Abstract
The primary function of the elbow is to position and stabilize the hand in space. It has been estimated that to obtain this, the required physiologic arc of movement is about 0–145° for extension and flexion, respectively, and of 70–85° for pronation and supination (Palastanga et al. 2006). Morrey et al. (1981) stated that, to perform the basic activity of daily living, a minimum arc of movement of 30–130° in extension and flexion and of 50–50° in pronation and supination is enough. A stiff elbow has been defined by Sojbjerg as one with a loss of extension greater than 30° and less than 120° of flexion (Sojbjerg 1996). From these data we must put our attention to the fact that a loss of terminal extension is less disabling than a loss of the same degree of terminal flexion: this will be important when we will deal with the rehabilitation program.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
The primary function of the elbow is to position and stabilize the hand in space. It has been estimated that to obtain this, the required physiologic arc of movement is about 0–145° for extension and flexion, respectively, and of 70–85° for pronation and supination (Palastanga et al. 2006). Morrey et al. (1981) stated that, to perform the basic activity of daily living, a minimum arc of movement of 30–130° in extension and flexion and of 50–50° in pronation and supination is enough. A stiff elbow has been defined by Sojbjerg as one with a loss of extension greater than 30° and less than 120° of flexion (Sojbjerg 1996). From these data we must put our attention to the fact that a loss of terminal extension is less disabling than a loss of the same degree of terminal flexion: this will be important when we will deal with the rehabilitation program.
It’s important to underline that elbow stiffness is poorly tolerated because of the lack of compensatory motions in adjacent joints. Therefore, it should not come as a surprise if some patients with particular occupational or recreational requests come to our attention requiring help and treatment even with articular limitation we judge of small amplitude.
It is very difficult to estimate the real incidence of this problem since, unfortunately, the elbow joint is prone to stiffness following a multitude of traumatic (including burns, head injury, and elbow surgery) and atraumatic (osteoarthritis and inflammatory joint disease, metabolic disease like in hemophiliacs, and congenital like arthrogryposis) etiologies.
Certainly, the most common cause among those aforementioned is elbow trauma. Not only trauma can directly alter the geometry of the joint, but it can also induce a number of secondary effects on the soft tissues around the elbow itself. Both situations can be further complicated by the formation of heterotopic ossification. Heterotopic ossifications commonly occur about the elbow in response to tissue trauma; these act as a physical block to elbow motion and might also create a synostosis between the radius and ulna, preventing forearm pronation/supination (Nandi et al. 2009).
Soft tissue contracture leads to stiffness by physically restricting elbow motion. These soft tissue changes typically occur with the bony pathology mentioned above because these situations are often followed by contracture of the articular capsule, collateral ligaments, and muscles (Sojbjerg et al. 2002).
When the skin covering the elbow is no longer supple following a burn, motion could be again compromised (Jupiter et al. 2003). But above all, one of the biggest changers trauma can induce in the joint capsule is represented by an increased number of myofibroblasts (i.e., fibroblasts with contractile ability) in its thickness. It has indeed demonstrated a significant correlation between joint range of motion and myofibroblast numbers, percentage of myofibroblast to total cells, and α-SMA (i.e., a contractile smooth muscle protein expressed by myofibroblast and therefore a myofibroblast marker) protein levels in the capsules of patients with post-traumatic joint contractures (Hildebrand et al. 2004).
Moreover, even if myofibroblastic proliferation occurs throughout the entire joint capsule, there seems to be a selectively greater increase of their number in the anterior part of the capsule compared to the posterior part. This is one of the reasons why most of elbow contractures occur in a flexed position (Germscheid and Hildebrand 2006).
In the same way, the anterior part of the post-traumatic joint capsule is an environment with high matrix turnover rates, which makes it much thicker than physiological (from 0.5 mm to 8 mm) with an extensive disorganization of the collagen fiber bundle arrangement. This is another reason explaining why the greater part of post-traumatic elbow contractures is in flexion (Hildebrand et al. 2005).
According to Morrey (2005), the high degree of congruity and complexity of the articular joint and the susceptibility of the tissues (particularly the capsule) to react to trauma are the two basic anatomic features that underlie the elbow loss of motion, but they’re not the only ones.
Indeed, another predisposing factor to elbow stiffness is the brachialis muscle. This muscle is broad and lies directly on the capsule as it crosses the elbow joint. It is highly vascularized, has no tendinous portion at this point, and, therefore, bleeds in response to trauma. Hematoma has been implicated as an inciting cause of heterotopic ossifications and subsequent capsular contracture (Husband and Hastings 1990). Moreover, the medial and lateral collateral ligaments are often injured in elbow fractures, dislocations, or even less traumatic injuries and have a propensity toward calcification (Weiss and Sachar 1994).
2 Clinical Evaluation
Patient coming to our attention with a stiff elbow needs to be carefully evaluated with an appropriate history and physical examination complemented by imaging studies.
During the medical visit, it is essential to understand the functional impact of the contracture on patient’s work or recreational activities, the way patient really lives this disability, and, above all, the compliance with rehabilitation or postoperative therapy. Everything must be investigated, with regard to both stiffness characteristics (onset, duration, clinical trend, prior treatments, etc.) and patient general health state (presence of comorbid conditions) and lifestyle in order to determine the level of demand that will be placed on the elbow. Usually the nature of the problem becomes clear from the history.
The etiology is usually post-traumatic. In these cases trauma dynamics, the presence of fractures, surgical treatment (approach, hardware presence, etc.), and immobilization time must be painstakingly evaluated.
If stiffness instead developed gradually by the years, we should try to understand if it was preceded by elbow pain, that the patient might have tried to mitigate at the expense of range of motion, with rigidity as a result of soft tissue contracture alone. This is the case of synovitis (rheumatic or neoplastic, mostly benign such as osteoid osteoma).
Differently, when stiffness has slow onset but with mild and sustainable pain, we must look for the cause in elbow cartilage damage and osteoarthritic changes (from loose bodies to osteophytes and intra-articular ossifications). These patients are usually heavy manual workers subject to repetitive mechanical stress which leads to the formation of anterior and posterior osteophytes, with progressive reduction of active and passive range of motion, as well as sportive patients with a history of unacknowledged osteochondritis dissecans or mild medial instability and repeated valgus stress during athletic activity.
If that is the case, the patient seeks our attention only when the range of motion limitation is so pronounced that it affects working or recreational activity; pain is usually minimum and supportable, mostly exacerbated by stretches over the permitted articular range.
Physical examination needs to include a complete evaluation of the entire upper limb involved and comparison with the contralateral. First, we can collect informations from the skin (burns, wounds, etc.). Active and passive elbow range of motion, for both flexion–extension and pronation–supination, should be examined with a goniometer, just as varus–valgus and rotational stability. Also, the quality of the end point is critical: the experienced examiner can often discern between a bony block and an advanced soft tissue contracture (Vardakas et al. 2002).
Motor strength and voluntary control of muscles in the upper limb should be carefully evaluated because an elbow with inadequate motor strength is unlikely to maintain motion after elbow release.
Fundamental is the neurovascular examination with particular attention to the ulnar nerve, which is commonly involved in elbow trauma and may require treatment at the time of surgery (King and Faber 2000).
3 Imaging
The first imaging studies to evaluate a stiff elbow should be plain radiographs, including anterior–posterior, lateral, and two oblique views (Nandi et al. 2009 ).
X-rays provide most of the informations regarding the cause and appropriate management of the contracture. In the event that we need further details, we can take advantage from the CT scan with two- and three-dimensional reconstructions (fundamental in heterotopic ossification study) or MRI if a soft tissue or synovial problem is suspected. Live fluoroscopy can be used to distinguish between a bony block and soft tissue contracture. An EMG could be necessary in cases of ulnar nerve impairment.
4 Etiology and Classification
Since the causes of elbow stiffness are so numerous, an etiology-based classification is an obvious first choice. It can be described as following:
-
Post-traumatic
-
Arthritis
-
Inflammatory
-
OA
-
Dysplasia, etc.
-
-
Neurogenic
-
Tumor
-
Others, etc. (burns, iatrogenic, etc.)
Each one of these disease can affect and reduce the range of motion due to internal and external articular damage.
Traditionally, elbow contractures are classified on the basis of the underlying pathology in extrinsic (e.g., thickening of the ligaments or heterotopic ossification), intrinsic (e.g., osteophyte formation or fracture malunion) and mixed, because since following intrinsic contractures patient may experience secondary contracture of the capsule, ligaments, and muscle of the elbow (Morrey 1990) (Table 30.1).
This is not a merely academic distinction but allows to choose the treatment for that elbow. As an example, it’s not possible to obtain motion improvement by passive manual stretching if we are facing an intrinsic stiffness.
Another useful stiffness classification is based on the severity: very severe (≤30°), severe (31–61°), moderate (61–91°), and poor (≥90°).
It’s important for the prognosis infact the worse is the stiffness the more difficult is gain the passive motion.
When we suggest the surgery, we have to remember that:
-
It’s impossible to guarantee the complete recovery also in more simple cases.
-
Patients with a poor stiffness have more high expectations and will be less satisfied with a partial joint recovery.
5 Conservative Treatment
The stiff elbow is challenging to treat, and thus, its prevention is of paramount importance.
Early identification and treatment of the base pathology, reducing immobilization as much as possible, precise re-education, and control of pain are the main principles to lower the risk of stiffness.
When stiffness already set in, we must find the most appropriate treatment. The conservative treatment is based on functional re-education, physical therapy, and use of splint and passive mobilization. This approach is mostly effective on soft tissue contracture without mechanical sources of stiffness. Actually, in most cases the soft tissue contracture worsens the stiffness caused by intrinsic or extrinsic joint alterations, such as heterotopic ossification. For this reason, a 3–6-month period of conservative treatment is still suggested before considering surgical treatment.
It is widely accepted as a severe or moderate post-traumatic stiffness can evolve, respectively, into a moderate or mild stiffness with conservative treatment alone. This can lead to make the stiffness much better tolerated by the patient (who might not wish for surgery anymore) or allow for a better outcome after the surgery if still needed.
The only exception is represented by the ulnar nerve irritation which can compromise the recovery of flexion movement. In the presence of dysaesthesia or paraesthesia during flexion manipulation, not regressing with rest and interfering with the re-education, an EMG is strongly suggested together with taking into consideration a neurolysis any time soon. More about this topic can be found in the rehabilitation section of this chapter.
6 Surgical Treatment (Open or Arthroscopic)
The surgical treatment for elbow stiffness is needed when the degree of rigidity left from the conservative treatment interferes with work/daily life activities of the patient. Pain and joint lockup during flexion–extension movement are suggestive of surgical indication.
In elbow pathology the diatribe between open and arthroscopic surgery is absent, since both techniques have advantages and disadvantages, often with comparable indications. The surgeon mastering both techniques is most likely to find the most useful and effective approach for each patient based on stiffness type and his own skills.
Arthroscopic techniques are, however, more difficult in cases of severe contracture or when previous surgeries have been undertaken, particularly when there is internal fixation in situ.
During preoperative timing, we must remind to the patient that stiffness, especially within the elbow, tends to recur (due to the new formation of heterotopic ossifications or soft tissue contracture) even when the surgical and rehabilitative treatments have been well performed and that almost 20% of the range of motion recovered after surgery can be lost again later.
This is especially true when initial stiffness and joint anatomical changes are more pronounced.
Another key element is patient’s motivation since he/she must be ready to undergo surgery and face the long re-educative course to reduce risk of recurrence or even worsening of initial stiffness.
We will now discuss elbow stiffness depending on its etiology.
7 Post-traumatic Elbow Stiffness
In a post-traumatic elbow stiffness, many elements need to be evaluated at the same time to decide the adequate treatment. Even for an expert and dedicated surgeon, it can be challenging to identify and define the algorithm he/she usually follows to define the best surgical treatment.
The existing classifications are descriptive, and they are not very useful to guide the type of treatment:
-
Cause (intrinsic and extrinsic)
-
Severity (very severe <30, severe from 30 to 60°, moderate from 61 to 90°, minimal >91°)
-
Involved movement (flexion–extension/pronation–supination)
We can identify four factors to decide the surgical treatment:
-
1.
Soft tissue contracture
-
2.
Arthritis
-
3.
Heterotopic ossification (HO)
-
4.
Malunion/nonunion
Different “surgery guiding factors” can be present at the same time in a single patient.
For example, a patient with distal humerus malunion can also present a secondary arthritis, HO, and soft tissue contracture.
However, one of the four elements is usually predominant and influences the choice of the treatment.
We propose the following classification (the SOD classification), an easy and effective way to guide the treatment (Table 30.2).
7.1 Prevalent Type of Stiffness: Soft Tissue Contracture
Stiffness is mainly due to a reduction of the joint space, with hypertrophic and anelastic capsule and ligaments. An anterior and posterior capsulectomy must be performed, saving the ulnar bundle of the lateral collateral ligament (LCL) and the anterior bundle of the medial collateral ligament (MCL).
This arthrolysis can be performed both arthroscopically and open. The neurolysis of the ulnar nerve must be performed if there’s any sign of chronic compression in the epithrocleo-olecranic groove or simply as a precaution when a recovery of over 30° is expected (to reduce the risk of postoperative neurapraxias). The subcutaneous anterior translocation of the ulnar nerve is rarely needed.
7.1.1 Arthroscopic Arthrolysis (Fig. 30.1)
The patient is in lateral decubitus or supine position, with pneumatic tourniquet at the proximal third of the arm. If needed, the neurolysis in the epithrocleo-olecranic groove can be performed with a small posteromedial incision.
Arthroscopic osteocapsular arthroplasty: arthroscopically is possible to manage anterior (a) and posterior (b) compartment by described portals. The stepwise sequence (get in, get ready, bone removal, and capsulectomy) is applied in each compartment to remove loose bodies/osteophytes (c) and the contracted capsule in order to improve the joint motion
Once the anatomic landmarks are done, 20–30 cc of saline solution are injected through the soft spot of the elbow (the space between olecranon tip, radial head, and the posterior edge of the lateral epicondyle).
We prefer to start with the anterior approach and access the joint through the anteromedial portal, while the instruments (shawer and radiofrequency ablator) are inserted through the anterolateral one.
The anterior joint space must be “recreated” removing the scar tissue from the articular surface and releasing the hypertrophic and anelastic capsule. The arthroscope and the instruments must switch places many times to complete the arthrolysis (from anteromedial to anterolateral and vice versa). An accessory portal (anterolateral or medial-proximal) as a tool to divaricate tissues during surgical maneuvering could be considered, but is not imperative.
Moving to the posterior approach, the accesses are posterior (trans-tricipital, about 3–4 cm from the olecranon tip) and posterior-lateral (close to the olecranon tip, where the end of the tricipital aponeurosis can be palpated). We suggest to initially insert the arthroscope through this last portal to work better and free the olecranon fossa from the scar tissue. Switching the instruments will allow to complete the arthrolysis on the posterolateral side. It is usually not necessary to reach for the posterior humeroradial joint as opposed to the osteocapsular arthrolysis that we will describe later on.
If the range of movement obtained is still not acceptable, the posterior bundle of the medial collateral ligament must be interrupted to obtain more flexion. This can be achieved in mini open surgery through the incision performed to free the ulnar nerve.
Anterior and posterior drains are set in place and will be removed about 48 h after surgery. The arm must be immobilized in extension with a cast, with pillow support, and with the hand kept 30 cm above the head for about 12–24 h, until the functional re-education begins.
Elbow arthroscopy is not recommended in patients who have undergone previous elbow procedures with changes to the normal anatomy.
Elbow arthroscopy after ulnar nerve transposition remains a relative contraindication. Steinmann et al. recommend extending the incision for the medial portal to identify and protect the nerve before inserting the arthroscope or instruments. An absolute contraindication for arthroscopic treatment of stiff elbows is a lack of experience with elbow arthroscopy. This procedure can be extremely difficult with a higher risk of nerve injury than other arthroscopic elbow procedures.
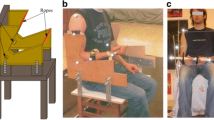
7.1.2 Open Arthrolysis (Fig. 30.2)
The patient is supine, with pneumatic tourniquet at the proximal third of the arm.
Open arthrolysis. Both anterior and posterior aspects of the joint can be visualized as well as by medial or lateral column procedures. The skin incision could be posterior (b) or direct medial (a) or lateral (c). Imperative is to avoid lesion to medial and lateral ligament. So we suggest the Hotchkiss approach (d) to reach the anterior (f) and posterior (g) camera for the medial column and the Kocher’s approach (e, h, i) for the lateral ones
A choice has to be made between a single long posterior incision and two shorter incisions on the medial and lateral epicondyle. In case of single incision, the skin flap must be large enough to reach the two columns, but it means any subsequent surgery (fractures, new arthrolysis, arthroplasty, etc.) will have to adopt the same access. Performing two incisions allows for a less aggressive surgery on the soft tissues, reducing the risk of necrosis of the skin flap and postoperative pain and swelling, therefore favoring a better outcome.
Independently of the incision choice, the ulnar nerve must be isolated in order to isolate the tendon of the triceps on the medial side and separate it from the posterior and posteromedial articular capsule. The same applies for the lateral side of the triceps in order to lift the muscle and its tendon. The posterior capsulectomy with the olecranon fossa cleaning is easily performed.
Once the posterior arthrolysis is finished, the anterior capsulectomy is next. Usually, either one of the two column procedures is sufficient. We suggest to start from the lateral side where the muscle is thinner. Through Kocher’s approach (which protects the LCL), the humeroradial joint is exposed.
It is necessary to disconnect the epicondylar muscles to uncover and remove the anterior articular capsule. If the range of motion is still not acceptable, we can move to the medial side, extending the release of the ulnar nerve inside the flexor carpi ulnaris (FCU). The superior part of the FCU together with the medial condylar muscles must be laterally reversed to uncover the anteromedial side of the articular capsule. Once the sublime tubercle is identified, which lays just below the point where the ulnar nerve enters the FCU, the anterior bundle of the medial collateral ligament has to be protected. Although a partial or even complete capsulectomy is often recommended, there is little evidence that the results are better when compared with a simple capsulotomy.
The medial and lateral condylar muscles must be carefully reinserted with transosseous stitches after an accurate hemostasis. Again two drains (anterior and posterior) are positioned, followed by compressive elastic bandage with fixing in extension.
7.2 Prevalent Type of Stiffness: Secondary Osteoarthritis
The secondary stiffness related to osteoarthritis can be roughly divided into two groups:
-
Mild or moderate stiffness, the joint line is preserved
The elbow is a joint able to develop a unique kind of osteoarthritis called “joint line sparring osteoarthritis.” Traditional osteoarthritis begins with cartilage depletion followed by subchondral geodes and osteophytes. In this case instead, we can observe the growth of large intra-articular osteophytes filling the distal humeral epiphysis fossas (for the coronoid, the radial head, and the olecranon) and enhancing the volume of the bone bulges (coronoid and olecranon). These osteophytes represent a mechanical obstacle to the articular movement. X-rays and CT scan show a preservation of the joint space indicating that, once the mechanical impediment is removed, the humeroulnar joint could recover and maintain a good range of movement.
An accurate CT scan reveals a more complex situation:
-
Frequent loose bodies in the anterior (between coronoid and its humeral fossa), posterior (between the olecranon and its fossa), and posterolateral (between the radial head and the capitulum) position
-
Ligaments’ insertion ossifications (humeral and ulnar LCL/MCL, ulnar anular ligament)
-
Osteophytosic deformation of the olecranon profile from medial to lateral (Mickey Mouse ears), of the coronoid profile, and of the radial head and capitulum (Lim et al. 2008)
It is not simple or trivial to identify the original shape and recompose it. For this reason we take advantage of 2D and 3D CT scan reconstructions (Nishiwaki et al. 2013) to help us plan the surgical treatment described as “osteocapsular arthrolysis.” In order to further improve the preoperative study, plastic models based on the 3D CT scan reconstruction can be produced (Fig. 30.3).
Post-traumatic intrinsic elbow contracture with a big osteochondral fragment inside the joint. The 3D model molded on the CT scan helps to better plan the surgery (open or arthroscopic arthrolysis). It is possible to notice the correspondence among CT scan, the 3D model (a), and the removed fragment (b)
The osteocapsular arthrolysis surgery can be performed both arthroscopically (arthroscopic osteocapsular arthrolysis) and open.
The AOA (Fig. 30.1) is similar to the arthroscopic arthrolysis previously described but much more challenging for the following reasons:
-
Entering the joint space, orienting the arthroscope and the instruments, setting up a working space, and identifying the anatomy are more arduous and therefore riskier.
-
Maintaining the joint space open is mandatory to remove loose bodies and osteophytes; it is therefore necessary to introduce a spatula through the accessory portals (proximal anterolateral, anteromedial, and posterolateral). It is not recommended to increase the inflow pressure of the arthroscopic pump.
-
It is necessary to perform the arthrolysis of the posterior humeroradial joint too. This is the most challenging site to work on; it must be explored from the posterolateral portal and the mediolateral portal (the soft spot).
-
Osteophyte removal must be performed ahead of the capsulectomy. We suggest to use an osteotome to dislodge the osteophytes making the loose bodies to remove. Only at the end that we perform the reshaping with burr of the osteophyte margins and of the articular fossas. The burr produces a large amount of debris that might be the cause of subsequent ossifications.
-
It is hard to decide how much bone to remove; it’s better to remember that the removal of 3 mm of abnormal bone from the olecranon tip will improve extension by approximately 15°, provided there is no other pathology.
-
The instruments must be switched from one portal to the other many times.
-
The ulnar nerve release is routinely executed with the aim of working more safely on the medial side and performing the release of the posterior bundle of medial collateral ligament which cannot be achieved arthroscopically.
-
The ulnar nerve may also be affected requiring decompression/transposition.
AOA can therefore only be used in selected cases, and the technique is demanding with a steep learning curve.
The open osteocapsular arthrolysis follows the same rules of the one described for the plain soft tissue contracture, except:
-
The exposition of the two columns is nearly mandatory to completely remove the osteophytes (Fig. 30.2).
-
If large osteophytes of the coronoid process are present, it’s advisable to perform the Hotchkiss approach instead of the FCU split.
-
Keep an articulated external fixator ready in case the joint resulted unstable because of iatrogenic collateral ligament resection (anelastic, retracted, and sometimes ossified).
The opportunity of a mixed technique must be kept in mind: anterior arthroscopic arthrolysis + posterior open arthrolysis. This to reduce, the aggressivity of the surgical approach to free the anterior camera. If posterior osteophytes are small and there is no need for ulnar nerve neurolysis, a small transtricipital access might be acceptable for exposing the olecranon fossa and the osteophytes of the medial and lateral side.
Once the surgery is over, the treatment continues the same way described for the soft tissue contracture arthrolysis.
There is an alternative surgery technique that is currently out of fashion but must be remembered since effective in some indications: it’s the Outerbridge–Kashiwagi (OK) technique.
By a triceps splitting approach, it is possible to obtain a wide view of the olecranon fossa. The anterior compartment can be accessed to a certain extent by creating a hole in the distal humerus, in the center of the olecranon fossa. The tip of the coronoid process can be debrided through the defect when the elbow is flexed. However, if sufficient release has not been achieved, a small additional incision can be made laterally and, if necessary, medially so that all compartments of the elbow joint can be reached.
-
Severe or very severe stiffness: The humeroulnar joint cartilage is completely depleted, and the subchondral bone emerges in the joint.
The humeroulnar joint is severely compromised. If the patient doesn’t complain about pain, surgical approach is not advised.
When the patient is more than 70 years old and has low functional requests, the total elbow arthroplasty (TEA) allows for a good recovery of the joint movement and resolution of the pain. However, the patient will have to closely follow the restriction imposed by the surgeon in order to reduce the risk of wear or mobilization of the prosthetic implant.
In younger manual working patients with painful incongruous joint surfaces and extensive intra-articular adhesions, only a salvage procedure is indicated. The so-called biologic interposition arthroplasty (Fig. 30.4) may require:
-
A complete lateral ligament complex/extensor origin release to be able to separate the joint surfaces and achieve an adequate exposure
-
Remolding the articular surface
-
Covering the trochlea and the greater sigmoid notch by omologus membrane (fascia lata, Achilles tendon, etc.)
-
An external fixator for at least 2 months for satisfactory correction
Biological interposition arthroplasty. (a) Pre-op range of motion and (b) X-ray evaluation. (c) Intraoperative joint dislocation and arthrolysis. (d) Fascia lata covering articular surface. (e) The ex–fix to protect stability during postoperative active motion. (f, g) X-ray evaluation and (h) range of motion 7 years after surgery
The aim of interposition arthroplasty is to reach a stable unpainful joint with an acceptable stiffness (around 50 degree of flexion–extension) in order to let the patients work again for a few years (Fig. 30.4).
7.3 Prevalent Type of Stiffness: Heterotopic Ossification
Heterotopic ossification is the formation of ectopic lamellar bone in soft tissues and is a poorly investigated sequela after trauma, brain injury, burns, or surgery. The disability incurred as a result of heterotopic ossification is quite variable.
The newly formed bone tissue follows the capsular bands and interstices between muscles, literally displacing the noble structures (nerves and vascular strands) as it grows. It is composed of mature new bone (lamellar under the microscope) and must not be confused with myositis ossificans (resulting from an intramuscular inflammatory process) or periarticular calcifications (amorphous calcium pyrophosphate collections without trabecular organization that is usually seen in the capsule and collateral ligaments).
These ossifications can either be very small or form bone bridges between the humerus and ulna or between the radius and ulna. They need to be isolated and removed in order to recover the movement.
The Hastings and Graham classification system uses clinical and radiographic data to categorize heterotopic ossification at the elbow into three classes (Hastings and Graham 1994) (Table 30.3).
Relying on the classification of forearm HO designed by Vince Miller, Jupiter and Ring (1998) subclassified Type I (proximal third) forearm synostosis into three types based on the location of ectopic bone: Type IIIA ectopic ossification is located at or distal to the bicipital tuberosity, Type IIIB involves the radial head and/or the proximal radioulnar joint, and Type IIIC is a proximal radioulnar synostosis. Viola and Hastings further subclassify forearm synostosis in: Subtype A, anterior involvement; Subtype B, posterior involvement; and Subtype C, intra-articular involvement of the proximal radioulnar joint (Viola and Hastings 2000) (Figs. 30.5 and 30.6).
Type I (proximal third) HO classification of forearm designed by Vince Miller, Jupiter, and Ring (1998) (Drawn by School of Anatomical Drawing, University of Bologna, Istituto Ortopedico Rizzoli). Type I ectopic ossification is located at or distal to the bicipital tuberosity, and Type II involves the radial head and/or the proximal radioulnar joint. Type III is a proximal radioulnar synostosis
Viola and Hastings further subclassify forearm synostosis (Viola and Hastings 2000) (Drawn by School of Anatomical Drawing, University of Bologna, Istituto Ortopedico Rizzoli): Subtype A, anterior involvement; Subtype B, posterior involvement; Subtype C, intra-articular involvement of the proximal radioulnar joint
HO have to be precisely classified on the based on the tac images and when they obstacle the joint movement have to be surgically removed. They are a relative contraindication to the arthroscopic arthrolysis every time nerves and vessels could be displaced by their presence. So open arthrolysis is the only possibility in most of the cases. Surgical approach is chosen case by case depending on the position and HO dimension. A preoperative CT scan is mandatory to schedule the procedure. In a few cases, a direct anterior approach is needed to remove the new bone formed among anterior cubital structures; also an external fixation could be necessary when it involves medial or lateral collateral ligament (Fig. 30.7).
Because of the possible recurrence, surgical excision of HO is usually delayed for 12 (6–18) months (from injury to operation) until the maturation of bone occurs knowing that clinical, laboratory, or radiographic indicators may not be reliable to reflect the state of HO. No guidelines have been published regarding the timing of removal, and the decisions remain on doctors’ experiences. Furthermore, less satisfactory function can be expected after too late excision because of soft tissue contracture and muscular atrophy.
After the removal, a prophylactic management strategy is necessary, even if nothing can guarantee a perfect result or the absence of a recurrence.
Studies have demonstrated that NSAIDs (indomethacin, 25 mg three times per day for three to 6 weeks, or Cox-2 inhibitors) and radiation (700 to 800 cGy in a single fraction from 24 h preoperatively until 48–72 h postoperatively) are quite effective preventing heterotopic ossification with no statistical differences.
7.4 Prevalent Type of Stiffness: Fracture Malunion/Nonunion
In case of an over-/intercondylar elbow fracture with stiffness at 6 months from conservative or surgical treatment, CT scan evaluation will be looking for signs of malunion or nonunion. If the fracture subverted, the shape of the trochlea stiffness is intrinsic, and surgery is not a viable solution. When throclea and capitulum are not distorted and the malunion only affects the inclination of the articular spool with respect to the longitudinal humeral axis, a corrective osteotomy can be considered. The approach will be triceps sparing in case of a single-plane osteotomy, while a TRAP approach or olecranon osteotomy will be needed in the event of a multiple-plane osteotomy (which is much more challenging). Once the osteotomy (closing wedge) is completed and an acceptable anatomy is restored, synthesis will be performed with one or two plates, parallel or at 90° (Fig. 30.8). The post-op period will be similar to the one described in the “Fractures” chapter.
Osteotomies are challenging procedures and we cannot guarantee any result to the patient; therefore, the indication must be extremely selective, case by case.
Nonunions or psudoarthrosis are extremely challenging situations too. First, the presence of infection has to be excluded via multiple blood culture, scintigraphy, and eventually antibiotic essay from an eco-guided fine needle aspiration. Once the infection is excluded, a curettage of the nonunion site must be performed in order to reach a bleeding bone surface. Matching surfaces and obtaining a stable synthesis often mean bone stock loss and alterations of the anatomy, inevitably affecting at least part of the range of movement.
There is an indication for TEA in patients over 70 with distal overcondylar pseudoarthrosis.
8 Arthritis
8.1 Primary Osteoarthritis
Primary osteoarthritis is related to a multifactorial genesis (familiarity, functional overload, mild instability, loose bodies, etc.).
It has been proved by mechanical studies that functional load spreads on the joint surface in a different way whether the articulation is in flexed or extended position (Rettig et al. 2008).
Work activity involving vibrating tools and sport activities with overhead throwing have different ways to put a strain on the humeroradial and humeroulnar joints.
The joint, slowly damaged over a long period of time, usually comes to our attention due to a progressive reduction of range of motion.
The distinction between arthritis with or without joint line preservation that we described for post-traumatic stiffness also applies for primary osteoarthritis, as well as for its treatment.
8.2 Inflammatory-Based Secondary Osteoarthrosis
Rheumatoid arthritis comes to our attention when conservative treatments cannot control pain anymore.
In the first stages, when the joint is not deformed but the hypertrophic synovial membrane reduces movements causing both a mechanical impediment and intense pain during flexion–extension, surgical synovectomy can provide a partial (and sometimes total) relief for an undetermined period of time (sometimes a few years).
Synovectomy can be performed arthroscopically as well as open. The more aggressive open surgery allows for better biopsies when needed to better typify the rheumatic disease. Arthroscopic surgery is not dissimilar from arthrolysis surgery, but it remains more delicate due to the weakness of the capsular component and the poor muscle mass of these patients (both factors that restrict the arthroscopic treatment to the expert surgeon, given the higher risk for neurovascular structures).
In the event that the joint is already severely compromised, total replacement is the only effective option, with all the known limitations.
8.3 Others (Neurogenic Elbow Stiffness, Tumor, Etc.)
Joint stiffness can have many other causes.
Since there is no room for an extensive coverage, we limit to a rare, but not so unusual, tumoral based cause of joint stiffness: the articular and periarticular osteoid osteoma.
It must be taken into consideration when the patient reports progressive worsening stiffness emerged with pain during months (sometimes years), stronger at night and well responding to NSAIDs.
NMR (if adequately powerful and executed) together with thin layer CT scan and Tc-99m whole-body scintigraphy usually allow for an accurate diagnosis.
Today, treatment is usually exclusive to the interventional radiology which, thanks to the CT scan-guided thermal ablation, is able to avoid the need of a surgical excision.
References
Germscheid NM, Hildebrand KA (2006) Regional variation is present in elbow capsules after injury. Clin Orthop Relat Res 450:219–224
Hastings H II, Graham TJ (1994) The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin 10(3):417–437
Hildebrand KA, Zhang M et al (2004) Myofibroblast numbers are elevated in human elbow capsules after trauma. Clin Orthop Relat Res 419:189–197
Hildebrand KA, Zhang M et al (2005) High rate of joint capsule matrix turnover in chronic human elbow contractures. Clin Orthop Relat Res 439:228–234
Husband JB, Hastings H II (1990) The lateral approach for operative release of posttraumatic contracture of the elbow. J Bone J Surg Am 72:1353–1358
Jupiter JB, Ring D (1998) Operative treatment of post-traumatic proximal radioulnar synostosis. J Bone Joint Surg 80A:248–257
Jupiter JB, O’Driscoll SW, Cohen MS (2003) The assessment and management of the stiff elbow. Instr Course Lect 52:93–111
King GJW, Faber KJ (2000) Posttraumatic elbow stiffness. Orthop Clin N Am 31(1):129–143
Lim YW, van Riet RP, Mittal R, Bain GI (2008) Pattern of osteophyte distribution in primary osteoarthritis of the elbow. Should Elb Surg 17(6):963–966
Morrey BF (1990) Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am 72:601–618
Morrey BF (2005) The posttraumatic stiff elbow. Clin Orthop Relat Res 431:26–35
Morrey BF, Askew RPT, An KN et al (1981) A biomechanical study of normal functional elbow motion. J Bone J Surg Am 63:872–876
Nandi S, Maschke S et al (2009) The stiff elbow. Hand (N Y) 4(4):368–379. doi:10.1007/s11552-009-9181-z
Nishiwaki M, Willing R, Johnson JA, King GJ, Athwal GS (2013) Identifying the location and volume of bony impingement in elbow osteoarthritis by 3-dimensional computational modeling. J Hand Surg [Am] 38(7):1370–1376. doi:10.1016/j.jhsa.2013.03.035
Palastanga NP, Field D, Soames R, American Society for Surgery of the Hand (2006) Anatomy and human movement: structure and function, 5th edn. Butterworth Heinemann, Inc., London, p 717. isbn:0-7506-8814-9
Rettig LA, Hastings H II, Feinberg JR (2008) Primary osteoarthritis of the elbow: lack of radiographic evidence for morphologic predisposition, results of operative debridement at intermediate follow-up, and basis for a new radiographic classification system. J Shoulder Elb Surg 17(1):97–105
Sojbjerg JO (1996) The stiff elbow. Acta Orthop Scand 67(6):626–631
Sojbjerg JO, Vardakas DG, Varitimidis SE, Goebel F, Vogt MT, Sotereanos DG (2002) Evaluating and treating the stiff elbow. Hand Clin 18(1):77–85
Vardakas DG, Varitimidis SE, Goebel F et al (2002) Evaluating and treating the stiff elbow. Hand Clin 18:77–85
Viola RW, Hastings H II (2000) Treatment of ectopic ossification about the elbow. Clin Orthop Relat Res 370:65–86
Weiss AP, Sachar K (1994) Soft tissue contractures about the elbow. Hand Clin 10(3):439–451
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Guerra, E., Marinelli, A., Rotini, M. (2018). Elbow Stiffness. In: Porcellini, G., Rotini, R., Stignani Kantar, S., Di Giacomo, S. (eds) The Elbow. Springer, Cham. https://doi.org/10.1007/978-3-319-27805-6_30
Download citation
DOI: https://doi.org/10.1007/978-3-319-27805-6_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-27803-2
Online ISBN: 978-3-319-27805-6
eBook Packages: MedicineMedicine (R0)