Abstract
The term “bowel dysfunction” includes constipation, diarrhoea and faecal incontinence.
Bladder bowel dysfunction (BBD) is a generic expression to describe children with lower urinary tract symptoms (LUTS) associated with intestinal dysfunction. The International Children’s Continence Society (ICCS) recommends the use of the Rome III Criteria for the diagnosis of functional disorders of evacuation in children. The Bristol Stool Form Scale (BSFS) is a practical tool utilized for the diagnosis and for the evaluation of the treatment response. Faecal incontinence has a considerable impact in children’s quality of life (QoL). The European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) developed different guidelines for treatment of constipation in infants and children.
Treatment requires a comprehensive programme, including the use of laxatives, toilet training, a proper diet, transanal irrigation and Malone Anterograde Continence Enemas (MACE). All these different approaches, conservatives or surgical, can be combined for a better efficacy and tailored on a single patient.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Bowel dysfunction
- Constipation
- Bladder bowel dysfunction (BBD)
- Bristol Stool Form Scale (BSFS)
- Faecal incontinence
- Lower urinary tract symptoms (LUTS)
- Polyethylene glycol (PEG)
- Transanal irrigation
- Malone Anterograde Continence Enemas (MACE)
The term “bowel dysfunction ” includes constipation, diarrhoea, faecal incontinence, inability to control bowel movements and rectal bleeding. The gastrointestinal and genito-urinary tract share several aspects, including the same embryonic origin, the same pelvic position, the same innervation and the same relation between pelvic floor and levator ani muscle.
The frequency of bowel movements in childhood decreases by an average of four per day in the first week of life, to 1.7 per day from the age of 2. During this period the stool volume increases up to ten times or more [1].
Respectively in the UK only the 34% of toddlers and in Brazil the 37% of children younger than 12 years old were defined constipated by their parents [2].
In absence of painful symptoms, parents often don’t take into account the bowel habits of children older than 4/5 years, and they pay less attention to the frequency of their children’s bowel movements while more to the urinary and faecal incontinence episodes [3].
Bladder bowel dysfunction (BBD) is a generic expression to describe children with lower urinary tract symptoms (LUTS) associated with intestinal dysfunction. In this clinical condition, bladder symptoms, such as urinary urgency, incontinence and urinary tract infections (UTI), are related to problems in bladder voiding . Commonly, constipation with or without faecal incontinence coexists with dysfunctional voiding as a result of non-relaxation of the pelvic muscle floor [3].
The International Children’s Continence Society (ICCS) recommends the use of the Rome III Criteria for the diagnosis of functional disorders of evacuation in children (Table 29.1).
We define constipation when the bowel movements are less than three per week, stools are hard and the evacuation is irregular and painful [4].
The Bristol Stool Form Scale (BSFS) represents a practical instrument extremely useful for the diagnosis and for the evaluation of the therapy response (Fig. 29.1).
In most children constipation is caused by bad eating habits. The result is the creation of hard stools, the reduction in frequency of bowel movements and abdominal pain that brings to voluntary refusal of evacuation. In other cases constipation is a chronic process in which the child, who is approaching the use of toilet and a voluntary faecal continence, has the tendency to retain the stools because of the unavailability of toilet or because occupied by games [5, 6].
Faecal incontinence usually is the result of leakage of loose stool that pass sideways to the hard stools present in the rectum. The loss occurs every time the child try to expel gases, and the muscles used to retain the stools do not ensure continence. Faecal incontinence is from three to six times more common among male than in female children. It has a significant impact in children’s quality of life (QoL) with a resulting loss of self-esteem, social isolation and depression [1].
The dilation of the rectum is caused by the presence of hard stools, which compress also the bladder. Furthermore, frequent pelvic spasms prevent full relaxation during urination and lead to an early termination of it with post-void residual. Klijn M et al. highlighted as in children with constipation and LUTS the average diameter of the rectal ampulla is 4.9 cm while in the control group is 2.1 cm [7]. Chronic constipation occurs in neurogenic bowel dysfunction (NBD), peripheral or central, such as spina bifida and spinal cord injuries. Faecal incontinence and constipation associated with myelomeningocele, anorectal malformations and Hirschsprung’s disease are common, debilitating and difficult to treat.
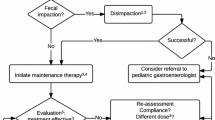
1 Bowel Dysfunction Management in Children
The treatment of constipation is different in infants and children. The European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) developed the guidelines and suggested to standardize the quality of health care, improving the evaluation and treatment of children with functional constipation . They also developed two algorithms: one for children <6 months of age and one for older children. The ESPGHAN insists on using the Rome III Criteria for classifying functional constipation . Children under 4 years should satisfy two of the criteria for at least 1 month, while those with more than 4 years should satisfy two of the criteria for at least 2 months. Abdominal pain , which is often associated, is not considered a criterion of functional constipation [8].
Functional constipation is often treated in infant with a high-fibre diet and regularization of water intake. If these measures are not successful, it is suggested the occasional administration of glycerin suppositories, which should be used carefully because they can cause anal irritation.
The treatment of chronic constipation and faecal incontinence in children requires a comprehensive programme, including the use of laxatives, toilet training and a proper diet [9].
The treatment of chronic constipation requires a complete voiding of the colon, in order to create a “working memory” and to make the intestine autonomous. The goal of the therapy is the passage of loose stools, preferably once per day.
During the treatment it is important to combine a diet that includes more fruits, raw vegetables, bran, whole bread, cereals and an adequate intake of liquids other than milk [8].
The use of probiotics to treat constipation in children is not supported by controlled trials in children and adults. They are defined as live microorganisms which, if given in adequate amounts, confer benefit to the host. Therapy with probiotics may be indicated together with other therapies.
Treatment with laxatives and toilet training is widely discussed in literature. Some studies support the combined use of both therapies [10, 11]. Some others support the laxative therapy as more effective than toilet training.
ESPGHAN and NASPGHAN suggest the use of polyethylene glycol (PEG without electrolytes—3350) from the first months of life. The treatment is generally effective and shows no side effects. The maintenance effective dose is about 0.8 g/kg of body weight per day [12].
The diagnostic and therapeutic approach to children with BBD should include the bladder voiding by bladder diary and the contemporary evaluation of constipation with BSFS (Fig. 29.1). Once anatomical abnormalities are excluded, behavioural therapy is generally regarded as the first-line treatment. The posture, the appropriate position on the toilet and the controlled voiding are the key points for the treatment of voiding dysfunction, associated with a proper bowel emptying [13].
Today an increasingly used technique is transanal irrigation of the bowel with appropriate devices as the Peristeen® irrigation kit (Coloplast A/S, Kokkedal, Denmark). This is particularly indicated in patients affected with neurogenic problems since their birth and all cases of chronic constipation or resistant to conventional therapy. Several studies demonstrated the effectiveness of transanal irrigation in reducing constipation, improving anal continence and improving QoL.
A randomized study compared transanal irrigation with best supportive bowel management without irrigation. As a result transanal irrigation significantly reduces the time of bowel management (47 vs. 74 min/day) and the rate of urinary tract infections and improves symptoms during and/or after defecation [14]. This procedure is relatively safe. The most severe complication is the risk of intestinal perforation, which occurs in 1 over 50,000 irrigations (0.002% of cases). Therefore transanal irrigation is not indicated in patients with bowel obstruction, inflammatory bowel disease and diverticulitis or in cases of recent abdomino-perineal surgery.
Patients with NBD can be treated in several ways. First of all, a conservative approach is suggested: the change of diet, drugs, electrical stimulation treatment, biofeedback and transanal irrigation. If conservative treatment is not effective, clinicians can suggest surgical procedures as MACE (Malone Anterograde Continence Enemas), colostomies and artificial bowel sphincters.
The antegrade delivery of cleansing solutions helps the patient to evacuate regularly the colon, avoid impaction of faeces and reduce faecal incontinence . Six open retrospective studies in children suggest how MACE can be an option in children with intractable constipation . Potential complication should be considered and examined with parents and children, as the development of granulation tissue, leakage around the tube, tube dislodgment, skin infection and stoma stenosis [8].
All these different approaches, conservatives or surgical, can be combined for better effectiveness and tailored on a single patient.
References
Abi-Hanna A, Lake AM. Constipation and encopresis in childhood. Pediatr Rev. 1998;19(1):23–31.
Loening-Baucke V. Urinary incontinence and urinary tract infection and their resolution with treatment of chronic constipation of childhood. Pediatrics. 1997;100(2, Part 1):228–32.
Halachmi S, Farhat WA. Interactions of constipation, dysfunctional elimination syndrome, and vesicoureteral reflux. Adv Urol. 2008;2008:828275.
Burgers RE, Mugie SM, Chase J, Cooper CS, von Gontard A, et al. Management of functional constipation in children with lower urinary tract symptoms: report from the standardization committee of the International children’s continence society. J Urol. 2013;190:29–36.
Issenman RM, Filmer RB, Gorski PA. A review of bowel and bladder control development in children: how gastrointestinal and urologic conditions relate to problems in toilet training. Pediatrics. 1999;103(6, Part 2):1346–52.
Solzi G, Di Lorenzo C. Are constipated children different from constipated adults? Dig Dis. 1999;17(5–6):308–15.
Klijn AJ, Asselman M, Vijverberg MAW, Dik P, de Jong TPVM. The diameter of the rectum on ultrasonography as a diagnostic tool for constipation in children with dysfunctional voiding. J Urol. 2004;172(5, Part 1):1986–8.
Tabbers MM, DiLorenzo C, Berger MY, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58:258.
Brazzelli M, Griffiths PV, Cody JD, Tappin D. Behavioural and cognitive interventions with or without other treatments for the management of faecal incontinence in children. Cochrane Database Syst Rev. 2011;12:CD002240.
Loening-Baucke V. Controversies in the management of chronic constipation. J Pediatr Gastroenterol Nutr. 2001;32(Suppl 1):S38.
Brooks RC, Copen RM, Cox DJ, et al. Review of the treatment literature for encopresis, functional constipation, and stool-toileting refusal. Ann Behav Med. 2000;22:260.
Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Members of Committees, Fourth International Consultation on Incontinence. Fourth international consultation on incontinence recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29:213–40.
Dos Santos J, Varghese A, Williams K, Koyle MA. Recommendations for the management of bladder bowel dysfunction in children. Pediat Therapeut. 2014;4:1.
Christensen P, Bazzocchi G, Coggrave M, et al. A randomized, controlled trial of transanal irrigation versus conservative bowel management in spinal cord-injured patients. Gastroenterology. 2006;131:738–47.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Masnata, G., Manca, V., Chia, L., Esu, F. (2018). Bowel Dysfunction Management. In: Mosiello, G., Del Popolo, G., Wen, J., De Gennaro, M. (eds) Clinical Urodynamics in Childhood and Adolescence. Urodynamics, Neurourology and Pelvic Floor Dysfunctions. Springer, Cham. https://doi.org/10.1007/978-3-319-42193-3_29
Download citation
DOI: https://doi.org/10.1007/978-3-319-42193-3_29
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42191-9
Online ISBN: 978-3-319-42193-3
eBook Packages: MedicineMedicine (R0)