Abstract
Polycythemia vera (PV; polycythemia rubra vera) is a chronic myeloproliferative neoplasm characterized by increased red blood cell production independent of normal regulatory mechanisms. The majority of patients with PV show the JAK2V617F mutation or another functional similar JAK mutation. In fully developed disease, there is hepatomegaly associated with hyperemia and eventually signs of hepatic infarcts. Histologically, the sinusoids are dilated and filled with erythrocytes which can form stacks or “rouleaus.” PV is complicated by hepatic venous outflow disorders, in particular hepatic vein thrombosis with Budd-Chiari syndrome, sometimes associated with factor V Leiden mutation. Portal vein thrombosis is a well-documented complication of PV. These hepatic blood flow disorders are frequently followed by nodular regenerative hyperplasia. PV can also cause perisinusoidal fibrosis with an increase in reticulin and fibrotic changes of the liver related to necrosis and infarction.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Hepatic Vein
- Portal Vein Thrombosis
- Polycythemia Vera
- Essential Thrombocythemia
- Myeloproliferative Disorder
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Polycythemia Vera
ICD-O Code 9950/3
Introduction
The 2008 WHO classification defines polycythemia vera (polycythemia rubra vera; PV; formerly also termed “plethora vera”) as a chronic myeloproliferative neoplasm characterized by increased red blood cell production independent of normal regulatory mechanisms. Practically all patients with PV harbor the JAK2V617F mutation or another functional similar JAK mutation, resulting in proliferation of all hematopoietic cell lineages (“panmyelosis”).
PV was first described by Vaquez, and Osler recognized it as a “new clinical entity” characterized by chronic cyanosis and polycythemia, hence using the term still employed today (Vaquez 1892; Osler 1903; review: Means 2008). PV is characterized by the insidious onset of erythroid proliferation (erythrocytosis) and secondary platelet and granulocyte overproduction; it can progress from a proliferative stage to a “metastatic” phase and further develop into a clinically malignant phase (Golden 2003; Gilbert 2003). In 1967, the Polycythemia Vera Study Group (PVSG) was organized to identify the optimal approach to diagnosis of PV (Table 1).
In modern classifications, three phases of PV may be recognized: (1) a prepolycythemic or prodromal phase with borderline to only mild erythrocytosis; (2) an overt polycythemic phase, characterized by a significantly increased red cell mass; and (3) a “spent” or post-polycythemic myelofibrosis phase, in which cytopenias, including anemia, are associated with bone marrow fibrosis, extramedullary hematopoiesis, and hypersplenism. PV can also evolve into myelodysplasia and acute leukemia.
Epidemiology
The disease is rare, with an estimated incidence of 2.3 per 100,000; it is more frequent in males and usually affects older individuals, although cases in young adults and children have been reported (Tefferi 2001). In a large retrospective study examining all in- and outpatient records of Olmsted County, Minnesota, over a period of 55 years, the incidence rate of PV was 1.9 per 100,000 persons and year, and incidence rates increased with advancing age for men up to 23.5 per 100,000 and year, the median age at presentation being 55–60 years (Ania et al. 1994).
Clinical Features
PV is a chronic myeloproliferative disorder characterized by panmyelosis, splenomegaly, and a predisposition to vascular thrombosis, myelofibrosis, and acute leukemia. Basically, it represents a clonal stem cell disease with persistently increased erythrocyte production and is the only known type of primary acquired polycythemia (reviews: Berlin and Wasserman 1997; Streiff et al. 2002; Golden 2003; Tefferi 2003).
Liver Pathology in Polycythemia Vera
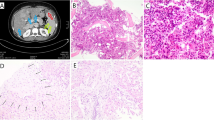
Macroscopy
A part of patients with PV show hepatomegaly. In fully developed disease, the enlarged and engorged liver shows a cut surface which is dark-red or gray-blue, sometimes with small nodular regenerates. In fresh state, cutting through the organ is followed by copious oozing of blood from the cut surface, sometimes intermingled with small granules of coagulated blood or thrombi (Hirschfeld 1906; Hamilton and Morse 1912; Mosse 1920). The liver capsule can show scarred depressions, probably sequelae of previous infarctions caused by venous thrombosis.
Histopathology
The sinusoids are markedly dilated and filled with erythrocytes which can form stacks or develop rouleau formation. A part of the sinusoids are so densely packed with red blood cells that the endothelial lining is no longer visible, the perisinusoidal space of Disse is effaced or compressed, and hepatocyte plates have undergone atrophy. Erythrocytes may enter the space of Disse, mimicking so-called Disse space hemorrhage. A slight increase of reticulin fibers may occur in the perisinusoidal space. Engorged vessels are also found in the portal tracts. In case of PV with myelofibrosis and myeloid metaplasia, there may be hepatic enlargement with extensive extramedullary hematopoiesis with dilatation of sinusoids, compression of hepatocyte plates, and hepatocyte atrophy and dysfunction, resulting in acute hepatic failure (McBrine et al. 1980).
Hepatic Venous Outflow Disorders in PV
Hepatic venous outflow disorders, and mainly Budd-Chiari syndrome (BCS) , occur as a complication of several types of myeloproliferative disorders (Poreddy and DeLeve 2002). As they are specifically well known for patients suffering from PV, these disorders are discussed in this paragraph. The BCS results from thrombogenic conditions and is caused by stenosis or obstruction of the hepatic venous outflow at the level of the hepatic veins and/or of the suprahepatic part of the inferior caval vein (Sherlock and Dooley 1993; Dilawari et al. 1994; Mahmoud et al. 1996; Valla 2002). The level of obstruction is reflected by two chief forms of BCS. The acute syndrome is invariably associated with extensive blockage of the major hepatic veins, and in a small fraction of patients, the caval vein is also occluded. Acute BCS causes a characteristic liver pathology with massive congestion and necrosis. In contrast, the chronic form of BCS is characterized by portal venous hypertension and a variably abnormal vasculature (Dilawari et al. 1994; Tilanus 1995; Iwai et al. 1998). On the other hand, it has been proposed to classify hepatic venous outflow disorders caused by thrombosis into two groups, the first representing “classical” BCS that is more common in the West and the second representing an obliterative disease predominantly affecting the hepatic portion of the inferior vena cava (“obliterative hepato-cavopathy”), the latter being predominant in developing countries and being “idiopathic” or then being associated with hepatocellular carcinoma (Okuda et al. 1995, 1998; Okuda 2002). A more recent expert panel classifies BCS on the one hand according to etiology (primary vs. secondary forms) and on the other hand according to the site of obstruction (small hepatic veins, large hepatic veins, inferior vena cava. and combined obstruction) (Janssen et al. 2003).
Pathogenically, BCS probably represents a spectrum of disease caused primarily by a hypercoagulable state and eventually promoted by vascular changes favoring local thrombosis, e.g., malignant tumors in the liver. Membranous obstruction (web) of the caval vein (MOVC) has formerly been regarded as a congenital alteration sometimes causing BCS, but is currently considered to be a sequela to thrombosis (Kage et al. 1992). However, a significant fraction of patients with BCS have no identifiable underlying condition, the percentage ranging from 13 % to 62 % in several studies (Hadengue et al. 1994; Slakey et al. 2001). Apart from PV, BCS developing as a complication of MPD is established for CML (Picardi et al. 2000).
The association of BCS and PV is well established for a long time (Chini 1954; Brown et al. 1955; Caroli and Soulier 1956; Cantwell et al. 1956; Chlumsky and Chlumska 1966; Siguier et al. 1967; Thomas and Caroli 1971; Retzlaff and Monge 1973; Balique 1981; Fechtner and DelDuca 1994). In one study on BCS, overt PV was the underlying cause in about 10 % of the cases, and essential thrombocythemia and chronic idiopathic myelofibrosis in only a very few (De Stefano et al. 1997). BCS associated with PV has also been observed in children from families with familial PV (Cario et al. 2003). Hepatic venous thrombosis in patients with PV is induced by other disorders with a genetic background, such as the factor V Leiden mutation and other thrombophilic coagulation disorders (Janssen 2000; Mohanty et al. 2001). It was shown that the factor V Leiden mutation is in fact the second most common etiology associated with BCS (Mahmoud et al. 1997; Delarive and Gonvers 1998; Simsek et al. 2000; Janssen et al. 2000; Deltenre et al. 2001), whereas other genetic disorders of thrombophilic factors are rarer causes of BCS (e.g., the G20210A mutation of the prothrombin gene; Poort et al. 1996; Bucciarelli et al. 1998; De Stefano et al. 1998; Oner et al. 1999; Minnema et al. 2000; Brancaccio et al. 2002). It has been observed that fulminant BCS in PV was associated with factor V Leiden mutation ( Akyildiz et al. 2006).
Portal Vein and/or Splanchnic Vein Thrombosis in Polycythemia Vera
The etiology of portal vein thrombosis (PVT) is heterogeneous, but important primary risk factors comprise cirrhosis, hepatobiliary malignancies, pancreatitis, and several disorders of the coagulation system (Mahmoud et al. 1997; review: Janssen 2000; Janssen et al. 2000). PVT is a well-documented complication of PV in its overt, masked, or early forms (Lommel 1906; Kratzeisen 1923; Alford et al. 1968; Valla et al. 1988; Drenou et al. 1992; Pati et al. 1998; Escher and Demarmels Biasiutti 1999; Randi et al. 2002). On the other hand, PVT is also known to be itself a complication of BCS that can be caused by PV. PVT, apart from its perfusion disorder of the liver, can cause compression of the bile duct in PV (Löhr et al. 1993). PV T in PV can be complicated by pylothrombophlebitis.
Why Is PV Associated with Thrombosis of Large Veins?
Thrombotic events are present in 20–50 % of patients with PCV at diagnosis and involve both large vessels and the microcirculation. It is estimated that the incidence of thrombosis is higher in PV than in essential thrombocythemia, and significant risk factors are increasing age and previous thrombosis (Orlandi et al. 1989; Pearson 2002). The pathogenic mechanisms underlying the increased incidence of thrombotic events in PV are still somewhat illusive. Prothrombotic factors such as an increased blood viscosity caused by an elevated hematocrit, abnormal platelet functions, and the procoagulative action of the cells involved have been proposed (Fields and Freeman 1993; Fiessinger 1994; Michiels 1997; Barbui and Finazzi 1997; Gumina et al. 2002; Friess et al. 2003). It has been shown that thrombocytes form heterotypic aggregates with leukocytes (platelet-neutrophil complexes; PNC) through platelet CD62P and leukocyte beta2-integrins, resulting in cell features with increased adhesion (Peters et al. 1999). A platelet-leukocyte conjugate formation occurring in myeloproliferative disorders, including PV, seems to indicate platelet activation, associated with platelet microparticle production serving as catalytic surfaces for thrombin generation (Villmow et al. 2002). In BCS or portal vein thrombosis, an increased expression of CD11b on neutrophils was detected, supporting a role for neutrophils in hepatic venous thrombosis (Alvarez-Larran et al. 2004). Increased CD11/CD18 expression on neutrophils is also found in essential thrombocythemia (Burgaleta et al. 2002). In addition, there is an “endothelial factor” in the pathogenic cascade of PV-associated thrombosis. PV seems to cause endothelial dysfunction in the preclinical phase of arterial disease, characterized by impaired flow-mediated vasodilatation (Neunteufl et al. 2001). On the other hand, there are findings indicating that hepatic erythropoietin production occurs in the acute phase of BCS and suggesting that, in some cases of BCS, erythrocytosis which resolves after the acute phase may be secondary to liver disease (Levy et al. 1985). A new line of thinking in regard to factors promoting thrombogenesis in PV and other myeloproliferative disorders is the pathogenic role of the JAK2V617F mutation in PV (Patel et al. 2006; Sozer et al. 2009; Benedik-Dolnicar et al. 2012; de Grandis et al. 2012; Yonal et al. 2012). This issue is discussed in more detail in the chapter on essential thrombocythemia.
Nodular Regenerative Hyperplasia in PV
Subacute or chronic BCS can result in a distinct hepatocyte response characterized by the production of numerous hepatocyte nodules not encircled by collagen fibers, but compressing the adjacent parenchyma. This is nodular regenerative hyperplasia (NRH) of the liver, occurring in several myeloproliferative disorders associated with hepatic venopathies and being a cause of portal hypertension (Al-Mukhaizeem et al. 2004). NRH is characterized by multiple enhancing nodules in CT during the hepatic arterial and portal venous phases and by hyperintense nodules in MR on T1-weighted images and hypointense or isointense nodules on T2-weighted images (Castellano et al. 1989; De Sousa et al. 1991; Wanless 1994; Clouet et al. 1999; Rha et al. 2000; Soler et al. 2000). NRH is discussed in more detail in another chapter. Even though NRH with small regenerative nodules may mimic multiple small metastases in the liver or produce a pseudotumoral presentation (Casillas et al. 1997; Clouet et al. 1999), a more difficult differential diagnostic situation arises in case of larger nodular lesions developing in the liver in chronic BCS. They include large regenerative (macroregenerative) nodules (that are mostly smaller than 4 cm) (Tanaka and Wanless 1998; Vilgrain et al. 1999; Zhou et al. 2000; Brancatelli et al. 2002; Ibarrola et al. 2004), adenomatous hyperplastic nodules (according to the older nomenclature; Soyer et al. 1993), FNH and FNH-like lesions (Schilling et al. 2000; Maetani et al. 2002; Ibarrola et al. 2004), and hepatocellular carcinoma, whereby the latter seems to be more frequent in patients with MOVC (Simson 1982; Nakamura and Takezawa 1982; Kew et al. 1989; Takayasu et al. 1994; Katoh and Shigematsu 1999; Havlioglu et al. 2003; Jang et al. 2003). In BCS, tumorous hepatic lesions may be mimicked by hemorrhagic necroses producing a mass (Shapiro et al. 1993).
Hepatic Fibrosis in PV
Apart from nodular lesions sometimes mimicking neoplastic disease, the liver in PV-associated BCS can undergo marked remodeling associated with fibrosis (Gundling et al. 2004). Severe hepatic fibrosis develops in BCS with a variety of histologic patterns. First, a part of the livers show a pattern of cirrhosis in which there is fibrous bridging between hepatic veins and the portal tracts (the so-called veno-portal cirrhosis); second, some livers in BCS exhibit a pattern of so-called reversed-lobulation cirrhosis (veno-centric cirrhosis), in which fibrous bridging between hepatic veins and portal tracts is minimal (Tanaka and Wanless 1998). In one study, all livers with veno-portal cirrhosis had severe portal vein obliteration, not seen to this degree in the other type of cirrhosis or in mixed forms, suggesting that portal vein obliteration in BCS plays a role in the pathogenesis of veno-portal bridging fibrosis (Tanaka and Wanless 1998). In the latter study, 9/15 BCS livers with these types of cirrhosis also showed large regenerative nodules histologically resembling focal nodular hyperplasia, also reported in another study (Schilling et al. 2000). In addition, fibrogenesis in PV may be mediated by activated JAK2-induced expression of galectin-3, known to involved in fibrosis and angiogenesis (Koopmans et al. 2012).
Portal Hypertension in PV and Other Hematological Disorders
As in other myeloproliferative disorders, portal hypertension may occur in PV, and not only due to thrombosis of large hepatic veins. The pathogenic mechanisms have been discussed in detail (Al-Mukhaizeem et al. 2004). These authors proposed to classify the pathogenic pathways as a function of the anatomical site(s) of the hematologic disorders’ manifestations. A first prehepatic (presinusoidal) cause of portal hypertension is, above all, portal vein and other splanchnic vein thrombosis. A second presinusoidal cause includes nodular regenerative hyperplasia of the liver, occurring in myeloproliferative disorders. Intrahepatic or sinusoidal blockage resulting in portal hypertension in myeloproliferative disorders is caused by extramedullary hemopoiesis, infiltration by abnormal hematopoietic cells, perisinusoidal fibrosis induced by hemopoietic cells located to the sinusoidal compartment (particularly fibrogenic megakaryocytes), nodular regenerative hyperplasia, liver cirrhosis, and amyloidosis. Postsinusoidal causes of portal hypertension comprise hepatic venous outflow disorders, as discussed above, and heart failure, e.g., owing to cardiac iron overload or amyloidosis.
PV can be associated with, or cause, acute obliterative endophlebitis of hepatic veins, lesions that can cause sinusoidal blockade and non-cirrhotic portal hypertension (Mandelbaum et al. 1953) .
Liver Cancer in Polycythemia Vera
Several reports document the association of erythrocytosis/polyglobulia with hepatocellular carcinoma (HCC) . In fact, erythrocytosis is one of the most common of the paraneoplastic syndromes in HCC, with an estimated incidence ranging from 2.2 % to 12 % (McFadzean et al. 1958; Jacobson et al. 1978; Sawabe et al. 1993; Chu et al. 1999; Trotter et al. 2002; Argumanis et al. 2002). From the etiologic point of view, at least four situations of this association have to be considered. The first situation refers to patients having bona fide PV and HCC (Toth and Bilodeau 1980; Gensini and Conti 2002). The second situation is characterized by HCCs thought to produce, or have been documented to produce, erythropoietin with secondary erythrocytosis (direct evidence: Funakoshi et al. 1993; Sakisaka et al. 1993; Muta et al. 1994; Matsuyama et al. 2000); (indirect evidence: McFadzean et al. 1958; Kan et al. 1961; Conte et al. 1964; Baume et al. 1965; Brownstein and Ballard 1966; McFadzean et al. 1967; Santer et al. 1967; Ruvidic and Ivaneski 1970; Zlatkina and Shcherbak 1970; Gordon et al. 1970; Nakai et al. 1972; Lizzi et al. 1973; Scott and Theologides 1974; Davidson 1976; Cornet et al. 1978; Jacobson et al. 1978; Okazaki et al. 1979; Kawasaki et al. 1979; Watanobe 1988; Shchekochikhin and Osipova 1991; Sawabe et al. 1993; Huang et al. 1994; Argumanis et al. 2002; Cheng et al. 2002). Of pathophysiologic interest are those situations where both elevated serum erythropoietin and erythrocytosis regressed after HCC resection (Regimbeau et al. 1999). Furthermore, erythropoietin production by HCCs seems to increase in response to hypoxia, for example, hepatic release of erythropoietin increases subsequent to chemoembolization of HCC (Pirisi et al. 1995). It has to be emphasized that elevated erythropoietin levels in patients with HCC may also be due to decreased erythropoietin clearance caused by underlying liver disease (Malaguarnera et al. 1996). An excess synthesis of erythropoietin by tumors was demonstrated in mice with spontaneous HCCs (Horiouchi et al. 1997). The third situation are patients developing HCC in the context of a hepatic venous outflow disorder, including BCS induced by PV (Havlioglu et al. 2003). Overall, HCC is rare in cases of hepatic venous outflow obstruction without concurrent thrombosis of the vena cava (Valla 2002). In fact, it is well known that HCC is a sequela of MOVC, but the incidence of HCC in MOVC varies according to geography (Simson 1982; Okuda 1982; Nakamura and Takezawa 1982; Rector et al. 1985; Kew et al. 1989; Hautekeete et al. 1990; Kage et al. 1992; Shrestha et al. 1996; Seo et al. 1998; Okuda et al. 1998; Karia et al. 2000). The fourth situation is represented by patients with PV exhibiting HCC after treatment, e.g., with radioactive phosphorus (Chudecki 1972), although a causal relationship has not been proven. The clinical triad of erythrocytosis, hemochromatosis, and hepatocellular carcinoma has been reported several times, this combination principally being found in elderly males (Lizzi et al. 1973; Scott and Theologides 1974; Raphael et al. 1979). Erythrocytosis in this situation has again been proposed to be caused by the action of erythropoietin derived from HCC. As HCC is a frequent complication of hemochromatosis, such a constellation might be expected to occur.
Cytogenetic and Molecular Features
About 20 % of patients show karyotypic abnormalities, including +8, +9, del(20q), del(13q), and del(9p). The most frequent molecular abnormality in PV is the gain-of-function mutation JAK2V617 F, occurring in more than 95 % of PV patients (Scott et al. 2007; Scott 2011). This mutation is not specific for PV but also occurs in other myeloproliferative disorders, including idiopathic myelofibrosis and essential thrombocythemia. The reason for this is that the mutation is manifest in a hematopoietic stem cell and is therefore transmitted to all cell lineages derived thereof. The remaining few % of patients show other mutations of JAK with the same functional consequences. Activation of JAK2 (Janus kinase 2), which phosphorylates signal transducer activator of transcription (STAT), promotes overexpression of the cell cycle regulator CDC25A (Gautier et al. 2012) and upregulates a broad array of growth factors, including VEGF, which may be responsible for angiogenesis in PV and other myeloproliferative disorders.
Pathogenic Pathways
The pathogenic mechanisms of PV are not fully understood, but the defect seems to involve hyperresponsiveness of PV progenitor cells to several cytokines (Prchal 2001). Diagnostic criteria and aspects of classification and molecular biology have been reviewed (Michiels and Juvonen 1997; Pearson 1998; Messinezy and Pearson 1999; Prchal and Prchal 1999; Golden 2003; Prchal 2003). It is known that patients with PV exhibit higher levels of a hemopoietic receptor, polycythemia rubra vera-1 (PRV-1) , in granulocytes/neutrophils, and it was proposed that this phenomenon provides a rapid, highly specific, and sensitive marker for the diagnosis of PV in comparison with nonneoplastic erythrocytoses (Klippel et al. 2003). However, another group found that the PRV-1 gene is constitutively expressed by bone marrow cells and does not discriminate PV from reactive and other chronic myeloproliferative disorders (Bock et al. 2003), whereas a more recent investigation confirmed that neutrophil PRV-1 upregulation is a characteristic feature of PV, although in itself not sufficient for the diagnosis of PV (Tefferi et al. 2004). One reason for this is that overexpression of the PRV-1 receptor is also found in other myeloproliferative disorders, e.g., essential thrombocythemia (Teofili et al. 2002). The PRV-1 gene encodes an open reading frame of 437 amino acids, containing a signal peptide and two cysteine-rich domains homologous to those found in the uPAR/Ly6/CD59/snake toxin-receptor superfamily, linked to the cell surface via a glycosylphosphatidylinositol (GPI) link (Temerinac et al. 2000; Klippel et al. 2002).
So-called Chronic Erythroid Leukemia
Introduction
This is a rare and heterogeneous group of intriguing disorders that have not yet been classified in a satisfactory way but has already been described by Di Guglielmo and a coworker (Di Guglielmo and Quattrin 1942). In fact, the term does not appear in modern classifications of leukemias and myeloproliferative disorders. The disorder is briefly discussed because the term appears in literature referring to liver involvement, and at least some of these leukemias seem to have a link to the respective acute leukemia forms. Based on the stem cell nature of the disorders, the beginning and evolution of this subset of leukemias are variable. For example, patients may first present with chronic erythroleukemia with refractory anemia, to later switch to acute erythroid leukemia (M6), and then to acute myeloid leukemia of the M0 type, also involving dysplastic features of other hemopoietic lineages, and therefore suggesting a stage-by-stage trilineage continuum (Michiels et al. 1997). There are several synonyms to denote disorders that are, or have been, interpreted to be chronic neoplastic erythroproliferative diseases. They include chronic erythroleukemia, chronic erythremia, chronic erythremic myelosis, chronic erythremic disease, chronic erythromyelosis, chronic Di Guglielmo syndrome, Di Guglielmo’s erythremia with prolonged course, primary chronic erythroblastosis, and Heilmeyer-Schöner disease (Heilmeyer and Schöner 1961; Starcich et al. 1963; Introzzi and Buscarini 1966; Thurm et al. 1967; Spremolla et al. 1970; Stewart 1971; Marsan et al. 1973; Kass 1975; Nunnensiek et al. 1976; Sroczynski and Hrycek 1976; Pivnik et al. 1987; Bindi et al. 1999). Heilmeyer and Schöner described the disorder having their eponyms under the term chronic pure erythroblastosis of the adult as a leukemic process going in parallel to the erythrocytic system (Heilmeyer and Schöner 1961). All or most of these manifestations of hematologic neoplasias seem to have in common a chronically persistent malignant proliferation of cell populations dominated by an erythroid lineage, although it has not been specified as to what percentage of erythroid cells must be involved and what exactly “chronic” means.
In chronic erythroid leukemia, the morphology of blast cells has been studied in detail, particularly in regard to the erythroblastic components. Erythroblasts can show several anomalies, including deviations between cytoplasmic baso- or eosinophilia and the nuclear chromatin features, and binucleated or trinucleated cells (Introzzi and Buscarini 1966). Ultrastructurally, the cells of interest may show cytoplasmic vacuolation and vesicular bodies and may display significant numbers of membrane-bound ferritin particles and also isolated ferritin crystals in the cytoplasm (Introzzi and Buscarini 1966).
Liver Involvement
There are only sparse data available in regard to liver involvement in chronic erythroid leukemia(s). In one patient, tumorous lesions containing erythroid cells (“erythrosarcomas”) were found in several organs, including the liver (Pivnik et al. 1987). Another case was characterized by the development of, as it was called, “malignant erythroblastomas” (Goreczky and Toth 1967). The autopsy of a patient with acute erythroid leukemia transforming in chronic erythremia revealed hepatomegaly (2,700 g) with increased consistency of the organ and grayish or hemorrhagic areas. Histologically, the portal tracts and the sinusoids were densely infiltrated by abnormal blastic cells, causing atrophy and dissolution of the liver cell plates. In the portal tracts, blast also occupied alterations looking like interface lesions/piecemeal necroses. The hepatocytes showed iron overload (Starcich et al. 1963; with a histologic figure of the liver changes).
References
Akyildiz M, Karasu Z, Dheir H, Osmanoglu N, Akay S, Ilter T (2006) Fulminant Budd-Chiari syndrome associated with polycythemia rubra vera and factor V Leiden mutation. Eur J Intern Med 17:66–67
Alford FP, Myers KA, Syme J (1968) Portal hypertension and bleeding varices due to thrombosis in the portal venous system complicating polycythaemia vera. Med J Aust 2:64–66
Al-Mukhaizeem KA, Rosenberg A, Sherker AH (2004) Nodular regenerative hyperplasia of the liver: an under-recognized cause of portal hypertension in hematological disorders. Am J Hematol 75:225–230
Alvarez-Larran A, Garcia-Pagan JC, Abraldes JG, Arellano E, Reverter JC, Bosch J, Cervantes F (2004) Increased CD11b neutrophil expression in Budd-Chiari syndrome or portal vein thrombosis secondary to polycythemia vera. Br J Haematol 124:329–335
Ania BJ, Suman VJ, Sobell JL, Codd MB, Silverstein MN, Melton LJ (1994) Trends in the incidence of polycythemia vera among Olmsted County, Minnesota residents, 1935–1989. Am J Hematol 47:89–93
Argumanis E, Quispe D, Ruiz E (2002) Erythrocytosis associated with hepatocellular carcinoma. Two case reports (in Spanish). Rev Gastroenterol Peru 22:84–87
Balique JG (1981) Budd-Chiari syndrome. Physiopathogenic hypothesis for polycythemia (in French). Nouv Presse Med 10:907–908
Barbui T, Finazzi G (1997) Risk factors and prevention of vascular complications in polycythemia vera. Semin Thromb Hemost 23:455–461
Baume P, Piper DW, Cumberland VH, Jones KO (1965) Primary hepatoma associated with polycythemia: report of a case with a study of tumour and urine erythropoietin levels. Med J Aust 2:833–835
Benedik-Dolnicar M, Homan M, Brecelj J (2012) JAK2V617F mutation in a 9-year-old girl with polycythemia vera and Budd-Chiari syndrome: a case report. J Pediatr Hematol Oncol 34:243–244
Berlin NI, Wasserman LR (1997) Polycythemia vera: a retrospective and reprise. J Lab Clin Med 130:365–373
Bindi M, Quartieri F, Siuti E, Stefanelli A, Mechelli S, Castiglioni MG (1999) Chronic erythremic myelosis (or chronic form of Di Guglielmo’s disease). A case report (in Italian). Recenti Prog Med 90:213–215
Bock O, Serinsoz E, Neusch M, Schlue J, Kreipe H (2003) The polycythaemia rubra vera-1 gene is constitutively expressed by bone marrow cells and does not discriminate polycythaemia vera from reactive and other chronic myeloproliferative disorders. Br J Haematol 123:472–474
Brancaccio V, Iannaccone L, Margaglione M, Guardascione MA, Amitrano L (2002) Multiple thrombophilic factors in a patient with Budd-Chiari syndrome. Clin Lab Haematol 24:61–63
Brancatelli G, Federle MP, Grazioli L, Golfieri R, Lecnioni R (2002) Benign regenerative nodules in Budd-Chiari syndrome and other vascular disorders of the liver: radiologic-pathologic and clinical correlation. Radiographics 22:847–862
Brown RN, Pidgeon JW, Johnson HA (1955) The Budd-Chiari syndrome complicating a case of polycythemia vera. Calif Med 83:37–39
Brownstein MH, Ballard HS (1966) Hepatoma associated with erythrocytosis. Am J Med 40:204–210
Bucciarelli P, Franchi F, Alatri A, Bettini P, Moia M (1998) Budd-Chiari syndrome in a patient heterozygous for the G20210A mutation of the prothrombin gene. Thromb Hemost 79:445–446
Burgaleta C, Gonzalez N, Cesar J (2002) Increased CD11/Cd18 expression and altered metabolic activity on polymorphonuclear leukocytes from patients with polycythemia vera and essential thrombocythemia. Acta Haematol 108:23–28
Cantwell D, Fitzgerald O, Fitzgerald P, Mehigan JA (1956) Diagnosis and treatment of the Budd-Chiari syndrome in polycythaemia vera. Br Med J 44:1343–1345
Cario H, Pahl HL, Schwarz K, Galm C, Hoffmann M, Burdelski M, Kohne E, Debatin KM (2003) Familial polycythemia vera with Budd-Chiari syndrome in childhood. Br J Haematol 123:346–352
Caroli J, Soulier JP (1956) Polycythemia vera and the Budd-Chiari syndrome: clinical, biological and endoscopic study; traitement with P34 and tromexam; apparent recovery (in French). Rev Med Chir Mal Foie 31:39–48
Casillas C, Marti-Bonmati L, Galant J (1997) Pseudotumoral presentation of nodular regenerative hyperplasia of the liver: imaging in five patients including MR imaging. Eur Radiol 7:654–658
Castellano G, Canga F, Solis-Herruzo JA, Colina F, Martinez-Montiel MP, Morillas JD (1989) Budd-Chiari syndrome associated with nodular regenerative hyperplasia of the liver. J Clin Gastroenterol 11:698–702
Cheng TI, Tsou MH, Yang PS, Sung SM, Chuang VP, Sung JL (2002) Dermatomyositis and erythrocytosis associated with hepatocellular carcinoma. J Gastroenterol Hepatol 17:1239–1240
Chini V (1954) Deficiency picture and Budd-Chiari syndrome in polycythemia vera (in Italian). Rass Clin Sci 30:168–174
Chlumsky J, Chlumska A (1966) Liver and polycythemia vera (Vaquez-osler disease). (in German). Gastroenterologia 105:366–374
Chu CW, Hwang SJ, Luo JC, Tsay SH, Li CP, Chang FY, Lee SD, Lui WY, Chiang JH (1999) Manifestations of hypercholesterolaemia, hypoglycaemia, erythrocytosis and hypercalcaemia in patients with hepatocellular carcinoma: report of two cases. J Gastroenterol Hepatol 14:807–810
Chudecki B (1972) Primary cancer of the liver following treatment of polycythaemia vera with radioactive phosphorus. Br J Radiol 45:770–774
Clouet M, Boulay I, Boudiaf M, Soyer P, Nemeth J, Kiselman R, Rymer R (1999) Imaging features of nodular regenerative hyperplasia of the liver mimicking hepatic metastases. Abdom Imaging 24:258–261
Conte M, Fouet P, Jacobs C, Conte-Marti (1964) Primary liver cancer and polycythemia (in French). Bull Mem Soc Med Hop Paris 115:1011–1016
Cornet A, Barbier JP, Benisty H, Carnot F, Fraitag B (1978) Polyglobulia as a manifestation of a primary of the liver (in French). Ann Med Interne (Paris) 129:279–281
Davidson CS (1976) Hepatocellular carcinoma and erythrocytosis. Semin Hematol 13:115–119
De Grandis M, Cambot M, Wautier MP, Cassinat B, Chomienne C, Colin Y, Wautier JL et al (2012) JAK2V617F activates Lu/BCAM-mediated red cell adhesion in polycythemia vera through an EpoR-independent Rap1/Akt pathway. Blood 121:658–665
De Sousa JMM, Portmann B, Williams R (1991) Nodular regenerative hyperplasia of the liver and the Budd-Chiari syndrome. J Hepatol 12:28–35
De Stefano V, Teofili L, Leone G, Michiels JJ (1997) Spontaneous erythroid colony formation as the clue to an underlying myeloproliferative disorder in patients with Budd-Chiari syndrome or portal vein thrombosis. Semin Thromb Hemost 23:411–418
De Stefano V, Chiusolo P, Paciaroni K, Teofili L, Ortu La Barbera E, Casorelli I, Leone G (1998) Hepatic vein thrombosis in a patient with mutant 20210A allele. Thromb Hemost 80:519
Delarive J, Gonvers JJ (1998) Budd-Chiari syndrome related to factor V Leiden mutation. Am J Gastroenterol 93:651–652
Deltenre P, Denninger MH, Hillaire S, Guillin MC, Casadevall N, Briere J, Erlinger S, Valla DC (2001) Factor V Leiden related Budd-Chiari syndrome. Gut 48:264–268
Di Guglielmo G, Quattrin N (1942) Mielosi eritremica cronica. Haematologica 24:1
Dilawari JB, Bambery P, Chawla Y, Kaur U, Bhusnurmath SR, Malhotra HS, Sood GK, Mitra SK, Khanna SK, Walia BS (1994) Hepatic outflow obstruction (Budd-Chiari syndrome). Experience with 177 patients and a review of the literature. Medicine (Baltimore) 73:21–36
Drenou B, Le Prise PY, Poilane B, Bernard-Griffiths I, Ghandour C, Fauchet R (1992) Polycythaemia and portal vein thrombosis. Nouv Rev Fr Hematol 34:399–403
Escher R, Demarmels BF (1999) Fall 9. Eine 26jährige Frau mit splanchnischer Venenthrombose als Initialmanifestation einer Polycythaemia vera. Ther Umschau 56:505–508
Fechtner L, DelDuca V (1994) Diagnosis by MRI of Budd-Chiari syndrome presenting with new onset of polycythemia. Del Med J 66:554
Fields W, Freeman NJ (1993) The hypercoagulability of polycythemia vera. Hosp Pract (Off Ed) 28(9A):65–68, 72–73
Fiessinger JN (1994) Thrombotic complications of polycythemia. The venous and arterial risk factors. Nouv Rev Fr Hematol 36:179–181
Friess D, Lämmle B, Alberio L (2003) Qualitative platelet defect and thrombohaemorrhagic complications in a patient with polycythaemia vera. Case 10. Hamostaseologie 23:138–143
Funakoshi A, Muta H, Baba T, Shimizu S (1993) Gene expression of mutant erythropoietin in hepatocellular carcinoma. Biochem Biophys Res Commun 195:717–722
Gautier EF, Picard M, Laurent C, Marty C, Villeval JL, Demur C, Delhommeau F, Hexner E et al (2012) The cell cycle regulator CDC25A is a target for JAK2V617F oncogene. Blood 119:1190–1199
Gensini GF, Conti AA (2002) Association between hepatocellular carcinoma and polycythemia vera (in Italian). Recenti Prog Med 93:25–27
Gilbert HS (2003) Modern treatment strategies in polycythemia vera. Semin Hematol 40(suppl 2):26–29
Golden C (2003) Polycythemia vera: a review. Clin J Oncol Nurs 7:553–556
Gordon AS, Zanjani ED, Zalusky R (1970) A possible mechanism for the erythrocytosis associated with hepatocellular carcinoma in man. Blood 35:151–157
Goreczky L, Toth J (1967) A case of malignant erythroblastoma. A rare form of Di Guglielmo’s syndrome (in German). Folia Haematol Int Mag Klein Morphol Blutforsch 88:45–53
Gumina RJ, Foley DA, Tefferi A, Rooke TW, Shields RC (2002) Polycythemia vera –a case report and discussion on pathogenic mechanisms of increased thrombosis. Angiology 53:587–591
Gundling F, Kreth F, Tröltzsch M, Tannapfel A, Bödeker H, Mössner J (2004) Unclear liver fibrosis in a 42-year-old patient with polycythemia vera (in German). Internist (Berl) 45:1293–1298
Hadengue A, Poliquin M, Vilgrain V et al (1994) The changing scene of hepatic vein thrombosis: recognition of asymptomatic cases. Gastroenterology 106:1042–1047
Hamilton A, Moise ME (1912) Erythrocythemia. Boston Med J 166:963–967
Hautekeete ML, Brenard R, Hadengue A, Degott C, Babany G, Arrive L, Lebrec D, Menu Y, Erlinger S, Benhamou JP (1990) membranous obstruction of the inferior vena cava and hepatocellular carcinoma in a Caribbean patient. J Clin Gastroenterol 12:214–217
Havlioglu N, Brunt EM, Bacon BR (2003) Budd-Chiari syndrome and hepatocellular carcinoma: a case report and review of the literature. Am J Gastroenterol 98:201–204
Heilmeyer L, Schöner W (1961) Die chronische reine Erythroblastose des Erwachsenen als Leukämie-paralleler Prozess des erythrocytären Systems. Dtsch Arch Klin Med 187:225–248
Hirschfeld H (1906) Zur Pathologischen Anatomine der Plethora Vera. Med Klin 8:588–592
Horiouchi A, Hayashi S, Ando T, Nonoyama T (1997) Secondary polycythemia in male B6C3F1 mice with spontaneously occurring hepatocellular carcinomas. Toxikol Pathol 25:511–515
Huang SJ, Lee SD, Wu JC et al (1994) Clinical evaluation of erythrocytosis in patients with hepatocellular carcinoma. Chin Med J (Taipei) 53:262–269
Ibarrola C, Castellano VM, Colina F (2004) Focal hyperplastic hepatocellular nodules in hepatic venous outflow obstruction: a clinicopathological study of four patients and 24 nodules. Histopathology 44:172–179
Introzzi P, Buscarini L (1966) Contribution to the study of chronic erythremic disease (in Italian). Haematologica 51:1–14
Iwai M, Kitagawa Y, Nakajima T, Takeda M, Okanoue T, Nakajima T, Ogasawara T, Suyama Y, Miyoshi M, Kashima K (1998) Clinical features, image analysis, and laparoscopic and histological liver findings in Budd-Chiari syndrome. Hepato-Gastroenterology 45:2359–2368
Jacobson RJ, Lowenthal MN, Kew MC (1978) Erythrocytosis in hepatocellular cancer. S Afr Med J 53:658–660
Jang JW, Yoon SK, Bae SH, Choi JY, Chung KW, Sun HS (2003) Rapidly progressing Budd-Chiari syndrome complicated by hepatocellular carcinoma. Korean J Intern Med 18:191–195
Janssen HL (2000) Changing perspectives in portal vein thrombosis. Scand J Gastroenterol, (Suppl 232):69–73
Janssen HL, Meinardi JR, Vleggaar FP, van Uum SH, Haagsma EB, van Der Meer FJ, van Hattum J et al (2000) Factor V Leiden mutation, prothrombin gene mutation, and deficiencies in coagulation inhibitors associated with Budd-Chiari syndrome and portal vein thrombosis: results of a case-control study. Blood 96:2364–2368
Janssen HLA, Garcia-Pagan JC, Elias E, Mentha G, Hadengue A, Valla DC, European Group for the Study of Vascular Disorders of the Liver (2003) Budd-Chiari syndrome: a review by an expert panel. J Hepatol 38:364–371
Kage M, Arakawa M, Kojiro M, Okuda K (1992) Histopathology of membranous obstruction of the inferior vena cava in the Budd-Chiari syndrome. Gastroenterology 102:2081–2090
Kan YW, McFadzean AJ, Todd D, Tso SC (1961) Further observations on polycythemia in hepatocellular carcinoma. Blood 18:592–598
Karia K, Mathur SK, Amarapurkar D, Punamiya SJ (2000) Hepatocellular carcinoma in association with membranous obstruction of inferior vena cava. Indian J Gastroenterol 19:90–91
Kass L (1975) Chronic erythremic myelosis profiling a refractory anemia. Postgrad Med 58:161–166
Katoh M, Shigematsu H (1999) Primary liver carcinoma complicating membranous obstruction of the inferior vena cava. Pathol Int 49:253–257
Kawasaki T, Taketa K, Ueda M, Watanabe A, Watanabe M, Shimamura J, Okazaki S, Mitani K, Nakata K, Endo H, Nagashima H, Ogawa K (1979) A case of hepatocellular carcinoma with hypercholesterolemia, erythrocytosis and hypoglycemia (in Japanese). Nippon Shokakibyo Gakkai Zasshi 76:1871–1877
Kew MC, McKnight A, Hodkinson J, Bukofzer S, Esser JD (1989) The role of membranous obstruction of the inferior vena cava in the etiology of hepatocellular carcinoma in Southern African blacks. Hepatology 9:121–125
Klippel S, Strunck E, Busse CE, Behringer D, Pahl HL (2002) Biochemical characterization of PRV-1, a novel hematopoietic cell surface receptor, which is overexpressed in polycythemia rubra vera. Blood 100:2441–2448
Klippel S, Strunck E, Temerinac S, Bench AJ, Meinhardt G, Mohr U, Leichtle R, Green AR, Griesshammer M et al (2003) Quantification of PRV-1 mRNA distinguishes polycythemia vera from secondary erythrocytosis. Blood 102:3569–3574
Koopmans SM, Bot FJ, Schouten HC, Janssen J, van Marion AM (2012) The involvement of galectins in the modulation of the JAK/STAT pathway in myeloproliferative neoplasia. Am J Blood Res 2:119–127
Kratzeisen E (1923) Polyzythämie und Pfortaderthrombose. Virchows Arch 244:467
Levy VG, Ruskone A, Baillou C, Theirman-Duffaud D, Najman A, Boffa GA (1985) Polycythemia and the Budd-Chiari syndrome: study of serum erythropoietin and bone marrow erythroid progenitors. Hepatology 5:858–861
Lizzi FA, Tartaglia AP, Adamson JW (1973) Hemochromatosis, hepatoma, erythrocytosis, and erythropoietin. N Y State J Med 73:1098–1100
Löhr JM, Kuchenreuter S, Grebmeier H, Hahn EG, Fleig WE (1993) Compression of the common bile duct due to portal-vein thrombosis in polycythemia vera. Hepatology 17:586–592
Lommel K (1906) Über Polyzythämie und Milztumor. Arch Klin Med 87:315
Maetani Y, Itoh K, Egawa H, Haga H, Sakurai T, Nishida N, Ametani F, Shibata T, Kubo T, Tanaka K, Konishi J (2002) Benign hepatic nodules in Budd-Chiari syndrome: radiologic-pathologic correlation with emphasis on the central scar. AJR Am J Roentgenol 178:869–875
Mahmoud AE, Mendoza A, Meshikhes AN, Olliff S, West R, Neuberger J, Buckels J, Wilde J, Elias E (1996) Clinical spectrum, investigations and treatment of Budd-Chiari syndrome. Q J M 89:37–43
Mahmoud AE, Elias E, Beauchamp N, Wilde JT (1997) Prevalence of the factor V Leiden mutation in hepatic and portal vein thrombosis. Gut 40:798–800
Malaguarnera M, bentivegna P, Di Fazio I, Laurino A, Romano M, Trovato BA (1996) Erythropoietin in hepatocellular carcinoma (in French). Bull Cancer 83:977–980
Mandelbaum H, Diamond D, Feldman F (1953) Acute obliterative endophlebitis of the hepatic veins secondary to polycythemia vera. N Y State J Med 53:2689–2692
Marsan C, Henon P, Boddaert A (1973) A case of chronic erythremic myelosis (in French). Arch Anat Pathol (Paris) 21:171–178
Matsuyama M, Yamazaki O, Horii K, Higaki I, Kawai S, Mikami S, Higashino M, Oka H, Nakai T, Inoue T (2000) Erythrocytosis caused by an erythropoietin-producing hepatocellular carcinoma. J Surg Oncol 75:197–202
McBrine PA, Miller A, Zimelman AP, Koff RS (1980) Polycythemia vera with myelofibrosis and myeloid metaplasia. Acute hepatic failure following splenectomy. Am J Clin Pathol 74:693–696
McFadzean AJ, Todd D, Tsang KC (1958) Polycythemia in primary carcinoma of the liver. Blood 13:427–435
McFadzean AJ, Todd D, Tso SC (1967) Erythrocytosis associated with hepatocellular carcinoma. Blood 29:808–811
Means RT (2008) Perspective: Osler’s 1903 paper on polycythemia vera. Am J Med Sci 335:418–419
Messinezy M, Pearson TC (1999) The classification and diagnostic criteria of the erythrocytoses (polycytaemias). Clin Lab Haematol 21:309–316
Michiels JJ (1997) Erythromelalgia and vascular complications in polycythemia vera. Semin Thromb Hemost 23:441–454
Michiels JJ, Juvonen E (1997) Proposal for revised diagnostic criteria of essential thrombocythemia and polycythemia vera by the Thrombocythemia Vera Study Group. Semin Thromb Hemost 23:339–347
Michiels JJ, van der Meulen J, Brederoo P (1997) The natural history of trilinear myelodysplastic syndrome and erythroleukemia. Haematologica 82:452–454
Minnema MC, Janssen HLA, Niermeijer P, de Man RA (2000) Budd-Chiari syndrome: combination of genetic defects and the use of oral contraceptives leading to hypercoagulability. J Hepatol 33:509–512
Mohanty D, Shetty S, Ghosh K, Pawar A, Abraham P (2001) Hereditary thrombophilia as a cause of Budd-Chiari syndrome: a study from Western India. Hepatology 34:666–670
Mosse E (1920) Die Polyglobulien. In: Kraus F, Brugsch T(eds) Handbuch der Specziellen Pathologie and Therapie. Urban and Schwarzenberg, Berlin, p 821
Muta H, Funakoshi A, Baba T, Uike N, Wakasugi H, Kozuru M, Jimi A (1994) Gene expression of erythropoietin in hepatocellular carcinoma. Intern Med 33:427–431
Nakai Y, Tamai Y, Minaguchi S, Yoshimi T, Hoshino T (1972) Primary hepatocellular carcinoma with polycythemia, hypercholesterolemia and various other clinical symptoms (in Japanese). Nippon Rinsho 30:2329–2334
Nakamura S, Takezawa Y (1982) Obstruction of the inferior vena cava in the hepatic portion and hepatocellular carcinoma. Tohoku J Exp Med 138:119–120
Neunteufl T, Heher S, Stefenelli T, Pabinger I, Gisslinger H (2001) Endothelial dysfunction in patients with polycythaemia vera. Br J Haematol 115:354–359
Nunnensiek C, Rössler R, Neumann G (1976) Chronic erythroleukemia in Di Guglielmo’s syndrome (in German). Med Welt 27:1154–1156
Okazaki N, Ozaki H, Arima M, Hattori N, Kimura K (1979) Hepatocellular carcinoma associated with erythrocytosis. A nine year survival after successful chemotherapy and left lateral hepatectomy. Acta Hepatogastroenterology (Stuttg) 26:248–252
Okuda K (1982) Membranous obstruction of the inferior vena cava: etiology and relation to hepatocellular carcinoma. Gastroenterology 82:376–379
Okuda K (2002) Inferior vena cava thrombosis at its hepatic portion (obliterative hepatocavopathy). Semin Liver Dis 22:15–26
Okuda H, Yamagata H, Obata H, Iwata H, Sasaki R, Imai F, Okudaira M, Ohbu M, Okuda K (1995) Epidemiological and clinical features of Budd-Chiari syndrome in Japan. J Hepatol 22:1–9
Okuda K, Kage M, Shrestha SM (1998) Proposal of a new nomenclature for Budd-Chiari syndrome: hepatic vein thrombosis versus thrombosis of the inferior vena cava at its hepatic portion. Hepatology 28:1191–1198
Oner AF, Arslan S, Caksen H, Ceylan A (1999) Budd-Chiari syndrome in a patient heterozygous for both factor V Leiden and the G20210A mutation on the prothrombin gene. Thromb Hemost 82:1366–1367
Orlandi E, Castelli G, Brusamolino E, canevari A, Morra E, Lazzarino M, Bernasconi C (1989) Hemorrhagic and thrombotic complications in polycythemia vera. A clinical study. Haematologica 74:45–49
Osler W (1903) Chronic cyanosis, with polycythemia and enlarged spleen: a new clinical entity. Am J Med Sci 126:176–201
Patel RK, Lea NC, Heeghan MA, Westwood NB, Milojkovic D, Thanigaikumar M et al (2006) Prevalence of the activating JAK2 tyrosine kinase mutation V617F in the Budd-Chiari syndrome. Gastroenterology 130:2031–2038
Pati HP, Dayal S, Kashyap R, Padhy AK (1998) Masked polycythaemia vera in a patient with extrahepatic portal venous obstruction. Eur J Gastroenterol Hepatol 10:883–885
Pearson TC (1998) Diagnosis and classification of erythrocytoses and thrombocytoses. Baillieres Clin Haematol 11:695–720
Pearson TC (2002) The risk of thrombosis in essential thrombocythemia and polycythemia vera. Semin Oncol 29(suppl 10):16–21
Peters MJ, Dixon G, Kotowicz KT, Hatch DJ, Heyderman RS, Klein NJ (1999) Circulating platelet-neutrophil complexes represent a subpopulation of activated neutrophils primed for adhesion, phagocytosis and intracellular killing. Br J Haematol 106:391–399
Peterson P, Wasserman LR (1995) The natural history of polycythemia vera. In: Wasserman LR, Berk PD, Berlin NI (eds) Polycythemia vera and the myeloproliferative disorders. W.B. Saunders, Philadelphia, pp 14–21
Picardi M, Muretto P, Luciano L (2000) Budd-Chiari syndrome in chronic myeloid leukemia. Haematologica 85:429
Pirisi M, Fabris C, Soardo G, Falleti E, Gasparini D, Vitulli D, Toniutto P, Gonano F, Bartoli E (1995) Hepatic release of erythropoietin induced by transarterial chemoembolization in patients with hepatocellular carcinoma. Hepatology 22:148–152
Pivnik AV, Idel’son LI, Ter-Grigorov VS, Gel’man VB, Khasenov BA (1987) Neoplastic form of chronic erythromyelosis (erythrosarcoma) with eosinophilia and cardiac lesions (in Russian). Ter Arkh 59:130–133
Poort SR, Rosendaal FR, Reitsma PH, Bertina RM (1996) A common genetic variation of the 3′-untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosis. Blood 88:3698–3703
Poreddy V, DeLeve LD (2002) Hepatic circulatory diseases associated with chronic myeloid disorders. Clin Liver Dis 6:909–931
Prchal JT (2001) Pathogenetic mechanisms of polycythemia vera and congenital polycythemic disorders. Semin Hematol 38(suppl 2):10–20
Prchal JT (2003) Classification and molecular biology of polycythemias (erythrocytoses) and thrombocytosis. Hematol Oncol Clin N Am 17:1151–1158
Prchal JF, Prchal JT (1999) Molecular basis for polycythemia. Curr Opin Hematol 6:100–109
Randi ML, Fabris F, Ruzzon E, Pacquola E, Cella G, Girolami A (2002) Splenectomy after portal thrombosis in patients with polycythemia vera and essential thrombocythemia. Haematologica 87:1180–1184
Raphael B, Cooperberg AA, Niloff P (1979) The triad of hemochromatosis, hepatoma and erythrocytosis. Cancer 43:690–694
Rector WG, Xu YH, Goldstein L, Peters RL, Reynolds TB (1985) Membranous obstruction of the inferior vena cava in the United States. Medicine (Baltimore) 64:134–143
Regimbeau JM, Rain JD, Sauvanet A, Bai YS, Belghiti J (1999) Regression of polycythemia and elevated serum erythropoietin after resection of hepatocellular carcinoma (in French). Gastroenterol Clin Biol 23:532–533
Retzlaff K, Monge JJ (1973) Polycythemia vera with acute Budd-Chiari syndrome. Minn Med 56:60–62
Rha SE, Lee MG, Lee YS, Kang GH, Ha HK, Kim PN, Auh YH (2000) Nodular regenerative hyperplasia of the liver in Budd-Chiari syndrome: CT and MR features. Abdom Imaging 25:255–258
Ruvidic R, Ivaneski M (1970) Polyglobulism associated with primary liver cancer (in French). Nouv Rev Fr Hematol 10:261–265
Sakisaka S, Watanabe M, Tateishi H, Harada M, Shakado S, Mimura Y, Gondo K, Yoshitake M, Noguchi K, Hino T et al (1993) Erythropoietin production in hepatocellular carcinoma cells associated with polycythemia: immunohistochemical evidence. Hepatology 18:1357–1362
Santer MA, Waldmann TA, Fallon HJ (1967) Erythrocytosis and hyperlipemia as manifestations of hepatic carcinoma. Arch Intern Med 120:735–739
Sawabe Y, Iida S, Tabata Y, Yonemitsu H (1993) Serum erythropoietin measurements by a one-step sandwich enzyme linked immunosorbent assay in patients with hepatocellular carcinoma and liver cirrhosis. Jpn J Clin Oncol 23:273–277
Schilling MK, Zimmermann A, Redaelli C, Seiler CA, Buchler MW (2000) Liver nodules resembling focal nodular hyperplasia after hepatic venous thrombosis. J Hepatol 33:673–676
Scott LM (2011) The JAK2 exon 12 mutations: a comprehensive review. Am J Hematol 86:668–676
Scott D, Theologides A (1974) Hepatoma, erythrocytosis and increased serum erythropoietin developing in long-standing hemochromatosis. Am J Gastroenterol 61:206–211
Scott LM, Tong W, Levine RL, Scott MA, Beer PA, Stratton MR, Futreal PA, Erber WN et al (2007) JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med 356:459–468
Seo JB, Chung JW, Park JH, Kim SH, Kim TK, Han JK, Choi BI, Han MC (1998) Benign obstruction of the hepatic inferior vena cava complicated by hepatocellular carcinoma: combined interventional management. AJR Am J Roentgenol 170:655–659
Shapiro RS, Maldjian JA, Stancato-Pasik A, Ramos R (1993) Hepatic mass in Budd-Chiardrome: CT and MRI findings. Comput Med Imaging Graph 17:457–460
Shchekochikhin SM, Osipova MV (1991) A case of combined hepatocellular carcinoma and erythremia (in Russian). Ter Arkh 63:139–140
Sherlock S, Dooley J (1993) Budd-Chiari (hepatic venous obstruction) syndrome. In: Sherlock S, Dooley J (eds) Diseases of the liver and biliary system. Blackwell Scientific Publications, Oxford, pp 183–192
Shrestha SM, Okuda K, Uchida T, Maharjan KG, Shrestha S, Joshi BL, Larsson S, Vaidya Y (1996) Endemicity and clinical picture of liver disease due to obstruction of the hepatic portion of the inferior vena cava in Nepal. J Gastroenterol Hepatol 11:170–179
Siguier F, Godeau P, Delluc G, Sraer JD (1967) Budd-Chiari syndrome with polycythemia. Considerations on the pseudo-tumoral aspect (in French). Bull Mem Soc Med Hop Paris 118:1235–1238
Simsek S, Verheesen RV, Haagsma EB, Lourens J (2000) Subacute Budd-Chiari syndrome associated with polycythemia vera and factor V Leiden mutation. Neth J Med 57:62–67
Simson IW (1982) Membranous obstruction of the inferior vena cava and hepatocellular carcinoma in South Africa. Gastroenterology 82:171–178
Slakey DP, Klein AS, Venbrux AC et al (2001) Budd-Chiari syndrome. Current management options. Ann Surg 233:522–527
Soler R, Rodriguez E, Pombo F, Gonzalez J, Pombo S, Prada C (2000) Benign regenerative nodules with copper accumulation in a case of chronic Budd-Chiari syndrome: CT and MR findings. Abdom Imaging 25:486–489
Soyer P, Lacheheb D, Caudron C, Levesque M (1993) MRI of adenomatous hyperplastic nodules of the liver in Budd-Chiari syndrome. J Comput Assist Tomogr 17:86–89
Sozer S, Fiel MI, Schiano T, Xu M, Mascarenhas J, Hoffman R (2009) The presence of JAK2V617F mutation in the liver endothelial cells of patients with Budd-Chiari syndrome. Blood 113:5246–5249
Spremolla G, Tomei GP, Biancalana D (1970) Chronic erythremic myelosis: morphological and cytochemical data (in Italian). Haematologica 55:435–459
Sroczynski J, Hrycek A (1976) Primary chronic erythroblastosis (Heilmeyer-Schöner disease) (in Polish). Pol Tyg Lek 31:811–812
Starcich R, Tardini A, Vitali-Mazza L (1963) Di Guglielmo’s erythremia with prolonged course (chronic erythremia): anatomoclinical and ultrastructural study (in Italian). Riv Anat Patol Oncol 24(suppl):709–748
Stewart C (1971) Chronic Di Guglielmo disease. Med J Aust 27:480–482
Streiff MB, Smith B, Spivak JL (2002) The diagnosis and management of polycythemia vera in the era since the Polycythemia Vera Study Group: a survey of American Society of hematology members’ practice patterns. Blood 99:1144–1149
Takayasu K, Muramatsu Y, Moriyama N, Wakao F, Makuuchi M, Takayama T, Kosuge T, Okazaki N, Yamada R (1994) Radiological study of idiopathic Budd-Chiari syndrome complicated by hepatocellular carcinoma. A report of four cases. Am J Gastroenterol 89:249–253
Tanaka M, Wanless IR (1998) Pathology of the liver in Budd-Chiari syndrome: portal vein thrombosis and the histogenesis of venocentric cirrhosis, veno-portal cirrhosis, and large regenerative nodules. Hepatology 27:488–496
Tefferi A (2001) Chronic myeloid disorders: classification and treatment overview. Semin Hematol 38:1–4
Tefferi A (2003) Polycythemia vera: a comprehensive review and clinical recommendations. Mayo Clin Proc 78:174–194
Tefferi A, Lasho TL, Wolanskyj AP, Mesa RA (2004) Neutrophil PRV-1 expression across the chronic myeloproliferative disorders and in secondary or spurious polycythemia. Blood 103:3547–3548
Temerinac S, Klippel S, Strunck E, Roder S, Lubbert M, Lange W, Azemar M, Meinhardt G, Schaefer HE, Pahl HL (2000) Cloning of PRV-1, a novel member of the uPAR receptor superfamily, which is overexpressed in polycythemia rubra vera. Blood 95:2569–2576
Teofili L, Martini M, Luongo M, Di Mario A, Leone G, De Stefano V, Larocca LM (2002) Overexpression of the polycythemia rubra vera-1 gene in essential thrombocythemia. J Clin Oncol 20:4249–4254
Thomas M, Caroli J (1971) Polycythemia and Budd-Chiari syndrome. Apropos of 17 cases (in French). Ann Med Interne (Paris) 122:1175–1186
Thurm RH, Casey MJ, Emerson CP (1967) Chronic Di Guglielmo syndrome. Am J Med Sci 253:399–405
Tilanus HW (1995) Budd-Chiari syndrome. Br J Surg 82:1023–1030
Toth J, Bilodeau B (1980) Polycythemia vera associated with hepatocellular carcinoma: apropos of a case (in French). Union Med Can 109:1638–1640
Trotter JF, Cohn A, Grant R (2002) Erythrocytosis in a patient with hepatocellular carcinoma. J Clin Gastroenterol 35:365–366
Valla D (2002) Hepatic vein thrombosis (Budd-Chiari syndrome). Semin Liver Dis 22:5–14
Valla D, Casadevall N, Huisse MG, Tulliez M, Grange JD, Muller O, Binda T, Varet B, Rueff B, Benhamou JP (1988) Etiology of portal vein thrombosis in adults. A prospective evaluation of primary myeloproliferative disorders. Gastroenterology 94:1063–1069
Vaquez H (1892) Sur une forme spéciale de cyanose s’accompagnant d’ hyperglobulie excessive et persistante. CR Soc Biol (Paris) 44:384–388
Vilgrain V, Lewin M, Vons C, Denys A, Valla D, Flejou JF, Belghiti J, Menu Y (1999) Hepatic nodules in Budd-Chiari syndrome: imaging features. Radiology 210:443–450
Villmow T, Kemkes-Matthes B, Matzdorff AC (2002) Markers of platelet activation and platelet-leukocyte interaction in patients with myeloproliferative syndromes. Thromb Res 108:139–145
Wanless IR (1994) Regenerative nodules in Budd-Chiari syndrome. Hepatology 19:139I
Watanobe H (1988) Hepatocellular carcinoma associated with a rare combination of polycythemia and chronic thyroiditis. Hepato-Gastroenterology 35:14–16
Yonal I, Pinarbasi B, Hindilerden F, Hancer VS, Nalcaci M, Kaymakoglu S, Diz-Kucukkaya R (2012) The clinical significance of JAK2V617F mutation for Philadelphia-negative chronic myeloproliferative neoplasms in patients with splanchnic vein thrombosis. J Thromb Thrombolysis 34:388–396
Zhou H, Wolff M, Pauleit D, Fischer HP, Pfeifer U (2000) Multiple macroregenerative nodules in liver cirrhosis due to Budd-Chiari syndrome. Case reports and review of the literature. Hepato-Gastroenterology 47:522–527
Zlatkina AR, Shcherbak EM (1970) Erythrocytosis in primary cancer of the liver (in Russian). Probl Gematol Pereliv Krovi 15:55–56
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this entry
Cite this entry
Zimmermann, A. (2017). Myeloid Neoplasms with an Erythroid Cell Lineage. In: Tumors and Tumor-Like Lesions of the Hepatobiliary Tract. Springer, Cham. https://doi.org/10.1007/978-3-319-26956-6_80
Download citation
DOI: https://doi.org/10.1007/978-3-319-26956-6_80
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26954-2
Online ISBN: 978-3-319-26956-6
eBook Packages: MedicineReference Module Medicine