Abstract
The ADCYAP1 gene, which is expressed in certain cancer cells, encodes for pituitary adenylate cyclase activating polypeptide (PACAP). The translated protein products for the ADCYAP1 gene include prepro PACAP (176 amino acids) as well as the biologically active PACAP-27 or PACAP-38. When secreted from cancer cells, PACAP-27 or PACAP-38 binds with high affinity to VPAC1, VPAC2, and PAC1. The activated PAC1 elevates cAMP and causes phosphatidylinositol turnover. PAC1 regulates the phosphorylation of numerous proteins in lung cancer including protein kinase C, paxillin, focal adhesion kinase, Src, the epidermal growth factor receptor, and extracellular signal-regulated kinase (ERK). The phosphorylated ERK enters the nucleus and increases the expression of the nuclear oncogenes c-fos and c-jun. The c-fos and c-jun form heterodimers altering the expression of growth factor genes. PACAP-27 or PACAP-38 stimulates the clonal growth of cancer cells. A PAC1 antagonist is PACAP(6–38), which inhibits the ability of PACAP-27 or PACAP-38 to increase protein phosphorylation, nuclear oncogene expression, and the proliferation of cancer cells.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- PACAP
- Lung cancer
- Proliferation
- PAC1
- PACAP(6–38)
- Signal transduction
- Tyrosine phosphorylation
- EGFR
- ERK
- Transactivation
Introduction
Pituitary adenylate cyclase-activating polypeptide (PACAP)-27 has sequence homology (67 %) with vasoactive intestinal peptide (VIP) [1]. PACAP-27, PACAP related peptide (PRP), and PACAP-38 are derived from a 176-amino acid precursor protein preproPACAP [2]. PACAP-38 contains PACAP-27 plus an addition 11 amino acids at the C-terminal [3, 4]. PACAP-38 and PACAP-27 were isolated from ovine hypothalamus and elevate cAMP in rat pituitary cells in culture. The PACAP-38 amino acid sequence is highly conserved and is identical in mammals [5]. In cellular extracts approximately an order of magnitude more PACAP-38 is detected than PRP or PACAP-27. PACAP-38 and PACAP-27 have approximately an order of magnitude more biological activity than does PRP [5].
PACAP-27 and PACAP-38 bind with high affinity to G-protein coupled receptors (GPCR; VPAC1, VPAC2, and PAC1) which are members of the class II or class B secretin-like receptors [6]. The activated VPAC1, VPAC2, or PAC1 interact with a stimulatory guanine nucleotide binding protein (Gs) increasing adenylylcyclase activity resulting in elevated cellular cAMP [7]. The increased cAMP activates protein kinase (PK) A causing phosphorylation of various proteins such as CREB leading to altered gene expression [8]. In addition, PAC1 interacts with Gq causing phospholipase (PL) C activation [9]. The PLC metabolizes phosphatidyl inositol (PI) 4,5 bisphosphate to inositol-1,4,5-trisphosphate and diacylglycerol which increase cytosolic calcium and PKC activity, respectively. PACAP-27 addition to cancer cells increases the phosphorylation of numerous proteins in lung cancer including PKC, paxillin, focal adhesion kinase (FAK), Src, the epidermal growth factor receptor (EGFR), and extracellular signal-regulated kinase (ERK) [10]. The phosphorylated ERK enters the nucleus and increases the expression of the nuclear oncogenes c-fos and c-jun [11, 12]. The c-fos and c-jun form heterodimers altering the expression of growth factor genes. PACAP-27 or PACAP-38 stimulates the growth of brain cancer [13], colon cancer [14], neuroendocrine tumors [15, 16], pancreatic cancer [17] and SCLC [18]. A PAC1 antagonist, PACAP(6–38), inhibits the growth of lung, breast and prostate cancer cells [19–22]. PAC1 has been detected in a wide variety of tumors including brain, breast, colon, lung, neuroendocrine, pancreatic, pituitary, and prostate cancer [23–25]. In this chapter, the role of PACAP in cancer is presented.
Lung Cancer
PACAP-38 has been detected in tumors of the colon, lung, and prostate [8, 26, 27]. PACAP binds with high affinity to small cell lung cancer (SCLC) cell lines [18]. SCLC is a neuroendocrine tumor which kills approximately 25,000 United States (US) citizens annually. Patients with SCLC are traditionally treated with chemotherapy and/or radiation therapy. While the therapy is initially effective, relapse occurs and the median survival time is less than 1 year [28]. SCLC contains high levels of dopa decarboxylase (DDC), neuron specific enolase (NSE), and bombesin (BB)-like peptides [29]. Specific binding of 125I-PACAP-27 to NCI-H345 or NCI-N417 SCLC cells was inhibited with high affinity by PACAP-27 or PACAP-38 and the IC50 values were 5 and 10 nM respectively [18]. In contrast, PACAP(6–38), PACAPhybrid and VIP bind to PAC1 with IC50 values of 1500, 750 and 500 nM, respectively (Table 47.1). The results indicate that PACAP-27 binds to PAC1 with approximately 2-orders of magnitude greater affinity than does VIP. PCR products for VIP, PACAP, VPAC1, and PAC1 were present in six of eight lung cancer cell lines tested, however, only two out of eight cell lines had VPAC2 [30]. PACAP-38 immunoreactivity is higher in the human lung cancer than normal lung biopsy specimens [27].
A general problem is that the VPAC1 density (100,000/cell) is much greater than that of PAC1 (14,000/cell) in lung cancer and PACAP binds with high affinity to PAC1, VPAC1 and VPAC2. The 61-amino acid maxadilan is selective for PAC1; however, it has little sequence homology to PACAP [31]. Recently 46 PACAP analogs were synthesized and evaluated for selectivity for PAC1 relative to VPAC1 and VPAC2 [32]. Fifteen of the 46 analogs tested had selectivity for PAC1 relative to VPAC1. (Iac1, Ala16,17, DLys38)PACAP-38 bound with higher affinity to PAC1 (IC50 = 0.3 nM) relative to VPAC1 (IC50 = 23 nM) or VPAC2 (IC50 = 3 nM). (Iac1, Ala16,17, DLys38)PACAP-38 [(IAAD)PACAP-38] was an agonist which was more potent at elevating cAMP using cells containing PAC1 (EC50 = 0.05 nM) relative to VPAC1 (EC50 = 1.5 nM) or VPAC2 (EC50 = 2.5 nM). The results indicate that (IAAD)PACAP-38 prefers PAC1 relative to VPAC1 by 50- to 80-fold and prefers PAC1 relative to VPAC2 by 10- to 50-fold. Previously it was found that PACAP-38 is metabolized by dipeptidyl peptidase IV [33]. Acetyl-[Ala15, Ala20]PACAP-38 propylamide and acetyl-PACAP-27-propylamide had improved biological activity and metabolic stability relative to PACAP-27 or PACAP-38. The results indicate that PACAP analogs are available which prefer PAC1 relative to VPAC1 or VPAC2.
PACAP-27 or PACAP-38 has a secondary structure in that it has a β-turn at amino acids 9–12 followed by an α-helix at amino acids 12–14, 15–20, and 22–24 [34, 35]. Also, an α-helix forms at amino acids 28–38 of PACAP-38. Site-directed mutagenesis studies indicate that several amino acids in the N-terminal of PAC1 such as Tyr138 and Glu137 are essential for high affinity PACAP binding [35]. Mutation of Val19, Tyr22, Val26, or Leu27 in PACAP impaired high affinity binding to PAC1. Modeling studies suggest that the C-terminal of PACAP binds to the N-terminal of PAC1, whereas the N-terminal of PACAP binds to the PAC1 extracellular (EC) loops and transmembrane (TM) domains [36].
PAC1 is a GPCR with 467 amino acids (null; [37]) which has seven TM domains. Splice variants (SV) have been identified and PAC1 SV-1 or the hip receptor has an additional 28-amino acid insert in intracellular loop (IC) 3 [38]. PAC1 SV-2 or the hop receptor (HOP1) contains 495 amino acids and has a different 28-amino acid insert in IC3. PAC1 SV-3 or the hip-hop receptor contains 523 amino acids and has both 28-amino acid inserts in IC3. All PAC1SVs interact with Gs and stimulate adenylyl cyclase. PAC1 SV-2 interacted strongly with Gq causing phosphatidylinositol (PI) turnover whereas PAC1 null, PAC1 SV-1 or PAC1 SV-3 have a weaker response [9]. C-Fos expression was strongly increased when PACAP-27 was added to cells containing PAC1 SV-2 relative to PAC1 null, PAC1 SV-1, or PAC1 SV-3 [39]. The Ca2+ response was maximal when PACAP-27 was added to cells containing PAC1 SV-2 relative to PAC1null, PAC1 SV-1 or PAC1 SV-3 [39]. The results indicate that PAC1 null, PAC1 SV-1, PAC1 SV-2, or PAC1 SV-3 interact with Gs, however, PAC1 SV-2 interacts better than PAC1 null, PAC1 SV-1, or PAC1 SV-3 with Gq.
When PAC1 activates Gs it stimulates adenylyl cyclase increasing the cAMP 5.5-fold (Table 47.2). Both PACAP-27 and PACAP-38 (1 nM) increased significantly the cAMP 5.5-fold after addition to lung cancer cells, however, PACAP(16–38) is inactive (Table 47.2). The increase in cAMP caused by PACAP-27 was antagonized significantly by 1 μM PACAPhybrid or PACAP(6–38) [20]. The results indicate that nM concentrations of PACAP-27 are required to elevate cAMP and that PACAP(6–38) or PACAPhybrid are PAC1 antagonists in cancer cells.
PACAP-27 or PACAP-38 (100 nM) increased the cytosolic Ca2+ in lung cancer cells. The increase in cytosolic Ca2+ caused by PACAP-27 was antagonized by 1 μM PACAPhybrid or PACAP(6–38) [20]. Figure 47.1 shows a dose–response curve for (Iac1, Ala16,17, DLys38)PACAP-38 to elevate cytosolic Ca2+. (Iac1, Ala16,17, DLys38)PACAP-38 had little effect on NCI-H838 cytosolic Ca2+ at a 0.1 or 1 nM dose, however, it moderately and strongly increased cytosolic Ca2+ at a 10 or 100 nM concentration, respectively. The results indicate that 10 nM doses of PACAP-27, PACAP-38, and (Iac1, Ala16,17, DLys38)PACAP-38 are needed to elevate the cytosolic Ca2+ in lung cancer cells and whereas lower doses are needed to elevate cAMP [32].
PACAP has additional signal transduction mechanisms. Addition of 10 nM PACAP-27 to non-SCLC (NSCLC) cell line NCI-H1299 cells increased ERK tyrosine phosphorylation [12]. The increase in ERK tyrosine phosphorylation caused by PACAP was reversed by PACAP(6–38) or PD98059, a MEK inhibitor. Phosphorylated ERK can enter the nucleus and alter gene expression. PACAP-27 or PACAP-38 increased c-fos mRNA in NCI-N417 cells after 4 h [11]. The increase in c-fos expression caused by PACAP was reversed by PACAP(6–38) or H7, a PKC inhibitor. C-fos and c-jun can form heterodimers and increase expression of genes with AP-1 sites. PACAP-27 (100 nM) addition to NCI-H1299 cells increased expression of vascular endothelial growth factor (VEGF) after 8 h [12]. The increase in VEGF mRNA caused by PACAP-27 was inhibited by PACAP(6–38) or PD98059. VEGF is an angiogenic factor which increases the vascularization of tumors.
PACAP-27 (10 nM) stimulated the clonal growth of lung cancer cells significantly to 178 % (Table 47.3). The increase in clonal growth stimulated by PACAP-27 was inhibited significantly by 1 μM PACAP(6–38). PACAP(6–38) reduced basal colony number to 63 %. Injection of 0.4 mg/kg of PACAP(6–38) into nude mice reduced NCI-H838 xenograft growth significantly to 67 %. The results suggest that PAC1 regulates the growth of lung cancer cells [19].
PACAP addition to NSCLC cells causes phosphorylation of numerous proteins. PACAP-27 addition to lung cancer cells causes tyrosine phosphorylation of focal adhesion kinase (FAK) and paxillin [40]. Tyrosine phosphorylation of FAK and paxillin are associated with reorganization of the actin cytoskeleton and assembly of focal adhesion plaques [41]. The ability of PACAP to increase FAK phosphorylation was reversed by PP2 (Src inhibitor), U73122 (PLC inhibitor), or PACAP(6–38) [40]. PACAP-27 addition to lung cancer cells caused tyrosine phosphorylation of proline-rich tyrosine kinase (PYK)2 [42]. PYK-2 interacts with paxillin which coordinates Rho family GTPases regulating the actin skeleton [43]. The ability of PACAP to increase PYK-2 phosphorylation was reversed by PP2, PACAP(6–38), U73122 or BAPTA, a Ca2+ chelator [42]. Finally PACAP-27 addition to lung cancer cells caused tyrosine phosphorylation of the EGFR. The ability of PACAP to cause EGFR transactivation was inhibited by PP2, PACAP(6–38) or gefitinib, an EGFR tyrosine kinase inhibitor (TKI) [44].
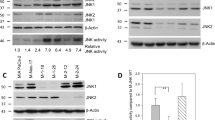
(IAAD)PACAP-38 addition to NSCLC cells increased EGFR tyrosine phosphorylation in a concentration-dependent manner (Fig. 47.2). Addition of 1, 10, or 100 nM (IAAD)PACAP-38 to NCI-H838 cells weakly, moderately and strongly, respectively increased EGFR tyrosine phosphorylation (Fig. 47.2, top) whereas total EGFR was unaffected (Fig. 47.2, bottom). The rapid transactivation of the EGFR caused by PACAP addition to lung cancer cells is matrix metalloprotease (MMP) dependent [10, 44]. Addition of the MMP inhibitor GM6001 to lung cancer cells inhibited the PAC1 regulation of EGFR transactivation [44]. Also, PACAP increased secretion of the EGFR ligand transforming growth factor (TGF) α from lung cancer cells that was inhibited significantly by GM6001. MMP may metabolize inactive proTGFα in lung cancer cells to biologically active TGFα. The TGFα binds with high affinity to the EGFR causing phosphorylated homodimers to form in lung cancer cells [45]. The results suggest that PACAP may stimulate lung cancer growth in an EGFR-dependent manner.
Gefitinib or erlotinib are EGFR TKI that are used to treat NSCLC patients which have certain EGFR mutations [46, 47]. Approximately 13 % of the lung cancer patients who respond to EGFR TKI have activating mutations. A goal is to increase the sensitivity of gefitinib in patients with wild type EGFR. Table 47.3 shows that gefitinib or PACAP(6–38) moderately inhibits the growth of NCI-H838 cells. Addition of both PACAP(6–38) and gefitinib strongly inhibits lung cancer growth suggesting that PACAP(6–38) is synergistic with gefitinib at inhibiting lung cancer growth in vitro. It remains to be determined if PACAP(6–38) is synergistic with gefitinib at inhibiting lung cancer growth in vivo.
Brain Tumors
Neuroblastoma cells have predominantly PAC1, some VPAC2 and little VPAC1. PAC1SVs are present in the N-terminal of PAC1 [48]. PAC1 has 18 exons and exons 1–6 encode for the N-terminal, whereas exons 7–17 encode for the seven TM domains and exon 18 encodes for the C-terminal. Alternative splicing of exon 5, exons 5, 6 or exons 4–6 result in deletions of 7, 21 (short) or 57 amino acids (very short) in the N-terminal of PAC1 [49]. Addition of PACAP-38 to neuroblastoma cell lines SH-SY5Y, SK-N-Be or NB100 increased the cAMP with EC50 values ranging from 0.05 to 1 nM [48]. The PAC1SVs which predominated in SH-SY5Y cells were the δ5,6null; δ5,6hop; and δ4,5,6null. Cells which expressed PAC1null, PAC1δ5null, PAC1δ5,6null but not PAC1δ4,5,6null bound 125I-PACAP-27 with high affinity [50]. These results indicate that the very short PAC1 is missing essential amino acids from the N-terminal of PAC1 that are critical to interact with the C-terminal of PACAP.
The ability of PAC1 SV to elevate cAMP and cause PI turnover was investigated. PACAP-38 was more potent at elevating cAMP in cells containing PAC1null or PAC1hop than PAC1hip. Similarly PACAP-38 was more potent at elevating cAMP in PAC1δ5null or PAC1δ5hop than PAC1δ5hip [51]. Also PACAP-38 was more potent at elevating cAMP in cells containing PAC1δ5,6null or PAC1δ5,6hop than PAC1δ5,6hip. The results indicate that the PAC1SV1 does not stimulate adenylylcyclase as well as PAC1null or PAC1SV2 regardless of whether the PAC1δ5 or PAC1δ5,6 is present. Previously it was found that PAC1hop was better than PAC1null or PAC1hip at causing PI turnover [9]. PACAP-38 was more potent at causing PI turnover in cells containing PAC1δ5hop than PAC1δ5null whereas PAC1δ5hip was ineffective. Also, PACAP-38 was more potent at causing PI turnover in cells containing PAC1δ5,6hop than PAC1δ5,6null whereas PAC1δ5,6hip was ineffective. The results indicate that PAC1hop strongly activates PLCβ, PAC1null moderately activates PLCβ whereas PAC1hip weakly activates PLCβ regardless of whether PAC1δ5 or PAC1δ5,6 is present. The results indicate that PAC1 IC3 regulates adenylylcyclase and/or PLC activity.
The signal transduction mechanisms of PAC1 SV were investigated in NG108-15 cells (mouse neuroblastoma × rat glioma hybrid). PACAP-38, 1 nM, strongly increased cAMP in cells transfected with PAC1null, PAC1hip, and PAC1hop. PACAP-38, 100 nM, strongly increased cytosolic Ca2+ in cells transfected with PAC1hop and PAC1null but not PAC1hip [52]. All PAC1SVs treated with PACAP-38 increased VIP gene expression and this expression was a function of cAMP/PKA activation [53]. All PAC1SVs treated with PACAP-38 increased stanniocalcin (STC1) expression which was dependent on ERK but not PKA activation [52]. The results indicate that the mechanism by which PAC1 alters gene expression is a function of the gene product.
PACAP has a biphasic dose–response curve on neuroblastoma cells with stimulation of proliferation at low nM concentrations and inhibition of proliferation at high μM concentrations [54]. Stimulation of proliferation was mediated by the MAP kinase pathway whereas inhibition of proliferation was mediated by PKA. PAC1 and PACAP mRNA were detected in numerous neuroblastoma tumors and cell lines [55]. PACAP inhibited cell growth and induced morphological differentiation of neuroblastoma cells in a cAMP dependent manner [56, 57]. It remains to be determined if the ability of PACAP to alter cancer growth varies as a function of PAC1SV status.
PAC1 is present in numerous brain tumors including astrocytomas, ependymomas, glioblastomas, and neuroblastomas [55, 58]. PAC1 mRNA is present in U87, U138, and U373 human glioblastoma cell lines [59]. Specific 125I-PACAP-27 binding was inhibited with high affinity by PACAP-27 but not VIP (IC50 values of 10 and 1500 nM, respectively). Addition of 30 nM PACAP-27 to U87 cells elevated the cAMP and cytosolic Ca2+. Addition of 10 nM PACAP-27 stimulated the clonal growth of human U87, U118, or U373 cells [59]. Also PACAP stimulated the proliferation of rat C6 glioma cells [60]. PACAP bound with high affinity to 70 % of the astroglial neoplasms, ependymomas, and oligodendroglioma membranes examined [58] and elevated cAMP. When PACAP-27 or PACAP-38 is added to human glioblastoma T98G cells, which have VPAC2, proliferation is reduced [61]. VPAC2 regulates increases in cAMP but not cytosolic Ca2+.
Disruption of a single copy of the PACAP gene increased medulloblastoma incidence in ptc1 mutant mice 2.5-fold [62]. Ptc1 is a sonic hedgehog receptor gene which is overexpressed in humans and mice with medulloblastoma. PACAP reduced gli1 gene expression and proliferation of primary medulloblastoma tumor spheres in a PKA-dependent manner [63]. The results indicate that PAC1 is present in many brain cancers.
Neuroendocrine Tumors
PAC1 is present on many neuroendocrine tumors (NETs) and regulates prominent growth effects [15, 16, 64–66]. In BON cells, PAC1 is present and its activation increases cAMP, cytosolic Ca2+, ERK tyrosine phosphorylation, EGFR tyrosine phosphorylation, release of serotonin, and growth [64–66]. Gene expression profiling indicated that BON cells have numerous neuroendocrine markers including NSE, DDC, substance P, somatostatin 2 receptors, and muscarinic acetylcholine receptor [67]. PACAP plays a critical role in hypergastrinemia resulting in the proliferation of enterochromaffin cells [15, 16]. PAC1 is important in regulating the proliferation of NET cells especially those secreting insulin [68].
PACAP causes PC12 cells, a rat pheochromocytoma, to decrease proliferation, increase survival, and induce neurite outgrowth [69, 70]. After activation, PAC1 is translocated into caveolae and stimulates neuritogenesis through a cAMP-Rap-1 dependent pathway [71, 72]. PACAP causes PC12 cellular differentiation through the ERK/MAPK cascade [73]. PACAP addition to PC12 adrenal pheochromocytoma cells increases the cAMP [74] and causes catecholamine secretion [75]. PAC1hop facilitated catecholamine secretion through 2-ABP-sensitive Ca2+ channels in PC12 cells [76].
PACAP addition to PC12 cells increases TrkA tyrosine phosphorylation [77, 78]. When PACAP was added to PC12 cells, Akt was phosphorylated in a TrkA-dependent manner. The TrkA and Akt phosphorylation caused by PACAP was reversed by the TKI K252a. Also, TrkA transactivation caused by PACAP was inhibited by PP1, an inhibitor of Src. Neuronal differentiation was stimulated by PACAP which activated Galpha/cAMP/exchange protein (Epac) in a cAMP-dependent manner utilizing Rit guanine nucleotide exchange factor [79]. The PACAP-mediated Rit activation involves the Src family kinase-dependent TrkA receptor transactivation. Addition of the Src inhibitor PP1 inhibited the ability of PACAP to cause Rit activation in a TrkA-dependent manner. The increase in TrkA and Akt tyrosine phosphorylation occurred 10 min after addition of PACAP-38 to PC12 cells. Further PACAP promotes survival and neuritogenesis in PC12 cells through the NF-kB pathway [80]. The results indicate that PAC1 regulation of Trk-A phosphorylation is essential for Epac to activate Rit GTPase leading to neuronal differentiation.
Prostate Cancer
PACAP and PAC1 immunoreactivity are present in prostate tissue [81]. In prostate cancer tissues anti-PAC1 antibody stained the apical portion of the prostate cancer cells. By RT-PCR, PAC1null mRNA was more abundant than PAC1SV1 or PAC1SV2. Addition of PACAP-27 of PACAP-38 to prostate cancer biopsy specimens increased adenylyl cyclase activity [82]. PACAP-27, PACAP-38, and PACAP(6–38) inhibited specific binding of 125I-PACAP-27 to PC-3 cells with IC50 values of 15, 10, and 300 nM, respectively [21]. PACAP-27 (1 nM) addition to PC-3 cells increased the cAMP threefold which was antagonized significantly by 1 μM PACAP(6–38). Addition of 10 nM PACAP-27 significantly increased PC-3 colony number which was antagonized by 1 μM PACAP(6–38). Injection of 0.4 mg/kg of PACAP(6–38) into nude mice significantly reduced xenograft proliferation by 50 %. Treatment of LNCaP cells with PACAP-27 short-term stimulated proliferation whereas chronic treatment resulted in elevated cAMP resulting in proliferation arrest and neuroendocrine differentiation [83]. Because PACAP binds with high affinity to membranes derived from human benign hyperplastic prostate, VPAC and PAC1 may be expressed early in the carcinogenic process [84].
Pituitary Tumors
PACAP regulates hormone secretion and cell proliferation in pituitary tumor cells. In human pituitary adenoma HP75 cells, PACAP-27 or PACAP-38 inhibits TGF-β induced apoptosis [85]. In human pituitary adenomas, PACAP administration increased ACTH release from three corticotrope tumors as well as GH release from a somatotrope tumor [86]. In mouse pituitary corticotroph AtT20 cells, nM concentrations of PACAP-27 or PACAP-38 increased cAMP, POMC gene transcription and ACTH release [87, 88]. PACAP addition to rat lactotrope 235–1 cells increases PRL release to 260 % and increases proliferation to 162 % [89]. PACAP stimulates LH and FSH release from gonadotrophinomas and potentiated the effects of TRH [90]. PACAP-27 or PACAP-38 addition to lactotrope/somatotrope rat GH3 cells increased PRL and GH release [91]. PACAP increases PRL mRNA is a cAMP/PKA/ERK dependent mechanism [92]. PACAP addition to somatolactotrope BH5C1 cells increase PRL gene expression in a cAMP/PKA/ERK/Rap1 dependent manner [93].
Breast Cancer
A 19.9 kDa prepro-PACAP was detected in human breast cancer biopsy specimens [26]. Also, a smaller molecular weight product was identified suggesting the prepro-PACAP can be processed by breast cancer cells. Also PAC1 null and PAC1 SV3 mRNA were present in breast cancer biopsy specimens [8]. Antibodies to PAC1 stained breast cancer biopsy specimens and recognized a 60-kDa protein [22]. PACAP-27, PACAP-38, and PACAP (6–38) inhibited specific 125I-PACAP-27 binding to T47D cells with IC50 values of 8, 17, and 750 nM respectively. Addition of 1 nM PACAP-27 to T47D cells increased the cAMP tenfold and the increase caused by PACAP-27 was significantly inhibited by 1 μM PACAP(6–38). PACAP(6–38) (0.4 mg/kg) inhibited significantly the growth of T47D xenografts in nude mice by 39 % [22].
A 99mTc-labeled VIP analog named TP-3645 has been developed to image tumors in breast cancer patients [94]. Subsequently a 64Cu-labeled VIP analog was developed named TP-3982 to image breast cancer patients [95]. It remains to be determined if a radiolabeled PACAP analog will be developed for early detection of cancer.
Pancreatic Cancer
The effects of PACAP were investigated on rat pancreatic carcinoma AR4-2J cells. Nanomolar concentration stimulated the growth and increased ornithine decarboxylase activity [17]. The effects of PACAP-27 on proliferation and ODC activity were reversed by the somatostatin analog SMS 201–995 or pertussis toxin. PACAP-27 addition to AR4-2J cells increased proliferation and PLD activity that was inhibited by SMS201-995 or wortmannin, a PI-3-K inhibitor [96]. The growth effects of PACAP on AR4-2J cells are preceded by increased expression of c-fos as well as c-jun [97]. The c-fos and c-jun activate the heterodimeric transcription factor AP-1. The effects of PACAP on c-fos/c-jun/AP-1 are reversed by PKC and PKA inhibitors as well as PACAP(6–38).
Colon Cancer
PACAP-38 immunoreactivity was detected in colon cancer biopsy specimens [27]. PAC1 was present in HCT8 human colonic tumor cell line HCT8 [14]. Addition of PACAP-38 to NCT8 cells increased the cAMP and cytosolic Ca2+ leading to increased proliferation. The effects of PACAP on HCT8 cells were antagonized by PACAP(6–38). The effects on PACAP on HCT8 cells on proliferation was impaired if the cells overexpressed PAC1SV1 [98]. Addition of PACAP-38 to the transfected cells increased cAMP but not cytosolic Ca2+ or proliferation. The results suggest that PACAP must cause PI turnover to increase colon cancer proliferation.
Other Cancers
In cervical cancer multiple cytosine guanine dinucleotides are found in the promoter region of the PACAP gene and these CpG sites are methylated early in the carcinogenic process [99]. It remains to be determined if methylation of the PACAP gene can be used for early detection of cervical cancer. Overexpression of the PACAP gene in cervical cancer cell lines reduced expression of secretory clusterin, an anti-apoptotic protein [100].
In human choriocarcinoma cell line JAR, PACAP facilitated the ability of hydrogen peroxide (H2O2) or CoCl2 to decrease survival [101]. Treatment of JAR cells with H2O2 plus PACAP decreased phosphorylation of Akt, p-38-MAPK and ERK. PACAP-38 or PACAP(6–38), however, it had little effect on the ability of methotrexate to cause apoptosis or necrosis of JAR cells [102]. The results suggest that PACAP may increase oxidative stress caused by H2O2.
In multiple myeloma proliferation of plasma cells in the bone marrow overproduce immunoglobulin light chains leading to secretion of interleukin 6 (IL-6) by bone marrow stromal cells (BMSC). PACAP suppressed light chain immunoglobulin myeloma release of IL-6 by BMSC [103]. PACAP infusion into the blood of a multiple myeloma patient increased the intravenous level of PACAP to 0.2 nM resulting in a reduction of immunoglobulin light chains in the urine. There were few side effects associated with the PACAP infusion and the half-life was approximately 5 min [104]. PACAP inhibited p38 MAPK and translocation of NFkappaB in renal proximal tubule cells [105]. PACAP-38 prevents renal injury in myeloma models in experimental animals. PACAP preserves renal function in a number of models of renal injury [106].
Summary
PACAP is a neuropeptide growth factor present in numerous cancers. PACAP stimulates the proliferation of both SCLC, a neuroendocrine tumor, and NSCLC, an epithelial tumor. PACAP-27 or PACAP-38, which can be derived from the precursor preproPACAP, binds with high affinity to PAC1, VPAC1, and VPAC2. Also, VIP, which is produced by SCLC and NSCLC cells, binds with high affinity to VPAC1 and VPAC2 but not PAC1. It is important to determine which ligand and which receptor regulates cancer proliferation.
For the first time, selective peptide agonists are now available for PAC1. (Iac1, Ala16,17, DLys38)PACAP-38 is a synthetic agonist which prefers PAC1 relative to VPAC1 by 50- to 80-fold and prefers PAC1 relative to VPAC2 by 10- to 50-fold [32]. Maxidilan is a 61-amino acid peptide from the sand fly is selective for PAC1, but has little sequence homology to PACAP and is not readily available [31]. (Lys17, Arg18, Leu27)VIP1-7GRF8-27 is a selective VPAC1 agonist and RO25-1553 is a selective VPAC2 agonist [105]. The selective peptide agonists can be used to determine which receptor regulates cancer cellular proliferation. For SCLC and NSCLC, PAC1 and VPAC1 but not VPAC2 agonists stimulated proliferation [107]. PACAP(6–38) is a peptide antagonist for PAC1. While it appears to be specific for PAC1 relative to VPAC1 or VPAC2, the IC50 value is in the μM range. Thus PACAP(6–38) will dissociate rapidly from PAC1. High affinity non-peptide antagonists for PAC1 are needed.
The signal transduction mechanisms for PACAP in cancer are complex. Figure 47.3 shows that PACAP addition to NSCLC cells increases cytosolic Ca2+ and activates PKC as well as PKA with seconds after addition to NSCLC cells. As a result Src is activated which leads to activation of MMP as well as PYK2, FAK, and paxillin phosphorylation leading to increased cellular motility, migration, and secretion. MMP metabolizes membrane-bound precursors into EGFR ligands such as TGFα, amphiregulin, and heparin binding-EGF [108]. When TGFα binds to NSCLC cells, proteins such as PI3K and the EGFR are tyrosine phosphorylated. PI3K activation leads to Akt and mTor phosphorylation leading to increased cellular survival and/or differentiation. The EGFR activates the Ras, Raf, MEK, ERK pathway, leading to increased cellular proliferation. When ERK or Creb are activated in the nucleus, gene expression is altered increasing proliferation. In NSCLC, PAC1 may regulate growth in an EGFR-dependent manner.
PAC1 signal transduction. Activated PAC1 can interact with Gαs stimulating adenylyl cyclase leading to elevated cAMP, PKA activation, Creb phosphorylation and altered gene expression. Activated PAC1 can interact with Gαq stimulating PLC causing PI turnover. The DAG activates PKC leading to Src phosphorylation whereas the IP3 causes Ca2+ release from the ER. Src can tyrosine phosphorylate FAK, paxillin, and PYK2, leading to altered cellular motility and migration. Src can activate MMP metabolizing TGFα from inactive precursors. The TGFα activates the EGFR leading to formation of homodimers with itself or heterodimers with HER2. This results in the tyrosine phosphorylation of the EGFR and protein substrates such as PI3K. The PI3K can activate PDK-1 leading to Akt and mTor phosphorylation increasing cellular survival. Also the EGFR can activate Ras and Raf leading to MEK and ERK tyrosine phosphorylation increasing cellular proliferation
In NSCLC, nM concentrations of PACAP increase colony number whereas higher concentrations have little effect [109]. The high concentration may chronically increase cAMP leading to cellular differentiation. Undifferentiated cancer cells growth rapidly, whereas proliferation is impaired when cells are differentiated. The role of PAC1 SVs in cancer cellular proliferation remains to be determined. In neuroblastoma PAC1 SVs exist in the N-terminal and well as IC loop3.
PACAP(6–38) is a PAC1 antagonist which inhibits NSCLC proliferation in vitro and in vivo. Unfortunately PACAP(6–38) is cytostatic in that when PACAP(6–38) administration was discontinued into nude mice, NSCLC tumors rapidly regrew. In contrast, the TKI gefitinib is cytotoxic for NSCLC cells. PACAP(6–38) potentiated the cytotoxicity of gefitinib in vitro. It remains to be determined if GPCR antagonists increase the potency of TKI in NSCLC patients.
Abbreviations
- AP:
-
Activator protein
- BB:
-
Bombesin
- DDC:
-
Dopa decarboxylase
- EC:
-
Extracellular
- EGFR:
-
Epidermal growth factor receptor
- ERK:
-
Extracellular signal-regulated kinase
- FAK:
-
Focal adhesion kinase
- GPCR:
-
G Protein coupled receptor
- IC:
-
Intracellular
- MEK:
-
Mitogen/extracellular signal-regulated kinase
- MMP:
-
Matrix metalloprotease
- NSE:
-
Neuron specific enolase
- PACAP:
-
Pituitary adenylate cyclase activating polypeptide
- PI:
-
Phosphatidyl inositol
- PK:
-
Protein kinase
- PL:
-
Phospholipase
- PRP:
-
PACAP related peptide
- PYK:
-
Proline-rich tyrosine kinase
- SCLC:
-
Small cell lung cancer
- SV:
-
Splice variant
- TGF:
-
Transforming growth factor
- TKI:
-
Tyrosine kinase inhibitor
- TM:
-
Transmembrane
- VEGF:
-
Vascular endothelial growth factor
- VIP:
-
Vasoactive intestinal peptide
References
Arimura A. Pituitary adenylate cyclase activating polypeptide (PACAP): discovery and current status of research. Regul Pept. 1992;37:287–303.
Sherwood NM, Krueckl SL, McRory JE. The origin and function of the pituitary adenylate cyclase activating polypeptide (PACAP)/glucagon superfamily. Endocr Rev. 2000;21:619–70.
Miyata A, Arimura A, Dahl RR, Minamino N, Uehara A, Jiang L, et al. Isolation of a novel 38 residue-hypothalamic polypeptide which stimulates adenylate cyclase in pituitary cells. Biochem Biophys Res Commun. 1989;164:567–74.
Miyata A, Jiang L, Dahl RD, Kitada C, Kubo K, Fujino M, et al. Isolation of a neuropeptide corresponding to the N-terminal 27 residues of the pituitary adenylate cyclase activating polypeptide with 38 residues (PACAP38). Biochem Biophys Res Commun. 1990;170:643–8.
Fahrenkrug J. VIP and PACAP. Results Probl Cell Differ. 2010;50:221–34.
Harmar AJ, Fahrenkrug J, Gozes I, Laburthe M, May V, Pisegna JR, et al. Pharmacology and functions of receptors for vasoactive intestinal peptide and pituitary adenylate cyclase –activating polypeptide. IUPHAR review 1. Br J Pharmacol. 2012;166:4–17.
Moody TW, Jensen RT. VIP and PACAP as autocrine growth factors in breast and lung cancer. In: Kastin AJ, editor. Handbook of biologically active peptides. Amsterdam: Elsevier; 2006. p. 493–8.
Moody TW, Chan D, Fahrenkrug J, Jensen RT. Neuropeptides as autocrine growth factors in cancer cells. Curr Pharm Des. 2003;9:495–509.
Pisegna J, Wank J. Cloning and characterization of the signal transduction of four splice variants of the human pituitary adenylate cyclase activation polypeptide receptor: evidence for dual coupling to adenylate cyclase and phospholipase C. J Biol Chem. 1996;271:17267–74.
Moody TW, Nuche-Berenguer B, Nakamura T, Jensen RT. EGFR transactivation by peptide G Protein-Coupled receptors in cancer. Curr Drug Targets. 2016;17(5):520–8.
Draoui M, Hida T, Jakowlew S, Birrer M, Zia F, Moody TW. PACAP stimulates c-fos mRNAs in small cell lung cancer cells. Life Sci. 1996;59:307–13.
Moody TW, Leyton J, Casibang M, Pisegna J, Jensen RT. PACAP-27 tyrosine phosphorylates mitogen activated protein kinase and increases VEGF mRNAs in human lung cancer cells. Regul Pept. 2002;109:135–40.
Nakamachi T, Sugiyama K, Watanabe J, Imai N, Kagami N, Hori M, et al. Comparison of expression and proliferative effect of pituitary adenylate cyclase-activating polypeptide (PACAP) and its receptors on human astrocytoma cell lines. J Mol Neurosci. 2014;54:388–94.
Le SV, Yamaguchi DJ, McArdle CA, Tachiki K, Pisegna JR, Germano P. PAC1 and PACAP expression, signaling and effect on the growth of HCT8 human colonic tumor cells. Regul Pept. 2002;109:115–25.
Lauffer JM, Modlin IMH, Inoue T, Kidd M, Zhang T, Schmid SW, et al. Pituitary adenylate cyclase-activating polypeptide modulates gastric enterochromaffin-like proliferation in rats. Gastroenterology. 1999;116:623–35.
Lauffer JM, Tang LH, Zhang T, Hinoue T, Rahbar S, Odo M, et al. PACAP mediates the neural proliferative pathway of Mastomys enterochromaffin-like cell transformation. Regul Pept. 2001;102:157–64.
Buscail L, Cambillau C, Seva C, Scemama JL, De Neef P, Robberecht P, et al. Stimulation of rat pancreatic tumoral AR4-2J cell proliferation by pituitary adenylate cyclase-activating peptide. Gastroenterology. 1992;103:1002–8.
Moody TW, Zia F, Makheja A. Pituitary adenylate cyclase activating polypeptide receptors are present on small cell lung cancer cells. Peptides. 1993;14:241–6.
Zia F, Fagarasan M, Bitar K, Coy DH, Pisegna JR, Wank SA, et al. Pituitary adenylate cyclase activating peptide receptors regulate the growth of non-small cell lung cancer cells. Cancer Res. 1995;55:4886–91.
Pisegna JR, Leyton J, Coelho T, Hida T, Jakowlew S, Birrer M, et al. PACAP hybrid: a new PACAP receptor antagonist. Life Sci. 1997;61:631–9.
Leyton J, Coelho T, Coy DH, Jakowlew S, Birrer MJ, Moody TW. PACAP(6-38) inhibits the growth of prostate cancer cells. Cancer Lett. 1998;125:131–9.
Leyton J, Gozes Y, Pisegna J, Coy D, Purdom S, Casibang M, et al. PACAP(6-38) is a PACAP receptor antagonist for breast cancer cells. Breast Cancer Res Treat. 1999;56:177–86.
Reubi JC. In vitro evaluation of VIP/PACAP receptors in healthy and diseased human tissues. Clinical implications. Ann N Y Acad Sci. 2000;921:1–25.
Reubi JC, Laderach U, Waser B, Gebbers JO, Robberecht P, Laissue JA. Vasoactive intestinal peptide/pituitary adenylate cyclase-activating peptide receptor subtypes in human tumors and their tissues of origin. Cancer Res. 2000;60:3105–12.
Schultz S, Rocken C, Mawrin C, Weise W, Holit V, Schulz S. Immunocytochemical identification of VPAC1, VPAC2 and PAC1 receptors in normal and neoplastic human tissues with subtype-specific antibodies. Clin Cancer Res. 2004;10:8235–42.
Garcia-Fernandez MA, Bodega G, Ruiz-Villaespesa A, Cortes J, Prieto JC, Carmena MJ. PACAP expression and distribution in human breast cancer and healthy tissue. Cancer Lett. 2004;205:189–95.
Szanto Z, Sarszegi Z, Reglodi D, Nemeth J, Szabadfi K, Kiss P, et al. PACAP immunoreactivity in human malignant tumor samples and cardiac diseases. J Mol Neurosci. 2012;48:667–73.
Kaufman J, Horn L, Carbone D. Molecular biology of lung cancer. In: DeVita Jr V, Lawrence TS, Rosenberg SA, editors. Cancer: principles and practice of oncology. Williams & Wilkins Philadelphia, PA: Lippincott; 2011. p. 789–98.
Carney DN, Gazdar AF, Bepler G, Guccion JG, Marangos PJ, Moody T, et al. Establishment and identification of small cell lung cancer cell lines having classic and variant features. Cancer Res. 1985;45:2913–23.
Moody TW, Walters J, Casibang M, Zia F, Gozes Y. VPAC1 receptors and lung cancer. Ann N Y Acad Sci. 2000;921:26–32.
Lerner EA, Iuga AO, Reddy VB. Maxadilan, a PAC1 receptor agonist from sand flies. Peptides. 2007;28:1651–4.
Ramos-Alvarez I, Mantey SA, Nakamura T, Nuche-Berenguer B, Moreno P, Moody TW, et al. A structure-function study of PACAP using conformationally restricted analogs: identification of PAC1 receptor-selective PACAP agonists. Peptides. 2015;66:26–42.
Bourgault S, Vaudry D, Botia B, Couvineau A, Laburthe M, Vaudry H, et al. Novel stable PACAP analogs with potent activity towards the PAC1 receptor. Peptides. 2008;29:919–32.
Wray B, Kakoschke C, Nokihara K, Naruse S. Solution structure of pituitary adenylate cyclase activating polypeptide by nuclear magnetic resonance spectroscopy. Biochemistry (Mosc). 1993;32:5832–41.
Sun C, Song D, Davis-Taber RA, Barrett LW, Scott VE, Richardson PL, et al. Solution structure and mutational analysis of pituitary adenylate cyclase-activating polypeptide binding to the extracellular domain of PAC1-R. Proc Natl Acad Sci U S A. 2007;104:7875–80.
Furness SG, Wootten D, Christopoulos A, Sexton PM. Consequences of splice variation on secretin family G protein coupled receptor function. Br J Pharmacol. 2012;166:98–109.
Pisegna JR, Wank SA. Molecular cloning and functional expression of the pituitary adenylate cyclase-activating polypeptide type 1 receptor. Proc Natl Acad Sci U S A. 1993;90:6345–9.
Spengler D, Waeber C, Pantaloni C, Holsboer F, Bochaert J, Seeberg PH, et al. Differential signal transduction by five slice variants of the PACAP receptor. Nature. 1993;365:170–5.
Pisegna JR, Moody TW, Wank SA. Differential signalling and immediate-early gene activation by four splice variants of the human pituitary adenylate cyclase activating polypeptide receptor. In: Arimura A, editor. VIP, PACAP and related regulatory peptides. Ann N Y Acad Sci. 1996;805:54–64.
Moody TW, Leyton J, Jensen RT. Pituitary adenylate cyclase-activating polypeptide causes increased tyrosine phosphorylation of focal adhesion kinase and paxillin. J Mol Neurosci. 2012;46:68–74.
Hanks SK, Calalb MD, Harper MC, Patel SK. Focal adhesion protein-tyrosine phosphorylation in response to cell attachment to fibronectin. Proc Natl Acad Sci U S A. 1992;89:8487–91.
Moody TW, diFlorio A, Jensen RT. PYK-2 is tyrosine phosphorylated after activation of pituitary adenylate cyclase activating polypeptide receptors lung cancer cells. J Mol Neurosci. 2012;48:660–6.
Bellis SL, Perotta JA, Curtis MS, Turner CE. Adhesion of fibroblasts to fibronectin stimulates both serine and tyrosine phosphorylation of paxillin. Biochem J. 1997;325:375–81.
Moody TW, Osefo N, Nuche-Berenguer B, Ridnour L, Wink D, Jensen RT. Pituitary adenylate cyclase activating polypeptide causes tyrosine phosphorylation of the EGF receptor in lung cancer cells. J Pharmacol Exp Ther. 2012;341:873–81.
Lemmon MA, Schlessinger J. Cell signaling by receptor tyrosine kinases. Cell. 2010;141:1117–34.
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–39.
Paez JG, Janne PA, Lee JC, Tracey S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–500.
Lutz EM, Ronaldson E, Shaw P, Johnson MS, Holland PJ, Mitchell R. Characterization of novel splice variants of the PAC1 receptor in human neuroblastoma cells: consequences for signaling by VIP and PACAP. Mol Cell Neurosci. 2006;31:193–209.
Blechman J, Levkowitz G. Alternative splicing of the pituitary adenylate cyclase-activating polypeptide receptor PAC1: mechanisms of fine tuning of brain activity. Front Endocrinol. 2013;4:55.
Ushiyama M, Ikeda R, Sugawara H, Yoshida M, Mori K, Kangawa K, et al. Differential intracellular signaling through PAC1 isoforms as a result of alternative splicing in the first extracellular domain and the third intracellular loop. Mol Pharmacol. 2007;72:103–11.
Ushiyama M, Ikeda R, Yoshida M, Mori K, Kangawa K, Sugarwara H, et al. Alternative splicing of the pituitary adenylate cyclase-activating polypeptide (PACAP) receptor contributes to the function of PACAP-27. J Mol Neurosci. 2010;42:341–8.
Holighaus Y, Mustafa T, Eiden LE. PAC1hop, null and hip receptors mediate differential signaling through cyclic AMP and calcium leading to splice variant specific gene induction in neural crest cells. Peptides. 2011;32:1647–55.
Falktoft B, Georg B, Fahrenkrug J. Signaling pathways in PACAP regulation of VIP gene expression in human neuroblastoma cells. Neuropeptides. 2009;43:53–61.
Lelievre V, Pineau N, Du J, Wen CH, Nguyen T, Janet T, et al. Differential effects of peptide histidine isoleucine (PHI) and related peptides on stimulation and suppression of neuroblastoma cell proliferation. J Biol Chem. 1998;273:19685–90.
Vertongen P, Devaick C, Sariban E, De Laet MH, Martelli H, Paraf F, et al. Pituitary adenylate cyclase activating peptide and its receptors are expressed in human neuroblastomas. J Cell Physiol. 1996;167:36–46.
Hoshino M, Li M, Zheng LQ, Suzuki M, Mochizuki T, Yanaihara N. Pituitary adenylate cyclase activation peptide and vasoactive intestinal polypeptide: differentiation effects on human neuroblastoma NB-OK-1 cells. Neurosci Lett. 1993;159:35–8.
Monaghan TK, Pou C, MacKenzie CJ, Plevin R, Lutz EM. Neurotropic actions of PACAP-38 and LIF on Human neuroblastoma SH-SY5Y cells. J Mol Neurosci. 2008;36:45–56.
Robberecht P, Woussen-Colle MC, Vertongen P, De Neef P, Hou X, Salmon I, et al. Expression of pituitary adenylate cyclase activating polypeptide (PACAP) receptors in human glial cell tumors. Peptides. 1994;15:661–5.
Sharma A, Walters J, Gozes Y, Fridkin M, Brenneman D, Gozes I, et al. A vasoactive intestinal peptide antagonist inhibits the growth of glioblastoma cells. J Mol Neurosci. 2001;17:331–9.
Dufes C, Alleaume C, Montoni A, Olivier JC, Muller JM. Effects of the vasoactive intestinal peptide (VIP) and related peptide on glioblastoma cell growth in vitro. J Mol Neurosci. 2003;21:91–102.
Vertongen P, Camby I, Darro F, Kiss R, Robberecht P. VIP and pituitary adenylate cyclase activating polypeptide (PACAP) have an antiproliferative effect on the T98G human glioblastoma cell line through interaction with VIP2 receptor. Neuropeptides. 1996;30:491–6.
Lelievre V, Seksenyan A, Nobuta H, Yong HW, Chhith S, Niewiadomski P, et al. Disruption of the PACAP gene promotes medulloblastoma in ptc1 mutant mice. Dev Biol. 2008;313:359–70.
Cohen JR, Resnick DZ, Niewiadomski P, Dong H, Liau LM, Waschek JA. Pituitary adenylyl cyclase activating polypeptide inhibits gli1 gene expression and proliferation in primary medulloblastoma derived tumorsphere cultures. BMC Cancer. 2010;10:676.
Lieu SN, Oh DS, Pisegna JR, Germano PM. Neuroendocrine tumors express PAC1 receptors. Ann N Y Acad Sci. 2006;1070:399–404.
Germano PM, Lieu SN, Xue J, Cooke HJ, Christiofi GL, Lu Y, et al. PACAP induces signaling and stimulation of 5-hydroxytrypamine release and growth in neuroendocrine tumor cells. J Mol Neurosci. 2009;39:391–401.
DiFlorio A, Sancho V, Moreno P, Delle Fave G, Jensen RT. Gastrointestinal hormones stimulate growth of foregut neuroendocrine tumors by transactivating the EGF receptor. Biochim Biophys Acta. 1833;2013:573–82.
Siddique ZL, Drozdov I, Floch J, Gustafsson BI, Stunes K, Pfragner R, et al. KRJ-I and BON cell lines: defining an appropriate enterochromaffin cell neuroendocrine tumor model. Neuroendocrinology. 2009;89:458–70.
Andersson M, Sillard R, Rokaeus A. Demonstration of [125]VIP binding sites and effects of VIP on cAMP-formation in rat insulinoma (RINm5F and RIN14B) cells. Regul Pept. 1992;40:41–9.
Deutsch PJ, Sun Y. The 38 amino acid pituitary adenylate cyclase activating polyeptide stimulates dual signaling cascades in PC12 cells and promotes neurite outgrowth. J Biol Chem. 1992;267:5108–13.
Vaudry D, Falluel-Morel A, Bourgault S, Basille M, Burel D, Wurtz O, et al. Pituitary adenylate cyclase-activating polypeptide and its receptors: 20 years after the discovery. Pharmacol Rev. 2009;61:283–357.
Zhang W, Duan W, Cheung NS, Huang Z, Shao K, Li QT. Pituitary adenylate cyclase activating polypeptide induces translocation of its G-protein coupled receptor into caveolin-enriched membrane microdomains, leading to enhanced cyclc AMP generation and neurite outgrowth in PC12 cells. J Neurochem. 2007;103:1157–67.
Ravni A, Bourgault S, Lebon A, Chan P, Galas L, Fournier A, et al. The neurotrophic effects of PACAP in PC12 cells: control by multiple transduction pathways. J Neurochem. 2006;98:321–9.
Vaudry D, Stork PJ, Lazarovici P, Eiden LE. Signaling pathways for PC12 cell differentiation: making the right connections. Science. 2002;296:1648–9.
Watanabe T, Ohtaki T, Kitada C, Tsuda M, Fujino M. Adrenal pheochromocytoma PC12 cells respond to pituitary adenylate cyclase-activating polypeptide. Biochem Biophys Res Commun. 1990;173:252–8.
Taupenot L, Mahata M, Mahata SK, O’Connor DT. Time-dependent effects of the neuropeptide PACAP on catecholamine secretion: stimulation and desensitization. Hypertension. 1999;34:1152–62.
Mustafa T, Walsh J, Grimaldi M, Eiden LE. PAC1hop receptor activation facilitates catecholamine secretion selectively through 2-APB-sensitive Ca(2+) channels in PC12 cells. Cell Signal. 2010;22:1420–6.
Lee FS, Rajagopal R, Kim AH, Chang PC, Chao MV. Activation of Trk neurotrophin receptor signaling by pituitary adenylate cyclase-activating polypeptides. J Biol Chem. 2002;277:9096–102.
Rajagopal R, Chen ZY, Lee FS, Chao MV. Transactivation of Trk neurotrophin receptors by G-protein-coupled receptor ligands occurs on intracellular membranes. J Neurosci. 2004;24:6650–8.
Shi GX, Jin L, Andres DA. Src-dependent TrkA transactivation is required for pituitary adenylate cyclase-activating polypeptide 38-mediated Rit activation and neuronal differentiation. Mol Biol Cell. 2010;21:1597–608.
Manecka DL, Mahmood SF, Grumolato L, Lihrmann I, Anouar Y. Pituitary adenylate cyclase-activating polypeptide (PACAP) promotes both survival and neuritogenesis in PC12 cells through activation of nuclear factor KB (NF-kB) pathway: involvement of extracelluar signal regulated kinase (ERK), calcium and c-REL. J Biol Chem. 2013;288:14936–48.
Mammi C, Frajese GV, Vespasiani G, Mariani S, Gnessi L, Farini D, et al. PAC1-R null isoform expression in human prostate cancer tissue. Prostate. 2006;66:514–21.
Garcia-Fernandez MO, Solano RM, Carmena MJ, Busto R, Bodega G, Ruiz-Villaespesa A, et al. Expression of functional PACAP/VIP receptors in human prostate cancer and healthy tissue. Peptides. 2003;24:893–902.
Farini D, Puglianiello A, Mammi C, Siracusa G, Moretti C. Dual effect of pituitary adenylate cyclase activating polypeptide on prostate tumor LNCaP cells: Short and long-term exposure affect proliferation and neuroendocrine differentiation. Endocrinology. 2003;144:1632–43.
Solano RM, Carmena MJ, Carrero I, Cavallaro S, Roman F, Hueso C, et al. Characterization of vasoactive intestinal peptide/pituitary adenylate cyclase-activating peptide receptors in human benign hyperplastic prostate. Endocrinology. 1996;137:2815–22.
Oka H, Jin L, Kulig E, Scheithauer BW, Lloyd RV. Pituitary adenylate cyclase- activating polypeptide inhibits transforming growth factor-beta 1 induced apoptosis in a human pituitary adenoma cell line. Am J Pathol. 1999;155:1893–900.
Desai BJ, Monson JP, Holdstock JG, Aylwin SJ, Geddes JF, Wood DF, et al. Effects of pituitary adenylate cyclase-activating polypeptide on hormone secretion by human pituitary adenomas in vitro. J Clin Endocrinol Metab. 1994;79:1771–7.
Koch B, Lutz-Bucher B. Vasopressin, unlike phorbol ester, fails to synergistically interact with pituitary adenylate cyclase activating polypeptide (PACAP) in stimulating cyclic AMP formation and ACTH secretion in cultured anterior pituitary cells. Mol Cell Endocrinol. 1993;92:175–81.
Boutillier AL, Monnier D, Koch B, Loeffler JP. Pituitary adenyl cyclase-activating polypeptide: a hypophysiotropic factor that stimulates proopiomelanocortin gene transcription and proopiomelanocortin-derived peptide secretion in corticotropic cells. Neuroendocrinology. 1994;60:493–502.
Hammond PJ, Smith DM, Akinsanya KO, Mufti WA, Wynick D, Bloom SR. Signalling pathways mediating secretory and mitogenic responses to galanin and pituitary adenylate cyclase-activating polypeptide in the 235-1 clonal rat lactotroph cell line. J Neuroendocrinol. 1996;8:457–64.
Peterson B, Buchfelder M, Fahlbusch R, Adams EF. Pituitary adenylate cyclase-activating polypeptide directly stimulates LH and FSH secretion by human pituitary gonadotrophinomas. Exp Clin Endocrinol Diabetes. 1996;104:250–5.
Propato-Mussafiri R, Kanse SM, Ghatei MA, Bloom SR. Pituitary adenylate cyclase activating-polypeptide releases 7B2, adrenocorticotrophin, growth hormone and prolactin from the mouse and rat clonal pituitary cell lines AtT-20 and GH3. J Endocrinol. 1992;132:107–13.
Yonehara T, Kanasaki H, Yamamoto H, Fukunaga K, Miyazaki K, Miyamoto E. Involvement of mitogen-activated protein kinase in cyclic adenosine 3′,5′monophosphate induced hormone gene expression in rat pituitary GH(3) cells. Endocrinology. 2001;142:2811–9.
Romano D, Magalon K, Ciampini A, Talet C, Enjalbert A, Gerard C. Differential involvement of the Ras and Rap1 small GTPases in vasoactive intestinal and pituitary adenylyl cyclase activating polypeptide control of the prolactin gene. J Biol Chem. 2003;278:51386–94.
Pallela VR, Thakur ML, Chakder S, Rattan S. 99mTc-labeled vasoactive intestinal peptide receptor agonist: functional studies. J Nucl Med. 1999;40:352–60.
Zhang K, Aruva MR, Shanthly N, Cardi CA, Patel CA, Rattan S, et al. Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase activating peptide (PACAP) receptor specific peptide analogues for PET imaging of breast cancer: In vitro/in vivo evaluation. Regul Pept. 2007;144:91–100.
Morisset J, Douziech N, Rydzewska G, Buscail L, Rivard N. Cell signaling pathway involved in PACAP-induced AR4-2J cell proliferation. Cell Signal. 1995;7:193–205.
Schafer H, Zheng J, Gundlach F, Gunther R, Schmidt WE. PACAP stimulates transcription of c-fos and c-jun and activates the AP-1 transcription factor in rat pancreatic carcinoma cells. Biochem Biophys Res Commun. 1996;221:111–6.
Germano PM, Le SV, Oh DS, Fan R, Lieu S, Siu A, et al. Differential coupling of the PAC1 SV1 splice variant on human colonic tumors to the activation of intracellular cAMP but not intracellular Ca2+ does not activate tumor proliferation. J Mol Neurosci. 2004;22:83–92.
Jung S, Yi L, Jeong D, Kim J, An S, Oh TJ, et al. The role of ADCYAP1, adenylate cyclase activating polypeptide 1, as a methylation biomarker for the early detection of cervical cancer. Oncol Rep. 2011;25:245–52.
Lee JH, Lee JY, Tho SB, Choi SJ, Lee DG, An S, et al. PACAP inhibits tumor growth and interferes with clusterin in cervical carcinomas. FEBS Lett. 2014;588:4730–9.
Boronkai A, Brubel R, Racz B, Tamas A, Kiss P, Horvath G, et al. Effects of pituitary adenylate cyclase activating polypeptide on the survival and signal transduction pathways in human choriocarcinoma cells. Ann N Y Acad Sci. 2009;1163:353–7.
Brubel R, Bornokai A, Reglodi D, Racz B, Nemeth J, Kiss P, et al. Changes in the expression of pituitary adenylate cyclase activating polypeptide in the human placenta during pregnancy and its effects on the survival of JAR choriocarcinoma cells. J Mol Neurosci. 2010;42:450–8.
Li M, Cortez S, Nakamachi T, Batuman V, Arimura A. Pituitary adenylate cyclase-activating polypeptide is a potent inhibitor of the growth of light chain-secreting human multiple myeloma cells. Cancer Res. 2006;66:8796–803.
Li M, Maderdrut JL, Lertora JJ, Batuman V. Intravenous infusion of pituitary adenylate cyclase-activating polypeptide (PACAP) in a patient with multiple myeloma and myeloma kidney: a case study. Peptides. 2007;28:1891–5.
Arimura A, Li M, Batuman V. Treatment of renal failure associated with multiple myeloma and other diseases by PACAP-38. Ann N Y Acad Sci. 2006;1070:1–4.
Arimura A, Li M, Batuman V. Potential protective action of pituitary adenylate cyclase-activating polypeptide. Blood. 2006;107:681–8.
Gourlet P, Vertongen P, Vandermeer P, Vandermeer-Pirot MC, Rathe J, DeNeef P. The long-lasting vasoactive intestinal polypeptide agonist RO 25-1553 is highly selective of the VIP2 receptor subclass. Peptides. 1997;18:403–8.
Bhola NE, Grandis JR. Crosstalk between G-protein-coupled receptors and epidermal growth factor receptor in cancer. Front Biosci. 2008;13:1857–65.
Moody TW, Gozes I. Vasoactive intestinal peptide receptors: a molecular target in breast and lung cancer. Curr Pharm Design. 2007;13:1099–104.
Acknowledgements
This research is supported by the intramural program on NCI and NIDDK of the NIH.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Moody, T.W., Jensen, R.T. (2016). PACAP and Cancer. In: Reglodi, D., Tamas, A. (eds) Pituitary Adenylate Cyclase Activating Polypeptide — PACAP. Current Topics in Neurotoxicity, vol 11. Springer, Cham. https://doi.org/10.1007/978-3-319-35135-3_47
Download citation
DOI: https://doi.org/10.1007/978-3-319-35135-3_47
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-35133-9
Online ISBN: 978-3-319-35135-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)