Abstract
Minimally invasive spine surgery (MISS), including percutaneous pedicle-screw fixation (PPSF), mini-open transforaminal lumbar interbody fusion (m-open TLIF), vertebroplasty, and stentoplasty, allows the preservation of neurological function and the restoration of spine stability, while reducing associated risks and complications. This study aimed to analyze the safety and efficacy of MISS in elderly patients suffering from degenerative or traumatic thoracolumbar diseases. Forty-five patients (28 females), with a mean age of 73 years (range 65–89), suffering from osteoporotic vertebral fractures (24), degenerative spondylolisthesis (15), and lumbar canal stenosis with instability and/or de novo scoliosis (6) were included.
Twenty-one patients underwent PPSF and m-open TLIF. The remaining patients received PPSF without interbody fusion, and in six of these fenestrated screws were used for vertebral body cement augmentation.
Functional evaluation was obtained with a visual analog scale (VAS) and the Oswestry Disability Index (ODI) pre- and postoperatively. Preoperative imaging included X-rays, computed tomography (CT), and magnetic resonance imaging (MRI). Patients were followed-up with X-rays, and a CT scan was also obtained at the last follow-up. Follow-up ranged from 6 to 59 months (mean 28 months). Follow-up CT scan documented intersomatic fusion in only 14 % of patients treated with m-open TLIF. Despite the high incidence of non-union, mean VAS and ODI scores showed a significant improvement, with a reduction of mean VAS from 9 to 4 and a reduction of mean ODI from 76.33 to 38.15 %. Only three patients developed postoperative complications. No patients showed neurological deficits.
Minimally invasive spine surgery for degenerative and traumatic spinal diseases is a safe and effective treatment also in elderly patients.
Access provided by CONRICYT-eBooks. Download conference paper PDF
Similar content being viewed by others
Keywords
- Oswestry Disability Index
- Degenerative Spondylolisthesis
- Osteoporotic Vertebral Fracture
- Spinal Canal Stenosis
- Oswestry Disability Index Score
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Spinal canal stenosis, degenerative spondylolisthesis, and vertebral body fractures represent major causes of morbidity in patients aged ≥65 years, needing rapid and effective treatment to achieve preservation of neurological function and restoration of spinal stability [1].
A growing body of studies suggests that in the adult population minimally invasive spine surgery (MISS) is a safe and feasible treatment option for degenerative and traumatic thoracolumbar spine diseases, avoiding or reducing postsurgical complications and improving early postoperative clinical outcome [2–4]. Recently, MISS has also been proposed for deformity surgery, with the intended goal of reducing the morbidity linked to open surgery [5–7]. When open surgery is chosen, the patient’s age is an important factor to consider. Elderly age, i.e., ≥ 65 years, is not always a contraindication for open surgery, but it can be an added risk factor; indeed, older patients are more prone to suffer from several medical comorbidities, including osteoporosis. And these conditions might consistently increase the risks associated with open surgery. In such a scenario, MISS might be a safe and effective alternative treatment modality [8–11]. Recent technical innovations, such as fenestrated pedicle screws [12] and expandable screws [13], have further expanded the feasibility of MISS fixations also in the elderly population.
This study analyses the prospectively collected clinical, functional, and radiological data of elderly patients treated with MISS for degenerative and traumatic thoracolumbar pathologies.
Patients and Methods
Forty-five patients (17 males, 28 females), with a mean age of 73 years (range 65–89), suffering from degenerative spondylolisthesis (15), lumbar canal stenosis with instability and/or de novo scoliosis (6), and traumatic osteoporotic vertebral fractures (24) were prospectively enrolled. Forty patients were treated at the Department of Neurological Surgery, Policlinico “G. Rodolico” University Hospital, Catania, Italy, and 5 patients were treated at the Department of Spine Surgery, Al-Razi Hospital, Kuwait.
Preoperatively, clinical and functional outcomes were measured with a visual analog scale (VAS) and the Oswestry Disability Index (ODI). The same outcome measures were then used at 1, 3, 6, and 12 months after the index procedure and yearly thereafter. Imaging included X-rays, with flexion/extension views, magnetic resonance imaging (MRI), and computed tomography (CT).
Because of the patients’ age, thorough and accurate clinical evaluation (cardiovascular and respiratory functions, blood tests, nutritional status) was performed before surgery to rule out comorbidities. Osteoporosis was not routinely investigated before surgery, as we assumed it to be widespread among elderly people. When a likely osteoporotic condition was suggested during surgery by a reduced device grip, we opted for cement augmented or expandable screws.
In 21 patients a MISS pedicle-screw fixation with mini-open transforaminal lumbar interbody fusion (m-open TLIF) was performed (14 single-level, 5 two-level, and 2 three-level cases). Of the remaining 24 patients treated with MISS, 18 underwent percutaneous pedicle-screw fixation (PPSF) with or without vertebral body cement augmentation (Confidence Spinal Cement; DePuy Spine,) and 6 underwent vertebroplasty or kyphoplasty.
The Viper percutaneous pedicle-screw fixation system with fenestrated screws (DePuy Spine Raynham, US) or the Illico percutaneous fixation system (Alphatec Spine Carlsbad, US, US) with expandable screws (Osseoscrew; Alphatec Spine Carlsbad, US) was used.
We performed m-open TLIF on the most symptomatic side, where the most severe spinal canal stenosis or neural structure compressionwas present. Either carbon fiber cages or polyether ether ketone (PEEK) cages were used. In patients with m-open TLIF a microsurgical unilateral facetectomy and hemilaminectomy was performed; the base of the spinous process was trimmed off, and the contralateral ligamentum flavum removed. Such maneuvers, together with a contralateral surgical table inclination [14], allowed us to recalibrate and enlarge the spinal canal and decompress the neural structures (Figs. 1 and 2).
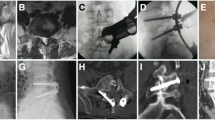
Illustrative case. Minimally invasive surgical treatment of multilevel lumbar canal stenosis with L4-L5 instability is shown. A 77-year-old woman suffering from left sciatica and neurogenic claudication underwent spine magnetic resonance imaging (MRI), documenting lumbar canal stenosis (a) with severe bilateral foraminal stenosis at L3-L4 (b) and L4-L5 (c) levels. Anteroposterior (d), lateral (e), and flexion/extension (f, g) X-rays showed L4-L5 instability with slight L3-L4 and L4-L5 spondylolisthesis. The patient underwent L2-L5 fixation with percutaneous screws and left-sided mini-open transforaminal lumbar interbody fusion (TLIF) at L4-L5 (h). Cannulated screws at L4 and L5 allowed cement augmentation (i). Postoperative X-rays documented correct device positioning (j, k)
Results
Follow-up ranged from 6 to 59 months, with a mean of 28 months.
VAS and ODI scores showed significant postoperative improvements; in particular, the mean VAS score decreased from 9 to 4 and the mean ODI score decreased from 76.33 to 38.15 %.
Three of the 45 patients (6.7 %) developed the following postoperative complications: spondylodiscitis (1), screw dislocation (1) (Fig. 3), and cage dislocation (1). No patients showed postoperative neurological deficits or any age-related or device-related complications.
Th12-L3 fixation performed in a 72-year-old woman for surgical treatment of L2 burst fracture, previously treated elsewhere with percutaneous cement injection (a, b). X-rays performed 3 weeks after the procedure documented the pull-out of L3 screws (c). Replacement and augmentation of the L3 screws was performed, together with caudal extension of instrumentation (d)
Solid intersomatic fusion was observed in 3 of the 21 (14 %) patients who had undergone m-open TLIF. Evaluation of intersomatic fusion was performed using multiplanar reconstructed CT scans at follow-up visits.
Discussion
Surgery in the elderly population is still a debatable issue. Boundaries between overtreatment and standard of care are often undefined and unclear; therefore, surgeons and anesthesiologists should evaluate surgical indications, as well as predict the complications, to balance the risks and benefits for patients [15]. Decision-making in the surgical management of elderly patients also has to consider the role of frailty and disability, aiming to obtain the best results with minimal risks for the delicate general homeostasis of the aging population.
Minimally invasive techniques applied to spinal surgery have gained appeal over the past decade, as they have demonstrated good clinical outcomes and low complication rates along with the well-known advantages of low invasiveness [4, 16, 17]. Currently, various spinal diseases (degenerative, neoplastic, or traumatic) may be approached using MISS techniques, with reduced blood loss, limited muscular dissection, better control of postoperative pain, and decreased hospitalization time [18]. To state the philosophy of MISS: elderly patients should be considered ideal candidates for spine surgery using less invasive techniques. Advances in MISS devices and techniques have led to an overall increase of surgical procedures in elderly patients, as demonstrated by the growing number of recently published reports on this topic [19–21].
In 2008, Lee et al. analyzed the clinical and radiological outcomes of 27 patients, aged over 65 years old, who underwent single-level m-open TLIF as surgical treatment for degenerative spondylolisthesis [19]. They documented a high fusion rate (77.8 %), good spinal realignment (improved segmental lordosis in all patients), and a low complication rate. However, a possible inclusion bias in their series could be related to the patients’ American Society of Anesthesiologists (ASA) grading, with a score ranging between 1 and 2 in all enrolled patients.
In 2011, Drazin et al. reviewed clinical data from the literature on complications and outcomes after spinal deformity surgery in patients over60 years old [7]. Interestingly, they supported the application of minimally invasive techniques in order to reduce the complication rate, encouraging future studies in this direction. A further review published in 2014 [22] highlighted the scant number of adequate clinical studies on this topic, pointing out the importance of CT scans for the thorough evaluation of fusion rates. Indeed, most of the published studies, including the previously cited one by Lee et al. [19], did not use CT scans in radiological follow-up.
A recent review of the existing literature on MISS in elderly patients [20] revealed a good clinical outcome with an acceptable complication rate, albeit that all the published studies reviewed had low-quality evidence, based on retrospective series. The authors concluded that symptomatic elderly patients may benefit from MISS techniques and they should not be excluded from surgery.
We have reported our experience with minimally invasive techniques in the surgical treatment of different spinal pathologies in a consecutive cohort of patients aged over 65 years old. Differently from Lee’s series, we included patients regardless of their ASA score or surgical techniques, aiming to observe the impact of MISS in improving clinical outcome and allowing a rapid recovery. Early patient mobilization and short hospitalization have been considered primary goals, and surgical indications have been advised accordingly. We included in this series 20 patients suffering from traumatic and osteoporotic vertebral fractures. In this subgroup, minimally invasive techniques (PPSF with or without cement augmentation or expandable screws, or simple vertebro/kyphoplasty) ensured rapid recovery from symptoms, with unequivocal clinical advantages, as documented by a reduction of the VAS score from 9.3 to 3.2 (considering only patients with vertebral fractures). In this subgroup, we observed only one case of screw displacement, requiring revision surgery. Moreover, we combined PPSF and cement augmentation of the fractured vertebral body in 5 of these 20 patients, following the positive clinical experience with such a technique reported by Gu et al. [21]. Short-segment percutaneous fixation has been proposed as a viable alternative to open posterolateral fusion in patients with thoracolumbar burst fractures [23, 24]; in our series, short fixation with expandable or fenestrated screws for cement augmentation and short screws in the pedicles of fractured vertebrae were used in 8 of 24 patients, whereas 10 patients underwent percutaneous fixation with screws placed two levels above and two levels below the fractured vertebra.
The surgery-related complication rate was definitely low in our cohort. The application of our previously reported surgical technique [4] for m-open TLIF increased the safety of the procedure, reducing the risks of dural and/or neural lesions. Interestingly, the incidence of inhadvertent dural lesions during MISS in an elderly population was reported as 5 % in the review by Shamji et al. [20], whereas in our experience it was 0 %.
Despite the clinical parameters in our series showing a good or excellent outcome, our fusion rate, assessed by CT scan, in the subgroup of patients treated with m-open TLIF was low (14 %). Nonunion after MISS has been suggested as a possible weakness of such a procedure, particularly in patients with low-quality bone [8, 19]. However, in our series, pseudoarthrosis was never associated with poor clinical outcome and no device-related complications, such as dislocations, were observed. We think that this low fusion rate may also be due to the technique used to assess fusion. Indeed, X-rays may overestimate the fusion rate in patients with interbody devices, whereas CT scans offer a more accurate evaluation of intersomatic fusion.
On analyzing our results, we felt that complications could be reduced and predicted with a thorough presurgical evaluation, including assessment of osteoporosis and comprehensive medical management. Although we did not perform routine evaluation of osteoporosis and relied on intraoperative data only, we acknowledge that in elderly patients a preoperative osteoporosis assessment is advisable.
Finally, the patient’s age was not a contraindication for instrumented MISS in our series, but tailored clinical evaluation and appropriate choice of a suitable device guided our indication, to achieve the best clinical results. Pseudoarthrosis did not correlate with poor clinical or functional outcome. When patients are carefully selected, MISS may be the best surgical strategy to obtain pain relief and improvement of myeloradicular signs and symptoms, as well as spinal stability.
Clinical trials with long-term follow-up should be designed to demonstrate the real impact of MISS in the management of degenerative or traumatic spinal diseases in elderly patients.
References
Whitehouse MK, Jeyaretna DS, Wright A, Whitfield PC (2015) Neurosurgical care in the elderly: increasing demands necessitate future healthcare planning. World Neurosurg. doi: 10.1016/j.wneu.2015.10.099 [Epub ahead of print]
Barbagallo GM, Certo F, Sciacca G, Albanese V (2013) Bilateral tubular minimally invasive approach for decompression, reduction and fixation in lumbosacral lythic spondylolisthesis. Neurosurg Focus 35(2 Suppl):Video 9
Barbagallo GM, Piccini M, Alobaid A, Al-Mutair A, Albanese V, Certo F (2014) Bilateral tubular minimally invasive surgery for low-dysplastic lumbosacral lytic spondylolisthesis (LDLLS): analysis of a series focusing on postoperative sagittal balance and review of the literature. Eur Spine J 23 Suppl 6:705–713
Barbagallo GM, Certo F, Visocchi M, Sciacca G, Piccini M, Albanese V (2015) Multilevel mini-open TLIFs and percutaneous pedicle screw fixation: description of a simple technical nuance used to increase intraoperative safety and improve workflow. Tips and tricks and review of the literature. Neurosurg Rev 38:343–354
Deukmedjian AR, Ahmadian A, Bach K, Zouzias A, Uribe JS (2013) Minimally invasive lateral approach for adult degenerative scoliosis: lessons learned. Neurosurg Focus 35(2):E4
Park P, Wang MY, Lafage V, Nguyen S, Ziewacz J, Okonkwo DO, Uribe JS, Eastlack RK, Anand N, Haque R, Fessler RG, Kanter AS, Deviren V, La Marca F, Smith JS, Shaffrey CI, Mundis GM Jr, Mummaneni PV, International Spine Study Group (2015) Comparison of two minimally invasive surgery strategies to treat adult spinal deformity. J Neurosurg Spine 22(4):374–380
Drazin D, Shirzadi A, Rosner J, Eboli P, Safee M, Baron EM, Liu JC, Acosta FL Jr (2011) Complications and outcomes after spinal deformity surgery in the elderly: review of the existing literature and future directions. Neurosurg Focus 31(4):E3
Rosen DS, O’Toole JE, Eichholz KM, Hrubes M, Huo D, Sandhu FA, Fessler RG (2007) Minimally invasive lumbar spinal decompression in the elderly: outcomes of 50 patients aged 75 years and older. Neurosurgery 60(3):503–510
Acosta FL Jr, McClendon J Jr, O’Shaughnessy BA, Koller H, Neal CJ, Meier O, Ames CP, Koski TR, Ondra SL (2011) Morbidity and mortality after spinal deformity surgery in patients 75 years and older: complications and predictive factors. J Neurosurg Spine 15:667–674
Lee JH, Chun HJ, Yi HJ, Bak KH, Ko Y, Lee YK (2012) Perioperative risk factors related to lumbar spine fusion surgery in Korean geriatric patients. J Korean Neurosurg Soc 51:350–358
Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH (2007) Adult spinal deformity surgery. Complications and outcomes in patients over Age 60. Spine 32(20):2230–2244
Pesenti S, Blondel B, Peltier E, Adetchessi T, Dufour H, Fuentes S (2014) Percutaneous cement-augmented screws fixation in the fractures of the aging spine: is it the solution? Biomed Res Int 2014:610675
Vishnubhotla S, McGarry WB, Mahar AT, Gelb DE (2011) A titanium expandable pedicle screw improves initial pullout strength as compared with standard pedicle screws. Spine J 11(8):777–781
Schonauer C, Bocchetti A, Barbagallo G, Albanese V, Moraci A (2004) Positioning on surgical table. Eur Spine J. 13 Suppl 1:S50–55
Murthy S, Hepner DL, Cooper Z, Bader AM, Neuman MD (2015) Controversies in anaesthesia for noncardiac surgery in older adults. Br J Anaesth 115(Suppl 2):15–25
Holly LT, Schwender JD, Rouben DP, Foley KT (2006) Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus 20(3):E6
Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J (2010) Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J 19:1780–1784
Khan NR, Clark AJ, Lee SL, Venable GT, Rossi NB, Foley KT (2015) Surgical outcomes for minimally invasive vs open transforaminal lumbar interbody fusion: an updated systematic review and meta-analysis. Neurosurgery 77(6):847–874
Lee DY, Jung TG, Lee SH (2008) Single-level instrumented mini-open transforaminal lumbar interbody fusion in elderly patients. J Neurosurg Spine 9(2):137–144
Shamji MF, Goldstein CL, Wang M, Uribe JS, Fehlings MG (2015) Minimally invasive spinal surgery in the elderly: does It make sense? Neurosurgery 77(Suppl 4):S108–415
Gu Y, Zhang F, Jiang X, Jia L, McGuire R (2013) Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty in the surgical treatment of thoracolumbar osteoporosis fracture. J Neurosurg Spine 18:634–640
Bach K, Ahmadian A, Deukmedjian A, Uribe JS (2014) Minimally invasive surgical techniques in adult degenerative spinal deformity: a systematic review. Clin Orthop Relat Res 472(6):1749–1761
Lee JK, Jang JW, Kim TW, Kim TS, Kim SH, Moon SJ (2013) Percutaneous short-segment pedicle screw placement without fusion in the treatment of thoracolumbar burst fractures: is it effective?: comparative study with open short-segment pedicle screw fixation with posterolateral fusion. Acta Neurochir 155:2305–2312
Van Middendorp JJ, Barbagallo G, Schuetz M, Hosman AJF (2012) Design and rationale of a Prospective, Observational European Multicenter study on the efficacy of acute surgical decompression after traumatic Spinal Cord Injury: the SCI-POEM study. Spinal Cord. 50(9):686–694
Conflict of Interest Statement
We declare that we have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this paper
Cite this paper
Barbagallo, G.M.V. et al. (2017). Restoration of Thoracolumbar Spine Stability and Alignment in Elderly Patients Using Minimally Invasive Spine Surgery (MISS). A Safe and Feasible Option in Degenerative and Traumatic Spine Diseases. In: Visocchi, M., Mehdorn, H.M., Katayama, Y., von Wild, K.R.H. (eds) Trends in Reconstructive Neurosurgery. Acta Neurochirurgica Supplement, vol 124. Springer, Cham. https://doi.org/10.1007/978-3-319-39546-3_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-39546-3_11
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-39545-6
Online ISBN: 978-3-319-39546-3
eBook Packages: MedicineMedicine (R0)