Abstract
The first metal-based drugs to show therapeutic efficacy against parasitic diseases, more specifically diseases caused by trypanosomatids, were arsenic and antimony complexes. Among these, pentavalent antimonials are still extensively used in the treatment of cutaneous and visceral leishmaniasis. This chapter will describe in details the current knowledge on the mechanism of action of antimonial drugs for leishmaniasis. Interestingly, pentavalent antimonials affect the parasite viability through both Sb(III)-induced imbalance of thiol metabolism in parasite and Sb(V)-induced stimulation of macrophage microbicidal activity, causing parasite death by oxidative stress. We will also discuss the mechanism of action of gold complexes under study as drug candidates for leishmaniasis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Antimony
- Gold
- Auranofin
- Antimonials
- Thiol
- Trypanothione
- Leishmaniasis
- Trypanosomiasis
- Resistance
- Oxidative stress
30.1 Historical Use of Metal Complexes Against Trypanosomatids
Trypanosomatids are protozoan parasites that cause various diseases in human, such as leishmaniasis, Chagas disease, and sleeping sickness. According to World Health Organization (WHO), trypanosomiasis and leishmaniasis are the most challenging among the neglected tropical diseases [1, 2].
At the beginning of the last century, Paul Ehrlich, considered the father of modern chemotherapy, discovered the anti-trypanosomal arsenic-based drug, atoxyl, for treatment of sleeping sickness [3]. However, atoxyl caused side effects, mainly blindness. In 1934, Ernst Friedheim, in the search for a safer drug, designed and developed melarsoprol which saved three millions of lives in the 1940s [4]. This arsenical drug is still in use for sleeping sickness, but is limited to cases of advanced infections with Trypanosoma brucei gambiense and rhodesiense. More recently, trivalent arsenicals in the form of As2O3 started to be used clinically in the treatment of acute promyelocytic leukemia [5].
Antimony-based drugs have also a long history of use in the treatment of infectious diseases. The importance of antimony in the early medicine is well-documented due to the debate created around their utilization in this period [6]. The first antimony compounds prepared for medicinal applications were introduced in the sixteenth and seventeenth centuries, with emphasis on antimony(III) potassium tartrate (tartar emetic). Tartar emetic was first obtained placing sour wine in glasses of antimony metal and its use was prescribed for many diseases, especially the lung diseases. During the late nineteenth century, tartar emetic was used for fever and pneumonia and its use declined slowly until the beginning of twentieth century.
At the beginning of the last century, the Brazilian physician Gaspar Vianna, pioneer researcher in the treatment of leishmaniasis, reported the efficacy of tartar emetic for clinical treatment of muco-cutaneous leishmaniasis [7]. In India, Brahmachari discovered in 1912 the organoantimonial compound urea stibamine, the first effective drug against visceral leishmaniasis, and was a nominee for the Nobel Prize in 1929 for this finding [8].
From the 1940s, these antimonials were substituted by the less toxic pentavalent antimony (Sb(V)) complexes, meglumine antimoniate and sodium stibogluconate (Fig. 30.1), in the therapeutics of leishmaniases. Typically, these Sb(V) drugs are given at 20 mg of Sb/kg per day intramuscularly or intravenously for 20–30 days [9]. Even though pentavalent antimonials are still the first-line drugs against all forms of leishmaniasis in most developing countries, their mechanism of action is still not fully understood and their use in the clinical setting is limited by their side effects and the emergence of resistance to antimony [9].
Structural formula proposed for meglumine antimoniate (a) and stibogluconate (b). Adapted from Frézard et al. [9]
Recent advances in understanding the molecular and cellular biology of leishmaniasis as well as the cellular accumulation pathways, mechanisms of resistance, and target identification allow a more systematic rationale-based approach for development of new anti-parasitic drugs [10–12]. In this context, complexes with other metals including gold showed promising pharmacological activities.
Most of the progress regarding drug development and mechanism of action was achieved using cell and animal models of leishmaniasis [13]. The in vitro models include extracellular log-phase leishmania promastigotes and established axenic leishmania amastigotes and the intracellular amastigotes in primary mouse peritoneal macrophages or monocyte transformed macrophages as host cells. The in vivo models use mostly inbred strains of mice infected with leishmania species causing either cutaneous or visceral leishmaniasis.
Interestingly, in the case of these metal-based compounds, evidence was obtained that those exert their antiparasitic action by causing oxidative stress. This chapter will describe in details the current knowledge on their mechanism of action, with emphasis on antimonial drugs and gold complexes for leishmaniasis.
30.2 Importance of Redox Systems in the Host–Leishmania Parasite Relationship
The protozoan leishmania parasite has a relatively simple life cycle with two principal stages: the flagellated mobile promastigote living in the gut of the sandfly vector and the intracellular amastigote within phagolysosomal vesicles of the vertebrate host macrophage. After recognition of Leishmania spp., macrophages are activated, triggering phagocytosis and various cellular processes to destroy the parasite. These cellular processes include production of phagolysosomal degradation enzymes, oxidative burst generation, and nitric oxide (NO) production. The oxidative burst provoked by the enzyme NADPH oxidase is a result of the increase in oxygen consumption as a consequence of the phagocytosis process. After macrophage activation, increased concentrations of various cytokines such as IFN-γ and TNF-α enhance NADPH oxidase activity and subsequently production of reactive oxygen species (ROS), such as superoxide radical. The production of superoxide radical leads to the spontaneous or enzymatic formation of hydrogen peroxide, hydroxyl radical, hypochlorite, and peroxynitrite. The increased NO and NO-metabolite levels in activated macrophages are the result of inducible nitric oxide synthase (iNOS) activation. Parasite persistence within the macrophages is determined by a balance between the ability of the immune response to sufficiently activate Leishmania-infected macrophages and the ability of the parasite to resist cytotoxic mechanisms of macrophage activation [14].
Although Leishmania species are susceptible in vitro to exogenous superoxide radical, hydrogen peroxide, nitric oxide, and peroxynitrite, they manage to survive the endogenous oxidative burst during phagocytosis and the subsequent elevated nitric oxide production in the macrophage. The parasite adopts various defense mechanisms against oxidative stress: the lipophosphoglycan membrane decreases superoxide radical production by inhibiting NADPH oxidase assembly and the parasite also protects itself through antioxidant enzymes [15]. Among the various parasite defense mechanisms against host attack, thiol metabolism appears as a first-line defense. One major system involved in the redox homeostasis in trypanosomatids is the trypanothione (T(SH)2)/trypanothione reductase (TR)system. The (T(SH)2)/TR system, which keeps T(SH)2 under the reduced state, replaces the nearly ubiquitous glutathione/GR system, protects trypanosomatids from oxidative damage, and delivers the reducing equivalents for DNA synthesis [16].
It has been reported that T(SH)2 is capable of reducing NO (generated by the host cell) and iron into harmless stable dinitrosyl iron complex with 600 time greater affinity than mammalian glutathione (GSH) reductase system [17]. This is the mechanism by which the parasite protects itself from such lethal environment.
30.3 Pentavalent Antimonial Drugs Against Leishmaniasis
The metabolism and mechanism of action of pentavalent antimonials against leishmania parasites are not fully understood [9]. However, the data available so far converge towards the central role of redox processes.
30.3.1 Drug Activation Though Metal Reduction
It is generally assumed that Sb(V) behaves as a prodrug, undergoing reduction within the organism into the more toxic and active trivalent form. This model is supported by several reports that Sb(V) is reduced into Sb(III) in the vertebrate host and that reduction could also happen in the parasite [18–22]. However, the exact microenvironment where the reduction occurs is still unclear.
Leishmania promastigote forms are insensitive to Sb(V). On the other hand, amastigote-like cultured parasites are sensitive to pentavalent antimonials, suggesting the occurrence of intracellular Sb(V) reduction in this life-cycle stage [23]. However, in the latter case, thiol availability from the culture medium and low pH as well as high temperature may also be determinant factors in Sb(V) to Sb(III) reduction and consequently high sensitivity to Sb(V) [24, 25].
The higher sensitivity of intramacrophagic amastigotes to Sb(V) compared to axenic amastigote-like favors the hypothesis of host-associated Sb(V) to Sb(III) reduction [23].
Thiols have been reported as potential reducing agents in this conversion [24, 26]. Reduction of Sb(V) to Sb(III) was found to occur spontaneously in the presence of the following thiols: (1) GSH, which is the main thiol in the cytosol of mammalian cells; (2) cysteine (Cys) and cysteinyl-glycine (Cys-Gly) found predominantly within lysosomes; and (3) the bis(glutathione)-spermidine conjugate T(SH)2, which is the main thiol within the parasite [27].
The observations that Cys, Cys-Gly, and T(SH)2 are more effective reducing agents than GSH and that this reaction is favored in acidic pH [18] led to the hypothesis that Sb(V) may be reduced in vivo by T(SH)2 within leishmania parasites and by Cys or Cys-Gly within the acidic compartments of mammalian cells. Both promastigotes and intracellular amastigotes maintain intracellular pH values close to neutral (~7) even in the presence of extracellular acidic pH (~4–5). This observation reinforces the hypothesis that thiol-mediated Sb(V) to Sb(III) reduction takes place preferentially in the host cell.
Other studies have suggested the participation of a parasite-specific enzymes in the process of reduction of Sb(V) to Sb(III) [28, 29]. However, these parasite-specific enzymes are expressed in both life-cycle stages and therefore it is difficult to accommodate the different toxicity of pentavalent antimony toward promastigotes and amastigotes.
Recently, the pentavalent antimonial drug meglumine antimoniate was found to contain up to 30 % of Sb(III), indicating that the mode of action of this drug could be mediated by this residual amount of Sb(III) [30]. Additionally, the availability of Sb(III) increased at low pH values, suggesting that this drug may act as molecular carrier releasing the active Sb(OH)3 form specifically in the acidic intracellular compartment where leishmania parasite resides.
30.3.2 Antimony-Induced Redox Imbalance
Sb(III) is classified as a borderline metal ion within Pearson’s hard-soft acid-base theory and has a high affinity towards nitrogen- and sulfhydryl-containing ligands. The anti-leishmanial mechanisms of Sb(III) are probably related to its interaction with sulfhydryl-containing biomolecules, including thiols, peptides, proteins, and enzymes.
Thus, Sb(III) was found to form stable complex with the major intracellular thiols, GSH and T(SH)2, in the form of a 1:3 and 1:1 Sb-thiol complexes, respectively [24, 26, 31]. Once Sb(III) is in the cell and conjugated to T(SH)2, the complex can be sequestered inside a vacuole or extruded by ATP-binding cassette (ABC) transporters [32, 33].
It has been reported that Sb(III) interferes with the thiol metabolism, not only by inducing efflux of intracellular T(SH)2 and GSH from intact leishmania cells, but also by inhibiting TR through specific interaction with the redox-active catalytic site [34], resulting in lower [T(SH)2]/[[T(S)2] ratio [35]. Both actions synergistically contribute to lowering the parasite-neutralizing capacity of reactive species coming from the host. It is worth noting that similar effects in thiol metabolism were observed with Sb(V) on axenic amastigotes in these studies. Now, it is also clearly established that Sb(III) triggered apoptotic cell death associated with ROS [36].
Whether the oxidative stress resulting from metal interference in thiol metabolism is sufficient to promote cell death or additional event involving metal interaction with other molecular target(s) takes place still has to be determined. In that sense, recent studies have identified zinc-finger protein as potential target of Sb(III) [37, 38]. The zinc finger domain is characterized by the coordination of a zinc atom by several amino acid residues, including cysteine and histidine. Zinc finger proteins sharing the CCHC motif have been identified in trypanosomatids and are likely to be involved in DNA replication, structure, and repair [39]. On the other hand, CCCH zinc finger domains, which are found mainly in RNA-binding proteins with regulatory functions at all stages of mRNA metabolism [40], are suspected to play a crucial role in the biology of kinetoplastid protozoa, because of the unusual emphasis on post-transcriptional control of gene expression in this group of organisms [41]. Interestingly, Sb(III) promotes Zn(II) ejection more effectively from CCCH zinc finger peptides than CCHC peptides [38], suggesting that the action of antimonial drugs could be related mainly to interaction of Sb(III) with CCCH zinc finger proteins.
Despite the strong evidence that Sb(III) mediates the antileishmanial action of pentavalent antimonials, some studies have suggested intrinsic pharmacological actions of Sb(V) [42–44].
Demicheli and co-workers have reported the formation of a complex between adenine ribonucleoside and Sb(V). This was the first report of a physiologically relevant biomolecule capable of forming stable complexes with Sb(V). Both 1:1 and 1:2 Sb(V)-ribonucleoside complexes were evidenced [19, 42, 45–47]. The large NMR resonance changes for H2′signal suggested that –OH groups in the ribosome are the binding sites for Sb(V) probably via ring chelation at C2′ and C3′.
Stibogluconate was found to be a potent inhibitor of protein tyrosine phosphatases, which leads to an increase in cytokine responses [44]. Another recent study revealed that this drug induced generation of ROS and NO via phosphoinositide 3-kinase and mitogen-activated protein kinase activation in Leishmania donovani-infected macrophages [48, 49], indicating that Sb(V) can stimulate the innate arm of the immune system. Meglumine antimoniate was also reported to increase the phagocytic capacity of monocytes and neutrophils and enhance superoxide anion production by phagocytes, which represent the first line of defense against the parasite [50].
As summarized in Fig. 30.2, these data taken altogether suggest that pentavalent antimonials affect the parasite viability through both Sb(III)-induced imbalance of thiol metabolism in parasite and Sb(V)-induced stimulation of macrophage microbicidal activity.
30.3.3 Redox Changes in Antimony-Resistant Parasites
Resistance of leishmania parasites to antimony has been extensively studied in both laboratory-selected resistant leishmania lines and field isolates [51, 52, 53], allowing important insights into the molecular and functional factors that modulate parasite sensitivity to the drug.
Most antimony-resistance associated genes are involved in metabolic process related to oxidative stress, cell redox homeostasis, and thiol biosynthesis [54], which is not surprising considering the mode of action of antimonial drugs.
A change often encountered in both laboratory-selected and field-isolated resistant leishmania parasites is overexpression of rate-limiting enzymes of thiol biosynthesis, such as ornithine decarboxylase and γ-glutamylcysteine synthetase, which causes an overproduction of intracellular thiols and extra protection against the oxidative stress upon drug exposure [55–58]. The higher rate of thiol synthesis may also result in enhanced rates of efflux through ABC transporters contributing to the resistance phenotype [33]. Overexpression of the multidrug resistance-associated protein A transporter responsible for sequestration of Sb-thiol conjugates in intracellular vesicles is another frequently observed change that contributes to the resistance phenotype in Leishmania [32]. Thiol depletion of these strains reestablished their susceptibility to Sb [57], indicating that the increased T(SH)2 levels are causing resistance.
Elevated levels of tryparedoxin and tryparedoxin peroxidase, key enzymes in hydroperoxide detoxification, were also observed in antimonial resistant parasites resulting in an increased metabolism of peroxides [59].
30.3.4 Redox-Related Toxicity of Antimonial Drugs
Even though pentavalent antimonials are still the first-line drugs in several countries against all forms of leishmaniasis, their use in the clinical setting has several limitations.
Antimony therapy is often accompanied by local pain during intramuscular injection and by severe side effects that include cardiotoxicity, pancreatitis, hepatotoxicity, and nephrotoxicity [9, 60].
Although the mechanism involved in the toxicity of pentavalent antimonials is not fully elucidated, it is generally accepted that Sb(III), either present as residue in pentavalent antimonials [61] or produced in the tissues through reduction [19], may be responsible for their side effects and antileishmanial action.
Studies of the mechanism of cytotoxicity of the trivalent tartar emetic drug suggest that Sb(III) compromises thiol homeostasis through depletion of intracellular glutathione and inhibition of glutathione reductase [22]. Then, Sb(III) enhances oxidative stress and leads to apoptosis through increase of ROS [22, 62–64].
Further evidence that pentavalent antimonials exert toxicity through induction of oxidative stress was obtained by Kato et al. [65], who demonstrated the protective effect of the antioxidant ascorbic acid during antimonial chemotherapy in a murine model of visceral leishmaniasis.
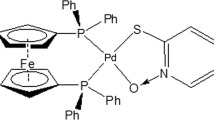
30.4 Gold Complexes Against Leishmaniasis
Auranofin (Fig. 30.3) is a US Food and Drug Administration-approved drug used t herapeutically for rheumatoid arthritis. It is the prototypical gold drug with remarkable broad-spectrum medicinal properties, inspiring the development of other Au(I) and Au(III) compounds [66]. More recently, the awarding of orphan-drug status to auranofin for the possible treatment of amebiasis (caused by Entamoeba histolytica, an intestinal protozoan parasite) has significant global health implications in developing countries [67]. Transcriptional profiling and thioredoxin reductase assays suggested that auranofin targets the E. histolytica thioredoxin reductase, preventing the reduction of thioredoxin and enhancing sensitivity of trophozoites to ROS-mediated killing. Auranofin also inhibits viral load in simian virus [68, 69]. In combination with auranofin, administration of buthionine sulfoximine, an inhibitor of glutathione synthesis, under a highly intensified antiretroviral treatment was followed, after therapy suspension, by a significant decrease of viral RNA and DNA in peripheral blood as compared to pre-therapy levels.
Auranofin has also shown antiparasitic (malaria, leishmaniasis) activity, very likely arising from inhibition of parasitic enzymes involved in the control of the redox metabolism [11, 66]. The validation of TR as a key enzyme of Leishmania infantum polyamine-dependent redox metabolism and a target for antileishmanial drugs suggested that thiophilic agents besides Sb(III) could be effective enzyme inhibitors and potential antileishmanial agents. The X-ray crystal structure of the auranofin–trypanothione reductase–NADPH complex resolved at 3.5 Å resolution showed gold bound to the two active site cysteine residues of TR [70]. The thiosugar moiety of auranofin is located at the trypanothione binding site, suggesting that auranofin may inhibit TR through a dual mechanism. Enzymatic assays revealed that auranofin causes a pronounced enzyme inhibition and the drug kills the promastigote stage of L. infantum at micromolar concentrations.
An integrated in vitro and in vivo screening platform incorporating multiple leishmania life cycles and species probed a focused library of pharmaceutically active compounds for identification and prioritization of bona fide cytotoxic chemotypes toward leishmania parasites. Auranofin was confirmed as a potent cytotoxic antileishmanial agent and inducer of apoptotic-like death in promastigotes. Significantly, the antileishmanial activity of auranofin transferred to cell-based amastigote assays as well as in vivo murine models [71].
Auranofin may represent a prototype drug that can be used to identify signaling pathways within the parasite and host cell critical for parasite growth and survival. Indeed, a structurally diverse group of Au(I)/Au(III) compounds behave as highly effective inhibitors of Leishmania infantum TR, some being even more effective than antimonials [72]. Simultaneous consideration of TR inhibition and antiproliferative potency has identified appropriate candidates for further evaluation. The current results suggest a foundation for potential exploitation of gold-based complexes as chemical tools or the basis of therapeutics for leishmaniasis.
Abbreviations
- ABC:
-
ATP-binding cassette
- Cys:
-
Cysteine
- Cys-Gly:
-
Cysteinyl-glycine
- GSH:
-
Glutathione
- iNOS:
-
Inducible nitric oxide synthase
- NO:
-
Nitric oxide
- MRPA:
-
Multidrug resistance-associated protein A
- ROS:
-
Reactive oxygen species
- TR:
-
Trypanothione reductase
- T(SH)2 :
-
Reduced trypanothione
- WHO:
-
World Health Organization
References
Nussbaum K, Honek J, Cadmus CM, Efferth T. Trypanosomatid parasites causing neglected diseases. Curr Med Chem. 2010;17:1594–617.
WHO [Internet]. C2015. Neglected tropical diseases. http://www.who.int/neglected_diseases/diseases/en/.
Riethmiller S. From atoxyl to salvarsan: searching for the magic bullet. Chemotherapy. 2005;51:234–42.
Chersterman C. Dr. Ernest A. H. Friedheim. A tribute on his eightieth birthday. Trans R Soc Trop Med Hyg. 1979;73:597–8.
Shen ZX, Chen GQ, Ni JH, Li XS, Xiong SM, Qiu QY, et al. Use of arsenic trioxide (As2O3) in the treatment of acute promyelocytic leucemia (APL): II. Clinical efficacy and pharmacokinetics in relapsed patients. Blood. 1997;89:3354–60.
Duffin J, René P. Anti-moine; anti-biotique: The public fortunes of the secret properties of antimony potassium tartrate (tartar emetic). J Hist Med Allied Sci. 1991;46:440–56.
Vianna G. Tratamento da leishmaniose tegumentar por injeções intravenosas de tártaro emético. 7 Congresso Brasileiro de Medicina Tropical de São Paulo, São Paulo, Brasil. 1912;4:426-8.
Peters W. The treatment of kala-azar. New approaches to an old problem. Indian J Med Res. 1981;73:1–18.
Frézard F, Demicheli C, Ribeiro RR. Pentavalent antimonials: new perspectives for old drugs. Molecules. 2009;14:2317–36.
Fricker SP, Mosi RM, Cameron BR, Baird I, Zhu Y, Anastassov V, et al. Metal compounds for the treatment of parasitic diseases. J Inorg Biochem. 2008;102:1839–45.
Navarro M, Gabiani C, Chiara M, Messore L, Gambino D. Metal-based drugs for malaria, trypanosomiasis and leishmaniasis: recent achievements and perspectives. Drug Discov Today. 2010;15:1070–8.
Setzer WN. Trypanosomatid disease drug discovery and target identification. Future Med Chem. 2013;5:1703–4.
Croft SL, Seifert K, Yardley V. Current scenario of drug development for leishmaniasis. Indian J Med Res. 2006;123:399–410.
Mukbel RM, Patten Jr C, Gibson K, Ghosh M, Petersen C, Jones DE. Macrophage killing of Leishmania amazonensis amastigotes requires both nitric oxide and superoxide. Am J Trop Med Hyg. 2007;76:669–75.
Van Assche T, Deschacht M, da Luz RA, Maes L, Cos P. Leishmania-macrophage interactions: insights into the redox biology. Free Radic Biol Med. 2011;51:337–51.
Krauth-Siegel RL, Comini MA. Redox control in trypanosomatids, parasitic protozoa with trypanothione-based thiol metabolism. Biochim Biophys Acta. 2008;1780:1236–48.
Bocedi A, Dawood KF, Fabrini R, Federici G, Gradoni L, Pedersen JZ, et al. Trypanothione efficiently intercepts nitric oxide as a harmless iron complex in trypanosomatid parasites. FASEB J. 2010;24:1035–42.
Ferreira CS, Martins PS, Demicheli C, Brochu C, Ouellette M, Frézard F. Thiol-induced reduction of antimony(V) into antimony(III): a comparative study with trypanothione, cysteinylglycine, cysteine and glutathione. Biometals. 2003;16:441–3.
Goodwin LC, Page JE. A study of the excretion of organic antimonials using a polarographic procedure. Biochem J. 1943;22:236–40.
Hansen C, Hansen EW, Hansen HR, Gammelgaard B, Sturup S. Reduction of Sb(V) in a human macrophage cell line measured by HPLC-ICP-MS. Biol Trace Elem Res. 2011;144:234–43.
Shaked-Mishan P, Ulrich N, Ephros M, Zilberstein D. Novel intracellular Sb(V) reducing activity correlates with antimony susceptibility in Leishmania donovani. J Biol Chem. 2001;276:3971–6.
Wyllie S, Fairlamb AH. Differential toxicity of antimonial compounds and their effects on glutathione homeostasis in a human leukaemia monocyte cell line. Biochem Pharmacol. 2006;71:257–67.
Sereno D, Cavaleyra M, Zemzoumi K, Maquaire S, Ouaissi A, Lemesre JL. Axenically grown amastigotes of Leishmania infantum used as an in vitro model to investigate the pentavalent antimony mode of action. Antimicrob Agents Chemother. 1998;42:3097–102.
Frézard F, Demicheli C, Ferreira CS, Costa MAP. Glutathione-induced conversion of pentavalent antimony to trivalent antimony in meglumine antimoniate. Antimicrob Agents Chemother. 2001;45:913–6.
Carrio J, de Colmenares M, Riera C, Gallego M, Arboix M, Portus M. Leishmania infantum: stage-specific activity of pentavalent antimony related with the assay conditions. Exp Parasitol. 2000;95:209–14.
Yan SC, Li F, Ding KY, Sun H. Reduction of pentavalent antimony by trypanothione and formation of a binary and ternary complex of antimony(III) and trypanothione. J Biol Inorg Chem. 2003;8:689–97.
Fairlamb AH, Cerami A. Metabolism and functions of trypanothione in the Kinetoplastida. Annu Rev Microbiol. 1992;46:695–729.
Denton H, McGregor JC, Coombs GH. Reduction of anti-leishmanial pentavalent antimonial drugs by a parasite-specific thiol-dependent reductase, TDR1. Biochem J. 2004;381:405–12.
Zhou Y, Messier N, Ouellette M, Rosen BP, Mukhopadhyay R. Leishmania major LmACR2 is a pentavalent antimony reductase that confers sensitivity to the drug Pentostam. J Biol Chem. 2004;279:37445–51.
Salaün P, Frézard F. Unexpectedly high levels of antimony (III) in the pentavalent antimonial drug Glucantime: insights from a new voltammetric approach. Anal Bioanal Chem. 2013;405:5201–14.
Sun H, Yan SC, Cheng WS. Interaction of antimony tartrate with the tripeptide glutathione. Eur J Biochem. 2000;267:5450–7.
Légaré D, Richard D, Mukhopadhyay R, Stierhof YD, Rosen BP, Haimeur A, et al. The Leishmania ATP-binding cassette protein PGPA is an intracellular metal-thiol transporter ATPase. J Biol Chem. 2001;276:26301–7.
Mukhopadhyay R, Dey S, Xu N, Gage D, Lightbody J, Ouellette M, et al. Trypanothione overproduction and resistance to antimonials and arsenicals in Leishmania. Proc Natl Acad Sci U S A. 1996;93:10383–7.
Baiocco P, Colotti G, Franceschini S, Ilari A. Molecular basis of antimony treatment in leishmaniasis. J Med Chem. 2009;52:2603–12.
Wyllie S, Cunningham ML, Fairlamb AH. Dual action of antimonial drugs on thiol redox metabolism in the human pathogen Leishmania donovani. J Biol Chem. 2004;279:39925–93.
Moreira W, Leprohon P, Ouellette M. Tolerance to drug-induced cell death favours the acquisition of multidrug resistance in Leishmania. Cell Death Dis. 2011;2, e201.
Demicheli C, Frézard F, Mangrum JB, Farrell NP. Interaction of trivalent antimony with a CCHC zinc finger domain: potential relevance to the mechanism of action of antimonial drugs. Chem Commun. 2008;39:4828–30.
Frézard F, Silva H, Pimenta AM, Farrell N, Demicheli C. Greater binding affinity of trivalent antimony to a CCCH zinc finger domain compared to a CCHC domain of kinetoplastid proteins. Metallomics. 2012;4:433–40.
Webb JR, McMaster WR. Molecular cloning and expression of a Leishmania major gene encoding a single-stranded DNA-binding protein containing nine “CCHC” zinc finger motifs. J Biol Chem. 1998;268:13994–4002.
Lai WS, Kennington EA, Blackshear PJ. Interactions of CCCH zinc finger proteins with mRNA: non-binding tristetraprolinmutants exert an inhibitory effect on degradation of AU-rich element-containing mRNAs. J Biol Chem. 2002;277:9606–13.
Clayton C, Shapira M. Post-transcriptional regulation of gene expression in trypanosomes and leishmanias. Mol Biochem Parasitol. 2007;156:93–101.
Demicheli C, Frézard F, Lecouvey M, Garnier-Suillerot A. Antimony(V) complex formation with adenine nucleosides in aqueous solution. Biochim Biophys Acta. 2002;1570:192–8.
Lucumi A, Robledo S, Gama V, Saravia NG. Sensitivity of Leishmania viannia panamensis to pentavalent antimony is correlated with the formation of cleavable DNA-protein complexes. Antimicrob Agents Chemother. 1998;42:1990–5.
Pathak MK, Yi T. Sodium stibogluconate is a potent inhibitor of protein tyrosine phosphatases and augments cytokine responses in hemopoietic cell lines. J Immunol. 2001;167:3391–7.
Chai Y, Yan S, Wong ILK, Chow LMC, Sun H. Complexation of antimony [Sb(V)] with guanosine 5′-monophosphate and guanosine 5′-diphospho-D-mannose: formation of both mono and bis-adducts. J Inorg Biochem. 2005;99:2257–63.
Demicheli C, Santos LS, Ferreira CS, Bouchemal N, Hantz E, Eberlin MN, et al. Synthesis and characterization of Sb(V)–adenosine and Sb(V)–guanosine complexes in aqueous solution. Inorg Chim Acta. 2006;359:159–67.
Hansen HR, Pergantis SA. Mass spectrometric identification and characterization of antimony complexes with ribose-containing biomolecules and an RNA oligomer. Anal Bioanal Chem. 2006;385:821–33.
Ghosh M, Roy K, Roy S. Immunomodulatory effects of antileishmanial drugs. J Antimicrob Chemother. 2013;68:2834–8.
Mookerjee Basu J, Mookerjee A, Sen P, Bhaumik S, Sen P, Banerjee S, et al. Sodium antimony gluconate induces generation of reactive oxygen species and nitric oxide via phosphoinositide 3-kinase and mitogen-activated protein kinase activation in Leishmania donovani-infected macrophages. Antimicrob Agents Chemother. 2006;50:1788–97.
Muniz-Junqueira MI, Paula-Coelho VN. Meglumine antimonate directly increases phagocytosis, superoxide anion and TNF-α production, but only via TNF-α it indirectly increases nitric oxide production by phagocytes of healthy individuals, in vitro. Int Immunopharmacol. 2008;8:1633–8.
Croft SL, Sundar S, Fairlamb AH. Drug resistance in leishmaniasis. Clin Microbiol Rev. 2006;19:111–26.
Decuypere S, Vanaerschot M, Brunker K, Imamura H, Muller S, Khanal B, et al. Molecular mechanisms of drug resistance in natural Leishmania populations vary with genetic background. PLoS Negl Trop Dis. 2012;6, e1514.
Ouellette M, Drummelsmith J, Papadopoulou B. Leishmaniasis: drugs in the clinic, resistance and new developments. Drug Resist Updat. 2004;7:257–66.
Frézard F, Monte-Neto R, Reis PG. Antimony transport mechanisms in resistant leishmania parasites. Biophys Rev. 2014;6:119–32.
Grondin K, Haimeur A, Mukhopadhyay R, Rosen BP, Ouellette M. Co-amplification of the gamma-glutamylcysteine synthetase gene gsh1 and of the ABC transporter gene pgpA in arsenite-resistant Leishmania tarentolae. EMBO J. 1997;16:3057–65.
Haimeur A, Guimond C, Pilote S, Mukhopadhyay R, Rosen BP, Poulin R, et al. Elevated levels of polyamines and trypanothione resulting from overexpression of the ornithine decarboxylase gene in arsenite-resistant Leishmania. Mol Microbiol. 1999;34:726–35.
Mandal G, Wyllie S, Singh N, Sundar S, Fairlamb AH, Chatterjee M. Increased levels of thiols protect antimony unresponsive Leishmania donovani field isolates against reactive oxygen species generated by trivalent antimony. Parasitology. 2007;134:1679–87.
Mukherjee A, Padmanabhan PK, Singh S, Roy G, Girard I, Chatterjee M, et al. Role of ABC transporter MRPA, gamma-glutamylcysteine synthetase and ornithine decarboxylase in natural antimony-resistant isolates of Leishmania donovani. J Antimicrob Chemother. 2007;59:204–11.
Wyllie S, Mandal G, Singh N, Sundar S, Fairlamb AH, Chatterjee M. Elevated levels of tryparedoxin peroxidase in antimony unresponsive Leishmania donovani field isolates. Mol Biochem Parasitol. 2010;173:162–4.
Marsden PD. Pentavalent antimonials: old drugs for new diseases. Rev Soc Bras Med Trop. 1985;18:187–98.
Dzamitika SA, Falcão CA, de Oliveira FB, Marbeuf C, Garnier-Suillerot A, Demicheli C et al. Role of residual Sb(III) in meglumine antimoniate cytotoxicity and MRP1-mediated resistance. Chem Biol Interact. 2006;160:217–24.
Lecureur V, Le Thiec A, Le Meur A, Amiot L, Drenou B, Bernard M, et al. Potassium antimonyl tartrate induces caspase- and reactive oxygen species-dependent apoptosis in lymphoid tumoral cells. Br J Haematol. 2002;119:608–15.
Lösler S, Schlief S, Kneifel C, Thiel E, Schrezenmeier H, Rojewski MT. Antimony trioxide- and arsenic-trioxide-induced apoptosis in myelogenic and lymphatic cell lines, recruitment of caspases, and loss of mitochondrial membrane potential are enhanced by modulators of the cellular glutathione redox system. Ann Hematol. 2009;88:1047–58.
Timerstein MA, Plews PI, Walker CV, Woolery MD, Wey HE, Toraason MA. Antimony induces oxidative-stress and toxicity in cultured cardiac myocytes. Toxicol Appl Pharmacol. 1995;130:41–7.
Kato KC, Morais-Teixeira E, Reis PG, Silva-Barcellos NM, Salaün P, Campos PP, et al. Hepatotoxicity of pentavalent antimonial drug: possible role of residual Sb(III) and protective effect of ascorbic acid. Antimicrob Agents Chemother. 2014;58:481–8.
Berners-Price SJ, Filipovska A. Gold compounds as therapeutic agents for human diseases. Metallomics. 2011;3:863–73.
Debnath A, Parsonage D, Andrade RM, He C, Cobo ER, Hirata K, et al. A high-throughput drug screen for Entamoeba histolytica identifies a new lead and target. Nat Med. 2012;18:956–62.
Lewis MG, DaFonseca S, Chomont N, Palamara AT, Tardugno M, Mai A et al. Gold drug auranofin restricts the viral reservoir in the monkey AIDS model and induces containment of viral load following ART suspension. AIDS. 2011;25:1347–56.
De Luca A, Hartinger CG, Dyson PJ, Lo Bello M, Casini A. A new target for gold(I) compounds: glutathione-S-transferase inhibition by auranofin. J Inorg Biochem. 2013; 119:38–42.
Ilari A, Baiocco P, Messori L, Fiorillo A, Boffi A, Gramiccia M, et al. A gold-containing drug against parasitic polyamine metabolism: the X-ray structure of trypanothione reductase from Leishmania infantum in complex with auranofin reveals a dual mechanism of enzyme inhibition. Amino Acids. 2012;42:803–11.
Sharlow ER, Leimgruber S, Murray S, Lira A, Sciotti RJ, Hickman M, et al. Auranofin is an apoptosis-simulating agent with in vitro and in vivo anti-leishmanial activity. ACS Chem Biol. 2014;9:663–72.
Colotti G, Ilari A, Fiorillo A, Baiocco P, Cinellu MA, Maiore L, et al. Metal-based compounds as prospective antileishmanial agents: inhibition of trypanothione reductase by selected gold complexes. ChemMedChem. 2013;8:1634–7.
Acknowledgment
We acknowledge the Brazilian agencies CNPq, FAPEMIG and CAPES for financial support. We thank the support of NSF-CHE-1413189 and Sciences Without Borders CAPES PVES 154/2012.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Demicheli, C., Frézard, F., Farrell, N.P. (2016). Redox-Active Metal Complexes in Trypanosomatids. In: Batinić-Haberle, I., Rebouças, J., Spasojević, I. (eds) Redox-Active Therapeutics. Oxidative Stress in Applied Basic Research and Clinical Practice. Springer, Cham. https://doi.org/10.1007/978-3-319-30705-3_30
Download citation
DOI: https://doi.org/10.1007/978-3-319-30705-3_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-30703-9
Online ISBN: 978-3-319-30705-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)