Abstract
AbstractDue to its increasing prevalence and associated health complications, Metabolic Syndrome (MetS) has become both a public health concern and a clinical challenge. Dietary approaches to prevention and treatment of MetS vary, yet nearly all experts agree that the clinical parameters of the syndrome are greatly improved through lifestyle changes including diet. Existing evidence suggest a positive link between adherence to diets with features resembling the principles of the traditional Mediterranean diet (MD) and improvement of metabolic abnormalities. Although, the overall evidence suggests such promising trend, discrepancy of the results can be attributed to factors such as quality, methodology, and the overall design of the studies. Not much clinical application can be instigated from the existing evidence unless several well-designed clinical trials are conducted to investigate the causal associations and potentially define the underlying mechanisms.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Key Points
-
Due to its increasing prevalence in the past two decades and its associated health complications, metabolic syndrome (MetS) has become both a public health concern and a clinical challenge. Dietary approaches for the prevention and treatment of MetS vary, yet there is general agreement that the clinical parameters of the syndrome are greatly improved through lifestyle changes including diet.
-
Existing evidence suggests a positive link between adherence to diets low in saturated fat, trans fat, cholesterol, added sugar, and sodium and high in unsaturated fats, complex unrefined carbohydrates, fruits, vegetables, and fish and improvement of metabolic abnormalities. Interestingly, these dietary features are characteristic of the traditional Mediterranean diet (MD). On the basis of the most current and available evidence including observational and intervention studies on management of MetS, adherence to the MD may be associated with improvements in various MetS parameters.
-
Although most epidemiological studies recognize that the MD has preventive effects against MeS, some studies have been inconclusive possibly because of differences in methodologies, overall design of the studies, and quality of the data.
-
Well-designed clinical trials are needed to investigate the cause–effect relationships between MD and onset of MetS and define the underlying mechanisms of actions of food components on pathways that contribute to the MetS.
Introduction
Mediterranean dietary traditions have historically been linked to overall good health. Plant-based foods constitute the core of daily dietary intake of individuals who adhere to the traditional Mediterranean dietary patterns which if consumed in sufficient amounts, provide all of the essential macronutrients and micronutrients, and fiber believed to promote overall health [1]. Metabolic syndrome (MetS) o r syndrome X is a collection of associated risk factors which significantly increase the risk of developing atherosclerosis and diabetes mellitus (DM) later in life. It has been suggested that individuals with MetS may benefit from aggressive lifestyle modifications through diet and physical activity, yet a uniform consensus is lacking as to which type of diet is optimal for prevention and treatment of this particular syndrome [2]. A growing body of scientific evidence has addressed the implications of the traditional Mediterranean diet (MD) and improvement of the MetS and its individual components. In this chapter, we summarize the existing scientific evidence on the impacts of the MD on MetS.
Metabolic Syndrome
Obesity, non-insulin-dependent diabetes mellitus, hypertension, and dyslipidemia, also referred to as the deadly quartet, are key characteristics of MetS. The concept of MetS was first described in 1920s by the Swedish physician, Kylin Studien, as a collection of metabolic and non-metabolic disturbances including hypertension, hyperglycemia and gout [2]. In 1947, the Marseilles physician, Jean Vague, made an important observation and drew attention to the important role that the upper body adiposity played in predisposing individuals to diabetes, atherosclerosis, and gout [2, 3]. Over the past two decades, the MeS has received increased attention from the health-care community , mainly due to a striking rise in its prevalence worldwide.
Definition and Diagnostic Criteria
Although the MeS has been in the spotlight for the past two decades, there has been considerable disagreement over the terminology, definition, and diagnosis criteria related to its diagnosis. In an effort to standardize the terminology used for MetS in the world of clinical practice, several organizations have undertaken the task of formulating simple criteria for the standardization of its diagnosis (Table 9.1) [4, 5]. The most commonly used criteria for clinical diagnosis of MetS, however, has been defined by the National Cholesterol Education Program (NCEP) Panel III (ATP III) as having at least three of the following [4, 5]:
-
1.
Abdominal obesity (waist circumference = WC> 102 cm for men and > 88 cm for women).
-
2.
High triglyceride (TG) levels (≥150 mg/dL).
-
3.
Low high density lipoprotein cholesterol (HDL-C) levels (<40 mg/dL in men or <50 mg/dL in women).
-
4.
High blood pressure (BP) (≥130/85 mmHg on at least two separate measurements).
-
5.
High fasting glucose (≥100 mg/dL or ≥5.6 mmol/L).
In an attempt to unify the criteria for clinical diagnosis of MetS, a joint interim consensus statement was prepared and published by the International Diabetes Federation Task Force on Epidemiology and Prevention in October of 2009 [4]. The statement was the result of a joint meeting between the following organizations: National Heart, Lung, and Blood Institute, the American Heart Association, World Heart Federation, International Atherosclerosis Society, and International Association for the Study of Obesity [4]. According to this new definition, MetS is defined as having at least three of the following criteria: abdominal obesity (waist circumference ≥94 cm for men and ≥80 cm for women), high blood pressure (systolic blood pressure/diastolic blood pressure ≥130/85 mmHg or antihypertensive medication), hypertriglyceridemia (≥1.7 mmol/L or fibrate medication), low HDL-cholesterolemia (<1.03 mmol/L for men or <1.29 mmol/L for women), and hyperglycemia (glycemia ≥ 5.6 mmol/L or antidiabetic medication) [4].
MeS: Prevalence and Clinical Significance
MetS is widespread among adults residing in developed countries, with a prevalence of about 20–30 %, or even higher [6]. According to reports from the National Health and Nutritional Examination Survey (NHANES), both unadjusted (27.9 ± 1.1 % to 34.1 ± 0.8 %, P < 0.001) and age-adjusted prevalence (29.2 ± 1.0 % to 34.2 ± 0.7 %, P < 0.001) of MetS among US adults showed a persistent increase from the periods 1988–1994 to 1999–2006 [7]. This increase in prevalence of MetS among US adults is a serious public health concern, given that it considerably raises the risks of developing DM and cardiovascular disease (CVD) later in life [7].
Another NHANES analysis of the prevalence and trends of MetS between 1999 and 2010 showed that while the prevalence of MetS (as it is currently defined by the ATP III) has slightly declined over time, there have been upward trends in abdominal obesity, particularly among female adults, and hyperglycemia across the entire US population compared to 1999 and 2000 [8]. This is particularly important, given that each condition related to the MeS is an independent risk factor for CVD and/or DM. However, when two or more conditions are clustered together, the MeS becomes increasingly atherogenic and diabetogenic raising the risk of stroke, diabetes-related complications including nephropathy, retinopathy, distal neuropathy, and cardiovascular morbidity and mortality [9]. In addition, MetS has been linked with other chronic diseases including fatty liver disease, some types of cancer, hypogonadism, and vascular dementia [10].
Mediterranean Diet in Prevention and Treatment of MeS
Dietary and lifestyle modification that include regular moderate to intense physical activity and reduction of central obesity remain the recommended cornerstone for the prevention and treatment of MetS [9–13]. While there is a general agreement over beneficial effects of regular physical activity and weight reduction for management of MetS, a uniform consensus is lacking as to which type of diet is optimal for this particular condition [14, 15]. Existing epidemiological evidence suggest a positive link between adherence to diets low in saturated fat, trans fat, cholesterol, added sugar, and sodium and high in unsaturated fats, complex unrefined carbohydrates, fruits, vegetables, and fish and improvement of metabolic abnormalities [10, 15]. Interestingly, these features resemble the principles of the traditional Mediterranean diet (MD) [15, 16].
Studies have documented that adherence to the MD lowers rates of morbidity, CVD, certain types of cancer, chronic inflammation, mortality, and improves overall health and quality of life [15, 16]. The term, MD, was described in 1960s and refers to dietary patterns found in olive-growing areas in the Mediterranean basin. Although there are several variations of the MD, common component s include: high monounsaturated to saturated fat ratio; moderate consumption of ethanol (mainly in the form of red wine); moderate consumption of milk and dairy products (mainly in the form of cheese and yogurt); low intake of red meat and meat products; and high intake of fresh fruits and vegetables and whole grains [13–15]. One of the main characteristics of MD is the use of olive oil as the main source of fat in cooking [15–17].
Cross-Sectional Studies
Cross-sectional studies investigated the relationships between adherence to a MD and the prevalence of MetS [18–20]. The first study, known as ATTICA, was a study that randomly enrolled 1514 men and 1528 women over the age of 18 years with no history of CVD or DM from the Attica area of Greece [18]. Adherence to MD, among several other factors, was assessed by a diet score (with higher values representing a closer adherence to the MD) which incorporated the inherent characteristics of this diet. Closer adherence to the MD was associated with a 19 % lower risk of developing the MetS. Adherence to the traditional MD was also associated with a significant reduction in the concentration of inflammatory and coagulation markers [18]. The study did not find significant associations between adherence to the MD and HDL-C and TG concentrations in obese and overweight individuals but found a negative association with blood pressure [18, 21].
These first data, however, were only partially supported by the results of a second cross-sectional study which examined the intakes of cereal, fruit, legumes, vegetables, fish, nuts, monounsaturated fat to saturated fat ratio, alcohol from red wine, whole fat dairy products, and red meat among a representative sample of 578 adults (>18 years) from the Canary Islands (Spain) who were participating in the Canarian Nutrition Survey (ENCA). According to the ENCA study, once adjusted, adherence to MD showed no significant association with prevalence of the MetS. However, participants in the third tertile of the MD adherence had a 70 % lower prevalence of blood pressure criteria and 2.5 times more prevalence of the gl ycemic criteria with respect to the first tertile. Higher intake of red meat was associated with higher prevalence of blood pressure criteria whereas moderate alcohol intake from red wine was associated with lower prevalence of blood pressure in women and lower prevalence of HDL-C criteria in men. Fruit intake showed a protective effect on TG criteria, whereas vegetable intake showed a protective effect on insulin resistance. Whole fat dairy intake showed a protective effect on the glycemia criteria and high monounsaturated to saturated fatty acid intake had a positive impact on insulin resistance. Overall, the study concluded that the MD showed protective effects on specific components of the MetS [19].
In 2009, Babio et al. conducted a cross-sectional study in 808 elderly participants with no history of CVD, yet at high risk for developing CVD from the PREvencio´n con DIeta MEDiterra´nea (PREDIMED) study [20]. The PREDIMED was a 5-year parallel group, multicenter, controlled clinical trial that aimed to examine the effects of the MD on the primary prevention of CVD [20]. Participants in the highest quartile with the highest adherence to the MD had 47–54 % lower odds of having low HDL-C and high TG compared to those in the lowest quartile. Some components of the MD including olive oil, legumes, and red wine were associated with lower prevalence of MetS. Overall, higher adherence to the MD was significantly associated with lower odds ratio of developing MetS in a population at high risk of CVD.
Romaguera et al. assessed a cross-sectional association between adherence to a modified MD (high in foods of plant origin including vegetables, legumes, fruits, nuts, cereals, and unsaturated fatty acids), BMI, and WC in a total of 497,308 men and women (70.7 %) aged 25–70 years from 10 European countries [22]. This study was conducted in participants of the European Prospective Investigation into Center and Nutrition-Physical Activity, Nutrition, Alcohol, Cessation of Smoking, Eating Out of Home and Obesity or EPIC-PANACEA project [22]. Although there was no association between modified MD and BMI, results revealed that adherence to this type of diet, regardless of heterogeneity among regions, was strongly associated with lower abdominal obesity measured by WC in European men and women. This result was confirmed in a following cross-sectional analysis of 773 individuals aged 30–94 years (mean age of 60 years) from the Adventist Health Study 2 [23]. Results of this study suggested that a plant-based dietary pattern, similar to the modified MD, was associated with significantly lower means for all metabolic risk factors except HDL-C and a lower risk of having MetS (OR: 0.44, 95 % CI; 0.30–0.64, P < 0.001). This relationship also persisted after adjusting for lifestyle and demographic factors.
Yahia et el. examined the association between MetS and the Mediterranean dietary patterns in a pilot study of 100 Lebanese Notre Dame University students (62 males and 38 females) aged 18–27 years. Students who had MetS had higher consumption of red meat and sweets and a lower consumption of legumes [24]. These results showed a pro mising trend with respect to lower consumption of animal foods and lower prevalence of MetS and its criteria.
Prospective Cohort Studies
Several prospective cohort studies have been published on the topic of adherence to MD and incidence of MetS in healthy individuals with no history of chronic diseases [25–27]. The Seguimiento University of Navarra (SUN) prospective cohort (an open-enrollment cohort) was the first study that assessed the relationship between adherence to the Mediterranean Food Pattern (MFP) and the subsequent development of MetS in 2563 Spanish university graduates (no risk factors present at baseline) for 6 years [25]. Results from the SUN cohort showed that the cumulative incidence of MetS was lower for those with the highest adherence to the MFP. In particular, participants with the highest MFP scores (highest adherence) showed an odds ratio of 0.20 (95 % CI, 0.06–0.63) in comparison to those with the lowest adherence. This difference also persisted after adjustment for age, sex, physical activity, smoking, and total energy intake [25]. Similar trends were observed by Rumawas et al. who examined the prospective association between a diet consistent with a Mediterranean-style dietary pattern and MetS traits and its incidence in 1918 nondiabetic US men and women of the Framingham Heart Study Offspring with baseline median age of 54 years followed for 7 years [26]. Results revealed that participants in the highest quintile category had a lower incidence (31.1 %) of MetS compared to those in the lowest quintile (38.5 %). Subjects with highest adherence to the diet had a 11.8 % less risk of developing MetS during the 7-year follow up period [26].
The SU.VI.MAX or Supplementation en Vitamines et Mineraux AntioXydants study was the first study that examined the associat ion between adherence to MD and risk of MetS using three different Mediterranean diet-based scores (traditional Mediterranean diet score, MDS; an updated Mediterranean score, MED; and Mediterranean style-dietary pattern score, MSDPS) [27]. In addition, this was the first study which employed the most recent definition of MetS [4, 27]. A cohort of 3232 French MetS-free adult participants from the SU.VI.MAX study (1994–2002) was followed for 6 years. SU.VI.MAX was a randomized placebo-controlled trial that included 13,017 individuals to test the efficacy of daily supplementation with antioxidant vitamins (vitamins C, E, and β-carotene) and minerals (selenium and zinc) at nutritional doses on the incidence of cancers, ischemic heart disease, and overall mortality [28]. Results from the SU.VI.MAX cohort study showed that all MD scores were associated with reduced criteria of MetS and MetS incidence. However, the strength of the association was dependent on the score used to assess adherence to the diet. The association between MED score and lower MetS risk was stronger than that observed with the traditional MDS, suggesting a critical role of refined grains and sweetened beverages. The widely used MDS [29, 30] showed a negative association with incidence of MetS, but only WC and blood TG were negatively associated with the MDS.
A 2009 study evaluated the association between MD and incidence of MetS in 160 Iranian renal transplant patients 1 year following transplantation [31]. The incidence of MetS in renal transplant recipients is usually estimated to be ~60 % 1 year post-transplant. This high incidence is partially due to the effect of immunosuppressive medications and increased risk of weight gain, hyperlipidemia, hypertension, and glucose intolerance, which characterize the MetS. Corticosteroids may also have an important role in the incidence of post-transplant MetS. After adjustment for age and sex, results showed that participants in the highest tertile of the Mediterranean dietary pattern score had lower odds for the MetS (OR: 0.52, 95 % CI; 0.21–1.24) than those in the lowest tertile. Conversely, those patients in the highest tertile of the saturated fats and sugars dietary pattern score had greater odds of the MetS (OR: 1.29; 95 % CI; 0.54–3.06) than those in the lowest tertile [31]. These results with renal transplant patients were considered of particular significance since they extended the benefits of adherence to the MD beyond those previously observed in healthy individuals.
Intervention Trials
To date, only few intervention trials have been conducted to examine the relationships between adherence to a Mediterranean-like diet and MetS. Esposito et al. conducted a randomized single-blinded study from June 2001 to January 2004 on 180 patients with MetS at a University hospital in Italy in order to assess the effects of a Mediterranean-style diet on endothelial functions and vascular inflammatory markers [32]. The intervention group (n = 90) was instructed to follow a Mediterranean-style diet and received advice on how to increase daily consumption of whole grains, fruits, vegetables, nuts, and olive oil. The intervention diet consisted of 50–60 % carbohydrates, 15–20 % protein, and <30 % total fat with less than 10 % coming from saturated fat and less than 300 mg cholesterol per day. Patients were encouraged to consume at least 250–300 g of fruits, 125–150 g of vegetables, 25–50 g of walnuts, 400 g of whole grains (legumes, rice, maize, and wheat) per day and to increase their intake of olive oil. The control group (n = 90) followed a prudent diet which consisted of 50–60 % carbohydrates, 15–20 % protein, and <30 % total fat. Compared with patients consuming the control diet, patients consuming the intervention diet had significantly reduced serum concentrations of inflammatory markers as well as insulin resistance. Endothelial function score also significantly improved in the intervention group (mean [±SD] change, +1.9 [±0.6]; P < 0.001) but remained nearly stable in the control group (+0.2 [±0.2]; P = 0.33). At 2 years of follow-up, only 40 patients in the intervention group were still classified as having MetS, compared to 78 patients in the control group (P < 0.001) [32].
In a 2008 PREDIMED study, 1 year effect of two behavioral interventions was compared with two high-fat, non-energy-restricted MDs, one supplemented with 1 L/week virgin olive oil (MD+VOO) and another supplemented with 30 g/day mixed nuts as 15 g walnuts, 7.5 g hazelnuts, and 7.5 g almonds (MD+nuts), with that of advice on a low-fat diet (control diet) in volunteers at high risk for CVD [33]. The study included 1224 participants who were recruited into the PREDIMED trial. All diets were ad libitum and there was no increase in physical activity for any of the intervention groups. After 1 year, the prevalence of MetS was significantly lower in the MD+nuts group (13.7 % vs. 6.7 % and 2.0 % in the MD+VOO and the control group respectively). Furthermore, logistic regression analysis confirmed that the MD+nuts was associated with lowering of MetS among those subjects who had the syndrome at baseline whereas the incident rates were not significantly different among groups (Fig. 9.1). The authors concluded that a non-energy restricted traditional MD supplemented with mixed nuts (high in fat, high in unsaturated fat, and palatable) was a useful approach in management of MetS [33]. The authors also stated that the study duration was too short to address clinical outcomes and that a longer follow-up of the entir e PREDIMED cohort might provide stronger evidence on protective effects of the MD on CVD.
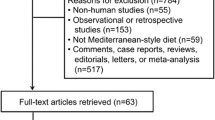
Impact of Mediterranea n diet, virgin olive oil, and nuts on MeS. Data represent odds ratio and confidence interval of 1-year reversion among participants with MetS at baseline and incidence among participants without MetS at baseline in the two MD groups in comparison with the control group [33]
One possibility is that the protective effects of the MD on MetS observed in most studies may be due to the weight loss that occurs when individuals change their behaviors and incorporate a healthier eating plan. In order to examine the modifying effects of weight loss on the impact of the MD on CVD risk factors, Richard et al. assessed the efficacy of MD with and without weight loss on CVD risk factors in 26 men (aged 24–62 years) with MetS [34]. Participants consumed a North American control diet for 5 weeks followed by a 5-week MD, both under-weight-maintaining conditions. Participants then underwent a 20-week weight loss period, after which they consumed the MD for 5 weeks under-weight-stable conditions. All foods were provided to participants during the weight-stable phases of the study. Results showed that in the absence of weight loss, the MD reduced total plasma cholesterol, LDL-C, and total cholesterol to HDL-C ratio compared to the control diet (all P < 0.04). The MD in combination with weight loss resulted in reduction of systolic blood pressure, diastolic blood pressure, TG, apolipoprotein B, fasting glucose and insulin compared to the control diet (all P < 0.001). Overall, the conclusion was that the MD in the absence of weight loss led to significant changes in plasma cholesterol concentration but had minor effects on other cardiometabolic risk factors of MetS [34].
In a 2011 study, the impact of a Mediterranean-style low-glycemic-load diet was examined in women with MetS [35]. In this 12-week, two-arm randomized clinical trial, women in the control group (n = 44) consumed a Mediterranean-style low-glycemic-load diet and women in the intervention group (n = 45) consumed the same diet as the control group plus a medical food containing phytosterols, soy protein, and extracts from hops and acacia. After 12 weeks, all participants showed significant decreases in WC, systolic and diastolic BP, and plasma TG in (P < 0.001 for all) with no differences between arms. The HDL-C levels significantly decreased in week eight but returned to baseline levels by week 12 while plasma glucose concentration did not change over the course of the study. Addition of the medical food resulted in a less atherogenic lipoprotein profile and lower plasma homocysteine in the intervention arm. Both groups experienced a significant weight loss despite the fact that no caloric restriction was applied in this study. Overall, a Mediterranean-style low-glycemic-load diet effectively reduced the variables of MetS in the women of this study [15, 35].
Recently, the results of a 1-year intervention study with the MD on plasma fatty acid composition and MetS were reported in a subset of high risk participants (n = 424, aged 55–80 years) who were randomly selected from the PREDIMED trial after completing a 1-year intervention program [6]. The detailed protocol of the PREDIMED study has been described earlier in this chapter [20, 33]. After a full year of intervention, the MD+VOO group showed a significant increase in plasma levels of palmitic and oleic acids and reduced proportions of margaric, ste aric, and linoleic acids whereas MD+nuts group showed a significant rise in levels of palmitic, linoleic, and α-linolenic acids, but reduced proportions of myristic, margaric, palmitoleic, and dihomo-γ-linoleic acids. No significant weigh changes were observed in any of the study arms. Increases in the biomarkers of foods supplied to the MD groups, i.e., oleic and α-linolenic acids, were beneficially associated with the incidence, improvement, and prevalence of MetS. In conclusion, both the MD+VOO and MD+nuts diets resulted in a fatty acid composition that showed promising effects on MetS. Therefore, according to the authors of this study, a MD that is rich in fats of plant origin may be beneficial for the management of MetS without the need for concerns over potential weight gain due to the high fat content of the diet. Another recent study confirmed the beneficial effects of adherence to the MD for three months on metabolic, oxidative, and inflammatory abnormalities in 84 healthy Algerian participants (11 males and 73 females) with MetS [36]. Participants were simply advised to reduce their intake of simple carbohydrate, saturated fats, cholesterol, animal proteins, and increase intake of monounsaturated fats, olive oil, fiber, fruits, and vegetables for 3 months.
Meta-analyses
In addition to major studies reviewed so far in this chapter, several smaller clinical trials and epidemiological studies have also examined the effects of adherence to the MD on MetS and its individual components. Kastorini et al. conducted a meta-analysis of original research including epidemiological studies and randomized clinical trials until April 30, 2010 through a computer-assisted published search of PubMed, Embase, Scopus, and the Cochrane Central Register of Controlled Trials database [37]. A total of 50 original studies including 35 clinical trials, two prospective cohort studies, and 13 cross-sectional studies with 534,906 participants were included in the final analysis. Analysis of prospective and clinical studies showed that adherence to the MD was associated with reduced risk of MetS (HR = 0.96; 95 % CI, 1.24–1.16) [37]. Results of clinical studies also revealed that the MD had a protective effect on individual components of the MeS, such as WC (mean difference, 0.42 cm), HDL-C (1.17 mg/dL), TG (6.14 mg/dL), glucose (3.89 mg/dL), and systolic blood pressure (2.35 mmHg) and diastolic blood pressure (1.58 mmHg). Overall, results from clinical studies, cross-sectional studies, and prospective studies support the health benefits of the MD aga inst MeS (Fig. 9.2).
Mediterranean diet and met abolic syndrome. Adherence to the Mediterranean diet was associated with a protective effect in two of two clinical trials, two of four cross-sectional studies, and one of two prospective studies, as compared with lower compliance with this pattern or with a control diet [37]
Conclusions and Future Opportunities
Dietary approaches for the prevention and treatment of MetS vary, but there is general agreement that clinical parameters associated with the MeS can be greatly improved through lifestyle changes related to diet and physical activity. In nutritional epidemiology research, interest has shifted from the study of single nutrients to the study of food groups and more recently, to learning more about dietary patterns and how interactions between nutrients (rather than single nutrients) produce protective effects against chronic diseases and improve overall health and quality of life. In this context, the study of the Mediterranean dietary patterns in respect to MetS has received considerable interest. A substantial proportion of individuals living in the Western nations suffer from multiple metabolic abnormalities that place them at a much greater risk category for developing CVD and DM. On the basis of the most current and available evidence from observational and intervention studies, the MD may be beneficial for ameliorating conditions associated with the MeS. Although there are variations of the MD, the term essentially refers to a primarily plant-based diet that constitutes an abundance of fruits, vegetables, whole-grain cereals, nuts, and legumes; with olive oil as the primary source of fat; fish and poultry consumed in low-to-moderate amounts and relatively low consumption of red meat and dairy; and with moderate consumption of wine, normally with meals. Although the MD has been shown to contribute to weight loss in many studies, the beneficial effects of the MD on MetS seem to be independent of the weight loss.
Finally, it should be considered whether or not opportunities exist for the implementation of the MD for the prevention of MeS in Western societies. On a daily basis, the majority of people in the Western world consume large amounts of processed foods high in saturated fats, added sugar, and salt. People in Western countries spend little or no time in the kitchen cooking their meals, but more time in fast-food driving lanes picking up daily meals and restaurant franchises. Because of complex cultural and economic conditions, adherence to a Mediterranean dietary pattern remains challenging in Western societies. More studies are needed to obtain research-based evidence about the health benefits of MD against MeS and development of nutrition and lifestyle education programs for its prevention.
References
Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6):1402S–6.
Eckel RH, Grundy SM, Zimmet PZ. The metabolic Syndrome. Lancet. 2005;365:1415–28.
Vague J. La differenciation sexuelle, facteur determinant des formes de l’obesite. Presse Med. 1947;30:339–40.
Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing metabolic syndrome: A Joint interim statement of the International and Blood Institute; American Heart Association; World Heart Federation; International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–45.
Grundy SM. Diagnosis and management of the metabolic syndrome An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52.
Mayneris-Perxachs J, Sala-Vila A, Chisaguano M, Castellote AI, Estruch R, Covas MI, et al. Effect of 1-year intervention with a Mediterranean diet on plasma fatty acid composition and metabolic syndrome in a population at high cardiovascular risk. PLoS ONE. 2014;9(3), e85202.
Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among U.S. adults: NHANES III to NHEANES 1999-2006. Diabetes Care. 2011;34:216–9.
Beltrán-Sánchez H, Harhay MO, Harhay MM, McElligott S. Prevalence and trends of metabolic syndrome in the adults U.S. population, 1999-2010. J Am Coll Cardiol. 2013;62(8):697–703.
Panagiotakos DB, Polychronopoulos E. The role of Mediterranean diet in the epidemiology of metabolic syndrome: Converting epidemiology to clinical practice. Lipids Health Dis. 2005;4:7.
Anagnostis P. Metabolic syndrome in the Mediterranean region: Current Status. Ind J Endocrinol Metab. 2012;16(1):72–80.
Cornier MA, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, et al. The metabolic syndrome. Endocr Rev. 2008;29:777–822.
World Health Organization Study Group: Diet, Nutrition, and the Prevention of Chronic Diseases. Geneva, Switzerland: World Health Organization; Technical Report Series, 916, 2003.
Kontogianni MD, Panagiotakos DB. Current epidemiological and clinical evidence on the relationship between Mediterranean diet and the metabolic syndrome. Curr Nutr Food Sci. 2007;3:296–9.
Baxter AJ, Coyne T, McClintock C. Dietary patterns and metabolic syndrome—a review of epidemiologic evidence. Asia Pac J Clin Nutr. 2006;15:134–42.
Kiortsis DN, Simos YV. Mediterranean diet for the prevention and treatment of metabolic syndrome: is it worth it? Angiology. 2014;65(1):5–8.
Pe’rez-Lo’pez FR, Chedraui P, Haya J, Cuadros JL. Effects of the Mediterranean diet on longevity and age-related morbid conditions. Maturitas. 2009;64:67–79.
Minich DM, Bland JS. Dietary management of the metabolic syndrome beyond macronutrients. Nutr Rev. 2008;66(8):429–44.
Panagiotakos DB, Pitsavos CH, Chrysohoou C, Skoumas J, Tousoulis D, Toutouza M, et al. Impact of lifestyle habits on the prevalence of the metabolic syndrome among Greek adults from the ATTICA study. Am Heart J. 2004;147:106–12.
Alvarez León EE, Henríquez P, Serra-Majem L. Mediterranean diet and metabolic syndrome: A cross-sectional study in the Canary Islands. Publ Health Nutr. 2006;9:1089–98.
Babio N, Bullò B, Basora J, Martínez-González MA. Fernández- Ballart J, Márquez-Sandoval F, et al. Adherence to the Mediterranean diet and risk of metabolic syndrome and its components. Nutr Metab Cardiovasc Dis. 2009;19:563–70.
Tzima N, Pitsavos C, Panagiotakos DB, et al. Mediterranean diet and insulin sensitivity, lipid profile and blood pressure levels, in overweight and obese people; The Attica study. Lipids Health Dis. 2007;6:22.
Romaguera D, Norat T, Mouw T, May AM, Bamia C, Slimani N. Adherence to the Mediterranean diet is associated with lower abdominal obesity in European men and women. J Nutr. 2009;139:1728–37.
Rizzo NS, Sabate J, Jaceldo-Siegl K, Fraser GE. Vegetarian dietary patterns are associated with a lower risk of metabolic syndrome. Diabetes Care. 2011;34:1225–7.
Yahia N, Hayek G, Shahin S. Obesity, metabolic syndrome, and the Mediterranean diet in a sample of Lebanese university students. Nutr Today. 2011;46(3):138–45.
Tortosa A, Bes-Rastrollo M, Sanchez-Villegas A, Basterra-Gortari FJ, Nunez-Cordoba JM, Martinez-Gonzalez MA. Mediterranean diet inversely associate with the incidence of metabolic syndrome: The SUN prospective cohort. Diabetes Care. 2007;30(11):2957–9.
Rumawas ME, Meigs JB, Dwyer JT, McKeown NM, Jacques PF. Mediterranea-style dietary pattern, reduced risk of metabolic syndrome traits, and incidence in the Framingham offspring cohort. Am J Clin Nutr. 2009;90:1608–14.
Kesse-Guyot E, Ahluwalia N, Lassale C, Hercberg S, Fezeu L, Lairon D. Adherence to Mediterranean diet reduces the risk of metabolic syndrome: A 6-year prospective study. Nutr Metab Cardiovasc Dis. 2013;23:677–83.
Hercberg S, Galan P, Preziosi P, Bertrais S, Mennen L, Malvy D, et al. The SU.VI.MAX Study: A randomized, placebo-controlled trial of the health effects of antioxidant vitamins and minerals. Arch Intern Med. 2004;164(21):2335e42.
Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, et al. Diet and overall survival in elderly people. Br Med J. 1995;311(7018):1457e60.
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599e608.
Nafar M, Noori N, Jalali-Farahani S, Hosseinpanah F, Poorrezagholi F, Ahmadpoor P, et al. Mediterranean diets are associated with a lower incidence of metabolic syndrome one year following renal transplantation. Kidney Int. 2009;76:1199–206.
Esposito K, Marfella R, Ciotola M, et al. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome. A randomized trial. J Am Med Assoc. 2004;292(12):1440–6.
Salas-Salvado J, Fernandez-Ballart J, Ros E, Martinez-Gonzalez MA, Fito M, Estruch R, et al. Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: One-year results from the PREDIMED randomized trial. Arch Intern Med. 2008;168(22):2449–58.
Richard C, Couture P, Charest A, Lamarche B. Effect of the Mediterranean diet with and without weight loss on cardiovascular risk factors in men with the metabolic syndrome. Nutr Metab Cardiovasc Dis. 2011;21:628–35.
Jones JL, Fernandez ML, McIntosh MS, Naim W, Calle MC. Kalynch c, et al. A Mediterranean-style low-glycemic-load diet improves variables of metabolic syndrome in women, and addition of a phytochemical-rich medical food enhances benefits on lipoprotein metabolism. J Clin Lipidol. 2011;5(3):188–96.
Bekkouche L, Bouchenak M, Malaisse WJ, Yahia DA. The Mediterranean diet adoption improves metabolic, oxidative, and inflammatory abnormalities in Algerian metabolic syndrome patients. Horm Metab Res. 2014;46:274–82.
Kastorini CM, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components. J Am Coll Cardiol. 2011;57:1299–313.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Khayef, G., Sabaté, J. (2016). Impact of Mediterranean Diet on Metabolic Syndrome. In: Romagnolo, D., Selmin, O. (eds) Mediterranean Diet. Nutrition and Health. Humana Press, Cham. https://doi.org/10.1007/978-3-319-27969-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-27969-5_9
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-27967-1
Online ISBN: 978-3-319-27969-5
eBook Packages: MedicineMedicine (R0)