Abstract
Acute kidney injury is a frequent complication of cardiac surgery that has significant prognostic implications. Therefore, there has been extensive research to find effective interventions for preventing this important complication. N-acetylcysteine has anti-inflammatory, antioxidant, and renal vasodilator properties that may mitigate several mechanisms of acute kidney injury after cardiac surgery. Consequently, it has been evaluated as a potential therapeutic agent in several randomized controlled trials in cardiac surgery. While a small single-center randomized controlled trial found a survival benefit with perioperative N-acetylcysteine treatment, these benefits were not confirmed in other trials or in meta-analyses of these trials. Conversely, N-acetylcysteine use during cardiac surgery appears safe. While some trials have observed increased perioperative blood loss with N-acetylcysteine use, this risk was not confirmed in a meta-analysis of contemporary trials. Overall, there is weak to no evidence for recommending N-acetylcysteine as a treatment to improve survival in patients undergoing cardiac surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute Kidney Injury
- Cardiac Surgery Patient
- Large Multicenter Trial
- Weak Recommendation
- Ischemic Renal Injury
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 General Principles
Acute kidney injury (AKI) is a frequent complication of cardiac surgery, affecting up to 30 % of patients [1, 2]. Patients who experience AKI after cardiac surgery have a higher risk for postoperative morbidity, as well as increased short-term and long-term mortality [1, 2]. The important prognostic implications of postoperative AKI have prompted extensive research in the quest to find treatments to reduce mortality in this population. Despite these efforts, there remains a paucity of interventions proven to prevent AKI after cardiac surgery. Most assessed interventions, such as diuretics, low-dose dopamine, and mannitol, have shown minimal, if any benefit, in small randomized controlled trials [3]. A few other interventions (e.g., fenoldopam, off-pump cardiac surgery) showed promise in initial small trials [4, 5] but then failed to confirm these benefits in larger multicenter trials [6, 7].
2 Pharmacologic Properties
AKI after cardiac surgery is likely multifactorial in etiology, with several different underlying mechanisms of injury [8]. These mechanisms include ischemic renal injury, reduced nitric oxide activity, and oxygen-free radical injury due to ischemia-reperfusion, cardiopulmonary bypass, nephrotoxins, or reduced plasma glutathione concentration. N-acetylcysteine (NAC) has the potential to inhibit several of these mechanisms [9], in that it directly scavenges free radicals, improves blood flow through nitric oxide-mediated pathways, and functions as a precursor for glutathione synthesis.
While there is physiological rationale for NAC being able to prevent postoperative AKI, it is likely that the major impetus for its application in cardiac surgery was due to the initial promising data in the setting of contrast-induced nephropathy. In 2000, Tepel and colleagues [10] published a small placebo-controlled randomized trial on 83 participants in which prophylactic oral administration of NAC significantly reduced AKI rates in patients with chronic renal failure receiving intravenous radiographic contrast agents. Their initial promising results led to numerous subsequent studies that evaluated the effects of different doses and formulations of NAC in the prevention of contrast-induced nephropathy. Despite the early enthusiasm, the benefits of NAC for preventing contrast-induced nephropathy were not consistently replicated in subsequent small trials [11], meta-analyses of such trials [12], or a single large multicenter trial involving 2308 participants [13]. Furthermore, doubts have been raised about the artifactual effect of NAC on biochemical assays for creatinine, which may have explained the positive results seen in some trials [14].
3 Main Evidence
Analogous to the evolution of evidence for the efficacy of N-acetylcysteine to prevent contrast-induced nephropathy, conflicting results have also emerged from research into its efficacy for preventing perioperative AKI in cardiac surgery patients. In general, research to date has identified no major consistent clinical benefits of NAC in cardiac surgery.
A recent meta-analysis (see Table 12.1) showed that the perioperative use of NAC has no proven benefit for clinically important outcomes in patients undergoing cardiac surgery, such as death or need for renal replacement therapy (RRT) [15]. In meta-regression analyses, treatment effects on AKI were not related to the dose of N-acetylcysteine. In addition, no significant differences were found between the NAC and placebo groups with respect to the risks of increase in serum creatinine concentration by 25 % or greater above baseline, acute myocardial infarction, atrial fibrillation, stroke, infection, intra-aortic balloon pump (IABP) support, vasopressor or inotropic support, prolonged mechanical ventilation, length of mechanical ventilation, intensive care unit (ICU) stay, or hospital length of stay [15].
Consistent with the findings of this meta-analysis, a recent web-based international consensus conference issued only a weak recommendation for NAC as a treatment to improve survival in patients undergoing cardiac surgery [16].
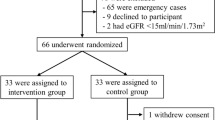
The basis for even a weak recommendation was a small single-center randomized controlled trial that found a survival benefit with NAC treatment in 177 cardiac surgery patients with moderate preexisting renal failure [17]. In this study, Wijeysundera and colleagues evaluated a high-dose intravenous N-acetylcysteine regimen (100 mg/kg bolus in 30 min after induction of anesthesia, followed by 20 mg kg−1 h−1 infusion until 4 h after cardiopulmonary bypass) in a randomized placebo-controlled trial where the primary outcome was the percent change in estimated glomerular filtration rate (GFR) during the first 72 postoperative hours [17]. While the authors found no significant effect on the primary outcome, they reported a significant reduction in all-cause mortality among individuals randomized to NAC. These findings should be viewed cautiously since all-cause mortality was a secondary outcome, and there were only seven mortality events in the trial. Furthermore, as indicated previously, these benefits with respect to mortality were not confirmed in subsequent trials and meta-analyses [16].
The absence of consistent benefit has also been observed in recent small randomized trials published after the previously described meta-analysis [15] and consensus conference [16]. For example, in a trial that assessed NAC for preventing AKI in 117 high-risk patients undergoing off-pump coronary artery bypass surgery, Song and colleagues [18] showed no significant benefits of this treatment as compared to placebo. Conversely, Santana-Santos and colleagues [19] reported that high-dose intravenous NAC (150 mg/kg bolus followed by 50 mg/kg infusion for 6 h) reduced the risk of AKI, abolished oxidative stress, and mitigated the negative effect of cardiopulmonary bypass on renal function in 70 patients with chronic kidney disease undergoing coronary artery bypass graft surgery. In contrast to some of the previous studies, Santana-Santos and colleagues offered evidence that NAC abolishes the increase in circulating reactive oxygen species observed in the control group, thus confirming a plausible mechanistic explanation for the observed nephroprotective effect.
4 Therapeutic Use
N-acetylcysteine can be administered orally or intravenously. The bioavailability after oral administration is approximately 6–10 %. Renal clearance constitutes 30 % of total body clearance, and the elimination half-life is 2.3 h. Several dosing regimens of NAC for patients undergoing cardiac surgery have been described in the literature. Some protocols included oral administration before and/or after surgery, with doses of 600 mg twice a day for different durations of time (3–7 days, starting preoperatively). Intravenous regimens typically involved a bolus (50–150 mg/kg) before the beginning of surgery, followed by subsequent boluses (600 or 1200 mg every 12 h until 24 or 36 h postoperatively) or infusion of varying doses (from approximately 2–20 mg kg−1 h−1) and duration (from until the end of surgery to 48 h postoperatively). The abovementioned recent meta-analysis reported that the median perioperative total dose used in previous studies of NAC in cardiac surgery was 9425 mg (range 2400–34,950 mg) [15].
In general, there are no contraindications to use NAC in cardiac surgery. It is not associated with major adverse effects. High-dose intravenous use, typically exceeding 150 mg/kg, carries the potential risk of anaphylactoid reactions [18]. Chronic systemic NAC administration has been shown to cause pulmonary hypertension in an experimental murine model [16], but no similar effects have been described to date in clinical or acute administration settings. Notably, both Wijeysundera and colleagues [20] and Naughton and colleagues [12] described the potential for NAC to be associated with increased blood loss and blood products transfusion in cardiac surgery patients with preexisting moderate renal failure. Nonetheless, further research did not confirm these findings, with the meta-analysis by Wang and colleagues [15] concluding that NAC had no significant impact on postoperative chest tube drainage, surgical re-exploration, reoperation for bleeding, and red blood cell transfusion requirements.
To date, no major consistent clinical benefits of N-acetylcysteine have been identified in the setting of cardiac surgery. There is weak to no evidence for recommending it as a treatment to improve survival in this patient population.
Clinical Summary
Drug/technique | Indications | Cautions | Side effects | Dose | Notes |
|---|---|---|---|---|---|
N-acetylcysteine (NAC) | Patients undergoing cardiac surgery with or without preexisting chronic renal dysfunction (not on preoperative dialysis) | There are some data suggesting that NAC interferes with the usual biochemical assay for creatinine. This finding might explain why measures of renal function sometimes appear better with the use of NAC | Side effects are rare They include anaphylactoid reactions. Increased blood loss and blood product transfusion requirements have been described; however, these side effects were not confirmed by recent meta-analysis | Multiple regimens described, with no proven differences between different protocols Oral 600 mg twice a day from preoperative day 1 to postoperative day 1–5 Intravenous bolus preoperatively/pre-cardiopulmonary bypass (1200 mg intravenous bolus or 50–150 mg/kg) followed by intravenous repeated bolus/infusion for up to 36 h postoperatively Median total dose among trials was 9425 mg (range 2400–34,950 mg) | The findings of several trials and meta-analyses only justify a weak recommendation for considering NAC as a treatment to improve survival in patients undergoing cardiac surgery |
References
Pickering JW, James MT, Palmer SC (2015) Acute kidney injury and prognosis after cardiopulmonary bypass: a meta-analysis of cohort studies. Am J Kidney Dis 65(2):283–293
Kandler K, Jensen ME, Nilsson JC et al (2014) Acute kidney injury is independently associated with higher mortality after cardiac surgery. J Cardiothorac Vasc Anesth 28(6):1448–1452
Park M, Coca SG, Nigwekar SU et al (2010) Prevention and treatment of acute kidney injury in patients undergoing cardiac surgery: a systematic review. Am J Nephrol 31(5):408–418
Zangrillo A, Biondi-Zoccai GG, Frati E et al (2012) Fenoldopam and acute renal failure in cardiac surgery: a meta-analysis of randomized placebo-controlled trials. J Cardiothorac Vasc Anesth 26(3):407–413
Nigwekar SU, Kandula P, Hix JK, Thakar CV (2009) Off-pump coronary artery bypass surgery and acute kidney injury: a meta-analysis of randomized and observational studies. Am J Kidney Dis 54(3):413–423
Garg AX, Devereaux PJ, Yusuf S et al (2014) Kidney function after off-pump or on-pump coronary artery bypass graft surgery: a randomized clinical trial. JAMA 311(21):2191–2198
Bove T, Zangrillo A, Guarracino F et al (2014) Effect of fenoldopam on use of renal replacement therapy among patients with acute kidney injury after cardiac surgery: a randomized clinical trial. JAMA 312(21):2244–2253
Rosner MH, Okusa MD (2006) Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol 1:19–32
Borgström L, Kågedal B, Paulsen O (1986) Pharmacokinetics of N-acetylcysteine in man. Eur J Clin Pharmacol 31(2):217–222
Tepel M, van der Giet M, Schwarzfeld C et al (2000) Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. N Engl J Med 343(3):180–184
Bagshaw SM, McAlister FA, Manns BJ et al (2006) Acetylcysteine in the prevention of contrast-induced nephropathy: a case study of the pitfalls in the evolution of evidence. Arch Intern Med 166:161e6
Naughton F, Wijeysundera D, Karkouti K et al (2008) N-acetylcysteine to reduce renal failure after cardiac surgery: a systematic review and meta-analysis. Can J Anaesth 55(12):827–835
ACT Investigators (2011) Acetylcysteine for prevention of renal outcomes in patients undergoing coronary and peripheral vascular angiography: main results from the randomized Acetylcysteine for Contrast-induced nephropathy Trial (ACT). Circulation 124(11):1250–1259
Hoffmann U, Fischereder M, Kruger B et al (2004) The value of N-acetylcysteine in the prevention of radiocontrast agent-induced nephropathy seems questionable. J Am Soc Nephrol 15:407e10
Wang G, Bainbridge D, Martin J, Cheng D (2011) N-acetylcysteine in cardiac surgery: do the benefits outweigh the risks? A meta-analytic reappraisal. J Cardiothorac Vasc Anesth 25(2):268–275
Landoni G, Bove T, Székely A et al (2013) Reducing mortality in acute kidney injury patients: systematic review and international web-based survey. J Cardiothorac Vasc Anesth 27(6):1384–1398
Wijeysundera DN, Beattie WS, Rao V et al (2007) N-acetylcysteine for preventing acute kidney injury in cardiac surgery patients with pre-existing moderate renal insufficiency. Can J Anesth 54(11):872–881
Koppen A, van Riel A, de Vries I, Meulenbelt J (2014) Recommendations for the paracetamol treatment nomogram and side effects of N-acetylcysteine. Neth J Med 72(5):251–257
Santana-Santos E, Gowdak LH, Gaiotto FA et al (2014) High dose of N-acetylcysteine prevents acute kidney injury in chronic kidney disease patients undergoing myocardial revascularization. Ann Thorac Surg 97(5):1617–1623
Wijeysundera DN, Karkouti K, Rao V et al (2009) N-acetylcysteine is associated with increased blood loss and blood product utilization during cardiac surgery. Crit Care Med 37(6):1929–1934
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Parotto, M., Wijeysundera, D.N. (2016). N-acetylcysteine to Reduce Mortality in Cardiac Surgery. In: Landoni, G., Pisano, A., Zangrillo, A., Bellomo, R. (eds) Reducing Mortality in Acute Kidney Injury. Springer, Cham. https://doi.org/10.1007/978-3-319-33429-5_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-33429-5_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-33427-1
Online ISBN: 978-3-319-33429-5
eBook Packages: MedicineMedicine (R0)