Abstract
Chronic kidney disease (CKD) is common among older adults and associated with adverse health outcomes. Despite the high burden of CKD at older ages, the general approach to kidney disease is based on evidence from young and middle-aged adults and may not apply to older adults with CKD. The purpose of this chapter is to identify the unique aspects of caring for older adults from early stages of CKD through end-of-life. We describe an approach that recognizes the impact of non-CKD factors on the lives of CKD patients and recommends geriatric assessment to facilitate the development of individualized care plans.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Chronic kidney disease (CKD) is common among older adults and associated with mortality, cardiovascular disease, and increased heath care utilization [1]. Despite the high burden of CKD at older ages , the general approach to kidney disease is based on evidence from young and middle-aged adults and may not apply to older adults with CKD. At younger ages, CKD is often a progressive disorder and the prevention of kidney failure is a key goal. Older patients with CKD may face different challenges [2]. The very old with CKD are 10–20 times more likely to die before progressing to kidney failure [3]. Older adults with CKD often have multiple chronic conditions and may be at increased risk for functional decline, cognitive impairment, and frailty. For the small proportion, but growing absolute number, of older adults who have CKD progression, initiation of dialysis is associated with a poor prognosis and high burden of functional impairment [4, 5].
The purpose of this chapter is to identify the unique aspects of caring for older adults from early stages of CKD through kidney failure and end-of-life. We describe an approach to older adults with CKD that recognizes the impact of non-CKD factors on the lives of CKD patients and recommends geriatric assessment to facilitate the development of individualized care plans. For background, we describe age-related changes in kidney structure and function, provide definitions of CKD, kidney failure, and related disorders, and report on the prevalence of kidney disease among older adults. Next we describe the limitations of a disease-oriented approach to kidney disease in older adults and propose an alternative approach that focuses on providing individualized, patient-centered care. Additionally, we provide detailed descriptions of the unique challenges that arise in older patients with acute kidney injury (AKI) , early stages of CKD, and among those with kidney failure. In the final two sections of this chapter we describe kidney disease in special patient populations and end-of-life considerations.
2 The Aging Kidney
Structural and functional changes in the kidney have been described with aging. Structural changes include a decrease in overall kidney mass with autopsy studies showing a decrease from 400 g at age 40 to less than 300 g at age 90 [6]. This decrease in mass has been shown to be primarily due to a decrease in the renal cortices with sparing of the renal medulla. While reductions in glomerular number have also been shown, there is a large amount of variability in glomerular number from one older adult to another. Additionally, the incidence of glomerular sclerosis increases with older age with sclerosis present in <5 % of the glomeruli of those 40 years old compared to 30 % of glomeruli exhibiting evidence of sclerosis at age 80 [6]. The contribution of age-related increase in collagen production in the glomerulus versus disease-related pathology remains poorly understood [7].
Declines in kidney function at older ages including reduced glomerular filtration rate (GFR ) have also been shown. Cross sectional studies have shown a lower median estimated GFR (eGFR) at older ages, but do not provide information about changes in kidney function within individual patients [6]. In one longitudinal study, declines in creatinine clearance, a maker of GFR, were shown to decrease on average by 0.75 ml/min/year among health aging study participants [8]. However, one third of participants without hypertension or urological disease experienced no decline in kidney function, raising the question of whether or not decrease in GFR is inevitable with aging [8]. The decrease in GFR with age has been attributed in part to increasing glomerular sclerosis with age. However, one analysis of kidney biopsies from renal transplant donors that included older adults reported poor correlation between level of GFR and the amount of sclerosis [9]. Therefore, the burden of sclerosis may not predict the level of kidney function. The relationship between aging, disease-related pathology, response mechanisms to increase glomerular filtration , and clinical markers of kidney function is complex and many of the biological processes remain unknown.
3 Kidney Disease Terminology and Epidemiology
3.1 Kidney Disease Definitions
CKD is defined as abnormalities in kidney structure or function that persist for at least 3 months and have implications for health [10]. Markers of kidney damage include the abnormal presence of protein (proteinuria) or albumin (albuminuria) in the urine. Kidney function is assessed using GFR. Because measuring GFR is rarely available in the clinical setting, definitions of CKD rely on eGFR from formulas that use serum creatinine, age, and race. Decreased eGFR is defined as <60 ml/min/1.73 m2. In Sect. 25.6 below, we discuss the challenges and controversies for identifying CKD in older populations using this cut-point to define CKD.
Current CKD clinical practice guidelines use these biomarkers of abnormal kidney function (i.e., eGFR and albuminuria ) to both define CKD and stage the disease based on prognosis for CKD-related outcomes. Guidelines recommend a classification and staging system that is based on (1) cause, (2) GFR category , and (3) albuminuria category (ACR) (Table 25.1) . While hypertension and diabetes are the most common causes of CKD among older adults, other causes include renal vascular disease, chronic urinary obstruction, systemic vasculitis, multiple myeloma or intrinsic kidney disorders such as glomerulonephritis or nephrotic syndrome. As with many multifactorial geriatric syndromes, for older adults, kidney disease may have more than one cause (e.g., renal vascular disease with chronic urinary obstruction). Clinical practice guidelines recommend categorizing kidney stage by both eGFR level and ACR level because of the improved risk stratification for mortality, kidney failure, AKI, and progressive CKD when eGFR and ACR are considered together. As an example, a patient with CKD related to diabetes with an eGFR of 32 ml/min/1.73 m2 and ACR of 150 mg/g would be classified as diabetic CKD, G3b, A2.
As CKD progresses , patients may develop kidney failure defined as an eGFR <15 ml/min/1.73 m2 or the need to initiate renal replacement therapy (RRT; hemodialysis or peritoneal dialysis) or kidney transplant [10]. End-stage renal disease (ESRD) is a related administrative term based on the payment for health care by the Medicare ESRD Program . ESRD is used to identify those receiving RRT or who have received a kidney transplant, regardless of eGFR level [11]. In Sect. 25.7 below, we describe the treatment of advanced kidney disease in older populations including dialysis, kidney transplant, and conservative management.
In contrast to CKD and kidney failure, which are considered chronic conditions, AKI is a sudden worsening in kidney function. The term AKI has replaced the diagnosis of acute renal failure to reflect that even small changes in kidney function may impact long-term kidney function and to emphasize the broad spectrum of kidney injury [12]. Current classification of AKI includes three stages based on both serum creatinine and urine output (UOP) (Table 25.2) [13]. In Sect. 25.5 below, we describe risk factors that predispose older adults to AKI and the impact of AKI on CKD progression.
3.2 Burden of Kidney Disease Among Older Adults
The overall prevalence of CKD has been reported to be 13.1 % in the adult US population. However, the prevalence of kidney disease increases markedly with age [1]. Nearly half of those with CKD are 70 years of age or older, and there is a graded increase in the prevalence of CKD at older ages. Among US adults, the prevalence of CKD , defined as an eGFR <60 ml/min/1.73 m2 was reported to be 0.9, 7.5, 26.5, and 51.1 % among those aged <60, 60–69, 70–79, and ≥80 years old. A similar, but less dramatic, increase in the prevalence of albuminuria, defined as an ACR >30 mg/g, of 6.8, 14.2, 21.3, and 32.7 % at ages 60–69, 70–79 and ≥80 years, respectively, has been reported.
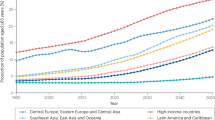
An increase in the prevalence of CKD over the past 2 decades has also been reported in the general US population, especially among older adults [14, 15]. For example, the prevalence of decreased eGFR (<60 ml/min/1.73 m2) in the US population ≥80 years was examined during three time periods: 1988–1994, 1999–2004, and 2005–2010. The prevalence of decreased eGFR was 40.5, 49.9, and 51.2 % during these time periods. A disproportionate increase in the prevalence of more severe CKD (eGFR <45 ml/min/1.73 m2) was found from 14.3 % to 18.6 % and 21.7 % in 1988–1994, 1999–2004, and 2005–2010, respectively. These findings were not completely explained by an increase in the prevalence of diabetes and hypertension in the older population during this time. Assuming that the prevalence of CKD remains stable in this age group, with the aging of the US population, the number of US adults ≥80 years old with eGFR <60 ml/min/1.73 m2 is estimated to increase from 4.6 million in 2005–2010 to 9.9 million and 15.8 million in 2030 and 2050, respectively (Fig. 25.1) [15].
The number of US adults ≥80 years old with CKD has doubled in the past 2 decades and will continue to increase with the aging of the populations . There has been a disproportionate increase in the prevalence of more severe CKD. eGFR estimated glomerular filtration rate, ACR albumin-to-creatinine ratio
While the prevalence of CKD defined as an eGFR <60 ml/min/1.73 m2 is highest at older age, older adults are much less likely to progress to kidney failure. The very old with CKD may be 10–20 times more likely to die before progressing to kidney failure. The competing risk of death has been examined by determining at what eGFR level is the risk of requiring RRT greater than the risk of death for different age groups. For example, among younger adults the risk of kidney failure requiring RRT is greater than the risk of death at an eGFR level of 45 ml/min/1.73 m2 and below [3]. For adults 65–84 years old, the risk of kidney failure requiring RRT is only greater than the risk of death at an eGFR of 15 ml/min/1.73 m2 and below. For those 85 years and older, the risk of death has been shown to exceeded the risk of kidney failure requiring RRT at any eGFR level.
In addition to the competing risk of death before reaching kidney failure, there are other possible explanations for the age difference in risk of kidney failure including a slower decline in kidney function among older adults. Additionally older adults may be less like to be offered or chose treatment with dialysis or transplantation in the face of kidney failure. For example, when kidney failure is categorized as treated (eGFR <15 ml/min/1.73 m2 and dialysis or kidney transplant) or untreated (eGFR <15 ml/min/1.73 m2, but no dialysis or kidney transplant), overall kidney failure is more common at older ages. However, at younger ages, treated kidney failure is more common than untreated kidney failure [16]. At older ages untreated kidney failure is much more common.
Although only a small proportion of older adults with CKD progress to kidney failure and receive RRT, the absolute number of older adults with ESRD (i.e., requiring RRT or kidney transplant regardless of eGFR) has increased over the past 20 years. Through 2010, the fastest growing group with ESRD was those 70 years and older [17]. Several factors may be contributing to the increased incidence of ESRD among older adults. This may be due in part to the increase in CKD prevalence among older adults, the aging US population, as well as an increase in the use of dialysis among older adults.
A similar pattern of graded increase in the incidence of AKI at older ages has been shown. Among hospitalized adults, the incidence of AKI among those 85 years and older is approximately 40 cases compared to 20 cases per 1000 discharges among those <65 years old [12]. The incidence of AKIs has been reported to have increased over the last 2 decades and has been explained by an increase in AKI risk factors, the aging population, as well as improvements in recognition of AKI.
4 Disease-Oriented Versus Patient-Centered Approach
4.1 Disease-Oriented Approach
The disease-oriented model of care is the prevailing clinical paradigm for the diagnosis and treatment of chronic conditions . This approach emphasizes the prevention, diagnosis, and treatment of individual disease processes [2, 18]. In the disease-oriented approach a direct causal relationship between clinical signs and symptoms and specific disease pathology is assumed. Treatments target the underlying pathophysiology and symptoms are thought to be best treated by interventions that impact the disease course, rather than as a target for intervention themselves. Treatment priorities are often determined by the availability of clinical trial evidence.
There are several strengths to this approach when applied to individual chronic conditions. The development and dissemination of CKD clinical practice guidelines have standardized CKD terminology and improved recognition and treatment of CKD. The disease-oriented approach provides a systemic framework for evidence-based management . Additionally, this approach is well suited for applying quality performance measurement and outcome tracking. Below, we describe the disease-oriented approach to CKD. Next, we describe limitations when applied specifically to older adults with CKD.
Existing CKD practice guidelines follow the disease-oriented model that assumes a direct and linear relationship between underlying kidney pathology with CKD progression, the development of concurrent CKD complications, kidney failure and ultimately death from CKD. Management strategies target the underlying risk factors for CKD and disease-specific biomarkers are used to track the progression of CKD. Clinical trials to prevent CKD progression are considered to provide the highest quality of evidence and are used to make recommendation for CKD treatment. Outcomes of interest are specific to CKD (e.g., kidney failure, mortality).
There are three main categories for CKD management : (1) slowing the progression of CKD to prevent kidney failure, (2) recognition and treatment of concurrent CKD complications, and (3) preparation for RRT [10]. Slowing the progression of CKD is considered a key goal. Approaches to slowing the progression include blood pressure (BP) control for all patients with CKD. For those with albuminuria, renin-angiotensin-aldosterone system (RAAS) interruption with angiotensin-converting enzyme inhibitors (ACE-Is ) or angiotensin receptor blockers (ARBs ) are recommended. Currently recommended BP goals for CKD patients are ≤140/90 for those with an ACR <30 mg/g and ≤130/80 for those with diabetes or ACR ≥30 mg/g. However, these recommendations are subject to change given findings from a recent clinical trial showing better outcomes among older adults who acheive lower BP targets. [19]. Guidelines also provide recommendations for protein intake, glycemic control, salt intake, and physical activity to prevent CKD progression.
The second category for CKD management is the recognition and treatment of concurrent CKD complications including anemia, metabolic bone disease, acidosis, and cardiovascular disease. Guidelines provide specific drug and lifestyle recommendations to manage these complications. In CKD, anemia is related to reduced erythropoietin and defined as <13.0 g/dL for men and <12.0 g/dL for women. Guidelines encourage evaluation for other causes of anemia and when erythropoietin stimulation agents are used, increasing hemoglobin concentrations to levels above 11.5 g/dL should be avoided. CKD metabolic bone disease includes abnormalities of calcium, phosphate, and parathyroid hormone (PTH) and is associated with increased risk of fractures. Current recommendations include dietary phosphate restriction or using oral binder to maintain serum phosphate within the normal range. Targets for treatment of hyperparathyroidism are more controversial. While clinical trials provide evidence that treatment to reduce PTH improves biomarkers of metabolic bone disease, the impact of these intermediate outcomes on clinically important outcomes such as fractures is limited. Guidelines also recommend treatment with oral bicarbonate supplementation for patients with serum bicarbonate levels <22 mmol/L with the goal to maintain bicarbonate within the normal range.
Lastly, guidelines provide recommendations for referral to nephrologists and preparation and time of RRT . Referral to nephrology is recommended, even if dialysis or transplantation is not a consideration in the presence of: AKI, eGFR <30 ml/min/1.73 m2, significant albuminuria (ACR >300 mg/g), progression of CKD, urinary red cell casts, hypertension refractory to treatment with four medications, persistent elevated serum potassium, recurrent nephrolithiasis, and hereditary kidney disease. Planning for RRT is based on the risk for progression to kidney failure. Recent studies have shown that the trajectory of CKD progression is often nonlinear and difficult to predict for older adults. Timing of RRT initiation is determined by the presence of kidney failure symptoms including serositis, acid–base or electrolyte abnormalities, pruritis, inability to control volume status or BP, progressive deterioration in nutritional status or cognitive impairment due to uremia. Recent studies have shown a trend towards initiation of RRT at higher levels of eGFR; however, evidence suggests no benefit or an increased risk for mortality among those with earlier initiation of dialysis in the course of CKD progression.
4.1.1 Limitations of the Disease-Oriented Approach
Despite the acceptance of the disease-oriented approach, there are several limitations of this approach when applied to older adults. Here, we describe four characteristics of older populations that may limit the relevance of the disease-oriented approach to CKD management [2]. These include (1) limited life expectancy, (2) a high burden of multimorbidity, and (3) heterogeneity in health goals and treatment preferences, and (4) exclusion from clinical trials.
Limited life expectancy is a key factor to consider for any disease-specific treatment plan for older adults. Both patients and providers recognize that there is a reduction in the years remaining in life expectancy at older ages and this has been shown in CKD. For example, a 70-year-old man with an eGFR 30–44 ml/min/1.73 m2 and ≥2+ dipstick proteinuria may expect on average to live 5 more years. In contrast, an 85-year-old with the same level of kidney function may live on average 2.6 additional years [20]. However, reports of average survival do not capture the remarkable heterogeneity in life expectancy and complexity estimating survival in older adults. One approach to determine the heterogeneity in life expectancy is to calculate not only the median survival, but also the interquartile range (IQR ) for survival defined as the 25th percentile to 75th percentile. The IQR for survival is 2.3–8.6 years for the 70-year-old man described above and 1.2–4.5 years for the 85 year old. This means that the highest 75th percentile of surviving 85 year olds may expect to live 4.5 year or longer. This suggests that many 85 year olds will live as long as or longer than the average 70 year old. Similar findings have been shown among older ESRD patients. The median survival for an 80-year-old incident ESRD patient is 1.3 years, however the interquartile range is 5 months to 3 years. Therefore, applying uniform recommendations to all older adults, some of whom may expect to live many more years and benefit from preventive treatments and others who are nearing end of life, is not appropriate.
Among older adults, CKD almost universally occurs in individuals with other chronic medical conditions. While multimorbidity , defined as the presence of two or more chronic conditions is common among older adults with CKD, existing clinical practice guidelines follow a “single disease” framework and do not account for the presence of other chronic conditions. As described above, the disease-oriented approach relies on CKD biomarkers (i.e., eGFR, ACR) to guide treatment decisions and focuses on preventing CKD-related outcomes. However, for older adults with multimorbidity, the application of multiple “single-disease” guidelines may lead to treatment recommendations that are complex and often contradictory or of limited benefit.
In addition to having multiple chronic conditions such as hypertension and diabetes, older adults with CKD have been shown to be at risk for co-occurring geriatric conditions. In the CKD population, the risk for mortality, hospitalizations, and emergency department (ED) visits increases at higher number of these problems. For example, among older adults with eGFR <60 more than two-thirds have 2 or more of 6 geriatric conditions (cognitive impairment, depressive symptoms, exhaustion, impaired mobility, falls, and polypharmacy) [21]. Compared to those with none of these problems, those with three or more experience twice the risk of dying, being hospitalized or requiring an ED visit. This “geriatric” multimorbidity is not considered in the disease-oriented clinical practice guidelines that only focus on CKD.
A third characteristic of older populations that may limit the relevance of the disease-oriented approach is heterogeneity in health goals and treatment preferences reported by older adults [2]. While CKD clinical practice guidelines prioritize the reduction of mortality and prevention of CKD related outcomes such as kidney failure, older adults often frame their health goals in terms of their overall health and maintaining functional independence. Universal health outcomes such as quality of life and functional independence may be viewed as more important than disease-specific outcomes. While a shift in health goals and preferences has been shown among older adults, it is important to recognize the variability in goals and preferences between older adults. The narrow focus on outcomes that are defined by the underlying disease pathology in the disease-oriented model often fails to address what is most important to an individual patient. Disease-oriented clinical practice guidelines lack the flexibility to allow providers to adapt the goals and treatment plans to the individual patient’s needs.
Lastly, older adults with complex multimorbidity or limited life expectancy are often excluded from clinical trials . This is often done because the magnitude of treatment effects for a given intervention is often larger in homogenous populations (i.e., smaller variability results in larger treatment effect) [18]. Exclusion of older adults limits the generalizability of individual studies to older adults and the clinical practice guidelines that generate recommendations based on these studies. For example, most of the trials underpinning the guideline recommendations for the use of ACE-Is and ARBs have been conducted in high risk populations and did not enroll participants older than 70. Because ACE-Is and ARBs may be most effective in those at highest risk for progression (e.g., among those with albuminuria), findings from these studies of a number needed to treat (NNT ) to prevent one case of ESRD ranging from 9 to 25 may not be generalizable to older adults. In fact, one recent simulation study using a real-world cohort of older adults with CKD showed large differences in the NNT based on the estimated baseline risk for ESRD. For older adults with the lowest risk of ESRD, they reported an NNT to prevent one case of ESRD to be 2500 [22].
4.2 Individualized, Patient-Centered Approach
There is an increasing awareness that a “one size fits all” approach to CKD management may not be appropriate. For example, the most recent CKD guidelines have added suggestions to tailor BP targets. However, approaches for how to individualize goals are not provided. Given the limitations of disease-oriented models of care in older populations, geriatricians often favor a more individualized patient-centered approach. The patient-centered approach embraces the complexity and acknowledges the importance of patient health goals and preferences for developing treatment plans. The patient-centered approach recognizes that existing evidence may not be relevant for individual patients. Symptoms are considered important targets for intervention, regardless of the underlying cause.
One approach to implementing a patient-centered approach to CKD is to include geriatric assessment as part of the clinical evaluation of CKD patients. Routine geriatric assessment could be used to identify contextual information (e.g., cognitive impairment, poor social support, markers of frailty, and limited life expectancy) to guide clinical care. It has been suggested that the recognition of geriatric conditions including functional impairment, frailty, mobility impairment, cognitive impairment, and depressive symptoms could be used to signal for the provider to consider a transition from the traditional disease-oriented approach to CKD care to a more individualized, patient-centered approach. For example, recognition of mild cognitive impairment and low social support may be used to tailor management goals such as glucose control in a patient with CKD and diabetes to reduce the risk for hypoglycemia. Recognition of these problems may also facilitate a shared decision-making approach to discussions about RRT. In these discussions, providers can address prognostic markers associated with poor survival on dialysis (e.g., non-ambulatory status, frailty) to help patients make an informed decision regarding dialysis versus conservative management. Eliciting goals of both the individual patient and family and caregivers can be used to prioritize outcomes beyond those reported in the CKD guidelines. In this approach, the CKD-specific diagnosis and management is not abandoned completely and may be incorporated into individualized treatment plans, depending on the extent to which disease-based recommendations are aligned with the preferences and goals of the patient. In Table 25.3, we highlight several components of geriatric assessment, their implications for CKD, and how these might be used to facilitate a patient-centered approach to CKD management.
5 Acute Kidney Injury
Older adults are vulnerable to AKI due to factors that are both intrinsic and extrinsic to the kidney. While several intrinsic factors underlying this increased risk have been proposed including age-related stress-induced cellular senescence, a key component of AKI risk in older adults is susceptibility to kidney injury from extrinsic factors. Older adults may have decreased physiologic reserve in the face of physiologic stressors. AKI in the older population may be thought of as multifactorial and explained by the presence of chronic predisposing factors and acute precipitating factors, analogous to the current conceptualization of geriatric syndromes such as delirium and falls [12]. Predisposing factors include age-related structural changes including vascular sclerosis, age-related kidney function decline, chronic inflammation, and the presence of underlying CKD. Furthermore, the prevalence of multimorbidity increases at older ages and older patients often need multiple medications or diagnostic tests and procedures. For example, in an older patient with both CKD and arthritis, the addition of NSAIDs to a medication regimen that includes an ACE-I can precipitate AKI. Other medications that have been linked to AKI include diuretics, ARBs , and antibiotics. The co-occurrence of CKD and cardiovascular disease is also common and these patients may be at increased risk for contrast induced nephropathy. Therefore, benefits of cardiac catheterization for diagnosing coronary artery disease must be balanced with the risk for AKI. Older adults may also be at risk for volume depletion due to renal sodium wasting, reduced renal response to antidiuretic hormone and diminished thirst, putting those with vascular kidney disease at higher risk for AKI [23]. Older adults may also be at increased risk for infection and sepsis is a leading cause of AKI. In the older population, prevention of AKI may require improved recognition of both predisposing and precipitating factors, rather than addressing only factors intrinsic to kidneys.
As described above, a disease-oriented approach that focuses only on preventing kidney outcomes may not always be appropriate. Considering a patient’s health goals and preferences may be necessary, especially when discordant recommendations arise in the setting of multimorbidity. For example, some older adults with arthritis pain may accept a small increase risk in AKI when taking NSAIDs in order to improve pain control and maintain functional independence.
When older adults have AKI they may be less likely to recover kidney function compared to younger adults. There is also growing recognition that the course of kidney disease progression is often not a predictable, linear decline towards kidney failure. For many older adults, kidney disease progression may result from repeated episodes of AKI. In these cases, it may be more effective to recognize AKI risk factors and prevent or lessen the impact of AKI to prevent progression to kidney failure, rather than management strategies such as BP and glucose control.
6 Chronic Kidney Disease
6.1 Disease Versus Normal Aging
Although the presence of CKD defined as an eGFR <60 ml/min/1.73 m2 has been shown to be associated with mortality, CVD, concurrent CKD complications and functional decline, even in older populations, the current CKD definitions remain controversial. Current guidelines define CKD based on eGFR or ACR cut-points regardless of age and disagreement remains regarding CKD definition in older populations. Those in favor of changing the CKD definition to require age calibration for the diagnosis of CKD argue that the current approach labels many millions of older adults with a disease which may actually be age-related decline in kidney function due to organ senescence. Those against changing the guidelines argue for the need of clear and simple definitions regardless of age [1].
6.2 Challenges Estimating GFR
A related controversy exists over the estimation of GFR in older adults. Measuring GFR in the clinical setting is not practically possible [1]. Estimation of GFR relies on formulas that use age, race, and sex along with serum creatinine. Because creatinine comes from the breakdown of muscle, it has been argued that these equations may not accurately account for age-related changes in muscle mass that result in lower serum creatinine. Very few research studies have a large number of very old participants and available data on measured GFR; therefore existing estimation equations were developed and validated in studies conducted primarily in the middle-aged and young-old. More recent studies have attempted to develop and validate estimating equations in the very old. However, these studies have been limited to white, European populations and questions remain about the equations’ validity in African American older adults [24]. Novel biomarkers such as cystatin-C can be used to estimate GFR and have been shown to be strong predictors of mortality [25]. However, GFR estimating equations that use cystatin-C identify CKD in an even large proportion of older than creatinine based equations [24]. For these reasons, an approach to diagnosis of CKD in older patients that takes into consideration the trajectory of renal function over time (e.g., stable versus declining), the presence of albuminuria, and the co-occurrence of conditions that worsen kidney function such as hypertension and diabetes may be more appropriate than relying on a single estimation of GFR to identify CKD.
7 Kidney Failure
7.1 Life Expectancy
Progression to kidney failure marks a significant decline in remaining life for older adults. Life expectancy for older adults who require RRT for kidney failure is approximately 25 % less than the life expectancy of older adults without kidney failure [26]. Survival after kidney failure is typically better for older adults who initiate RRT compared to those who decline RRT (2-year survival rate 76 % vs. 47 %) [26]. This survival benefit is not only due to RRT itself. Older adults who initiate RRT tend to have fewer comorbid conditions and less functional impairment than those who decline RRT, confounding the association between treatment option and survival.
Among older adults who initiate RRT, life expectancy ranges from less than 3 months to 4.5 years [27]. Prognosis is worse as comorbidity burden, functional limitations, and age increases. Other factors that contribute to prognosis after dialysis initiation are shown in Table 25.4. These factors can be used to calculate risk scores to estimate the probability of death after initiating dialysis [26]. Although evaluated in a cohort of prevalent dialysis patients, the “surprise” question is an additional tool for prognostication. By answering the following question yourself: “Would I be surprised if this patient died in the next 12 months?”, clinicians directly use their clinical judgment for prognostication. This clinical judgment is important for informing decisions for both initiation and withdrawal of RRT.
7.2 Shared Decision-Making
Because life expectancy is limited in older adults with kidney failure, it is essential to use shared decision-making for clinical decision-making for all medical procedures and intensive therapies (e.g., major surgery, chemotherapy). Most older adults make RRT decisions based on their personal preferences and consideration of the challenges of adjusting to life with RRT. Therefore, shared decision-making allows patients and their caregivers to communicate their preferences to the clinician. In turn, the clinician using a risk benefit analysis is able to guide the patient towards a decision that addresses the patient’s health goals.
For frail older adults, the SPIRES communication framework is an ideal approach to the shared decision-making process [28]. SPIRES involves the following six steps: Setup, Perceptions and Perspectives, Invitation, Recommendation, Empathize, and Summarize and Strategize (Table 25.5). Through this process, the clinician combines prognostic information from the patient’s medical records with patient perspectives to develop a recommendation in favor of or against RRT initiation. The clinician develops an individualized treatment plan that involves monitoring for signs or symptoms that RRT is meeting the patient’s expectations. This monitoring allows the SPIRES shared decision-making framework to be cyclical. If the patient experiences worsening health status, the clinician can use this new prognostic information (and potentially new patient preferences) to develop a new recommendation regarding continuation of RRT. Thus, SPIRES would facilitate discussions about dialysis withdrawal and end-of-life care.
7.3 Treatment Options
Central to dialysis decision-making is consideration of treatment options [e.g., RRT (hemodialysis and peritoneal dialysis), transplantation, and conservative management] for managing ESRD. To provide a recommendation, the clinician should first determine if the patient has any contraindications to specific treatment options. Then, the clinician should determine the patient’s preferences and psychosocial status to determine the potential challenges of each treatment option to the individual patient (Table 25.6).
7.4 Renal Replacement Therapy
Although RRT is the most common treatment option for older adults approaching kidney failure, it is not the most appropriate treatment option for all older adults. Age is not a contraindication to RRT. However, nephrologists may choose not to initiate RRT in older adults if the risks outweigh the benefits. The benefit of RRT is lower in older adults who have severe cognitive impairment lacking ability to follow commands or respond to their environment. Also, older adults with a terminal illness, aside from kidney failure, would also have low benefit from RRT (unless it is palliative) and are likely be advised to forgo RRT [29].
Timing of preparation for RRT can be challenging for older adults. Early preparation for RRT involves dialysis access placement for hemodialysis or peritoneal dialysis (e.g., arteriovenous access, central venous catheter (CVC) , Tenckhoff catheter). However, it is not clear if an individual patient will progress to kidney failure or die before there is a need for RRT. This uncertainty is challenging for both patients and clinicians when deciding the appropriate timing for dialysis access placement. Early access placement, although recommended, can create physical and emotional burdens on a patient who may not ever initiate RRT.
Hemodialysis access placement is an additional potential challenge for older adults. Clinical guidelines recommend arteriovenous fistula (AVF ) as hemodialysis access for all dialysis patients. However, AVF maturation time is approximately 6 months, and less than 50 % of older adults have mature AVFs because of vascular calcifications and reduced vascular elasticity [26]. Compared to younger patients, older adults tend to undergo more procedures to create and maintain patency of AVF . Because of the maturation time and recurrent procedures, AVFs may be less ideal for older adults who have limited life expectancy (i.e., less than 2 years) [27]. Arteriovenous grafts (AVG ) and CVCs are more likely to be successfully placed after a single procedure; however, these alternative accesses are associated with greater risks of infection and long-term patency issues. Thus, AVGs and CVCs are more appropriate for older adults with limited life expectancy and/or unsuccessful AVF maturation. Importantly, AVG should be attempted prior to CVC placement because of higher risk of mortality associated with CVC use. Still, some older adults prefer CVC because it allows avoidance of needles and recurrent procedures.
The benefits of RRT are similar with peritoneal dialysis and hemodialysis; however, some older adults may not be able to receive peritoneal dialysis. Peritoneal dialysis is typically conducted in the home by the patient and/or caregiver after intensive training in sterile technique and equipment use. Therefore, older adults who would have difficulty with peritoneal dialysis include those who do not live in a home with dedicated space for equipment and those with functional limitations (e.g., visual impairment, cognitive impairment, ADL dependence, or mobility disability) and no caregivers available to conduct their treatments. Some older adults who receive peritoneal dialysis can encounter new challenges that require transition from peritoneal dialysis to hemodialysis. Such challenges can be recognized by recurrent peritonitis, inadequate ultrafiltration, or waste removal despite adjustments to the treatment regimen. Also, some older adults may develop functional limitations or experience loss of their social support that makes it difficult to continue peritoneal dialysis.
7.5 Transplantation
Renal transplantation provides better survival benefit and quality of life than RRT and is not contraindicated in older adults [26]. However, individual transplant centers have age limits for transplant listing. For transplant listing, older adults may find it burdensome to undergo multiple diagnostic tests (e.g., cardiac stress test, CT scans). These tests may identify abnormalities or yield false positive results that can lead to emotional distress [27]. Still, transplantation can be an ideal option for ESRD for older adults who are not frail and have minimal comorbidities and functional limitations. These patients are more likely to be able to survive their wait-list interval, withstand the physical stress of the surgery, and be adherent to the extensive immunosuppression medication regimen. Clinical trajectories can change over time; therefore, reassessment of comorbidity burden and functional status during the wait-list interval is important to ensure the patient remains to be an eligible transplant candidate. After transplantation, older adults may develop problems with drug interactions between chronic medications and immunosuppression medications, as well as an increased risk of infections and malignancies.
7.6 Conservative Management
For many older adults with kidney failure , RRT or transplantation may not be appropriate. Aside from apparent contraindications to RRT described above, some older adults decline RRT because they value quality over quantity of life and prefer to not spend significant time in dialysis sessions during their remaining lifetime [28]. Traditionally, it was thought that there was little to offer these patients. However, there is growing appreciation that older adults who decline RRT benefit from active treatment. This “conservative management” involves routine outpatient visits that focus on CKD management and symptom management as kidney failure progresses. These patients may also receive hospice care. Existing observational studies also suggest that patients who receive conservative management experience fewer hospitalizations and more palliative care services than those who receive RRT [26]. Increasing use of shared decision-making and prognostication of patient’s life expectancy may yield an increase in the proportion of older adults receiving conservative management.
8 Kidney Failure in Special Patient Populations
8.1 Hospital Patients
Older adults receiving dialysis often require hospitalizations and are admitted on average twice per year. Additionally, the majority of older adults who start dialysis do so during an inpatient hospitalization. These patients often require prolonged hospitalization and receive high intensity health care during this time despite an overall poor prognosis. For example, among older Medicare beneficiaries more than 20 % require hospitalization for ≥2 weeks at dialysis initiation and over 15 % of those require one or more intensive procedures including mechanical ventilation, feeding tube placement or cardiopulmonary resuscitation [30]. Higher intensity care during the hospitalization is associated with an increased risk for death. Among those 80 years and older who require ≥2 weeks in the hospital at dialysis initiation, median survival is only 1 year or less and 10–20 % of their remaining days of life are spent hospitalized. These reports may suggest the need for earlier involvement of palliative care in the treatment of hospitalized ESRD patients .
Rehospitalizations are also common among older adults with ESRD. More than one in three older dialysis patients who are discharged from the hospital return within 30 days [31]. The high rates of rehospitalization have been reported to contribute to or parallel the high mortality, low quality of life and increasing health care costs in this population. Data are limited on interventions to reduce rehospitalizations specifically for older adults with kidney failure. However, one analysis that used a quasi-experimental approach showed that more frequent provider visits in the month following hospitalization was associated with a decreased risk for readmission. Whether or not inpatient models of care that focus on improving outcomes for hospitalized older adults such as Acute Care of the Elderly (ACE) units in combination with care transition support and more frequent disease-specific follow-up with nephrology providers would reduce readmissions in this high risk population needs to be determined. Chapter 7 provides detailed suggestions in caring for hospitalized seniors.
8.2 Post-Acute and Long-Term Care Patients
Because the majority of older adults initiating dialysis do so during a hospitalization these patients are often eligible for post-acute care services in a skilled nursing facility (SNF) . These patients may also be eligible for post-acute care services following hospitalizations not related to the initiation of dialysis. The Medicare SNF benefit is provided on a short-term basis after a hospitalization for patients who have skilled nursing or rehabilitation needs. The goal of this program is to improve the patient’s condition within pre-determined time period or to prevent the condition from worsening. However, because older ESRD patients are medically complex and three times a week dialysis may interfere with daily physical therapy treatments, they may experience worsening health and be less likely to return home or achieve functional independence. For patients who are discharged from an SNF , there are high rates of hospitalization or ED visits within 30 days of returning home [32].
Those requiring long-term nursing home care are a particularly high risk group, however this population has not been well studied. While utilization of nursing home care is common among older adults initiating dialysis, it is poorly recognized by nephrologists. For example, 28 % of the 27,913 U.S. older adults who started dialysis in 2006 required nursing home care at the time of initiation. However, only 33 % of these patients were accurately identified by their dialysis providers as receiving nursing home care [33]. Older nursing home residents initiating dialysis also face a high burden of functional decline. One analysis of long-term nursing home residents found that initiation of dialysis was associated with a significant and sustained functional decline. In this patient group, mortality rates were 24, 41, 51, and 58 %, at 3, 6, 9, and 12 months, respectively [4].
9 End-of-Life Considerations
9.1 Symptom Burden
Older adults with kidney failure may experience a high burden of symptoms, especially at the end-of-life. For example, in the last month of life older adults with kidney failure treated with conservative management more than half of all patients reported: lack of energy, drowsiness, dyspnea, poor concentration, poor appetite, swelling of the arms or legs, dry mouth, constipation, and nausea [34]. A similar burden of symptoms has been reported among those who receive dialysis as well, suggesting that dialysis alone may not mitigate these symptoms.
9.2 Role of Palliative and Supportive Care
Palliative and supportive care is an important resource for older adults with kidney failure. While traditionally palliative care has been reserved for end-of-life or those who decline dialysis, the role of palliative care across the spectrum of kidney disease is increasing. Evaluation by palliative care specialist can provide prognostic information, help elicit patient and family health goals, and support advanced care planning and shared decision-making about dialysis. Palliative care support can also improve the recognition and treatment of complex symptoms. See Chap. 6. Palliative Care and End of Life Issues.
10 Summary
Clinical specialists caring for older patients will increasingly encounter those with CKD and/or AKI. While clinical practice guidelines exist for the diagnosis and management of CKD, providers should be prepared to recognize the limitations of these disease-oriented recommendations and the unique aspects of caring for older adults with CKD. We recommend an approach that considers a patient’s health goals, life expectancy, and presence of multimorbidity and geriatric conditions, to help tailor treatment plans. Furthermore, clinicians should understand the challenges and controversies for using eGFR to define CKD in this population. For older adults, kidney failure carries a poor prognosis and a shared decision-making approach to RRT is necessary.
References
Bowling CB, Muntner P. Epidemiology of chronic kidney disease among older adults: a focus on the oldest old. J Gerontol Ser A Biol Med Sci. 2012;67(12):1379–86.
Bowling CB, O’Hare AM. Managing older adults with CKD: individualized versus disease-based approaches. Am J Kidney Dis. 2012;59(2):293–302. Pubmed Central PMCID: 3261354.
O’Hare AM, Choi AI, Bertenthal D, Bacchetti P, Garg AX, Kaufman JS, et al. Age Affects outcomes in chronic kidney disease. J Am Soc Nephrol. 2007;18(10):2758–65.
Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med. 2009;361(16):1539–47. Pubmed Central PMCID: 2789552.
Kutner NG, Zhang R, Allman RM, Bowling CB. Correlates of ADL difficulty in a large hemodialysis cohort. Hemodial Int. 2014;18(1):70–7. Pubmed Central PMCID: 3887518.
Weinstein JR, Anderson S. The aging kidney: physiological changes. Adv Chronic Kidney Dis. 2010;17(4):302–7. Pubmed Central PMCID: 2901622.
Anderson S, Halter JB, Hazzard WR, Himmelfarb J, Horne FM, Kaysen GA, et al. Prediction, progression, and outcomes of chronic kidney disease in older adults. J Am Soc Nephrol. 2009;20(6):1199–209.
Lindeman RD, Tobin J, Shock NW. Longitudinal studies on the rate of decline in renal function with age. J Am Geriatr Soc. 1985;33(4):278–85.
Rule AD, Amer H, Cornell LD, Taler SJ, Cosio FG, Kremers WK, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med. 2010;152(9):561–7. Pubmed Central PMCID: 2864956.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2013;3:1–150
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. American J Kidney Dis. 2002;39(2 Suppl 1):S1–266. Epub 2002/03/21. eng.
Anderson S, Eldadah B, Halter JB, Hazzard WR, Himmelfarb J, Horne FM, et al. Acute kidney injury in older adults. J Am Soc Nephrol. 2011;22(1):28–38.
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. 2012;2:1–138.
Bowling CB, Sharma P, Fox CS, O’Hare AM, Muntner P. Prevalence of reduced estimated glomerular filtration rate among the oldest old from 1988-1994 through 2005-2010. JAMA. 2013;310(12):1284–6. Pubmed Central PMCID: 4406347.
Bowling CB, Sharma P, Muntner P. Prevalence, trends and functional impairment associated with reduced estimated glomerular filtration rate and albuminuria among the oldest-old U.S. adults. Am J Med Sci. 2014;348(2):115–20. Pubmed Central PMCID: 4406350.
Hemmelgarn BR, James MT, Manns BJ, O’Hare AM, Muntner P, Ravani P, et al. Rates of treated and untreated kidney failure in older vs younger adults. JAMA. 2012;307(23):2507–15.
United Stages Renal Data System. USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States Bethesda, MD: National Institution of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2013.
O'Hare AM, Rodriguez RA, Bowling CB. Caring for patients with kidney disease: shifting the paradigm from evidence-based medicine to patient-centered care. Nephrol Dial Transplant. 2015;31:368–75.
Group SR, Wright Jr JT, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
Bowling CB, Batten A, O’Hare AM. Distribution of survival times in a real-world cohort of older adults with chronic kidney disease: the median may not be the message. J Am Geriatr Soc. 2015;63(5):1033–5. Pubmed Central PMCID: 4591036.
Bowling CB, Booth 3rd JN, Gutierrez OM, Kurella Tamura M, Huang L, Kilgore M, et al. Nondisease-specific problems and all-cause mortality among older adults with CKD: the REGARDS Study. Clin J Am Soc Nephrol. 2014;9(10):1737–45. Pubmed Central PMCID: 4186504.
O’Hare AM, Hotchkiss JR, Kurella Tamura M, Larson EB, Hemmelgarn BR, Batten A, et al. Interpreting treatment effects from clinical trials in the context of real-world risk information: end-stage renal disease prevention in older adults. JAMA Intern Med. 2014;174(3):391–7.
Phillips PA, Rolls BJ, Ledingham JG, Forsling ML, Morton JJ, Crowe MJ, et al. Reduced thirst after water deprivation in healthy elderly men. N Engl J Med. 1984;311(12):753–9.
Schaeffner ES, Ebert N, Delanaye P, Frei U, Gaedeke J, Jakob O, et al. Two novel equations to estimate kidney function in persons aged 70 years or older. Ann Intern Med. 2012;157(7):471–81.
Shlipak MG, Matsushita K, Arnlov J, Inker LA, Katz R, Polkinghorne KR, et al. Cystatin C versus creatinine in determining risk based on kidney function. N Engl J Med. 2013;369(10):932–43. Pubmed Central PMCID: 3993094.
Berger JR, Hedayati SS. Renal replacement therapy in the elderly population. Clin J Am Soc Nephrol. 2012;7(6):1039–46. Pubmed Central PMCID: 3362311, Epub 2012/04/21. eng.
Tamura MK, Tan JC, O’Hare AM. Optimizing renal replacement therapy in older adults: a framework for making individualized decisions. Kidney Int. 2012;82(3):261–9. Pubmed Central PMCID: 3396777, Epub 2011/11/18. eng.
Schell JO, Cohen RA. A communication framework for dialysis decision-making for frail elderly patients. Clin J Am Soc Nephrol. 2014;9(11):2014–21. Pubmed Central PMCID: Pmc4220751, Epub 2014/06/28. eng.
Moss AH. Shared decision-making in dialysis: the new RPA/ASN guideline on appropriate initiation and withdrawal of treatment. Am J Kidney Dis. 2001;37(5):1081–91. Epub 2001/04/28. eng.
Wong SP, Kreuter W, O’Hare AM. Healthcare intensity at initiation of chronic dialysis among older adults. J Am Soc Nephrol. 2014;25(1):143–9. Pubmed Central PMCID: 3871783.
Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J. Physician visits and 30-day hospital readmissions in patients receiving hemodialysis. J Am Soc Nephrol. 2014;25(9):2079–87. Pubmed Central PMCID: 4147977.
Hall RK, Toles M, Massing M, Jackson E, Peacock-Hinton S, O’Hare AM, et al. Utilization of acute care among patients with ESRD discharged home from skilled nursing facilities. Clin J Am Soc Nephrol. 2015;10(3):428–34. Pubmed Central PMCID: 4348677.
Bowling CB, Zhang R, Franch H, Huang Y, Mirk A, McClellan WM, et al. Underreporting of nursing home utilization on the CMS-2728 in older incident dialysis patients and implications for assessing mortality risk. BMC Nephrol. 2015;16:32. Pubmed Central PMCID: 4408561.
Murtagh FE, Addington-Hall J, Edmonds P, Donohoe P, Carey I, Jenkins K, et al. Symptoms in the month before death for stage 5 chronic kidney disease patients managed without dialysis. J Pain Symptom Manag. 2010;40(3):342–52.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bowling, C.B., Hall, R.K. (2017). Kidney Disease. In: Burton, J., Lee, A., Potter, J. (eds) Geriatrics for Specialists. Springer, Cham. https://doi.org/10.1007/978-3-319-31831-8_25
Download citation
DOI: https://doi.org/10.1007/978-3-319-31831-8_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-31829-5
Online ISBN: 978-3-319-31831-8
eBook Packages: MedicineMedicine (R0)