Abstract
As with other diseases of the eye, glaucoma patients face a number of challenges to efficient drug delivery such as low bioavailability due to transport barriers in the eye. It is important to note, however, that the pathophysiology of glaucoma, though not well understood, makes it a particularly challenging disease to address using traditional drug delivery techniques. Researchers have therefore begun to investigate approaches using nanotechnology, and in particular nanoscale biomaterials, to improve upon the delivery of approved and pipeline therapeutic agents. In addition to well-characterized vehicles like liposomes and polymer formulations, a wide variety of other devices like drug-loaded contact lenses and intraocular implants are in development. The primary goal of these drug delivery systems is to improve bioavailability, which may lead to increased adherence to treatment and decreased systemic side effects. Secondary goals like imaging and anti-scarring applications are also relevant to this widespread, vision-threatening disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Drug delivery to the eye presents a vast array of challenges that researchers are trying to address with modern nanotechnology. Much interest has been generated recently in this area, particularly for the treatment of glaucoma [1–3]. Emerging drugs [4–6], new therapeutic targets [7, 8], and an evolving understanding of the progression of the disease [9] make glaucoma an attractive application for translation of nanobiomaterials to the clinic. However, the eye is a complex organ, and each potential application possesses a unique set of issues to address. This chapter will focus on the additional barriers to drug delivery presented by glaucoma.
17.1 Drug Delivery Barriers Specific to Glaucoma
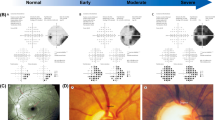
One must appreciate the complexities of glaucoma and its progression to understand why treating it is different from other ocular conditions. First, there is still much to learn about the pathogenesis of glaucoma [10], which makes treatment a much more formidable task. Much of the burden is placed on the patient for self-administration of eyedrop medication to treat the associated increase in intraocular pressure (IOP) [11]. Doctors treating patients with glaucoma must determine which, if any, of the many drug formulations are suitable given a patient’s age, disease severity, contraindications, and other factors [12]. Often, patients must also undergo surgery, which can introduce even more barriers to successful drug delivery. These and other challenges are described in detail below.
17.1.1 Patient Adherence
Perhaps the greatest barrier to effective glaucoma drug delivery is patient adherence to the prescribed treatment regimen. One study reports less than 30 % compliance with eyedrops for glaucoma [13], with another study determining that over a quarter of newly diagnosed patients discontinue use of their medication within 3 months [14]. Furthermore, even when patients do administer the drops, it is estimated that nearly 90 % do not instill drops correctly, leading to unintentional noncompliance [15]. The issue of patient adherence in glaucoma is of particular importance because of the implications of not treating the disease. As a progressive and chronic neurological disease, patients who are not properly treated are at a greatly increased risk of vision loss and blindness [16]. In fact, glaucoma accounts for up to 12 % of all cases of blindness in the US alone and is the second leading cause of blindness worldwide [17].
Most glaucoma medications aim to lower IOP in order to slow or stop the progression of the disease [11]. While these modern medications, the most common of which is the prostaglandin analog latanoprost (with over two million prescriptions in Europe alone in 2012 [18]), are quite effective when used properly, many patients struggle with doing so. One of the primary reasons for this lack of compliance is the frequency with which the drops must be self-administered. Latanoprost is administered once daily, which in itself can be challenging, while others such as brimonidine and timolol are delivered two to three times as often [19, 20].
Another significant obstacle is the difficulty in self-administration that many patients experience. Approximately one in ten individuals over 75 are diagnosed with glaucoma [21], which contributes to the high rates of patients who experience difficulty properly instilling the topical drops [15]. Many elderly patients lack the dexterity to self-administer their daily drops. Mobile phone applications, such as “EyeDROPS” (HarPas International), and educational programs [22] have been developed to try to improve compliance with regular reminders, yet these still cannot address the inherent challenges of drop self-administration.
One additional reason why patients may not adhere strictly to their topical drop regimen is the apparent lack of symptoms in those whose disease has not yet progressed [23]. Glaucoma is a largely painless disease and can go untreated for months or years before patients begin to see a decrease in vision [22]. The sometimes slow and often unnoticeable progression of glaucoma can result in patients placing less priority on their medication [15]. Doing so can have devastating effects, however, as vision loss due to glaucoma is irreversible [24].
17.1.2 Side Effects
One 2010, study showed a significant positive correlation between concerns about the side effects of eyedrop medication and intentional noncompliance with the prescribed treatment regimen [25]. Side effects such as blurred vision, burning or itching of the eyes, dry eye, foreign body sensation, and tearing are frequently reported with topical glaucoma medication use [26]. These inconvenient and sometimes painful side effects may prevent patients from appropriately administering drops [23, 25]. Additionally, any reformulation of existing glaucoma medication must take into account the potential side effects associated with the drug. As will be described further below, controlled release of drugs may be able to circumvent this issue by administering lower doses of drug while maintaining effectiveness [3].
17.1.3 Site of Action
When determining the best way to deliver glaucoma drugs, one must consider the site of action. Some drugs act on multiple sites [27], while for others, the primary site of action remains somewhat unclear, particularly for emerging neuroprotective agents [28, 29]. Brimonidine, for instance, is an alpha-adrenergic agonist used to lower IOP primarily through suppressing aqueous humor production and increasing uveoscleral outflow [30] that has also demonstrated potent systemic effects [31] and neuroprotective qualities [32, 33]. Successful drug delivery for glaucoma must factor in the targeted site of action and take steps to deliver the drug most efficiently to that site. For example, drugs acting on the posterior of the eye, like neurotropic factors, would be ideally delivered as an intravitreal injection to bypass the diffusion hindrances of the anterior tissues [24].
17.1.4 Limited Uptake
Depending on the site of action, as described above, the medication delivered can have variable uptake to the affected tissue. Topical drops in particular are unable to reach intraocular tissues in appreciable amounts [24]. The amount of drug that reaches various parts of the eye is heavily influenced by the structure of the drug. For example, small, lipophilic drugs are more readily absorbed through the cornea to the aqueous humor [34], while the permeability of the conjunctiva to larger, hydrophilic molecules is higher than both the sclera and cornea [35, 36]. A portion of drug is also taken up systemically, which can result in unwanted adverse effects [37, 38]. These factors cause the overall uptake to the aqueous humor to remain low, at less than 10 % [24]. This amount is difficult to increase through drop volume alone, due to the constant tear film turnover and size limitations of the conjunctival cul-de-sac [39].
17.1.5 Contraindications
While understanding the site of action and desired drug uptake are critical to designing a successful drug delivery system for glaucoma, some patients are contraindicated for certain methods. One such method is in intraocular injection, which can cause a temporary spike in IOP as well as a risk of retinal detachment, inflammation, and hemorrhage [40]. Patients with a history of acute inflammation in reaction to previous injections, active external ocular infection, or a recent history of thromboembolic events are not recommended for such treatments [41]. The design of intraocular implants or injections for glaucoma patients who are able to receive them would still need to ensure that there was no prolonged increase in IOP due to the implant. For example, one study demonstrates an increase over time in IOP for blank particles injected in the subconjunctival space [42], suggesting that the safety of this potential nanomaterial delivery route should be investigated further.
17.1.6 Pharmacokinetic Considerations
Current approved glaucoma medications have the intended effect of IOP reduction as a method of treating glaucoma. The hypotensive effect of these drugs can be achieved with discrete doses throughout the day, but as with many drugs, the pharmacokinetic profile is not ideal. More specifically, IOP can fluctuate greatly throughout the day based on a number of factors including activity level, posture, and time of day [43–45]. These fluctuations can lead to high IOP levels in certain patients and have been identified as a risk factor for progression of the disease [46, 47]. Peak IOP in patients has been shown to reach dangerous levels (greater than 21 mmHg) due to the peak/trough concentration dynamics of drug throughout the day as drops are administered, which may contribute to the percentage of patients whose disease progresses despite proper treatment [48]. An ideal drug release profile for many glaucoma drugs may be constant, linear (“zero order”) release kinetics, which can be difficult to achieve with common controlled-release biomaterial s [49].
17.1.7 Other Challenges
Glaucoma presents a number of other challenges that could potentially be addressed using nanotechnology. One such challenge is that of IOP monitoring , which is of primary importance because of the aforementioned fluctuations. These fluctuations vary widely from patient to patient and can be unpredictable [50]. Clinicians should monitor IOP closely in high-risk patients; however, the current standard of care provides only discrete measurements during office visits. One retrospective analysis determined that 24-h IOP monitoring led to increased early detection of glaucoma and changes in treatment for 79 % of patients in the studies included [51].
Uncontrolled IOP or other complications in glaucoma patients can require that surgery be performed to provide filtration of the aqueous humor. Trabeculectomy or shunting surgeries, as with any ocular procedure, introduce a risk of infection or inflammation. Patients are prescribed drops to decrease this risk, which can often lead to further complications. Drug delivery in these situations for glaucoma is made even more challenging by the need to incorporate postoperative care.
Another significant challenge to glaucoma drug delivery is the lack of information about the pathogenesis of the disease. Researchers are working to elucidate the mechanisms of the disease using imaging techniques that explore the outflow pathways and pathology associated with the disease [52–54]. Though not drug delivery in the traditional sense, nanotechnology could also aid in these studies to further improve the treatment options available to glaucoma patients.
17.2 Potential Advantages of Nanotechnology
Recently, there has been rapid progress in the field of nanoscale materials and devices for a number of drug delivery applications. In particular, this field has produced promising advances for a number of diseases that, similar to glaucoma, have unique challenges to successful drug delivery. One obvious example is cancer, where chemotherapeutic agents are being reformulated with nanocarriers for targeted delivery and diagnostics [55]. Nanomedicine has also been used to develop tuberculosis treatments aimed at increasing patient compliance rates, which are thought to be low due to the daily dosing requirements and significant side effects [56].
These examples highlight the versatility of nanotechnology for drug delivery. Such nanoscale systems can theoretically be used to deliver any ocular therapeutic, from small molecule drugs to viruses [2]. They can be administered through a variety of methods, including but not limited to drops, injections, and implants [57]. This adaptability is a prime advantage for a disease like glaucoma, where the individual needs of the patient must be considered when designing a drug delivery system. For instance, an elderly patient may not have the ability to instill topical drops, while a younger patient may prefer the freedom of self-administration.
The incredibly small size afforded by nanotechnology also offers the advantage of high payloads in a small dose [58], which is important in parts of the eye with limited volume like the anterior chamber. Additionally, the relatively small size of most nanocarriers and nanoscale excipients is ideal when conjugated with larger molecules like proteins and antibodies because they less likely affect their function in vivo [57]. Many of the materials that can be used in these drug delivery systems are already being used in FDA-approved formulations or devices, such as poly(lactic-co-glycolic acid) (PLGA). The proven track record of FDA approval for such nanomaterials can facilitate a faster and easier translation to the clinic [59].
17.3 Nanomaterials for Glaucoma Treatment
Perhaps the greatest research effort to use nanotechnology in treating glaucoma has been the field of nanoscale biomaterials for drug delivery. These materials aim to improve upon current drug formulations in a number of ways, which include lowering dosages, localized delivery, sustained release, and improved retention time. Yet other classes of nanomaterials for glaucoma are investigating experimental treatments for glaucoma, often taking advantage of the protection and targeted administration that is offered by some nanocarriers. Here we review various therapeutic biomaterial s that aim to address the aforementioned challenges in treating glaucoma. As with current drug formulations, these materials primarily seek to treat glaucoma through IOP reduction. Often, these materials involve a combination of approaches, such as sustained-release formulations incorporating a mucoadhesive carrier.
17.3.1 Vehicle Additives
Although topical drops for glaucoma are associated with low patient adherence rates, they are still a convenient and familiar method for administering antiglaucoma medication. Thus, many researchers have persisted with this route of administration using vehicle additives to improve the retention time of the drug in the precorneal surface and thereby increase the bioavailability of drug. The estimated retention time in the tear film for drugs is approximately 5–7 min due to the constant turnover of tear film, at a rate of about 13–20 % per minute [60].
One method to increase bioavailability is to add hydrogels to the eyedrop formulation. Some examples include hydroxypropyl methylcellulose (HPMC), carboxymethylcellulose (CMC), and propylene glycol [61, 62]. These additives and their polymeric variations act to absorb water and expand the tear film (which also makes them ideal for lubricants in dry eye therapy), thereby increasing retention time [63]. Increased retention time can result in fewer daily doses, leading to fewer systemic side effects and a reduced burden on the patient. Such was the case in a clinical investigation of 0.5 % aqueous timolol maleate (TM) drops versus 0.1 % hydrogel TM drops [64]. The hydrogel TM drops were administered once daily, resulting in a peak drug concentration of 1/6 that of the twice-daily aqueous drops and fewer cardiovascular side effects. These excipients can also serve to stabilize suspensions of nanocrystalline preparations of poorly soluble drugs, such as brinzolamide [65], to increase absorption [66].
Other additives focus on increasing mucoadhesion , the adhesion of two surfaces including a mucosal layer. Chitosan, a biodegradable polysaccharide, and hyaluronic acid (HA), a glycosaminoglycan abundantly found in extracellular matrix, are frequently added to aqueous eyedrop suspensions to increase bioavailability via mucoadhesion [67]. One study demonstrated significantly decreased IOP and improved mucoadhesion using a HA-modified chitosan carrier for the glaucoma drugs timolol and dorzolamide [68]. Surface modification of drug-loaded micellar structures demonstrated similarly positive results in vitro and in vivo [69].
The addition of bioadhesive polymers like CMC or HA can also help protect the ocular surface and reduce toxicity effects. In vitro tolerance of human corneal-limbal epithelial and conjunctival cells to bioadhesive formulations of TM was shown to be significantly higher in one study [70]. Similar results were seen in a separate in vivo study of the melatonin receptor agonist 5-methoxy-carbonylamino-N-acetyltryptamine, with the added benefit of over 30 % decrease in IOP for up to 7 h [71].
17.3.2 Nanoemulsions and Liposomes
Submicron emulsions offer a potential solution for delivering poorly water-soluble drugs. Also called nanoemulsions, these systems comprise a surfactant molecule surrounding a core of the hydrophobic drug [72]. The drug is dissolved in an oil phase which is then encapsulated in a surfactant usually labeled “generally recognized as safe” (GRAS) by the Food and Drug Administration (FDA), forming droplets tens to hundreds of nanometers in diameter. These droplets can be formed acoustically [73] or mechanically [74]. While simpler autoemulsification processes are possible, the high concentration of surfactant required generally makes these formulations unsafe for use in the eye [72].
Often, these formulations will also contain a mucoadhesive additive to further improve bioavailability, as with the formulation described by Ying et al. [75]. A nanoscale lipid emulsion of fluorescently labeled drug-containing poloxamer and chitosan surface modifiers was administered as a topical drop and resulted in significantly greater uptake to the posterior segment versus relevant control groups [75].
The glaucoma drug dorzolamide was also tested as a nanoemulsion using a number of different surfactants [76]. The emulsified forms of the drug showed no signs of irritation in a rabbit model and demonstrated significantly prolonged drug release behavior in vitro. These and similar results have the potential to reduce toxicity effects and dosing frequency for common hydrophobic glaucoma medications, notably prostaglandin analogs [77].
Liposomes are similar to nanoemulsions in that the drug material is contained within an outer layer, in this case made up of a lipid bilayer [78]. The advantages offered by liposomes are the ability to functionalize the surface for targeted delivery, increased solubility (as with submicron emulsions), enhanced biocompatibility, and protection of the drug from degradation [79, 80]. One such study demonstrated that liposomal acetazolamide (ACZ) resulted in less irritation (as determined by increased tear production), increased stability, and an extended hypotensive effect compared to ACZ solution [81].
One of the main drawbacks of both nanoemulsions and liposomes is the rapid release of drug from the core due to membrane diffusion across a very short path length (5–10 nm), which typically results in drug delivery times that cannot be sustained beyond several hours. The recent publication by Natarajan et al. [82], however, describes a liposomal nanocarrier with the latanoprost embedded in the bilayers that can sustain IOP-lowering effect for 120 days [82]. The authors hypothesize that drug release is sustained because transport is controlled by partitioning rather than by diffusion, as with traditional nanovesicles. The liposomes are administered as a subconjunctival injection, which has been reported in separate studies to be a preferred treatment method for glaucoma patients when the frequency of injections is low enough [83].
17.3.3 Polymeric Nanoparticles
Any particle with a diameter on the order of one to hundreds of nanometers can technically be considered a nanoparticle, which would include several of the aforementioned formulations such as nanocrystals, nanoemulsions, and liposomes. Also included within this definition are nanostructures consisting of degradable polymer or dendrimer matrices or combinations of materials. These nanoparticles are distinct because drug is embedded within a solid polymer matrix. The primary advantage offered by these solid nanospheres is the ability to sustain drug release for long periods of time while protecting the unreleased drug from the surrounding environment [78].
Drug release from solid nanospheres is controlled primarily by degradation of the polymer matrix, allowing for diffusion of the drug. One common material is poly(lactic-co-glycolic) acid (PLGA), which is commonly used to make slightly larger microparticles for glaucoma drug delivery lasting up to 1 month [42, 84]. Smaller, nano-sized particles typically cannot sustain drug release for as long and may undergo faster clearance when injected transsclerally, making them better suited for topical delivery to the anterior chamber [85]. The incorporation of drug-loaded PLGA nanoparticles in a polyamidoamine (PAMAM) dendrimer hydrogel has been shown to sustain drug release for 1 week in vivo, with ocular hypotensive effects lasting nearly as long [86]. These particles have the added advantage of low cytotoxicity and high versatility, with single and dual drug-releasing systems in development [87].
Polymer and dendrimer particles are also particularly well suited for delivery of biological therapeutic agents because they are protected from denaturation for the duration of drug release, which can last up to 1 month or more. One such formulation seeks to deliver matrix metalloproteinase-3 (MMP-3) to the trabecular meshwork to prevent buildup of extracellular matrix materials and subsequent IOP increase [88]. Biodegradable nano- or microspheres are also commonly used to deliver neurotrophic agents to the retina for neuroprotection in glaucoma models [89–91].
17.3.4 Hydrogels
A simple definition of a hydrogel is a water-soluble polymer whose properties allow it to be formed into particles, films, coatings, or formed solids [92]. These materials are attractive for drug delivery applications because their physical properties are highly tunable, like porosity, swelling ratio, and degradability. They are also highly biocompatible, primarily because of their high water content and mechanical properties resembling that of extracellular matrix (ECM) [93].
Drug release from the gel matrix is typically controlled by diffusion through the cross-linked polymer network, which often results in faster drug release than from water-insoluble polymer formulations [92, 94]. The highly porous structure also leads to low tensile strength and instability upon injection [92]. Many hydrogel formulations take advantage of copolymer additives to increase the cross-linking density and therefore alter the physical properties. Some examples include hydrogels that triggerably form a solid matrix after a change in temperature, pH, ionic strength, shear stress, and more [95, 96].
Hydrogel-based formulations have been widely investigated for ocular drug delivery via subconjunctival injection [97], nanogel eyedrops [98], and combination systems such as hydrogel-embedded liposomes. One system containing colloidal nanocarriers in a chitosan-based gel was able to sustain IOP reduction for 40 days in a rabbit glaucoma model [99]. Hydrogel-based intravitreal injections are also used for administering anti-VEGF (bevacizumab) in neovascular age-related macular degeneration [100, 101] and may also be used as a carrier for sustained delivery of a neuroprotective payload to the retina.
17.3.5 Contact Lenses
Since the widespread adoption of soft, gas permeable contact lenses in the 1980s, contact lenses have become a familiar and convenient option for vision correction, with a 2010 FDA report estimating 30 million users in the USA. The same materials used to make vision-correcting lenses are now being investigated for their potential as a drug delivery system. One major consideration for contact lens-based drug delivery is maintaining oxygen permeability and optical transparency.
Adsorption of drug onto traditional contact lenses is a simple method for increasing residence time of the drug on the cornea and offers a potential replacement for eyedrop administration [102]. However, these systems cannot sustain drug release beyond 1 day and require high levels of drug to ensure adequate loading, which can lead to an unwanted burst release [103]. To remedy this, other groups have investigated novel materials for contact lens-based drug delivery [104, 105]. One such system uses timolol-loaded nanoparticles within a silicone hydrogel contact lens [106]. Another system uses lenses molecularly imprinted by timolol at the nanoscale that can sustain drug delivery for up to twice as long as lenses without pre-imprinting [107].
The largest drawback to contact lenses for drug delivery is the potential for low patient compliance rates, estimated to be as low as 53 % for replacement of lenses and 45 % for proper handling [108]. This tendency could be problematic for drug delivery applications, as lenses would need to be changed at the appropriate intervals to ensure that therapeutic drug levels are being delivered. Additionally, improper handling and poor compliance could lead to additional complications such as contact lens-related dry eye and ocular surface infections.
17.3.6 Implants or Inserts
Although eyedrops may be more practical for some patients, such as those in developing nations, inserts, implants, and refillable devices have been explored for other patient populations that may benefit from a clinician-controlled drug delivery system. These systems are more frequently investigated for their use in treating posterior segment diseases, as with dexamethasone (Ozurdex®, Allergan) and fluocinolone acetonide (Retisert®, Bausch + Lomb) intravitreal implants for treating macular edema and uveitis, respectively [109]. This type of treatment would especially hold potential for treatment of neovascular glaucoma, using anti-VEGF [110], or neurotrophic factors for neuroprotection of retinal ganglion cells [111]. Care must be taken, however, as secondary glaucoma is a potential side effect for intravitreal implants and injection [40]. Similar rod-shaped implants have been tested for use in the subconjunctival space, providing months of release [112] from an administration method that one study suggests over 62 % of patients would prefer as a replacement for frequent eyedrops [113].
Nanoporous ocular inserts have also been described for use in treating glaucoma by releasing antiglaucoma drugs from within the conjunctival cul-de-sac for up to 28 days [114]. This device uses modern controlled-release polymer technology to improve upon passive diffusion-based systems that are no longer used [115, 116]. Building on the ocular insert concept is the latanoprost-loaded nanosheet, which can be applied directly to the cornea and provides up to 9 days of IOP reduction [117]. Similar results were also seen using an electrospun nanofiber patch placed in the conjunctival cul-de-sac [118].
Another unique device utilizes a microelectromechanical drug pump implanted similarly to a glaucoma drainage device [119]. This electrolysis-based pump is designed to provide 4–6 weeks of drug delivery with each transconjunctival drug refill. One distinct advantage of this type of nanodevice is that it could theoretically be loaded with any drug without having to redesign the device.
17.4 Other Uses of Nanotechnology for Glaucoma
Beyond antiglaucoma drug delivery , nanotechnology can serve other roles in the treatment of glaucoma patients. In patients receiving glaucoma filtration surgery, concomitant placement of drug-loaded nanoparticles can modulate the wound-healing response, thereby reducing scarring and improving the function of the bleb [120–122]. Nanocarriers loaded with corticosteroids that would traditionally be administered topically following trabeculectomy can also be used to provide autonomous postoperative care [123, 124].
Nanotechnology has also led to recent advances in the overall understanding of outflow pathways in the eye. Nano-sized tracers are injected into the anterior chamber and monitored over time [125] and can even be used in conjunction with antiglaucoma medication to determine the effect on drainage [54]. These techniques may aid in elucidating the pathophysiology of glaucoma and help identify potential new treatment methods for the disease.
As more is understood about glaucoma, the need for more reliable frequent IOP monitoring arises [126]. However, most patients only have IOP measured during visits to the clinic, which may miss peak IOP levels occurring at other times throughout the day [127]. Thus, some groups are using nanoscale devices, either implanted [128, 129] or embedded in a soft contact lens [130, 131], as a way of tracking IOP continuously and wirelessly reporting measurements back to the clinician. One recent publication describes a sensitive and precise microfluidic device whose output can be read using a smart phone camera, enabling at-home monitoring of IOP [132].
These and other applications of nanotechnology for glaucoma could potentially be combined with sustained-release drug delivery systems described above. Despite the challenges inherent to glaucoma drug delivery, nanoscale materials and devices offer myriad solutions that may one day improve the diagnosis, treatment, and outcomes for patients with glaucoma.
References
Egan P, Harris A, Siesky B, Abrams-Tobe L, Gerber AL, Park J, Holland S, Kim NJ, Januleviciene I (2014) Comparison of intraocular pressure in glaucoma subjects treated with Xalatan((R)) versus generic latanoprost. Acta Ophthalmol 92(5):e415–e416. doi:10.1111/aos.12321
Kim NJ, Harris A, Gerber A, Tobe LA, Amireskandari A, Huck A, Siesky B (2014) Nanotechnology and glaucoma: a review of the potential implications of glaucoma nanomedicine. Br J Ophthalmol 98(4):427–431. doi:10.1136/bjophthalmol-2013-304028
Pita-Thomas DW, Goldberg JL (2013) Nanotechnology and glaucoma: little particles for a big disease. Curr Opin Ophthalmol 24(2):130–135. doi:10.1097/ICU.0b013e32835cfe92
Bagnis A, Papadia M, Scotto R, Traverso CE (2011) Current and emerging medical therapies in the treatment of glaucoma. Expert Opin Emerg Drugs 16(2):293–307. doi:10.1517/14728214.2011.563733
Wang SK, Chang RT (2014) An emerging treatment option for glaucoma: Rho kinase inhibitors. Clin Ophthalmol 8:883–890. doi:10.2147/OPTH.S41000
Wu JH, Zhang SH, Gao FJ, Lei Y, Chen XY, Gao F, Zhang SJ, Sun XH (2013) RNAi screening identifies GSK3beta as a regulator of DRP1 and the neuroprotection of lithium chloride against elevated pressure involved in downregulation of DRP1. Neurosci Lett 554:99–104. doi:10.1016/j.neulet.2013.08.057
Dey S, Mitra AK (2005) Transporters and receptors in ocular drug delivery: opportunities and challenges. Expert Opin Drug Deliv 2(2):201–204. doi:10.1517/17425247.2.2.201
Crooke A, Colligris B, Pintor J (2012) Update in glaucoma medicinal chemistry: emerging evidence for the importance of melatonin analogues. Curr Med Chem 19(21):3508–3522
Yucel YH, Johnston MG, Ly T, Patel M, Drake B, Gumus E, Fraenkl SA, Moore S, Tobbia D, Armstrong D, Horvath E, Gupta N (2009) Identification of lymphatics in the ciliary body of the human eye: a novel “uveolymphatic” outflow pathway. Exp Eye Res 89(5):810–819. doi:10.1016/j.exer.2009.08.010
Gemenetzi M, Yang Y, Lotery AJ (2012) Current concepts on primary open-angle glaucoma genetics: a contribution to disease pathophysiology and future treatment. Eye (Lond) 26(3):355–369. doi:10.1038/eye.2011.309
Quigley HA (2011) Glaucoma. Lancet 377(9774):1367–1377. doi:10.1016/S0140-6736(10)61423-7, Epub 2011/04/02. S0140-6736(10)61423-7 [pii]
Morrison JC, Pollack IP (2011) Glaucoma: science and practice. Thieme, New York
Campbell JH, Schwartz GF, LaBounty B, Kowalski JW, Patel VD (2014) Patient adherence and persistence with topical ocular hypotensive therapy in real-world practice: a comparison of bimatoprost 0.01% and travoprost Z 0.004% ophthalmic solutions. Clin Ophthalmol 8:927–935. doi:10.2147/OPTH.S49467
Kashiwagi K, Furuya T (2014) Persistence with topical glaucoma therapy among newly diagnosed Japanese patients. Jpn J Ophthalmol 58(1):68–74. doi:10.1007/s10384-013-0284-2
Gupta R, Patil B, Shah BM, Bali SJ, Mishra SK, Dada T (2012) Evaluating eye drop instillation technique in glaucoma patients. J Glaucoma 21(3):189–192. doi:10.1097/IJG.0b013e31820bd2e1
Musch DC, Gillespie BW, Niziol LM, Lichter PR, Varma R, Group CS (2011) Intraocular pressure control and long-term visual field loss in the collaborative initial glaucoma treatment study. Ophthalmology 118(9):1766–1773. doi:10.1016/j.ophtha.2011.01.047
Quigley HA, Vitale S (1997) Models of open-angle glaucoma prevalence and incidence in the United States. Invest Ophthalmol Vis Sci 38(1):83–91
Painter SL, Mead AL (2014) Patient experience of the transition from Xalatan to generic latanoprost. Eye (Lond) 28(7):911. doi:10.1038/eye.2014.71
Cantor LB (2006) Brimonidine in the treatment of glaucoma and ocular hypertension. Ther Clin Risk Manag 2(4):337–346
Moisseiev E, Kurtz S, Lazar M, Shemesh G (2013) Intraocular pressure reduction using a fixed combination of timolol maleate 0.5% and brimonidine tartrate 0.2% administered three times daily. Clin Ophthalmol 7:1269–1273. doi:10.2147/OPTH.S47760
Klein R, Klein BE (2013) The prevalence of age-related eye diseases and visual impairment in aging: current estimates. Invest Ophthalmol Vis Sci 54(14):ORSF5–ORSF13. doi:10.1167/iovs.13-12789
Waterman H, Evans JR, Gray TA, Henson D, Harper R (2013) Interventions for improving adherence to ocular hypotensive therapy. Cochrane Database Syst Rev 4:CD006132. doi:10.1002/14651858.CD006132.pub3
Lacey J, Cate H, Broadway DC (2009) Barriers to adherence with glaucoma medications: a qualitative research study. Eye (Lond) 23(4):924–932. doi:10.1038/eye.2008.103
Ghate D, Edelhauser HF (2008) Barriers to glaucoma drug delivery. J Glaucoma 17(2):147–156. doi:10.1097/IJG.0b013e31814b990d
Rees G, Leong O, Crowston JG, Lamoureux EL (2010) Intentional and unintentional nonadherence to ocular hypotensive treatment in patients with glaucoma. Ophthalmology 117(5):903–908. doi:10.1016/j.ophtha.2009.10.038
Pisella PJ, Pouliquen P, Baudouin C (2002) Prevalence of ocular symptoms and signs with preserved and preservative free glaucoma medication. Br J Ophthalmol 86(4):418–423
Robin AL, Burnstein Y (1998) Selectivity of site of action and systemic effects of topical alpha agonists. Curr Opin Ophthalmol 9(2):30–33
Levkovitch-Verbin H, Waserzoog Y, Vander S, Makarovsky D, Ilia P (2014) Minocycline mechanism of neuroprotection involves the Bcl-2 gene family in optic nerve transection. Int J Neurosci. doi:10.3109/00207454.2013.878340
Roos JC, Haridas AS (2014) Prolonged mydriasis after inadvertent topical administration of the calcium channel antagonist amlodipine: implications for glaucoma drug development. Cutan Ocul Toxicol. doi:10.3109/15569527.2014.896016
Greenfield DS, Liebmann JM, Ritch R (1997) Brimonidine: a new alpha2-adrenoreceptor agonist for glaucoma treatment. J Glaucoma 6(4):250–258
Sy GY, Bruban V, Bousquet P, Feldman J (2002) Nitric oxide discriminates the sites and mechanisms of action of centrally acting anti-hypertensive drugs in rabbits. Neuropharmacology 43(8):1330–1338
Dong CJ, Guo Y, Agey P, Wheeler L, Hare WA (2008) Alpha2 adrenergic modulation of NMDA receptor function as a major mechanism of RGC protection in experimental glaucoma and retinal excitotoxicity. Invest Ophthalmol Vis Sci 49(10):4515–4522. doi:10.1167/iovs.08-2078
Fujita Y, Sato A, Yamashita T (2013) Brimonidine promotes axon growth after optic nerve injury through Erk phosphorylation. Cell Death Disease 4:e763. doi:10.1038/cddis.2013.298
Schoenwald RW (1997) Ocular pharmacokinetics. In: Z TJ (ed) Textbook of ocular pharmacology., pp 119–138
Ahmed I, Gokhale RD, Shah MV, Patton TF (1987) Physicochemical determinants of drug diffusion across the conjunctiva, sclera, and cornea. J Pharm Sci 76(8):583–586
Sasaki H, Igarashi Y, Nagano T, Nishida K, Nakamura J (1995) Different effects of absorption promoters on corneal and conjunctival penetration of ophthalmic beta-blockers. Pharm Res 12(8):1146–1150
Korte JM, Kaila T, Saari KM (2002) Systemic bioavailability and cardiopulmonary effects of 0.5% timolol eyedrops. Graefes Arch Clin Exp Ophthalmol 240(6):430–435. doi:10.1007/s00417-002-0462-2
Lama PJ (2002) Systemic adverse effects of beta-adrenergic blockers: an evidence-based assessment. Am J Ophthalmol 134(5):749–760
Mishima S, Gasset A, Klyce SD Jr, Baum JL (1966) Determination of tear volume and tear flow. Invest Ophthalmol 5(3):264–276
Frenkel MP, Haji SA, Frenkel RE (2010) Effect of prophylactic intraocular pressure-lowering medication on intraocular pressure spikes after intravitreal injections. Arch Ophthalmol 128(12):1523–1527. doi:10.1001/archophthalmol.2010.297
Semeraro F, Morescalchi F, Duse S, Gambicorti E, Romano MR, Costagliola C (2014) Systemic thromboembolic adverse events in patients treated with intravitreal anti-VEGF drugs for neovascular age-related macular degeneration: an overview. Expert Opin Drug Saf 13(6):785–802. doi:10.1517/14740338.2014.911284
Fedorchak MV, Conner IP, Medina CA, Wingard JB, Schuman JS, Little SR (2014) 28-day intraocular pressure reduction with a single dose of brimonidine tartrate-loaded microspheres. Exp Eye Res 125:210–216. doi:10.1016/j.exer.2014.06.013
Liu JH, Zhang X, Kripke DF, Weinreb RN (2003) Twenty-four-hour intraocular pressure pattern associated with early glaucomatous changes. Invest Ophthalmol Vis Sci 44(4):1586–1590
Mansouri K, Weinreb RN, Liu JH (2012) Effects of aging on 24-hour intraocular pressure measurements in sitting and supine body positions. Invest Ophthalmol Vis Sci 53(1):112–116. doi:10.1167/iovs.11-8763
Wilensky JT, Gieser DK, Dietsche ML, Mori MT, Zeimer R (1993) Individual variability in the diurnal intraocular pressure curve. Ophthalmology 100(6):940–944
Lee YR, Kook MS, Joe SG, Na JH, Han S, Kim S, Shin CJ (2012) Circadian (24-hour) pattern of intraocular pressure and visual field damage in eyes with normal-tension glaucoma. Invest Ophthalmol Vis Sci 53(2):881–887. doi:10.1167/iovs.11-7846
Renard E, Palombi K, Gronfier C, Pepin JL, Noel C, Chiquet C, Romanet JP (2010) Twenty-four hour (Nyctohemeral) rhythm of intraocular pressure and ocular perfusion pressure in normal-tension glaucoma. Invest Ophthalmol Vis Sci 51(2):882–889. doi:10.1167/iovs.09-3668
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, Parrish RK 2nd, Wilson MR, Gordon MO (2002) The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 120(6):701–713, discussion 829–30
Mohammadi-Samani S, Taghipour B (2014) PLGA micro and nanoparticles in delivery of peptides and proteins; problems and approaches. Pharm Dev Technol. doi:10.3109/10837450.2014.882940
Tanaka S, Watanabe M, Inatomi S, Umeda K, Yoshida K, Ohguro I, Ohguro H (2014) Effects of several anti-glaucoma medications on the circadian intraocular pressure fluctuations in patients with primary open-angle glaucoma. J Ocul Pharmacol Ther 30(1):12–20. doi:10.1089/jop.2013.0121
Hughes E, Spry P, Diamond J (2003) 24-hour monitoring of intraocular pressure in glaucoma management: a retrospective review. J Glaucoma 12(3):232–236
Ho LC, Conner IP, Do CW, Kim SG, Wu EX, Wollstein G, Schuman JS, Chan KC (2014) In vivo assessment of aqueous humor dynamics upon chronic ocular hypertension and hypotensive drug treatment using gadolinium-enhanced MRI. Invest Ophthalmol Vis Sci 55(6):3747–3757. doi:10.1167/iovs.14-14263
Tam AL, Gupta N, Zhang Z, Yucel YH (2011) Quantum dots trace lymphatic drainage from the mouse eye. Nanotechnology 22(42):425101. doi:10.1088/0957-4484/22/42/425101
Tam AL, Gupta N, Zhang Z, Yucel YH (2013) Latanoprost stimulates ocular lymphatic drainage: an in vivo nanotracer study. Transl Vis Sci Technol 2(5):3. doi:10.1167/tvst.2.5.3
Aslan B, Ozpolat B, Sood AK, Lopez-Berestein G (2013) Nanotechnology in cancer therapy. J Drug Target 21(10):904–913. doi:10.3109/1061186X.2013.837469
Dube A, Lemmer Y, Hayeshi R, Balogun M, Labuschagne P, Swai H, Kalombo L (2013) State of the art and future directions in nanomedicine for tuberculosis. Expert Opin Drug Deliv 10(12):1725–1734. doi:10.1517/17425247.2014.846905
Kompella UB, Amrite AC, Pacha Ravi R, Durazo SA (2013) Nanomedicines for back of the eye drug delivery, gene delivery, and imaging. Prog Retin Eye Res 36:172–198. doi:10.1016/j.preteyeres.2013.04.001
Zarbin MA, Montemagno C, Leary JF, Ritch R (2010) Nanomedicine in ophthalmology: the new frontier. Am J Ophthalmol 150(2):144–162.e2. doi:10.1016/j.ajo.2010.03.019
Danhier F, Ansorena E, Silva JM, Coco R, Le Breton A, Preat V (2012) PLGA-based nanoparticles: an overview of biomedical applications. J Control Release 161(2):505–522. doi:10.1016/j.jconrel.2012.01.043, Epub 2012/02/23
Greaves JL, Wilson CG (1993) Treatment of diseases of the eye with mucoadhesive delivery systems. Adv Drug Deliver Rev 11(3):349–383. doi:10.1016/0169-409x(93)90016-W
Cohen S, Martin A, Sall K (2014) Evaluation of clinical outcomes in patients with dry eye disease using lubricant eye drops containing polyethylene glycol or carboxymethylcellulose. Clin Ophthalmol 8:157–164. doi:10.2147/OPTH.S53822
Jansook P, Stefansson E, Thorsteinsdottir M, Sigurdsson BB, Kristjansdottir SS, Bas JF, Sigurdsson HH, Loftsson T (2010) Cyclodextrin solubilization of carbonic anhydrase inhibitor drugs: formulation of dorzolamide eye drop microparticle suspension. Eur J Pharm Biopharm 76(2):208–214. doi:10.1016/j.ejpb.2010.07.005
Mayol L, Quaglia F, Borzacchiello A, Ambrosio L, La Rotonda MI (2008) A novel poloxamers/hyaluronic acid in situ forming hydrogel for drug delivery: rheological, mucoadhesive and in vitro release properties. Eur J Pharm Biopharm 70(1):199–206. doi:10.1016/j.ejpb.2008.04.025
Uusitalo H, Kahonen M, Ropo A, Maenpaa J, Bjarnhall G, Hedenstrom H, Turjanmaa V (2006) Improved systemic safety and risk-benefit ratio of topical 0.1% timolol hydrogel compared with 0.5% timolol aqueous solution in the treatment of glaucoma. Graefes Arch Clin Exp Ophthalmol 244(11):1491–1496. doi:10.1007/s00417-006-0328-0
Wu W, Li J, Wu L, Wang B, Wang Z, Xu Q, Xin H (2013) Ophthalmic delivery of brinzolamide by liquid crystalline nanoparticles: in vitro and in vivo evaluation. AAPS PharmSciTech 14(3):1063–1071. doi:10.1208/s12249-013-9997-2
Tuomela A, Liu P, Puranen J, Ronkko S, Laaksonen T, Kalesnykas G, Oksala O, Ilkka J, Laru J, Jarvinen K, Hirvonen J, Peltonen L (2014) Brinzolamide nanocrystal formulations for ophthalmic delivery: reduction of elevated intraocular pressure in vivo. Int J Pharm 467(1–2):34–41. doi:10.1016/j.ijpharm.2014.03.048
Kaur IP, Smitha R (2002) Penetration enhancers and ocular bioadhesives: two new avenues for ophthalmic drug delivery. Drug Dev Ind Pharm 28(4):353–369. doi:10.1081/DDC-120002997
Wadhwa S, Paliwal R, Paliwal SR, Vyas SP (2010) Hyaluronic acid modified chitosan nanoparticles for effective management of glaucoma: development, characterization, and evaluation. J Drug Target 18(4):292–302. doi:10.3109/10611860903450023, Epub 2009/12/01
Lin HR, Chang PC (2013) Novel pluronic-chitosan micelle as an ocular delivery system. J Biomed Mater Res B Appl Biomater 101(5):689–699. doi:10.1002/jbm.b.32871
Andres-Guerrero V, Vicario-de-la-Torre M, Molina-Martinez IT, Benitez-del-Castillo JM, Garcia-Feijoo J, Herrero-Vanrell R (2011) Comparison of the in vitro tolerance and in vivo efficacy of traditional timolol maleate eye drops versus new formulations with bioadhesive polymers. Invest Ophthalmol Vis Sci 52(6):3548–3556. doi:10.1167/iovs.10-6338
Andres-Guerrero V, Molina-Martinez IT, Peral A, de las Heras B, Pintor J, Herrero-Vanrell R (2011) The use of mucoadhesive polymers to enhance the hypotensive effect of a melatonin analogue, 5-MCA-NAT, in rabbit eyes. Invest Ophthalmol Vis Sci 52(3):1507–1515. doi:10.1167/iovs.10-6099
Vandamme TF (2002) Microemulsions as ocular drug delivery systems: recent developments and future challenges. Prog Retin Eye Res 21(1):15–34
Sivakumar M, Tang SY, Tan KW (2014) Cavitation technology – a greener processing technique for the generation of pharmaceutical nanoemulsions. Ultrason Sonochem 21(6):2069–2083. doi:10.1016/j.ultsonch.2014.03.025
Benita S, Levy MY (1993) Submicron emulsions as colloidal drug carriers for intravenous administration: comprehensive physicochemical characterization. J Pharm Sci 82(11):1069–1079
Ying L, Tahara K, Takeuchi H (2013) Drug delivery to the ocular posterior segment using lipid emulsion via eye drop administration: effect of emulsion formulations and surface modification. Int J Pharm 453(2):329–335. doi:10.1016/j.ijpharm.2013.06.024
Ammar HO, Salama HA, Ghorab M, Mahmoud AA (2009) Nanoemulsion as a potential ophthalmic delivery system for dorzolamide hydrochloride. AAPS PharmSciTech 10(3):808–819. doi:10.1208/s12249-009-9268-4
Linden C (2001) Therapeutic potential of prostaglandin analogues in glaucoma. Expert Opin Investig Drugs 10(4):679–694. doi:10.1517/13543784.10.4.679
Honda M, Asai T, Oku N, Araki Y, Tanaka M, Ebihara N (2013) Liposomes and nanotechnology in drug development: focus on ocular targets. Int J Nanomedicine 8:495–503. doi:10.2147/IJN.S30725
Gan L, Wang J, Jiang M, Bartlett H, Ouyang D, Eperjesi F, Liu J, Gan Y (2013) Recent advances in topical ophthalmic drug delivery with lipid-based nanocarriers. Drug Discov Today 18(5–6):290–297. doi:10.1016/j.drudis.2012.10.005
Swaminathan J, Ehrhardt C (2012) Liposomal delivery of proteins and peptides. Expert Opin Drug Deliv 9(12):1489–1503. doi:10.1517/17425247.2012.735658
Pisal PB, Joshi MA, Padamwar MN, Patil SS, Pokharkar VB (2014) Probing influence of methodological variation on active loading of acetazolamide into nanoliposomes: biophysical, in vitro, ex vivo, in vivo and rheological investigation. Int J Pharm 461(1–2):82–88. doi:10.1016/j.ijpharm.2013.11.034
Natarajan JV, Darwitan A, Barathi VA, Ang M, Htoon HM, Boey F, Tam KC, Wong TT, Venkatraman SS (2014) Sustained drug release in nanomedicine: a long-acting nanocarrier-based formulation for glaucoma. ACS Nano 8(1):419–429. doi:10.1021/nn4046024
Chong RS, Su DH, Tsai A, Jiang Y, Htoon HM, Lamoureux EL, Aung T, Wong TT (2013) Patient acceptance and attitude toward an alternative method of subconjunctival injection for the medical treatment of glaucoma. J Glaucoma 22(3):190–194. doi:10.1097/IJG.0b013e318237c6c4
Bertram JP, Saluja SS, McKain J, Lavik EB (2009) Sustained delivery of timolol maleate from poly(lactic-co-glycolic acid)/poly(lactic acid) microspheres for over 3 months. J Microencapsul 26(1):18–26. doi:10.1080/02652040802095250
Amrite AC, Edelhauser HF, Singh SR, Kompella UB (2008) Effect of circulation on the disposition and ocular tissue distribution of 20 nm nanoparticles after periocular administration. Mol Vis 14:150–160
Yang H, Tyagi P, Kadam RS, Holden CA, Kompella UB (2012) Hybrid dendrimer hydrogel/PLGA nanoparticle platform sustains drug delivery for one week and antiglaucoma effects for four days following one-time topical administration. ACS Nano 6(9):7595–7606. doi:10.1021/nn301873v, Epub 2012/08/11
Zhou HY, Hao JL, Wang S, Zheng Y, Zhang WS (2013) Nanoparticles in the ocular drug delivery. Int J Ophthalmol 6(3):390–396. doi:10.3980/j.issn.2222-3959.2013.03.25
Turturro S, Sunoqrot S, Ying H, Hong S, Yue BY (2013) Sustained release of matrix metalloproteinase-3 to trabecular meshwork cells using biodegradable PLGA microparticles. Mol Pharm 10(8):3023–3032. doi:10.1021/mp4001052
Checa-Casalengua P, Jiang C, Bravo-Osuna I, Tucker BA, Molina-Martinez IT, Young MJ, Herrero-Vanrell R (2011) Retinal ganglion cells survival in a glaucoma model by GDNF/Vit E PLGA microspheres prepared according to a novel microencapsulation procedure. J Control Release 156(1):92–100. doi:10.1016/j.jconrel.2011.06.023
Ward MS, Khoobehi A, Lavik EB, Langer R, Young MJ (2007) Neuroprotection of retinal ganglion cells in DBA/2J mice with GDNF-loaded biodegradable microspheres. J Pharm Sci 96(3):558–568. doi:10.1002/jps.20629
Xiao JH, Zhang MN (2010) Neuroprotection of retinal ganglion cells with GDNF-Loaded biodegradable microspheres in experimental glaucoma. Int J Ophthalmol 3(3):189–191. doi:10.3980/j.issn.2222-3959.2010.03.01
Hoare TR, Kohane DS (2008) Hydrogels in drug delivery: progress and challenges. Polymer 49(8):1993–2007. doi:10.1016/J.Polymer.2008.01.027
Gauvin R, Parenteau-Bareil R, Dokmeci MR, Merryman WD, Khademhosseini A (2012) Hydrogels and microtechnologies for engineering the cellular microenvironment. Wiley Interdiscip Rev Nanomed Nanobiotechnol 4(3):235–246. doi:10.1002/wnan.171
Yang H, Leffler CT (2013) Hybrid dendrimer hydrogel/poly(lactic-co-glycolic acid) nanoparticle platform: an advanced vehicle for topical delivery of antiglaucoma drugs and a likely solution to improving compliance and adherence in glaucoma management. J Ocul Pharmacol Ther 29(2):166–172. doi:10.1089/jop.2012.0197
Joglekar M, Trewyn BG (2013) Polymer-based stimuli-responsive nanosystems for biomedical applications. Biotechnol J 8(8):931–945. doi:10.1002/biot.201300073
Klouda L, Mikos AG (2008) Thermoresponsive hydrogels in biomedical applications. Eur J Pharm Biopharm 68(1):34–45. doi:10.1016/j.ejpb.2007.02.025
Cheng YH, Hung KH, Tsai TH, Lee CJ, Ku RY, Chiu AW, Chiou SH, Liu CJ (2014) Sustained delivery of latanoprost by thermosensitive chitosan-gelatin-based hydrogel for controlling ocular hypertension. Acta Biomater. doi:10.1016/j.actbio.2014.05.031.PubMed
Abd El-Rehim HA, Swilem AE, Klingner A, el Hegazy SA, Hamed AA (2013) Developing the potential ophthalmic applications of pilocarpine entrapped into polyvinylpyrrolidone-poly(acrylic acid) nanogel dispersions prepared by gamma radiation. Biomacromolecules 14(3):688–698. doi:10.1021/bm301742m
Hsiao MH, Chiou SH, Larsson M, Hung KH, Wang YL, Liu CJ, Liu DM (2014) A temperature-induced and shear-reversible assembly of latanoprost-loaded amphiphilic chitosan colloids: characterization and in vivo glaucoma treatment. Acta Biomater 10(7):3188–3196. doi:10.1016/j.actbio.2014.03.016
Rauck BM, Friberg TR, Medina Mendez CA, Park D, Shah V, Bilonick RA, Wang Y (2014) Biocompatible reverse thermal gel sustains the release of intravitreal bevacizumab in vivo. Invest Ophthalmol Vis Sci 55(1):469–476. doi:10.1167/iovs.13-13120
Wang CH, Hwang YS, Chiang PR, Shen CR, Hong WH, Hsiue GH (2012) Extended release of bevacizumab by thermosensitive biodegradable and biocompatible hydrogel. Biomacromolecules 13(1):40–48. doi:10.1021/bm2009558
Peng CC, Ben-Shlomo A, Mackay EO, Plummer CE, Chauhan A (2012) Drug delivery by contact lens in spontaneously glaucomatous dogs. Curr Eye Res 37(3):204–211. doi:10.3109/02713683.2011.630154
Karlgard CC, Wong NS, Jones LW, Moresoli C (2003) In vitro uptake and release studies of ocular pharmaceutical agents by silicon-containing and p-HEMA hydrogel contact lens materials. Int J Pharm 257(1–2):141–151
Ciolino JB, Stefanescu CF, Ross AE, Salvador-Culla B, Cortez P, Ford EM, Wymbs KA, Sprague SL, Mascoop DR, Rudina SS, Trauger SA, Cade F, Kohane DS (2014) In vivo performance of a drug-eluting contact lens to treat glaucoma for a month. Biomaterials 35(1):432–439. doi:10.1016/j.biomaterials.2013.09.032
Kim HJ, Zhang K, Moore L, Ho D (2014) Diamond nanogel-embedded contact lenses mediate lysozyme-dependent therapeutic release. ACS Nano 8(3):2998–3005. doi:10.1021/nn5002968
Jung HJ, Abou-Jaoude M, Carbia BE, Plummer C, Chauhan A (2013) Glaucoma therapy by extended release of timolol from nanoparticle loaded silicone-hydrogel contact lenses. J Control Release 165(1):82–89. doi:10.1016/j.jconrel.2012.10.010
Hiratani H, Fujiwara A, Tamiya Y, Mizutani Y, Alvarez-Lorenzo C (2005) Ocular release of timolol from molecularly imprinted soft contact lenses. Biomaterials 26(11):1293–1298. doi:10.1016/j.biomaterials.2004.04.030
Ramamoorthy P, Nichols JJ (2014) Compliance factors associated with contact lens-related dry eye. Eye Contact Lens 40(1):17–22. doi:10.1097/ICL.0000000000000009
Choonara YE, Pillay V, Danckwerts MP, Carmichael TR, du Toit LC (2010) A review of implantable intravitreal drug delivery technologies for the treatment of posterior segment eye diseases. J Pharm Sci 99(5):2219–2239. doi:10.1002/jps.21987
Simha A, Braganza A, Abraham L, Samuel P, Lindsley K (2013) Anti-vascular endothelial growth factor for neovascular glaucoma. Cochrane Database Syst Rev 10:CD007920. doi:10.1002/14651858.CD007920.pub2
Payne AJ, Kaja S, Sabates NR, Koulen P (2013) A case for neuroprotection in ophthalmology: developments in translational research. Mo Med 110(5):429–436
Jessen BA, Shiue MH, Kaur H, Miller P, Leedle R, Guo H, Evans M (2013) Safety assessment of subconjunctivally implanted devices containing latanoprost in Dutch-belted rabbits. J Ocul Pharmacol Ther 29(6):574–585. doi:10.1089/jop.2012.0190
Foo RC, Lamoureux EL, Wong RC, Ho SW, Chiang PP, Rees G, Aung T, Wong TT (2012) Acceptance, attitudes, and beliefs of Singaporean Chinese toward an ocular implant for glaucoma drug delivery. Invest Ophthalmol Vis Sci 53(13):8240–8245. doi:10.1167/iovs.12-10393
Mealy JE, Fedorchak MV, Little SR (2014) In vitro characterization of a controlled-release ocular insert for delivery of brimonidine tartrate. Acta Biomater 10(1):87–93. doi:10.1016/j.actbio.2013.09.024
Macoul KL, Pavan-Langston D (1975) Pilocarpine ocusert system for sustained control of ocular hypertension. Arch Ophthalmol 93(8):587–590
Strohmaier K, Snyder E, Adamsons I (1998) A multicenter study comparing dorzolamide and pilocarpine as adjunctive therapy to timolol: patient preference and impact on daily life. J Am Optom Assoc 69(7):441–451
Kashiwagi K, Ito K, Haniuda H, Ohtsubo S, Takeoka S (2013) Development of latanoprost-loaded biodegradable nanosheet as a new drug delivery system for glaucoma. Invest Ophthalmol Vis Sci 54(8):5629–5637. doi:10.1167/iovs.12-9513
Gagandeep, Garg T, Malik B, Rath G, Goyal AK (2014) Development and characterization of nano-fiber patch for the treatment of glaucoma. Eur J Pharm Sci 53:10–16. doi:10.1016/j.ejps.2013.11.016
Saati S, Lo R, Li PY, Meng E, Varma R, Humayun MS (2010) Mini drug pump for ophthalmic use. Curr Eye Res 35(3):192–201. doi:10.3109/02713680903521936
Butler MR, Prospero Ponce CM, Weinstock YE, Orengo-Nania S, Chevez-Barrios P, Frankfort BJ (2013) Topical silver nanoparticles result in improved bleb function by increasing filtration and reducing fibrosis in a rabbit model of filtration surgery. Invest Ophthalmol Vis Sci 54(7):4982–4990. doi:10.1167/iovs.13-12047
Chen X, Zhu X, Li L, Xian G, Wang W, Ma D, Xie L (2013) Investigation on novel chitosan nanoparticle-aptamer complexes targeting TGF-beta receptor II. Int J Pharm 456(2):499–507. doi:10.1016/j.ijpharm.2013.08.028
Shao T, Li X, Ge J (2011) Target drug delivery system as a new scarring modulation after glaucoma filtration surgery. Diagn Pathol 6:64. doi:10.1186/1746-1596-6-64
Sabzevari A, Adibkia K, Hashemi H, De Geest BG, Mohsenzadeh N, Atyabi F, Ghahremani MH, Khoshayand MR, Dinarvand R (2013) Improved anti-inflammatory effects in rabbit eye model using biodegradable poly beta-amino ester nanoparticles of triamcinolone acetonide. Invest Ophthalmol Vis Sci 54(8):5520–5526. doi:10.1167/iovs.13-12296
Swaminathan S, Vavia PR, Trotta F, Cavalli R (2013) Nanosponges encapsulating dexamethasone for ocular delivery: formulation design, physicochemical characterization, safety and corneal permeability assessment. J Biomed Nanotechnol 9(6):998–1007
Guignier B, Bourahla K, Bekaert V, Brasse D, Gaucher D, Speeg-Schatz C, Bourcier T (2013) Scintigraphic study of the lymphatic drainage of the anterior chamber of the mouse eye and its pathophysiological implications. J Fr Ophtalmol 36(10):836–842. doi:10.1016/j.jfo.2012.11.021
Mansouri K, Weinreb RN (2012) Meeting an unmet need in glaucoma: continuous 24-h monitoring of intraocular pressure. Expert Rev Med Devices 9(3):225–231. doi:10.1586/erd.12.14
Agnifili L, Mastropasqua R, Frezzotti P, Fasanella V, Motolese I, Pedrotti E, Iorio AD, Mattei PA, Motolese E, Mastropasqua L (2014) Circadian intraocular pressure patterns in healthy subjects, primary open angle and normal tension glaucoma patients with a contact lens sensor. Acta Ophthalmol. doi:10.1111/aos.12408
Chitnis G, Maleki T, Samuels B, Cantor LB, Ziaie B (2013) A minimally invasive implantable wireless pressure sensor for continuous IOP monitoring. IEEE Trans Biomed Eng 60(1):250–256. doi:10.1109/TBME.2012.2205248
Ha D, de Vries WN, John SW, Irazoqui PP, Chappell WJ (2012) Polymer-based miniature flexible capacitive pressure sensor for intraocular pressure (IOP) monitoring inside a mouse eye. Biomed Microdevices 14(1):207–215. doi:10.1007/s10544-011-9598-3
Chen GZ, Chan IS, Leung LK, Lam DC (2014) Soft wearable contact lens sensor for continuous intraocular pressure monitoring. Med Eng Phys 36(9):1134–1139. doi:10.1016/j.medengphy.2014.06.005
Sanchez I, Laukhin V, Moya A, Martin R, Ussa F, Laukhina E, Guimera A, Villa R, Rovira C, Aguilo J, Veciana J, Pastor JC (2011) Prototype of a nanostructured sensing contact lens for noninvasive intraocular pressure monitoring. Invest Ophthalmol Vis Sci 52(11):8310–8315. doi:10.1167/iovs.10-7064
Araci IE, Su B, Quake SR, Mandel Y (2014) An implantable microfluidic device for self-monitoring of intraocular pressure. Nat Med. doi:10.1038/nm.3621
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Fedorchak, M.V. (2016). Barriers to Glaucoma Drug Delivery and Resolving the Challenges Using Nanotechnology. In: Pathak, Y., Sutariya, V., Hirani, A. (eds) Nano-Biomaterials For Ophthalmic Drug Delivery. Springer, Cham. https://doi.org/10.1007/978-3-319-29346-2_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-29346-2_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29344-8
Online ISBN: 978-3-319-29346-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)