Abstract
The availability of safe and effective endoscopic techniques has caused a major shift in the management of Barrett’s associated dysplasia and early cancer from primarily surgical to endoscopic therapy. Prior to contemplating endoscopic therapy, careful selection of patients is essential and best served by evaluation with multidisciplinary team at specialized centers. This requires detailed examination of Barrett’s segment with removal of nodules or suspicious areas with endoscopic mucosal resection and expert confirmation of dysplasia by at least two gastrointestinal pathologists. This should be followed by eradication of remaining Barrett’s segment with ablation and ongoing vigilant surveillance as recurrences have been reported. Endoscopic therapy is considered in Barrett’s associated intramucosal cancer, Barrett’s esophagus with high-grade dysplasia, confirmed cases of low-grade dysplasia, and rare instances of non-dysplastic Barrett’s such as those with long segment and family history as complete eradication of Barrett’s esophagus is associated with marked reduction in cancer risk. Palliative therapy with photodynamic therapy or cryotherapy can be considered in selected cases of inoperable cancer.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Ablation Catheter
- Intestinal Metaplasia
- Endoscopic Mucosal Resection
- Endoscopic Therapy
- Complete Eradication
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
4.1 Introduction
Since the recognition of Barrett’s esophagus as a precancerous condition, efforts have focused on its eradication. Aggressive acid suppression with medical or surgical anti-reflux therapy led to inconsistent results in regression of Barrett’s epithelium. It has been observed that Barrett’s can revert to normal squamous epithelium when it is ablated and maximal acid suppression is maintained. This has led to initial reports of ablation of non-dysplastic Barrett’s using endoscopic laser therapy [1]. Subsequent efforts were focused on endoscopic therapy in Barrett’s patients with high-grade dysplasia (HGD) who were poor surgical candidates as they are at highest risk of progression to cancer. Since then, ablative therapies have evolved and have become the mainstay of therapy for Barrett’s associated neoplasia.
Removal of dysplastic areas only without complete eradication of entire Barrett’s segment is associated with high risk of developing metachronous neoplasia [2]. Hence, the current standard of management for Barrett’s includes endoscopic mucosal resection (EMR) of visible abnormalities followed by ablation to eradicate remaining Barrett’s epithelium with ongoing surveillance. Although endoscopic therapy cannot cure neoplasms that have metastasized to regional lymph nodes, such nodal involvement is present in only 1–2 % of patients with intramucosal adenocarcinoma in Barrett’s esophagus and therefore is useful in selected cases of intramucosal cancers. Currently, endoscopic therapy is recommended in patients with HGD and intramucosal cancer and is considered in confirmed cases of low-grade dysplasia (LGD) as there is a higher risk of progression. In addition, there have been recent case series describing the use of endoscopic therapy in early submucosal cancers.
4.2 Ablative Techniques
The various available ablative therapies include radiofrequency ablation (RFA), photodynamic therapy (PDT), cryotherapy, argon plasma coagulation (APC), and multipolar electrocoagulation (MPEC). What are the criteria of an ideal ablation technique in Barrett’s esophagus? As described by Bergman et al. [3], firstly it should remove all dysplasia and intestinal metaplasia . Secondly, the neosquamous mucosa that develops after ablation should be free of oncogenetic abnormalities such as those present in the pretreatment metaplastic mucosa, and no residual areas of metaplastic columnar mucosa should remain hidden underneath it (“buried Barrett’s”). Thirdly, it should be very precisely targeted at the mucosa without damaging the deeper layers, thereby minimizing complications and preserving the normal functional characteristics of the esophagus. Finally, it should be quick and easy, removing all Barrett’s mucosa, preferentially in one procedure. No such ideal ablation technique exists, but RFA has demonstrated efficacy, durability, and safety in multiple clinical trials making it the preferred technique of ablation.
4.3 Radiofrequency Ablation
The most widely used ablation technique for Barrett’s dysplasia is RFA using HALO system first developed in 2000. Well designed, randomized controlled trials and subsequent experience have demonstrated its superior efficacy and safety profile in ablation of dysplastic Barrett’s. RFA is performed using the Barrx FLEX system (previously HALO FLEX system), which is comprised of two distinct types of ablation catheters: the circumferential ablation catheter or Barrx 360 for primary ablation and focal ablation catheters which include Barrx 90, Barrx 90 ULTRA, and Barrx 60 and through the scope Channel RFA device. The FLEX generator is used for both circumferential and focal RFA (Fig. 4.1).
4.3.1 Technique
Circumferential ablation : The Barrx 360 ablation catheter consists of a 165-cm-long shaft with a balloon at its distal end that contains a 3-cm-long bipolar electrode. The electrode array encircles the balloon through which radiofrequency energy is applied, ablating the Barrett’s mucosa. The ablation catheter is available in five outer diameters (18, 22, 25, 28, and 31 mm once inflated). After careful determination of landmarks and exam for visible abnormalities in the Barrett’s segment, the esophagus is cleaned by washing with 1 % acetylcysteine or water. Then, the diameter of esophageal lumen at different levels is assessed by passing a sizing catheter over a guidewire. Based on the size of lumen, a Barrx 360 catheter of appropriate size is selected and advanced over a guidewire. Under endoscopic visualization, the catheter is placed 1 cm above the most proximal extent of the BE and inflated after which radiofrequency energy is applied. Then, the catheter is moved distally and radiofrequency energy is delivered sequentially. Then, the ablation catheter is removed, and the coagulum is scraped off with a cap attached to the tip of the endoscope. Subsequently, a second series of ablation is performed. Recently, a 4-cm-long circumferential 360 Express RFA Balloon catheter is developed which bypasses the need for sizing. Eight to twelve weeks after the first circumferential ablation treatment, patients undergo additional therapy with either Barrx 360 or Barrx 90 depending on the extent of residual Barrett’s.
Focal ablation : Barrx 90 consists of 20 × 13-mm-sized electrode mounted on the tip of endoscope and placed at the 12 o’clock position in the endoscopic video image. Then, the endoscope is passed, and radiofrequency energy (at 12 J/cm2 in the United States and 15 J/cm2 in Europe) is applied twice after the endoscope is deflected and electrode is closely applied to the esophageal wall. Then, the coagulated tissue is scraped off with the catheter and ablation is repeated as described before. Simplified regimens without a cleaning phase in between have also been described. Barrx 90 Ultra has a larger surface area and has potential application in patients with dilated and tortuous esophagus when close opposition with Barrx 360 is not feasible. Barrx 60 and Channel catheter can be used in patients with esophageal strictures or tight upper esophageal sphincter.
After ablation, patients are on high-dose twice daily proton pump inhibitor therapy along with liquid sucralfate 4 times a day for 10–14 days. They stay on liquid diet for a day and advance to solid food as tolerated. Then, the procedure is repeated again in 2–3 months.
4.3.2 Efficacy
RFA is highly efficacious in eradication of metaplasia (71–93 %) and dysplasia (91–100 %). The most compelling evidence for the use of RFA in BE with dysplasia comes from AIM dysplasia trial [4], a US multicenter randomized sham-controlled trial of 127 patients. At 1-year follow-up, 81 % in HGD and 90 % in LGD had eradication of dysplasia. The effect seems to be durable with eradication of dysplasia persisting in more than 85 % of patients at the end of 3 years [5]. Another study demonstrating efficacy of RFA comes from SURF trial, a randomized controlled trial of 136 patients with confirmed LGD. At the end of 2 years, RFA reduced risk of progression to HGD or cancer (1.5 % in RFA group vs. 26.5 %, in surveillance arm p < 0.001) [6].
4.3.3 Complications
RFA is a safe procedure with few adverse events. The most commonly reported in order of decreasing frequency are strictures (5 %), chest pain (3 %), and bleeding (1 %).
4.4 Cryotherapy
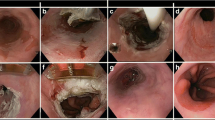
Cryotherapy is based on the principle of ablating Barrett’s tissue by application of a cryogen leading to extremely cold temperatures. Repeated cycles of rapid freezing followed by slow thawing lead to cell membrane rupture. Delayed injury includes tissue anoxia due to the loss of microcirculation and immune-related processes. There are two types of cryotherapy devices commercially available: one is cryospray (CSA Medical) which uses liquid nitrogen delivered at −196 C (Fig. 4.2), and the other is Polar Wand (GI supply) which utilizes carbon dioxide gas cooled to −78 C. A recently developed simplified through the scope focal cryoballoon system (C2 Therapeutics) is being studied for Barrett’s ablation. Since cryoablation does not require any contact, it is useful for patients with tortuous esophagus and nodular uneven mucosal surface.
4.4.1 Technique
Cryotherapy is performed by passing the catheter through the accessory channel of an endoscope, and the tip of the catheter is held 5–10 mm away from the target tissue. The foot pedal is depressed, which triggers the release of the cryogen. The cryogen is sprayed onto the target tissue until it turns white, which means that freezing has taken place. This generally occurs after 10–15 s of application. Thawing usually takes place within 10–30 s. The same area is typically subjected to the freezing–thawing cycle 3 or 4 times to achieve ablation. In cryospray system, a decompression tube is used to evacuate the excess gas from the stomach, whereas in Polar Wand system, suction catheter is attached to the tip of the endoscope.
4.4.2 Efficacy
The evidence of efficacy comes from retrospective studies. In a study of 60 Barrett’s patients with HGD who underwent cryospray therapy, 87 % had complete eradication of all dysplasia with persistent non-dysplastic intestinal metaplasia, and 57 % had complete eradication of all intestinal metaplasia during a mean follow-up of 10.5 months [7]. The effect seems to be durable as reported by a retrospective study of 32 patients with HGD with a mean follow-up of 37 months where HGD was eradicated in 97 % and eradication of intestinal metaplasia was observed in 81 % [8]. Recurrent HGD was found in 6 (18 %) which was treated by cryotherapy. In another study of 49 patients with esophageal cancer (46 with adenocarcinoma), complete response was seen in 75 % with intramucosal cancer during a mean follow-up of 10.6 months [9]. In a small study of 39 patients published in abstract form, cryotherapy with carbon dioxide was effective in complete eradication of dysplasia in 80.6 % and eradication of metaplasia in 42 % [10].
4.4.3 Complications
Cryotherapy is generally well tolerated, with few side effects and rare complications reported. Common side effects include chest pain (17.6 %), dysphagia (13.3 %), and odynophagia (12.1 %) [11]. One case of gastric perforation occurred in a patient with Marfan syndrome, and another patient developed a lip ulcer, as a result of cold injury from contact with the endoscope, which resolved in 4 days without specific treatment [12]. Esophageal stricture noted in 3–13 % of the patients that responded to balloon dilation therapy [8, 9].
4.5 Photodynamic Therapy (PDT)
PDT was one of the most widely studied ablative therapies used in the treatment of Barrett’s esophagus prior to advent of RFA. It was initially used for palliation of advanced esophageal cancer but subsequently found to be useful in management of patients with Barrett’s and HGD and early esophageal cancer who are poor surgical candidates.
4.5.1 Technique
Photodynamic therapy is based on the principle of cell destruction induced by photosensitizers when stimulated by light. In the United States, porfimer sodium (Photofrin, Pinnacle Biologics Inc) at a dose of 2 mg/kg of body weight is given as an intravenous bolus over 3–5 min. Two days later, visible red light at approximately 630 nm is transmitted by an optical fiber passed through accessory channel of endoscope or a balloon diffusing fiber. For treatment of Barrett’s with HGD, the light dose recommended is 130–200 J/cm fiber. A second endoscopy is performed 2–3 days later to repeat the treatment if necessary. In Europe, other photosensitizers such as 5-aminolevulinic acid (5-ALA) and m-tetrahydroxyphenyl chlorin (mTHPC) are also used. ALA can be administered orally, has shorter duration of skin photosensitivity (24–48 h), and reduced incidence of strictures.
4.5.2 Efficacy
PDT is the first ablation technique proven to be effective and durable in a randomized controlled trial. In this trial of 208 patients with HGD randomized to either porfimer sodium PDT plus omeprazole versus omeprazole alone, complete ablation of HGD was achieved in 77 % of PDT group compared with 39 % in the control group (p < .0001) on mean follow-up of 24 months [13]. Complete eradication of metaplasia was seen in 52 % of patients in the PDT group compared with 7 % in the omeprazole group (p < .0001). There was also a significant difference in progression to cancer, with 13 % of patients in the PDT group developing cancer compared with 28 % in the omeprazole group. Eradication of HGD at 5-year follow-up was achieved in 77 % of those treated with PDT plus omeprazole and 39 % of those treated with omeprazole alone. Progression to esophageal cancer at 5-year follow-up was 15 % in the PDT group and 29 % in the omeprazole-only arm [14]. PDT can also be used for eradication of Barrett’s after EMR of intramucosal cancer. In a study of 17 patients who underwent PDT following EMR, 94 % remained in remission at 13 months [15]. Comparative retrospective data of patients undergoing PDT vs. surgical esophagectomy for BE HGD at a high-volume expert center demonstrated comparable overall survival over 5 years of median follow-up (83 % in patients treated with EMR only or EMR followed by PDT versus 95 % IN patients who underwent esophagectomy for intramucosal cancer [16]. These data established porfimer sodium PDT as a viable alternative to esophagectomy, particularly among individuals – whether due to advanced age, comorbid illness, or preference against surgical esophagectomy.
4.5.3 Complications
The most common adverse events reported with porfimer sodium use were photosensitivity reactions (69 %), esophageal strictures (36 %), vomiting (32 %), noncardiac chest pain (20 %), pyrexia (20 %), and dysphagia (19 %) [13]. 5-aminolevulinic acid has less frequent side effects but not widely used in the United States.
4.6 Argon Plasma Coagulation (APC)
APC is a noncontact technique wherein ionized argon gas is delivered at energy settings of 40–90 W to ablate Barrett’s. It was used for eradication of non-dysplastic Barrett’s and LGD but incomplete eradication is common. Buried glands were reported in up to 40 % of patients [17]. APC was also described in ablation of Barrett’s with HGD. In a study of 32 patients with HGD, 78 % had eradication of HGD and 69 % had eradication of Barrett’s. However, there was 13 % progression to EAC in a mean follow-up period of 34 months [18]. Another potential role is in palliative treatment of advanced cancer causing dysphagia or bleeding [19]. Complications include strictures, fever, bleeding, and, rarely, perforation.
4.7 MPEC
Ablation of Barrett’s using multipolar electrocoagulation (MPEC) is a fairly simple technique. A 10 French MPEC probe is passed through a therapeutic endoscope, and thermal energy is applied at 15–20 W setting till a white coagulum appears. Treatment is continued in a circumferential fashion at intervals of few weeks till entire Barrett’s is ablated. It has been mainly studied in non-dysplastic Barrett’s [20], few cases of LGD [21], and a small case series of intramucosal cancer in combination with laser [22]. Eradication rate is about 78 % with subsquamous intestinal metaplasia (SSIM) observed in about 5–27 % [20, 21]. Since it is time-consuming to treat large areas of Barrett’s with this technique, it is best reserved for treating small areas of residual Barrett’s after prior ablative therapy with different technique.
4.8 Endoscopic Therapy Versus Esophagectomy
The traditional treatment for Barrett’s with HGD and intramucosal cancer had been esophagectomy. The advantage of esophagectomy is that it not only removes the neoplasia but also the at-risk mucosa thereby eliminating the risk of recurrence and also the periesophageal lymph nodes to allow accurate staging. However, it is associated with high rate of morbidity in a range of 30–50 % and a small but definite risk of mortality in even high-volume centers. There are no randomized controlled trials comparing endoscopic therapy to esophagectomy, but a number of studies show comparable long-term outcomes and much fewer complications with added advantage of preserving the esophagus. A recently published meta-analysis of 870 patients with early esophageal neoplasia [23] showed that there was no significant difference between endotherapy and esophagectomy in the neoplasia remission rate (relative risk [RR], 0.96; 95 % CI, 0.91–1.01). The remission rate varied from 97 to 100 % in patients with esophagectomy and 84 to 97 % in patients with endoscopic treatment. In addition, there was no difference in overall survival rate at 5 years (RR 1.00). The cumulative death rate was 11.4 % in the endotherapy group and 8.7 % in the surgery group during follow-up. Most patients died of baseline comorbidities including cardiovascular disease, pulmonary disease, diabetes, and prior malignancy. The neoplasia-related mortality was 0.2 % in the endotherapy group and 0.3 % in the surgery group. Patients undergoing endotherapy had a higher neoplasia recurrence rate (RR 9.50) and fewer major adverse events (RR 0.38). Most patients (77.8–100 %) with neoplasia recurrence underwent endoscopic retreatment and got neoplasia remission again or had stable disease.
4.9 Postablation Surveillance
There are two issues which need to be taken into consideration after successful eradication of Barrett’s which make postablation surveillance mandatory: first is the subsquamous intestinal metaplasia (SSIM or buried Barrett’s ), and second is the postablation recurrences after successful eradication of Barrett’s.
4.10 Subsquamous Intestinal Metaplasia (SSIM)
SSIM or “buried Barrett’s ” is the presence of intestinal metaplasia in the lamina propria beneath overlying squamous mucosa. This is not visible by endoscopic inspection and is detected either by histological sampling or enhanced imaging techniques. Theoretically, SSIM may have a lower neoplastic potential due to lack of exposure to gastric acid and bile, but there are numerous reports of HGD or cancer developing from SSIM [24]. SSIM is known to exist both prior to and after ablation. The origins are uncertain but thought to be from neosquamous overgrowth over intestinal metaplasia in biopsy sites or as a consequence of ablation. The reported prevalence of SSIM varies from 0 to 28 % [25], but this may not be a true estimate as most of the endoscopic biopsies are not adequate to include subepithelial lamina propria [26]. Studies on SSIM in EMR specimens reported a prevalence of 28–98 % prior to any ablation therapy [27, 28]. The effect of ablation on prevalence of SSIM is not clear but may decrease following RFA. A recent systematic review on SSIM after endoscopic ablation procedures found SSIM in 14.2 % of patients treated with PDT and in 0.9 % of patients after RFA [29]. In view of this uncertainty, patients need to stay in surveillance program even after complete eradication of surface metaplasia.
4.11 Recurrences and Predictors of Recurrence
Recurrences are common and range from 20 to 33 % in up to a 3-year follow-up period. In a multicenter consortium of 448 patients who underwent RFA, 56 % had complete remission of which 33 % had disease recurrence within the next 2 years [29]. Most recurrences were non-dysplastic and endoscopically manageable, but continued surveillance after RFA is essential. Among 5521 patients in the US RFA registry [30], 85 % achieved complete eradication of intestinal metaplasia. In a mean follow-up of 2.4 years after complete eradication, metaplasia recurred 20 % and was non-dysplastic or indefinite for dysplasia in 86 % of patients. In Kaplan–Meier analysis, more advanced pretreatment histology was associated with an increased yearly recurrence rate. Compared with patients without recurrence, patients with recurrence were more likely to be older, have longer BE segments, be non-Caucasian, have dysplastic Barrett’s before treatment, and require more treatment sessions. The treatment strategy for recurrent dysplasia is similar to primary dysplasia. EMR is performed for any visible abnormalities for treatment and staging purposes followed by ablative therapy for recurrent flat areas. If resistant to one modality, switching to a different mucosal ablation technique should be considered.
4.12 Follow-Up Intervals
Continued endoscopic surveillance following endotherapy is recommended, with intervals guided by prior grade of dysplasia and response to treatment. Currently, there is no consensus on the frequency of surveillance or biopsy protocol in postablation patients. As per recently published British guidelines [31], in patients treated for HGD, endoscopic follow-up is recommended every 3 months for 1 year and yearly thereafter. This should include biopsies at the cardia and within the previous extent of the Barrett’s epithelium. For patients with LGD, annual surveillance is recommended.
4.13 Patient Selection and Technical Considerations
Patients referred for endoscopic therapy should have a detailed white light exam with a high-definition endoscope to identify landmarks and any visible abnormalities. Four quadrant surveillance biopsies should be performed every 1 cm along with endoscopic resection of suspicious areas. Diagnoses of dysplasia need to be confirmed by an expert gastrointestinal pathologist. In cases of HGD and intramucosal cancer with low risk of lymph node metastases such as lesion size less than 2 cm, well-differentiated histology, and absence of lymphovascular invasion, endoscopic therapy is preferred over esophagectomy. After EMR of visible lesions, residual Barrett’s needs to be ablated in view of high risk of metachronous neoplasia. In the absence of visible lesions, ablative therapy is the treatment of choice. In view of risk of recurrence, patients need to be on ongoing surveillance with treatment of recurrences endoscopically.
Due to the lack of head-to-head randomized controlled trials comparing different ablative therapies, no one ablation modality suits all patients. A comparison of different ablation techniques is presented in Table 4.1. In patients with long-segment Barrett’s where large surface areas need to be treated, RFA is the treatment modality of choice. Other options include PDT and cryotherapy. For small areas of residual Barrett’s, APC and MPEC may be cost-effective modalities. For patients with nodular disease where close apposition with RFA is not possible, options are cryotherapy, PDT, and stepwise radical EMR. In patients with persistent areas of Barrett’s in spite of repeated ablation, EMR can be used.
References
Berenson MM, Johnson TD, Markowitz NR et al (1993) Restoration of squamous mucosa after ablation of Barrett’s esophageal epithelium. Gastroenterology 104:1686–1691
Pech O, Behrens A, May A et al (2008) Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett’s oesophagus. Gut 57:1200–1206
Bergman JJGHM, Fockens P (2006) Ablating Barrett’s metaplastic epithelium: are the techniques ready for clinical use? Gut 55(9):1222–1223
Shaheen NJ, Sharma P, Overholt BF et al (2009) Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med 360:2277–2288
Shaheen NJ, Overholt BF, Sampliner RE et al (2011) Durability of radiofrequency ablation in Barrett’s esophagus with dysplasia. Gastroenterology 141:460–468
Phoa KN, van Vilsteren FGI, Weusten LAM et al (2014) Radiofrequency ablation vs endoscopic surveillance for patients with Barrett Esophagus and low-grade dysplasia. A randomized clinical trial. JAMA 311(12):1209–1217
Shaheen NJ, Greenwald BD, Peery AF et al (2010) Safety and efficacy of endoscopic spray cryotherapy for Barrett’s esophagus with high-grade dysplasia. Gastrointest Endosc 71:680–685
Gosain S, Mercer K, Twaddell WS et al (2013) Liquid nitrogen spray cryotherapy in Barrett’s esophagus with high-grade dysplasia: long-term results. Gastrointest Endosc 78(2):260–265
Greenwald BD, Dumot JA, Abrams JA et al (2010) Endoscopic spray cryotherapy for esophageal cancer: safety and efficacy. Gastrointest Endosc 71(4):686–693
Canto MI, Gorospe EC, Shin EJ et al (2009) Carbon dioxide (CO2) Cryotherapy is a safe and effective treatment of Barrett’s Esophagus (BE) with HGD/Intramucosal Carcinoma. Gastrointest Endosc 69:AB341
Greenwald BD, Dumot JA, Horwhat D, Lightdale CJ, Abrams JA (2010) Safety, tolerability, and efficacy of endoscopic low-pressure liquid nitrogen spray cryotherapy in the esophagus. Dis Esophagus 23:13–19
Dumot JA, Vargo JJ, Falk GW et al (2009) An open-label, prospective trial of cryospray ablation for Barrett’s esophagus high-grade dysplasia and early esophageal cancer in high-risk patients. Gastrointest Endosc 70:635–644
Overholt BF, Lightdale CJ, Wang KK et al (2005) Photodynamic therapy with porfimer sodium for ablation of high-grade dysplasia in Barrett’s esophagus: international, partially blinded, randomized phase III trial. Gastrointest Endosc 62(4):488–498
Overholt BF, Wang KK, Burdick JS et al (2007) Five-year efficacy and safety of photodynamic therapy with Photofrin in Barrett’s high-grade dysplasia. Gastrointest Endosc 66(3):460–468
Pacifico RJ, Wang KK, Wongkeesong LM et al (2003) Combined endoscopic mucosal resection and photodynamic therapy versus esophagectomy for management of early adenocarcinoma in Barrett’s esophagus. Clin Gastroenterol Hepatol 1:252–257
Prasad GA, Wu TT, Wigle DA et al (2009) Endoscopic and surgical treatment of mucosal (T1a) esophageal adenocarcinoma in Barrett’s esophagus. Gastroenterology 137:815–823
Grade AJ, Shah IA, Medlin SM et al (1999) The efficacy and safety of argon plasma coagulation therapy in Barrett’s esophagus. Gastrointest Endosc 50:18–22
Lewis CJ, Caplin S, Armstrong G et al (2003) Argon Beam Plasma Coagulation as an ablative therapy for high grade dysplasia in Barrett’s Oesophagus. Clin Gastroenterol Hepatol 1(4):258–263
Akhtar K, Byrne JP, Bancewicz J et al (2000) Argon Beam Plasma Coagulation in the management of cancers of the esophagus and stomach. Surg Endoscopy 14:1127–1130
Sampliner RE, Faigel D, Fennerty MB et al (2001) Effective and safe endoscopic reversal of nondysplastic Barrett’s esophagus with thermal electrocoagulation combined with high dose acid suppression: a multicenter study. Gastrointest Endosc 53:554–558
Sharma P, Bhattacharyya A, Garewal HS et al (1999) Durability of new squamous epithelium after endoscopic reversal of Barrett’s Esophagus. Gastrointest Endosc 50:159–164
Sharma P, Jaffe PE, Bhattacharyya A et al (1999) Laser and multipolar electrocoagulation ablation of early Barrett’s adenocarcinoma. Gastrointest Endosc 49:442–446
Wu J, Pan Y, Wang T et al (2014) Endotherapy versus surgery for early neoplasia in Barrett’s esophagus: a meta-analysis. Gastrointest Endosc 79(2):233–241
Titi M, Overhiser A, Ulusarac O et al (2012) Development of subsquamous high-grade dysplasia and adenocarcinoma after successful radiofrequency ablation of Barrett’s esophagus. Gastroenterology 143:564–566
Gray NA, Odze RD, Spechler SJ (2011) Buried metaplasia after endoscopic ablation of Barrett’s esophagus: a systematic review. Am J Gastroenterol 106:1899–1908
Gupta N, Mathur SC, Dumot JA et al (2012) Adequacy of esophageal squamous mucosa specimens obtained during endoscopy: are standard biopsies sufficient for postablation surveillance in Barrett’s esophagus? Gastrointest Endosc 75:11–18
Anders M, Lucks Y, El-Masry MA et al (2014) Subsquamous extension of intestinal metaplasia is detected in 98% of cases of neoplastic Barrett’s esophagus [published online July 23, 2013]. Clin Gastroenterol Hepatol 12(3):405–410. doi:http://dx.doi.org/10.1016/j.cgh.2013.07.013
Chennat J, Ross AS, Konda VJ et al (2009) Advanced pathology under squamous epithelium on initial EMR specimens in patients with Barrett’s esophagus and high-grade dysplasia or intramucosal carcinoma: implications for surveillance and endotherapy management. Gastrointest Endosc 70:417–421
Gupta M, Iyer PG, Lutzke L et al (2013) Recurrence of esophageal intestinal metaplasia after endoscopic mucosal resection and radiofrequency ablation of Barrett’s esophagus: results from a US Multicenter Consortium. Gastroenterology 145:79–86
Pasricha S, Bulsiewicz WJ, Hathorn K et al (2014) Durability and predictors of successful radiofrequency ablation for Barrett’s Esophagus. Clin Gastroenterol Hepatol 12(11):1840–1847
Fitzgerald RC, di Pietro M, Ragunath K et al (2014) British Society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut 63:7–42
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Thota, P.N. (2017). Ablation Techniques for Barrett’s Esophagus and Dysplasia. In: Giacopuzzi, S., Zanoni, A., de Manzoni, G. (eds) Adenocarcinoma of the Esophagogastric Junction. Springer, Cham. https://doi.org/10.1007/978-3-319-28776-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-28776-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28774-4
Online ISBN: 978-3-319-28776-8
eBook Packages: MedicineMedicine (R0)