Abstract
Boswellic acids, which are pentacyclic triterpenes belong to the active pharmacological compounds of the oleogum resin of different Boswellia species. In the resin, more than 12 different boswellic acids have been identified but only KBA and AKBA received significant pharmacological interest. Biological Activity: In an extract of the resin of Boswellia species multiple factors are responsible for the final outcome of a therapeutic effect, be it synergistic or antagonistic. Moreover, the anti-inflammatory actions of BAs are caused by different mechanisms of action. They include inhibition of leukotriene synthesis and to a less extend prostaglandin synthesis. Furthermore inhibition of the complement system at the level of conversion of C3 into C3a and C3b. A major target of BAs is the immune system. Here, BEs as well as BAs including KBA and AKBA, have been shown to decrease production of proinflammatory cytokines including IL-1, IL-2, IL-6, IFN-γ and TNF-α which finally are directed to destroy tissues such as cartilage, insulin producing cells, bronchial, intestinal and other tissues. NFĸB is considered to be the target of AKBA. The complex actions of BEs and BAs in inflamed areas may be completed by some effects that are localized behind the inflammatory process as such tissue destruction. In this case, in vitro- and animal studies have shown that BAs and BEs suppress proteolytic activity of cathepsin G, human leucocyte elastase, formation of oxygen radicals and lysosomal enzymes. Pharmacokinetics: Whereas KBA is absorbed reaching blood levels being close to in vitro IC50, AKBA which is more active in in vitro studies than KBA, but undergoes much less absorption than KBA. However, absorption of both is increased more than twice when taken together with a high-fat meal.Clinical Studies There are a variety of chronic inflammatory diseases which respond to treatment with extracts from the resin of Boswellia species. Though, the number of cases is small in related clinical studies, their results are convincing and supported by the preclinical data. These studies include rheumatoid arthritis, osteoarthritis, chronic colitis, ulcerative colitis, collagenous colitis, Crohn’s disease and bronchial asthma. It can not be expected that there is cure from these diseases but at least improvement of symptoms in about 60–70 % of the cases. Side Effects The number and severity of side effects is extremely low. The most reported complaints are gastrointestinal symptoms. Allergic reactions are rare. And most authors report, that treatment with BEs is well tolerated and the registered side effects in BE- and placebo groups are similar.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Boswellic acids
- Boswellic extracts
- Leukotrienes
- Prostaglandins
- Proteolytic enzymes
- Cytokines
- Pharmacokinetics
- Rheumatoid arthritis
- Inflammatory bowel diseases
- Bronchial asthma
- Diabetes
- Side effects
13.1 Introductory Remarks
Boswellic acids (BAs) belong to the active pharmacological principles of the oleo gum resin from the trees of different Boswellia species. These trees are plants typically found in the deserts, where the aborigines since thousands of years, scratch the bark and collect fluid, during dry periods. Burning the resin, the fumes are used for disinfection, improvement of the scent of the air, as well as for ceremonial and medical purposes. The resins are known as salai guggal (India), frankincense (pure incense), incense and olibanum.
This chapter summarizes the present knowledge about medical history, pharmacological active ingredients and therapeutical uses of the resin with special impact on the anti-inflammatory mechanisms of boswellic acids.
13.2 Medical History
The oldest written document, which mentions frankincense as a drug is the Papyrus Ebers. In 1873, Moritz Fritz Ebers, professor of Egyptology, received a more than 20 m long papyrus from an Arab businessman [40] describing the medical use of frankinsence in Egypt. In India, the therapeutic applications of the oleogum resin of Boswellia serrata, called Salai guggal (SG), are already described in early Ayurvedic textbooks (Charaka Samhita, 1st–2nd century AD and in Astangahrdaya Samhita, seventh century AD).
Remedies containing preparations from frankincense (here Boswellia carterii) were also prescribed by the famous physicians Hippocrates, Celsus, Galenus, Dioskurides and others for the treatment of tumours, carcinomas, edemas, inflammatory diseases including diarrhoea, and diseases of the respiratory tract [40].
Olibanum, the resin of various Boswellia species (Table 13.1), was also known as a remedy in Europe from ancient times till the beginning of the twentieth century. Then it disappeared from the list of doctoral prescriptions since scientific evidence for therapeutical efficacy was missing. Only when Singh and Atal [69] and Ammon et al. [3] showed that an extract from resin of Boswellia serrata inhibited inflammation in an animal model resp. formations of leukotrienes in an in vitro model, the scientific community became interested and the first human pilot studies were initiated. By now, preparations of the resin are widely used to treat a variety of chronic inflammatory disorders.
13.3 Composition of the Resin
The resin of Boswelli species consists of mucus, volatile oil and resin acids (Table 13.2). However, the quantitative composition of these constituents varies from species to species.
The resin acids contain pentacyclic and tetracyclic triterpenes. Among the pentacyclic triterpenes, only some boswellic acids are responsible for many of the pharmacological effects; but also tirucallic acids (TAs), from the tetracyclic triterpenic acids, have been shown to be biologically active .
Pentacyclic Triterpenes:
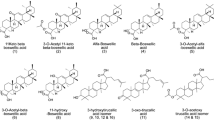
Büchele et al. [9] identified 12 different pentacyclic triterpenes in the samples of Boswellia extracts (BEs) (Table 13.3). From these 12, the chemical structures of the two most active boswellic acids (BAs) are shown in Fig. 13.2.
The authors reported significant quantitative differences of pentacyclic triterpenes between various species: A striking difference was observed in the content of the boswellic acids, i.e. KBA and AKBA (Table 13.3). Recently Beisner et al. [5] identified a new pentacyclic triterpene from Boswellia serrata, it was just one, 3α-acetyl-20(29)-lupene-24-oic acid and Verhoff et al. [80] observed biological activity of a novel C(28)-hydroxylated lupeolic acid. Though BAs received most attention through the group of pentacyclic triterpenes, some other, including lupeol, exhibit pharmacological activity as well, which are also considered boswellic acids [49].
Tetracyclic Triterpenes:
Among the tetracyclic triterpenes, three TAs have been identified: 3-oxotirucallic acid, 3-hydroxytirucallic acid and 3-acetoxytirucallic acid. Other resin compounds with pharmacological activities are: betulinic acid, epi-lupeol, lupenoic acid, 1-ursene-2-diketone-incensole acetate, isoincensole and isoincensole acetate and as well as terpenes that can be found in the volatile oil.
13.4 Preclinical Studies
13.4.1 Anti-inflammatory Actions
The first scientific publication with the title “Analgesic effect of the oleogum resin of Boswellia serrata Roxb”. by Karr and Mennon appeared 1969 [31]. Singh and Atal [69] published a paper entitled: “Pharmacology of an extract of salai guggal ex-Boswellia serrata, a new non steroidal anti-inflammatory agent”. In this study, Singh and Atal [69] observed that the oral administration of an alcoholic extract of the oleogum resin of Boswellia serrata caused inhibition of the carrageenan- and dextran-induced edema in the paws of rats and mice, suggesting anti-phlogistic action of a BE. Since such an effect could also be observed in adrenalectomized rats, the authors concluded that the anti-inflammatory effect of the BE was not due to the liberation of glucocorticoids. Significant anti-arthritic activity of an acetone extract from Boswellia carterii in lewis rats was reported by Fan et al. [19]. Moreover, anti-inflammatory, anti-noceptive and antioxidant activities have been described using extracts from other Boswellia species; in this case, Boswellia longata [44]. Boswellia extracts were also effective in the treatment of skin inflammations [71].
A reduction of the carrageenan-induced edema in the paws of mice after oral or intraperitoneal application of 1 mg/kg β-BA was recently reported by Siemoneit et al. [68].
Introducing a new model, i.e. papaya latex also causing rat paw inflammation, Gupta et al. [21] tested a variety of anti-rheumatic agents and BAs and compared their effects with the actions of carrageenan in relation to rat paw inflammation. It turned out that in the carrageenan model the inhibitory effects of indomethacin, piroxicam, ibuprofen and acetylsalicylic acid were more pronounced than those of BAs, whereas BAs were much more effective in the papaya latex model. The action of prednisolone was almost similar in both models. This suggests that the anti-inflammatory mechanism of BAs is different from the so-called “aspirin-like” drugs and prednisolone (Fig. 13.3).
13.4.1.1 The Arachidonic Acid Cascade: Cyclooxygenase and Cyclooxygenase Products
Activation of the arachidonic acid cascade by the membrane bound enzyme phospholipase A2 (PLA2) is the initial step to start production of mediators of inflammation. In this cascade (Fig. 13.3) cyclooxygenases and 5-lipoxigenase produce prostaglandines and leukotrienes, which eventually lead to the typical inflammatory symptoms. The mechanism of anti-inflammatory action of BEs and BAs on members of the arachidonic acid cascade has been studied by several scientists.
Inhibition of 6-keto-PGF1α formation in human platelets by an alcoholic extract of salai guggal (SG). 100 % = 277 pg 6-keto-PGF1α/107 cells. Number of experiments are given in parentheses [3]
Boswellic Extracts:
Based on the observations of Singh and Atal [69], Ammon et al. [3] studied whether or not an alcoholic extract of the BS resin, could affect prostaglandin synthesis in vitro. For this study, human platelets which contain cyclooxygenase-1 (COX-1) were used. After in vitro stimulation with the Ca ionophore A 23187, the extract inhibited 6-keto-PKF-1α synthesis, a product of COX-1, up to 50 % at a concentration of 100 µg/ml (Fig. 13.4).
In another in vitro model extracts from Boswellia frereana suppressed cytokine IL-1A-induced prostaglandin E2 synthesis and COX-2. In this case, epi-lupeol was identified as a principal constituent [6].
Boswellic Acids:
As discussed above, the resins contain a variety of compounds which could be responsible for their anti-inflammatory actions. These boswellic acids are listed in Fig. 13.2.
Among these in a variety of studies most evidence has been gained from acetyl-11-keto-β-boswellic acid (AKBA) and 11-keto-β-boswellic acid (KBA). Thus, it was near at hand to study their effect on the production of the arachidonic acid cascade intermediates. In the assay that used human platelets, AKBA produced 50 % inhibition of 12-hydroxyheptadecatrienoic acid (12-HHT) at a concentration of 10 μM. Acetyl-boswellic acid (ABA) on the contrary showed no such effect. Inhibition of COX products by AKBA was also observed by Siemoneit et al. [66, 68], using the human platelets model. BAs, preferably AKBA, inhibited COX-1 product formation with an IC50 ~ 6 μM. The authors also reported that COX-1 is more sensitive to inhibition by AKBA than COX-2. In this sense, Siemoneit et al. [68] described the inhibition of prostaglandin E 2 synthase-1 as the molecular basis for the anti-inflammatory actions of boswellic acids. This means that BAs, in particular AKBA, directly interfere with COX-1 and may mediate their anti-inflammatory actions not only by suppression of lipoxygenases, as discussed later, but also by inhibiting cyclooxygenases, preferentially COX-1 [66]. On the other hand, β-boswellic acid (β-BA) and AKBA stimulated arachidonic acid release and 12-lipoxigenase activity in human platelets, where AKBA was less potent than β-BA [47].
Cao et al. [12] observed, that, in addition to AKBA, β-BA, acetyl-α-BA, acetyl-β-BA and betulinic acid are also inhibitors of COX-1. The IC50 was estimated to be 10 μM.
Other compounds: Verhoff et al. [80] reported that a novel, yet unknown C(28)-hydroxylated lupenoic acid (LA), that is 3α-acetoxy-28-hydroxylup-20(29)-en-4β-oic acid (Ac-OH-LA) inhibits the biosynthesis of COX-, 5-LO- and 12-Lipoxigenase (12-LO)-derived eicosanoids from endogenous arachidonic acid (AA) in activated platelets, neutrophils and monocytes from human blood with consistent IC50 values of 2.3–6.9 µM. Thus, the data discussed suggests that cyclooxygenases are targets of a variety of compounds in the resins of Boswellia species.
13.4.1.2 The Arachidonic Acid Cascade: 5-Lipoxigenase and 5-Lipoxigenase Products
Until 1991, there was no drug known which could predominantly inhibit the synthesis of leukotrienes despite the need for such compounds to treat diseases where leukotrienes have a major impact. It was the publication of Ammon et al. [3] that showed that BEs not only affected formation of COX products, but to a much larger extend also inhibited LTB4 synthesis. This publication and a later paper [50], indicating that certain BAs are responsible for this effect, received large attention by the scientific community.
Boswellic Extracts:
After the stimulation of leukotriene synthesis with the calcium ionophore A 231876 in polymorphmononuclear neutrophils (PMN)—which contained 5-LO but no COX the same extract that was used for the studies on prostaglandin synthesis [3] in a concentration-dependent manner inhibited synthesis of leukotriene B4 (LTB4) and 5-hydroxyeicosatetraenoic acid (5-HETE) (a metabolite of the 5-LO cascade) formation at concentrations between 10 and 80 μg/ml (Fig. 13.5). In this case, 50 % inhibition occurred at a concentration of 30 μg/ml, indicating that the inhibitory action of the extract was significantly more pronounced than its effect on COX-1 [3].
Concentration-dependent inhibition of LTB4-formation by salai guggal (SG) ethanolic extract in stimulated rat peritoneal PMNL (a), and the decrease in the inhibition of the sum of 5-LOx products (b) [3]. x-axis represents a and b
Boswellic Acids:
Concerning the actions of BAs, Safayhi et al. reported in 1992 BAs to be specific, non-redox inhibitors of 5-LO. In this study, isomers of (α- and β-) of BAs and their acetyl derivatives were isolated from the oleogum resin of BS. It was observed that BAs partly decreased the formation of LTB4 in calcium-ionophore-stimulated PMN in a concentration-dependent manner. AKBA was most effective with an IC50 value of 1.5 µM.
Structure–Action Relationships:
This observation posed the question whether or not certain chemical motif in the molecular structure of BAs are required for the inhibition of leukotriene production. In this sense, Sailer et al. [53] studied the effect of a variety of derivatives of BAs on leukotriene synthesis in Ca ionophore-stimulated PMN. From the IC50 values, it was obvious that not all tested compounds inhibited synthesis of leukotrienes and that some of them exhibited only a partial effect. Taking into account the different chemical structures of the tested BAs, the data revealed that a hydrophilic function at C-4 position in combination with an 11-keto group appears to be essential for the inhibition of leukotriene synthesis by BAs (Table 13.4).
5-LO as target: In intact PMN, signal transduction cascade of events that starts with the external stimulation of leukocytes, where the participation of calcium ions is necessary, results in the production of leukotrienes by intracellular 5-LO. In order to study whether or not BAs might directly interfere with 5-LO, in a cell-free system from PMN, where this cascade is interrupted, the effect of various derivatives of BAs on 5-LO activity was tested after addition of exogenous arachidonic acid. It was found that the effects of different BAs were qualitatively similar to those in intact PMN. However, the IC50 was higher than in intact cells which may be due to the different environment of 5-LO in a cell-free system. [54].
Mechanism of 5-LO Inhibition:
Further studies addressing the mechanism of direct 5-LO inhibition used the supernatant of PMN. In this study, pentacyclic triterpenes lacking the 11-keto function and/or carboxyl function on ring A (e.g. amyrin and ursolic acid) did not or only partially inhibit 5-LO (Table 13.4). These compounds even caused a concentration-dependent reversal of 5-LO inhibition by AKBA, whereas the inhibitory actions of 5-LO inhibitors from different chemical classes were not modified. Thus, it was concluded that AKBA acts directly on the 5-LO enzyme at a site selective for pentacyclic triterpenes which is different from the arachidonate substrate binding site [51]. Using photoaffinity labelling, it was studied whether or not 4-azido-5-125 iodo-salicyl-β-alanyl-11-keto-β-boswellic acid, a photoaffinity analogue inhibiting 5-LO activity as efficiently as a lead compound, could be displaced from its binding site by AKBA. This was in fact the case. On the other hand, AA had no such effect. This data also suggests that AKBA in the presence of calcium binds to a site distinct from the substrate (AA) binding site of 5-LO [54].
13.4.2 Proteolytic Enzymes: Human Leucocyte Elastase (HLE)
Another factor in the inflammatory process is the release of proteolytic enzymes from PMN which are involved in the destruction of cartilage. Tausch et al. [78] observed that BAs suppressed the proteolytic activity of cathepsin G in a competitive reversible manner with an estimated IC50 value of 0.6 μM. The same effect was observed in humans after oral administration of a BE.
HLE is a serine protease produced and released by PMN. Using pure HLE, Safayhi et al. [52] screened several pentacyclic triterpenes for inhibitory actions on HLE. In this study AKBA decreased the activity of HLE with an IC50 value of roughly 15 μM. Among the pentacyclic triterpenes, tested in concentrations up to 20 μM, substantial inhibition by β-BA, amyrin and ursolic acid was observed.
13.4.3 Oxygen Radicals
Oxygen radicals which are formed in PMN through the action of leukotrienes are also involved in cartilage destruction in rheumatoid arthritis. Heil et al. [27] studied the effects of AKBA and of BEs on SOD-quenchable O2-radical formation in intact PMNs and in a cell-free system. AKBA (IC50 ~ 10 µM) and extracts (IC50 ~ 13 µg/ml) consistently inhibited phorbol-12-myristate-13-acetate (PMA)-stimulated NADPH oxidase activity in rat peritoneal PMNs and reduced n-formyl-methionyl-leucyl-phenylazanin (f-MLP) and PMA-induced oxidative burst in stimulator-sensitive human blood PMN preparations.
13.4.4 The Complement System
The complement system is part of the non-specific humoral defence. It is an important link between immuno- and inflammatory reactions.
Boswellic Acids:
As early as 1987, inhibition of the guinea pig complement system by α-BA and β-BA in concentration range between 5 and 100 μM has been reported by Wagner et al. Anticomplementary activities of a mixture of BAs were also described by Kapil and Moza [30]. They observed that BAs inhibited the in vitro immunohemolysis of antibody-coated sheep erythrocytes by pooled guinea pig serum. The reduced immunohemolysis was found to be due to an inhibition of C3 convertase of the classical complement pathway.
The threshold concentration for inhibition was 100 μg per 0.1 ml diluted buffer added to the assay. Thus, at least in vitro, BAs can suppress the conversion of C3 into C3a and C3b and therefore its proinflammatory actions of this system.
Summarizing the anti-inflammatory actions of BEs and BAs:
The resin of Boswellia species contains a variety of compounds with anti-inflammatory properties. Among these are BAs but also some other constituents have been described. Members of the arachidonic acid cascade are targets of BEs and BAs as well as proteolytic enzymes, oxygen radicals, and the complement system.
Most information is available from AKBA and KBA. Among the cyclooxygenases, COX-1 seems to be most sensible to inhibition by BAs. Of special interest is the inhibitory action of BAs on 5-LO. 5-LO produces leukotrienes, which are responsible for plasma exudation, edema production, chemotaxis and activation of white blood cells which release proteolytic enzymes and oxygen radicals. 5-LO is more sensitive to BAs than cyclooxygenases. In addition, BAs directly inhibit proteolytic enzymes and oxygen radical formation in PMN, and last but not least also the complement system, which is an important link between immune and inflammatory reaction. Thus, especially BEs—a multicomponent product as well as BAs—in contrast to the widely used NSAID drugs—exhibit their anti-inflammatory action simultaneously affecting a variety of parameters that are involved in inflammatory processes.
13.4.5 The Immunosystem
White blood cells play an important role in the defence system of the body. Granulocytes, monocytes, macrophages and lymphocytes cover the non-specific as well as the humoral and cellular defence. However, under certain conditions, they are also closely related to inflammatory autoimmune disorders. Humoral and cellular defence have also been the subject of studies with BEs and BAs.
13.4.5.1 Humoral Defence
Humoral defence is one of the important measures of the body against infectious diseases. It is related to the activation of B lymphocytes. After contact with antigens, B cells differentiate to plasma cells, which then produce antibodies belonging to the family of immunoglobulins.
13.4.5.1.1 Antibody Titres
Boswellic Acids:
Humoral antibody synthesis in mice treated with sheep erythrocytes was studied by Sharma et al. [62] by determining the hemagglutinating antibody titers in the serum. Here, primary antibody production (after a first antigen injection) and secondary antibody production (after a second injection) were tested.
It was found that a single dose of a mixture of BAs (50–200 mg/kg)—as isolated by Singh et al. [70] on the day of sensitization produced a dose related reduction (10.4–32.8 %) in primary hemagglutinating antibody titers on day 4. Significant reduction in antibody production was obtained with 100 and 200 mg/kg doses. On the other hand the secondary antibody titers were significantly enhanced at lower doses, the effect being more prominent at 50 mg/kg. Azathioprine was administered as a reference compound (200 mg/kg p.o.) following the same schedule and resulted in only 10.4 % inhibition of primary antibody synthesis and had no effect on the secondary antibody production.
Usually, the second injection of antigens causes earlier antibody production with higher affinity and is mainly due to immunoglobulin G (IgG).
Using the technique of complement fixing, a method for analysing antigen and antibody titers, oral administration of a mixture containing BAs for 5 days around the time of immunization resulted in a significant decrease in primary and secondary complement fixing antibody titers at 100 mg/kg [62]. On the contrary, when a BA mixture (25–100 mg/kg) was given orally for 5 days around immunization a marked increase (15.38–26.92 %) in antibody production on day +7 was observed. The effect was more pronounced at a dose of 25 mg/kg than at 50 or 100 mg/kg. The secondary antibody titers were only marginally increased. Azathioprine treatment (100 mg/kg) had no significant effects on primary as well as on secondary antibody titers.
In mice, in which treatment with BAs was initiated 7 days prior to immunization, BAs (25–100 mg/kg) elicited a dose related increase (37.93–63.79 %) in the primary humoral response without significantly affecting the expression of the secondary response. Levamisole (2.5 mg/kg, p.o.), an immunopotentiating agent, displayed only a 25 % increase in primary and a 6.66 % increase in secondary antibody titers.
13.4.5.1.2 Immunoglobulins
Boswellic Extract
As far as low doses of BEs are concerned, the data received with antibody titers finds their equivalent when immunoglobulins were determined in the blood of sensitized mice. Previously, it was shown by Khajuria et al. [33] that oral administration of a biopolymeric fraction (BOS 2000) from B. serrata (1–10 mg/kg) elicited a dose related increase in the delayed hypersensitivity reaction (early 24 h and delayed 48 h) in mice. It also stimulated the immunoglobulin M (IgM) and IgG titers expressed in the form of plaques (PFC) and the complement fixing antibody titre.
Gupta et al. [26] studied a possible immunological adjuvant effect of BOS 2000 on specific antibody and the cellular response to ovalbumin in mice. Mice were immunized s. c. with ovalbumin 100 µg and received BOS 2000, 80 µg on days 1 and 15. Two weeks later, BOS 2000, 80 µg corresponding to about 3.5 mg/kg bw significantly increased IgG, IgG1 and IgG2a antibody levels in the serum compared to the ovalbumin group.
At a dose of 80 µg BOS 2000, there was also a significant increase of lymphocytes CD4/CD8 and CD80/CD 86 analyzed in spleen cells and with cytokines (IL-2 and IFN-γ) profiles in the spleen cell culture supernatant. From their data, the authors conclude, that BOS 2000 seems to be a promising balanced Th1- and Th2 lymphocytes directing immunological adjuvant which can enhance the immunogenicity of vaccines.
Thus, regarding the humoral defence in the in vivo experiments, it appears that BAs have a dual effect on antibody titers: at lower doses, there is an increased formation, whereas at higher doses, BAs may even have inhibitory effects. Whether or not this data is of relevance for humans remains to be established. And the question remains: what is a high and what is a low-dose regarding humans.
13.4.5.2 Cellular Defence: Effect on Leucocytes
Cellular defence against infectious microorganisms is mediated by the actions of white blood cells. This includes proliferation, transformation, and activation of lymphocytes, as well as induction of infiltration and phagocytosis by macrophages and neutrophil granulocytes.
Their functions are organized through the crosstalking among related cells via cytokines produced and released from various leucocytes. Numerous authors have dealt with the question whether or not extracts from the Boswellia resin, its volatile oil, and/or boswellic acids would affect the activity of white blood cells and whether or not such effects could be attributed to an interaction with the system of cross talking between white blood cells by cytokines.
Boswellic Extracts and Essential Oils:
In their studies on lymphocyte transformation, Badria et al. [4] used an assay with lymphocytes isolated from venous human blood. In this study, a methylene chloride extract from the oleogum resin of Boswellia carterii in the presence of phytohemaglutinin (PHA) or concanavalin A (CON A) at 1 mg/ml stimulated lymphocyte transformation by 90 % (EC50 = 0.55 mg/ml). Several compounds from the essential oil were also biologically active. The different BAs and TAs tested, including acetyl-β-BA, acetyl-α-BA, 3-oxo-TA, AKBA, β-BA, 3-hydroxy-TA and KBA, showed a similar activity with EC50 values from 0.001 to 0.005 μM.
Mikhaeil et al. [41], who studied the chemical composition of frankincense oil, also reported that the oil exhibited strong immunostimulant activity (90 %) of lymphocyte transformation, when assessed in a lymphocyte proliferation assay. From these studies, it may be concluded, that a variety of components of an extract from Boswellia resins are effective in stimulating lymphocyte transformation and thus can contribute to cellular defence.
Boswellic Acids:
Sharma et al. [62] reported that, if spleen cells from non-immunized mice were used, a mixture of various BAs in the range of 1.95–125.0 μg/ml showed no spontaneous mitogenic activity and the cell viability was comparable to controls. However, when, the test, was performed in the presence of mitogen stimulating lipopolysaccharides (LPS, PHA, CON A and alloantigen), a concentration-dependent inhibition of lymphocyte proliferation by BAs was observed.
The effect of a mixture of BAs on phagocytosis was also studied by Sharma et al. [62]. Preincubation of peritoneal macrophages with different concentrations of BAs (1.95–125 μg/ml) resulted in an enhanced phagocytotic function of adherent macrophages with a maximal effect occurring at 62.25 μg/ml.
The studies discussed so far have been performed in vitro. They showed stimulating and inhibitory effects of BAs and BEs, respectively, employing different concentrations. At present, the data is difficult to interpret and transferred to the human situation.
In an in vivo experiment studying the anti-arthritic activity of boswellic acids employing bovine serum albumin (BSA) induced arthritis, Sharma et al. [61] observed that oral administration of a mixture of BAs (25, 50 and 100 mg/kg/day) reduced the population of leucocytes when BSA was injected into the knee, and changed the electrophoretic pattern of the synovial fluid proteins. The local injection of BAs (5, 10 and 20 mg) into the knee 15 min prior to BSA challenge also reduced infiltration of leucocytes into the knee joint and inhibited the migration properties of PMN in vitro. As discussed above some BAs are inhibitors of 5-Lo. So, the mechanism of action of BAs on leucocyte infiltration could be the inhibition of LTB4—synthesis, i.e. reducing their chemotactic action.
13.4.5.3 The Cross Talk in Cellular Defence
NFκB plays a key role for the function of cytokines in their crosstalk between immune competent cells. NFκB, which is usually present in the cytosol, is produced by neutrophil granulocytes. This compound regulates the release of cytokines from various white blood cells being responsible for proliferation, activation and function of these cells.
13.4.5.3.1 Nuclear Transcription Factor ĸB (NFκB)
As far as possible effects of BEs are concerned, AKBA, as one of their pharmacological active compounds, has turned out to be a natural inhibitor of NFκB [16]. Thus, AKBA applied in vivo in mice (100 μmol/kg) for 1 week inhibited the NFκB activation. Suppression of NFκB and NFκB-regulated gene expression by AKBA is also reported by Takada et al. [77].
When AKBA was given systemically or locally in a mouse model with psoriasis, the signalling action of NFκB and subsequent NFκB-dependent cytokine production by macrophages was significantly suppressed. This was associated with profound improvement of the psoriasis disease activity score [82]. As far as the mechanism of action on NFκB is concerned, Syrovets et al. [76] reported that acetyl-boswellic acids inhibit constitutively activated NFκB signalling by intercepting the IκB-kinase activity in an in vitro model of PC-3 prostate cancer cells. However, inhibition of NFκB is not only due to an action of BAs in extracts from Boswellia species. Previously, Moussaieff et al. [45] reported that incensole acetate, a compound isolated from Boswellia resins, also inhibits NFκB activation. This action was combined with an anti-inflammatory effect in the inflamed mouse paw model.
13.4.5.3.2 Cytokines
Crosstalk between leucocytes is organized by a group of compounds released from monocytes, macrophages and T cells, called cytokines. These include interleukines (IL), interferone-γ (IFN-γ) and tumornekrosisfactor-α (TNF-α), which regulate different functions of white blood cells. Since on the one hand cytokines are under regulation of NFĸB but on the other hand NFĸB is a target of AKBA a compound of the resin of Boswellia species it was just logical to study whether or not BEs and BAs would affect production/serum levels of various cytokines.
13.4.5.3.2.1 Interleukines/IFN-γ
Interleukins belong to the group of cytokines. There are pro- and anti-inflammatory interleukins produced by macrophages and T cells following the recognition of a pathogen.
Chervier et al. [13] studied the effect of an extract from Boswellic carterii on the production of TH-1 and TH-2 cytokines by murine splenocytes. The use of an extract with sesame oil as solvent resulted in a dose-dependent inhibition of IL-2 and IFN-γ and a dose-dependent potentiation of IL-4 and IL-10. Gayathri et al. [19] observed that a crude methanolic extract from BS and 12-ursine-2-diketone, a pure compounds of BS, inhibited TNF-α, IL-1 B and IL-6 in cultured Peripheral Blood Mononuclear Cells (PBMC). Observations on TH1/TH2 cytokines also revealed marked down regulation of IFN-γ and IL-12, whereas IL-4 and IL-10—which are anti-inflammatory interleukins—was upregulated upon treatment with a crude extract and the pure compound 1-ursene-2-diketone. This indicates that both are capable of carrying out anti-inflammatory activities at sites where chronic inflammation is present by switching off the proinflammatory cytokines.
Employing an acetone extract from Boswellia carterii Birdw. Fan et al. [18], in an adjuvant arthritis model in lewis rats 900 mg/kg for 10 consecutive days, observed significant decrease of arthritic scores. This was associated with suppression of local tissue IL-1B and TNF-α. On the other hand, in a study of Khajuria et al. [33], the authors demonstrated that oral administration of 1–10 mg/kg of a polymeric fraction from BS (BOS 2000) increased levels of IL-4, IFN-γ and TNF-α in the serum.
13.4.5.3.2.2 Tumor Necrosis Factor-alpha (TNF-α)
TNF-α is also an important cytokine which activates local restriction of infections.
TNF-α released from macrophages, natural killer (NK) cells, and T cells activates vascular endothel, increases permeability of vessels for proteins and cells and entry of IgG and complement into tissues. TNF-α induces fever. Massive liberation of TNF-α from macrophages can even cause shock.
Inhibition of TNF-α and its signalling has been recognized as a highly successful strategy for the treatment of chronic inflammatory diseases such as rheumatoid arthritis. Previously it has been shown by Syrovets et al. [76] that acetyl-α-BA and AKBA inhibited the generation of TNF-α in concentrations between 1 and 10 μM in LPS-stimulated human monocytes. AKBA was found to be the most active compound. The effect was mediated by an indirect inhibition of NFκB and subsequent downregulation of TNF-α expression in human monocytes. In these cells, Borsches and Grim (personal communication 2000) observed a concentration-dependent decrease of TNF-α and IL-1B production in a concentration range of 5–20 μM.
The data from this chapter, covering cytokines, suggest that low doses of Boswellia preparations increase production of proinflammatory cytokines, whereas high doses are even suppressive. In other words, low doses of BEs may stimulate cellular defence f.i. in case of infections and high doses may be useful in defeating the proinflammatory actions of cytokines in autoimmune inflammatory disorders.
13.4.5.3.2.3 Cytokines in Autoimmune Diabetes
Type 1 diabetes is an autoimmune disease, where a chronic inflammatory process finally causes death of insulin producing β-cells of pancreatic islets and insulin deficiency. Autoimmune diseases are—as discussed—associated with overexpression of proinflammatory cytokines. Among these, in patients with type 1 diabetes NFκB, TNF-α, IFN-γ, IL-1B and IL-2 have been found to be increased in splenocytes and PBMC [15].
Application of multiple low doses of streptozotocin (MLD-STZ) is a method to induce autoimmune diabetes in animals similar to type 1 diabetes in humans.
Shehata et al. [64] studied whether or not a BE could prevent hyperglycemia, inflammation of pancreatic islets and increase of proinflammatory cytokines in the blood in MLD-STZ treated mice. In this study, treatment with streptozotocin (STZ) (40 mg/kg i.p. for 5 days) after 10 days produced a permanent increase of blood glucose, infiltration of lymphocytes into pancreatic islets, apoptosis of periinsular cells and after 35 days shrinking of islet tissue. This was associated with an increase of proinflammatory cytokines (IL-1A, IL-1B, IL-2, IL-6, IFN-γ, TNF-α) in the blood. In STZ treated mice, simultaneous i.p. injection of 150 mg/kg of BE over a period of 10 days prevented animals from increase of blood glucose levels (Fig. 13.6). Histochemical studies showed, that BE avoided lymphocyte infiltration into pancreatic islets, apoptosis of peri-insular cells and shrinking of islet size.
Effect of boswellic extract (150 mg/kg i.p. for 10 days) on blood glucose levels of MLD-STZ-treated mice (mean ± SE; n = 4) [64]
As far as the cytokines tested are concerned, there was a significant inhibition of the increase of IL-1A, IL-1B, IL-2, IL-6, IFN-γ and TNF-α in the blood. It was concluded that extracts from the gum resin of Boswellia serrata prevent islet destruction and consequent hyperglycemia in an animal model of type 1 diabetes, probably by inhibition of the production/action of cytokines related to induction of islet inflammation in an autoimmune process (Fig. 13.7).
Effect of Boswellic extract (150 mg/kg i.p. for 10 days) on proinflammatory cytokines in the serum of MLD-STZ-treated mice. C control (mean ± SE; n = 4) [64]
When these experiments were repeated with KBA or AKBA the same results were achieved [65]. So far, however, no clinical data is available to support these animal experiments.
13.5 Antimicrobial and Antiparasitical Effects
Resins in general protect the stems of trees from any microbial attack.
Raja et al. [48] studied the antimicrobial activities of various Boswellic acids against 112 pathogenic bacterial isolates including ATCC strains. Here, AKBA exhibited the most potent antibacterial activity showing a Minimal Inhibitory Concentration (MIC) range of 2–8 μg/ml against the entire Gram-positive bacterial pathogens tested. It exhibited a concentration-dependent toxicity of Staphylococcus aureus ATCC 29213 up to 8 × MIC. The antibacterial mode of action of AKBA probably occurred via disruption of the microbial membrane structure.
In another study, methanolic and aqueous extracts from Boswellia dalziellia also showed a broad spectrum of inhibitory activity against bacteria, both Gram positive, Gram negative and fungi [2].
Serratol, a diterpene isolated from the gum resin of Boswellia serrata, was previously tested by Schmidt et al. [57] for its antiprotozoal activity. It was found to be active against Tripanosoma brucie, Rhode siense (sleeping sickness) and Plasmodium falciparum (Tropical Malaria).
Essential oils of the gum resin from different Boswellia species including Boswellia carterii (Somalia), Boswellia papyrifera (Ethiopia), Boswellia serrata (India) and Boswellia rivae (Ethiopia) were tested by Camardes et al. [11] and showed antimicrobial activity.
13.6 Clinical Studies
So far, only extracts from the gum resin of Boswellia serrata have been used for clinical trials. Studies with isolated compounds are still missing. The studies focus on chronic inflammatory diseases.
13.6.1 Pharmacokinetics of Boswellic Acids
In modern pharmacology, the therapeutic effects of drugs are closely related to their pharmacokinetic properties. However, as far as extracts from herbal medicine are concerned, it is impossible to establish pharmacokinetic data since they contain a variety of compounds which are involved in the final therapeutic actions. Moreover, their contents vary from species to species. Thus, the only possibility for a rough standardization is to determine one or more components of an extract where significant pharmacological effects can be expected. At present, in case of BEs, these are KBA and AKBA. Studies with isolated KBA and AKBA in humans do not exist yet. (Table 13.5)
13.6.1.1 Blood Levels of AKBA and KBA
In an open uncontrolled trial with 12 healthy male volunteers [63], a single oral dose of a commercial product of an extract out of gum resin from Boswellia serrata (WokVel™) containing 333 mg was given after standard breakfast. The extract contained 6.44 % KBA, 2 % AKBA, 18.51 % β-BA, 8.58 % 3-O-acetyl-β-BA, 6.93 % α-BA and 1.85 % 3-O-acetyl-αBA. In this study, only the concentration of KBA in the plasma was measured (Fig. 13.8). As shown in Table 13.6 maximum concentration of KBA was found after 4.5 h 2.72 µM. This concentration is in the range of the IC50 of KBA for the inhibition of leukotriene synthesis in vitro. In this study, the elimination half life (t1/2b) was 5.97 h. This suggests that when the above treatment is given every 6 h, the steady state plasma concentration of KBA is reached after approximately 30 h.
Mean plasma concentration of 11-keto-β-boswellic acid versus time after oral administration of 333 mg Boswellia serrata extract WokVel™ containing 6.44 % KBA [63]
As discussed in Sect. 3, Büchele and Simmet [8] identified 12 different pentacyclic triterpenic acids in an extract of Boswellia serrata. Their structures and contents are shown in Fig. 13.2 and Table 13.3. Using high-performance liquid chromatography and photodiode array detection, after 10 days of treatment with an oleogum resin extract of Boswellia serrata (4 × 786 mg per day), the authors could most of them (Table 13.3) identify in the plasma of a patient with brain tumor.
After intake of BEs by humans AKBA in the blood is below its IC50 in vitro, but at least KBA is near to its in vitro value of about 2.4 µM. As far as β-BA is concerned, which represents the highest percentage in a BE (around 19 % s. Table 13.3) its concentration in the blood after oral injection of a BE was found to be there in effective concentrations [68].
Effect of Food Intake:
It is very well known that absorption of drugs may be related to food intake and to the kind of food. In this sense, Sterk et al. [74] studied the effect of food intake on the bioavailability of BAs from a herbal preparation of Boswellia. Twelve healthy subjects fasted 10 h before and 4 h after drug administration (group A). A second group (B) received a high-fat meal together with the drug. The volunteers swallowed a single dose of 3 capsules with 282 mg (total of 786 mg) extract, containing 143.4 mg β-BA, 103.71 mg α-BA, 82.71 mg acetyl-β-BA, 48.12 mg KBA, 28.71 mg AKBA and 26.25 mg acetyl-α-BA. The time course of the plasma concentrations of the most active boswellic acids, i.e. KBA and AKBA, was dramatically different between fasted and high-fat meal volunteers. The calculated pharmacokinetic parameters are shown in Table 13.7.
It is obvious that in the high-fat meal group Cmax of KBA is about 2.7 times and AKBA 4.8 times higher than in the fasting group. This can be explained by the lipophilic character of KBA and AKBA. Consequently, BEs should be taken together with food.
13.6.1.2 Absorption
Extract preparations from the resin of Boswellia species, in most cases, are administered by oral route. Compared to the concentrations of BAs, in extract preparations their concentrations in the blood after oral application are very low. This holds true, especially for the most active BA, i.e. AKBA. Krüger et al. [37] explain this phenomenon to be due to poor permeability of AKBA and also moderate absorption of KBA.
13.6.1.3 Distribution
According to Siemoneit et al. [67] 11-keto-boswellic acids show > 95 % plasma protein binding. However, due to their lipophilic properties it is possible, that BAs may accumulate in lipophilic tissues.
13.6.1.4 Metabolism
In rat liver microsomes, human liver microsomes and hepatocytes, Krüger et al. [36] found that KBA but not AKBA undergoes extensive phase I metabolism. Oxidation to hydroxylated metabolites is the principal metabolic route. In vitro, KBA yielded metabolic profiles similar to those obtained in vivo in rat plasma and liver, whereas no metabolites of AKBA could be identified in vivo. Unexpectedly, AKBA is not deacetylated to KBA.
13.6.1.5 Topical Administration
Extracts from the gum resin of BS are frequently used topically in ointment preparations for skin diseases. Singh et al. [71] reported anti-inflammatory activity of BAs through this route in different acute and chronic models of inflammation such as arachidonic acid- and croton-oil-induced mouse ear edema, carrageenan-induced rats paw edema and adjuvant-induced arthritis in rats. The results of the study revealed that the antiphlogistic effect observed through this route is in accordance with the study conducted with the systemic application.
13.6.2 Chronic Inflammatory Diseases
From the preclinical studies it is reasonable to conclude that BEs and their active constituents will be effective in inflammatory disorders, since they inhibit the responsible related factors, i.e. products of the arachidonic acid cascade, especially leukotrienes, members of the complement system—and especially factors of the immune system which are related to the inflammatory autoimmune system. However, their actions will not be as immediate as it is the case with nonsteroidal anti-inflammatory drugs (NSAIDs) or glucocorticoids since it is evident, from pharmacokinetc studies, that the concentration of the most active compounds, i.e. KBA and AKBA in the blood does not reach effective levels after a single administration. This is in accordance with the experience of patients who report that the therapeutic effect of BEs occurs with a certain delay of 1 or 2 weeks.
13.6.2.1 Rheumatoid Diseases
As early as 1986, Singh and Atal [69] reported that in an arthritic model in rats a mixture of boswellic acids showed anti-inflammatory activity and Sharma et al. [61] observed that in another arthritis model a mixture of BAs reduced infiltration of leucocytes into an arthritic knee. Very recently, Umar [79] studied the effect of an extract from Boswellia serrata in the collagen-induced arthritis model in rats on most of the inflammatory parameters discussed. BE was administered at doses of 100 and 200 mg/kg body weight once daily for 21 days. The effects of the treatment in rats were assessed by biochemical parameters (articular elastase, LPO, GSH, catalase, SOD and NO), inflammatory mediators (IL-1B, IL-6, TNF-α, IL-10, IFN-γ and PGE2), and histopathology in joints. In this study, BE was effective bringing significant changes to all the tested parameters (articular elastase, LPO, GSH, catalase, SOD and NO). Oral administration of BE resulted in significantly reduced levels of inflammatory mediators (IL-1B, IL-6, TNF-α, IFN-γ and PGE2), and increased levels of IL-10. The protective effects of BE against RA were also evident from the decrease in arthritis scores and bone histology. On the basis of these studies and traditional experiences, a variety of clinical studies have been initiated including subjects suffering from rheumatoid arthritis and osteoarthritis.
13.6.2.1.1 Rheumatoid Arthritis
Rheumatoid arthritis belongs to the class of autoimmune diseases. The rheumatoid lesion, which is located in the synovial membrane, includes invasion of macrophages and lymphocytes that release cytokines such as interleukines and TNF-α. Neutrophils which are present in the synovial fluid of the inflamed joints produce leukotrienes, oxygen radicals and elastase activity, which finally cause synovialitis and destruction of cartilage.
Boswellic Extracts:
Etzel [17] summarized the results of 11 mostly unpublished studies using extracts from the oleogum resin of Boswellia serrata in patients with chronic polyarthritis. The criteria were pain, swelling, sensitivity and tolerance. In five studies, patients were treated intraindividually in 2 placebo-controlled studies. In a meta-analysis of the above studies, about 50–60 % of the patients responded to this treatment. Pain and swelling of joints were improved by the commercial product H15™ (produced by Gufic Ltd. Mumbai, India), when compared to the placebo group (p < 0.05). Unfortunately, not all of these studies could be re-examined by the author of this chapter as they were not published. As a consequence, the quality and the outcome of these studies were critiqued by the German Society of Rheumatology in 1998. The arguments are mainly based on a study of Sander et al. [55]. In this multicentre controlled trial, the authors studied the effect of H 15™ versus placebo over a period of 12 weeks in 37 outpatients with rheumatoid arthritis and chronic polyarthritis being under constant therapy with steroids and disease-modifying antirheumatic drugs. The patients received 9 tablets of H 15™ (3600 mg) or placebo daily in addition to their previous therapy. Doses of NSAIDs could be adjusted on demand. Efficacy parameters were the index for swelling and pain, ESR and CRP. Pain and NSAID doses were documented at the beginning and at 6 and 12 weeks after initiation. In this study, treatment with H15™ resulted in no measurable effect. However, this study suffers from the drawback that the effect of the BE alone in comparison to standard therapy was not tested. It can be assumed that administration of H15™ to patients who are being already treated with steroids and patients with basic therapy will not experience an additional effect.
13.6.2.1.2 Osteoarthritis
Osteoarthritis is a common chronic, progressive, skeletal degenerative disorder, which often affects the knee joint and the shoulder.
Gupta et al. [22] investigated the effect of S-Compound™ (Rahul Pharma, Jammu Tawi, India), a mixture of various boswellic acids in patients suffering from chronic osteoarthritis (OA) of the primary type. A total of 50 patients were treated with either S-Compound™ (30 patients) or with Ibuprofen (20 patients) for 12–24 weeks. In this study, 60 % of the patients treated with S-Compound™ showed relief of symptoms in 12 weeks. 33.3 % out of the remaining 40 % recovered in 24 weeks but 2 patients had no relief. Only 30 % of the patients improved with Ibuprofen.
In a randomized, double-blind, placebo-controlled cross-over study, Kimmatkar et al. [34] studied efficacy, safety and tolerability of a BE preparation (trade name WokVel™ capsules) in 30 patients with osteoarthritis in the knee, 15 of them receiving the drug or placebo for 8 weeks. Each capsule of WokVel™ contained a standardized extract of Boswellia serrata oleogum resin with a minimum of 65 % organic acids or a minimum of 40 % total boswellic acids. The patients received one capsule with 333 mg of the extract three times a day and after a washout phase the alternative treatment. All patients reported decreased knee pain, increased knee flexion, an increase in the walking distance and in the ability to climb stairs. The symptoms returned after withdrawal of the treatment.
In a different double-blind, randomized, placebo-controlled study, Sengupta et al. [59] evaluated the efficacy and safety of 5-Loxin™ (Laila Natura, New Dehli, India) for treatment of OA of the knee. 5-Loxin™ is a novel Boswellia serrata extract enriched with 30 % AKBA.
Seventy-five OA patients were included in the study. The patients received either 100 mg (n = 25) or 250 mg (n = 25) of 5-Loxin™ daily or a placebo (n = 25) for 90 days. Each patient was evaluated for pain and physical functions using the standard tools (visual analogue scale, Lequesne’s Functional Index, and Western Ontario and McMaster Universities Osteoarthritis Index) at the baseline (day 0), and at days 7, 30, 60 and 90. Additionally, the cartilage degrading enzyme matrix metalloproteinase-3 was evaluated in the synovial fluid from OA patients. Measurement of a battery of biochemical parameters in the serum, haematological parameters and urine analysis were performed to evaluate the safety of 5-Loxin™. At the end of the study, both doses of 5-Loxin™ conferred clinically and statistically significant improvements in pain scores and physical function scores. Interestingly, improvements in pain score and functional ability were recorded not immediately but first 7 days after the start of treatment. Corroborating the improvements in pain scores in the treatment groups, the authors also noted significant reduction in synovial fluid matrix metalloproteinase-3. In a further study with 40 patients (20 with the same product and 20 with placebo), Sengupta et al. [60] reported similar results. Moreover, in an open randomized controlled study, Sontakke et al. [72] compared the effect of the Boswellia extract preparation WokVel™ capsules three times daily with a selective COX-2-inhibitor Valdecoxib (10 mg once daily) over a period of 6 months. Both groups showed comparable improvement as far as pains, stiffness and physical movement are concerned.
13.6.2.2 Chronic Inflammatory Bowel Diseases
Treatment of the symptoms of bowel disease with preparations containing olibanum/frankincense has a long tradition (see Chap. 2). Modern science has attributed these symptoms to different acute and chronic disorders. The latter include ulcerative colitis, chronic colitis, collagenous colitis and Crohn’s disease. Moreover, it has been recognized that certain mediators of inflammation and immunological parameters, i.e. cytokines, play an important role in these disorders.
Thus, it is known that the mucosa of patients with chronic inflammatory bowel diseases is synthesizing considerable amounts of leukotrienes LTB4, LTD4 and LTE4, which increase the production of mucus and stimulate contraction of the smooth muscle of the gastrointestinal tract. As far as the immune system is concerned, autoimmune antibodies have been detected in patients with ulcerative colitis and Crohn’s disease. In addition, IL-1 and TNF-α have also been shown to be of importance in intestinal inflammations [73]. Based on these findings, the effect of oleogum resin preparations from Boswellia serrata were tested in patients with different chronic inflammatory bowel diseases.
13.6.2.2.1 Ulcerative Colitis
Ulcerative colitis is a chronic inflammatory disease with remissions and exacerbations affecting primarily the rectal mucosa, the left colon, but in many instances also the entire colon. It is characterized by rectal bleeding and diarrhoea affecting mainly, but not exclusively, the youth and early middle age.
Boswellic Extract:
In 34 patients, suffering from ulcerative colitis grades II and III, the effect of an alcoholic extract of Boswellia serrata oleogum resin was studied according to Singh et al. [70] 350 mg thrice daily for 6 weeks, analyzing stool properties, histopathology, rectal biopsies via scan microscopy, and blood parameters including Hb, serum iron, calcium phosphorus, proteins, total leucocytes, and eosinophils [23]. Eight patients received sulfasalazine (1 g thrice daily) serving as controls. All parameters tested improved after treatment with the extract. 82 % out of treated patients went into remission while the remission rate for sulfasalazine was 75 %.
13.6.2.2.2 Chronic Colitis
This disease was characterized by the authors [25] as vague lower abdominal pain, bleeding per rectum with diarrhoea and palpable tender descending and sigmoid colon. Its pathophysiology seems to be different from that of ulcerative colitis.
Boswellic Extract:
In this study, 30 patients, 17 males and 13 females age 18–48 years, were included. Twenty patients were given a preparation of the oleogum resin of Boswellia serrata (S-Compound™) containing KBA 0.63 %, AKBA 0.7 %, acetyl-β-BA and β-BA 1.5 % (900 mg daily divided in three doses for 6 weeks) and ten patients receiving sulfasalazine (3 mg daily divided in three doses for 6 weeks) served as controls. Out of the 20 patients treated with Boswellia oleogum resin, 18 patients showed an improvement in one or more of the following parameters: stool properties, histopathology as well as scanning electron microscopy, Hb, serum iron, calcium, phosphorus, proteins, total leukocytes, and eosinophils.
13.6.2.2.3 Collagenous Colitis
A rarer chronic inflammatory bowel disease is collagenous colitis. It is characterized by aqueous diarrhoea, histological thickness of the mucosa and a subepithelial collagen band.
Boswellic Extract:
In a randomized, placebo-controlled, double-blind multicenter study, quality of life and histology were studied in 25 patients receiving either 400 mg BE (H15™) three times a day or a placebo. After 6 weeks of treatment, significant improvements were reported for 58.3 % of the Boswellia group and for 30.8 % in the placebo group [38].
13.6.2.2.4 Crohn’s Disease
Crohn’s disease (Ileitis terminalis) is a chronic inflammatory disease of the entire gastrointestinal tract from the oral cavitity up to the anal area. Most common locations are the terminal ileum, colon and rectum. Typical symptoms are abdominal pain, diarrhoea with mucus, purulency and aqueous stools. The anti-inflammatory treatment at present consists of the use of mesalazine and sulfasalazine.
Boswellic Extracts:
Gerhardt et al. [20] studied the effect of a BE (H15™) on symptoms in an active state of Crohn’s disease. In a double-blind, verum-controlled parallel group comparison, 102 patients were randomized. The protocol population included 44 patients treated with BE H15™ and 39 patients treated with mesalazine. As primary parameter, the change of the Crohn’s Disease Activity Index (CDAI) from the beginning to the end of the therapy was chosen. H15™ was tested for non-inferiority compared to the standard treatment with mesalazine. In this study, the CDAI after treatment with H15™ was reduced by 90 and after therapy with mesalazine by 53 score points in the mean. A difference between both treatments could not be proven to be statistically significant. Thus, the data suggest that in treatment of Crohn’s disease in an active state the extract from the oleogum resin of Boswellia serrata is at least as effective as a standard medication under the conditions of this study.
In a previous study [28] it was investigated whether or not, in a period of 2 years, permanent treatment with Boswellan™ (special BE extract from Pharmasan Company—Freiburg, Germany) would increase the time of remission. This was, however, not the case. Obviously, the Boswellia preparations are only effective in an acute phase of the disease, improving factors related to the CDAI.
13.6.2.3 Respiratory Diseases: Bronchial Asthma
Since ancient times (see Chap. 2) respiratory symptoms are treated with preparations of olibanum/frankincense. This still holds for bronchitis including cough and expectoration. A special case is bronchial asthma.
Bronchial asthma is a chronic inflammatory condition characterized by bronchial hyper-responsiveness and reversible airways obstruction.
Increased production of leukotrienes both during episodes of asthma and in patients with stable asthma was shown by Chanarin and Johnston [14]. Bronchial asthma is also a case of autoimmune diseases.
Boswellia Extracts:
In a double-blind, placebo-controlled trial with asthma patients Gupta et al. [24] tested forty patients with a mean duration of bronchial asthma of 9.58 ± 6.07 years. They received a preparation of oleogum resin of Boswellia serrata (S-Compound™) of 300 mg three times daily over a period of 6 weeks. In this study, 70 % of the patients showed improvement of the disease measured by the disappearance of physical symptoms and by signs such as dyspnoea, rhonchi, the number of obstructive attacks, increase in respiratory parameters, including FEV1, FVC and PEFR as well as by a decrease in eosinophilic count and ESR. In the control group of 40 patients only 27 % of these patients showed improvements.
13.6.2.4 Autoimmune Diabetes: Tyrosinephosphatase Antibody
Autoimmune Diabetes is associated with an increase of specific markers in the blood including tyrosinephosphatase antibody (IA2-A), which indicate presence of insulitis. So far there exists no clinical study whether or not a BE or BA are effective in human autoimmune diabetes.
Recently in a case report it was shown that a BE decreased blood levels of IA2-A in a patient with “Late onset Autoimmune Diabetes of the Adult” (LADA). A female patient 50 years old with a body weight of 72 kg where diabetes was first diagnosed in November 2012 and who was under insulin therapy (Humalog™, Humaninsulin basal™) received a BE “Indian Boswellia the Original™, a new product from Indian Boswellia Laboratory, Agra India, containing 3.6 % KBA and 1.4 % AKBA. The patient received 3 times daily 2 tablets (400 mg BE each) per oral route over a period of 8.5 weeks.
During this time IA2-A levels in the blood dropped from 25 to 10 K/U/L indicating improvement of insulitis [58].
The authors are aware, that this is only one case with all its restrictions. But it may stimulate other attempts to strengthen the hypothesis that BEs or BAs including KBA and AKBA may be an option for prevention/treatment of autoimmune diabetes.
What do the clinical studies teach:
In the clinical studies, that have been performed so far between 6 and 13 weeks and with a limited number of patients, improvement of symptoms in patients suffering from rheumatoid arthritis, osteoarthritis, chronic inflammatory bowel diseases and bronchial asthma were reported. This is in line with preclinical in vitro and in vivo studies showing pharmacological activity of BEs and some BAs on mediators of inflammation as well as on factors related to autoimmune disorders. It should, however, be taken into consideration that the effects of BEs are more likely to be an overall action of several components of the extract than of single compounds. Nevertheless, for future clinical studies, extracts should be standardized according to regional pharmacopoeias, for instance European Pharmacopoea, using KBA and or AKBA as leading compounds.
13.6.3 Side Effects
Taking into account the wide use of oleogum resin from different Boswellia species in ancient times and nowadays, side effects do not appear to be a critical point. This is also the outcome of the published material. Most of the side effects, if at all, are related to the gastrointestinal tract. In detail:
Gastrointestinal Tract:
In the study using S-Compound™ [22], dyspeptic symptoms in form of pain in abdomen, distension of abdomen, sour eructation and loss of appetite were reported in 8 % while 60 % of patients treated with Ibuprofen had dyspeptic symptoms.
In a further trial with S-Compound™, two from 40 patients complained about epigastric pain, hyperacidity, and nausea [24]. In a study dealing with ulcerative colitis [23], 6 out of 34 patients reported retrosternal burning, nausea, fullness of abdomen, epigastric pain and anorexia.
Böker and Winking [7], studying the effect of H15™, reported that some patients developed nausea and vomiting. The side effects were reversible after omission of the treatment. Comparing the effect of H15™ (44 patients) with mesalazine (39 patients) suffering from Crohn’s disease), Gerhardt et al. [20] reported no drug related side effects in the H15™ group but 4 patients treated with mesalazine suffered from headache and gastrointestinal symptoms. In the study of Gupta et al. [25], out of 20 patients treated with Boswellia gum resin, only 2 patients complained of heartburn and Streffer et al. [75] reported that the preparation H15™ was well tolerated, only some gastrointestinal complains were observed. BE (15 patients) was also well tolerated in the study of Kimmatkar et al. [34] exept for minor gastrointestinal reactions. In the study of Sontakke et al. [72], one patient out of 33 receiving BE complained about diarrhoea and abdominal cramps.
Boswellic extracts in higher doses are used in treatment of cerebral edemas caused by brain tumours. In a prospective, randomized, placebo-controlled double-blind pilot study [35], where 22 patients with brain tumours received 4200 mg of a BE (H15™) or placebo, diarrhoea grade 1–2 occurred in 6 patients of the BE group. Other side effects were the same as in the placebo group.
Respiratory Tract:
There is a case report from a patient who complained about asthma symptoms after exposure to fume of incense in the church [46].
Skin:
In an other case report Acebo et al. [1] describe a patient suffering from allergic contact dermatitis using an extract from Boswellia serrata in a naturopathic cream.
In two patients being treated with H15™ for brain edema, Böker and Winking [7] described skin irritations. The side effects were reversible after omission of the treatment.
General Tolerability:
No adverse reactions were observed in a double-blind placebo-controlled study in 20 volunteers receiving topical formulation cream containing boswellic acids [39]. No side effects were also observed in the pharmacokinetic study of Sharma et al. [63] and in the study on OA by Sengupta et al. [59]. And the study of Holtmeier et al. [28] confirmed good tolerance of the preparation Boswellan™ over a period of 52 weeks.
When Aflapin™ (Laila Impex R & D Center, New Dehli, India) and 5-Loxin™ were used to treat osteoarthritis in comparison to a placebo [59, 60], the safety parameters were almost unchanged in the treatment group. In a retrospective analysis in 2000, the laboratory parameters before and after the treatment of patients suffering from rheumatoid arthritis, ulcerative colitis, Crohn’s disease, neurodermitis, lupus erythematosus, multiple sclerosis, astrocytoma, glioblastoma, bronchial asthma and psoriasis were tested receiving the Boswellia preparation H15™ over a period of 6 years.
No significant changes related to the therapy were observed [10].
All together, it appears that extracts from the oleogum resin of Boswellia species are relatively safe as far as side effects are concerned. This is one of the big advantages compared to all anti-inflammatory remedies being in use presently.
Abbreviations
- AA:
-
Arachidonic Acid
- ABA:
-
Acetyl-boswellic acid
- Ac-OH-LA:
-
3α-Acetoxy-28-hydroxylup-20 (29)
- AKBA:
-
Acetyl-11-keto-β-Boswellic acid
- α-BA:
-
α-Boswellic acid
- β-BA:
-
β-Boswellic acid
- BA:
-
Boswellic acid
- BE:
-
Boswellic extract
- BS:
-
Boswellia serrata
- BSA:
-
Bovine serum albumin
- CD4:
-
CD4 lymphocytes
- CD8:
-
CD8 lymphocytes
- CIA:
-
Collagen-induced arthritis
- COX:
-
Cyclooxygenase
- CRP:
-
C-reactive protein
- CDAI:
-
Crohn’s Disease Activity Index
- ConA:
-
Concavalin A
- ESR:
-
Erythrocyte Sedimentation Rate
- FCV:
-
Forced vital capacity
- FEV1 :
-
Forced expiratory volume
- GSH:
-
Reduced glutathione
- Hb:
-
Hemoglobin
- HETE:
-
Hydroxyeicosatetraenoic acid
- 12-HHT:
-
12-Hydroxyheptadecatrienoic acid
- HLE:
-
Human Leucozyte Elastase
- IA2-A:
-
Tyrosinephosphatase antibody
- IFN-γ:
-
Interferon-γ
- IgG:
-
Immunoglobulin G
- IgM:
-
Immunoglobulin M
- IL:
-
Interleukin
- IMG:
-
Immune globulin
- KBA:
-
11-Keto-β-Boswellic acid
- LA:
-
Lupenoic acid
- LADA:
-
Late onset autoimmune diabetes of the adult
- 5-LO:
-
5-Lipoxigenase
- 12-LO:
-
12-Lipoxigenase
- LPO:
-
Lipid peroxidase
- LPS:
-
Lipopolysaccharide
- LTB4 :
-
Leukotriene B
- LTC4 :
-
Leukotriene C4
- LTD4 :
-
Leukotriene D4
- LTE4 :
-
Leukotriene E4
- MIC:
-
Minimal inhibitory concentration
- f-MLP:
-
n-formylmethionyl-leucyl-phenylalanine
- MLD-STZ:
-
Multiple low-dose streptozotocin
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate hydrate
- NFκB:
-
Nuclear transcription factor κB
- NK cells:
-
Natural killer cells
- NO:
-
Nitrogen monoxide
- NSAID:
-
Nonsteroidal anti-inflammatory drugs
- OA:
-
Osteoarthritis
- PEFR:
-
Peak expiratory flow rate
- PGE2 :
-
Prostaglandin E2
- PBMC:
-
Peripheral blood mononuclear cells
- PEFR:
-
Peak expiratory flow rate
- PGE1 :
-
Prostaglandin E1
- PHA:
-
Phytohemagglutinin
- PMA:
-
Phorbol 12-myristate 13-acetate
- PMN:
-
Polymorph mononuclear neutrophil leucocyte
- RA:
-
Rheumatoid arthritis
- SG:
-
Salai guggal
- SOD:
-
Superoxid dismutase
- STZ:
-
Streptozotocin
- TA:
-
Tirucallic acid
- Th1 :
-
Th1 lymphocytes
- Th2 :
-
Th2 lymphocytes
- TNF-α:
-
Tumor necrosis factor alpha
- t1/2:
-
Half-life
References
Acebo E, Raton JA, Saulua S, Eizaguirre X, Trébol J, Perez JLD (2004) Allergic contact dermatitis from Boswellia serrata extract in a naturopathic cream. Contact Dermat 51:91
Adelakun EA, Finbar EA, Agina SE, Makinde AA (2001) Antimicrobial activity of Boswellia dalzielii stern bark. Fitoterapia 72:822–824
Ammon HP, Mack T, Singh GB, Safayhi H (1991) Inhibition of leukotriene B4 formation in rat peritoneal neutrophils by an ethanolic extract of the gum resin exudates of Boswellia serrata. Planta Med 57:203–207
Badria FA, Mikhaeil BR, Maatooq GT, Amer MM (2003) Immunmodulatory terpenoids from the oleogum resin of Boswellia carterii Bordwood. Z Naturforsch 58:506–516
Beisner K, Büchele B, Werz U, Simmet T (2003) Structural analysis of 3-α-acetyl-20(29)-lupene-24-oic acid, a novel pentacyclic triterpene isolated from the gum resin of Boswellia serrata, by NMR spectroscopy. Magn Reson Chem 41:629–632
Blain EJ, Ali AY, Duance VC (2010) Boswellia frereana (frankincense) suppresses cytokine-induced matrix metalloproteinase expression and production of proinflammatory molecules in articular cartilage. Phytother Res 24:905–912
Böker DK, Winking M (1997) Die Rolle von Boswellia-Säuren in der Therapie maligner Gliome. Dtsch Ärztebl 94:B-958–B-960
Büchele B, Simmet T (2003) Analysis of 12 different pentacyclic triterpenic acids from frankincense in human plasma by high performance liquid chromatography and photodiode array detection. J Chromatogr B 795:355–362
Büchele B, Zugmaier W, Simmet T (2003) Analysis of pentacyclic triterpenic acids from frankincense gum resins and related phytopharmaceuticals by high-performance liquid chromatography. Identification of lupeolic acid, a novel pentacyclic triterpene. J Chromatogr B 791:21–30
Buvari PG (2001) Wirksamkeit und Unbedenklichkeit der H15 Ayurmedica-Therapie bei chronisch entzündlichen Erkrankungen. Dissertation, University of Mannheim-Heidelberg
Camardes L, Dayton T, Di Stefano V, Pitonzo R, Schillaci D (2007) Chemical composition and antimicrobial activity of some oleogum resin essential oils from Boswellia spp. (Burseraceae). Ann Chim 97:837–844
Cao H, Yu R, Choi Y, Ma ZZ, Zhang H, Xiang W, Lee DY et al (2010) Discovery of cyclooxygenase inhibitors from medicinal plants used to treat inflammation. Pharmacol Res 61:519–524
Chervier MR, Ryan AE, Lee DY, Zhongze M, Wu-Yan Z, Via CS (2005) Boswellia carterii extract inhibits TH1 cytokines and promotes TH2 cytokines in vitro. Clin Diagn Lab Immunol 1:575–580
Chanarin N, Johnston SL (1994) Leukotrienes as a target in asthma therapy. Drugs 47:12–24
Cnop M, Welsh N, Jonas JC et al (2005) Mechanisms of pancreatic beta-cell death in type 1 and type 2 diabetes: many differences, few similarities. Diabetes 54(Suppl. 2):97–107
Cuaz-Pérolin C, Billiel L, Baugé E, Copin C, Scott-Algaria D, Genze F, Rouis M et al (2008) Antiinflammatory and antiatherogenic effects of NF-Kappa B inhibitor acetyl-11-beta-boswellic acid in LPS-challenged ApoE-/- mice. Arterioscler Thromb Vasc Biol 28:272–277
Etzel R (1996) Special extract of Boswellia serrata (H15) in the treatment of rheumatoid arthritis. Phytomedicine 3:91–94
Fan AY, Lao L, Zhang RX, Wang LB, Lee DY, Ma ZZ et al (2005) Effects of an acetone extract of Boswellia carterii Birdw. (Burseraceae) gum resin on rats with persistent inflammation. J Altern Complement Med 11:323–331
Gayathri B, Manjula N, Vinaykumar KS, Lakshmi BS, Balakrishnan A (2007) Pure compound from Boswellia serrata extract exhibits anti-inflammatory property in human PBMCs and mouse macrophages through inhibiton of TNF alpha, IL-1beta, NO and MAP kinases. Int Immunopharmacol 7:472–482
Gerhardt H, Seifert F, Buvari P, Vogelsang H, Repges RZ (2001) Therapie des aktiven Morbus Crohn mit Boswellia serrata Extract H 15. Z Gastroenterol 39:11–17
Gupta OP, Sharma N, Chand DA (1992) Sensitive and relevant model for evaluating anti-inflammatory activity-papaya latex-induced rat paw inflammation. J Pharmacol Toxicol Methods 28:15–19
Gupta J, Gupta S (1993) Parihar A. S-compound-A traditional drug for osteoarthritis patients. The Indian Practitioner 46:69–72
Gupta I, Parihar A, Malhotra P, Singh GB, Lüdtke R, Safayhi H, Ammon HP (1997) Effects of Boswellia serrata gum resin in patients with ulcerative colitis. Eur J Med Res 2:37–43
Gupta I, Gupta V, Parihar A, Gupta S, Lüdtke R, Safayhi H, Ammon HP (1998) Effects of Boswellia serrata gum resin in patients with bronchial asthma: results of a double-blind, placebo-controlled, 6-week clinical study. Eur J Med Res 3:511–514
Gupta I, Parihar A, Malhorta P, Gupta S, Ludtke R, Safayhi H et al (2001) Effects of gum resin of Boswellia serrata in patients with chronic colitis. Planta Med 67:391–395
Gupta A, Khajuria A, Singh J, Singh S, Suri KA, Qazi GN (2011) Immunological adjuvant effect of Boswellia serrata (BOS 2000) on specific antibody and cellular response to ovalbumin in mice. Int Immunopharmacol 11:968–975
Heil K, Ammon HP, Safayhi H (2001) Inhibiton of NADPH-oxidase by AKBA in intact PMNs. Naunyn Schmiedebergs Arch Pharmacol 3635:R14
Holtmeier WH, Zeuzem S, Preiß J, Kruis W, Böhm S, Maaser Ch et al (2010) Randomized, placebo-controlled, double-blind trial of Boswellia serrata in maintaining remission of Crohn’s Disease: good safety profile but lack of efficacy. Inflamm Bowel Dis 17(2):573–582
Hussein G, Miyashiro H, Nakamura N, Hattori M, Kakiuchi N, Shimotohno K (2000) Inhibitory effects of sudanese medicinal plant extracts on hepatitis C virus (HCV) protease. Phytother Res 14:510–516
Kapil A, Moza N (1991) Anticomplementary activity of Boswellia acids—an inhibitor of C3-convertase of the classical complement pathway. Int J Immunopharmacol 14:1139–1143
Karr A, Menon MK (1969) Analgesic effect of the gum resin of Boswellia serrata Roxb. Life Sci 8:1023–1028
Kela SL, Ogunsusi RA, Ogbogu VC, Nwude N (1989) Screening of some Nigeria plants for molluscicidal activity. Rev Elev Med Vet Pays Trop 42:195–202
Khajuria A, Gupta A, Suden P, Singh S, Malik F, Singh J et al (2008) Immunmodulatory activity of biopolymeric fraction BOS 2000 from Boswellia serrata. Phytother Res 22:340–348
Kimmatkar N, Thawani V, Hingorani L, Khiyani R (2003) Efficacy and tolerability of Boswellia serrata extract in treatment of osteoarthritis of knee—a randomized double blind placebo controlled trial. Phytomedicine 10:3–7
Kirsten S, Treier M, Wehrle SJ, Becker G, Abdel-Tawab M, Gerbeth K et al (2011) Boswellia serrata acts on cerebral edema in patients irradiated for brain tumors. Cancer 117:3788–3795
Krüger P, Daneshfar R, Eckert GP, Klein J, Volmer DA et al (2008) Metabolism of boswellic acids in vitro and in vivo. Drug Metabol Distpos 36:1135–1142
Krüger P, Kanzer J, Hummel J, Fricker G, Schubert-Zsilavecz M, Abdel-Tawab M (2009) Permeation of Boswellia extract in the Caco-2 model and possible interactions of its constituents KBA and AKBA with OATP1B3 and MRP2. Eur J Pharm Sci 36:275–284
Madisch A, Miehlke S, Eichele O, Bethke B, Mrwa J, Kuhlisch E et al (2005) Boswellia serrata Extrakt bei kollagener Kolitis – eine randomisierte, placebo-kontrollierte, doppelblinde Multicenterstudie. Dtsch Ges Verdau Stoffw Erkr. Gastroenterol 43(Suppl. Z):P061
Martelli L, Berardesca E, Martelli M (2000) Topical formulation of a new plant extract complex with refirming properties. Clinical and non-invasive evaluation in a double-blind trial. Int J Cosmet Sci 22:201–206
Martinez D, Lohs K, Janzen J (1989) Weihrauch und Myrrhe. Kulturgeschichte und wirtschaftliche Bedeutung. Botanik, Chemie, Medizin. Wissenschaftliche Verlagsgesellschaft, Stuttgart
Mikhaeil BR, Maatooq GT, Badria FA, Amer MM (2003) Chemistry and immunomodulatory activity of frankincense oil. Z Naturforsch C 58:230–238
Mothana RA, Lindequist U (2005) Antimicrobial activity of some medicinal plants of the island Sogotra. J Ethnopharmacol 96:177–181
Mothana RA, Mentel R, Reiss C, Lindequist U (2006) Phytochemical screening and antiviral activity of some medicinal plants from the island Sogotra. Phytother Res 20:298–302
Mothana RA (2011) Anti-inflammatory, antinociceptive and antioxidant activities of the endemic Sogotraen Boswellia elongata Balf. F. and Jatropha unicostata Balf. F. in different experimental models. Food Chem Toxicol 49:2594–2599
Moussaieff A, Shohami E, Kashman Y, Fride E, Schmitz ML, Renner F et al (2007) Incensolate acetate, a novel anti-inflammatory compound isolated from Boswellia resin, inhibits nuclear factor-kappa B activation. Mol Pharmacol 72:1657–1664
O’Connor TM, Cusack R, Lauders S, Bredin CP (2014) Holy Saturday asthma. BMJ Case Rep doi:10.1136/bcr-2014-203861
Poeckel D, Tausch L, Kather N, Jauch J, Werz O (2006) Boswellic acids stimulate arachidonic acid release and 12-lipoxygenase activity in human platelets independent of Ca2+ and differentially interact with platelet-type 12-lipoxygenase. Mol Pharmacol 70:1071–1078
Raja AF, Ali F, Khan IA, Shawl AS, Arora DS (2011) Acetyl-11-keto-β-boswellic acid (AKBA); targeting oral cavity pathogens. BMC Res Notes 4:406
Reddy KP, Singh AB, Puri A, Srivastava K, Narender T (2009) Synthesis of novel triterpenoid (lupeol) derivatives and their in vivo antihyperglycemic and antidyslipidemic activity. Bioorg Med Chem Lett 19:4463–4466
Safayhi H, Mack T, Sabieraj J, Anazodo MI, Subramanian LR, Ammon HP (1992) Boswellic acids: novel, specific, nonredox inhibitors of 5-lipoxygenase. J Pharmacol Exp Ther 261:1143–1146
Safayhi H, Sailer ER, Ammon HP (1995) Mechanism of 5-lipoxygenase inhibition by acetyl-11-keto-beta-boswellic acid. Mol Pharmacol 47:1212–1216
Safayhi H, Rall B, Sailer ER, Ammon HP (1997) Inhibition by Boswellic acids of human leukocyte elastase. J Pharmacol Exp Ther 281:460–463
Sailer ER, Subramanian LR, Rall B, Hoernlein RF, Ammon HP, Safayhi H (1996) Acetyl-11-keto-beta-boswellic acid (AKBA): structure requirements for binding and 5-lipoxygenase inhibitory activity. Br J Pharmacol 117:615–618
Sailer ER, Schweizer S, Boden SE, Ammon HP, Safayhi H (1998) Characterization of an acetyl-11-keto-beta-boswellic acid and arachidonate-binding regulatory site of 5-lipoxygenase using photoaffinity labeling. Eur J Biochem 256:364–368
Sander O, Herborn G, Rau R (1998) Is H15 (extract of Boswellia serrata “incense”) an efficient supplementation to established drug therapy of rheumatoid arthritis? Results of a double-blind pilot trial. Z Rheumatol 57:11–16
Schillaci D, Arizza V, Dayton T, Camarda L, Di SV (2008) In vitro anti-biofilm activity of Boswellia spp. Oleogum resin essential oils. Lett Appl Microbiol 47:433–438
Schmidt TJ, Kaiser M, Brun R (2011) Complete structural assignment of serratol, a cembrane-type diterpene from Boswellia serrata and evaluation of its antiprotozoal activity. Planta Med 77:849–850
Schrott E, Laufer S, Lämmerhofer M, Ammon HPT (2014) Extract from gum resin of Boswellia serrata decreases IA2-antibody in a patient with “Late onset Autoimmune Diabetes of the Adult” (LADA). Phytomedicine 21:786
Sengupta K, Alluri KV, Satish AR, Mishra S, Golakoti T, Sarma KV et al (2008) A double blind, randomised, placebo controlled study of the efficacy and safety of 5-Loxin for treatment of osteoarthritis of the knee. Arthritis Res Ther 10:R85
Sengupta K, Krishnaraju AV, Vishal AA, Mishra A, Trimurtulu G, Sarma KV et al (2010) Comperative efficacy and tolerability of 5-Loxin and Aflapin. Against osteoarthritis of the knee: a double blind, randomized, placebo controlled clinical study. Int J Med Sci 7:366–379
Sharma ML, Bani S, Singh CB (1989) Antiarthritic activity of boswellic acids in bovine serum albumin (BSA)-induced arthritis. Int J Immunopharmacol 11:647-652
Sharma ML, Kaul A, Khajuria A, Singh S, Singh GB (1996) Immunomodulatory activity of boswellic acids (pentacyclic triterpene acids) from Boswellia serrata. Phytother Res 10:107–112
Sharma S, Thawani V, Hingorani L, Shrivastava M, Bhate VR, Khiyani R (2004) Pharmacokinetic study of 11-keto-beta-boswellic acid. Phytomedicine 11:255–260
Shehata AM, Quintanilla-Fend L, Bettio S, Singh CB, Ammon HP (2011) Prevention of multiple low-dose streptozotocin (MLD-STZ) diabetes in mice by an extract from gum resin of Boswellia serrata (BE). Phytomedicine 18:1037–1044
Shehata AM, Quintanilla-Fend L, Bettio S, Jauch J, Scior T, Scherbaum WA, Ammon HPT (2015) 11-Keto-β-Boswellic acids prevent development of autoimmune reactions, insulitis and reduce hyperglycemia during induction of multiple low dose streptozotocin (MLD-STZ) diabetes in mice. Horm Metab Res 47:463–469
Siemoneit U, Hofmann B, Kather N, Lamkemeyer T, Madlung J, Franke L et al (2008) Identification and functional analysis of cyclooxygenase-1 as a molecular target of Boswellic acids. Biochem Pharmacol 75:503–513
Siemoneit U, Pergola C, Jazzar B, Northoff H, Skarke C, Jauch J, Werz O (2009) On the interference of Boswellic acids with 5-lipoxygenase: mechanistic studies in vitro and pharmacological relevance. Eur J Pharmacol 606:246–254
Siemoneit U, Koeberle A, Rossi A, Dehm F, Verhoff M, Reckel S et al (2011) Inhibition of microsomal prostaglandin E2 synthase-1 as a molecular basis for the anti-inflammatory actions of Boswellic acids from frankincense. Br J Pharmacol 162:147–162
Singh GB, Atal CH (1986) Pharmacology of an extract of salai guggal ex Boswellia serrata, a new non-steroidal anti-inflammatory agent. Agents Actions 18:407–412
Singh GB, Singh S, Bani S (1996) Alcoholic extract of salai-guggal ex Boswellia serrata, a new natural source NSAID. Drugs Today 32:109–112
Singh S, Khajuria A, Taneja SC, Khajuria RK, Singh J, Johri RK, Qazi GN (2008) Boswellic acids: a leukotriene inhibitor also effective through topical application in inflammatory disorders. Phytomedicine 15:400–407
Sontakke S, Thawani V, Pimpalkhute S, Kabra P, Bubhulkar S, Hingorani L (2007) Open, randomized controlled clinical trial of Boswellia serrata extract as compared to valdecocib in osteoarthritis of knee. Indian J Pharmacol 39:27–29
Stange EF, Schreiber S, Raedler A et al (1997) Therapie des Morbus Crohn. Z Gastroenterol 35:541–554
Sterk V, Büchele B, Simmet T (2004) Effect of food intake on the bioavailability of boswellic acids from a herbal preparation in healthy volunteers. Planta Med 70:1155–1160
Streffer JR, Bitzer M, Schabet M, Dichganz J, Weller M (2001) Response of radiochemotherapy-associated cerebral edema a phytotherapeutic agent, H15. Neurology 56:1219–1221
Syrovets T, Büchele B, Krauss C, Laumonnier Y, Simmet T (2005) Acetylboswellic acids inhibit lipopolysaccharide-mediated TNF-alpha induction in monocytes by direct interaction with IkappaB kinase. J Immunol 174:498–506
Takada Y, Ichikawa H, Badmaev V, Aggarwal BB (2006) Acetyl-11-keto-beta-boswellic acid potentiates apoptosis, inhibits invasion and abolishes osteoclastogenesis by suppressing NF-kappa B and NF-kappa B-regulated gene expression. J Immunol 176:3127–3140
Tausch L, Henkel A, Siemoneit U, Poeckel D, Kather N, Franke L et al (2009) Identification of human cathepsin G as a functional target of boswellic acids from the anti-inflammatory remedy frankincense. J Immunol 183:3433–3442
Umar S, Umar K, Saarwar AH, Khan A, Ahmad N (2014) Boswellia serrata extract attenuates inflammatory mediators and oxidative stress in collagen induced arthritis. Phytomedicine 21:847–856
Verhoff M, Seitz S, Northoff H, Jauch J, Schaible AM, Werz O (2012) A novel C(28)-hydroxylated lupeolic acid suppresses the biosynthesis of eicosanoids through inhibition of cytosolic phospholipase A(2). Biochem Pharmacol 84:681–691
Wagner H, Knaus W, Jordan E (1987) Pflanzeninhaltsstoffe mit Wirkung auf das Komplementsystem. Z Phytother 8:148–149
Wang H, Syrovets T, Kess D, Büchele B, Hainzl H, Lunov O et al (2009) Targeting NF-kappa B with a natural triterpenoid alleviates skin inflammation in a mouse model of psoriasis. J Immunol 1:4755–4763
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Ammon, H.P.T. (2016). Boswellic Acids and Their Role in Chronic Inflammatory Diseases. In: Gupta, S., Prasad, S., Aggarwal, B. (eds) Anti-inflammatory Nutraceuticals and Chronic Diseases. Advances in Experimental Medicine and Biology, vol 928. Springer, Cham. https://doi.org/10.1007/978-3-319-41334-1_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-41334-1_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-41332-7
Online ISBN: 978-3-319-41334-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)