Abstract
This section provides a comprehensive procedural report for percutaneous transluminal embolization of Type II endoleak procedure with up-to-date explanatory notes, synopsis of the indications and contraindications, and potential complications in an organized and practical format.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
INTRODUCTION
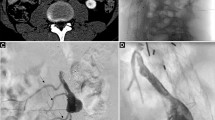
Endovascular aneurysm repair (EVAR) of abdominal aortic aneurysms has become a widely accepted alternative to open repair with similar survival and rupture outcomes. There are five subtypes of endoleak following EVAR; type II endoleak is the most common (40 %) and involves perigraft blood flow via an artery arising from the aneurysm sac [1]. There are two subtypes of type II endoleaks, single vessel inflow and outflow is characterized as IIA and multiple inflow/outflow vessels are characterized as IIB. The annual incidence of type II endoleaks following endovascular aneurysm repair is approximately 5–8 % [2, 3]. The presence of a type II endoleak on imaging is associated with a very low risk of rupture if there is no accompanying increase in aneurysm sac diameter and these endoleaks often resolve spontaneously. However, growth of the aneurysm sac associated with a type II endoleak is concerning for impending rupture. A 5 mm interval increase in maximum diameter of the sac over a 6-month period is a widely accepted treatment threshold [4]. Treatment of a type II endoleak requires cessation of the inflow/outflow of perigraft blood by embolization either via a percutaneous transluminal or transarterial approach. These two techniques have been shown to have similar success and complication outcomes [5]. Regardless of technique, the sac must be embolized centrally much like the nidus of an arteriovenous malformation to achieve success. Percutaneous puncture of the aneurysm sac can be achieved by a translumbar or transabdominal approach and is typically performed with computed tomography (CT), ultrasound (US), or fluoroscopic guidance.
COMMON INDICATIONS [4, 6]
Absolute Indications:
-
5 mm or greater increase in maximum aneurysm sac diameter over a 6-month period during EVAR surveillance
Relative Indications:
-
Less than 5 mm increase in maximum aneurysm sac diameter over a 6-month surveillance period
-
5 mm or greater increase in maximum aneurysm sac diameter over a surveillance period longer than 6 months
COMMON CONTRAINDICATIONS
-
Unsafe window for percutaneous access to aneurysm sac
-
Severe coagulopathy that cannot be corrected (relative contraindication)
PREPROCEDURAL ASSESSMENT AND PLANNING [8–10]
-
History, indications, and physical examination (Appendix 1 in Chap. 149 )
-
Evaluation of diagnostic imaging studies to determine the relevant anatomy and a safe approach for percutaneous access to aneurysm sac
-
Periprocedural management of coagulation status (Appendices 2 in Chap. 150 and 3 in Chap. 151 )
-
Antibiotic prophylaxis: Not routinely recommended [8] (Appendices 4 in Chap. 152 and 5 in Chap. 153 )
-
Imaging modality for guidance: CT or US
-
Positioning: Supine for transabdominal approach, prone for translumbar approach
PROCEDURE NOTE
Procedure: Percutaneous transluminal embolization of type II endoleak
-
Staff: [_]
-
Fellow: [_]
-
Resident: [_]
-
Clinical History and Indications: Describe history and indication (include date of endograft placement and specify interval increase in aneurysm sac diameter and length of surveillance period)
-
Allergies: None known/Allergic to [specify/type of allergy]
-
Anesthesia: Local anesthesia/Conscious sedation/General anesthesia
-
Medications: List any relevant medications used
-
Contrast Material: (_) mL of [type] contrast material was used for intravenous injection (CT) /None (US)
-
Field: Sterile
-
Procedure classification: Clean
-
Position: Supine/Prone
-
Monitoring: Intravenous access line was secured and vital signs were continuously monitored by nursing staff/anesthesia team throughout the procedure
-
Total fluoroscopy time: (_) min
-
Cumulative radiation dose: (_) mGy
Description of Procedure:
The risks, benefits, alternatives, and procedure itself were explained to the patient/patient’s Power of Attorney/patient’s legal guardian, and informed written consent was obtained. Time out was performed to confirm the correct patient, procedure, and site. The site of the procedure was identified and marked.
The patient was positioned supine/prone, with the arms placed above the head. The patient’s abdomen/back was prepped and draped in usual sterile fashion. Limited CT/US examination was performed to visualize the aneurysm sac and determine a safe approach for percutaneous access. Local anesthesia was administered. The chosen access site was punctured under CT/US guidance using a (…)-gauge [type] needle. The needle was advanced into the aneurysm sac using CT/CT fluoroscopy/real-time US guidance. Once the needle tip was properly placed in perfused portion of the aneurysm demonstrating contrast enhancement (CT) /color Doppler flow (US) and confirmed with free return of blood, embolization was performed using [embolic material of choice—coils, N-isobutyl cyanoacrylate (glue), ethylene vinyl alcohol polymer (Onyx), gelfoam, thrombin]. Embolization was performed to stasis and confirmed with repeat CT/lack of Doppler signal on US.
The needle was removed and adequate hemostasis was achieved at the percutaneous access site. Sterile dressing was applied and the patient was transferred to the floor/recovery room following the procedure in a stable condition. Staff was present for the entire procedure.
Intra-Procedure Findings: List all relevant findings.
Immediate Complications: None encountered during or directly after the procedure. List complications if any.
-
Bed rest for 2 h with patient positioned to keep percutaneous access site down [positioning depends on access site location].
-
Check the access site for any bleeding or hematoma formation every 15 min for 1 h, then every 30 min for 1 h; inform interventional radiology team if any complications are observed.
-
Monitor vital signs every 15 min for 1 h, then every 30 min for 1 h; notify interventional radiology team if systolic blood pressure <90 mmHg, or heart rate >110 beats/min.
-
Resume diet and previous orders as needed and if not otherwise contraindicated.
-
Continue adequate intravenous hydration and monitor fluid (intake–output) status.
-
Follow up imaging, typically with CT angiography, recommended at 1 month, 6 months, 12 months, and annually thereafter to monitor aneurysm sac for continued/new expansion. Continued growth of aneurysm sac may require additional embolization or open surgical repair.
Impression:
-
Percutaneous transluminal embolization of abdominal aortic aneurysm type II endoleak using [embolic material above].
-
The patient tolerated the procedure well and left the interventional unit in stable condition.
-
The patient was unstable and the procedure was canceled/terminated prematurely.
-
List any other relevant or important information/finding.
Abbreviations
- EVAR:
-
Endovascular aneurysm repair
- IMA:
-
Inferior mesenteric artery
- CT:
-
Computed tomography
- US:
-
Ultrasound
References
Bashir MR, Ferral H, Jacobs C, McCarthy W, Goldin M. Endoleaks after endovascular abdominal aortic aneurysm repair: management strategies according to CT findings. AJR Am J Roentgenol. 2009;192(4):W178–86.
van Marrewijk C, Buth J, Harris PL, Norgren L, Nevelsteen A, Wyatt MG. Significance of endoleaks after endovascular repair of abdominal aortic aneurysms: the EUROSTAR experience. J Vasc Surg. 2002;35(3):461–73.
Mehta M, Sternbach Y, Taggert JB, Kreienberg PB, Roddy SP, Paty PS, et al. Long-term outcomes of secondary procedures after endovascular aneurysm repair. J Vasc Surg. 2010;52(6):1442–9.
Hausegger KA. Endoleaks: Classification, Diagnosis, and Treatment. In: Mauro MA, Murphy KPJ, Thomson KR, Venbrux AC, Morgan RA, editors. Image-guided interventions. 2nd ed. Philadelphia: Saunders Elsevier; 2014. p. 334–47.
Stavropoulos SW, Park J, Fairman R, Carpenter J. Type 2 endoleak embolization comparison: translumbar versus modified transarterial embolization. J Vasc Interv Radiol. 2009;20(10):1299–302.
Lookstein RA, Giordano CF. Diagnosis and Management of Endoleaks. In: Kandarpa K, Machan L, editors. Handbook of interventional radiologic procedures. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2011. p. 198–205.
Sarac TP, Gibbons C, Vargas L, Liu J, Srivastava S, Bena J, et al. Long-term follow-up of type II endoleak embolization reveals the need for close surveillance. J Vasc Surg. 2012;55(1):33–40.
Venkatesan AM, Kundu S, Sacks D, Wallace MJ, Wojak JC, Rose SC, et al. Practice guidelines for adult antibiotic prophylaxis during vascular and interventional radiology procedures. J Vasc Interv Radiol. 2010;21:1611–30.
Taslakian B, Sebaaly MG, Al-Kutoubi A. Patient evaluation and preparation in vascular and interventional radiology: what every interventional radiologist should know (part 1: patient assessment and laboratory tests). Cardiovasc Intervent Radiol. 2016;39(3):325–33.
Taslakian B, Sebaaly MG, Al-Kutoubi A. Patient evaluation and preparation in vascular and interventional radiology: what every interventional radiologist should know (part 2: patient preparation and medications). Cardiovasc Intervent Radiol. 2016;39(4):489–99. doi: 10.1007/s00270-015-1239-4. [Epub 2015 Nov 25].
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Aaltonen, E.T. (2016). Percutaneous Transluminal Embolization of Type II Endoleak. In: Taslakian, B., Al-Kutoubi, A., Hoballah, J. (eds) Procedural Dictations in Image-Guided Intervention. Springer, Cham. https://doi.org/10.1007/978-3-319-40845-3_77
Download citation
DOI: https://doi.org/10.1007/978-3-319-40845-3_77
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-40843-9
Online ISBN: 978-3-319-40845-3
eBook Packages: MedicineMedicine (R0)