patients discharged with planned ventral hernias at 3-month intervals to assess the readiness of removal of their skin graft and definitive reconstruction.
Review of Abdominal Wall Anatomy
Published in 1990 by Ramirez et al. [1], component separation is based on subcutaneous lateral dissection, fasciotomy lateral to the rectus abdominis muscle, and dissection on the plane between external and internal oblique muscles with the medial advancement of the block that includes the rectus muscle and fascia. This release allows 3–5 cm of the additional length on each side. Because of the giant abdominal wall defects (Fig. 19.3) that occur after open abdomens, we developed a modification that results in an additional 20 cm in the umbilical region that allows the closure of many giant planned ventral hernias with native tissue only.
Preoperative images of a patient with a planned ventral hernia. Giant abdominal wall defect is covered with skin graft over the abdominal viscera. Reproduced with permission from Dicocco et al. [7]
Before describing the technique in depth, a brief review of the abdominal wall anatomy (Fig. 19.4) will facilitate understanding the procedure. The rectus muscle is surrounded by the anterior and posterior rectus sheaths. The external is a component of the anterior rectus sheath for the entire length of the rectus. The internal oblique splits and contributes to both the anterior sheath and posterior sheath above the arcuate line. However, below the arcuate line, the entirety of the internal oblique joins the anterior sheath. The transversus abdominis also contributes to the posterior sheath above the level of the arcuate line, but likewise joins the anterior sheath inferior to this landmark. This leaves no posterior sheath below the arcuate line and where only the peritoneum is present.
Diagram of abdominal wall anatomy, shown from the intraperitoneal surface, with cut edge representing the cephalad portion. The arcuate line, vascular supply, and components of the rectus fascia can be seen. Reproduced with permission from Dicocco et al. [7]
The blood supply to the rectus is supplied by the superior epigastric and the deep inferior epigastric arteries, with the inferior providing the major component. The inferior epigastric artery lies between the internal oblique and transversus abdominis muscles. It enters the rectus sheath around the arcuate line. Therefore, separation of the anterior rectus sheath laterally does not compromise blood supply. Blood supply to the anterior sheath is also from epigastric vessels. For this reason, separation of the anterior sheath from the rectus is not ideal. The posterior sheath obtains its vasculature from the vessels supplying the peritoneum and can be separated from the rectus without becoming devascularized.
Preoperative Evaluation in Preparation for Planned Ventral Hernia Repair
Patients that are managed with an open abdomen and a staged management algorithm often have a prolonged hospital course. Upon discharge, we closely follow these patients in clinic. Once out of the acute phase, we see these patients at 3-month intervals to assess the readiness of the skin graft for removal. The technique, as mentioned before and seen in Fig. 19.3, requires lifting and “pinching” the graft to see whether it can be lifted off the underlying viscera. The technique takes some experiences, and the decision to proceed with definitive abdominal wall reconstruction is made by the attending physician. In preparation for reconstruction, many of these patients also have diverting ostomies that require endoscopy and/or contrasted enemas to determine whether they are ready to be reversed. These studies are obtained concurrently with the preparation for their planned ventral hernia repair. Because we use the modification of the component separation at our institution frequently, if we anticipate the patient will have a planned ventral hernia, the initial ostomy location can be placed lateral to the rectus sheath so that the fascial defect from the ostomy can be closed primarily or with a small piece of biologic mesh. Again, we strive to repair all planned ventral hernias between 8 and 12 months after the placement of the skin graft to avoid the loss of domain that comes if the operation is delayed for more than 1 year.
Preoperative assessment can be deceiving, so the reconstruction technique should be decided intraoperatively. Patients who have very large defects may have mobile fascia and can be closed with a standard component separation. Conversely, some patients with small defects may require the Memphis modification and possible addition of prosthetic material.
This patient population has had significant physical and psychological stress due to their major trauma and prolonged hospital course. We have long discussions with these patients before proceeding with definitive reconstruction. They are again faced with a 7- to 10-day hospital stay, if no complications arise. We review in-depth complications that can occur and make patients aware that abdominal wall reconstruction results in a significant abdominal pressure and transient discomfort postoperatively. We often use epidural catheters perioperatively in these patients to help with pain control.
Operative Technique of Memphis Modification for Component Separation
Now we would like to provide a step-by-step description of our technique and include some intraoperative pearls and pitfalls that we have learned [7].
-
1.
Removal of the skin graft. Beginning in an area that is loosely adherent, there will be areas with dense adhesions. In these areas, a plane between the dermis and epidermis is developed. Small areas of skin graft can be left on the viscera to avoid serosal injuries without any consequence. The skin graft is excised from the native abdominal wall laterally to preserve skin edges. Once the graft is removed, the bowel is examined thoroughly for serosal injuries or enterotomies, which are not uncommon. Ostomy reversal is done at this point.
Pearls/Pitfalls: It is started at the midpoint of the skin graft because this is the least adherent area. The graft is often very densely adhered to the liver so the use of sharp dissection can avoid violation of Glisson’s capsule. The musculofascial junction is left for last, and the rest of the dissection is completed circumferentially dissecting the skin graft from the underlying viscera and omentum.
-
2.
Raise full-thickness skin flaps. After the skin graft has been removed, skin flaps are raised on each side with the plane of dissection being just superficial to the fascia. There are perforating vessels that are encountered, and we attempt to preserve these. We raise flaps laterally to the level of the mid-axillary line (Fig. 19.5).
Fig. 19.5 Step 2. Skin flaps, with attached subcutaneous tissue, are raised to expose the underlying fascia. a The skin flap is raised several centimeters lateral to the border of the rectus sheath. b Skin and subcutaneous tissue flap are being raised. Reproduced with permission from Dicocco et al. [7]
Pearls/Pitfalls: The correct plane is found just superficial to the fascia. Failure to do so will result in a longer and bloodier dissection. Going too deep will result in defects in the fascia and complicate the reconstruction. Be cautious and avoid devascularization of the skin by keeping as much fat as possible with the cutaneous flap. This is very important with thin patients.
-
3.
Release of the external oblique. The lateral edge of the rectus muscle is identified. The location can be confirmed by placing a hand in the abdomen with the palmar surface deep to the rectus and the thumb on top. The external oblique is nicked 1 cm lateral to the rectus border using a scalpel. A hemostat is inserted into the opening to elevate the external oblique and extend the incision with electrocautery. The extent of the release of the external oblique is from the costal margin to the level of the pubic symphysis (Fig. 19.6). There is a loose areolar tissue between the external and internal oblique laterally. Blunt dissection of this plane allows improved medial mobilization. Also, the serratus anterior may be encountered during the cephalad dissection, and release of this muscle will help with mobilization.
Fig. 19.6 Step 3. The external oblique release is extended cephalad toward the costal margin and caudally to the level of the pelvis. a Once the external oblique fascia is incised, the internal oblique can be visualized deep to this. b The elevated skin flap and cut external oblique fascia are shown. Reproduced with permission from Dicocco et al. [7]
Pearls/Pitfalls: Care must be taken to only incise the external oblique. The internal oblique can be easily pulled up and inadvertently incised, and this will compromise the repair. It is important to make sure that you correctly identify the lateral border of the rectus and make a nick 1 cm lateral to this landmark. If the incision is too medial (over the lateral border of the anterior sheath), there will be much less ability to mobilize the rectus.
Steps 1–3 constitute a standard component separation. The Memphis modification begins with the remaining steps.
-
4.
Dissection of the posterior rectus sheath. The medial portion of the rectus sheath is incised for the entire length of the muscle. This exposes the anterior and posterior fascia and rectus muscle as 3 distinct layers (Fig. 19.7). Next the posterior sheath is freed from the rectus muscle. This dissection is carried out to the level of the arcuate line. At this level, the posterior rectus sheath is comprised only of peritoneum.
Fig. 19.7 Step 4. The medial edge of rectus sheath is divided, as seen from midline. a The posterior sheath is dissected off the rectus muscle to the level of the arcuate line caudally. b The 4 layers apparent at this stage: Skin flap, released external oblique, rectus muscle with the attached anterior sheath, and posterior sheath. Reproduced with permission from Dicocco et al. [7]
Pearls/pitfalls: The dissection plane between the rectus and the posterior sheath is relatively avascular. Usually, the epigastric vessels are intramuscular, but can run deep to the rectus muscle so be cautious so as not to avulse them.
-
5.
Release of internal oblique. Once the posterior sheath is freed, a hand is placed between the rectus muscle and the posterior sheath. With this hand cupping the rectus, the index finger is used to identify the lateral border of the rectus muscle. Now the anterior fascia is sharply incised over the index finger 1 cm lateral to the rectus. This maneuver opens the anterior portion of the internal oblique fascia and protects the posterior sheath. The incision extends the length of the rectus from the costal margin down to the arcuate line (Fig. 19.8). The rectus muscle with the adherent anterior sheath is now free medially and laterally.
Fig. 19.8 Step 5. Release of internal oblique component. a Technique used to open the internal oblique component of the anterior rectus sheath. The dorsum of the hand is lying on the posterior sheath with the palmar surface cupping the rectus muscle. The incision is made directly over the surgeon’s finger to ensure that only the anterior component is divided. b Once step 5 is completed, the anterior sheath and rectus muscle are attached at only the cephalad and caudad portions. The posterior sheath is still in continuity with the native abdominal wall. Reproduced with permission from Dicocco et al. [7]
Pearls/Pitfalls: The technique of placing your hand between the posterior fascia and rectus muscles is the key to this step that allows your index finger to identify the correct location to incise the anterior component of the internal oblique. Cutting laterally to this (where the anterior and posterior portions of the internal oblique have combined) will result in a lateral defect. The umbilicus is generally close to the level of the arcuate line and can be used as a landmark. It is imperative that the dissection not be extended below the arcuate line because a lateral hernia will occur since there is no fascial component below this level.
-
6.
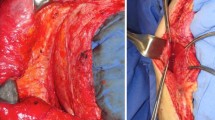
Translocation of the anterior fascia and muscle. At this point, the rectus muscle and the anterior fascia are attached only at their superior and inferior portions. These remaining attachments ensure that the blood supply is maintained. The posterior sheath remains in continuity with the native abdominal wall laterally. The rectus muscle and the anterior fascia can be pulled medially, and this provides the additional length that is obtained with the modification (Fig. 19.9). Now the medial aspect of the posterior sheath is sutured to the lateral aspect of the anterior sheath. This can be accomplished with running or interrupted figure-of-eight sutures.
Fig. 19.9 Step 6. The rectus muscle, along with the anterior sheath, is translocated medially. The posterior rectus sheath remains in continuity with the native abdominal wall laterally. a The rectus fascia is being mobilized. b The anchoring stitch is being placed, attaching the lateral border of the anterior fascia to the medial border of the posterior sheath. Reproduced with permission from Dicocco et al. [7]
Pearls/Pitfalls: Because fascia from 2 separate planes is being approximated, care is taken when placing the anchor stitch to close the potential space. The superior and inferior aspects of the suture lines will be puckered.
-
7.
Closure. The anterior sheath is then sutured in the midline in the normal fashion. This results in 3 separate suture lines (Fig. 19.10). The most difficult area to gain adequate length is in the epigastrium. If the fascia cannot be closed in the midline without tension, a prosthetic bridge may be necessary. We always closely communicate with anesthesia during closure to ensure that peak airway pressures are monitored and that we are notified with any significant change. Because we often combine ostomy reversal with abdominal wall reconstruction and the high incidence of enterotomies with this procedure, we prefer a biologic when a mesh is needed. The skin flaps are re-inspected to ensure hemostasis has been obtained. We insert four flat, closed suction drains (2 superiorly and 2 inferiorly). After debriding skin edges, the skin is reapproximated in the midline using interrupted nylon sutures.
Fig. 19.10 Step 7. Final closure. a Final fascial closure with 3 suture lines. The mobilized anterior sheath is sutured in midline. b Four closed suction drains are placed, and the skin flaps are reapproximated in the midline. Reproduced with permission from Dicocco et al. [7]
Pearls/Pitfalls: Hemostasis is critical because postoperative hematomas can lead to reoperation, skin necrosis, and failure of the repair. We place abdominal binders on all patients and instruct them to avoid heavy lifting for 6 weeks.
Wound Complications
Wound infection and/or skin necrosis are among the top reasons for failure of the repair. Wound seroma and hematoma prevention are imperative because both contribute to wound complications. Hematomas can be prevented intraoperatively with meticulous attention to hemostasis. All patients will have serous output from their drains due to the extent of mobilization. We only remove 1 drain at a time and generally remove the last drain between postoperative days 5–7.
Patients with high BMIs are especially at high risk for superficial skin necrosis due to the tension that their increased abdominal girth places on the skin edges and closure. If this occurs, the non-viable skin is debrided and local wound care is initiated. Thin patients are more susceptible to large areas of skin necrosis. This is thought to be due to the devascularization that can occur during the creation of skin flaps as a result of their decreased subcutaneous tissue and limited perforating vessels. After debridement of large areas, the fascia can be exposed, and we have utilized negative-pressure dressings to salvage repairs in these situations. A skin graft can be placed after granulation tissue develops. Although an infrequent complication, these patients have a high risk of recurrence.
Long-term Follow-up and Recurrence Rates
We have reviewed our experience with planned ventral hernias over a 15-year period with a mean follow-up greater than 5 years [8]. The spectrum of repairs ranged from patients that required no component separation or prosthetic to patients that required the modified component repair with the addition of a prosthetic mesh bridge. The highest rate of recurrence occurred in those patients with prosthetic-assisted closure with this group having a fourfold increase in the incidence of recurrence.
Higher BMI and female gender were also found to be risk factors for recurrence in this review. We were not surprised that increasing BMI was associated with recurrence. These patients often have larger defects and seem to have more substantial loss of domain. The reason for female gender being associated with recurrence is unclear. Theories that we have proposed include the weakening of the abdominal wall due to pregnancy and/or inherent anatomic muscular differences in men and women. We also noted that the presence of a fistula or ostomy was not associated with hernia recurrence.
For our patients who underwent a modified component separation without any prosthetic material, our recurrence rate with long-term follow-up was 5 %. This low recurrence rate with the excellent follow-up intervals provides good data which we feel shows that the Memphis modification for component separation is the procedure of choice for repair of giant planned ventral hernias.
We have also had the opportunity to review our long-term follow-up data on the quality of life after abdominal wall reconstruction [9]. These patients are essentially undergoing a “second hit” at the time of abdominal wall reconstruction after having a prolonged initial hospitalization that has left them physically and psychologically weakened. However, the results from this study show that the majority of patients can return to near normal quality of life after abdominal wall reconstruction, but this process can take several years. We follow these patients long term and provide support to assist them at achieving both physical and psychological goals.
Clinical Scenario
48-year old woman 3 years s/p Hartman’s for perforated diverticulitis. She has a right-sided transverse colostomy and a known complex hernia (two defects, the length of the incision, largest with a neck diameter 12 cm and a bulge diameter 20 cm, and a sizable medial paracolostomy hernia). She presents with bowel obstruction, intermittently decompressed with NG tube and intermittent air and stool from stoma.
The patient presented here represents a very different patient population than the population that has been the focus of our chapter on planned ventral hernias. Incisional hernias and planned ventral hernia are different entities. The fascia in a patient with a planned ventral hernia is usually normal, because most trauma patients are young and healthy. Incisional hernias often occur in patients who are older, have multiple comorbidities, and have shown that their fascia is compromised. The modified component separation technique is not ideal for patients with poor fascia or problems with wound healing, because it will likely result in recurrent hernia.
For the patient in this scenario, we would plan to take the patient to the operating room for reversal of her stoma, lysis of all adhesions, and repair of her midline incisional and parastomal hernia. Given the concomitant reversal of her colostomy, we would use a biologic mesh of choice of the operating surgeon. We would choose a piece of mesh large enough to obtain good overlap in the area of the parastomal hernia. The mesh would be fixated in an underlay fashion with an attempt to close the patient’s attenuated fascia over the mesh.
Key Questions
-
1.
What is the best way to reduce the risk of skin/flap necrosis?
-
2.
Which patients are at increased risk of failure of primary fascial repair?
References
Ramirez OM, Ruas E, Dellon AL. “Component Separation” method for closure of abdominal-wall defects: an anatomic and clinic study. Plast Reconstr Surg. 1990;86:519–26.
Jernigan TW, Fabian TC, Croce MA, Moore N, Pritchard FE, Minard G, et al. Staged management of giant abdominal wall defects: acute and long-term results. Ann Surg. 2003;238:349–55.
DuBose JJ, Scalea TM, Holcomb JB, Shrestha B, Okoye O, Inaba K, et al. Open abdominal management after damage-control laparotomy for trauma: a prospective observational American Association for the Surgery of Trauma Multicenter Study. J Trauma Acute Care Surg. 2012;74:113–22.
Pommerening MJ, DuBose JJ, Zielinski MD, Phelan HA, Scalea TM, Inaba K, et al. Time to first take-back operation predicts successful primary fascial closure in patients undergoing damage control laparotomy. Surgery. 2014;156:431–8.
Fabian TC, Croce MA, Pritchard FE, Minard G, Hickerson WL, Howell RL, et al. Planned ventral hernia. Staged management for acute abdominal wall defects. Ann Surg. 1994;219:643–50.
Bee TK, Croce MA, Magnotti LJ, Zarzaur BL, Maish GO, Minard G, et al. Temporary abdominal closure techniques: a prospective randomized trial comparing polyglactin 910 mesh and vacuum-assisted closure. J Trauma. 2008;65:337–44.
Dicocco JM, Fabian TC, Emmett KP, Magnotti LJ, Goldberg SP, Croce MA. Components separation for abdominal wall reconstruction: the memphis modification. Surgery. 2011;151:118–25.
Dicocco JM, Magnotti LJ, Emmett KP, Zarzaur BL, Croce MA, Sharpe JP, et al. Long term follow-up of abdominal wall reconstruction after planned ventral hernia: a 15-year experience. J Am Coll Surg. 2009;210:686–95.
Zarzaur BL, Dicocco JM, Shahan CP, Emmett KP, Magnotti LJ, Croce MA, et al. Quality of life after abdominal wall reconstruction following open abdomen. J Trauma. 2010;70:285–91.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Barnard, D.L., Fabian, T.C. (2017). The Planning for the “Planned Ventral Hernia”. In: Diaz, J., Efron, D. (eds) Complications in Acute Care Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-42376-0_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-42376-0_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42374-6
Online ISBN: 978-3-319-42376-0
eBook Packages: MedicineMedicine (R0)