Abstract
The success of total knee arthroplasty can be jeopardized by wound-healing complications. This statement has been supported by a large retrospective study from Mayo Clinic that showed patient with early superficial wound complications requiring surgical intervention after primary total knee arthroplasties (TKAs) had an increased 2-year cumulative probabilities of major subsequent surgery and deep infection compared with patient without early surgical intervention, 5.3 % and 6.0 % versus 0.6 % and 0.8 %, respectively [1]. Many techniques and modalities have been incorporated in the practice of joint replacement surgeons with the intent to reduce wound complication, drainage, and subsequent infection. Often, these modalities are borrowed from other specialities and have not been validated in orthopedics. This chapter will review the most recent literature regarding wound managements related with TKAs and total knee revisions (TKRs) and will discuss our current practice.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Hyperbaric oxygen therapy
- Intraoperative management, TKA/TKR
- Adhesives
- Betadine bath
- Incision screening
- Intraoperative and early postoperative soft tissue defects
- Prophylactic flap coverage
- Suture
- Vancomycin powder
- Minor superficial wound complications, TKA/TKR
- Negative-pressure wound therapy (NPWT)
- Postoperative management, TKA/TKR
- Antiseptic use
- Dressings
- Hair removal
- Hyperbaric oxygen therapy
- Incision planning
- Negative-pressure wound therapy
- Plastic adhesive drapes
- Soft tissue expansion
- Primary wound closure, TKA/TKR
- SPY Elite®
- Total knee arthroplasty (TKA)
- Intraoperative management
- Minor superficial wound complications
- Postoperative management
- Primary wound closure
- Wound drainage
- Total knee revision (TKR)
- Wound drainage, TKA/TKR
The success of total knee arthroplasty can be jeopardized by wound-healing complications. This statement has been supported by a large retrospective study from Mayo Clinic that showed patient with early superficial wound complications requiring surgical intervention after primary total knee arthroplasties (TKAs) had an increased 2-year cumulative probabilities of major subsequent surgery and deep infection compared with patient without early surgical intervention, 5.3 % and 6.0 % versus 0.6 % and 0.8 %, respectively [1]. Many techniques and modalities have been incorporated in the practice of joint replacement surgeons with the intent to reduce wound complication, drainage, and subsequent infection. Often, these modalities are borrowed from other specialities and have not been validated in orthopedics. This chapter will review the most recent literature regarding wound managements related with TKAs and total knee revisions (TKRs) and will discuss current best practice.
Postoperative Management
General Overview
The knee has a thin overlying soft tissue envelope that must be protective, well vascularized, and supple enough to allow for the large degrees of stretch and shear required for a functional range of motion (ROM). Although most TKAs and TKRs can be performed with standard protocols, a comprehensive approach when to apply specific soft tissue management is mandatory in complex cases. Preoperative evaluation should always include a complete history and physical examination, with special emphasis in skin condition and degree of the deformity. Systemic risk factors related with general clean wound complications are obesity, malnutrition, and diabetes mellitus [2]. Among them, history of diabetes mellitus has been significantly associated with the development of early wound complications requiring surgical intervention in TKA [1]. Other systemic factors believed to be associated with increased risks of wound complication are rheumatoid arthritis, vascular compromise, prolonged use of steroids, and a history of smoking [3–5]. Local risk factors for wound complications include the inability to incorporate a previous incision into the planned incision, a small skin bridge between the previous incision and the planned incision, local radiation or burns, and dense or adherent scar tissue. As mentioned before, correction of severe knee deformity may add difficulty with closure. Special caution should be applied in patients with severe varus and rotational deformity because, as the deformity is corrected, there may not be enough skin to close the inferior aspect of the wound over the subcutaneous surface of tibia. Prior trauma about the knee may also affect adequate wound closure, and some of those problems are related to previously placed skin incisions, significant scarring, and loss of skin. A preoperative consultation with plastic surgery is advisable in any patient undergoing complex knee surgery in conjunction with systemic or local risk factors for wound complications.
Hair Removal
Hair removal has been advocated as a strategy to reduce surgical site infections (SSIs) basically by preventing hair interference with wound closure; however, a recent meta-analysis that compared 19 trials confirmed that there is lack of evidence to support preoperative hair removal in reducing SSIs. This meta-analysis also confirmed that whenever hair removal is performed, shaving was associated with higher incidence of SSIs when compared with clipping and depilatory cream [6, 7].
The Use of Antiseptic
A Cochrane systematic review that included 13 clinical trials found some evidence that preoperative skin preparation with 0.5 % chlorhexidine in methylated spirits was associated with lower rates of SSIs compared with alcohol-based povidone-iodine. Also, there is some evidence that alcohol-based products had the highest probability of being effective in reducing the SSIs. Their conclusion states that based on this poor evidence, physicians in general should make their selection using other factors such as cost and potential side effects [8]. New clinical trials are needed to define whether iodine-containing or chlorhexidine-containing solutions and the type of solution used (alcohol vs. aqueous) are superior in reducing SSIs.
Plastic Adhesive Drapes
Plastic adhesive drapes were introduced mainly with the intention of reducing infection. A practical benefit of keeping the surgical drapes in place during surgery has been another reason for its use. A Cochrane systematic review including seven RCTs found no evidence to support the use of plastic adhesive drape. Furthermore, there is some evidence that they may increase SSI. When compared iodine-impregnated plastic drapes with no drapes, iodine-impregnated drapes fail to show benefit in reducing SSIs [9]. One of the seven trials included orthopedic patients (hip fractures). One hundred and twenty patients with hip fractures were randomized to plastic adhesive drapes or left uncovered. The “drape” group had four positive wound swabs at the end of the surgery compared with only in “no drape” groups and there were no differences in postoperative SSIs [10].
Incision Planning
Previous anterior incisions present a concern regarding both the planned approach and healing potential of the skin and underlying tissue. A balance must be achieved between the ability to expose the knee through a prior incision and avoiding extensive undermining of the subcutaneous flaps. A clear history of the previous incision should be obtained, including the age of the wound, subcutaneous dissection and procedure performed, and any wound complications encountered. The previous surgical reports often provide critical information.
Understanding of the local anatomy and blood supply is also necessary. Terminal branches of the peripatellar anastomotic ring of arteries are responsible for most of the blood supply to the anterior skin and subcutaneous tissues. This occurs through a subdermal plexus supplied by arterioles in the subcutaneous fascia. Thus, flap formation over the anterior aspect of the knee must be limited and performed deep to the subcutaneous fascia. A midline skin incision is optimal and should be used whenever possible. This approach reduces the dimensions of the lateral skin flap at which lower skin oxygen tension is noted [11]. Previous longitudinal incisions can be used safely. Some degree of modification is often required to incorporate previous paramedian incisions. If multiple parallel longitudinal incisions exist, the most lateral incision is chosen, because the predominant blood supply enters medially. Johnson [11] has shown a reduction in oxygenation of the skin in the lateral region after skin incisions about the knee by the measurement of transcutaneous oxygen. Clarke and associates [12] also have described decreased oxygen tension in the incisional skin margins when using tourniquets. This hypoxia increased with tourniquet tightness. The recommended pressure is 125 mmHg above the mean blood pressure.
Transverse skin incisions, such as those from previous patellar surgery or osteotomy, can be safely approached at a 90° angle. Short oblique incisions, such as from previous meniscectomies, can often be ignored. Caution should be exercised when crossing longer oblique incisions or oblique incisions that cross the midline, because crossing these incisions may result in a narrow point at which the incisions intersect. When the planned surgical incision and prior incision create an angle of less than 60°, alternative techniques should be considered.
Soft Tissue Expansion
Soft tissue expanders are indicated when insufficient or inadequate soft tissue is present for wound healing [13, 14]. This may occur with multiple crossing and combined incisions, previous skin grafts or flaps, or severe preoperative deformity or when expanded soft tissue coverage is required. For example, when an extensor mechanism allograft as well as a TKA is to be performed, the added bulk of the extensor mechanism reconstruction may necessitate soft tissue expansion, and 8–10 weeks must be allocated for this procedure.
Intraoperative Management
Incision Screening
Laser-assisted indocyanine green angiography (LA-ICGA) has been used mainly by plastic surgeons to obtain a real-time measurement of perfusion of flaps [15]. In the setting of revision surgery, although not yet validated for knee surgery, it presents as a reasonable tool to determine the better perfused area of the skin to place the incision (Fig. 1).
Betadine Bath
In an acute periprosthetic joint infection (PJI) model in rabbits, Betadine bath in conjunction with polyethylene exchange showed a statistically significant decrease in the bacterial count on a stainless steel screw and polyethylene washer but no difference in soft tissue growth [16]. A recent meta-analysis that included 15 trials related with general, cardiovascular, orthopedic spine and urologic surgery found that povidone-iodine lavage with concentrations ranging from 0.35 % to 10 % had a reduced rate of SSI [17]. A retrospective study that included around 2500 primary total hip and knee replacement showed a statistically significant reduction in the SSIs when a 3-min Betadine lavage (0.35 %) before wound closure was incorporated into the practice of a single surgeon [18]. Although evidence leans toward a beneficial effect of intraoperative use of Betadine lavage, there is still a need for well-designed and appropriately powered clinical trial to recommend routine incorporate of this practice in joint replacement surgery.
Vancomycin Powder
Most of the literature related with the use of intra-site vancomycin powder to prevent SSIs is coming from spinal surgery practice. In a recent systematic review, the use of vancomycin powder in spinal surgery is challenged. Several poor quality studies with different definitions of SSI and different dosage made impossible an adequate evidence to support this strategy. Based on the limited literature and evidence currently available, there appears to be a protective effect of intra-site vancomycin powder on the incidence of SSIs, without evidence of side effects. Extrapolation should be performed with caution [19].
Suture
Barbed suture incorporates tiny barbs spaced evenly along the length of the suture. The principle of this knotless type of suture is to create an evenly distributed wound tension across the length of the suture line rather than at the knotted end. Barbed sutures come in both absorbable and nonabsorbable forms. The theoretical benefits are less time to close the incision, as multiple layers (subcutaneous and dermis) can be closed together with one continuous running suture; less suture “spitting,” as there are no knots to be dissolved; and minimal strangulation of tissue. While Dr. J. H. Alcamo was granted the first US patent for a unidirectional barbed suture in 1956, the concept dates back to 1951 when the idea of using barbed sutures was presented for tendon repair. Unidirectional barbed suture V-LocTM (Covidien, Mansfield, Massachusetts) was FDA approved in 2009. Initial reports showed some failures that obscured its expansion in the surgical field [20]. Bidirectional barbed suture QuillTM (Columbia, Canada) was first FDA approved in the USA in 2004. The barbs are arrayed helically around the suture and are facing in opposite directions starting from the midpoint. A cadaveric study performed by our group showed that bidirectional barbed sutures provide a more watertight closure after closure of medial parapatellar arthrotomy [21]. A biomechanical study that compared knee arthrotomy closures using interrupted biodegradable sutures and running bidirectionally barbed sutures in cadaveric specimens showed bidirectional barbed sutures were more resistant to failure after cyclic loading [22]. A recent meta-analysis assessed the clinical outcomes of barbed suture use in closure of total knee arthroplasty. Five RCTs were included with sample sizing ranging from 178 to 416. Fixed-effect analysis showed that the use of barbed sutures was associated with increased superficial infection rate and shorter estimated closure time [23]. Questioning of the real effect of decreasing TKA wound closure by several minutes and difference in skin closure among the studies makes results confusing. Despite these controversies, we believe barbered sutures may have benefits over comparable sutures.
One of the most studied antimicrobial sutures is triclosan-coated suture (e.g., Vicryl Plus®, Monocryl Plus®, and PDS Plus, Ethicon). Evidence to support the use of this type of suture is still contradictory and may be influenced by the location and the type of surgical wound. A recent systematic review and meta-analysis that included 23 randomized clinical trials, mainly related with abdominal surgery, found a robust evidence (26 % reduction in SSI) in favor of triclosan-coated suture in the prevention of SSIs when compared with non-coated suture [24]. However, a well-conducted RCT published in Lancet, triclosan-coated PDS Plus did not reduce the occurrence of surgical site infection after elective midline laparotomy [25]. Currently, there is a large multicentric clinical trial ongoing aiming to determine if the addition of triclosan-coated sutures to a standard regimen can reduce the rate of SSI after total knee replacement (TKR) and total hip replacement (THR). Results should be available soon [26].
Recently, an RCT conducted at Mayo Clinic compared the real-time perfusion of wound edges using LA-ICGA after closure of primary THA using one of the following techniques: (1) running subcuticular (3-0 monofilament), (2) vertical mattress (2-0 nylon), or (3) skin staples. The running subcuticular closure demonstrated the least impairment of perfusion among the closures compared [27].
Adhesives
PrineoTM ® (Ethicon Products, Somerville, NJ, USA) is a two-component wound closure system consisting of a self-adhering mesh together with a liquid adhesive (octyl-2-cyanoacrylate). Two clinical trials in abdominal surgery have concluded that PrineoTM ® is comparable with intradermal sutures for abdominoplasty with regard to cosmesis, safety, and effectiveness [28]. Although there are some cases of allergic reaction to Dermabond®[29, 30], this method of suture seems to be safe and effective in joint replacement surgery. Further adequately powered trials will be needed to support the use of this system instead of other suture methods.
Prophylactic Flap Coverage
The best candidates for prophylactic flap coverage are patients with prior skin graft, local irradiation, or densely adherent scar tissue. The choice of flap depends on the location of the lesion, extent of coverage required, and status of the limb. Most lesions can be covered adequately with a medial or lateral gastrocnemius muscle flap or myocutaneous flap. Lesions proximal to the superior pole of the patella may require a free flap. The principles involve excision of the area of concern followed by soft tissue coverage. A minimum of 12 weeks should be allowed between coverage and subsequent arthroplasty. Available data demonstrate successful outcomes in most patients. However, because the indications for this procedure are few, results are extremely limited.
Intraoperative and Early Postoperative Soft Tissue Defects
The treatment of soft tissue defects about the knee depends on the site, location, presence of infection, and, perhaps most importantly, if there is bone, tendon or implant exposure. Necrotic tissues and contaminated foreign materials must be removed. The size of the soft tissue defect should be estimated with the knee at a maximum flexion and the “like with like” tissue replacement principle should always be applied. Generally speaking the options are conservative wound management and debridement with or without reconstruction. When the resulting defect is deep with exposed bone or hardware, or infection is documented, flaps are needed to successful salvage of the lower extremity [31]. In general, the ability to perform a medial gastrocnemius muscle flap and skin graft is an invaluable skill in complex cases where primary wound closure cannot be achieved. Gravvanis et al. propose the following reconstructive algorithm [32].
Small (Less Than 4 cm)
In non-exposed defects, split thickness skin grafts with or without vacuum-assisted closure (VAC) therapy are advised. If the defects are not complicated with infection, skin flaps present the advantage of less morbidity, pliable, and better cosmesis outcomes. Perforator flaps, such as medial sural artery perforator flap, are versatile but require microsurgical expertise. Muscular flaps are indicated particularly in infected wound defects. Gastrocnemius flap is a reliable option with minimal donor site morbidity. Supra-patellar soft tissue defects are better approached with distally based thigh muscle flaps such as sartorius or gracilis.
Moderate Defects (4–6 cm)
When the defects are not more than superficial defects, medial sural artery perforator flap and distally based anterolateral thigh (ALT) flap are recommended. If the defect is deep, a gastrocnemius flap or distally based vastus lateralis flap are recommended. Results with gastrocnemius flap coverage following TKA have been good, with series reporting up to a 96 % success rate. Poor results have been demonstrated in the face of chronic infection and delayed soft tissue coverage. Complication rates increase with attempted coverage of more proximal lesions over the patellar or quadriceps tendon. Nahabedian et al. [31] published their results on the operative management and outcome of complex wounds following total knee arthroplasty. Of 27 patients requiring coverage with a medial gastroc flap, 9 patients (33 %) required a second operation and the prosthesis was salvaged in 83 % of patients
Large Defects (>6 cm)
For large defects or severely damaged limbs, the best solution is a free flap. ALT, vastus lateralis, or latissimus dorsi free flaps are the most commonly used. A comprehensive vascular imaging study is recommended to choose the appropriate recipient vessel. The choice of the recipient vessels may direct the choice of the most suitable flap. Free flaps around the knee are indicated when local flaps are insufficient due to the location or size of defect or the compromised status of the traditional gastrocnemius flap. Usually defects larger than 6 cm require free flaps [32]. In a recent report, in 34 cases of soft tissue reconstruction of the knee with free flaps, 33 (97 %) of 34 flaps survived [33].
Postoperative Management
Dressings
A systematic review showed that there is insufficient evidence as to whether covering surgical wounds healing by primary intention with wound dressings reduces the risk of SSI. Also, whether any particular wound dressing is more effective than others in reducing the rates of SSIs, improving scarring, pain control, patient acceptability, or ease of dressing removal still remains unclear. Therefore, authors conclude that decisions on wound dressing should be based on dressing costs and the symptom management properties offered by each dressing type, e.g., exudate management [34]. Whether early dressing removal (within 48 h) increases the risk of SSI compared with late removal (after 48 h), a recent systematic review found no detrimental effect on outcomes in early removal of dressings from clean or clean-contaminated surgical wounds. Authors mentioned though, these conclusion are based on poor quality evidence and further randomized controlled trials are required to investigate whether dressings are necessary after 48 h in different types of surgery and levels of contamination [35].
Negative-Pressure Wound Therapy
The theoretical benefits of negative-pressure wound therapy (NPWT) include removing fluids and infectious materials from the incision site, reducing tension across the surgical incision, improving blood flow to the peri-incisional tissue, and acting as a barrier to external infectious sources. Evidence to support the use of NPWT to prevent surgical site infection SSIs and wound dehiscence in wounds healing by secondary intension remains unclear [36]. The use of incisional NPWT (INPWT) was first introduced in 2006 as a means to provide a clean, dry environment for high-risk wounds. An RCT has shown lower rates of wound drainage and dehiscence and strong trend in decreasing infection rate in high-risk lower extremities fractures [37]. Another RCT has shown decreased development of postoperative seromas, reduction of total wound secretion days, and reduction of needed time for dressing changes and wound healing after femoral neck fracture (FNF) treated with hip hemiarthroplasty (HA) [38]. Despite this promising evidence, a recent systematic review and meta-analysis concluded that further studies are needed for proper recommendations on INPWT [39, 40]. Currently there is no rigorous evidence available regarding the clinical effectiveness of INPWT in the treatment of surgical wounds following total joint arthroplasty. The authors experience with INPWT for high-risk wounds in the morbidly obesity, revision and reimplantation surgery, and for early management of wound drainage has anecdotally been promising.
Hyperbaric Oxygen Therapy
There is sufficient evidence to support the use of hyperbaric oxygen therapy (HBOT) in the managements of complex wound with HBOT in combination with standard wound care principles, especially in wounds augmented with flaps [41, 42]. Further investigation is required before it can be recommended as a mainstay in adjuvant wound therapy for complex knee wounds [43].
Our Current Protocol
Wound closure and management has changed dramatically over the past 5 years. The changes have led to an anecdotal improvement in patient satisfaction, a less surgeon involvement for routine wound care, a lower superficial wound complication rates, and ultimately a trend toward a lower infection rate.
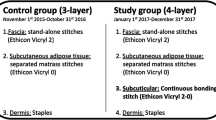
Primary Wound Closure
The knee arthrotomy is closed with #2 polydioxanone bidirectional barbed suture (Fig. 2). The subcutaneous fat is then re-approximated with #0 polydioxanone bidirectional barbed suture (Fig. 3), and the subcuticular layer is closed with bidirectional barbed 3-0 monofilament suture (Fig. 4). By using bidirectional barbed suture, TKA wound closure times have been reduced by 50 % from an average of 22 to 12 min. The incision is then reinforced with PrineoTM ® system (Ethicon Products, Somerville, NJ, USA.) (Fig. 5), a topical skin adhesive and a flexible self-adhesive mesh. The combined use of barbed suture and the liquid adhesive, has reduced any immediate wound drainage or leakage. This has allowed for a simple approach to the surgical dressing with a single layer of non-adherent gauze and a transparent film (3 M Tegaderm®) (Fig. 6).
The initial surgical dressing is changed on POD #2 for visual inspection of the wound. The dressing is replaced with the same non-adherent gauze and transparent film. The dressing is left in place until POD #10 and then discarded and the wound is left open to air. The PrineoTM ® dressing is peeled from the skin at the first postoperative visit at 3 weeks from surgery.
Incisional NPWT systems (PrevenaTM, KCI Licensing 2013) are utilized in high-risk patients. Pre-sized and customizable options exist depending on incision length and shape. While a strict protocol has not been established, morbid obesity (body mass index >45), revision surgery, reimplantation surgery, and surgeries for active infection include some current indications for use. The incisional NPWT dressing is left in place for 7 days postoperatively and then discarded (Fig. 7).
Minor Superficial Wound Complications
An additional benefit of the use of the bidirectional barbed suture closure is that the surgeon may move away from the subcuticular interrupted suture. Subcuticular interrupted suture often results in minor wound disruption during suture resorption and breakdown. This can often lead to “suture abscess” formation and minor wound dehiscence. For the routine suture reaction, observation without antibiotics and wound care frequently shows wound healing without complication. If oral antibiotics are considered, knee aspiration should be strongly considered first. In the event that the presumed superficial wound complication is the first sign of a more substantial “deep” infection, it will be critical to obtain an accurate wound culture for subsequent treatment before antibiotics are implemented.
Encouraging results have been reported using a topical clostridium hemolyticus collagenase ointment (Santyl®, Smith & Nephew) for treatment of diabetic foot ulcers [44, 45]. Although there is no literature to support the use of this debridement ointment in knee surgery wound complications, this practice to treat superficial wound dehiscences associated with devitalized tissue is effective (Figs. 8 and 9). The wound is cleaned with sterile saline, and then the collagenase is liberally applied directly to the open wound daily and covered with sterile gauze. The collagenase is most effective in a moist environment; so if the wound is very dry, some additional saline may be added to the wound bed. The collagenase is continued until the wound is epithelized.
Wound Drainage
Wound drainage has been pointed out as a risk factor for periprosthetic joint infection (PJI) [46]. In a study coming from Mayo Clinic, obesity, the use of low-molecular-weight heparin, and high drain output were identified as risk factors for draining wound in primary THA [47].
The majority of wound closures with a tight layered closure and skin adhesives should be completely dry. If slight spotting on the surgical dressings is noted during the first 3 days post-op, postoperative protocols are not changed. The rescue plan is employed if the dressings become saturated early or any drainage persists after 3 days. The initial rescue plan consists of holding aggressive chemical anticoagulation (low-molecular-weight heparins are changed to aspirin), the placement of a bulky compressive dressing, and knee immobilization. Daily dressings are then performed and routine postoperative care resumes once the wound is dry for 24 h. If drainage persists more 2 days despite immobilization and a bulky compressive dressing or if drainage remains significant, the placement of an incisional NPWT dressing is considered. Commercially available systems can be used, but if drainage is significant, a standard NPWT system with a larger canister is often necessary. The incisional NPWT dressing is left in place up to 7 days post-op. If any drainage persists after 1 week, return to the operating room is strongly considered.
References
Galat DD, et al. Surgical treatment of early wound complications following primary total knee arthroplasty. J Bone Joint Surg Am. 2009;91(1):48–54.
Cruse PJ, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107(2):206–10.
Escalante A, Beardmore TD. Risk factors for early wound complications after orthopedic surgery for rheumatoid arthritis. J Rheumatol. 1995;22(10):1844–51.
Vince K, Chivas D, Droll KP. Wound complications after total knee arthroplasty. J Arthroplasty. 2007;22(4 Suppl 1):39–44.
Sorensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(6):1069–79.
Tanner J, Norrie P, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011;11:CD004122.
Lefebvre A, et al. Preoperative hair removal and surgical site infections: network meta-analysis of randomized controlled trials. J Hosp Infect. 2015;91(2):100–8.
Dumville JC, et al. Preoperative skin antiseptics for preventing surgical wound infections after clean surgery. Cochrane Database Syst Rev. 2015;4:CD003949.
Webster J, Alghamdi A. Use of plastic adhesive drapes during surgery for preventing surgical site infection. Cochrane Database Syst Rev. 2015;4:CD006353.
Chiu KY, et al. Plastic adhesive drapes and wound infection after hip fracture surgery. Aust N Z J Surg. 1993;63(10):798–801.
Johnson DP. Midline or parapatellar incision for knee arthroplasty. A comparative study of wound viability. J Bone Joint Surg. 1988;70(4):656–8.
Clarke MT, et al. Tourniquet-induced wound hypoxia after total knee replacement. J Bone Joint Surg. 2001;83(1):40–4.
Long WJ, et al. 15-year experience with soft tissue expansion in total knee arthroplasty. J Arthroplasty. 2012;27(3):362–7.
Manifold SG, et al. Long-term results of total knee arthroplasty after the use of soft tissue expanders. Clin Orthop Relat Res. 2000;380:133–9.
Munabi NC, et al. The ability of intra-operative perfusion mapping with laser-assisted indocyanine green angiography to predict mastectomy flap necrosis in breast reconstruction: a prospective trial. J Plast Reconstr Aesthet Surg JPRAS. 2014;67(4):449–55.
Gilotra M, et al. Dilute betadine lavage reduces implant-related bacterial burden in a rabbit knee prosthetic infection model. Am J Orthop. 2015;44(2):E38–41.
Fournel I, et al. Meta-analysis of intraoperative povidone-iodine application to prevent surgical-site infection. Br J Surg. 2010;97(11):1603–13.
Brown NM, et al. Dilute betadine lavage before closure for the prevention of acute postoperative deep periprosthetic joint infection. J Arthroplasty. 2012;27(1):27–30.
Kang DG, et al. Intrasite vancomycin powder for the prevention of surgical site infection in spine surgery: a systematic literature review. Spine J Off J N Am Spine Soc. 2015;15(4):762–70.
Patel RM, et al. Wound complications in joint arthroplasty: comparing traditional and modern methods of skin closure. Orthopedics. 2012;35(5):e641–6.
Nett M, et al. Water-tight knee arthrotomy closure: comparison of a novel single bidirectional barbed self-retaining running suture versus conventional interrupted sutures. J Knee Surg. 2011;24(1):55–9.
Vakil JJ, et al. Knee arthrotomy repair with a continuous barbed suture: a biomechanical study. J Arthroplasty. 2011;26(5):710–3.
Meena S, et al. Barbed versus standard sutures in total knee arthroplasty: a meta-analysis. Eur J Orthop Surg Traumatol. 2015;25(6):1105–10.
Apisarnthanarak A, et al. Triclosan-coated sutures reduce the risk of surgical site infections: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36(2):169–79.
Diener MK, et al. Effectiveness of triclosan-coated PDS Plus versus uncoated PDS II sutures for prevention of surgical site infection after abdominal wall closure: the randomised controlled PROUD trial. Lancet. 2014;384(9938):142–52.
Sprowson AP, et al. The effect of triclosan coated sutures on rate of Surgical Site Infection after hip and knee replacement: a protocol for a double-blind randomised controlled trial. BMC Musculoskelet Disord. 2014;15:237.
Wyles CC, et al. The Chitranjan Ranawat award: running subcuticular closure enables the most robust perfusion after TKA: a Clin Orthop Relat Res. 2016;474(1):47–56.
Richter D, et al. A comparison of a new skin closure device and intradermal sutures in the closure of full-thickness surgical incisions. Plast Reconstr Surg. 2012;130(4):843–50.
Dunst KM, et al. Extensive allergic reaction to a new wound closure device (Prineo (TM)). Allergy. 2010;65(6):798–9.
Durando D, et al. Allergic contact dermatitis to dermabond (2-octyl cyanoacrylate) after total knee arthroplasty. Dermat Contact Atopic Occup Drug. 2014;25(2):99–100.
Nahabedian MY, et al. Salvage procedures for complex soft tissue defects of the knee. Clin Orthop Relat Res. 1998;356:119–24.
Gravvanis A, et al. Flap reconstruction of the knee: a review of current concepts and a proposed algorithm. World J Orthop. 2014;5(5):603–13.
Louer CR, et al. Free flap reconstruction of the knee an outcome study of 34 cases. Ann Plast Surg. 2015;74(1):57–63.
Dumville JC, et al. Dressings for the prevention of surgical site infection. Cochrane Database Syst Rev. 2014;9:CD003091.
Toon CD, et al. Early versus delayed dressing removal after primary closure of clean and clean-contaminated surgical wounds. Cochrane Database Syst Rev. 2015;9:CD010259.
Dumville JC, et al. Negative pressure wound therapy for treating surgical wounds healing by secondary intention. Cochrane Database Syst Rev. 2015;6:CD011278.
Stannard JP, et al. Incisional negative pressure wound therapy after high-risk lower extremity fractures. J Orthop Trauma. 2012;26(1):37–42.
Hansen E, et al. Negative pressure wound therapy is associated with resolution of incisional drainage in most wounds after hip arthroplasty. Clin Orthop Relat Res. 2013;471(10):3230–6.
Webster J, et al. Negative pressure wound therapy for skin grafts and surgical wounds healing by primary intention. Cochrane Database Syst Rev. 2014;10:CD009261.
Scalise A, et al. Improving wound healing and preventing surgical site complications of closed surgical incisions: a possible role of Incisional Negative Pressure Wound Therapy. A systematic review of the literature. Int Wound J. 2015. [Epub ahead of print].
Dauwe PB, et al. Does hyperbaric oxygen therapy work in facilitating acute wound healing: a systematic review. Plast Reconstr Surg. 2014;133(2):208e–15.
Gehmert S, et al. Evaluation of hyperbaric oxygen therapy for free flaps using planar optical oxygen sensors. Preliminary results. Clin Hemorheol Microcirc. 2011;48(1):75–9.
Eskes A, et al. Hyperbaric oxygen therapy for treating acute surgical and traumatic wounds. Cochrane Database Syst Rev. 2013;12:CD008059.
Motley TA, et al. Cost-effectiveness of clostridial collagenase ointment on wound closure in patients with diabetic foot ulcers: economic analysis of results from a multicenter, randomized, open-label trial. J Foot Ankle Res. 2015;8:7.
Tallis A, et al. Clinical and economic assessment of diabetic foot ulcer debridement with collagenase: results of a randomized controlled study. Clin Ther. 2013;35(11):1805–20.
Saleh K, et al. Predictors of wound infection in hip and knee joint replacement: results from a 20 year surveillance program. J Orthop Res Off Publ Orthop Res Soc. 2002;20(3):506–15.
Patel VP, et al. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89(1):33–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this entry
Cite this entry
Nett, M., Norambuena, G.A. (2016). Advances in Wound Closure. In: Scuderi, G., Tria, A. (eds) Minimally Invasive Surgery in Orthopedics. Springer, Cham. https://doi.org/10.1007/978-3-319-34109-5_132
Download citation
DOI: https://doi.org/10.1007/978-3-319-34109-5_132
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-34107-1
Online ISBN: 978-3-319-34109-5
eBook Packages: MedicineReference Module Medicine