Abstract
Liquid profiling is a traditional concept in laboratory diagnostics using patterns of blood-derived biochemical molecules for disease detection and characterization. Beyond protein and cellular parameters, molecular biomarkers at the DNA, RNA and miRNA level have been developed as promising diagnostic tools in metabolic and malignant diseases as new technologies for ultrasensitive profiling of nucleic acids in blood and body fluids became available. In cancer disease, they are successfully applied for the stratification of patients for individually tailored therapies, treatment monitoring and the sensitive detection of minimal residual disease. Due to its minimally invasive nature, blood-based qualitative and quantitative determinations of targeted and global molecular changes can be applied serially and complement well-established molecular tissue diagnostics. Interdisciplinary interaction between laboratory medicine, pathology and human genetics will speed up the development of liquid nucleic acid profiling as a most valuable tool for precision medicine.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
Circulating Nucleic Acids in Disease Detection and Management
Circulating blood is in contact with all organs in the human body and transports their genetic and metabolic products as well as molecules of cell damage or cell death. Qualitative and quantitative characterization of the biochemical constituents of the blood enables the diagnosis and staging of many diseases. Therefore, laboratory diagnostics in blood and other bodily fluids gained high importance in various medical disciplines. In most cases, the patterns of diverse proteins, lipids, glycans and nucleic acids were more meaningful than single markers and the understanding of the connection between the parameters became more relevant. Molecular medicine founded a new diagnostic era and has routinely been used for the identification of risk alleles in multifactorial diseases such as thrombosis or bleeding risk, of metabolic disorders as well as for pharmacogenetic testing. Molecular genetic testing efficiently complements the traditional strengths of phenotypical diagnosis and enables better understanding of complex medical issues by laboratory medicine approaches in interdisciplinary interplay with pathology and human genetics.
Beyond the identification of genetic risk factors, increasingly sensitive analytical methods have enabled the detection of circulating tumor cells (CTCs) as well as the qualitative and quantitative analysis of circulating cell-free DNA (cfDNA ) , RNA and microRNA in plasma and subcellular compartments like exosomes . The latter are nucleic acid-containing microvesicles actively secreted from cells with immunogenic properties. The different types and sources of circulating nucleic acids will gain increasing importance in all parts of diagnostic laboratory medicine.
During the last decades, circulating cell-free nucleic acids in plasma or serum (CNAPS) were detected in elevated concentrations after physical activity and in a variety of acute and chronic diseases such as in intensive care patients with organ dysfunctions, during sepsis, after trauma, myocardial infarction and stroke, organ transplantation and during cancer disease. Here it showed relevance for diagnosis, evaluation of prognosis and therapy monitoring of tumor diseases (reviewed in Fleischhacker and Schmidt 2007; Holdenrieder and Stieber 2009; Schwarzenbach et al. 2011; Crowley et al. 2013).
However, only disease-specific changes of CNAPS supported the better characterization and management of diseases, particularly in cancer disease. These include single mutations with loss or gain of gene sequences (e.g. in case of loss of heterozygosity (LOH) or microsatellite instability (MSI)) and numerical chromosomal aberrations ; further reversible epigenetic changes in the DNA methylation pattern of promotor sequences or various histone modifications that play a major role in transcriptional regulation; finally non-coding RNA markers like the 19–24 bp microRNAs or the long-non-coding RNAs (lncRNA) and gene expression profiles (mRNA) in various blood cells and compartments (reviewed in Fleischhacker and Schmidt 2007; Schwarzenbach et al 2011; Schwarzenbach 2015; Crowley et al 2013; Gezer and Holdenrieder 2014; Holdenrieder 2014). While these new diagnostic approaches are currently still at the research level they probably will greatly enrich the possibilities in future blood -based diagnostics.
The rapid developments in the techniques of massive parallel DNA sequencing (next generation sequencing, NGS) have recently enabled in-depth characterization of cfDNA right down to single bases. Nowadays, this is mainly applied in human genetics e.g. for the characterization of fetal DNA in maternal circulation, but recently has successfully been applied in the blood -based molecular characterization of cancer disease (Chiu et al. 2011; Diaz and Bardelli 2014). In this context, exact clarification of either individual, tumor-associated or specific molecular defects were performed as well as the identification of the entire tumor signatures from plasma cfDNA and CTCs (Speicher and Pantel 2014; Lianidou 2014). Beyond pure cancer diagnosis, so-called druggable targets were detected on CNAPS that allowed the individual stratification of patients for precise pathway-specific medications (Crowley et al. 2013). Circulating tumor DNA (ctDNA ) was reported to derive from necrosis , apoptosis or secretion of malignant cells or from circulating tumor cells (CTC) during minimal residual disease (Fleischhacker and Schmidt 2007; Schwarzenbach et al. 2011). It can be applied for various indications during the course of cancer disease:
-
(1)
characterization of genetic and epigenetic changes for individual therapy stratification
-
(2)
follow-up on molecular changes during therapy for monitoring the effectiveness of therapy
-
(3)
detection and characterization of molecular resistance under therapy
-
(4)
highly sensitive detection of minimum residual disease or preclinical progress.
Time- and space-dependent plasticity and complexity of tumor biology cause the necessity of genetic pattern recognition and characterization of molecular changes over time for optimal individual therapy adaptation.
Liquid Profiling – A Traditional Concept with New Implications
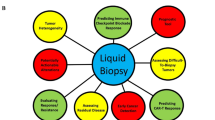
In the context of cfDNA and CTC analysis, the term “liquid biopsy ” is frequently used for the identification of tumor characteristics (Lianidou 2010; Diaz and Bardelli 2014). However, “biopsy” is a well-established term in tissue-based diagnostics that provides important information on complex relationships of a tumor and its environment. This includes tumor classification criteria such as tumor necrosis , signs of hypoxia, tumor vascularization, phenotypic features of tumor cell heterogeneity, stroma reaction of the normal tissue and infiltration of the tumor by immune cells.
In contrast, the so-called “liquid biopsy ” allows only insights in the molecular characteristics of the tumor itself by use of molecular changes of cfDNA in the blood . Similarly, tumor characteristics have been detected and monitored in the blood or bodily fluids for years by different approaches of laboratory medicine – first at the protein level as tumor markers and cellular phenotyping of leukemia cells and increasingly at the molecular level. This shows that the differentiation between tumor and normal tissue or the identification of a prognostically relevant profile of a tumor disease can be done at all levels of available biomarkers . As tumor characteristics are most efficiently assessed by multiparametric patterns, the term “liquid profiling” would express most adequately this complex diagnostic approach. Further it explains that the examination is performed in blood or bodily fluids and not in tumor tissue (Neumaier and Holdenrieder 2015) While “liquid profiling” has already widely been used in various blood -related diagnostic disciplines it now experiences a revival with respect to cfDNA and CTCs.
Companion Diagnostics for Therapy Stratification in Cancer Diseases
The molecular diagnostic characterization of cancer diseases has assumed great importance because new biological therapies target components of growth signaling pathways that are deregulated in tumor cells, e.g. due to specific mutations. Extracellularly acting antibodies or intracellularly docking small molecules block permanently expressed components and thus inhibit tumor growth. As these therapies are only effective if specific molecular changes are present, so-called driver mutations must be detected in the tumor tissue prior to therapy onset (Crowley et al. 2013; Duffy and Crown 2013). This defines which patients will most probably benefit from these targeted treatments.
Examples of the use of companion diagnostics are the detection of activating mutations (L858R or exon-19 deletion) of the epithelial growth factor receptor (EGFR) as a precondition for treatment with the EGFR tyrosine kinase inhibitors gefitinib, erlotinib and afatinib in non-small cell lung cancer (NSCLC ) , the detection of the activating BRAF mutation V600E for the treatment with the BRAF inhibitors vemurafenib and dabrafenib in malignant melanoma and the absence of downstream mutations KRAS and NRAS as preconditions for treatment with EGFR antibodies cetuximab and panitumumab in colorectal carcinoma (Crowley et al. 2013; Duffy and Crown 2013; Bokemeyer et al. 2015).
While the use of companion diagnostics has increased the response rates in the qualified patient groups, further improvements are necessary: In NSCLC , only 70 % of first line patients and 50 % of second line patients respond to treatment with tyrosine kinase inhibitors (TKI) (Ciardiello and Tortora 2008; Petrelli et al. 2012). Also, numerous relapses and secondary progressions have been reported which, in part, result from additional resistance mutations such as the EGFR T790M mutation or the ALK-EML fusion gene – which can also be treated with crizotinib and cerotinib (Ciardiello and Tortora 2008; Crowley et al. 2013).
One reason for non-response, despite the presence of qualifying mutations, is the frequently observed molecular heterogeneity within a tumor, between primary tumor and metastases and the temporal and spatial plasticity of the tumors (Gerlinger et al. 2012).
All molecular markers from different tumor manifestations can be found in blood . Additionally, molecular changes can be followed over time with less-invasive serial blood -based diagnosis and used for monitoring therapy, early relapse diagnosis and molecular characterization of resistance (Diaz and Bardelli 2014). Lastly, liquid profiling can be performed even if the biopsy of suitable tissue material is not possible and to avoid potential biopsy-associated complications (Overman et al. 2013) Fig. 11.1.
Tissue nucleic acid diagnostics are relevant for molecular characterization of tumor disease at time of diagnosis of a primary or an advanced tumor. Identification of druggable molecular defects are preconditions for the application of individually tailored therapies. Plasma nucleic acid diagnostics support the stratification of tumor patients for specific therapies when a tissue biopsy is not available. Further serial, minimal-invasive molecular assessments are valuable for the early and sensitive recurrence detection , for the identification of new molecular changes (e.g. resistance genes) and for monitoring the response to therapies. While tissue diagnostics allow a snap shot on the molecular tumor status at a given time point, liquid profiling of circulating nucleic acids overcomes the limitations of tumor heterogeneity and plasticity and mirrors the dynamics of individual tumor biology
High-Throughput Technologies in Molecular Diagnosis
Only with the development of highly parallel amplifying technologies did the ultrasensitive detection of tumor-specific nucleic acids become possible so enabling, today, a resolution of one out of 10,000 DNA molecules (Diaz and Bardelli 2014). With the commonly applied digital or clonal methods of amplification, single DNA molecules can be highly specifically amplified via emulsion PCR or cluster formation to enable selection via FACS, mass spectrometric analysis or highly parallel sequencing (Diehl et al. 2006; Chen et al. 2013; Forshew et al. 2012; Taly et al. 2013). Several current clinical studies are based on the so-called BEAMing method (Beads, Emulsion, Amplification and Magnetics), which combines digital droplet emulsion PCR with flow cytometry detection (Diehl et al. 2006, 2008). Classic next generation sequencing (NGS) approaches (e.g. Illumina, Ion Torrent), whereby single or multiple gene segments are directly sequenced, also play an important role. Here, the depth of analysis, i.e. the coverage of single gene segments, is the relevant factor for the reliable detection of single DNA molecules. Due to the, at times, small amount of DNA in blood and the small proportion of tumor DNA (sometimes less than 0.1 %) a sufficiently large initial volume of several milliliters of plasma must be collected in order to detect a tumor DNA molecule with a high degree of statistical probability. Nevertheless, a comprehensive study with 640 patients suffering from a variety of tumor diseases has shown that tumor-specific mutations of cfDNA are found in 82 % of patients with advanced tumors (excluding brain tumors) and in 55 % of patients with localized tumor stages. Of note, cfDNA was detected in plasma from the majority of tumor patients eligible for companion diagnosis (Bettegowda et al. 2014). When the frequency of KRAS mutations were compared in circulating tumor cells (CTC), cfDNA and tissues of 82 lung cancer patients, a significantly lower diagnostic sensitivity of only 52 % (at 88 % specificity) was found for CTCs vs. 96 % (at 95 % specificity) for cfDNA (Freidin et al. 2015). Bettegowda et al. also reported a significantly lower prevalence of tumor-specific rearrangements in CTCs compared to cfDNA (Bettegowda et al. 2014).
Clinical Studies on Liquid Profiling in Cancer Diseases
Liquid profiling can be effectively used in the stratification of therapy when a biopsy is not possible or when tissue samples cannot provide conclusive evidence. However, a high concordance of results from cfDNA and tumor tissue is postulated as a precondition for the available technologies. For the BEAMing method, such high concordance was found in several studies. Higgins et al. found, in 34 retrospective and 51 prospective cfDNA samples, a 100 % concordance with FFPE tissue samples when using BEAMing in both materials (Higgins et al. 2012). Bettegowda et al., comparing KRAS mutations in cfDNA and tumor tissue of 206 patients with metastasized colorectal cancer , found that sensitivity was 87 % with a specificity of 99 % (Bettegowda et al. 2014). Janku et al. examined 21 mutations in the BRAF, EGFR, KRAS and PIK3CA genes in patients with advanced cancer via BEAMing in comparison to standard tissue diagnosis. The obtained concordance rates were 91 % for BRAF, 99 % for EGFR, 83 % for KRAS and 91 % for PIK3CA mutations. Also, high cfDNA mutation rates were associated with poor prognosis (Janku et al. 2015). These studies show a high concordance of tumor-specific mutations in plasma cfDNA and tumor tissue. When investigating the KRAS status in the tissue and plasma of pancreatic cancer patients, we recently observed that discrepancies were also meaningful as the cfDNA was associated with a more accurate prediction of therapy response and prognosis (Holdenrieder et al. 2015). Further studies will address this phenomenon in different clinical settings.
During Tumor Therapy
the volume of circulating mutant DNA correlates with the tumor mass, as shown by Diehl et al. for APC, TP53 and KRAS mutations in patients with colorectal cancer (Diehl et al. 2008). After complete surgical tumor removal, the values dropped with a half-life period of about 2 h to less than 1 % of the initial value after 24 h, whereas in the case of an existing residual tumor, they remained high. cfDNA showed a stronger dynamic and had a higher predictive value for the detection of a tumor relapse than the established tumor marker CEA (Diehl et al. 2008). Similarly convincing results were found for PIK3CA and TP53, which were detected in cfDNA of 97 % (29 of 30) of female patients with metastasizing breast cancer, while sensitivities for CTCs and CA 15–3 were found to be only 87 % and 78 %, respectively. Also, correlation with tumor load and accurate detection of a relapse was significantly better for ctDNA (89 %) than for CTC (37 %) or CA 15–3 (50 %). In 53 % of female patients at advanced stage, ctDNA was the first marker to indicate an insufficient therapy effect (Dawson et al. 2013) with a mean lead-time of 5 months to the imaging findings. Several further studies were published on the monitoring of EGFR mutations in NSCLC patients. Here, too, a correlation between relative ctDNA changes and therapy response was found (Bai et al. 2012; Nakamura et al. 2011). These studies showed that, with known mutation status, cfDNA markers are highly suitable as “individual tumor markers” for disease monitoring during and after therapy.
The sensitive detection of detectable secondary resistance mutations has been described by Misale et al. (2012). In six of 10 patients with colorectal cancer and resistance to cetuximab and panitumumab, new KRAS mutations were detected up to 4 months prior to a CEA increase and 9 months before radiological relapse diagnosis. While the tumor cells showed a resistance to EGFR inhibitors, they remained sensitive to a combination of EGFR and MEK inhibitors, which enabled an early and individual therapy adjustment (Misale et al. 2012). Diaz et al. also reported on new KRAS mutations in nine of 24 patients treated with panitumumab, in whom originally a KRAS wild type was found and who subsequently developed therapy resistance 5–6 months after therapy onset. Based on a mathematical model, the authors were able to show that the expanding sub-clones had already been present before therapy onset (Diaz et al. 2012). Bettegowda et al. found new mutations of KRAS, NRAS and other genes of the MAP kinase signalling pathway in 23 of 24 (96 %) patients with EGFR-resistant colorectal cancer (Bettegowda et al. 2014). These findings correlate with data from tumor tissue, where up to 27 % of the non-mutated KRAS genes in exon 2 exhibited genetic variants in other segments of the gene or in NRAS (Schwartzberg et al. 2014; Heinemann et al. 2014). When Murtaza et al. examined genomic changes in six tumor patients using massively parallel exome sequencing , they could identify new resistance-causing and activating mutations, such as EGFR T790M, PIK3CA and RB1 (Murtaza et al. 2013).
Characterization of KRAS and EGFR resistance genes in plasma of 62 patients with metastasizing colorectal cancer with acquired anti-EGFR resistance revealed five new EGFR mutations and 27 new KRAS mutations especially in codons 61 and 146. In the respective (classified as KRAS wild type) pre-therapeutic tissue samples, these mutations were already present in low allele frequency in 35 % of the patients, correlating with poor prognosis (Morelli et al. 2015). Siravegna et al. described several acquired resistance mutations (such as KRAS, NRAS, MET, ERBB2, FLT3, EGFR and MAP2K1) in cfDNA during EGFR-inhibiting therapy. When, upon treatment, disruption of the mutated KRAS levels decreased, anti-EGFR therapy could be renewed (Siravegna et al. 2015). In a most recently published study, Garcia-Murillas et al. demonstrated in 55 female patients with localized breast cancer after successful neo-adjuvant chemotherapy and curative resection, that one-off as well as serial ctDNA determination can predict occurrence of relapse – with a median time of 7.9 months before the clinically detected manifestation. Using targeted sequencing , the authors identified several new mutations in plasma ctDNA at the time of minimum residual disease with a stronger correlation with the genetic status of the detected relapse than with the genetic changes in the primary tumor (Garcia-Murillas et al. 2015). These studies show that new resistance gene cfDNA can be detected and characterized with high sensitivity. However, future clinical application of this knowledge will require the development of respective targeted therapies.
Summary
The new technical possibilities of molecular diagnostics allow sensitive and specific characterization of targeted information on circulating nucleic acids in peripheral blood that is relevant for the detection and profiling of various diseases, especially malignant diseases. Apart from pure diagnosis, this approach enables the stratification of patients for individually tailored therapies, treatment monitoring and sensitive detection of minimal residual disease. As recent developments show, blood -based CNAPS diagnostics will quickly become a highly useful complement to well-established molecular tissue diagnostics as it is less invasive and overcomes limitations like tumor heterogeneity and plasticity. Interdisciplinary dialogue and interaction between laboratory medicine, pathology and human genetics will be paramount to establish CNAPS diagnostics as a most valuable tool for precision medicine in which the whole is more than the sum of its items.
References
Bai H, Wang Z, Chen K et al (2012) Influence of chemotherapy on EGFR mutation status among patients with non-small-cell lung cancer. J Clin Oncol 30:3077–3083
Bettegowda C, Sausen M, Leary RJ et al (2014) Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med 6:224ra24
Bokemeyer C, Köhne CH, Ciardiello F et al (2015) FOLFOX4 plus cetuximab treatment and RAS mutations in colorectal cancer. Eur J Cancer 51:1243–1252
Chen WW, Balaj L, Liau LM et al (2013) BEAMing and droplet digital PCR analysis of mutant IDH1 mRNA in glioma patient serum and cerebrospinal fluid extracellular vesicles. Mol Ther Nucleic Acids 2:e109
Chiu RW, Akolekar R, Zheng YW et al (2011) Non-invasive prenatal assessment of trisomy 21 by multiplexed maternal plasma DNA sequencing: large scale validity study. BMJ 342:c7401
Ciardiello F, Tortora G (2008) EGFR antagonists in cancer treatment. N Engl J Med 358:1160–1174
Crowley E, Di Nicolantonio F, Loupakis F et al (2013) Liquid biopsy: monitoring cancer-genetics in the blood. Nat Rev Clin Oncol 10:472–484
Dawson SJ, Tsui DW, Murtaza M et al (2013) Analysis of circulating tumor DNA to monitor metastatic breast cancer. N Engl J Med 368:1199–1209
Diaz LA Jr, Bardelli A (2014) Liquid biopsies: genotyping circulating tumor DNA. J Clin Oncol 32:579–586
Diaz LA Jr, Williams RT, Wu J et al (2012) The molecular evolution of acquired resistance to targeted EGFR blockade in colorectal cancers. Nature 486:537–540
Diehl F, Li M, He Y, Kinzler KW et al (2006) BEAMing: single-molecule PCR on microparticles in water-in-oil emulsions. Nat Methods 3:551–559
Diehl F, Schmidt K, Choti MA et al (2008) Circulating mutant DNA to assess tumor dynamics. Nat Med 14:985–990
Duffy MJ, Crown J (2013) Companion biomarkers: paving the pathway to personalized treatment for cancer. Clin Chem 59:1447–5146
Fleischhacker M, Schmidt B (2007) Circulating nucleic acids (CNAs) and cancer – a survey. Biochim Biophys Acta 1775:181–232
Forshew T, Murtaza M, Parkinson C et al (2012) Noninvasive identification and monitoring of cancer mutations by targeted deep sequencing of plasma DNA. Sci Transl Med 4:136ra68
Freidin MB, Freydina DV, Leung M et al (2015) Circulating tumor DNA outperforms circulating tumor cells for KRAS mutation detection in thoracic malignancies. Clin Chem 13. pii: clinchem.2015.242453
Garcia-Murillas I, Schiavon G, Weigelt B et al (2015) Mutation tracking in circulating tumor DNA predicts relapse in early breast cancer. Sci Transl Med 7:302ra133
Gerlinger M, Rowan AJ, Horswell S et al (2012) Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med 366:883–892
Gezer U, Holdenrieder S (2014) Posttranslational histone modifications in circulating nucleosomes in patients with colorectal cancer. In Vivo 28:287–292
Heinemann V, von Weikersthal LF, Decker T et al (2014) FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol 15:1065–1075
Higgins MJ, Jelovac D, Barnathan E et al (2012) Detection of tumor PIK3CA status in metastatic breast cancer using peripheral blood. Clin Cancer Res 18:3462–3469
Holdenrieder S (2014) Circulating nucleic acids in therapy monitoring. In: Gahan PB (ed) Circulating nucleic acids in early diagnosis, prognosis and treatment monitoring, vol 5, Advances in predictive, preventive and personalised medicine. Springer, Dordrecht, pp 309–348
Holdenrieder S, Stieber P (2009) Clinical use of circulating nucleosomes. Crit Rev Clin Lab Sci 46:1–24
Holdenrieder S, Prinz I, Ormanns S, Baechmann S, Haas M, Ross C, Angenendt P, Heinemann V, Diehl F, Boeck S (2015) Liquid profiling of KRAS-status on circulating plasma-DNA in patients with pancreatic cancer – a novel tool for therapy response prediction and prognosis. Presentation at CNAPS IX, 10.-12.09.2015 at Berlin, Germany
Janku F, Angenendt P, Tsimberidou AM et al (2015) Actionable mutations in plasma cell-free DNA in patients with advanced cancers referred for experimental targeted therapies. Oncotarget 6:12809–12821
Lianidou ES (2014) Molecular characterization of circulating tumor cells: holy grail for personalized cancer treatment? Clin Chem 60:1249–1251
Lianidou ES, Mavroudis D, Sotiropoulo G, Agelaki S, Pantel K (2010) What’s new on circulating tumor cells? A meeting report. Breast Cancer Res 12:307–314
Misale S, Yaeger R, Hobor S et al (2012) Emergence of KRAS mutations and acquired resistance to anti-EGFR therapy in colorectal cancer. Nature 486:532–536
Morelli MP, Overman MJ, Dasari A et al (2015) Characterizing the patterns of clonal selection in circulating tumor DNA from patients with colorectal cancer refractory to anti-EGFR treatment. Ann Oncol 26:731–736
Murtaza M, Dawson SJ, Tsui DW et al (2013) Non-invasive analysis of acquired resistance to cancer therapy by sequencing of plasma DNA. Nature 497:108–112
Nakamura T, Sueoka-Aragane N, Iwanaga K et al (2011) A noninvasive system for monitoring resistance to epidermal growth factor receptor tyrosine kinase inhibitors with plasma DNA. J Thorac Oncol 6:1639–1648
Neumaier M, Holdenrieder S (2015) Molecular laboratory medicine diagnostics in peripheral blood and bodily fluids Klin. Chem Mitt 46(3):139–148
Overman MJ, Modak J, Kopetz S et al (2013) Use of research biopsies in clinical trials: are risks and benefits adequately discussed? J Clin Oncol 31:17–22
Petrelli F, Borgonovo K, Cabiddu M et al (2012) Efficacy of EGFR tyrosine kinase inhibitors in patients with EGFR-mutated non-small-cell lung cancer: a meta-analysis of 13 randomized trials. Clin Lung Cancer 13:107–114
Schwartzberg LS, Rivera F, Karthaus M et al (2014) PEAK: a randomized, multicenter phase II study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) or bevacizumab plus mFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal cancer. J Clin Oncol 32:2240–2247
Schwarzenbach H (2015) The clinical relevance of circulating, exosomal miRNAs as biomarkers for cancer. Expert Rev Mol Diagn 15:1159–1169
Schwarzenbach H, Hoon DS, Pantel K (2011) Cell-free nucleic acids as biomarkers in cancer patients. Nat Rev Cancer 11:426–437
Siravegna G, Mussolin B, Buscarino M et al (2015) Clonal evolution and resistance to EGFR blockade in the blood of colorectal cancer patients. Nat Med 21:795–801
Speicher MR, Pantel K (2014) Tumor signatures in the blood. Nat Biotechnol 32:441–443
Taly V, Pekin D, Benhaim L et al (2013) Multiplex picodroplet digital PCR to detect KRas mutations in circulating DNA from the plasma of colorectal cancer patients. Clin Chem 59:1722–1731
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this paper
Cite this paper
Holdenrieder, S. (2016). Liquid Profiling of Circulating Nucleic Acids as a Novel Tool for the Management of Cancer Patients. In: Gahan, P., Fleischhacker, M., Schmidt, B. (eds) Circulating Nucleic Acids in Serum and Plasma – CNAPS IX. Advances in Experimental Medicine and Biology, vol 924. Springer, Cham. https://doi.org/10.1007/978-3-319-42044-8_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-42044-8_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42042-4
Online ISBN: 978-3-319-42044-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)