Abstract
Despite years of intense research, acute ischemic stroke remains a leading cause of death and long-term disabilities worldwide. Although preclinical studies lead to the identification of over 1000 potential neuroprotective compounds, the current treatments for brain ischemia only rely on clot thrombolysis through injection of recombinant-tissue plasminogen activator (r-tPA) or mechanical revascularization, which benefit to less than 10 % of stroke victims due to a narrow therapeutical time window and side effects. Consequently, there is a crucial need for the identification of new molecules and the development of other strategies that could target later phases of the pathophysiological cascade of mechanisms following stroke. Indeed, because stroke initiates a complex series of pathophysiological events evolving both in time and location, putative therapeutic molecules need to be effective on several of the biochemical processes evoked by stroke. Pituitary adenylate cyclase-activating polypeptide (PACAP) has been reported to decrease infarct volume and improve functional recovery in several models of global and focal brain ischemia. The unique particularity of PACAP relies on its ability to act on various pathological processes of cerebral ischemia. PACAP can counteract excitotoxicity, inhibit apoptosis, reduce oxidative stress, modulate inflammation, and promote brain repair mechanisms. Nevertheless, due to several limitations, the pertinence of a potential therapeutical use of PACAP is still under investigation to successfully ensure the bench to bedside continuum.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Brain Stroke
Definition and Epidemiology
Stroke is a cerebrovascular accident caused by an abrupt reduction of cerebral blood flow (CBF) generating irreversible cerebral tissue damages. Although stroke can sometimes be due to intracerebral hemorrhage, the ischemic origin accounts for 87 % of the cases and results from the occlusion of an arterial cerebral vessel responsible for sudden focal neurological deficits. According to the World Health Organization, stroke encompasses the transient ischemic attack defined as neurological deficits disappearing spontaneously in less than 1 h without neither sequel nor brain imaging abnormalities, and the acute ischemic stroke (AIS) corresponding to clinical symptoms persisting beyond 24 h which will be in the scope of this review article.
In the United States, 795,000 Americans experience a new or recurrent stroke with 610,000 first-ever cases each year. It represents one stroke victim every 40 s and it is responsible for one death every 4 min. We assume that 6.6 million Americans already experienced a stroke event, an estimated stroke prevalence of 2.6 % on the 2009–2012 period. Stroke is considered as the third cause of death after heart diseases and cancer, the second cause of dementia after Alzheimer’s disease, and the first cause of nontraumatic acquired disability in adults. The consequences after cerebral ischemia vary, but are often dramatic. Mortality rate was 20 % at 1 month and from 32 to 60 % after 3 years. While 25 % of patients recover without apparent sequel, 75 % of stroke survivors have various physical and psychological handicaps depending on the location and severity of the lesions. Among people bearing irreversible deficits, 30 % will not be autonomous in their daily activities and 40 % will not be able to resume their work. The management of stroke victims represents therefore a significant societal cost. In Europe, about 3–4 % of public health expenditures are dedicated to stroke, which represents a total of 64 billion € each year [1, 2]. The incidence and prevalence of stroke being closely associated with the aging of the population in industrialized countries, the projections for 2030 foresee a 20.5 % increase in prevalence of stroke in the United States [3]. Thus, it becomes obvious that stroke victims will represent a major public health and economic concerns.
Pathophysiology
Representing 2 % of the total body weight but consuming 20 % of cardiac output, the brain is particularly dependent on the continuous supply of oxygen and nutrients. The transient or permanent decrease in CBF observed in stroke results in 30 % of cases from occlusion of the middle cerebral artery (MCA) or one of its collaterals. The consecutive energetic depletion initiates a complex series of pathophysiological events, which evolve in a spatiotemporal fashion and lead to a massive and progressive neurodegeneration responsible for disabling functional deficits [4].
From the spatial point of view, the hypoperfusion gradient from the periphery to the ischemic core delimits two distinct zones. The ischemic core, where energy supply is insufficient to allow cell survival, is the location of rapid and irreversible cell death, whereas the penumbra area, surrounding the ischemic core, is defined as an electrically silent but metabolically active tissue, thanks to the presence of arterial collaterals sufficient to support cell survival at least for a short period of time.
From the temporal point of view, the cascade of pathophysiological events responsible for the extension of the lesions, spreading from the ischemic core toward the penumbra, can be seen as a set of entangled processes taking place in two phases: an acute phase occurring during the first hours after the occlusion which mainly involves excitotoxic and oxidative stress processes, and a chronic phase developing over days and weeks after the stroke onset which includes apoptotic and inflammatory mechanisms. All these events lead to cerebral infarction whose size and location determine the nature and severity of the neurological deficits among stroke’s victims.
Despite years of intense research and preclinical identification of numerous potential neuroprotective compounds, the current treatments for brain ischemia only rely on clot thrombolysis through injection of recombinant-tissue plasminogen activator (r-tPA) or mechanical revascularization. However, these treatments benefit to less than 10 % of stroke victims due to a narrow therapeutical time window and side effects [5]. Consequently, there is a crucial need for the development of other strategies that could target the overall pathophysiological cascade of events following stroke in the acute and chronic phases.
The PACAPergic System, an Endogenous Mechanism for Cell Protection After Stroke
The PACAPergic System
Pituitary adenylate cyclase-activating polypeptide (PACAP) was first isolated by Arimura and his colleagues from ovine hypothalamus extracts on the basis of its capacity to stimulate adenylate cyclase activity [6]. This neuropeptide exists in two forms, with a 38-amino acid peptide (PACAP38) and a truncated 27-residue fragment (PACAP27). PACAP, which exhibits 68 % sequence identity with vasoactive intestinal peptide (VIP), was classified as a member of the secretin/glucagon/growth hormone-releasing hormone (GHRH) superfamily [7]. Interestingly, the biologically active region of PACAP, i.e., its N-terminal part, has been highly conserved during evolution, from fish to mammals, suggesting that this neuropeptide must exert essential biological functions.
PACAP binds to three different seven-transmembrane G protein-coupled receptors named by the International Union of Pharmacology PAC1, VPAC1, and VPAC2 receptors according to their respective affinity toward PACAP and VIP [8]. Indeed PAC1 receptor exhibits a high affinity for both PACAP isoforms and a much lower affinity for VIP [9] whereas VPAC1 and VPAC2 receptors show similar affinity for PACAP and VIP [7]. More detailed information on PACAP and its receptors has already been published and is available in other published reviews [7, 10].
Several studies have reported the wide distribution of PACAP and its receptors in the central nervous system (CNS) and in peripheral tissues, supporting the hypothesis that PACAP exerts important biological activities. In fact, in the developing brain, PACAP exerts neurotrophic effects by modulating cell proliferation [11, 12], enhancing neuronal differentiation [13, 14] and blocking apoptosis [15–17]. In peripheral organs, PACAP has a strong dilatory activity on the vascular system [18] and bronchi [19]. Moreover, in vitro and in vivo studies have revealed that PACAP acts as a potent regulator of the immune system, exerting a general anti-inflammatory effect on innate [20, 21] and adaptive responses [21–23]. Altogether, these data indicate that PACAP is a unique neuropeptide which acts through a complex interplay of cellular and molecular mechanisms to inhibit cell death, promote neurotrophic activities, and regulate inflammatory responses.
Endogenous PACAP Expression After Cerebral Ischemia
Several studies have shown that PACAP expression is rapidly upregulated after brain artery occlusion, suggesting that the neuropeptide may play a role in the early pathophysiological events of ischemia. In a permanent model of MCA occlusion (MCAO), Stumm et al. have identified a biphasic regulation of PACAP in rat cortical pyramidal cells. They demonstrated that PACAP mRNA level in the fronto-parietal cortex was increased by 95 % 6 h after artery occlusion but was reduced by 74 % 2 days after ischemia as compared with sham-operated animals [24]. A similar pattern of expression was also observed after transient MCAO in mice with an increase of PACAP mRNA by 251 % after 6 h [24], suggesting that the rapid upregulation of PACAP is independent of the stroke model. In accordance with this hypothesis, an increase of PACAP transcript is also observed in a mouse model of global ischemia, with a very strong elevation of PACAP mRNA expression in the granule cell layer of the dentate gyrus of the hippocampus 1 and 3 days after stroke [25]. According to these reports, PACAP mRNAs are essentially localized in cortical and pyramidal neurons [24, 25], suggesting that neurons are the main source of PACAP after stroke. Nevertheless, recent data revealed that in the penumbral region, PACAP upregulation is not restricted to neurons but can also be observed in astrocytes and endothelial cells. Interestingly, some blood-derived CD34+ cells may also produce the neuropeptide upon infiltration in ischemic brain regions and can contribute to the elevated PACAP expression observed in human brain samples from patients who died 1–3 days after stroke [26]. Finally, the importance of endogenous PACAP expression in stroke models has been highlighted in PACAP-deficient mice which exhibit increased infarct volumes and functional deficits when compared to their control littermates [27, 28].
Although the molecular mechanisms of PACAP upregulation are still unclear, it is likely that PACAP may be expressed in response to stress-related environmental factors appearing in ischemic conditions. Stumm et al. showed that PACAP upregulation is mediated by the activation of the NMDA receptor and excessive glutamatergic neurotransmission, a hallmark of the initial ischemic cascade [24]. Another mechanism by which PACAP expression may increase is through activation of the hypoxic inducible factor-1α (HIF-1α) transcription factor whose transcriptional activity is strongly enhanced in hypoxic conditions. Indeed, no increased PACAP expression can be observed in HIF-1α deficient mice or after chemical inhibition during experimental ischemia [26]. In parallel, Zhang et al. demonstrated that PACAP expression is upregulated in sensory neurons in a model of adjuvant-induced inflammation in rat paw, suggesting that inflammatory conditions stimulate PACAP expression in neuronal cells [29].
Thus, these observations lead to the conclusion that in pathological conditions, endogenous PACAP expression is triggered in response to stress-related cues such as cell death, tissue lesion, or local inflammation, suggesting that the PACAPergic system could be part of an endogenous mechanism of protection aimed to support cell survival and to modulate the inflammatory response.
Expression of PACAP Receptors After Stroke
If less data are available regarding expression of PACAP receptors after stroke, they also support the idea that the endogenous PACAPergic system contributes to a mechanism of protection initiated after brain injury. Indeed, from day 1 to day 3 after ischemia, a transient increase of the PAC1 mRNA expression has been reported in neurons at the level of the post-ischemic fronto-parietal cortex, primary olfactory cortex, and caudate putamen in models of focal cerebral ischemia [24, 30, 31]. Similar results are observed in a mouse model of global ischemia where numerous PAC1 positive neurons are detected in the hippocampus 1 day after transient MCAO. In contrast, transcriptomic analysis revealed a significant decrease of VPAC1 mRNA at day 3, while VPAC2 mRNA levels remained unchanged over time [32]. From day 3, the PAC1 receptor is no longer detectable in neurons but its expression gradually increases in astrocytes. Indeed, an increase of PAC1 mRNA was observed in astrocytes of the corpus callosum in a permanent MCAO model [24]. Nakamachi and collaborators have also reported an elevation of PAC1 mRNA in hippocampal astrocytes surrounding the damaged CA1 pyramidal 7 days after ischemia [32], suggesting that the PACAPergic system may play a role in the reactive astrogliosis occurring after brain injury.
Altogether, these data reinforce the hypothesis of a participation of the PACAPergic system in an endogenous protective mechanism through the targeting at different levels of many pathophysiological processes in order to promote cell survival.
PACAP’s Therapeutical Potential in Stroke Models: Mechanisms of Action
Neuroprotective Action of Exogenous PACAP’s Delivery After Ischemia
Since its discovery, numerous studies using different approaches have demonstrated the neuroprotective effects of PACAP against ischemic lesions in various animal models of brain ischemia (Table 34.1).
The therapeutic benefit of exogenous PACAP administration for the treatment of cerebral ischemia was reported for the first time in 1996 in a rat model of transient global ischemia. A chronic intracerebroventricular (i.c.v.) infusion of PACAP, 1 pmol/h for 7 days, started immediately after induction of the ischemic lesion significantly reduced hippocampal neuronal cell death [31]. Other studies, using global ischemia models, confirmed that i.c.v. administration of PACAP before or during the ischemia induction correlates with a reduction of infarct volumes [33, 34]. Similarly, in animal models of transient focal cerebral ischemia, the intravenous (i.v.) injection of PACAP induces beneficial effects when administered before the induction of ischemia and up to 4 h after arterial occlusion, including a reduction of lesion volume and functional deficits [28, 35–37]. Finally, the therapeutic potential of PACAP was also confirmed in permanent models of cerebral ischemia, in which PACAP was administrated either i.v. or i.c.v. up to 1 h after stroke [27, 28, 38, 39].
These data highlight that PACAP is a potent neuroprotective agent when administered during the acute phase of brain ischemia, specifically within the first hours after artery occlusion. Nevertheless, a study also reports that a delayed delivery of PACAP beyond the acute phase can also improve functional recovery 7 and 14 days after stroke. Such effect was obtained using a stem cell-based strategy to deliver PACAP in the vicinity of the infarct area 3 days after the stroke onset in a mouse model of permanent MCAO and indicates that PACAP may represent an interesting therapeutical candidate to counteract the delayed pathophysiological processes occurring during the chronic phase of cerebral ischemia and therefore constitutes a novel alternative for stroke treatment in a currently unexploited therapeutical time window [40].
Antiapoptotic Role of PACAP
The impairment of blood supply after vessel occlusion in a brain territory initiates a pathophysiological cascade of events leading to a massive neuronal loss. If cell death responsible for ischemic lesions has firstly been considered only of necrotic nature, it is now established that part of the cells also die by apoptosis [41]. Apoptotic processes preferentially develop within the penumbra and participate in the extension of the lesions from the infarct core toward the ischemic penumbra, therefore representing a potentially important therapeutic target [42]. Several in vitro and in vivo studies on ischemia report that the protective effect of PACAP is based on its well-recognized antiapoptotic properties as illustrated in rats by a 50 % reduction of apoptotic cell death after i.c.v. administration of PACAP (2 μg) immediately before permanent MCA occlusion [43].
The antiapoptotic property of the neuropeptide relies on its ability to interfere at multiple levels of the neurotoxic cascade that ends to cell apoptosis. The O2 and glucose withdrawal impairs the activity of critical ATP-dependent ionic pumps such as ATP-dependent Na+/K+ and Ca2+ pumps disrupting ionic homeostasis and transmembrane gradients resulting in a massive release of excitatory amino acids, especially glutamate [44]. Lucas and Newhouse in 1957 and then Olney in 1969 have established a correlation between extracellular glutamate concentration and cytotoxicity, and shown that glutamate neurotoxicity is due to its excitatory effect, leading to the concept of excitotoxicity [45–47]. The binding of glutamate to its ionotropic NMDA, AMPA, and kainate receptors increases the permeability of these channel receptors to Cl-, Na+, and Ca2+ ions. Furthermore, the intracellular accumulation of Ca2+ triggers molecular events leading to the activation of apoptotic processes. At high concentration (above 10 nM), PACAP inhibits glutamate receptors transmission, from NMDA- as well as AMPA-type receptors [48, 49] and increases glial glutamate uptake and metabolism in astrocytes by promoting the expression of GLT-1, GLAST transporters, and glutamine synthetase [50]. Thus, PACAP can interfere in a first step with this initial excitotoxic cascade by modulating glutamate signaling (Fig. 34.1).
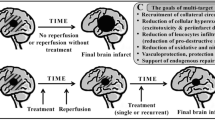
Summary of PACAP’s neuroprotective effects during acute ischemic stroke. PACAP acts on the different physiopathological events of the ischemic cascade developing in the early as well as the late phase of brain stroke. During the acute phase of ischemia, PACAP prevents neuronal cell death directly by regulating the caspase-dependent apoptotic pathways and indirectly by reducing oxidative stress and glutamate excitotoxicity. Moreover, PACAP affects the local inflammatory response in both phases of ischemia by modulating the balance between pro- and anti-inflammatory mediators and promoting the redirection of the microglial cell response toward a neuroprotective M2 phenotype. In the late phase, the PACAP-dependent redirection of the microglial response combined to the neurotrophic properties of the peptide on neural progenitors amplifies the post-ischemic neurogenesis and neoangiogenesis processes improving the endogenous tissue repair and functional recovery
Consecutively to energetic depletion and associated excitotoxicity, the increased cytosolic Ca2+ concentration initiates the uncoupling of the mitochondrial oxidative phosphorylation, leading to deleterious free radicals production. In oxidative stress conditions, such as after hydrogen peroxide exposure [17], lipopolysaccharide-induced dopaminergic neurotoxicity [51] or controlled cortical impact [52], PACAP reduces the production of reactive oxygen species by inhibiting the activity of NADPH oxidase and inducing the expression of Glutathione Peroxidase-1 (GPx-1) and Superoxide Dismutase-2 (SOD-2) antioxidant enzymes. Moreover, in a model of global ischemia, PACAP counteracts hippocampal CA1 neuronal death consecutive to oxidative DNA damages via induction of apurinic/apyrimidinic endonuclease 1 DNA repair enzyme [53]. Therefore, it appears that PACAP’s antiapoptotic effect results not only from the modulation of glutamatergic transmission but also depends on a powerful antioxidant activity, two of the initial processes responsible for the activation of the apoptotic cascade (Fig. 34.1).
Besides the inhibition of these initial steps of the neurotoxic cascade, the investigation of the mechanisms involved in the protective action of PACAP revealed its ability to inhibit directly the caspase-dependent mitochondrial apoptotic pathway. Western blot analysis performed in PACAP-deficient mice reported a rapid decrease, within 6 h after permanent focal ischemia, of Bcl-2 expression levels in the mitochondrial fraction and a concomitant cytosolic accumulation of cytochrome c release [28]. PACAP can also regulate the expression of other members of the Bcl-2 family. In particular, in an in vitro model of cortical neurons submitted to oxygen/glucose deprivation, PACAP promotes cell survival through the phosphorylation and therefore the inactivation of Bad [24]. Similarly, the neuroprotective effect of PACAP against monosodium glutamate-induced retinal degeneration is mediated by inhibition of pro-apoptotic signaling pathways and relies on the ability of PACAP to phosphorylate Bad but also to decrease cytochrome c and apoptosis inducing factor (AIF) release [54] (Fig. 34.1).
Altogether, these observations demonstrate that PACAP has a potent antiapoptotic activity due to combined inhibitory actions on the initiation phase as well as the effector phase of the apoptotic pathway.
Immunomodulatory Effects of PACAP
The post-ischemic inflammation is a complex process initiated early after the stroke onset, sustained over weeks, exerting both detrimental and beneficial roles and controlled by microglia, a unique immunocompetent cell population in the brain parenchyma. A correlation between the neuroprotective effect of PACAP and its immunomodulatory role was first proposed in 1998 by Shioda and coworkers. In a rodent model of global cerebral ischemia, i.c.v. infusion of PACAP for 48 h before ischemia causes an increase in interleukin (IL)-6 levels in the cerebrospinal fluid of animals correlated to a decrease of brain lesions [34]. Immunofluorescence studies highlighting IL-6 production in PAC1-expressing cortical neurons and absence of PACAP-mediated neuroprotection in IL-6 knock-out mice following MCAO suggest that PACAP’s neuroprotective properties rely on the PACAP-dependent IL-6 production (Fig. 34.1). Although the mechanisms underlying the protective effects of PACAP through the production of IL-6 are not clearly identified to date, such results illustrate the close link between modulation of the inflammatory response and neuroprotection.
Microarray-based transcriptomic studies showed in a mouse model of permanent focal ischemia that i.c.v. administration of the neuropeptide PACAP immediately after MCA occlusion modulates the expression of numerous genes encoding inflammatory mediators 6 and 24 h after PACAP injection. Among these genes, Il-22 and Il-11 were found upregulated after PACAP treatment whereas tumor necrosis factor (tnf) was downregulated [38] (Fig. 34.1). Similarly, i.v. administration of very low quantity of PACAP (0.02 μg/kg) in a rat model of transient ischemia negatively regulates the expression of pro-inflammatory compounds such as TNF-α, the nitric oxide synthase (NOS)-2, the chemokine MIP-1α, and the transcription factor NF-kB (Fig. 34.1). Importantly, the modulation of the local inflammatory response seems to correlate with a reduction in lesion volume and neurological deficits in animals suggesting that the anti-inflammatory properties of the neuropeptide PACAP could account for a large part of its neuroprotective effects [35]. Interestingly, these results have been confirmed in a model of delayed PACAP delivery 3 days after the stroke onset [40]. In this study, the observed modulation of the local inflammatory response after delayed PACAP delivery reveals a PACAP-dependent shift of the inflammatory response toward a resolutive phenotype, supporting cell survival and tissue repair, that correlates with decreased neurological deficits in animals. This PACAP-dependent skewing of the inflammatory response relies, at least partly, on direct or indirect neuropeptide’s effects on microglial cells (Fig. 34.1). Indeed, we report a PACAP-dependent polarization of microglial cell phenotype toward a neuroprotective M2-like phenotype as illustrated by an increased number of Arginase-1 positive microglial cells in the peri-infarct zone [40].
Altogether, these studies highlight that therapeutical strategies aimed at targeting the inflammatory process in the early phase as well as in the late phase of stroke and more specifically by skewing the microglial response toward a neuroprotective response rather than simply inhibiting inflammation could improve functional recovery in stroke victims.
Neurotrophic Properties of PACAP
PACAP exerts other important biological activities capable of interfering with the delayed pathophysiological events following stroke. More particularly, PACAP could mobilize different endogenous mechanisms of tissue repair including modulation of inflammation but also processes such as neurogenesis and angiogenesis, which in concert improve tissue homeostasis, neuroplasticity, and neuronal functions.
Following stroke, neurogenesis processes, which promote the generation of new parenchymal cells from neural stem cells and progenitor cells, are increased in the subventricular zone and in the dentate gyrus of the hippocampus. However, only 0.2 % of dead neurons are efficiently replaced by newborn cells [55], which is insufficient to achieve a complete functional recovery. Although there is no direct demonstration of a beneficial effect of PACAP in the neurogenic processes in in vivo models of ischemia, evidence from in vivo and in vitro studies using neural cells indicates that PACAP, due to its neurotrophic properties, may represent a promising pharmacological tool to improve such mechanisms. Indeed, besides an in vitro pro-mitogenic effect of PACAP on various cell types including neural stem/progenitor cells [56, 57], i.c.v. PACAP administration in naive mice as well as delayed PACAP delivery 3 days after ischemia (unpublished observations) increase the number of BrdU-positive cells in the subventricular zone and in the dentate gyrus [12, 56], indicating that PACAP enhances in vivo adult neurogenesis. Although the molecular mechanisms involved are not clearly identified so far, the pro-mitogenic effect of PACAP seems mediated through the PAC1 receptor which is expressed in the neurogenic areas [56].
Confirming further the potential of PACAP to enhance neurogenesis, several studies also report that PACAP signaling can guide stem/progenitor cell differentiation toward a neuronal phenotype. In particular, in the presence of PACAP, embryonic stem (ES) cells grown as embryoid bodies present an increased number of neuritic extensions compared to control cells, reflecting the neurogenic effect of the neuropeptide in the earliest stages of development. Furthermore, electrophysiological data demonstrate that PACAP enhances the amplitude of outward currents in these embryoid bodies-derived cells after 2 weeks of treatment [13], illustrating the functionality of the newly formed neurons. Furthermore, recent work revealed that in a murine stroke model, PACAP increases the expression of the collapsing response mediator protein 2 (CRMP2), known to participate in axonal growth and neuronal differentiation, suggesting that PACAP could promote neuroregeneration through CRMP2 induction [58]. The fact that migration and differentiation of neural cells contribute to the mechanisms associated with endogenous neurogenesis to improve functional recovery [59, 60] suggests that PACAP could enhance post-stroke neurogenesis and consequently improve neurological and functional outcomes (Fig. 34.1).
Another mechanism that plays a critical role in improving long-term recovery after stroke is the reestablishment of a functional microvasculature in the ischemic penumbra. Indeed, neuronal function is critically dependent on regulation of CBF [61]. Among the numerous factors regulating angiogenesis and vascular maturation, the vascular endothelial growth factor (VEGF) appears to be a key player. In rodents, VEGFc and its receptors are overexpressed during the first 7–10 days after transient MCA occlusion and would be involved in post-ischemic revascularization processes [62, 63]. Previous investigations have demonstrated that PACAP stimulates VEGF production in rat pituitary folliculostellate cells [64], suggesting that it may play an important role in angiogenesis. Such pro-angiogenic properties of PACAP have recently been confirmed in a transient model of MCAO in rat where intraperitoneal (i.p.) injections of PACAP for 5 consecutive days after MCA ligation lead to a higher cerebral microvascular perfusion and to an increased number of cerebral blood vessels in the penumbral area compared with control animals, as visualized with FITC-dextran. Moreover, a significant elevation of CBF in the ischemic cortex of PACAP-treated animals was observed 1 week after ischemia [26], confirming that PACAP may be considered as a potent angiogenic factor after stroke (Fig. 34.1).
PACAP Therapeutical Potential for Stroke Treatment: Limitations and Possibilities
All the above-mentioned observations indicate that PACAP could be useful as a therapeutic agent to reduce cell loss and promote neurological and functional recovery after ischemic stroke. However, its clinical use may be compromised by a poor bioavailability, a short half-life, and potential side effects as discussed below.
Time Window for PACAP Administration
Although PACAP represents a very interesting candidate for stroke treatment, its ability to induce tissue protection and functional recovery has mainly been investigated early after administration of the peptide, i.e., within the first 4 h after the stroke onset [33, 35, 36, 38]. It should be remembered that a narrow time window of only 4.5 h is one of the most important limitations of the current available treatments for brain ischemia which are only given to about 10 % of stroke victims. As a consequence, the development of therapeutical strategies with enlarged time window is a priority and in this context, our recent findings of a beneficial effect of PACAP 3 days after the stroke onset offer new avenues for the use of PACAP as a therapeutic drug with unexploited therapeutical window that could benefit to a larger number of stroke patients [40].
PACAP Bioavailability and Administration Route
Numerous studies using rodent models of cerebral ischemia demonstrate promising results after an intravenous injection of PACAP, as illustrated in Table 34.1. In human however, strategies based on a systemic administration of pharmacological agents are restricted by the difficulties to access the damaged cerebral tissues especially after cerebrovascular disruption. Interestingly, while the passage of numerous molecules is restricted by the blood brain barrier (BBB), PACAP38 crosses the BBB via the specific peptide transporter system 6 (PTS-6) [65]. Moreover, in two different models of brain ischemia, one caused by cardiac arrest and the other by MCAO, a rapid transient increase of PACAP influx into the brain within 4 h after i.v. injection has been shown [66, 67]. Although the exact mechanisms involved in the observed influx of PACAP have not been directly demonstrated, these changes of PACAP permeability are more likely attributable to an enhanced PTS-6 activity across the BBB rather than the ischemia-induced increased BBB permeability. This ability of PACAP to rapidly enter the brain may account for the neuroprotective effects observed early after the stroke onset [35–37]. Nevertheless, treatment with the native peptide starting 8 or 12 h after occlusion did not result in reduced infarct or improve functional recovery [35–37], which could be explained by the decreased entry of PACAP beginning 6 h after ischemia [66]. Thus it appears that while intravenous PACAP injection at early time points after ischemia may represent a relevant approach for neuroprotection, after the first 4 h, i.v. PACAP injections do not reach efficiently the brain parenchyma to promote neurological improvement and functional recovery. Thus, alternative strategies to improve the delivery of PACAP in the vicinity of the infarct area, such as stem cell-expressing PACAP injected 3 days after stroke [40], may be of great interest. Moreover, by enhancing the rate of entry of PACAP in the CNS, neuroprotection would be achieved with lower doses of the peptide, leading to a reduction of the adverse side effects associated with an i.v. injection.
PACAP Stability
In the systemic circulation, PACAP, as most natural peptides, is rapidly degraded by plasmatic enzymes including carboxypeptidase and endopeptidase, greatly reducing its biological half-life and therefore restricting its use as a therapeutical agent. Furthermore, in vitro and in vivo studies revealed that PACAP is rapidly metabolized by dipeptidyl peptidase-IV (DPP-IV), a ubiquitous aminopeptidase that releases dipeptides from the N-terminal fragment of diverse peptides. Thus, after intravenous injection to mice, the half-life of PACAP in plasma is less than 2 min [68]. In human, a case study in an elderly male patient estimated PACAP blood half-life between 5 and 10 min [69], while in healthy volunteers PACAP exhibits a mean plasma half-life of 3.5 ± 1.3 min [70]. Moreover, the cleavage of PACAP by DPP-IV generates two metabolites PACAP(3-38) and PACAP(5-38) [68] that behave as PAC1 antagonists [71], reducing further the biological effects of PACAP. As a consequence, obtaining an effective therapeutical dose of PACAP in the ischemic territory may be hampered by this low metabolic stability.
Potential Side Effects
PACAP and its receptors are widely distributed throughout the CNS and peripheral tissues. Such a large distribution implies that this neuropeptide exerts numerous biological activities [7], some of them being potential side effects when injected systemically, therefore preventing the safe therapeutic use of the peptide. For instance, PACAP and its receptors are expressed in the cardiovascular system [72–74]. Considering that cerebral ischemia results from vascular impairment, potential effects of PACAP on the cardiovascular system have to be considered very carefully. In fact, in healthy volunteers, intravenous infusion of PACAP (10 pmol/kg/min) for 20 min significantly increases heart rate [70]. As PACAP was reported to be a potent and long-lasting vasodilator, this tachycardia probably results from the peripheral vasodilatation caused by the peptide [75, 76]. It has also been showed that PACAP in a dose-dependent manner can cause tachycardia, bradycardia, and auricular fibrillation [77], various events that may lead to the occurrence of ischemic stroke. Moreover, it is worth noting that in human, all subjects who received an i.v. injection of PACAP experienced a sustained skin flushing on the face and chest [70] and some of them were subjected to headache [78]. Because such physiological responses may impede the use of PACAP as a safe therapeutical drug for stroke treatment, the development of approaches to limit PACAP side effects represents an important goal. As discussed below, different strategies may be considered to counteract the limitations associated with PACAP poor bioavailability and side effects, including the design of stable analogs of PACAP with improved selectivity and the development of strategies to enhance its specific brain delivery.
Development of Stable Analogs
One possibility to increase PACAP metabolic stability is to develop PACAP stable analogs presenting a reduced sensitivity to plasmatic endopeptidase and DPP-IV. In this attempt, chemical modifications at potential peptidase cleavage sites into the peptide sequence can drastically improve its resistance to enzymatic degradation. For instance, the sequence of PACAP contains two potential cleavage sites for plasmatic endopeptidases represented by two dibasic pairs Arg14-Lys15 and Lys20-Lys21 [79]. Therefore, the replacement of the Lysine amino acid by an Alanine residue confers an increased resistance to enzymatic digestion. Similarly, N-terminal acetylation of the peptide abolished its degradation by DPP-IV. Structure-activity relationship studies led to the development of two metabolically stable PACAP analogs, i.e., acetyl-[Ala15, Ala20]PACAP38-propylamide and acetyl-PACAP27-propylamide that exhibit a complete resistance to DPP-IV degradation and an increased plasmatic half-life while remaining highly active [79]. It has been shown in a rat model of transient cerebral ischemia that PACAP38 and its analog acetyl-[Ala15, Ala20]PACAP38-propylamide, when administered intravenously at very low dose (0.02 μg/kg), present similar potency and act through same mechanisms to reduce neuronal cell loss and functional deficits [35]. These results indicate that picomolar doses of PACAP and analogs are sufficient to exert maximal neuroprotective activities in case of stroke and it is tempting to speculate that at such low doses, side effects associated with the systemic administration of PACAP would be considerably reduced.
Nevertheless, PACAP analogs have also shown detrimental effects in animal stroke models. As a matter of fact, the administration of a VPAC2 agonist worsens neuronal damages after stroke [80]. Therefore, development of Ac-[Phe(pI)6, Nle17]PACAP(1-27) which activates PAC1 and VPAC1 receptors but not VPAC2 could be a new tool to reduce PACAP side effects [81]. Actually, in an in vivo model of Parkinson disease, this analog was as potent as PACAP to restore tyrosine hydroxylase expression and to modulate the inflammatory response in the substantia nigra but had significantly less effects on mean arterial pressure when compared to PACAP [82].
Enhancement of Brain Delivery
Another possible approach to counteract the limitations associated with the plasmatic instability of PACAP and its potential peripheral side effects is the development of strategies aiming at enhancing the specific delivery of PACAP within the ischemic brain.
Intranasal Delivery
During the last few decades, the nasal route for drug delivery into the brain has been extensively investigated. The “nose-to-brain” delivery is of great interest because this route is noninvasive and can deliver drugs directly into the brain, bypassing the BBB which is impermeable for a high percentage of molecules. Additionally, such approach avoids rapid metabolism in the systemic circulation as well as peripheral side effects, therefore representing a promising hope for counteracting the limitations associated with the intravenous injection of PACAP. Several therapeutic proteins such as granulocyte-colony stimulating factor, transforming growth factor-beta, erythropoietin (EPO), and insulin-growth factor-1 have been successfully delivered into the brain of rodents in different models of stroke [83–85], indicating that intranasal drug delivery is a promising method to specifically provide therapeutical compounds into the ischemic brain. Moreover, different formulations including simple drop (nanogel) or nasal spray (insoluble powder or emulsions) can be designed to maximize the convenience and comfort of patients. Interestingly, nasal application of PACAP can reach the brain rapidly and was effective to slow down Alzheimer’s disease-like pathology in a mice transgenic model [86]. Noteworthy, such administration of the peptide has also been reported in human and did not affect heart rate and blood pressure in patients [86], indicating that using the “nose-to-brain” route for PACAP delivery can efficiently avoid the side effects of PACAP on the cardiovascular system.
Colloidal Carriers
The use of colloidal carriers including liposomes and nanoparticles could represent another interesting avenue for a selective and prolonged delivery of PACAP and its derivatives into the ischemic brain. Colloidal carriers are drug vectors, particles, or vesicles in the nanometer size range used for the transport of loaded drugs to a target site. These systems are biocompatible, nontoxic, and biodegradable and therefore represent a promising tool for a clinical use. They can carry various therapeutic agents (hydrophilic, lipophilic, and amphoteric drug molecules) which are generally encapsulated, entrapped, adsorbed, or chemically attached to the carrier surface [87]. These encapsulation systems offer the advantage to protect drug molecules from enzymatic degradation in the blood circulation, significantly increasing their bioavailability. The biocompatibility and longevity of such particles can be achieved through surface modifications involving a coating of biodegradable polymers such as chitosan, PLGA (poly(lactic-co-glycolic acid) copolymer), PLA (polylactic acid), and PEG (polyethylene glycol) [88]. In particular, PEGylation of drug-loaded liposomes is very efficient to enhance the longevity of particles in the systemic bloodstream [89]. Such surface modifications are also used to achieve tissue specificity. For example, the biopolymer polysorbate, PLGA, and PEG have been successful in delivering therapeutics into the brain parenchyma [90, 91]. Other ligands can also be added to specifically target the brain including insulin, transferrin, lactoferrin, glutathione, and apolipoprotein [92]. It is worth mentioning that such nanocarrier formulations also exist for nose-to-brain delivery [93].
Colloidal vectors, in particular polymeric nanoparticles and liposomes, have been used with success to transport therapeutically relevant agents into the brain parenchyma in various animal models of brain ischemia. For instance, in a transient model of MCAO, chitosan-nanoparticles loaded with the basic fibroblast growth factor and/or with an inhibitor of caspase-3 have been administrated systematically just before the induction of ischemia. In this study the authors found that nanoparticles rapidly transport the active molecules to the brain parenchyma in their active form, which results in reduced infarct volume and functional impairment [94]. PEGylated liposomes administrated within 3 h after the stroke onset also accumulate in the ischemic penumbral area in a time-dependent manner with a peak of accumulation at 24 h [95]. Hence, the long-lasting accumulation of the nanocarriers in the vicinity of the infarct area could lead to a prolonged drug delivery and an increased therapeutic efficacy of PACAP. Supporting this hypothesis, asialo-erythropoietin (AEPO, a metabolite of EPO) loaded liposomes present higher protective effect compared to native AEPO [95]. Furthermore, magnetic resonance imaging studies revealed that 100 nm-liposomes, injected intravenously 1 or 2 h after permanent MCAO in rats, accumulated in the ipsilateral parenchyma [96]. These results raise the possibility that liposome-based strategies may be possible even in the absence of reperfusion and could therefore benefit to patients who are not eligible for r-tPA treatment. All these observations indicate that application of such technologies to PACAP could not only enhance its therapeutic efficacy to improve neurological and functional ischemia-induced deficits, but also enable a reduction of the dose of peptide which must be administered to achieve a therapeutic response, thus minimizing its adverse side effects. Remarkably, encapsulation systems may also present the advantage of targeting PACAP delivery at the cellular level. As discussed previously a possible mechanism underlying the beneficial effect of PACAP during cerebral ischemia relies on its immunoregulatory activity on microglial cells. Thus, incorporating molecules specifically recognized by microglial cells in the surface of liposomes or nanoparticles would be of great interest. For instance, it would be interesting to evaluate the therapeutical potential of PACAP-loaded particles coated with molecules known to activate microglia phagocytic function without triggering a pro-inflammatory program such as the agonist of the TREM2 receptor Hsp60 [97].
Altogether, these approaches represent alternative strategies for the stabilization and development of pharmaceutical formulation of PACAP and its derivatives to benefit from its neuroprotective properties while overcoming its limitations in the context of brain stroke.
Conclusion
In conclusion, there is now clear evidence that PACAP exerts a potent neuroprotective activity and improves functional recovery in various models of cerebral ischemia. PACAP acts at very low doses on the main pathophysiological events developing in the early and in the late phases of brain stroke, making PACAP a potential therapeutical candidate for stroke treatment even in still unexploited therapeutical windows. Interestingly, several pathophysiological processes modulated by PACAP in stroke models are known to be involved in many other neurodegenerative diseases among which Parkinson’s disease, multiple sclerosis, spinal cord injury, or Alzheimer’s disease, suggesting that PACAP could represent also a novel alternative for the treatment of these neurological troubles. Nevertheless, because of the wide distribution of PACAP and its receptors, a systemic delivery of the peptide would have many peripheral actions responsible for numerous side effects limiting the PACAP’s therapeutical use. Therefore, it is now necessary to develop selective analogs and efficient route of administration to specifically and locally target the signaling mechanisms and cell responses relaying the protective effects of PACAP without affecting peripheral organs.
Abbreviations
- AEPO:
-
Asialo-erythropoietin
- AIF:
-
Apoptosis inducing factor
- AIS:
-
Acute ischemic stroke
- BBB:
-
Blood brain barrier
- CBF:
-
Cerebral blood flow
- CNS:
-
Central nervous system
- CRMP2:
-
Collapsing response mediator protein 2
- DPP-IV:
-
Dipeptidyl peptidase IV
- EPO:
-
Erythropoietin
- GHRH:
-
Growth hormone-releasing hormone
- GPx-1:
-
Glutathione peroxidase-1
- HIF-1α:
-
Hypoxic inducible factor-1α
- i.c.v.:
-
Intracerebroventricular
- i.p.:
-
Intraperitoneal
- i.v.:
-
Intravenous
- IL:
-
Interleukin
- MCA:
-
Middle cerebral artery
- MCAO:
-
Middle cerebral artery occlusion
- NOS2:
-
Nitric oxide synthase 2
- PACAP:
-
Pituitary adenylate cyclase-activating polypeptide
- PEG:
-
Polyethylene glycol
- PLA:
-
Polylactic acid
- PLGA:
-
Poly(lactic-co-glycolic acid) copolymer
- PTS-6:
-
Peptide transporter system 6
- r-tPA:
-
Recombinant-tissue plasminogen activator
- SOD2:
-
Superoxide dismutase-2
- TNF:
-
Tumor necrosis factor
- VEGF:
-
Vascular endothelial growth factor
- VIP:
-
Vasoactive intestinal peptide
References
Evers SMAA, Struijs JN, Ament AJHA, van Genugten MLL, Jager JHC, van den Bos GAM. International comparison of stroke cost studies. Stroke. 2004;35:1209–15.
Olesen J, Gustavsson A, Svensson M, Wittchen H-U, Jönsson B. The economic cost of brain disorders in Europe. Eur J Neurol. 2012;19:155–62.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. 1999;22:391–7.
Donnan GA, Davis SM, Parsons MW, Ma H, Dewey HM, Howells DW. How to make better use of thrombolytic therapy in acute ischemic stroke. Nat Rev Neurol. 2011;7:400–9.
Miyata A, Arimura A, Dahl RR, Minamino N, Uehara A, Jiang L, et al. Isolation of a novel 38 residue-hypothalamic polypeptide which stimulates adenylate cyclase in pituitary cells. Biochem Biophys Res Commun. 1989;164:567–74.
Vaudry D, Falluel-Morel A, Bourgault S, Basille M, Burel D, Wurtz O, et al. Pituitary adenylate cyclase-activating polypeptide and its receptors: 20 years after the discovery. Pharmacol Rev. 2009;61:283–357.
Harmar AJ, Arimura A, Gozes I, Journot L, Laburthe M, Pisegna JR, et al. International Union of Pharmacology. XVIII. Nomenclature of receptors for vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide. Pharmacol Rev. 1998;50:265–70.
Lutz EM, MacKenzie CJ, Johnson M, West K, Morrow JA, Harmar AJ, et al. Domains determining agonist selectivity in chimaeric VIP2 (VPAC2)/PACAP (PAC1) receptors. Br J Pharmacol. 1999;128:934–40.
Harmar AJ, Fahrenkrug J, Gozes I, Laburthe M, May V, Pisegna JR, et al. Pharmacology and functions of receptors for vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide: IUPHAR review 1. Br J Pharmacol. 2012;166:4–17.
Nicot A, DiCicco-Bloom E. Regulation of neuroblast mitosis is determined by PACAP receptor isoform expression. Proc Natl Acad Sci U S A. 2001;98:4758–63.
Ohta S, Gregg C, Weiss S. Pituitary adenylate cyclase-activating polypeptide regulates forebrain neural stem cells and neurogenesis in vitro and in vivo. J Neurosci Res. 2006;84:1177–86.
Chafai M, Louiset E, Basille M, Cazillis M, Vaudry D, Rostène W, et al. PACAP and VIP promote initiation of electrophysiological activity in differentiating embryonic stem cells. Ann N Y Acad Sci. 2006;1070:185–9.
Gonzalez BJ, Basille M, Vaudry D, Fournier A, Vaudry H. Pituitary adenylate cyclase-activating polypeptide promotes cell survival and neurite outgrowth in rat cerebellar neuroblasts. Neuroscience. 1997;78:419–30.
Masmoudi-Kouki O, Douiri S, Hamdi Y, Kaddour H, Bahdoudi S, Vaudry D, et al. Pituitary adenylate cyclase-activating polypeptide protects astroglial cells against oxidative stress-induced apoptosis. J Neurochem. 2011;117:403–11.
Vaudry D, Falluel-Morel A, Basille M, Pamantung TF, Fontaine M, Fournier A, et al. Pituitary adenylate cyclase-activating polypeptide prevents C2-ceramide-induced apoptosis of cerebellar granule cells. J Neurosci Res. 2003;72:303–16.
Vaudry D, Pamantung TF, Basille M, Rousselle C, Fournier A, Vaudry H, et al. PACAP protects cerebellar granule neurons against oxidative stress-induced apoptosis. Eur J Neurosci. 2002;15:1451–60.
Huang M, Shirahase H, Rorstad OP. Comparative study of vascular relaxation and receptor binding by PACAP and VIP. Peptides? 14:755–62.
Lindén A, Yoshihara S, Chan B, Nadel JA. Inhibition of bronchoconstriction by pituitary adenylate cyclase activating polypeptide (PACAP 1-27) in guinea-pigs in vivo. Br J Pharmacol. 1995;115:913–6.
Delgado M, Miller Jonakait G, Ganea D. Vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide inhibit chemokine production in activated microglia. Glia. 2002;39:148–61.
Delgado M, Munoz-Elias EJ, Gomariz RP, Ganea D. VIP and PACAP inhibit IL-12 production in LPS-stimulated macrophages. Subsequent effect on IFNgamma synthesis by T cells. J Neuroimmunol. 1999;96:167–81.
Tan Y-V, Abad C, Lopez R, Dong H, Liu S, Lee A, et al. Pituitary adenylyl cyclase-activating polypeptide is an intrinsic regulator of Treg abundance and protects against experimental autoimmune encephalomyelitis. Proc Natl Acad Sci U S A. 2009;106:2012–7.
Tan Y-V, Abad C, Wang Y, Lopez R, Waschek JA. VPAC2 (vasoactive intestinal peptide receptor type 2) receptor deficient mice develop exacerbated experimental autoimmune encephalomyelitis with increased Th1/Th17 and reduced Th2/Treg responses. Brain Behav Immun. 2015;44:167–75.
Stumm R, Kolodziej A, Prinz V, Endres M, Wu DF, Höllt V. Pituitary adenylate cyclase-activating polypeptide is up-regulated in cortical pyramidal cells after focal ischemia and protects neurons from mild hypoxic/ischemic damage. J Neurochem. 2007;103:1666–81.
Riek-Burchardt M, Kolodziej A, Henrich-Noack P, Reymann KG, Höllt V, Stumm R. Differential regulation of CXCL12 and PACAP mRNA expression after focal and global ischemia. Neuropharmacology. 2010;58:199–207.
Lin C-H, Chiu L, Lee H-T, Chiang C-W, Liu S-P, Hsu Y-H, et al. PACAP38/PAC1 signaling induces bone marrow-derived cells homing to ischemic brain. Stem Cells. 2015;33:1153–72.
Chen Y, Samal B, Hamelink CR, Xiang CC, Chen Y, Chen M, et al. Neuroprotection by endogenous and exogenous PACAP following stroke. Regul Pept. 2006;137:4–19.
Ohtaki H, Nakamachi T, Dohi K, Aizawa Y, Takaki A, Hodoyama K, et al. Pituitary adenylate cyclase-activating polypeptide (PACAP) decreases ischemic neuronal cell death in association with IL-6. Proc Natl Acad Sci U S A. 2006;103:7488–93.
Zhang Y, Danielsen N, Sundler F, Mulder H. Pituitary adenylate cyclase-activating peptide is upregulated in sensory neurons by inflammation. Neuroreport. 1998;9:2833–6.
Gillardon F, Hata R, Hossmann K-A. Delayed up-regulation of Zac1 and PACAP type I receptor after transient focal cerebral ischemia in mice. Mol Brain Res. 1998;61:207–10.
Uchida D, Arimura A, Somogyvári-Vigh A, Shioda S, Banks WA. Prevention of ischemia-induced death of hippocampal neurons by pituitary adenylate cyclase activating polypeptide. Brain Res. 1996;736:280–6.
Nakamachi T, Tsuchida M, Kagami N, Yofu S, Wada Y, Hori M, et al. IL-6 and PACAP receptor expression and localization after global brain ischemia in mice. J Mol Neurosci. 2012;48:518–25.
Dohi K, Mizushima H, Nakajo S, Ohtaki H, Matsunaga S, Aruga T, et al. Pituitary adenylate cyclase-activating polypeptide (PACAP) prevents hippocampal neurons from apoptosis by inhibiting JNK/SAPK and p38 signal transduction pathways. Regul Pept. 2002;109:83–8.
Shioda S, Ozawa H, Dohi K, Mizushima H, Matsumoto K, Nakajo S, et al. PACAP protects hippocampal neurons against apoptosis: involvement of JNK/SAPK signaling pathway. Ann N Y Acad Sci. 1998;865:111–7.
Dejda A, Seaborn T, Bourgault S, Touzani O, Fournier A, Vaudry H, et al. PACAP and a novel stable analog protect rat brain from ischemia: Insight into the mechanisms of action. Peptides. 2011;32:1207–16.
Reglodi D, Somogyvari-Vigh A, Vigh S, Kozicz T, Arimura A. Delayed systemic administration of PACAP38 is neuroprotective in transient middle cerebral artery occlusion in the rat. Stroke. 2000;31:1411–7.
Reglodi D, Somogyvari-Vigh A, Vigh S, Maderdrut JL, Arimura A. Neuroprotective effects of PACAP38 in a rat model of transient focal ischemia under various experimental conditions. Ann N Y Acad Sci. 2000;921:119–28.
Hori M, Nakamachi T, Rakwal R, Shibato J, Ogawa T, Aiuchi T, et al. Transcriptomics and proteomics analyses of the PACAP38 influenced ischemic brain in permanent middle cerebral artery occlusion model mice. J Neuroinflammation. 2012;9:256.
Reglodi D, Tamás A, Somogyvári-Vigh A, Szántó Z, Kertes E, Lénárd L, et al. Effects of pretreatment with PACAP on the infarct size and functional outcome in rat permanent focal cerebral ischemia. Peptides. 2002;23:2227–34.
Brifault C, Gras M, Liot D, May V, Vaudry D, Wurtz O. Delayed pituitary adenylate cyclase—activating polypeptide delivery after brain stroke improves functional recovery by inducing m2 microglia/macrophages polarization. Stroke. 2015;46:520–8.
Linnik MD, Zobrist RH, Hatfield MD. Evidence supporting a role for programmed cell death in focal cerebral ischemia in rats. Stroke. 1993;24:2002–8.
Charriaut-Marlangue C, Margaill I, Represa A, Popovici T, Plotkine M, Ben-Ari Y. Apoptosis and necrosis after reversible focal ischemia: an in situ DNA fragmentation analysis. J Cereb Blood Flow Metab. 1996;16:186–94.
Reglodi D, Fábián Z, Tamás A, Lubics A, Szeberényi J, Alexy T, et al. Effects of PACAP on in vitro and in vivo neuronal cell death, platelet aggregation, and production of reactive oxygen radicals. Regul Pept. 2004;123:51–9.
Katsura K, Kristián T, Siesjö BK. Energy metabolism, ion homeostasis, and cell damage in the brain. Biochem Soc Trans. 1994;22:991–6.
Lucas DR, Newhouse JP. The toxic effect of sodium L-glutamate on the inner layers of the retina. AMA Arch Ophthalmol. 1957;58:193–201.
Olney JW. Glutamate-induced retinal degeneration in neonatal mice. Electron microscopy of the acutely evolving lesion. J Neuropathol Exp Neurol. 1969;28(3):455–74.
Olney JW, Adamo NJ, Ratner A. Monosodium glutamate effects. Science. 1971;172(3980):294.
Costa L, Santangelo F, Li Volsi G, Ciranna L. Modulation of AMPA receptor-mediated ion current by pituitary adenylate cyclase-activating polypeptide (PACAP) in CA1 pyramidal neurons from rat hippocampus. Hippocampus. 2009;19:99–109.
Liu GJ, Madsen BW. PACAP38 modulates activity of NMDA receptors in cultured chick cortical neurons. J Neurophysiol. 1997;78:2231–4.
Figiel M, Engele J. Pituitary adenylate cyclase-activating polypeptide (PACAP), a neuron-derived peptide regulating glial glutamate transport and metabolism. J Neurosci. 2000;20:3596–605.
Yang S, Yang J, Yang Z, Chen P, Fraser A, Zhang W, et al. Pituitary adenylate cyclase-activating polypeptide (PACAP) 38 and PACAP4-6 are neuroprotective through inhibition of NADPH oxidase: potent regulators of microglia-mediated oxidative stress. J Pharmacol Exp Ther. 2006;319:595–603.
Miyamoto K, Tsumuraya T, Ohtaki H, Dohi K, Satoh K, Xu Z, et al. PACAP38 suppresses cortical damage in mice with traumatic brain injury by enhancing antioxidant activity. J Mol Neurosci. 2014;54:370–9.
Stetler RA, Gao Y, Zukin RS, Vosler PS, Zhang L, Zhang F, et al. Apurinic/apyrimidinic endonuclease APE1 is required for PACAP-induced neuroprotection against global cerebral ischemia. Proc Natl Acad Sci U S A. 2010;107:3204–9.
Rácz B, Gallyas F, Kiss P, Tóth G, Hegyi O, Gasz B, et al. The neuroprotective effects of PACAP in monosodium glutamate-induced retinal lesion involve inhibition of proapoptotic signaling pathways. Regul Pept. 2006;137(1-2):20–6.
Arvidsson A, Collin T, Kirik D, Kokaia Z, Lindvall O. Neuronal replacement from endogenous precursors in the adult brain after stroke. Nat Med. 2002;8:963–70.
Mercer A, Rönnholm H, Holmberg J, Lundh H, Heidrich J, Zachrisson O, et al. PACAP promotes neural stem cell proliferation in adult mouse brain. J Neurosci Res. 2004;76(2):205–15.
Hori M, Nakamachi T, Shibato J, Rakwal R, Tsuchida M, Shioda S, et al. PACAP38 differentially effects genes and CRMP2 protein expression in ischemic core and penumbra regions of permanent middle cerebral artery occlusion model mice brain. Int J Mol Sci. 2014;15:17014–34.
Zhang R, Zhang L, Zhang Z, Wang Y, Lu M, Lapointe M, et al. A nitric oxide donor induces neurogenesis and reduces functional deficits after stroke in rats. Ann Neurol. 2001;50:602–11.
Zhao Y, Guan Y-F, Zhou X-M, Li G-Q, Li Z-Y, Zhou C-C, et al. Regenerative neurogenesis after ischemic stroke promoted by nicotinamide phosphoribosyltransferase-nicotinamide adenine dinucleotide cascade. Stroke. 2015;46:1966–74.
Pratt PF, Medhora M, Harder DR. Mechanisms regulating cerebral blood flow as therapeutic targets. Curr Opin Investig Drugs. 2004;5(9):952–6.
Shin S-H, Lee J, Lim KS, Rhim T, Lee SK, Kim Y-H, et al. Sequential delivery of TAT-HSP27 and VEGF using microsphere/hydrogel hybrid systems for therapeutic angiogenesis. J Control Release. 2013;166:38–45.
Shin Y-J, Choi J-S, Lee J-Y, Choi J-Y, Cha J-H, Chun M-H, et al. Differential regulation of vascular endothelial growth factor-C and its receptor in the rat hippocampus following transient forebrain ischemia. Acta Neuropathol. 2008;116:517–27.
Gloddek J, Pagotto U, Paez Pereda M, Arzt E, Stalla GK, Renner U. Pituitary adenylate cyclase-activating polypeptide, interleukin-6 and glucocorticoids regulate the release of vascular endothelial growth factor in pituitary folliculostellate cells. J Endocrinol. 1999;160:483–90.
Dogrukol-Ak D, Kumar VB, Ryerse JS, Farr SA, Verma S, Nonaka N, et al. Isolation of peptide transport system-6 from brain endothelial cells: therapeutic effects with antisense inhibition in Alzheimer and stroke models. J Cereb Blood Flow Metab. 2009;29:411–22.
Mizushima H, Banks WA, Dohi K, Shioda S, Matsumoto H, Matsumoto K. The effect of cardiac arrest on the permeability of the mouse blood-brain and blood-spinal cord barrier to pituitary adenylate cyclase activating polypeptide (PACAP). Peptides. 1999;20(11):1337–40.
Somogyvári-Vigh A, Pan W, Reglödi D, Kastin AJ, Arimura A. Effect of middle cerebral artery occlusion on the passage of pituitary adenylate cyclase activating polypeptide across the blood–brain barrier in the rat. Regul Pept. 2000;91:89–95.
Zhu L, Tamvakopoulos C, Xie D, Dragovic J, Shen X, Fenyk-Melody JE, et al. The role of dipeptidyl peptidase IV in the cleavage of glucagon family peptides: in vivo metabolism of pituitary adenylate cyclase activating polypeptide-(1-38). J Biol Chem. 2003;278:22418–23.
Li M, Maderdrut JL, Lertora JJL, Batuman V. Intravenous infusion of pituitary adenylate cyclase-activating polypeptide (PACAP) in a patient with multiple myeloma and myeloma kidney: a case study. Peptides. 2007;28:1891–5.
Birk S, Sitarz JT, Petersen KA, Oturai PS, Kruuse C, Fahrenkrug J, et al. The effect of intravenous PACAP38 on cerebral hemodynamics in healthy volunteers. Regul Pept. 2007;140:185–91.
Robberecht P, Gourlet P, De Neef P, Woussen-Colle MC, Vandermeers-Piret MC, Vandermeers A, et al. Structural requirements for the occupancy of pituitary adenylate-cyclase-activating-peptide (PACAP) receptors and adenylate cyclase activation in human neuroblastoma NB-OK-1 cell membranes. Discovery of PACAP(6-38) as a potent antagonist. Eur J Biochem. 1992;207:239–46.
Cardell LO, Uddman R, Luts A, Sundler F. Pituitary adenylate cyclase activating peptide (PACAP) in guinea-pig lung: distribution and dilatory effects. Regul Pept. 1991;36:379–90.
Miyata A, Sato K, Hino J, Tamakawa H, Matsuo H, Kangawa K. Rat aortic smooth-muscle cell proliferation is bidirectionally regulated in a cell cycle-dependent manner via PACAP/VIP Type 2 receptor. Ann N Y Acad Sci. 1998;865:73–81.
Shigyo M, Aizawa H, Inoue H, Matsumoto K, Takata S, Hara N. Pituitary adenylate cyclase activating peptide regulates neurally mediated airway responses. Eur Respir J. 1998;12:64–70.
Dorner GT, Wolzt M, Schmetterer L, Eichler HG. Effect of pituitary adenylate cyclase activating polypeptide 1–27 on ocular, cerebral and skin blood flow in humans. Naunyn Schmiedebergs Arch Pharmacol. 1998;358:657–62.
Warren JB, Cockcroft JR, Larkin SW, Kajekar R, Macrae A, Ghatei MA, et al. Pituitary adenylate cyclase activating polypeptide is a potent vasodilator in humans. J Cardiovasc Pharmacol. 1992;20:83–7.
Chang Y, Lawson LJ, Hancock JC, Hoover DB. Pituitary adenylate cyclase-activating polypeptide: localization and differential influence on isolated hearts from rats and guinea pigs. Regul Pept. 2005;129:139–46.
Schytz HW, Birk S, Wienecke T, Kruuse C, Olesen J, Ashina M. PACAP38 induces migraine-like attacks in patients with migraine without aura. Brain. 2009;132:16–25.
Bourgault S, Vaudry D, Botia B, Couvineau A, Laburthe M, Vaudry H, et al. Novel stable PACAP analogs with potent activity towards the PAC1 receptor. Peptides. 2008;29:919–32.
Darsalia V, Mansouri S, Wolbert P, Barde S, Sjöholm A, Patrone C. The specific VPAC2 agonist Bay 55-9837 increases neuronal damage and hemorrhagic transformation after stroke in type 2 diabetic rats. Neuropeptides. 2013;47:133–7.
Doan N-D, Bourgault S, Dejda A, Létourneau M, Detheux M, Vaudry D, et al. Design and in vitro characterization of PAC1/VPAC1-selective agonists with potent neuroprotective effects. Biochem Pharmacol. 2011;81:552–61.
Lamine A, Létourneau M, Doan ND, Maucotel J, Couvineau A, Vaudry H, et al. Characterizations of a synthetic pituitary adenylate cyclase-activating polypeptide analog displaying potent neuroprotective activity and reduced in vivo cardiovascular side effects in a Parkinson’s disease model. Neuropharmacology. 2016;108:440–50.
Fletcher L, Kohli S, Sprague SM, Scranton RA, Lipton SA, Parra A, et al. Intranasal delivery of erythropoietin plus insulin-like growth factor-I for acute neuroprotection in stroke. Laboratory investigation. J Neurosurg. 2009;111:164–70.
Guerra-Crespo M, Sistos A, Gleason D, Fallon JH. Intranasal administration of PEGylated transforming growth factor-alpha improves behavioral deficits in a chronic stroke model. J Stroke Cerebrovasc Dis. 2010;19:3–9.
Sun B, He M, Han X, Sun J, Yang M, Yuan H, et al. Intranasal delivery of granulocyte colony-stimulating factor enhances its neuroprotective effects against ischemic brain injury in rats. Mol Neurobiol. 2014. In press.
Kinhult J, Adner M, Uddman R, Cardell LO. Pituitary adenylate cyclase-activating polypeptide, effects in the human nose. Clin Exp Allergy. 2003;33:942–9.
Denora N, Trapani A, Laquintana V, Lopedota A, Trapani G. Recent advances in medicinal chemistry and pharmaceutical technology—strategies for drug delivery to the brain. Curr Top Med Chem. 2009;9:182–96.
Dikpati A, Madgulkar AR, Kshirsagar SJ, Chahal AS. Targeted drug delivery to CNS using nanoparticles. J Adv Pharm Sci. 2012;2:179–91.
Malik DK, Baboota S, Ahuja A, Hasan S, Ali J. Recent advances in protein and peptide drug delivery systems. Curr Drug Deliv. 2007;4(2):141–51.
Kreuter J, Ramge P, Petrov V, Hamm S, Gelperina SE, Engelhardt B, et al. Direct evidence that polysorbate-80-coated poly(butylcyanoacrylate) nanoparticles deliver drugs to the CNS via specific mechanisms requiring prior binding of drug to the nanoparticles. Pharm Res. 2003;20:409–16.
Simşek S, Eroğlu H, Kurum B, Ulubayram K. Brain targeting of atorvastatin loaded amphiphilic PLGA-b-PEG nanoparticles. J Microencapsul. 2013;30:10–20.
Alyautdin R, Khalin I, Nafeeza MI, Haron MH, Kuznetsov D. Nanoscale drug delivery systems and the blood-brain barrier. Int J Nanomed. 2014;9:795–811.
Gartziandia O, Herran E, Pedraz JL, Carro E, Igartua M, Hernandez RM. Chitosan coated nanostructured lipid carriers for brain delivery of proteins by intranasal administration. Colloids Surf B Biointerfaces. 2015;134:304–13.
Yemisci M, Caban S, Gursoy-Ozdemir Y, Lule S, Novoa-Carballal R, Riguera R, et al. Systemically administered brain-targeted nanoparticles transport peptides across the blood-brain barrier and provide neuroprotection. J Cereb Blood Flow Metab. 2015;35:469–75.
Ishii T, Asai T, Oyama D, Fukuta T, Yasuda N, Shimizu K, et al. Amelioration of cerebral ischemia-reperfusion injury based on liposomal drug delivery system with asialo-erythropoietin. J Control Release. 2012;160:81–7.
Ishii T, Fukuta T, Agato Y, Oyama D, Yasuda N, Shimizu K, et al. Nanoparticles accumulate in ischemic core and penumbra region even when cerebral perfusion is reduced. Biochem Biophys Res Commun. 2013;430:1201–5.
Neumann H, Takahashi K. Essential role of the microglial triggering receptor expressed on myeloid cells-2 (TREM2) for central nervous tissue immune homeostasis. J Neuroimmunol. 2007;184:92–9.
Tamás A, Reglõdi D, Szántó Z, Borsiczky B, Németh J, Lengvári I. Comparative neuroprotective effects of preischemic PACAP and VIP administration in permanent occlusion of the middle cerebral artery in rats. Neuro Endocrinol Lett. 2002;23:249–54.
Scharf E, May V, Braas KM, Shutz KC, Mao-Draayer Y. Pituitary adenylate cyclase-activating polypeptide (PACAP) and vasoactive intestinal peptide (VIP) regulate murine neural progenitor cell survival, proliferation, and differentiation. J Mol Neurosci. 2008;36:79–88.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Brifault, C., Vaudry, D., Wurtz, O. (2016). The Neuropeptide PACAP, a Potent Disease Modifier Candidate for Brain Stroke Treatment. In: Reglodi, D., Tamas, A. (eds) Pituitary Adenylate Cyclase Activating Polypeptide — PACAP. Current Topics in Neurotoxicity, vol 11. Springer, Cham. https://doi.org/10.1007/978-3-319-35135-3_34
Download citation
DOI: https://doi.org/10.1007/978-3-319-35135-3_34
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-35133-9
Online ISBN: 978-3-319-35135-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)