Abstract
Congenital anomalies of the kidney and urinary tract (CAKUT) cover a wide range of structural malformations that result from defects in the morphogenesis of the kidney and/or urinary tract (see also chapter “Congenital Anomalies of the Renal Pelvis and Ureter”). CAKUT occur in approximately 1:500 live-born fetuses and are the most common cause of chronic kidney disease in children worldwide (Renkema et al. 2011; Vivante et al. 2014). Congenital anomalies of the kidney include renal agenesis, renal hypo-/dysplasia with or without cysts, and multicystic dysplastic kidneys (Weber 2012). While most CAKUT cases are sporadic, renal abnormalities are found in close relatives in approximately 10 % of cases (Winyard and Chitty 2008). Although CAKUT typically occur as isolated malformations, they occasionally develop in association with additional congenital anomalies outside the urinary tract, such as in the renal coloboma syndrome or the renal cysts and diabetes syndrome; they may also be associated with cardiac malformations. Currently, more than 20 monogenic CAKUT-causing genes have been identified, and recent findings suggest that CAKUT may arise from a multitude of different single-gene causes (Vivante et al. 2014). The malformation phenotypes vary from normally appearing kidneys with preserved renal function (i.e., incomplete penetrance) to severe hypo-/dysplasia and end-stage renal disease. Features linked to worse prognosis are (1) bilateral disease, (2) decreased functional mass (which encompasses not just small kidneys but also large ones where cysts replace normal architecture), (3) lower urinary tract obstruction, and (4) anhydramnios or severe oligohydramnios (Winyard and Chitty 2008). Current management of CAKUT includes observation, surgical interventions, prophylaxis and treatment of urinary tract infections, strict blood pressure control, supplements for renal support, and nephroprotective treatment to slower the progression of chronic kidney disease.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Congenital Anomalies Of The Kidney And Urinary Tract (CAKUT)
- Renal Coloboma Syndrome
- Multicystic Dysplastic Kidney (MCDK)
- Simple Renal Cysts
- Autosomal Recessive Polycystic Kidney Disease (ARPKD)
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Congenital anomalies of the kidney and urinary tract (CAKUT) cover a wide range of structural malformations that result from defects in the morphogenesis of the kidney and/or urinary tract (see also chapter “Congenital Anomalies of the Renal Pelvis and Ureter”). CAKUT occur in approximately 1:500 live-born fetuses and are the most common cause of chronic kidney disease in children worldwide (Renkema et al. 2011; Vivante et al. 2014). Congenital anomalies of the kidney include renal agenesis, renal hypo-/dysplasia with or without cysts, and multicystic dysplastic kidneys (Weber 2012). While most CAKUT cases are sporadic, renal abnormalities are found in close relatives in approximately 10 % of cases (Winyard and Chitty 2008). Although CAKUT typically occur as isolated malformations, they occasionally develop in association with additional congenital anomalies outside the urinary tract, such as in the renal coloboma syndrome or the renal cysts and diabetes syndrome; they may also be associated with cardiac malformations. Currently, more than 20 monogenic CAKUT-causing genes have been identified, and recent findings suggest that CAKUT may arise from a multitude of different single-gene causes (Vivante et al. 2014). The malformation phenotypes vary from normally appearing kidneys with preserved renal function (i.e., incomplete penetrance) to severe hypo-/dysplasia and end-stage renal disease. Features linked to worse prognosis are (1) bilateral disease, (2) decreased functional mass (which encompasses not just small kidneys but also large ones where cysts replace normal architecture), (3) lower urinary tract obstruction, and (4) anhydramnios or severe oligohydramnios (Winyard and Chitty 2008). Current management of CAKUT includes observation, surgical interventions, prophylaxis and treatment of urinary tract infections, strict blood pressure control, supplements for renal support, and nephroprotective treatment to slower the progression of chronic kidney disease.
Renal cysts are clinically and genetically heterogeneous conditions. Inherited cystic kidney disorders mainly include polycystic kidney diseases and entities comprising the nephronophthisis and medullary cystic kidney disease complex. These diseases are now categorized as ciliopathies – a disease concept characterized by dysfunction of the primary cilium, a hairlike cellular organelle (Hildebrandt et al. 2011). Cilia sense a wide variety of extracellular signals and transduce them into decisions regarding proliferation, polarity, nerve growth, differentiation, or tissue maintenance (Goetz and Anderson 2010). Since cilia are expressed in variable tissues, ciliopathies may affect multiple organs, and numerous pleiotropic human disorders have been attributed to defective cilia formation. It has become increasingly evident that many ciliopathies have a renal cystogenic component, making kidney cyst formation a hallmark feature of ciliopathies (Bergmann 2012). Renal dysplasia may as well occur as a result of defective differentiation during kidney development. Notably, cystic kidneys and renal dysplasia are important features of numerous genetic syndromes, such as the mainly recessively inherited ciliopathies Bardet-Biedl, Joubert, Meckel, and Jeune syndromes or the dominant disorders of tuberous sclerosis, von Hippel-Lindau disease, and branchio-oto-renal syndrome (Bergmann 2015). At present, treatment of ciliopathies still remains symptomatic. Several medications are being investigated that might influence ciliary function and, for example, also may delay cyst formation and growth in the kidneys or will reduce the future extrarenal disease burden.
Details on imaging appearance and typical findings can be found in chapter “Imaging in Renal Agenesis, Dysplasia, Hypoplasia, and Cystic Diseases of the Kidney” which addresses all aspects of imaging including the respective imaging modalities, particularly focusing on ultrasonography (US) which is the most commonly used and often diagnostically sufficient modality in these entities.
Take Away
Congenital anomalies of the kidney are part of the CAKUT spectrum. Renal ciliopathies are frequently characterized by renal cyst formation; imaging heavily relies on US and is essential for initial evaluation and follow-up.
2 Renal Agenesis
Unilateral renal agenesis is characterized by the one-sided absence of renal tissue resulting from failure of embryonic kidney development (Woolf and Hillman 2007). The general incidence of unilateral renal agenesis has been estimated to be 1 in 2,000 (Westland et al. 2013). Renal agenesis occurs when the ureteric bud fails to form the ureter, renal pelvis, and renal mesenchyma that are necessary for the development of nephrons (Kerecuk et al. 2008). In these patients one frequently finds no ipsilateral ureter, as well as associated aplasia, hypoplasia, or anomalies of genital structures originating from the ipsilateral Wolffian and Mullerian ducts. Associated CAKUT have been identified in ~32 % of unilateral renal agenesis patients, the most common being vesicoureteric reflux (VUR) (24 %) (Westland et al. 2013). Extrarenal anomalies involving the gastrointestinal tract, heart, or musculoskeletal system were reported in 31 % of patients. Injury of the solitary functioning kidney may lead to hypertension, microalbuminuria, and/or a decrease in glomerular filtration rate. Therefore, these patients need nephrological long-term follow-up, particularly in the absence of compensatory hypertrophy of the solitary kidney.
Bilateral renal agenesis occurs in 1 of 3,000 pregnancies and is considered almost uniformly fatal (Woodward et al. 2011). Affected fetuses die in utero from cord compression, or newborns die within hours after birth from severe pulmonary hypoplasia due to anhydramnios.
Take Away
In unilateral renal agenesis, sonographic evaluation and monitoring of the contralateral kidney are obligatory.
3 Renal Dysplasia and Hypoplasia
Dysplastic kidneys are abnormally developed kidneys with poorly branched or differentiated nephrons and collecting ducts, increased stroma, and, occasionally, cysts and metaplastic tissues, such as cartilage (Woolf et al. 2004). Dysplastic kidneys range in size from large distended kidneys with multiple large cysts to small kidneys with or without cysts (Rosenblum and Salomon 2008). They are common malformations affecting up to 1 in 1,000 of the general population and comprise part of the spectrum of CAKUT (Ichikawa et al. 2002). Renal dysplasia may be the only CAKUT manifestation or be associated with hydronephrosis, UPJO, megaureter, ureter duplex, VUR, and posterior urethral valve (Schedl 2007). Simple renal hypoplasia is defined as a small kidney with a reduced number of nephrons but maintained normal architecture. However, dysplastic features can be detected in most of these kidneys histologically as well (Watkins et al. 1997). As a consequence, a small kidney without cysts but with sonographical signs of dysplasia is often clinically referred to as a hypo-dysplastic kidney.
Apart from isolated cases of CAKUT, combined malformations with various extrarenal manifestations have been observed. More than 500 syndromes involving CAKUT have been described as yet (Weber 2012) (see also chapter “Genetics in Nephrourology”). However, until recently, only a little more than 20 monogenic CAKUT-causing genes have been identified (Vivante et al. 2014). Among them, autosomal dominant mutations in HNF1ß (renal cysts and diabetes syndrome), PAX2 (renal coloboma syndrome) and EYA1 (branchio-oto-renal syndrome) are the most important (Weber et al. 2006). Renal cysts and diabetes syndrome may include renal dysplasia, diabetes mellitus, hyperuricemia, hypomagnesemia, elevated liver function tests, and malformations of female internal genitalia (Ulinski et al. 2006; Adalat et al. 2009). Renal coloboma syndrome is characterized by coloboma of the optic nerve and renal dysplasia with/without VUR (Sanyanusin et al. 1995). Branchio-oto-renal syndrome is genetically heterogeneous and comprises variable combinations of anomalies of the kidneys, brachial arches (cysts or fistulae), and external and inner ear (deafness) (Chang et al. 2004).
Take Away
Nowadays, renal hypo dysplasia is mostly detected by fetal or postnatal US. Imaging of associated anomalies of the urinary tract as well as potential extrarenal malformations is important for a correct diagnosis as well as for adequate therapeutic decisions and follow-up.
4 Cystic Kidney Disease
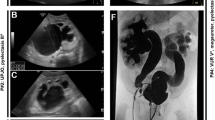
4.1 Autosomal Recessive Polycystic Kidney Disease (ARPKD)
ARPKD is a recessively inherited ciliopathy caused by mutations of the polycystic kidney and hepatic disease 1 gene (Bergmann et al. 2003). The incidence is approximately 1 in 20,000 live births. Its principal manifestations are polycystic kidney disease and congenital hepatic fibrosis (Bergmann et al. 2005).
The majority of patients are severely affected and ARPKD is frequently detected in late pregnancy or at birth. Fetuses with ARPKD display massively enlarged kidneys and oligohydramnios due to fetal renal failure (see also chapter “Urogenital Fetal Imaging: US and MRI”). Approximately 30–50 % of affected neonates die shortly after birth from respiratory failure due to pulmonary hypoplasia and thoracic compression by the excessively enlarged kidneys. Those surviving the neonatal period frequently take a prolonged course and may develop end-stage renal failure in the second decade of life (Guay-Woodford and Desmond 2003). Moderately affected patients without perinatal manifestation may even enter adulthood with preserved renal function (Adeva et al. 2006).
While the early presentation of ARPKD is clearly dominated by renal disease and early-onset hypertension, liver disease with congenital hepatic fibrosis and biliary duct ectasia is also present in every ARPKD patient. The hepatobiliary complications may also dominate the clinical picture, particularly in older patients. Progressive hepatic fibrosis leads to portal hypertension causing hypersplenism with pancytopenia as well as esophageal varices with bleeding complications. ARPDK patients with extensive dilatations of intra- and extrahepatic bile ducts (Caroli’s disease) are also at risk of ascending bacterial cholangitis (Kashtan et al. 1999).
Take Away
In ARPKD imaging should always include monitoring of congenital hepatic fibrosis and its potential complications.
4.2 Autosomal Dominant Polycystic Kidney Disease (ADPKD)
ADPKD is the most frequent life-threatening genetic disease (prevalence 1/500–1/1,000 live births) affecting approximately 12.5 million individuals worldwide (Harris and Torres 2009). About 50 % of ADPKD patients develop end-stage renal failure by the age of 60 years. While clinical symptoms usually only arise in adulthood, there is considerable phenotypic variability even within the same family. In children, diagnosis of ADPKD is frequently made by family screening or as an incidental finding on US. About 60 % of ADPKD children aged less than 5 years have already one or more renal cysts detectable by US (Gabow et al. 1997). In general, the finding of even one renal cyst should alert the physician to the possibility of ADPKD because simple cysts are otherwise rare in childhood. Therefore family history and investigation, in particular parental US, are obligatory. In children with parental ADPKD, the finding of one cyst can already be considered diagnostic (Ravine et al. 1994).
About 2 % of ADPKD patients manifest clinically before age 15 years (Bergmann 2012). ADPKD-related symptoms include arterial hypertension, pain, episodes of hematuria, renal calculi, proteinuria, infection, or a palpable mass. Risk factors for a more rapid progression of ADPKD are (1) renal enlargement early in life, (2) having more than ten renal cysts before age of 12 years, and (3) having blood pressures above the 75th percentile for age, height, and gender (Fick-Brosnahan et al. 2001). Occasional ADPKD cases are even associated with significant perinatal morbidity and mortality and may be indistinguishable from severe forms of ARPKD (Fick et al. 1993; Bergmann et al. 2011).
ADPKD is a systemic ciliopathy, and cysts may also arise in other organs, e.g., liver, pancreas, seminal vesicles, and arachnoid membrane (Torres et al. 2007). About 8 % of ADPKD patients develop intracranial aneurysms, particularly those with a positive family history for intracranial aneurysm and/or hemorrhage (Rossetti et al. 2003). Approximately 10 % of first aneurysmal ruptures were reported to occur before age 20 years (Chauveau et al. 1994). Cardiac valve disease, mainly mitral valve prolapse, has been detected in 26 % of ADPKD patients (Lumiaho et al. 2001).
4.3 Nephronophthisis (NPHP) and Medullary Cystic Kidney Disease (MCKD)
Nephronophthisis (NPHP) comprises a clinically and genetically heterogeneous group of autosomal recessive ciliopathies (Hildebrandt et al. 2011). NPHP is the most frequent genetic cause of end-stage renal disease during the first three decades of life (median age 13 years). Renal histopathology is characterized by the triad of (1) tubular basement disruption, (2) tubulointerstitial fibrosis with cell infiltration, and (3) tubular cysts, mainly at the corticomedullary junction (Waters and Beales 2011). Although NPHP is generally referred to as a cystic kidney disease, cysts are not an obligatory feature and frequently occur only after patients have progressed to end-stage renal failure. NPHP manifests clinically with a urinary concentration defect leading to polyuria and polydipsia, as well as anemia and progressive renal failure (Bergmann 2012). Since cilia are found in virtually all organs and serve distinct functions in different tissues, ciliopathies may cause a broad range of organ involvement. In NPHP extrarenal manifestations are frequent and bear a significant comorbidity (Waters and Beales 2011). Ciliopathies may involve the eyes (retinitis pigmentosa, oculomotor apraxia), the brain (cerebellar vermis hypo-/aplasia associated with the “molar tooth sign” on MRI, mental retardation, encephalocele), the liver (cholangiociliopathies with liver fibrosis), and the bones (short ribs, cone-shaped epiphyses, postaxial polydactyly). Based on the pattern of organ involvement, numerous syndromes with high phenotypic variability and considerable overlap have been described.
MCKD is often considered the autosomal dominant variant of NPHP with a usually later onset of renal failure than in the recessive forms. Mutations in the gene encoding the ciliary protein uromodulin (Tamm-Horsfall glycoprotein) can lead to different tubulointerstitial nephropathies including MCKD2, glomerulocystic kidney disease, and familial juvenile hyperuricemic nephropathy (Vylet’al et al. 2006).
Take Away
In the majority of ADPKD patients, renal cysts arise already during childhood, and family history and parental US are mostly the key to diagnosis. Familial clustering of valvular heart disease and intracranial aneurysms must be taken in account.
Take Away
In NPHP patients additional imaging of potential extrarenal manifestations involving, for example, the liver, brain, or bones, is essential for a correct and complete diagnosis as well as during follow-up.
4.4 Glomerulocystic Kidney Disease (GCKD)
GCKD is defined histologically by the occurrence of glomerular cysts with dilatation of the Bowman’s space and glomerular tufts (Bernstein 1993). GCKD was described, e.g., in various ciliopathies including ADPKD (particularly in young infants), NPHP, and MCKD (type 2), as well as tuberous sclerosis and the renal cysts and diabetes syndrome (Mache et al. 2002). GCKD has also been associated with renal dysplasia and urinary tract obstruction (Bissler et al. 2010).
Take Away
GCKD is a histological finding in various cystic kidney diseases. Since in most of these patients no renal biopsy is performed, this diagnosis is rarely made and often missed, as there are no specific imaging or laboratory features that would suggest the diagnosis. However, this has no implication on treatment and prognosis.
4.5 Multicystic Dysplastic Kidney (MCDK)
Unilateral MCDK is the most common form of cystic renal dysplasia with an incidence of 1 in 2,200 to 1 in 4,300 live births (Schreuder et al. 2009). The ipsilateral ureter is frequently atretic and sometimes even absent, supporting the theory that MCDK results from early ureteral pathology during nephrogenesis (Woolf 1997). It usually affects the entire kidney, but rarely can also involve only a part of the kidney, e.g., in a duplex system (Jeon et al. 1999). Unilateral MCKD is commonly a sporadic malformation, incidental reports exist on MCDK in siblings, twins and families (Srivastava et al. 1999). Bilateral MCKD is usually incompatible with extrauterine life.
Renal function depends on the solitary functioning contralateral kidney. Abnormalities of the contralateral renal unit may be found in one-third of patients, mainly VUR (Schreuder et al. 2009). In the absence of compensatory hypertrophy, renal hypo-/dysplasia should be suspected. Injury of the solitary kidney may lead to hypertension, microalbuminuria, and/or a decrease in glomerular filtration rate. Furthermore, associated ipsilateral genital anomalies are found in up to 50 %, such as cystic dysplasia of the rete testis or the seminal vesicle. Previous concerns about an increased risk of hypertension and malignancy have been allayed based on results from longer follow-up studies and systematic reviews, as well as on some immature blastema found in surgery specimen that hypothetically allows for an increased risk of malignant differentiation later on (Narchi 2005a, b; Aslam et al. 2006).
Clinically, MCDK is commonly detected by fetal US. MCDK is now generally regarded as a benign condition with conservative management and long-term follow-up predominating over surgical removal. Nephrectomy is mostly restricted to cases with continuous growth leading to compression of adjacent structures, infection, hemorrhage, or suspected tumors. Spontaneous involution of MCKD was reported to be 35 % by 2 years, 47 % by 5 years, and 62 % by 10 years of age, respectively (Hayes et al. 2012). Larger postnatal MCDK (>5 cm) are less likely to involute already during the first decade of life than smaller MCDK (Hayes et al. 2012; Poggiali and Oliveira 2012).
Take Away
The task of imaging is to establish the diagnosis, to evaluate the contralateral renal unit, to detect rare complications, and to monitor the involution of MCKD.
4.6 Medullary Sponge Kidney (MSK)
MSK is a kidney malformation of unknown etiology that generally becomes manifest with nephrocalcinosis, recurrent renal stones, and pre-calyceal duct ectasias (erroneously diagnosed as cysts) (Fabris et al. 2013) (see also chapter “Urolithiasis and Nephrocalcinosis”). Clinically, MSK may present with renal colic, episodes of hematuria, pyelonephritis, or renal failure. Frequent findings are hypercalciuria as well as renal acidification and concentration defects. MSK rarely presents in childhood and may be a familial disease in up to 10 % of cases.
Take Away
In childhood MSK is a rare and mostly sporadic diagnosis suspected and established by the radiologist. Due to its probably heterogeneous etiology, a comprehensive nephrological work-up is mandatory.
4.7 Simple Renal Cyst
Simple renal cysts can occur spontaneously or be familial. They are rare in childhood with a reported incidence of 0.22 % (McHugh et al. 1991). Simple cysts do not bare any consequences or associated risks except for a few occasions, when growing cysts lead to hypertension, compression of adjacent structures, or obstruction of the collecting system (Churchill et al. 1975). In adults, cysts are much more common (up to 50 %), and the development of simple renal cysts is seen as a normal aging phenomenon (Baert and Steg 1977; Tada et al. 1983).
Acquired cysts can occur in post-traumatic and post-inflammatory (tuberculous, etc.) settings or spontaneously develop in kidney parenchyma during chronic renal failure and on dialysis (Dunill et al. 1977; Leichter et al. 1988; Hogg 1992). As in end-stage kidneys with acquired cysts malignancy may develop, they need to be monitored (Bretan et al. 1986; Levine 1992).
Simple renal cysts are rare in infancy and childhood. US usually detects them as an incidental finding. Possible manifestation of a polycystic or dysplastic renal disease must be considered, and follow-up is warranted.
Take Away
In children, a renal cyst may be a feature of ADPKD or cystic renal dysplasia and always warrants at least a follow-up US examination.
4.8 Complicated Renal Cyst, Multiloculated Cyst, and Cystic Renal Tumor
“Complicated cyst” is a term coined by descriptive radiology. The exact definition varies depending on the imaging modality applied and the age of the patient. A complicated cyst is defined as a cystic lesion with some abnormalities, therefore not matching all criteria necessary for a simple cyst. These are small size, clear and sharp margins, no echoes or contents in the clear fluid, and no parenchymal rim or inclusion. The radiological changes of a complicated cyst may originate from secondary hemorrhage or sedimentation of proteins and of membrane cells. Calcifications may also occur, or infection may be present. Differentiation of these cysts, usually discovered by US, is essential and achieved in part by CT/MRI, in part in conjunction with clinical and laboratory findings (Table 1).
Tumors have to be recognized and imaged/treated appropriately. Many tumor entities can present as a cystic renal tumor; the histologies range from benign renal neoplasms to cystic Wilms’ tumor, cystic mesoblastic nephroma, and cystic renal adenocarcinoma (Theissig et al. 1986; Babut et al. 1993; Upadhyay and Neely 1989). Definite diagnosis is often only made histologically as imaging features may not be characteristic in the individual case (see also chapter “Neoplasms of the Genitourinary System”).
Take Away
If a renal cyst does not match the criteria of a “simple” cyst on US, further imaging modalities are necessary and determine whether a biopsy is taken or follow-up is scheduled.
Conclusion
Congenital anomalies of the kidney and cystic renal diseases comprise many entities that may be diagnostically challenging. Family history and investigation, clinical presentation and evolution, renal imaging, and searching for extrarenal manifestations are valuable diagnostic tools. In addition, next-generation sequencing-based approaches allow parallel analysis of multiple genes involved in nephrogenesis and ciliary function and increasingly provide accurate genetic diagnoses. An accurate diagnosis is essential for genetic counseling, prenatal diagnostics, and the clinical management of patients and their families.
References
Adalat S, Woolf AS, Johnstone KA et al (2009) HNF1B mutations associate with hypomagnesemia and renal magnesium wasting. J Am Soc Nephrol 20:1123–1131
Adeva M, El-Youssef M, Rossetti S (2006) Clinical and molecular characterization defines a broadened spectrum of autosomal recessive polycystic kidney disease (ARPKD). Medicine (Baltimore) 85:1–21
Aslam M, Watson AR, Trent & Anglia MCDK Study Group (2006) Unilateral multicystic dysplastic kidney: long term outcomes. Arch Dis Child 91:820–823
Babut JM, Bawab F, Jouan H et al (1993) Cystic renal tumors in children–a diagnostic challenge. Eur J Pediatr Surg 3:157–160
Baert L, Steg A (1977) On the pathogenesis of simple renal cysts in the adult. Urol Res 5:103–108
Bergmann C (2012) Ciliopathies. Eur J Pediatr 171:1285–1300
Bergmann C (2015) ARPKD and early manifestations of ADPKD: the original polycystic kidney disease and phenocopies. Pediatr Nephrol 30(1):15–30
Bergmann C, Senderek J, Sedlacek B et al (2003) Spectrum of mutations in the gene for autosomal recessive polycystic kidney disease (ARPKD/PKHD1). J Am Soc Nephrol 13:76–89
Bergmann C, Senderek J, Windelen E (2005) Clinical consequences of PKHD1 mutations in 164 patients with automoal recessive polycystic kidney disease (ARPKD). Kidney Int 67:829–848
Bergmann C, von Bothmer J, Ortiz Brüchle N et al (2011) Mutations in multiple PKD genes may explain early and severe polycystic kidney disease. J Am Soc Nephrol 22:2047–2056
Bernstein J (1993) Glomerulocystic kidney disease – nosological considerations. Pediatr Nephrol 7:464–470
Bissler JJ, Siroky BL, Yin H (2010) Glomerulocystic kidney disease. Pediatr Nephrol 25:2049–2059
Bretan PN Jr, Bush MP, Hricak H et al (1986) Chronic renal failure: a significant risk factor in the development of acquired renal cysts and renal cell carcinoma. Case report and review of the literature. Cancer 57:1871–1879
Chang EH, Menezes M, Meyer NC et al (2004) Branchio-oto-renal syndrome: the mutation spectrum in EYA1 and its phenotypic consequences. Hum Mut 23:582–589
Chauveau D, Pirson Y, Verellen-Dumoulin C et al (1994) Intracranial aneurysms in autosomal dominant polycystic kidney disease. Kidney Int 45:1140–1146
Churchill E, Kimoff R, Pinshy M et al (1975) Solitary intrarenal cyst: correctable cause of hypertension. Urology 6:485–488
Dunill MS, Millard PR, Oliver D (1977) Acquired cystic disease of the kidneys: a hazard of long term intermittent maintenance haemodialysis. J Clin Pathol 30:868–877
Fabris A, Anglani F, Lupo A et al (2013) Medullary sponge kidney: state of the art. Nephrol Dial Transpl 28:1111–1119
Fick GM, Johnson AM, Strain JD et al (1993) Characteristics of very early onset autosomal dominant polycystic kidney disease. J Am Soc Nephrol 3:1863–1870
Fick-Brosnahan GM, Tran ZV, Johnson AM et al (2001) Progression of autosomal dominant polycystic kidney disease in children. Kidney Int 59:1654–1662
Gabow PA, Kimberling WJ, Strain JD (1997) Utility of ultrasonography in the diagnosis of autosomal dominant polycystic kidney disease in children. J Am Soc Nephrol 8:105–110
Goetz SC, Anderson KV (2010) The primary cilium: a signalling centre during vertebrate development. Nat Rev Genet 11:331–344
Guay-Woodford LM, Desmond RA (2003) Autosomal recessive polycystic kidney disease: the clinical experience in North America. Pediatrics 111:1072–1080
Harris PC, Torres VE (2009) Polycystic kidney disease. Annu Rev Med 60:321–337
Hayes WN, Watson AR, Trent & Anglia MCKD Study Group (2012) Unilateral multicystic dysplastic kidney: does initial size matter? Pediatr Nephrol 27:1335–1340
Hildebrandt F, Benzing T, Katsanis N (2011) Ciliopathies. New Engl J Med 364:1533–1543
Hogg RJ (1992) Acquired cystic kidney disease in children prior to the start of dialysis. Pediatr Nephrol 6:176–178
Ichikawa I, Kuwayama F, Pope JC 4th et al (2002) Paradigm shift from classical anatomic theories to contemporary cell biological views of CAKUT. Kidney Int 61:889–898
Jeon A, Cramer BC, Walsh E et al (1999) A spectrum of segmental multicystic renal dysplasia. Pediatr Radiol 29:309–315
Kashtan CE, Primack WA, Kainer G (1999) Recurrent bacteremia with enteric pathogens in recessive polycystic kidney disease. Pediatr Nephrol 13:678–682
Kerecuk L, Schreuder MF, Woolf AS (2008) Renal tract malformations: perspectives for nephrologists. Nat Clin Pract Nephrol 4:312–325
Leichter HE, Dietrich R, Salusky I et al (1988) Acquired cystic kidney disease in children undergoing long-term dialysis. Pediatr Nephrol 2:8–11
Levine E (1992) Renal cell carcinoma in uremic acquired renal cystic disease: incidence, detection and management. Urol Radiol 13:203–210
Lumiaho A, Ikaheimo R, Miettinen R et al (2001) Mitral valve prolapse and mitral regurgitation are common in patients with polycystic kidney disease type 1. Am J Kidney Dis 38:1208–1216
Mache CJ, Preisegger KH, Kopp S et al (2002) De novo HNF-1 beta gene mutation in familial hypoplastic glomerulocystic kidney disease. Pediatr Nephrol 17:1021–1026
McHugh K, Stringer D, Hebert D (1991) Simple renal cyst in children: diagnosis and follow-up with US. Radiology 178:383–385
Narchi H (2005a) Risk of hypertension with multicystic dysplastic kidney disease: a systematic review. Arch Dis Child 90:921–924
Narchi H (2005b) Risk of Wilms’ tumor with multicystic dysplastic kidney disease: a systematic review. Arch Dis Child 90:147–149
Poggiali IV, Oliveira EA (2012) Renal size and sonographic involution of multicystic dysplastic kidney. Pediatr Nephrol 27:1601–1602
Ravine D, Gibson RN, Walker RG et al (1994) Evaluation of ultrasonographic diagnostic criteria for autosomal dominant polycystic kidney disease 1. Lancet 343:824–827
Renkema KY, Winyard PJ, Skovorodkin IN et al (2011) Novel perspectives for investigating congenital anomalies of the kidney and urinary tract. Nephrol Dial Transpl 26:3843–3851
Rosenblum ND, Salomon R (2008) Disorders of kidney formation. In: Geary DF, Schaefer F (eds) Comprehensive pediatric nephrology. Mosby Elsevier, Philadelphia, pp 131–141
Rossetti S, Chauveau D, Kubly V et al (2003) Association of mutation position in polycystic kidney disease 1 (PKD1) gene and development of a vascular phenotype. Lancet 361:2196–2201
Sanyanusin P, Schimmenti LA, McNoe LA et al (1995) Mutation of the PAX2 gene in a family with optic nerve colobomas, renal anomalies and vesicoureteral reflux. Nat Genet 9:358–364
Schedl A (2007) Renal abnormalities and their developmental origin. Nature Rev Genet 8:791–792
Schreuder MF, Westland R, van Wijk JAE (2009) Unilateral multicystic dysplastic kidney: a meta-analysis of observational studies on the incidence, associated urinary tract malformations and the contralateral kidney. Nephrol Dial Transpl 24:1810–1818
Srivastava T, Garola RE, Hellerstein S (1999) Autosomal dominant inheritance of multicystic dysplastic kidney. Pediatr Nephrol 13:481–483
Tada S, Yamagishi J, Kobayashi H et al (1983) The incidence of simple renal cysts by computed tomography. Clin Radiol 34:437–439
Theissig F, Hempel J, Schubert J (1986) Multilocular cystic nephroma simulating kidney carcinoma. Ztschr Urol Nephrol 79:263–267
Torres VE, Harris PC, Pirson Y (2007) Autosomal dominant polycystic kidney disease. Lancet 369:1287–1301
Ulinski T, Lescure S, Beaufils S et al (2006) Renal phenotypes related to hepatocyte nuclear factor-1beta (TCF2) mutations in a pediatric cohort. J Am Soc Nephrol 17:497–503
Upadhyay AK, Neely JAC (1989) Cystic nephroma: an emerging entity. Ann R Coll Surg Engl 71:381–383
Vivante A, Kohl S, Hwang DY et al (2014) Single-gene causes of congenital anomalies of the kidney and urinary tract (CAKUT) in humans. Pediatr Nephrol 29:695–704
Vylet’al P, Kublova M, Kalbacova M et al (2006) Alterations of uromodulin biology: a common denominator of the genetically heterogeneous FJHN/MCKD syndrome. Kidney Int 70:1155–1169
Waters AM, Beales PL (2011) Ciliopathies: an expanding disease spectrum. Pediatr Nephrol 26:1039–1056
Watkins SL, McDonald RA, Avner ED (1997) Renal dysplasia, hypoplasia and miscellaneous cystic disorders. In: Barrat MT, Avner ED, Harmon WE (eds) Pediatric nephrology. Lippincott Williams & Wilkins, Baltimore, pp 415–426
Weber S (2012) Novel genetic aspects of congenital anomalies of kidney and urinary tract. Curr Opin Pediatr 24:212–218
Weber S, Moriniere V, Knüppel T et al (2006) Prevalence of mutations in renal developmental genes in children with renal hypodysplasia: results of the ESCAPE study. J Am Soc Nephrol 17:2864–2870
Westland R, Schreuder MF, Ket JCF et al (2013) Unilateral renal agenesis: a systematic review on associated anomalies and renal injury. Nephrol Dial Transplant 28:1844–1855
Winyard P, Chitty LS (2008) Dysplastic kidneys. Semin Fetal Neonatal Med 13:142–151
Woodward PJ, Kennedy A, Sohaey R et al (2011) Diagnostic imaging – obstetrics. Amirsys, Salt Lake City, pp 2–28
Woolf AS (1997) The kidney: embryology. In: Barrat MT, Avner ED, Harmon WE (eds) Pediatric nephrology. Lippincott Williams & Wilkins, Baltimore, pp 1–17
Woolf AS, Hillman KA (2007) Unilateral renal agenesis and the congenital solitary functioning kidney: developmental, genetic and clinical perspectives. BJU Int 99:17–21
Woolf AS, Price KL, Scrambler PJ et al (2004) Evolving concepts in human renal dysplasia. J Am Soc Nephrol 15:998–1007
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Mache, C., Hubmann, H. (2018). Renal Agenesis, Dysplasia, Hypoplasia, and Cystic Diseases of the Kidney. In: Riccabona, M. (eds) Pediatric Urogenital Radiology. Medical Radiology(). Springer, Cham. https://doi.org/10.1007/978-3-319-39202-8_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-39202-8_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-39200-4
Online ISBN: 978-3-319-39202-8
eBook Packages: MedicineMedicine (R0)