Abstract
Background
The detection of small deep schwannomas of the peripheral nerves has been increasing since the the use of precise neuroimaging techniques has become more widespread; however, although nonpalpable lesions can be well defined by images, it is often difficult to identify them during the surgical procedure. The authors report seven cases of nonpalpable small deep schwannomas surgically treated after their identification using the radioguided occult lesion localization (ROLL) technique.
Methods
Seven men, whose ages ranged from 34 to 70 years (mean 52 years), presented with symptomatic nonpalpable peripheral nerve lesions; two cases involved the sciatic nerve, two the femoral nerve, two the radial nerve, and one the tibial nerve. Before the operation, all the patients were studied by ultrasonography and magnetic resonance imaging (MRI); 1 h before the surgery 3–5 MBq of 99mTc labeled with human albumin macroaggregates was injected into the lesion. A gamma detection probe permitted the preoperative and intraoperative detection of the nonpalpable schwannomas.
Conclusions
The ROLL technique provides good support for identifying small lesions of the peripheral nerves both preoperatively and intraoperatively. This technique permits the use of minimally invasive approaches performed with local anesthesia, with good cosmetic results and acceptance by the patients.
Access provided by CONRICYT-eBooks. Download conference paper PDF
Similar content being viewed by others
Keywords
Introduction
Schwannomas, also called neurilemmomas or peripheral neurinomas, are benign tumors arising from the perineurium of peripheral nerves [4]. The term neurinoma was coined in 1910 by Verocay to indicate a tumor that originated from Schwann cells and that was histologically different from a neurofibroma [9]. Schwannomas constitute 5 % of all benign soft-tissue tumors; men and women are equally affected, most frequently in their third decade of life [4, 6]. The most frequent localization is in the lower extremity, followed by upper extremity, dorsal roots, and retroperitoneum.
To determine the diagnosis of peripheral nerve neurinomas, magnetic resonance imaging (MRI) can clearly define the lesion's characteristics. The mass is usually isointense relative to skeletal muscles on T1-weighted images, and eccentric relative to the involved nerve that is displaced to the periphery; a capsule can be visualized; thus, the margins are well defined. On T2-weighted images the lesion is hyperintense. Schwannomas usually show enhancement after gadolinium injection [1, 3]. Clinically, these lesions can cause pain and motor or sensory deficits in the territory of the involved nerve [9]. On examination of the patient, a peripheral neurinoma can be visible and palpated as a round, well-defined mass that can be mobilized from side to side but not along the axis of the nerve [5]. Tinel’s sign is very often evocable over the mass [9]. Microsurgical excision with an interfascicular dissection technique is the most effective treatment, and complete recovery can be obtained; biopsies are no longer indicated [9].
The surgical strategy can be optimized by the use of radioguided occult lesion localization (ROLL). This technique was developed in 1997 by Paganelli et al. [8] to identify sentinel nodes in breast cancer and small nonpalpable lesions. Starting from these considerations, it was possible to extend the method to detect small nonpalpable lesions of the peripheral nerves.
Methods
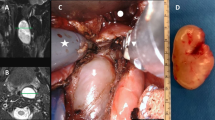
Seven patients with deep nonpalpable suspicious peripheral nerve schwannomas previously studied by ultrasound and MRI underwent surgical excision after the preoperative localization of the lesion by the ROLL technique (Table 1). The radiotracer used was 99mTc labeled with human albumin macroaggregates (99mTc MAA), with a diameter of 10–150 μm (TechneScan LyoMAA; Mallinckrodt Medical, Petten, The Netherlands). One hour before the surgery 3–5 MBq of 99mTc MAA in 0.2 ml of saline solution was injected into the lesion under ultrasound guidance (Fig. 1). The site was marked with a dermographic pen. Front and lateral images of the lesion were acquired with a gamma detection system Neoprobe (Dublin, Ohio, U.S.A.) and the patients were then brought to the operating room.
The patients underwent preoperative detection of the lesion, using a sterile gamma probe to identify the gamma rays emanating from the radioactive tracer injected into the neurinoma (Fig. 2).
Detection of the radiotracer, performed with a sterile probe. Precise localization of the lesion (case 1 in Table 1) was possible with a minimally invasive approach
The probe was connected to an instrument that analyzes the signals and transduces them into a digital scale together with acoustic signal. The intensity of the signal is directly proportional to the radioactivity detected and represent the relative distance of the probe to the lesion.
After the identification of the “hot spot”, the neurosurgeon performed a small tailored incision. During surgery the lesion’s positions were checked to guide their isolation. Using a microsurgical technique, the neurosurgeon dissected unaffected nerve fascicles from the tumor capsule and the lesions were then resected (Fig. 3).
Results
The diagnosis of peripheral Schwannoma was confirmed in all seven patients.
Complete removal of the lesion was performed in all cases and all patients presented with resolution of the pain. In one patient a preoperative motor deficit had been described (muscle strength 4/5 on the Medical Research Council [MRC] scale) and improvement was reported at 18-months follow up; of five patients who presented with preoperative sensory deficits, complete recovery had occurred in four patients at 10–18 months. All the treated patients were pain-free after the surgery (Table 1).
In six of the seven patients the surgical procedures were performed with local anesthesia.
Discussion
Small and deep lesions of the peripheral nerve can be identified in the early stages using new neuroimaging techniques. However, despite the excellent visualization of these lesions so provided, it is often difficult to find them during surgery, and invasive interventions can be necessary for their removal.
In this series, we used the ROLL technique – a well known method to localize sentinel nodes and small lesions in breast cancer – to detect small and deep peripheral nerve schwannomas preoperatively and during surgery.
The use of the ROLL technique to detect occult breast tumors was described by Paganelli et al. in 1997 [8], but this technique has not been reported previously for the detection of peripheral nerve schwannomas.
In a previous study, it was shown that there was no movement of the radiotracer from the lesion; thus, the radiotracer’s captation can be considered as a guide for the surgeon to identify occult lesions during operation [2]. Starting from these considerations, in our institution the ROLL technique was used for the first time for preoperatively and intraoperatively identifying deep and/or small peripheral nerve lesions, in seven patients.
One hour before the surgery, a radiotracer (99mTc MAA) was injected into the lesion under ultrasound guidance; image acquisition with a gamma camera was required and then the surgical excision was made. Using a sterile probe that detected the 99mTc MAA radiation, the lesion was localized, and consequently it was possible to plan a small incision for a minimally invasive surgical approach (Fig. 2). The surgical procedures were performed with local anesthesia in six of the seven patients. Thus, we conclude that the gamma detection system permits the easy identification of lesions in the superficial layers and also those in deep layers during surgery.
We have to report that the preoperative 99mTc MAA intralesional injection done under ultrasound guidance can be painful (four cases). Due to the short half-life of 99mTc, the procedure is safe for the patient, for the surgeon, and for the operating room personnel. The complete removal of the lesion injected with the radiotracer also removes the radioactivity from the patient’s body.
These results of a preliminary case series suggest that the ROLL technique is safe and could be used for the removal of multiple deep peripheral nerve schwannomas during the same surgical procedure. We note that the surgeon can manage the sterile probe by himself/herself in order to localize the lesion during open surgery.
This ROLL technique requires interdisciplinary cooperation, but it provides good support for preoperatively and intraoperatively identifying small lesions of the peripheral nerves. It permits a minimally invasive approach, performed with local anesthesia, with a shorter operative time, and minor costs, together with good cosmetic results and better patient acceptance.
References
Beaman FD, Kransdorf MF, Menke DM (2004) Schwannoma: radiologic-pathologic correlation. RadioGraphics 24:1481–1497
De Cicco C, Cremonesi M, Luini A, Bartolomei M, Grana C, Prisco G, Galimberti V, Calza P, Viale G, Veronesi U, Paganelli G (1998) Lymphoscintigraphy and radioguided biopsy of the sentinel axillary node in breast cancer. J Nucl Med 39:2080–2084
Hems TE, Burge PD, Wilson DJ (1999) The role of magnetic resonance imaging in the management of peripheral nerve tumours. J Hand Surg [Br] 22:57–60
Lee JA, Boles CA (2004) Peripheral Schwannoma lacking enhancement on MRI. Am J Roentgenol 182:534–535
Lewis D, Hart D (1930) Tumors of peripheral nerves. Ann Surg 92:961–983
Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT (1999) From the archives of the AFIP Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiodraphics 19:1253–1280
Oberle J, Kahamba J, Richter HP (1997) Peripheral nerve Schwannomas – an analysis of 16 patients. Acta Neurochir 139:949–953
Paganelli G, De Cicco C, Luini A (1997) Radioguided surgery in non-palpable breast lesions. Eur J Nucl Med 24 (Suppl):893
Paganelli G, Luini A, Veronesi U (2002) Radioguided occult lesion localization (ROLL) in breast cancer: maximizing efficacy, minimizing mutilation. Ann Oncol 13:1839–1840
Conflict of Interest Statement
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this paper
Cite this paper
Stevanato, G. et al. (2017). Radioguided Occult Lesion Localization in Deep Schwannomas of the Peripheral Nerves: Results of a Preliminary Case Series. In: Visocchi, M., Mehdorn, H.M., Katayama, Y., von Wild, K.R.H. (eds) Trends in Reconstructive Neurosurgery. Acta Neurochirurgica Supplement, vol 124. Springer, Cham. https://doi.org/10.1007/978-3-319-39546-3_46
Download citation
DOI: https://doi.org/10.1007/978-3-319-39546-3_46
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-39545-6
Online ISBN: 978-3-319-39546-3
eBook Packages: MedicineMedicine (R0)