Abstract
Hypertension (HT) remains the main risk factor for developing coronary artery disease, congestive heart failure, stroke and kidney disease [1]. Its prevalence continues to increase exponentially due to better detection and an increase in associated factors such as obesity, physical inactivity and diabetes mellitus. Data from the National Health and Nutritional Examination Survey (NHANES) between 2007 and 2010 show that HT affects 33 % (77.9 million) of people aged ≥ 20 years in the United States [2] and the prevalence is estimated to increase to 37.3 % by 2030 [3]. This trend is spreading, even in countries that traditionally have a lower cardiovascular risk, such as Spain, where, in a cohort of 11,957 persons aged ≥ 18 years, 33 % (3983 persons) had a BP ≥ 140/90 mmHg, but > 40 % were unaware of this [4]. These data alert us to the magnitude of the problem and the need for increased efforts to improve the diagnosis, treatment and, especially, the prevention of hypertensive disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Hypertension (HT) remains the main risk factor for developing coronary artery disease, congestive heart failure, stroke and kidney disease [1]. Its prevalence continues to increase exponentially due to better detection and an increase in associated factors such as obesity, physical inactivity and diabetes mellitus. Data from the National Health and Nutritional Examination Survey (NHANES) between 2007 and 2010 show that HT affects 33 % (77.9 million) of people aged ≥ 20 years in the United States [2] and the prevalence is estimated to increase to 37.3 % by 2030 [3]. This trend is spreading, even in countries that traditionally have a lower cardiovascular risk, such as Spain, where, in a cohort of 11,957 persons aged ≥ 18 years, 33 % (3983 persons) had a BP ≥ 140/90 mmHg, but > 40 % were unaware of this [4]. These data alert us to the magnitude of the problem and the need for increased efforts to improve the diagnosis, treatment and, especially, the prevention of hypertensive disease.
By 1970, Keys et al. were already highlighting the influence of lifestyles on the development and/or prevention of cardiovascular disease (CVD), with particular emphasis on the important role of diet. This was the basis for the Seven Countries Study [5], an ecological study of 12,770 participants aged 40–59 years from Finland, Greece, Italy, Japan, Netherlands, Norway, the United States and Yugoslavia, who were followed for 5 years. The study found significant differences between cohorts, with a higher incidence of CVD in Finland, the USA and the Netherlands compared with the Southern European countries and Japan. The differences were not accounted for by other traditional risk factors, such as smoking, obesity or physical activity. However, when dietary aspects were analysed, the authors found a significant association between the consumption of mono- and polyunsaturated fats and a lower incidence of CVD, suggesting that Southern European dietary patterns, with a low intake of saturated fat and a high intake of fruits and vegetables, was a key factor in lower cardiovascular mortality [6]. The results of this study are the pillar that supports today’s growing evidence of the benefits associated with the so-called “Mediterranean Diet” (MD).
The north–south gradient with respect to CVD has been confirmed in several epidemiological studies, as evidenced by data from the MONICA Project (multinational monitoring of trends and determinants in cardiovascular disease) [7], which showed that Catalonia, the South of France and Italy had a lower incidence of mortality due to coronary heart disease (CHD) (in both men and women) than Northern European countries and the United States. Subsequently, numerous studies have shown the benefits of adherence to a “healthy diet” in reducing CVD. The results of the CARDIA study (Coronary Artery Risk Development in Young Adults) by Liu et al. [8] which was conducted in 3154 participants aged 18–30 years, underline the importance of maintaining a healthy lifestyle over a 20-year follow-up. In this study, adherence to a “healthy diet” increased the maintenance of a low cardiovascular risk profile (28.3 % for a healthy diet vs. 22.4 % for an unhealthy diet; P <0.01) on reaching adulthood, thus reducing, the likelihood of future CVD (Fig. 12.1).
Furthermore, the results of a systematic review by Mente et al. [9] on the effect of different dietary patterns on CHD, including prospective cohort studies and fewer randomized clinical trials (the latter only exploring effects of the Mediterranean diet) support the beneficial link between healthy dietary factors characterized by a high intake of vegetables, fruits, legumes, whole grains, fish and other seafood (healthy diet), a higher consumption of monounsaturated fatty acids (MUFA) and polyunsaturated fatty acids (PUFA) than saturated fatty acids, and reductions in CHD. More recently, a meta-analysis by Martinez-Gonzalez et al. [10] reinforced the beneficial effect of the MD, showing that a two-point increase in adherence to the MD (0–9 score) was associated with a significant reduction in cardiovascular events (pooled risk ratio: 0.87; 95 % CI: 0.85–0.90) with no evidence of heterogeneity between studies.
The strongest evidence for the benefits of the MD comes from the multicentre, randomized PREDIMED study in 4,774 patients at high cardiovascular risk. Patients were assigned to one of three arms of a dietary intervention: MD supplemented with extra-virgin olive oil (VOO), MD supplemented with nuts, or a control low fat diet. The study was halted prematurely at 4.8 years of follow up in accordance with data obtained in an interim analysis. The PREDIMED [11] study is the first randomized trial in primary prevention of CVD to show that the MD supplemented with VOO or nuts significantly reduced the incidence of major cardiovascular events, with a HR of 0.70 (95 % CI, 0.54–0.92) and 0.72 (95 % CI, 0.54–0.96), respectively.
Better understanding of the contribution of risk factors to the disease burden has motivated several comparative studies in the past few decades. Although these risk factor-specific or cause-specific analyses are useful for policy, a more comprehensive global assessment of the disease burden attributable to risk factors could strengthen the rationale for actions to reduce the disease burden and promote health. The latest review by Lim et al. [12] estimated global attributable mortality and disability adjusted life-years in 1990 and 2010 for each of the 67 risk factors and clusters of risk factors. In 2010, the three leading risk factors for the global disease burden were high blood pressure (7.0 %; 95 % CI 6.2–7.7), smoking, including second-hand smoke (6.3 %; 95 % CI 5.5–7.0), and dietary risk factors and physical inactivity (10.0 %; 95 % CI 9.2–10.8), with the most prominent dietary risks being diets low in fruit or high in sodium (Fig. 12.2).
Despite worldwide clinical and therapeutic efforts to improve BP control, it remains low and persists as a leading risk factor associated with cardiovascular mortality. The strong evidence on the effect of diet on CV disease has motivated the inclusion of specific dietary recommendations in all cardiovascular prevention guidelines, making diet and lifestyle a cornerstone in the reduction and prevention of CVD [13]. Lifestyle changes that have shown benefits in reducing BP values include reduction of body weight, low sodium intake, high potassium intake, reduction of excessive alcohol intake, and the DASH diet (Dietary Approaches to Stop Hypertension) [14, 15], which initially, potentiated increased consumption of fruits, vegetables and fatty dairy products, with a relatively low intake of total and saturated fat [16], although restrictions in sodium intake were later added in order to achieve greater reductions in BP values [17].
A total of 412 participants were randomly assigned to eat either a control diet (typical or usual diet in the United States) or the DASH diet. Within the assigned diet, participants ate foods with high, intermediate, and low levels of sodium for 30 consecutive days each, in random order. The three sodium levels were defined as high (a target of 150 mmol per day with an energy intake of 2,100 kcal, reflecting typical consumption in the USA), intermediate (a target of 100 mmol per day, reflecting the upper limit of current USA recommendations), and low (a target of 50 mmol per day, reflecting a level that might produce an additional lowering of blood pressure). Progressively-lower levels of sodium intake produced a greater BP response. In the control diet, a reduction in sodium intake of about 40 mmol per day from the intermediate sodium level lowered BP more than a similar reduction in sodium intake from the high level (P = 0.03 for systolic BP, P = 0.045 for diastolic BP). The DASH diet, as compared with the control diet, resulted in significantly-lower systolic BP (SBP) at every sodium level and in significantly-lower diastolic BP (DBP) at high and intermediate sodium levels (Fig. 12.3), with a larger effect on both SBP and DBP at high sodium levels than at low ones (P < 0.001 for the interaction).
Subsequently, the Optimal Macronutrient Intake Trial to Prevent Heart Disease (OmniHeart) evaluated the effect of a dietary intervention based on modifications of the DASH diet aimed at maximizing the hypotensive effect on BP in individuals with prehypertension or established hypertension. The results showed that, compared with a diet rich in carbohydrates, increased consumption of vegetable protein significantly reduced SBP by 1.4 mmHg (p = 0.002), with a reduction of 3.5 mmHg (p = 0.006) in subjects with hypertension, while a diet rich in unsaturated fat, with an increase in monounsaturated fatty acids (MUFA), was associated with a reduction in SBP of 1.3 mmHg (p = 0.005) in the overall cohort and 2.9 mmHg (p = 0.02) in hypertensives compared with the diet rich in carbohydrates [18].
In recent decades, the vasculoprotective potential of diet and nutrients has been increasingly recognized, with more solid evidence on the benefits of the MD emerging in recent years, although there is little data on its effect on BP reduction. Since the 1990s, evidence on the benefits of the MD in the prevention of CVD and the reduction of BP and cholesterol levels and/or diabetes has become stronger, although the level of evidence remains very heterogeneous. The MD is characterized by a diet rich in fruits, vegetables and cereals, with a high intake of mono- and polyunsaturated fats, and with olive oil being the main source of fat. Likewise, the MD encourages moderate fish and poultry consumption and a low consumption of dairy products, red meat, prepared meats and sweets and pastries. The MD also promotes moderate consumption of wine, preferably red, during meals [19].
Since the pioneering study by Keys et al. [5], data have been collected from more than 12 cross-sectional studies included in the ATTICA registry, which enrolled nearly 3,000 participants aged 18–89 years from the Greek region of Attica between 2001 and 2002. Overall, the studies showed that adherence to the MD is associated with a reduction in the incidence of diabetes, obesity, and CVD, and an improvement in the lipid profile and BP values. The data from two large cohort studies provide similar results: the Greek European Prospective Investigation into Cancer and Nutrition cohort (EPIC) and the Seguimiento Universidad de Navarra (SUN) study. The EPIC study now encompasses nearly half a million persons from 10 European countries and is the largest population-based cohort study focused on the beneficial effects of the MD on cardiovascular health. Substudies in Greece, Italy and Spain have found an inverse relationship between adherence to the MD and BP values, the BMI, the incidence of type-2 diabetes [20] and the tendency to obesity. More recent data from the Greek-EPIC cohort of 23,601 participants free of CVD showed that increasing adherence to the MD (determined by an increase of 2 points in the MD score) was inversely associated with the incidence of stroke (HR 0.85; 95 % CI 0.74–0.96), an association that was even stronger for women and for ischemic stroke vs. haemorrhagic stroke [21].
The SUN study of more than 15,000 Spanish university students without cardiovascular risk factors showed that adherence to the MD conditioned a lower incidence of metabolic syndrome (MetS) and type-2 diabetes, and a reduction in BP values [22]. Similar results were observed in the randomized, parallel Medi-RIVAGE study [23] which compared the effects of the MD in 180 patients with MetS compared with a control diet (carbohydrates 50–60 %, proteins 15–20 %, total fat <30 %). After 2 years follow up, patients assigned to the MD had a significant reduction in the prevalence of MetS and associated cardiovascular risk factors. Data from the first randomized study in secondary prevention, the Lyon Diet Heart Study [24], confirmed the benefits of the MD in reducing cardiovascular risk.
The cardioprotective role of the MD was confirmed in the meta-analysis by Sofi et al. [25]. Although evidence on the effects of the MD on BP has been scarce, probably because BP was usually a secondary outcome in nutritional studies, the preliminary results of the PREDIMED study [26] and the final results in the entire cohort [11] showed that adherence to the traditional MD significantly reduced the risk of cardiovascular disease. The risk reduction was highly significant for stroke, whose association with BP values is well established. Preliminary data from the PREDIMED study after the first 3 months of follow-up showed that, compared with the low-fat diet, the MD supplemented with VOO or nuts reduced office SBP by 5.9 mmHg (95 % CI: −8.7 to −3.1 mmHg) and 7.1 mmHg (95 % CI: −10.0 to −4.1 mmHg), respectively, and office DBP by 0.38 (95 % CI: −0.55 to−0.22) and 0.26 mmHg (95 % CI: −0.42 to −0.10), respectively [26]. However, in later results encompassing the whole PREDIMED cohort, the changes in office BP in 7,158 participants (mean age 67 years) were lower, although a trend to BP reduction was observed throughout the follow up [27]. The percentage of participants achieving good BP control increased significantly during the follow up in the three intervention groups, without between-group differences (31.9 % at baseline versus 41.3 % at study end; p <0.001). However, compared with patients assigned to the control diet, significantly-reduced DBP was observed in participants assigned to the MD supplemented with VOO (1.53 mmHg, 95 % CI: −2.01 to −1.04) and the MD supplemented with nuts (0.65 mmHg, 95 % CI: −1.15 to −0.15). No significant between-group differences in SBP were observed [27]. As the authors mention, a longer follow up, poor data with respect to changes in antihypertensive treatment during the study and a trend to greater adherence to the MD in the control group in the last years of follow-up may partly explain the differences in the results of long-term office BP. The other limitation was the technique for measuring office BP itself.
Prior studies of the effects of the MD on BP have relied on clinic (office) BP measurements, which are limited by poor reproducibility, the white-coat effect and observer and patient variability. Twenty-four hour ambulatory BP monitoring (ABPM) is considered the gold standard for the assessment of the effects of interventions on BP, as repeated measurements more accurately reflect usual BP than isolated office measurements.
The latest evidence of the beneficial effect of the MD on BP comes from the recent substudy of the PREDIMED study by Domenech et al. [28], which included 235 subjects (56.5 % female; mean age, 66.5 years) at high cardiovascular risk (85.4 % with hypertension). The results showed that the MD supplemented with either VOO or nuts directly resulted in significant reductions in 24-h ABPM compared with a control diet in individuals at high risk of CVD (85 % under hypertensive treatment), without considering the confounding effects of weight loss or changes in physical activity, sodium intake or alcohol consumption. The net differences between the MD supplemented with VOO and nuts and the control diet were −4.0 for mean systolic BP, −4.3 mmHg for mean diastolic ABPM, and −1.9 mmHg for both MD after adjustment for between-diet imbalances in baseline BP and for trial changes in antihypertensive medication (Fig. 12.4).
The impact of such BP changes, even if their magnitude seems small, could be remarkable at the population level. It has been estimated that a reduction of 3 mmHg in office systolic BP would reduce stroke mortality by 8 % and coronary heart disease mortality by 5 % [29].
The known limitations of office BP measurement versus 24-h ABPM, with repeated measurements during usual living conditions, apply to the results of the total PREDIMED sample. The advantages of 24-h ABPM are well-known [13], especially for non-pharmacologic interventions with expected smaller individual BP effects. Table 12.1 shows the control rates of hypertension, defined by standard cutoffs, which were dissimilar between the three intervention groups in the PREDIMED substudy according to both office BP and 24-h ABPM measurements. In all groups, office BP control was similar at baseline and after the intervention. However, 24-h and daytime ABPM control improved variably from baseline in the MD groups, whereas nighttime ABPM control worsened in the control group. BP control was always better with ABPM monitoring compared with office BP, with the differences ranging between 16 % and 42, which can be equated with white-coat hypertension in the office setting.
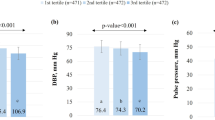
The proportion of participants with good BP control at both baseline and after 1 year of the intervention was similar in PREDIMED substudy and in the full PREDIIMED cohort [26], further supporting the differential added value of the ABPM results. The reduction in ABPM associated with the MD in different subgroups defined by sex, age, and cardiovascular risk factors were comparable with those of the whole group for SBP except for diabetic participants, in whom greater reductions with the MD versus the control diet were observed compared with participants without diabetes mellitus (P for interaction, 0.031), reinforcing the global effect of adding dietary interventions in high risk populations (Fig. 12.5).
In conclusion, there is robust evidence that increasing adherence to the MD is associated with lower BP. Taking into account the lack of BP control rates despite pharmacological treatment, these results could have public health implications because the MD, a vegetable and high-unsaturated fat based dietary pattern, seems to be a useful adjunct to established dietary and pharmacological approaches to improving hypertension control while incurring little or no expense for the health system.
References
Ford ES. Trends in mortality from all causes and cardiovascular disease among hypertensive and nonhypertensive adults in the United States. Circulation. 2011;123:1737–44.
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics – 2013 update – a report from the American Heart Association. Circulation. 2013;127:143–52.
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–44.
Banegas JR, Graciani A, de la Cruz-Troca JJ, León-Muñoz LM, Guallar-Castillón P, Coca A, et al. Achievement of cardiometabolic goals in aware hypertensive patients in Spain. A nationwide population-based study. Hypertension. 2012;60:898–905.
Keys A, et al. Coronary heart disease in seven countries. Circulation. 1970;41(Suppl I):1–211.
Menotti A, Keys A, Kromhout D, Nissinen A, Blackburn H, Fidanza F, et al. Twenty-five-year mortality from coronary heart disease and its prediction in five cohorts of middle-aged men in Finland, the Netherlands, and Italy. Prev Med. 1990;19:270–8.
Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial Infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612.
Liu K, Daviglus ML, Loria CM, Colangelo LA, Spring B, Moller AC, Donald M. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: the Coronary Artery Risk Development in (Young) Adults (CARDIA) Study. Circulation. 2012;125:996–1004.
Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659–69.
Martinez-Gonzalez MA, Bes-Rastrollo M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr Opin Lipidol. 2014;25:20–6.
Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, PREDIMED Study Investigators, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–90.
Lim SS, Voss T, Faxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). 2013 ESH/ESC Guidelines for the management of arterial hypertension. J Hypertens. 2013;31:1281–357.
Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006;47:296–308.
Sacks FM, Campos H. Dietary therapy in hypertension. N Engl J Med. 2010;362:2102–12.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure: DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–24.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller 3rd ER, Simons-Morton DG, Karanja N, Lin PH, DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10.
Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller 3rd ER, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, Charleston J, McCarron P, Bishop LM, OmniHeart Collaborative Research Group. Effects of protein, monounsatured fat, and carbohydrate intake on blood pressure and serum lipids. Results of the OmniHeart randomized trial. JAMA. 2005;294:2455–64.
Willett WC, Sacks F, Trichopoulou A, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(Suppl):1402S–6.
Rossi M, Turati F, Lagiou P, Trichopoulos D, Augustin LS, La Vecchia C, Trichopoulou A. Mediterranean diet and glycaemic load in relation to incidence of type 2 diabetes: results from the Greek cohort of the population-based European Prospective Investigation into Cancer and Nutrition (EPIC). Diabetologia. 2013;56:2405–13.
Misirli G, Benetou V, Lagiou P, Bamia C, Trichopoulos D, Trichopoulou A. Relation of the traditional Mediterranean diet to cerebrovascular disease in a Mediterranean population. Am J Epidemiol. 2012;176(12):1185–92.
Núñez-Córdoba JM, Valencia-Serrano F, Toledo E, Alonso A, Martínez-González MA. The Mediterranean diet and incidence of hypertension: the Seguimiento Universidad de Navarra (SUN) study. Am J Epidemiol. 2009;169:339–46.
Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, D’Armiento M, D’Andrea F, Giugliano D. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA. 2004;292(12):1440–6.
de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–85.
Sofi F, Abbate R, Gensini GF, et al. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and metaanalysis. Am J Clin Nutr. 2010;92:1189–96.
Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, on behalf of the PREDIMED Study Investigators, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med. 2006;145:1–11.
Toledo E, Hu FB, Estruch R, Buil-Cosiales P, Corella D, Salas-Salvadó J, on behalf of the PREDIMED Study Investigators, et al. Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: results from a randomized controlled trial. BMC Med. 2013;11:207.
Doménech M, Roman P, Lapetra J, García de la Corte FJ, Sala-Vila A, de la Torre R, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Lamuela-Raventós RM, Toledo E, Estruch R, Coca A, Ros E. Mediterranean diet reduces 24-hour ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension. 2014;64:69–76.
Stamler R. Implications of the INTERSALT study. Hypertension. 1991;17(1 Suppl):I16–20.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Domenech, M., Coca, A. (2016). The Role of Diet in the Prevention of Cardiovascular Disease. In: Andreadis, E. (eds) Hypertension and Cardiovascular Disease. Springer, Cham. https://doi.org/10.1007/978-3-319-39599-9_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-39599-9_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-39597-5
Online ISBN: 978-3-319-39599-9
eBook Packages: MedicineMedicine (R0)