Abstract
Fatal outcomes after hospital treatment are of particular interest for clarification of their causes, particularly when they occur unexpectedly or following surgery or intervention. Postmortem imaging methods offer an excellent opportunity for confirming clinical findings or supplementing them, which can be understood as a part of clinical quality assurance process. An accusation regarding medical malpractice can be clarified by a legal autopsy, which should be complemented by postmortem angiography when acute injuries from punctures or catheter systems are a concern. The malposition of a medical device such as an indwelling catheter, a drainage catheter, or a respiratory tube in native postmortem computed tomography (PMCT) can serve as an indication for multiphase PMCT angiography. A particular strength of postmortem angiography is the detection of hemorrhage sources caused by complications under catheter-based cardiovascular interventions. Hemorrhage complications are demonstrated in cases of cardiac catheterizations and after endovascular aortic stenting for the treatment of aneurysms and dissections. Complications from punctures often are associated with emergencies, as shown by intracardiac malposition of catheters for pericardiocentesis, which may intensify an existing tamponade or even cause one, thus contributing to the death of a patient.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Fatal outcomes after hospital treatment are of particular interest for clarification of their causes, particularly when they occur unexpectedly or following surgery or intervention. Postmortem imaging methods offer an excellent opportunity for confirming clinical findings or supplementing them, which can be understood as a part of clinical quality assurance process. An accusation regarding medical malpractice can be clarified by a legal autopsy, which should be complemented by postmortem angiography when acute injuries from punctures or catheter systems are a concern. The malposition of a medical device such as an indwelling catheter, a drainage catheter, or a respiratory tube in native postmortem computed tomography (PMCT) can serve as an indication for multiphase PMCT angiography. A particular strength of postmortem angiography is the detection of hemorrhage sources caused by complications under catheter-based cardiovascular interventions. Hemorrhage complications are demonstrated in cases of cardiac catheterizations and after endovascular aortic stenting for the treatment of aneurysms and dissections. Complications from punctures often are associated with emergencies, as shown by intracardiac malposition of catheters for pericardiocentesis, which may intensify an existing tamponade or even cause one, thus contributing to the death of a patient.
1 Punctures and Catheters
Catheters are inserted into the body to treat diseases or perform a surgical procedure. They are in widespread and increasing use in different fields such as cardiovascular, gastrointestinal, urologic, and neurovascular applications.
Catheters can be inserted into a body cavity, duct, or arterial or venous vessel. They allow drainage of wound cavities, administration of fluids, and access by surgical instruments. Depending on the type of catheter, a wide variety of potential further tasks is possible. Indwelling catheters may be left in the body, either temporarily or permanently. Many of them are detected postmortem if they have not been removed before transport to the morgue.
Vascular catheters can be in malposition, about which PMCT furnishes hints, but multiphase PMCT angiography (MPMCTA) supports the definitive diagnosis because of distinct differentiation of intra- and extravascular spaces. It should be kept in mind that preceding vascular punctures may have failed even if a catheter is in a standard position at the time of death.
Successful punctures and unsuccessful and abortive punctures of arteries and veins may induce a vascular occlusion or bleeding (Fig. 24.1). Therefore, when performing MPMCTA, it is advisable to be informed about the results of the external postmortem examination of the body. The radiologist should focus on the sites usually used for vascular punctures; these are the groin (femoral vein and artery), neck (jugular vein), upper chest (subclavian and axillary vein and artery), elbow (cubital vein and brachial artery), and proximal tibia (bone marrow). This approach is especially important when information is lacking about whether a vascular puncture has occurred and which vessel was punctured.
A vascular catheter can sometimes be observed in an anomalous position in postmortem imaging in cases of hospital-related fatalities; it may kink, loop, and perforate [1, 2]. This possibility applies equally to electrodes that are placed for permanent use as part of pacemakers or implantable cardioverter defibrillators or as transient stimulation catheters during complicated heart surgery. They can cause local complications and also fail to stimulate: A pacemaker electrode in an aberrant position does not regulate the cardiac rhythm (Fig. 24.2), which may contribute to the death of a patient.
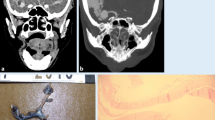
The heart demands special attention: Malposition and perforation of a pericardiocentesis catheter can explain a fatal outcome [3]. The visualization of the pathology demands different reconstructions. In general, it is advisable that PMCT precede MPMCTA and that reconstructions follow the vessels, catheters, and—if applicable—the path of contrast agent extravasation. Figures 24.3 and 24.4 demonstrate two cases with penetration of catheters for pericardiocentesis into the right ventricle and pulmonary artery, but MPMCTA demonstrates hemopericardium caused by this malposition in only one of the cases.
In the abdomen and chest, punctures for drainage (pleural and peritoneal effusions) and diagnosis (parenchymal organs, lymph nodes, and space-occupying lesions) may cause bleeding. A suprapubic puncture for a urinary catheter can result in paravesical hemorrhage [4]. MPMCTA can show the bleeding vessel (Fig. 24.5) or malformations such as vesicoarterial or arterial-enteric fistulas [5].
The criteria for assessing or proving a hemorrhage of antemortem origin are space-occupying masses with an opacity typical for blood in PMCT and contrast agent extravasation in MPMCTA. This contrast agent extravasation must have contact with the suspected blood visualized in PMCT. It is essential to be informed about the clinical records and postmortem external body inspection. If this information is not available, a visible pathologic examination at least suggests medical interventions, for example, an antemortem puncture in cases of major pleural effusions.
MPMCTA, dynamic phase, three-dimensional reconstruction. Complications (bleeding, thrombosis, and vascular occlusion) of vascular punctures. Left groin, antemortem puncture: contrast agent extravasation (arrows). The femoral vein is occluded below the inguinal ligament. The site of the occlusion corresponds to the entrance of a venous catheter. This catheter is not radiopaque but shows contrasting markers (C). In addition to the external iliac artery (35), the external iliac vein shows a perfusion defect (TH). Note that this defect does not correspond to a thrombus in this case but rather to an intravascular gas bubble, persisting across different phases of MPMCTA. Superficial femoral artery (L1)
Anomalous position of a cardiac stimulation catheter, inserted from the right jugular vein in an intraoperative emergency during failing liver transplantation surgery. The electrode ends in a vein of the mediastinum. (a) (PMCT, three-dimensional reconstruction) and (b) (MPMCTA, venous phase, MIP display): The electrode forms a loop in the cardiac right ventricle and ends in a small vein (internal thoracic vein), which is a tributary of the left brachiocephalic vein (DD perforation). Visible are a tracheal tube and a central venous catheter ending in the superior vena cava (40). (c) (MPMCTA, venous phase, three-dimensional reconstruction), and (d) (detail): The electrode tip is stuck in the proximal part of the left internal thoracic vein, which has been deformed and kinked. Right atrium (RA), right ventricle (RV), left ventricle (LV), left brachiocephalic vein (42), ascending aorta (1), superior vena cava (40), left brachiocephalic vein (42)
Malposition of a draining catheter and perforation causing pericardial tamponade in a case of myocardial infarction: A pigtail catheter for drainage of a pericardial effusion was inserted beneath the sternum into the pericardium, perforating the myocardium of the right ventricle (RV), passing through the pulmonary valve into the pulmonary artery (60). (a) PMCT, lateral view. Pericardial effusion and pigtail catheter. Right ventricle (RV), pulmonary artery (60). (b) MPMCTA, arterial phase, three-dimensional reconstruction, lateral left-side view. Pigtail catheter anterior to the left ventricle and lateral to the ascending aorta. The pigtail catheter surpasses the upper end of the pericardium. It cannot end in the pericardium; therefore, malposition and perforation seem likely. Left ventricle (LV), ascending aorta (1), aortic arch (2), thoracic aorta (3), internal thoracic artery (23). (c) MPMCTA, venous phase, MIP, lateral right-side view. Pigtail catheter in the pulmonary artery. The pigtail catheter is introduced into the pericardium below the sternum, perforates the anterior wall of the heart (myocardium of the right ventricle [RV]), passes the valve of the pulmonary artery, and ends in the pulmonary artery (60). Contrast agent extravasation (arrows) is seen out of the right ventricle into the pericardium and from the pericardium into the mediastinum. The contrast extravasation occurs where the pigtail catheter penetrates. This sign suggests that the perforation has contributed to the hematopericardium. Left ventricle (LV), right ventricle (RV), left atrium (LA), aortic arch (2), thoracic aorta (3), pulmonary artery (60)
In this case, the same malposition of a draining catheter as in Fig. 24.3 did not cause the pericardial tamponade: hemopericardium occurred following rupture of the left anterior descending artery (LAD) during coronary angioplasty. A stent (arrows) was placed for closing the rupture. A pigtail catheter (for drainage of the pericardial blood) can be seen perforating the myocardium of the right ventricle and ending in the pulmonary artery. Right ventricle (RV), superior caval vein (40). (a) MPMCTA, dynamic phase, thick slab mean intensity reconstruction. Visualization of the heart with contrast agent, the aorta (1), and the superior vena cava (40). The pigtail catheter placed for drainage passes through the RV via the pulmonary valve into the pulmonary artery (60). No contrast agent is seen in the pericardium. (b) Reconstruction along the LAD. MPMCTA venous phase, maximum intensity projection (MIP). Left anterior descending coronary artery (LAD) with stent (arrows); no contrast agent extravasation is seen, despite rupture of the LAD in coronary angioplasty before death, leading to pericardial tamponade. (c) Curved view. MPMCTA venous phase, MIP. LAD with stent (arrows). No contrast agent extravasation. (d) Autopsy. Hemopericardium after dissection of the pericardium. Note the pigtail catheter and the coagulated blood layer on the epicardium, which may impede contrast extravasation. (e) Autopsy. Subepicardial hemorrhage adjacent to the LAD causing hemopericardium in this case. (f) Autopsy. Pigtail catheter penetrating the wall of the RV. Note that this region shows no subepicardial hemorrhage
Transcatheter aortic valve implantation via minithoracotomy (TAVI), initially complicated by hemorrhage from the access point at the apex cordis, then stabilized by mattress sutures in an emergency operation. Death caused by hemorrhagic shock and coagulation disorder. Left-sided hematothorax with suspected dehiscence at the sutured apex cordis at autopsy. However, MPMCTA revealed bleeding from the left phrenic artery (26) following puncture of a pleural effusion. (a) PMCT. Axial reconstruction. Hyperdense effusion (arrows) with density of blood and layering in the dorsal part of the left chest cavity. (b, c) MPMCTA, arterial phase. Reconstruction following the left phrenic artery, MIP. Contrast agent extravasation (arrows) into the left side of the chest out of two terminal branches of the left phrenic artery (26). The blood in the left thoracic cavity displaces the diaphragm downward. Note the phrenic artery (26) on the right showing the diaphragm in the normal position. On the left, the pulmonary vessels are distanced from the chest wall by the effusion. Beneath the diaphragm: coeliac trunk, common hepatic artery (11), splenic artery (12), superior mesenteric artery (14), proper hepatic artery (72), and the renal artery (16). Note left atrium and left ventricle without leakage of contrast material
2 Cardiac Catheterization
Cardiac catheterization is performed for different procedures, such as percutaneous transluminal coronary angioplasty (PTCA) and stenting, transcatheter aortic valve implantation (TAVI), mitral clipping and annuloplasty of the mitral valve, balloon interventions for valve dilatations, electrophysiology studies, or catheter ablation.
Procedures can be diagnostic or therapeutic. Coronary angiography is a diagnostic left-sided heart catheterization procedure that allows the interventional cardiologist to visualize the coronary vessels and insert mechanical stents to increase blood flow in stenosed or occluded vessels if the blockade is not better suited for coronary artery bypass surgery. Another diagnostic procedure includes the evaluation of pressure differences across the major heart valves or the estimation of the cardiac blood volume output. The range of potential complications refers to heart attacks, arrhythmias, stroke, allergic reactions to dye or medication, and infection [6]. Postmortem angiography is particularly apt for demonstrating cardiovascular injuries such as damage to the artery where the catheter was inserted (pseudoaneurysm) [7, 8], kidney damage, tearing aortic and cardiac tissue or coronary arteries [9], and coronary blood clotting. Coronary vessel perforations (see Fig. 24.4) may occur (1) during insertion of the thin, flexible wires into either the femoral artery or the radial artery followed by threading it toward the heart and into the coronary ostia and into the coronary arteries, or (2) after guidance of a catheter over the wire and performance of balloon or stent dilatations (see Fig. 24.4). MPMCTA and other PMCT angiography techniques [10, 11] demonstrate not only the extravasation of contrast medium but also the flow through the vessel [12]. Sometimes, a dissection of the wall during catheter manipulation of a spontaneous coagulation may have obliterated the vessel during the intervention. This effect can be confirmed by MPMCTA, which can demonstrate the extent of the blockade. Erroneous inferences resulting from an impaired postmortem contrast flow through the vessel for technical reasons should be excluded by autopsy.
For right-sided heart catheterization, the heart is accessed via the femoral or jugular vein. The determination of the cardiac output is possible by releasing a small amount of normal saline into one area of the heart and measuring temperature changes over time in another area. Catheter ablation via transseptic access to the left atrium is another indication. Right-sided heart catheterization may result in complications from aberrant catheter tips that end up in or perforate small mediastinal veins (see Fig. 24.2). The postmortem contrast distribution in accordance with the final position of catheter devices can point to inferences about the mechanism of a complication.
After cardiovascular intervention with catheters, MPMCTA aids in visualizing the procedure, complications, underlying disease, and accidental findings.
Dilating the coronary artery in PTCA and placing a stent can be complicated by rupture of the coronary artery. PMCT shows the blood in the pericardium, mediastinum, and pleural space. In singular cases, the contrast agent injected during the antemortem procedure is visible (Fig. 24.6a–c). MPMCTA confirms the localization of the rupture of the coronary artery, which is sometimes less precisely described by autopsy.
After TAVI, PMCT shows the position of the replaced aortic valve. MPMCTA aids in visualization of potential valvular insufficiency or the obliteration of the coronary ostia by the covered skirt of the self-expandable prosthesis (Fig. 24.7a–c), with the replaced valve deforming the anterior cusp of the mitral valve by dislocating the chordae tendineae (Fig. 24.7c). MPMCTA shows intracardiac shunts (Fig. 24.8) and ruptures of the aorta into the pericardium, the mediastinum, and/or the pleural space caused by dilation during implantation [1, 13]. Furthermore, peripheral arteries may be injured from the passage of the catheter or from the puncture for insertion of a sheath, which can lead to complications after application of arteriotomy closure systems [14, 15]. Periprocedural anticoagulation is a major risk factor [9].
Mitral valve clipping is a method for repairing mitral valve regurgitation [16]. A catheter with the open device is introduced into the right atrium via the venous system. The catheter is introduced into the left atrium by a transseptal puncture and then via the mitral valves into the left ventricle. The open device grabs the two mitral leaflets and fixes them together. Thus, the movement of the leaflets is reduced, and the regurgitation of the mitral valve diminishes or disappears. MPMCTA shows the connection through the atrial septum, the position of the mitral clip, and the leaflets/cusps of the mitral valve (Fig. 24.9a, b).
Transcatheter mitral valve annuloplasty is another approach to repairing mitral valve regurgitation [17]. Several modifications are possible, depending on whether they target the leaflets, annulus, chordae tendineae (percutaneous chordal implantation), or left ventricle (percutaneous left ventricle modeling).
Perforation of the LAD following PTCA with 18 bar prestent balloon dilatation with subsequent placement of covered emergency stents. During resuscitation trials, cardiologists reported no indication for pericardial tamponade in echocardiography. (a) PMCT, axial reconstruction. Pericardial tamponade caused by contrast agent injected into the LAD during PTCA. Contrast agent injected during PTCA forms a hyperdense layer topping the less dense blood level (arrows). Localization of the subepicardial leakage is visible (dashed circle). (b) MPMCTA, dynamic phase, axial reconstruction. The trail of the contrast agent leakage has become enhanced (dashed circle); the hemopericardium volume has increased. (c) Autopsy demonstrates leakage area in the proximal LAD (blue arrows) and epicardial perforation at two sites (dashed arrow: leakage site at damaged LAD; continuous arrow: epicardial perforation)
Implanted aortic valve with potential covering of the ostia of the coronary arteries. There are two overlapping aortic valve replacements, implanted with a catheter after dilatation of the aortic valve (TAVI). Contrast agent between the inner surface of the aorta and the implanted aortic valves (arrows) indicates leakage. (a) MPMCTA, arterial phase, axial reconstruction. MIP. (b) Three-dimensional reconstruction. The perfusion of the coronary ostia seems to be unimpeded. (c) Frontal reconstruction. In the left ventricle (LV), the lower rim of the implanted valve impairs the chordae tendineae (arrows); therefore mitral valve insufficiency induced by the TAVI procedure should be considered. The passage of the contrast agent from the left ventricle into the left atrium (LA) strengthens this suggestion
Mitral valve clip (MC). Replaced aortic valve (AV). The passage of the contrast agent above and below the MC is visible, as is the connection between the left atrium (LA) and the right atrium (RA) resulting from the puncture and the passage of the catheter when inserting the MC (arrows). Left ventricle, LV. Pacemaker and central venous catheters. MPMCTA, arterial phase. (a) Frontal view. Thick slab mean reconstruction. (b) Frontal view, MIP
3 Endovascular Aortic Repair (EVAR)
EVAR was introduced to treat aortic aneurysm, but it has attracted interest as an emergency intervention for aortic dissections [18]. When used to treat aneurysms of the thoracic aorta, the procedure is designated as thoracic endovascular aortic/aneurysm repair (TEVAR). One or several expandable, coated stents is placed in the aortic lumen with a catheter-based approach. The aim is to induce aortic remodeling by stabilizing the aortic wall or to reopen a true aortic lumen after a dissection, causing a thrombosis in the false lumen. For maintenance of the cervical and visceral perfusions, tailor-made stents with holes (via fenestration) and branches (via hoses) are available. Hybrid procedures combine one or several surgical bypasses with EVAR or TEVAR: The endograft is positioned over major aortic branches after surgical bypasses have safeguarded their perfusion [19, 20].
PMCT shows the stents and the underlying disease (aortic aneurysm and its rupture) as well as complications of the procedure and attempts to handle them (Fig. 24.10). Complications refer either to the integrity of the stent (stent migration, stenosis, or angulation) or to endoleaks [21]. Endoleaks may expose the aneurysm to dangerous pressure again or to side effects of the passage of the catheter carrying the stent (hematoma near the femoral artery, iliac artery, and aorta, particularly the aortic arch) [22]. MPMCTA helps to localize vascular injuries and visualize an unimpaired or a deficient perfusion of the branches of the aortic arch, the thoracic and abdominal aorta, and the iliac arteries. Its capacity includes visualization of nonradiopaque bypasses and demonstration of perfusion of the organs in question (Fig. 24.11) [1].
To sum up, MPMCTA serves as an indispensable standard for the detection of cardiovascular hemorrhage sources after complicated nonsurgical clinical interventions with a fatal outcome when a bleeding probably still occurred at the time of death.
EVAR 18 months before death caused by abdominal aneurysm with subsequent paraplegia caused by spinal hemorrhage and fatal pneumonia; stents in the aortic arch, descending thoracic aorta, abdominal aorta, and common iliac arteries. Suture in the ascending aorta (arrows) owing to replacement of the aortic valve by a biovalve together with a prosthetic replacement of the ascending aorta, debranching of the supra-aortic arteries, and reimplantation; no fenestration is visible in the stent in the aortic arch. (a) PMCT, three-dimensional reconstruction of the thoracic and abdominal aorta. (b) Three-dimensional reconstruction of fenestrated endograft in the abdominal aorta, with endografts/stents to both renal arteries, the coeliac artery, and the superior mesenteric artery. Two stents overlap above the level of aortic bifurcation. Stents have been inserted into the common iliac arteries up to the aortic bifurcation. (c) MPMCTA, arterial phase, oblique reconstruction, MIP; stented aorta and cervical anastomoses. Note pancreatic leakage artefact (arrow). (d) Detail, oblique reconstruction: Unimpaired perfusion of fenestrated stent-reinforced nonradiopaque bypass to the coeliac artery (arrows). (e) Detail, oblique reconstruction: Unimpaired perfusion of fenestrated stent-reinforced left renal artery (arrows). (f) Aortic bifurcation with dorsally oriented endoleak in MPMCTA (arrows). (g) Autopsy: Dissected abdominal aorta. (h) Detail: Fenestrations for renal artery stents (arrows). Displaced stent insertion of coeliac bypass (curved arrow), which demonstrates the sheer impracticality at autopsy to handle the specimen without damage. Dissection did not reveal the endoleak
Aortic medionecrosis. Thoracic EVAR 10 days before death. Hemorrhagic shock after aortic rupture into left thoracic cavity. EVAR with multiple visceral bypasses (“Octopus”; the term “Octopus” refers to the multiple tentacles of the animal). Dissection of the thoracic aorta and of the abdominal aorta treated with TEVAR and EVAR. The TEVAR had been combined with reconstruction of the aortic arch, including debranching of the supra-aortic arteries. The EVAR had been combined with debranching of the visceral arteries and “Octopus” bypasses. Three bypasses originate from the right external iliac artery and supply the superior mesenteric artery and both renal arteries. Another bypass connects the superior mesenteric artery with the common hepatic artery. (a) MPMCTA, dynamic phase, orthograde multiplanar reconstruction. Left-sided contrast extravasation (crosshairs, center) from a mediastinal endoleak at the level of a stent angulation. (b) Arterial phase. Frontal reconstruction of the aorta, MIP. Note stents in the thoracic aorta and abdominal aorta, and reconstructed supra-aortic arteries and four bypasses from the right external iliac artery to the visceral arteries of the abdomen (dashed circle). Left-sided contrast agent extravasation in the abdomen. (c) MPMCTA, arterial phase, three-dimensional reconstruction: “Octopus” bypasses from the external iliac artery to the right renal artery (red arrow), to the superior mesenteric artery (yellow arrow), and to the left renal artery (dashed red arrow). Another bypass between the superior mesenteric artery and the common hepatic artery (dashed yellow arrow). (d) Detail: Right iliac artery with the anastomoses of the bypass to the right renal artery (narrowing of the anastomosis, arrows), to the superior mesenteric artery (with kinking, arrows), and to the left renal artery (with narrowing, arrows)
References
Vogel B, Heinemann A, Gehl A, Hasegawa I, Höpker WW, Poodendaen C, et al. Post-mortem computed tomography (PMCT) and PMCT-angiography after transvascular cardiac interventions. Arch Med Sadowej Kryminol. 2013;63:255–66.
Wichmann D, Heinemann A, Weinberg C, Vogel H, Hoepker WW, Grabherr S, et al. Virtual autopsy with multiphase postmortem computed tomographic angiography versus traditional medical autopsy to investigate unexpected deaths of hospitalized patients: a cohort study. Ann Intern Med. 2014;160:534–41.
Tsang TS, Freeman WK, Barnes ME, Reeder GS, Packer DL, Seward JB. Rescue echocardiographically guided pericardiocentesis for cardiac perforation complicating catheter-based procedures. The Mayo Clinic experience. J Am Coll Cardiol. 1988;32:1345.
Palmiere C, Lobrinus JA, Mangin P, Grabherr S. Detection of coronary thrombosis after multi-phase postmortem CT-angiography. Legal Med. 2013;15:12–8.
Rashid SN, Bouwer H, O’Donnell C. Lethal haemorrhage from a ureteric-arterial-enteric fistula diagnosed by postmortem CT angiography. Forensic Sci Med Pathol. 2012;8:430–5.
Cherr GS, Travis JA, Ligush Jr J, Plonk G, Hansen KJ, Braden G, Geary RL. Infection is an unusual but serious complication of a femoral artery catheterization site closure device. Ann Vasc Surg. 2001;15:567.
Katzenschlager R, Ugurluoglu A, Ahmadi A, Hülsmann M, Koppensteiner R, Larch E, et al. Incidence of pseudoaneurysm after diagnostic and therapeutic angiography. Radiology. 1995;195:463.
Michaud K, Grabherr S, Lesta Mdel M, Augsburger M, Doenz F, Mangin P. Ruptured pseudo-aneurysm of a femoral artery in a drug abuser revealed by post-mortem CT angiography. Int J Legal Med. 2013;127:819–23.
Popma JJ, Satler LF, Pichard AD, Kent KM, Campbell A, Chuang YC, et al. Vascular complications after balloon and new device angioplasty. Circulation. 1993;88:1569.
Westphal SE, Apitzsch JC, Penzkofer T, Kuhl CK, Mahnken AH, Knüchel R. Contrast-enhanced postmortem computed tomography in clinical pathology: enhanced value of 20 clinical autopsies. Hum Pathol. 2014;45:1813–23.
Roberts ISD, Benamore RE, Peebles C, Roobottom C, Traill ZC. Diagnosis of coronary artery disease using minimally invasive autopsy: evaluation of a novel method of post-mortem coronary CT angiography. Clin Radiol. 2011;66:645–50.
Palmiere C, Binaghi S, Doenz F, Bize P, Chevallier C, Mangin P, Grabherr S. Detection of haemorrhage source: the diagnostic value of post-mortem CT-angiography. Forensic Sci Int. 2012;222:33–9.
Vogel B, Heinemann A, Gulbins H, Treede H, Reichenspurner H, Puschel K, Vogel H. Post-mortem computed tomography and post-mortem computed tomography angiography following transcatheter aortic valve implantation. Eur J Cardiothorac Surg. 2016;49(1):228–33.
Koreny M, Riedmüller E, Nikfardjam M, Siostrzonek P, Müllner M. Arterial puncture closing devices compared with standard manual compression after cardiac catheterization: systematic review and meta-analysis. JAMA. 2004;291:350.
El-Jack SS, Ruygrok PN, Webster MW, Stewart JT, Bass NM, Armstrong GP, et al. Effectiveness of manual pressure hemostasis following transfemoral coronary angiography in patients on therapeutic warfarin anticoagulation. Am J Cardiol. 2006;97:485.
Maisano F, Godino C, Giacomini A, Denti P, Arendar I, Buzzatti N, et al. Clinical trial experience with the MitraClip catheter based mitral valve repair system. Int J Cardiovasc Imaging. 2011;27:1155–6.
Feldman T, Young A. Percutaneous approaches to valve repair for mitral regurgitation. J Am Coll Cardiol. 2014;63:2057–68.
Bos WT, Verhoeven EL, Zeebregts CJ, Tielliu IF, Prins TR, Oranen BI, van den Dungen JJ. Emergency endovascular stent grafting for thoracic aortic pathology. Vascular. 2007;15:12–7.
Obitsu Y, Koizumi N, Iida Y, Satou K, Watanabe Y, Takae H, et al. Hybrid treatment of multiple aortic aneurysms by combined conventional surgery and endovascular aortic repair. Ann Vasc Dis. 2008;1:40–4.
Torsello G, Can A, Umscheid T, Tessarek J. Hybrid thoracoabdominal aneurysm repair with simultaneous antegrade visceral revascularization and supra-aortic debranching from the ascending aorta. J Endovasc Ther. 2007;14:342–6.
Cao P, De Rango P, Verzini F, Parlani G. Endoleak after endovascular aortic repair: classification, diagnosis and management following endovascular thoracic and abdominal aortic repair. J Cardiovasc Surg (Torino). 2010;51:53–69.
Bown MJ, Fishwick G, Sayers RD. The post-operative complications of endovascular aortic aneurysm repair. J Cardiovasc Surg (Torino). 2004;45:335–47.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Vogel, H., Heinemann, A. (2016). Postmortem Angiography and Clinical Pathology. In: Grabherr, S., Grimm, J., Heinemann, A. (eds) Atlas of Postmortem Angiography. Springer, Cham. https://doi.org/10.1007/978-3-319-28537-5_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-28537-5_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28535-1
Online ISBN: 978-3-319-28537-5
eBook Packages: MedicineMedicine (R0)