Abstract
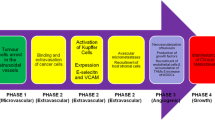
In order to enter an invasive and metastatic cascade, cancer cells must be released and individualized. Cell budding is a process characterized by single cells or small clusters of cancer cells that leave the invasion front. These individualized cells are capable to invade blood vessels and lymph vessels, a process which requires cell motility, differential cell-matrix adhesion, production of invadopodia, and the secretion of lytic enzymes, including metalloproteinases. The invasion armamentarium of cancer cells is not only an inborn feature of these cells but is also modulated by nonneoplastic cells encountered by cancer cells on their invasive track. For example, stromal cell-derived factor 1/CXCL12 stimulates motility and migration of cancer cells that express the respective receptor, CXCR4. Apart from budding cells that are prone to become invasive cells, malignant neoplasms can release, already in early phases, cells that will evolve independent from the primary tumor. These so-called premalignant cells or circulating tumor cells (CTCs) have a fate of their own and possess a high degree of plasticity. There is evidence that such cells are capable to induce premetastatic niches in target organs and to generate a cancer field within the body. Along their metastatic spread and within the premetastatic niche, cancer cells can fuse with normal cell partners of the microenvironment, forming chimeras that play a role in the regulation of growth and epithelial-mesenchymal transition (EMT).
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Tumor Cell Budding, Motility, and Invasion as Driving Forces for Liver Metastases
Tumor Cell Budding as a Mode of Tumor Cell Individualization
Colorectal Carcinoma (CRC) cells exert distinct growth patterns that affect disease progression and prognosis, in particular tumor cell budding at the invasive margin. Budding (or sprouting) is defined as small clusters of individualized and poorly differentiated carcinoma cells in or outside the invasion front. The presence of such dissociated, dedifferentiated tumor cells at the tumor-host interface is predictive of lymphatic involvement of CRC (Ogawa et al. 2009), lymphovascular invasion (also in early stage N0 CRC; Wang et al. 2009), predicts local and distant metastases (Nakamura et al. 2005; Zlobec et al. 2008; Suzuki et al. 2009), including lymph node metastasis (Yamauchi et al. 2008), and is correlated with an enhanced malignant potential in CRC (Okuyama et al. 2002; Prall 2007; Kanazawa et al. 2008). These budding cells have undergone epithelial-mesenchymal transition (EMT) and are growth-arrested due to increased expression of p16 and other mechanisms (Jung et al. 2001). Low cellular proliferation at the invasion front, the niche of budding cells, has been associated with poor prognosis in CRC (Palmqvist et al. 1999). Loss of expression of the adhesion molecule, E-cadherin, and APAF-1 were independent predictors of budding, and the loss was associated with more frequent peritumoral lymphocytes and tumor-infiltrating lymphocytes (Zlobec et al. 2007).
Motility, Migration, and Invasion of Tumor Cells: The Role of Invadopodia
The dissociation process of budding cells at the invasion front requires distinct modes of motility/cell locomotion linked to the tumor cells’ cytoskeleton. Individualized cancer cells are capable to migrate through the extracellular matrix (ECM) and can form ECM-degrading, actin-rich ventral membrane protrusions called invadopodia, similar to the podosomes of macrophages. These dynamic organelle-like structures adhere to, and proteolytically digest, collagens, laminin, and fibronectin located in the ECM (Yamaguchi et al. 2006; Stylli et al. 2008).
The formation of invadopodia requires WAVE2 expression but seems to be independent of the tubulin system (Kikuchi and Takahashi 2008). In the regulation pathways programming the conversion between rounded and elongated modes of cancer cell movement, DOCK3, NEDD9, WAVE2, and ARHGAP22 are key factors regulating Rac and Rho signaling (Croft and Olson 2008). The formation of diverse types of lamellipode with actin reassembly at the leading edge requires the membrane transport of WAVE2. The membrane transport of WAVE2 requires the association between the constitutive complex of betaPIX and GIT1 with WAVE2 (Morimura et al. 2009) and a small GTPase, Rac1, the motor protein kinesin, and microtubules (the latter not of importance in invadopodia). The p21-activated kinase Pak1 is a downstream effector of Rac1 and binds to WAVE2 and is transported with WAVE2 to the leading edge by stimulation with hepatocyte growth factor. Concomitantly, phosphorylation of tubulin-bound stathmin/Op18 at serine 25 and serine 38, microtubule growth, and stathmin/Op18 binding to the kinesin-WAVE2 complex are induced (Takahashi and Suzuki 2009). The human ortholog of mammalian enabled (hMena), an actin regulatory phosphoprotein involved in the control of cell motility, is expressed at the invasion margin of CRC and here particularly in budding cells (Toyoda et al. 2009).
Immunohistochemical staining for the cytoskeletal component, beta(III)-tubulin, was evident in budding CRC cells, suggesting that changes in tubulin isotypes could modulate the invading activity of these cells (Portyanko et al. 2009). 14-3-3 sigma is frequently expressed in budding tumor cells in the invasive area, and overexpression of the protein modulates cell migration in the presence of the ECM protein, tenascin-C (Ide et al. 2007). As motile dissociated cancer cells (including budding/sprouting cells) with a decreased level of differentiation play a crucial role in carcinoma invasion, the actin remodeling system critically participating in the locomotion machinery is studied in cancer, including CRC. At the leading edge of migrating cells (lamellipodia and invadopodia), protrusive forces are developed by the assembly of F-actin filaments organized in dendritic array at the front and a more distal lamellar linear array. Production and remodeling of F-actin depends on several proteins acting in a highly orchestrated fashion. Tropomyosin markedly inhibits lamellipodium formation and facilitates the distal lamellar linear array, in that it competes with the actin nucleator, actin-related protein 2/3 (Arp2/3) during filament branching, and counteracts the effects of the neural Wiskott-Aldrich syndrome protein, N-WASP (Bugyi et al. 2010). Cortactin is an F-actin-binding protein that stabilizes F-actin networks and promotes actin polymerization by activating the Arp 2/3 complex. Overexpression of cortactin stimulates cell migration in cancer cells, and in CRC cells, cortactin interacts with the zona occludens-1(ZO-1) protein, and expression of this complex favors an invasive and spreading/metastasizing phenotype (Hirakawa et al. 2009). Actin-related protein 2 (Arp2) colocalizes with WAVE2 in CRC cells and this is correlated with liver metastasis (Iwaya et al. 2007). Two CARMIL (capping protein, Arp2/3, and myosin-I linker) family proteins exert important regulatory functions. CARMIL1 localizes to lamellipodia and macropinosomes, and loss of its function causes loss of lamellipodial actin, along with defects in protrusion, ruffling, and macropinocytosis. CARMIL2 colocalizes with vimentin, and loss of its function causes a distinct multipolar phenotype, associated with decreased levels of myosin-IIB (Liang et al. 2009). An important group of regulating factors are members of the TOCA family of F-BAR-containing proteins. These proteins bind to and remodel lipid bilayers in a clathrin-dependent manner via their conserved F-BAR domains and regulate actin dynamics via their N-WASP binding SH3 domains. In mammalian cells, TOCA1 is associated with N-WASP and WPS-1 directly or WAVE2 indirectly via ABI-1 (Giuliani et al. 2009). Generally, BAR (Bin-Amphiphysin-Rvs) domain proteins can sense membrane curvature and recruit actin to membranes. They are also critically involved in clathrin-mediated endocytosis, in which actin polymerization mediated by the Arp2/3 complex is essential for membrane tubulation and vesicle formation and fission. The tubulated membrane between the future endocytic vesicle and the plasma membrane seems to form an arc upon scission of the endocytic vesicle, and the formation of this structure depends on arc sensing mediated by the RFC/F-BAR domain protein, FBP17 (Suetsugu 2009). In endocytosis, BAR proteins also interact with other components of the endocytic and cytoskeletal machinery, including the GTPase dynamin (which mediates vesicle fission), N-WASP (an Arp2/3 complex regulator), and synaptojanin (a phosphoinositide phosphatase). Three classes of BAR proteins have been defined, i.e., BAR, N-BAR, and F-Bar (Dawson et al. 2006).
Stromal Factors Exerting an Influence on Tumor Cell Migration and Invasion
CXCL12 (stromal cell-derived factor 1) is an important factor for the stimulation of cancer cell motility and migration. CXCL12 promotes motility in neoplastic cells that express the receptor, CXCR4 (Do Carmo et al. 2010). CXCL12+ tumor budding in CRC is a significant prognostic factor (Akishima-Fukasawa et al. 2009). CXCR4 is also known to enhance the proliferation of certain cancer cells via AKT and ERK-dependent pathways (Shen et al. 2010). The liver has high concentrations of CXCL12 (Kim et al. 2005) that could provide a specific homing target and promoting factor for CXCR4-expressing CRC cells. CXCL12 is a constitutively expressed chemokine which orchestrates a large array of functions. Six different isoforms exist in humans (α, β, γ, δ, ε, and ϕ), all differing in their C-terminal domain (Yu et al. 2006). CXCL12 binds to the receptor, CXCR4, which is transcriptionally regulated by HIF-1alpha and a constitutively activated EGFR variant, EGFRvIII (Rahimi et al. 2010). Angiogenesis is promoted by attraction of motile endothelial cells by CXCL12. The axis markedly affects the migration of tumor cells to metastatic sites, allowing cancer cells to access cellular niches expressing the CXCR4 receptor favoring cell survival and growth (“metastatic homing” of cancer cells; Murphy 2001; Burger and Kipps 2006; Dewan et al. 2006). In CRC, CXCR4 expression was found to increase the risk for recurrence, liver metastasis, and poor survival (Kim et al. 2005). The role of the microvascular bed in mechanisms of tumor cell spread surfaced in the observation that concomitant overexpression of CXCR4 and vascular endothelial growth factor (VEGF) in the tumors predicts early distant relapse in stage II-III CRC patients (Ottaiano et al. 2006).
Pathogenic Features of Liver Metastases: Dissemination and Evolution of Premalignant Cells (Circulating Tumor Cells, CTCs) and the “Wandering Field”/“Cancer Field” Hypotheses
In the previous paragraph, it was outlined that the settling of tumor cells and their progenitors at future metastatic sites requires the establishment of a premetastatic niche that permits circulating cells to home to tissues and to interact with the host organ (Sleeman 2012). On the other hand, the early metastatic process also requires that subpopulations of cells are released that are capable to home to a niche and to produce a metastatic growth. The capacity of tumor cells to escape from the primary tumor, individualize, migrate, invade, and spread to remote tissues was described as a phenomenon resembling Darwinian selection (Klein 2013). However, this may represent a simplistic view, as the so-called invasion and metastasis cascade does not seem to exactly work that way. Rather, there is recent evidence that tumor cells and particularly their progenitors (cancer stem cells) individualize and disseminate in very early and primordial malignant neoplasms already, having a still not well-studied status of “premalignant” cells (PMCs), single disseminated tumor cells (DTCs), or circulating tumor cells (CTCs) (Klein 2000; Diamond et al. 2012) that will evolve almost or completely independent from the primary tumor (Ansieau et al. 2008). These individualized cells have a fate of their own and possess a high degree of plasticity (Bednarz-Knoll et al. 2012). It is these PMCs that will acquire, by progressive genomic instability and selection pressures, distinct genomic signatures, and these alterations will render PMCs capable to induce, and interact with, future premetastatic niches. In this setting, spread of cancer may be described by the features of a “wandering field hypothesis,” meaning that PMCs and their induced premetastatic niches form a cancer field that is distributed within the host. The generation and distribution of tumor cells that can finally give rise to metastases in “field-like” body structure has been addressed by methods of systems biology, discussing selection-driven independence, invasion, and so-called swarm intelligence (Tarabichi et al. 2013).
Pathogenic Features of Liver Metastases: Parallel and Nonparallel Progression of Tumor and Metastases
Introduction
An older view of metastatic spread identified the primary tumor as the single important engine determining metastasis through the production and release of fully metastasis-capable cells. A second hypothesis, termed the parallel progression model (Klein 2009), proposes parallel, independent progression of metastases arising from early disseminated cells (single disseminated tumor cells (DTCs); see above). Clonal expansion mechanisms and a marked genetic disparity between primary tumors and disseminated tumor cells (Stoecklein and Klein 2010) support this hypothesis. Other findings were not compatible with the parallel progression model, but the linear progression model in this hypothesis works when it is assumed that tumors harbor two types of cells, i.e., metastasis-forming cells (MFCs), likely to derive from tumor stem cells, and a second set that is not capable to produce metastases. There is evidence that the proportion of MFCs decreases as a function of increasing tumor size, one possible explanation for the observation that at least part of large tumors have a lesser probability to produce metastases (review: Koscielny and Tubiana 2010).
Do Primary Tumors and Their Metastases Share a Parallel Evolution?
Animal experimentation had already shown that removal of a primary malignancy can be followed by rapid outgrowth of metastases. This observation illustrates that primary tumors might exert an effect on growth of their metastases and that primary tumor and metastases may not have parallel growth patterns. In human CRCs, resection of the primary tumor was associated with a modest increase in cancer cell proliferation of synchronous hepatic metastases and a significant decrease in metastatic tumor cell apoptosis. These findings suggest that primary tumors can inhibit growth of their metastases (Peeters et al. 2006).
Pathogenic Features of Liver Metastases: Tumor Self-seeding and Cross-seeding in Metastasis
Introduction
According to classical concepts, metastasis has been considered to be a unidirectional process, whereby cancer cells are released by, or actively emigrate from, the primary tumor and seed cells into lymph nodes and to remote organs. This pathogenetic view, oriented on a mode “as the river flows,” has not been questioned for a long time. There is now evidence that metastasis is a multidirectional process, whereby cancer cells can not only seed to distant sites but also back to the primary tumor. The process of recolonizing of the primary tumor and its premetastatic niche is termed, tumor self-seeding. This hypothesis is based on the presence of tumor cell-supporting noncancerous cells not only in remote tissues but also in the primary tumor. The self-seeding model may answer many open questions regarding the complexity of the metastatic process (Norton and Massagué 2006; Norton 2008; Kim et al. 2009; reviews: Leung and Brugge 2009; Aguirre-Ghiso 2010; Hahnfeldt 2010; Norton 2011; Comen et al. 2011; Sleeman et al. 2011; Comen 2012; Comen and Norton 2012). In mice tumor models, it was shown that the self-seeding process can select more aggressive cells involved in cancer progression (Kim et al. 2009). Circulating tumor cells were found to enhance primary tumor growth, probably through stromal paracrine effects (Hahnfeldt 2010).
Homing Mechanisms in Tumor Self-seeding
How are tumor cells attracted to reinfiltrate primary tumors? Circulating tumors studied in mice secrete factors (“seed-derived factors”) that favor stromal recruitment and angiogenesis also in the primary lesion, including the chemokine CXCL1 (Kim et al. 2009). It has been shown that the protein chromogranin A inhibits the shedding of cancer cells into circulation from primary tumors, as well as the reinfiltration of primary tumors, via decreased vascular leakage in tumors and inhibition of transendothelial migration of cancer cells (Dondossola et al. 2012).
Pathogenic Features in Liver Metastases: Cell Clone Ecology Hypothesis
In the cell clone ecology hypothesis, it is assumed that the survival and fate of cell clones that behave like “parasites” in the organism and result in cancer are governed by the principles of ecology. The hypothesis is based on the concept that mutated and aneuploid cell clones undergoing progressive genomic instability are prone to degradation rather than becoming “successfully progressing clones,” with an inherent risk to become extinct or enfeebled to become a benign condition. In order to establish a “fit” clone, the cells of a so-called transient clone must undergo cell-cell fusion (the cell fusion model of cancer progression and metastasis). Cell-cell fusion provides, according to this hypothesis, a sex-like mode of reproduction essential for an ecologically fit parasite organism, provides the opportunity required by tumors to rejuvenate cell lines containing abnormal and instable genomes, and serves to overcome erosion of telomeres during clone expansion (Parris 2006a, b).
Pathogenic Features in Liver Metastases: Cancer Cell-Normal Cell Fusion Theory of Metastasis
Introduction
Invasion and spread of cancer cells require an intricate interaction between the tumor cells and normal cells of their invaded tissue environment, involving complex patterns or mutual cross talk between tumor cells, stromal cells, and leukocytes (the so-called seed and soil theory; review : Mareel and Madani 2006). In this complex interplay, cells involved create close contacts through cell-to-cell adhesion and enter a complex interactomics (van der Bij et al. 2005). This may potentially lead to the secretion of factors involved in tumor-stromal interactions (e.g. the matricellular protein SPARC; Podhajcer et al. 2008) and mutual signaling via exchange of signaling substances between normal cells and tumor cells. For example, secreted activated leukocyte adhesion molecule (sALCAM) attenuates melanoma cell invasion (van Kilsdonk et al. 2008). Leukocytes infiltrating tumors facilitate dissemination in that they disrupt intercellular junctions and cell surface adhesion molecules (Man et al. 2011). Leukocytes in contact with tumor cells can create a premetastatic niche (Oppenheimer 2006), but they may also act as myeloid-derived suppressor cells (review: Nardin and Abastado 2008). Furthermore, information may be exchanged between stem cells and cancer cells via horizontal genomic transfer (large-scale transfer of DNA and chromatin; Glinsky 2005). This has been suggested for cancer cells expressing antigen of tumor-associated macrophages (TAMs) (Shabo and Svanvik 2011). However, there is evidence of a more intimate interaction between normal cells and cancer cells (Lagarde 1986). It has been found that macrophages and other bone marrow-derived cells can fuse with cancer cells forming heterologous chimeras (Vignery 2005; Vignery 2008). Cell-to-cell fusion results in a complex sharing of several cellular features by the chimeras and the eventual emergence of novel types of behavior, including a metastatic phenotype (Lagarde and Kerbel 1985; Parris 2008). Somatic cell fusion is a potent source of genetic rearrangement leading to potentially metastatic cell variants (Larizza and Schirrmacher 1984; Carter 2008). In vitro fusion of a nonmetastatic tumor cell type with a bone marrow-derived macrophage results in the tumor cell’s high metastatic capacity (Larizza et al. 1984a). In animal tumor xenograft models, this phenomenon was associated with tumor metastasis (review : Pawelek and Chakraborty 2008).
Macrophage-Tumor Cell Chimeras
It is known that diverse types of malignant neoplastic cells acquire distinct sets of macrophage properties, including morphological appearance, surface adhesion, phagocytosis, motile behavior, and membrane lipid composition (Huysentruyt et al. 2008). This phenomenon has led to the concept of “cancer as a macrophage-mediated autoaggressive disease” (Muntarova and Kovarik 1987). It has been observed that such features may be acquired through heterologous cell-to-cell hybridization (Kerbel et al. 1983; Lagarde and Kerbel 1985). Tumor cell fusion with leukocytes is a source of myeloid traits in cancer, including the acquisition of typical motile behaviors (Rachkovsky et al. 1998; Pawelek 2005). Also the distinct features of tumor-associated macrophages (TAMs) may be acquired by tumor cells via cell fusion (review: Pawelek et al. 2006). Fusion of melanoma cells with macrophages results in acquired melanocyte stimulating hormone-inducible chemotaxis in the tumor cells (Rachkovsky and Pawelek 1999). Macrophage-melanoma cell fusion-induced hybrids upregulate N-acetylglucosaminyltransferase V (beta 1,6-branching; Gnt-V) (Chakraborty et al. 2001), acquire specific motility patterns, are highly metastatic in vivo, and express macrophage-associated traits of increased Gnt-V (Chakraborty and Pawelek 2003; Chakraborty and Pawelek 2007). Gnt-V forms beta 1,6 branching on the trimannosyl terminus of N-glycans, causing the production of beta 1,6 Glc-NAc-bearing oligosaccharide, important for the adhesion and motile behavior of both normal granulocytes and tumor cells. In macrophage-melanoma cell hybrids, these oligosaccharides colocalize with coarse melanin granules (Rupani et al. 2004). It has been proposed that mechanisms allowing escape from the extracellular matrix are important for migration and invasion, and such escape strategies may be acquired through cell fusion (review: Parris 2006b). Macrophages are capable to fuse with epithelial cells of murine intestinal tumors, resulting in nuclear reprogramming with the expression of unique subsets of transcripts (Powell et al. 2011). There is suggestive evidence that the highly metastatic variant ESb of the T cell lymphoma Eb is derived from spontaneous fusion with a host macrophage (Larizza et al., 1984b). Leukocyte-cancer cell fusion might act as the initiator for the use of aerobic glycolysis as a metabolic energy source of cancer cells, the Warburg effect (Lazova et al. 2011).
Tumor Cell-Normal Cell Chimeras
Native or damaged tumor cells can fuse with nonneoplastic host cells, e.g., following irradiation (Wiener et al. 1974a; Ber et al. 1978). Heterospecifc chimeras are a mechanism for horizontal transmission of malignancy (Goldenberg 2012). Normal diploid cells fused to malignant neoplastic cells can suppress the malignant phenotype in the chimeras (Harris et al. 1969; Wiener et al. 1974b). On the other hand, murine melanoma–macrophage hybrids showed enhanced metastatic behavior (Rachkovsky et al. 1998). A fusion-induced alteration in the cell surface structure, involving N-glycosylation of membrane proteins mediated by N-acetylglucosaminyltransferase V, is involved in this mechanism (Sodi et al. 1998; Chakraborty et al. 2001).
Tumor Cell-Tumor Cell Chimeras
There is strong evidence that tumor cells can form hybrids/chimeras among each other by cell fusion. The capability to fuse is not restricted by the type of cell origin or cell lineages involved, in that epithelial cells can form somatic hybrids with mesenchymal cells or germ cell tumor cells (Peterson and Weiss 1972; Litwack and Croce 1979; Fortuna et al. 1989). Fusion of tumor cells, also in vivo, can alter the biological behavior of the cells and effect invasion and spread. Spontaneous fusion of two mouse tumor cell subpopulations resulted in a more aggressive tumor cell variant (Miller et al. 1989), in part with enhanced metastatic potential (Mi et al. 2012), but loss of malignancy of hybrids derived from two murine malignant cell lines has also been observed (Jami and Ritz 1975). A predominance of a metastatic phenotype has been observed in hybrids formed by fusion of mouse and human melanoma cells (van Golen et al. 1996). Certain oncogenic features expressed in tumor cell chimeras can behave in a switchable dominant manner (Zimmermann et al. 1981).
Fusion of Intact Cancer Cells with Cancer Cell Components
Cells can not only fuse with intact partner cells but also with parts of the partner cell body, e.g., organelles and plasma membrane vesicles. Fusion of plasma membrane vesicles from highly metastatic cancer cells affect arrest and metastasis of blood-borne tumor cells (Poste and Nicolson 1980). Fusion of plasma membrane vesicles from highly metastatic cancer cells with blood-borne tumor cells can modify the arrest and mestatatic behavior of the recipient cells (Poste and Nicolson 1980).
Stem Cell-Tumor Cell Chimeras
As a mechanism of pathogenesis of cancer it has long been hypothesized that cancer cells might arise from a hybrid cell which derives from normal somatic cell fusion but obtains a proliferative advantage (Qian 1993). On the other hand, it has been suggested that distinct features of stem cells can be transferred to tumor cells through cell fusion. According to this concept, cancer can result from a fusion between an “altered” premalignant cell and a bone marrow-derived stem cell, aneuploidy as a typical feature of tumor cells being the direct result of this fusion process. This model might explain striking similarities between stem cells and cancer cells (He et al. 2005).
Organelle Chimeras of Normal Cells
Through cell fusion, cells can uptake organelles from partner cells. The resulting organelle chimera is heteroplasmic (heteroplasmy). On a genomic level, heteroplasmy denotes a situation characterized by the presence of a mixture of more than one type of organelle genomes, mainly mitochondrial DNA and plastid DNA, within a cell or individual. However, the term heteroplasmy is most often employed to describe a distinct state of the mitochondrial genome. Mitochondrial heteroplasmy results from mutations in the mitochondrial genome, whereby microheteroplasmy with numerous independent mutations is normally found in organisms. There is evidence that the most dramatic effects of heteroplasmy on the fate of the chimeric cells are obtained in case of mitochondrial chimeras, which contain two or more sets of mitochondrial DNA (Hua et al. 2012). Very low-level heteroplasmy mitochondrial DNA variations are an inherited trait in humans (Guo et al. 2013). Normal mammalian cells can even be propagated after integration of organelles as foreign as those of plants, e.g., chloroplasts (Nass 1969).
Heterosis
Heterosis or hybrid vigor (synonym: outbreeding enhancement) denotes the phenomenon that hybrids of two genetically pure cell lines grow more rapidly or give rise to more cells than the parental pure lines. The phenomenon of heterosis results in increased yield of cellular offspring and therefore increased biomass (Shull 1948; McDaniel and Sarkissian 1966; Baranwal et al. 2012; Groszmann et al. 2013). Effects of gene dosage imbalances play a significant role in heterosis. The underlying mechanisms seem to involve cumulative positive effects in the differential expression of sets of genes on yield-producing metabolic pathways (reviews: Kamb 2003; Baranwal et al. 2012). For a heterotic phenotype to occur, genetic and genomic studies have shown that gene expression in hybrids is regulated by the interactions of the two parental epigenetic systems and their genomes (review: Groszmann et al. 2013).
Cell Chimeras and Nuclear Alterations
Fusion of two contiguous tumor cells will increase the chromosome content of the resultant chimera, and this increase of ploidy could facilitate and heighten the inherent genomic instability of the lineage. This phenomenon has been observed as spontaneous fusion between metastatic mammary tumor subpopulations (Miller et al. 1988; review: Hart 1983). Murine fusion-derived hepatocytes showed ploidy reductions (Duncan et al. 2009).
Cancer Cell Chimeras and Cell Differentiation
Progression of cancer, including the establishment of a metastatic phenotype, depends on the proliferative status and the differentiation of the neoplastic cells. It is known that hybrid formation between cells affects differentiation of the fusion partners. In hybridization experiments using cells of defined and different histotypes, it turned out that both parental determinations are retained by hybrid cells and that parental differentiation modes are repressed only in a mutually exclusive fashion (Fougère and Weiss 1978). On the other hand, fusion of interspecific cells (rat and mouse) demonstrated that one specific function of one of the fusion partners can be expressed in the hybrid cells (Peterson and Weiss 1972). In hybrids between murine melanoma and teratocarcinoma cells, the formation of “supermelanotic chimeras” depends on the activation of genes involved in differentiation (Watanabe 1984).
Fusion of Human Cells with Cells of Nonhuman Organisms
It has been theorized that normal cells might acquire “dangerous” genetic information by integration of genetic information other than that of viruses. One hypothesis suggests that tumorigenic cells in part originate from fusions between normal human cells and bacteria, the fusion product termed “bactocytes” (Shaw 2003).
Pathogenic Features of Liver Metastases: Transfer of Cell-Free Genomic and Signaling Components Between Metastatic Cells and Between Normal Cells and Tumor Cells. An Extended Concept of Metastasis
Introduction
There is evidence that genetic and signaling information can spread from cancer cells to other cancer cells or normal, nontransformed cells (review: Garcia-Olmo et al. 2012). Through such mechanisms, metastasis of cancer has lived a conceptual extension from spread of malignant cells to spread and intracorporeal distribution of subcellular elements and components.
Exosomes
Exosomes are defined as small membrane-bound vesicles which cells can release into their microenvironment and from there to blood and lymph. The morphogenesis and biogenesis of exosomes involve a process of inward budding of membrane compartments into the lumen of late endosomes, followed by the fusion of the proto-multivesicular bodies with the plasma membrane. The cargo of exosomes consists of noncoding RNAs (including microRNAs and onco-miRs), signaling substances, adhesion molecules, and lipids (Rak 2010; Ludwig and Giebel 2012). As exosomes carry and transport bioactive lipids, and are enriched in cholesterol and sphingolipids in comparison with their parental cells, exosomes can serve as structures mediating intercellular communication dependent on lipid signaling (Record et al. 2014). The transfer of this exosomal cargo may induce pathologic alterations at the exosomal terminals (so-called exosomopathies; Korc 2015). Circulating exosomes and their cargo can successfully be employed as molecular biomarkers for diagnosis, classification, and monitoring of various malignant neoplasms.
Circulating Nuclear DNA (fcDNA)
In cancers, release of intact nuclear DNA or of DNA fragments from cancer cells is a common phenomenon, due to ongoing decay of neoplastic cells and their nuclei caused by apoptosis and necrosis. This DNA enters circulation in the form of free circulating DNA (fcDNA; circulating nucleic acids in plasma and serum, CNAPS; Schwarzenbach et al. 2011; Garcia-Olmo and Garcia-Olmo 2012; Garcia-Olmo et al. 2012; Gonzalez-Masia et al. 2013). In addition to cancer cells, also normal cells and cells of benign tumor release fcDNA. Assessments of fcDNA can be used as diagnostic markers, molecular characterization of primary and metastatic tumors, and design of personalized therapies (Goessl 2003; Fleischhacker and Schidt 2010; Vlassov et al. 2010; Ulivi and Silvestrini 2013).
Circulating Nucleosomes (cNUCs)
Nucleosomes as complexes of nuclear DNA and histone proteins can be released as intact particles from stressed, dying, or dead cells, including cancer cells. In patients with various malignancies, plasma and serum concentrations of nucleosomes are frequently elevated (Gezer et al. 2013). This “nucleosomics” can serve as a biomarker, e.g., for the detection of colorectal cancer (Holdenrieder et al. 2014) and the prognostication in cancer patients undergoing chemotherapy (Stoetzer et al. 2012). Nucleosomes are released from cells stimulated intrinsically or extrinsically to undergo apoptotic cell death, but in certain cells, e.g., neutrophils, nucleosomes can also be released by an active secretion process (Holdenrieder et al. 2012). Increased circulating nucleosomes (cNUCs) are also detected in autoimmune diseases, psoriasis, sepsis, trauma, and situations of large tissue necrosis. As a vehicle for DNA, circulating nucleosomes in cancer patients can be employed similar to fcDNA for diagnostic and monitoring purposes (Holdenrieder et al. 2001; Holdenrieder et al. 2008, Holdenrieder and Stieber 2009; Stoetzer et al. 2012; Wittwer et al. 2013). Nucleosomes and in particular their histones can also form the cargo of exosomes. Interestingly, cancer patients show distinct posttranslational modifications, including trimethylated histone tails, of histones carried by exosomes (Gezer et al. 2012; Leszinski et al. 2012; Gezer and Holdenrieder 2014).
Circulating Mitochondrial DNA (ccfmtDNA)
Similar to nuclear DNA, also mtDNA can escape from damaged normal and cancer cells and enter circulation, either as free mtDNA or in the setting of mitochondria. Circulating mtDNA (circulating cell-free mtDNA, ccfmtDNA) increases with age and can act as so-called damage-associated molecular pattern (DAMP) agents and are considered to be a pathogenic component for a low-grade chronic inflammatory status occurring in elderly subjects, a condition termed “inflamm-aging” (review : Pinti et al. 2014). mtDNA can undergo characteristic mutational changes in various tumors. Circulating cancer-derived mutant mtDNA can therefore be used as a predictive biomarker in several neoplasms (Ellinger et al. 2012; Uzawa et al. 2012; Yu 2012).
microRNAs (miRNAs) and Other Noncoding RNAs
Micro-RNAs play an important role in the pathogenesis of metastases, as they control the expression of stem cell molecules and molecules involved in invasion and spread (Nicoloso et al. 2009). All examined biological fluids in the body contain extracellular miRNAs that are nuclease resistant. In patients with cancer, neoplastic cells can release miRNA and via this mechanism transfer part of their molecular signature into the organism. In addition to represent a cancer marker, extracellular miRNA are considered molecules with an important cell-to-cell communication function (Turchinovich et al. 2013). Part of miRNAs released into the extracellular space enter blood and lymph circulation and thus become circulating miRNAs. As these miRNAs are highly stable, they are suitable as diagnostic cancer markers that can easily be detected and measured. Circulating miRNAs have now been utilized as markers for several solid neoplasms and hematologic malignancies (Zheng et al. 2013). In particular, plasma miRNA have been identified and evaluated for the early detection, monitoring, and outcome prediction of CRCs and their metastases (Giraldez et al. 2013; Luo et al. 2013; Kjersem et al. 2014). Certain species of miRNA are characteristic for CRCs, such as circulating miRNA-106a, −130b, −378, and −484 (Kjersem et al. 2014; Zanutto et al. 2014). MicroRNA signatures can discriminate between colorectal cancer recurrences to lymph nodes and liver and between CRC metastases and primary hepatic tumors (Drusco et al. 2014). Lymph node metastases of colorectal cancer express distinct patterns of long noncoding RNAs (lncRNAs) (Han et al. 2014), a phenomenon that might, similar to microRNAs, be transferred to remote areas in the body. Apart from microRNAs, other types of noncoding RNAs can be released into circulation, including small interfering RNA (Valiunas et al. 2015).
Exosome-Derived MicroRNAs (miRNAs)
Apart from miRNAs freely circulating in blood and lymph following their release from normal and cancer cells, miRNA can also travel in circulation as cargo located within exosomes (Camacho et al. 2013; Kosaka et al. 2013). Exosomal miRNAs (exomiRNAs) are thought to have a significant role in intercellular communication and transfer of specific signals, as circulating exomiRNA can be taken up by recipient cells to alter gene expression in these cells via RNA interference. This mechanism can induce several functional changes in recipient cells, including induction of pro-inflammatory cytokine expression (Mobergslien and Sioud 2014); exomiRNAs are increasingly employed as noninvasive biomarkers for diagnosing and screening of malignancies (Cazzoli et al. 2013).
References
Aguirre-Ghiso JA (2010) On the theory of tumor self-seeding: implications for metastasis progression in humans. Breast Cancer Res 12:304
Akishima-Fukasawa Y, Nakanishi Y, Ino Y, Moriya Y, Kanai Y, Hirohashi S (2009) Prognostic significance of CXCL12 expression in patients wirh colorectal carcinoma. Am J Clin Pathol 132:202–210
Ansieau S, Hinkal G, Thomas C, Bastid J, Puisieux A (2008) Early origin of cancer metastases. Dissemination and evolution of premalignant cells. Cell Cycle 7:3659–3663
Baranwal VK, Mikkilineni V, Zehr UB, Tyagi AK, Kapoor S (2012) Heterosis: emerging ideas about hybrid vigour. J Exp Bot 63:6309–6314
Bednarz-Knoll N, Alix-Panabières C, Pantel K (2012) Plasticity of disseminating cancer cells in patients with epithelial malignancies. Cancer Metastasis Rev 31:673–687
Ber R, Wiener F, Fenyö EM (1978) Proof of in vivo fusion of murine tumor cells with host cells by universal fusers. J Natl Cancer Inst 60:931–933
Bugyi B, Didry D, Carlier MF (2010) How tropomyosin regulates lamellipodial actin-based motility: a combined biochemical and reconstituted motility approach. EMBO J 29:14–26
Burger JA, Kipps TJ (2006) CXCR4: a key receptor in the crosstalk between tumor cells and the microenvironment. Blood 107:1761–1767
Camacho L, Guerrero P, Marchetti D (2013) MicroRNA and protein profiling of brain metastasis competent cell-derived exosomes. PLoS One 8, e73790
Carter A (2008) Cell fusion theory: can it explain what triggers metastasis? J Natl Cancer Inst 100:1279–1281
Cazzoli R, Buttitta F, Di Nicola M, Malatesta S, Marchetti A, Rom WN, Pass HI (2013) microRNAs derived from circulating exosomes as noninvasive biomarkers for screening and diagnosing lung cancer. J Thorac Oncol 8:1156–1162
Chakraborty AK, Pawelek JM (2003) GnT-V, macrophage and cancer metastasis: a common link. Clin Exp Metastasis 20:365–373
Chakraborty AK, Pawlek J (2007) Beta 1,6-branched oligosaccharides regulate melanin content and motility in macrophage-melanoma fusion hybrids. Melanoma Res 17:9–16
Chakraborty AK, Pawelek J, Ikeda Y, Miyoshi E, Kolesnikova N, Funasaka Y, Ichichhashi M et al (2001) Fusion hybrids with macrophage and melanoma cells up-regulate N-acetylglucosaminyltransferase V, beta1-6 branching, and metastasis. Cell Growth Differ 12:623–630
Comen EA (2012) Tracking the seed and tending the soil: evolving concepts in metastatic breast cancer. Discov Med 14:97–104
Comen E, Norton L (2012) Self-seeding in cancer. Recent Results Cancer Res 195:13–23
Comen E, Norton L, Massagué J (2011) Clinical implications of cancer self-seeding. Nat Rev Clin Oncol 8:369–377
Croft DR, Olson MF (2008) Regulating the conversion between rounded and elongated modes of cancer cell movement. Cancer Cell 14:349–351
Dawson JC, Legg JA, Machesky LM (2006) Bar domain proteins: a role in tubulation, scission and actin assembly in clathrin-mediated endocytosis. Trends Cell Biol 16:493–498
Dewan MZ, Ahmed S, Iwasaki Y, Ohba K, Toi M, Yamamoto N (2006) Stromal cell-derived factor-1 and CXCR4 receptor interaction in tumor growth and metastasis of breast cancer. Biomed Pharmacother 60:273–276
Diamond E, Lee GY, Akhtar NH, Kirby BJ, Giannakakou P, Tagawa ST, Nanus DM (2012) isolation and characterization of circulating tumor cells in prostate cancer. Front Oncol 2:131
Do Carmo A, Patricio I, Cruz MT, Cavalheiro H, Oliveira CR, Lopes MC (2010) CXCL12/CXCR4 promotes motility and proliferation of glioma cells. Cancer Biol Ther 9:56–65
Dondossola E, Crippa L, Colombo B, Ferrero E, Corti A (2012) Chromogranin A regulates tumor self-seeding and dissemination. Cancer Res 72:449–459
Drusco A, Nuovo GJ, Zanesi N, Di leva G, Pichiorri F, Volinia S, Fernandez C, Antenucci A, Costinean S et al (2014) MicroRNA profiles discriminate among colon cancer metastasis. PLoS One 9:e96670
Duncan AW, Hickey RD, Paulk NK, Culberson AJ, Olson SB, Finegold MJ, Grompe M (2009) Ploidy reductions in murine fusion-derived hepatocytes. PLoS Genet 5, e1000385
Ellinger J, Müller DC, Müller DC, Hauser S, Heukamp LC, von Ruecker A, Bastian PJ et al (2012) Circulating mitpchondrial DNA in serum: a universal diagnostic biomarker for patients with urological malignanices. Urol Oncol 30:509–515
Fleischhacker M, Schmidt B (2010) Free circulating nucleic acids in plasma and serum (CNAPS) – useful fort he detection of lung cancer patients? Cancer Biomark 6:211–219
Fortuna MB, Dewey MJ, Furmanski P (1989) Cell fusion in tumor development and progression: occurrence of cell fusion in primary methycholanthrene-induced tumorigenesis. Int J Cancer 44:731–737
Fougère C, Weiss MC (1978) Phenotypic exclusion in mouse melanoma-rat hepatoma hybrid cells: pigment and albumin production are not reexpressed simultaneously. Cell 15:843–854
Garcia-Olmo DC, Garcia-Olmo D (2012) Circulating nucleic acids in plasma and serum: an intriguing phenomenon. Expert Opin Biol Ther 12(suppl 1):S1–S2
Garcia-Olmo DC, Picazo MG, Garcia-Olmo D (2012) Transformation of non-tumor host cells during tumor progression: theories and evidence. Expert Opin Biol Ther 12(suppl 1):S199–S207
Gezer U, Holdenrieder S (2014) Post-translational histone modifications in circulating nucleosomes as new biomarkers in colorectal cancer. In Vivo 28:287–292
Gezer U, Mert U, Ozgür E, Yörüker EE, Holdenrieder S, Dalay N (2012) Correlation of histone methyl marks with circulating nucleosomes in blood plasma of cancer patients. Oncol Lett 3:1095–1098
Gezer U, Ustek D, Yörüker EE, Cakiris A, Abaci N, Leszinski G, Dalay N, Holderieder S (2013) Characterization of H3K9me3- and H4K20me3-associated circulating nucleosomal DNA by high-throughput sequencing in colorectal cancer. Tumour Biol 34:329–336
Giraldez MD, Lozano JJ, Ramirez G, Hijona E, Bujanda L, Castells A, Gironella M (2013) Circulating microRNAs as biomarkers of colorectal cancer: results from a genome-wide profiling and validation study. Clin Gastroenterol Hepatol 11:681–688
Giuliani C, Troglio F, Bai Z, Patel FB, Zucconi A, Malabarba MG, Disanza A, Stradal TB et al (2009) Requirements for F-BAR proteins TOCA-1 and TOCA-2 in actin dynamics and membrane trafficking during caenorhabditis elegans oocyte growth and embryonic epidermal morphogenesis. PLoS Genet 5(10):E1000675
Glinsky GV (2005) Death-from-cancer signatures and stem cell contribution to metastatic cancer. Cell Cycle 4:1171–1175
Goessl C (2003) Diagnostic potential of circulating nucleic acids for oncology. Expert Rev Mol Diagn 3:431–442
Goldenberg DM (2012) Horizontal transmission of malignancy by cell-cell fusion. Expert Opin Biol Ther 12(suppl 1):S133–S139
Gonzalez-Masia JA, Garcia-Olmo D, Garcia-Olmo DC (2013) Circulating nucleic acids in plasma and serum (CNAPS): applications in oncology. Onco Targets Ther 6:819–832
Groszmann M, Greaves IK, Fujimoto R, Peacock WJ, Denis ES (2013) The role of epigenetics in hybrid vigour. Trends Genet 29:684–690
Guo Y, Li CI, Sheng Q, Winther JF, Cai Q, Boice JD, Shyr Y (2013) Very low-level heteroplasmy mtDNA variations are inherited in humans. J Genet Genomics 40:607–615
Hahnfeldt P (2010) Significance of tumor self-seeding as an augmentation to the classic metastasis paradigm. Future Oncol 6:681–685
Han J, Rong LF, Shi CB, Dong XG, Wang J, Wang BL, Wen H, He ZY (2014) Screening of lymph nodes metastasis associated lncRNAs in colorectal cancer patients. World J Gastroenterol 20:8139–8150
Harris H, Miller OJ, Klein G, Worst P, Tachibana T (1969) Suppression of malignancy by cell fusion. Nature 223:363–368
Hart IR (1983) Tumor cell hybridization and neoplastic progression. Symp Fundam Cancer Res 36:133–143
He X, Tsang TC, Pipes BL, Ablin RJ, Harris DT (2005) A stem cell fusion model of carcinogenesis. J Exp Ther Oncol 5:101–109
Hirakawa H, Shibata K, Nakayama T (2009) Localization of cortactin is associated with colorectal cancer development. Int J Oncol 35:1271–1276
Holdenrieder S, Stieber P (2009) Clinical use of circulating nucleosomes. Crit Rev Clin Lab Sci 46:1–24
Holdenrieder S, Stieber P, Bodenmüller H, Busch M, Fertig G, Fürst H, Schalhorn A et al (2001) Nucleosomes in serum of patients with benign and malignant diseases. Int J Cancer 95:114–120
Holdenrieder S, Nagel D, Schalhorn A, Heinemann V, Wilkowski R, von Pawel J, Raith H et al (2008) Clinical relevance of circulating nucleosomes in cancer. Ann NY, Acad Sci 1137:180–189
Holdenrieder S, Kolligs FT, Braess J, Manukyan D, Stieber P (2012) Nature and dynamics of nucleosome release from neoplastic and non-neoplastic cells. Anticancer Res 32:2179–2183
Holdenrieder S, Dharuman Y, Standop J, Trimpop N, Herzog M, Hettwer K, Simon K, Uhlig S, Micallef J (2014) Novel serum nucleosomics biomarkers for the detection of colorectal cancer. Anticancer Res 34:2357–2362
Hua S, Lu C, Song Y, Li R, Liu X, Quan F, Wang Y, Liu J, Su F, Zhang Y (2012) High levels of mitochondrial heteroplasmy modify the development of ovine-bovine interspecies nuclear transferred embryos. Reprod Fertil Dev 24:501–509
Huysentruyt LC, Mukherjee P, Banerjee D, Shelton LM, Seyfried TN (2008) Metastatic cancer cells with macrophage properties: evidence from a new murine tumor model. Int J Cancer 123:73–84
Ide M, Saito K, Tsutsumi S, Tsuboi K, Yamaguchi S, Asao T, Kuwano H, Nakajima T (2007) Over-expression of 14-3-3sigma in budding colorectal cancer cells modulates cell migration in the presence of tenascin-C. Oncol Rep 18:1451–1456
Iwaya K, Oikawa K, Semba S, Tsuchiya B, Mukai Y, Otsubo T, Nagao T, Izumi M, Kuroda M et al (2007) Correlation between liver metastasis of the cololocalization of actin-related protein 2 and 3 complex and WAVE2 in colorectal carcinoma. Cancer Sci 98:992–999
Jami J, Ritz E (1975) Nonmalignancy of hybrids derived from two mouse malignant cells. II. Analysis of malignancy of LM (TK-) CI 1D parental cells. J Natl Cancer Inst 54:117–122
Jung A, Schrauder M, Oswald U, Knoll C, Sellberg P, Palmqvist R, Niedobitek G, Brabletz T, Kirchner T (2001) The invasion front of human colorectal adenocarcinomas shows co-localization of nuclear β-catenin, cyclin D1, and p16INK4A and is a region of low proliferation. Am J Pathol 159:1613–1617
Kamb A (2003) Consequences of nonadaptive alterations in cancer. Mol Biol Cell 14:2201–2205
Kanazawa H, Mitomi H, Nishiyama Y, Kishimoto I, Fukui N, Nakamura T, Watanabe M (2008) Tumour budding at invasive margins and outcome in colorectal cancer. Colorectal Dis 10:41–47
Kerbel RS, Lagarde AE, Dennis JW, Donaghue TP (1983) Spontaneous fusion in vivo between normal host and tumor cells: possible contribution to tumor progression and metastasis studied with a lectin-resistant mutant tumor. Mol Cell Biol 3:523–538
Kikuchi K, Takahashi K (2008) WAVE2-and microtubule-dependent formation of long protrusions and invasion of cancer cells cultured on three-dimensional extracellular matrices. Cancer Sci 99:2252–2259
Kim J, Takeuchi H, Lam ST, Turner RR, Wang HJ, Kuo C, Foshag L, Bilchik AJ, Hoon DS (2005) Chemokine receptor CXCR4 expression in colorectal cancer patients increases the risk for recurrence and for poor survival. J Clin Oncol 23:2744–2753
Kim MY, Oskarsson T, Acharyya S, Nguyen DX, Zhang XH, Norton L, Massagué J (2009) Tumor self-seeding by circulating cancer cells. Cell 139:1315–1326
Kjersem JB, Ikdahl T, Lingiaerde OC, Guren T, Tveit KM, Kure EH (2014) Plasma microRNAs predicting clinical outcome in metastatic colorectal cancer patients receiving first-line oxaliplatin-based treatment. Mol Oncol 8:56–67
Klein CA (2000) The biology and analysis of single disseminated tumour cells. Trends Cell Biol 10:489–493
Klein CA (2009) Parallel progression of primary tumours and metastases. Nat Rev Cacner 9:302–312
Klein CA (2013) Selection and adaptation during metastatic cancer progression. Nature 501:365–372
Korc M (2015) Pancreatic cancer-associated diabetes is an “exosomopathy”. Clin. Cancer Res pii:clincanres.2990.2014
Kosaka N, Yoshioka Y, Hagiwara K, Tominaga N, Katsuga T, Ochiya T (2013) Trash and treasure: extracellular microRNAs and cell-to-cell communication. Front Genet 4:173
Koscielny S, Tubiana M (2010) Parallel progression of tumour and metastases. Nat Rev Cancer 10:156
Lagarde AE (1986) Sporadic somatic fusion between MDAY-D2 murine tumor cells and DBA/2 host cells: role in metastasis. Int J Cancer 37:905–910
Lagarde AE, Kerbel RS (1985) Somatic cell hybridization in vivo and in vitro in relation to the metastatic phenotype. Biochim Biophys Acta 823:81–110
Larizza L, Schirrmacher V (1984) Somatic cell fusion as a source of genetic rearrangement leading to metastatic variants. Cancer Metastasis Rev 3:193–222
Larizza L, Schirrmacher V, Pflüger E (1984a) Acquisition of high metastatic capacity after in vitro fusion of a nonmetastatic tumor line with a bone marrow-derived macrophage. J Exp Med 160:1579–1584
Larizza L, Schirrmacher V, Graf L, Pflüger E, Peres-Martinez M, Stöhr M (1984b) Suggestive evidence that the highly metastatic variant ESb of the T-cell lymphoma Eb is derived from spontaneous fusion with a host macrophage. Int J Cancer 34:699–707
Lazova R, Chakraborty A, Pawelek JM (2011) Leukocyte-cancer cell fusion: initiator of the Warburg effect in malignancy? Adv Exp Med Biol 714:151–172
Leszinski G, Gezer U, Siegele B, Stoetzer O, Holdenrieder S (2012) Relevance of histone marks H3K9me3 and H4K20me3 in cancer. Anticancer Res 32:2199–2205
Leung CT, Brugge JS (2009) Tumor self-seeding: bidirectional flow of tumor cells. Cell 139:1226–128
Liang Y, Niederstrasser H, Edwards M, Jackson CE, Cooper JA (2009) Distinct roles for CARMIL isoforms in cell migration. Mol Biol Cell 20:5290–5305
Litwack G, Croce CM (1979) Somatic cell hybrids between totipotent mouse teratocarcinoma and rat hepatoma cells. J Cell Physiol 101:1–8
Ludwig AK, Giebel B (2012) Exosomes: small vesicles participating in intercellular communication. Int J Biochem Cell Biol 44:11–15
Luo X, Stock C, Burwinkel B, Brenner H (2013) Identification and evaluation of plasma microRNAs for early detection of colorectal cancer. PLoS One 8, e62880
Man YG, Mason J, Harley R, Kim YH, Zhu K, Gardner WA (2011) Leukocyte-mediated cell dissemination and metastasis: findings from multiple types of human tumors. J Cell Biochem 112:1154–1167
Mareel M, Madani I (2006) Tumour-associated host cells participating at invasion and metastasis: targets for therapy ? Acta Chir Belg 106:635–640
McDaniel RG, Sarkissian IV (1966) Heterosis: complementation by mitochondria. Science 152:1640–1642
Mi R, Pan C, Bian X, Song L, Tian W, Cao F, Yin J, Peng H, Ma J (2012) Fusion between tumor cells enhances melanoma metastatic potential. J Cancer Res Clin Oncol 138:1651–1658
Miller FR, McInerney D, Rogers C, Miller BE (1988) Spontaneous fusion between metastatic mammary tumor subpopulations. J Cell Biochem 36:129–136
Miller FR, Mohamed AN, McEachern D (1989) Production of a more aggressive tumor cell variant by spontaneous fusion of two mouse tumor subpopulations. Cancer Res 49:4316–4321
Mobergslien A, Sioud M (2014) Exosome-derived miRNAs and cellular miRNAs activate innate immunity. J Innate Immun 6:105–110
Morimura S, Suzuki K, Takahashi K (2009) BetaPIX and GIT1 regulate HGF-induced lamellipodia formation and WAVE2 transport. Biochem Biophys Res Commun 382:614–619
Muntarova M, Kovalik J (1987) Is cancer a macrophage-mediated autoaggressive disease? Lancet 1:952–954
Murphy PM (2001) Chemokines and the molecular basis of cancer metastasis. N Engl J Med 345:833–835
Nakamura T, Mitomi H, Kikuchi S, Ohtani Y, Sato K (2005) Evaluation of the usefulness of tumor budding on the prediction of metastasis to the lung and liver after curative excision of colorectal cancer. Hepatogastroenterology 52:1432–1435
Nardin A, Abastado JP (2008) Macrophages and cancer. Front Biosci 13:3494–3505
Nass MM (1969) Uptake of isolated chloroplasts by mammalian cells. Science 165:1128–1131
Nicoloso MS, Spizzo R, Shimizu M, Rossi S, Calin GA (2009) MicroRNAs – the micro steering wheel of tumour metastases. Nat Rev Cancer 9:293–302
Norton L (2008) Cancer stem cells, self-seeding, and decremented exponential growth: theoretical and clinical implications. Breast Dis 29:27–36
Norton L (2011) Tumor self-seeding in breast cancer. Clin Adv Hematol Oncol 9:541–542
Norton L, Massagué J (2006) Is cancer a disease of self-seeding? Nat Med 12:875–878
Ogawa T, Yoshida T, Tsuruta T, Tokuyama W, Adachi S, Kikuchi M, Mikami T, Saigenji K, Okayasu I (2009) Tumor budding is predicitive of lymphatic involvement and lymph node metastases in submucosal invasive colorectal adenocarcinomas and in non-polypoid compared with polypoid growths. Scand J Gastroenterol 44:605–614
Okuyama T, Oya M, Yamaguchi M (2002) Budding (sprouting) as a useful prognostic marker in colorectal mucinous carcinoma. Jpn J Clin Oncol 32:412–416
Oppenheimer SB (2006) Cellular basis of cancer metastasis: a review of fundamentals and new advances. Acta Histochem 108:327–334
Ottaiano A, Franco R, Aiello Talamanca A, Liguori G, Tatangelo F, Delrio P, Nasti G et al (2006) Overexpression of both CXC chemokine receptor 4 and vascular endothelial growth factor proteins predicts early distant relapse in stage II-III colorectal cancer patients. Clin Cancer Res 12:2795–2803
Palmqvist R, Sellberg P, Oberg A, Tavelin B, Rutegard JN, Stenling R (1999) Low tumour cell proliferation at the invasive margin is associated with a poor prognosis in Dukes’ stage B colorectal cancers. Br J Cancer 79:577–581
Parris G (2006a) The cell clone hypothesis and the cell fusion model of cancer progression and metastasis: history and experimental support. Med Hypotheses 66:76–83
Parris G (2006b) The cell clone ecology hypothesis and the cell fusion model of cancer progression and metastasis (II): three pathways for spontaneous cell-cell fusion and escape from the intercellular matrix. Med Hypotheses 67:172–176
Parris GE (2008) Cell-cell fusion is the rate-limiting step in causation and progression of clinically significant cancers. Cancer Genet Cytogenet 185:113
Pawelek JM (2005) Tumour-cell fusion as a source of myeloid traits in cancer. Lancet Oncol 6:988–993
Pawelek JM, Chakraborty AK (2008) The cancer cell-leukocyte fusion theory of metastasis. Adv Cancer Res 101:397–444
Pawelek J, Chakraborty A, Lazova R, Yilmaz Y, Cooper D, Brash D, Handerson T (2006) Co-opting macrophage traits in cancer progression: a consequence of tumor cell fusion? Contrib Microbiol 13:138–155
Peeters CF, de Waal RM, Wobbes T, Westphal JR, Ruers TJ (2006) Outgrowth of human liver metastases after resection of the primary colorectal tumor: a shift in the balance between apoptosis and proliferation. Int J Cancer 119:1249–1253
Peterson JA, Weiss MC (1972) Expression of differentiated functions in hepatoma cell hybrids: induction of mouse albumin production in rat hepatoma-mouse fibroblasts hybrids. Proc Natl Acad Sci U S A 69:571–575
Pinti M, Cevenini E, Nasi M, De Biasi S, Salvioli S, Monti D, Benatti S, Gibellini L, Cotichini R et al (2014) Circulating mitochondrial DNA increases with age and is a familiar trait: implications for “inflamm-aging”. Eur J Immunol 44:1552–1562
Podhajcer OL, Benedetti L, Girotti MR, Prada F, Salvatierra E, Llera AS (2008) The role of the matricellular protein SPARC in the dynamic interaction between the tumor and the host. Cancer Metastasis Rev 27:523–537
Portyanko A, Kovalev P, Gorgun J, Cherstvoy E (2009) Beta(III)-tubulin at the invasive margin of colorectal cancer: possible link to invasion. Vorchows Arch 454:541–548
Poste G, Nicolson GL (1980) Arrest and metastasis of blood-borne tumor cells are modified by fusion of plasma membrane vesicles from highly metastatic cells. Proc Natl Acad Sci U S A 77:399–403
Powell AA, Anderson EC, Davies PS, Silk AD, Pelz C, Impey S, Wong MH (2011) Fusion between intestinal epithelial cells and macrophages in a cancer context results in nuclear reprogramming. Cancer Res 71:1497–1505
Prall F (2007) Tumour budding in colorectal carcinoma. Histopathology 50:151–162
Qian LW (1993) A hypothesis on the pathogenesis of cancer: cancer might arise following an event of normal somatic cell fusing. Med Hypotheses 41:521–524
Rachkovsky M, Pawelek J (1999) Acquired melanocyte stimulating hormone-inducible chemotaxis following macrophage fusion with Cloudman S91 melanoma cells. Cell Growth Differ 10:517–524
Rachkovsky M, Sodi S, Chakraborty A, Avissar Y, Bolognia J, McNiff JM, Platt J, Bermudes D et al (1998) Melanoma x macrophage hybrids with enhanced metastatic potential. Clin Exp Metastasis 16:299–312
Rahimi M, George J, Tang C (2010) EGFR variant-mediated invasion by enhanced CXCR4 expression through transcriptional and post-transcriptional mechanisms. Int J Cancer 126:1850–1860
Rak J (2010) Microparticles in cancer. Semin Thromb Hemost 36:888–906
Record et al. (2014). http://www.ncbi.nlm.nih.gov/pubmed/24140720
Rupani R, Handerson T, Pawelek J (2004) Co-localization of beta 1,6-branched oligosaccharides and coarse melanin in macrophage-melanoma fusion hybrids and human melanoma cells in vitro. Pigment Cell Res 17:281–288
Schwarzenbach H, Hoon DS, Pantel K (2011) Cell-free nucleic acids as biomarkers in cancer patients. Nat Rev Cancer 11:426–437
Shabo I, Svanvik J (2011) Expression of macrophage antigens by tumor cells. Adv Exp Med Biol 714:141–150
Shaw A (2003) Bactocytes: a new cancer hypothesis. Med Hypotheses 60:739–741
Shen X, Arunyan A, Jackson D, Thomas RM, Lowy AM, Kim J (2010) Chemokine receptor CXCR4 enhances proliferation in pancreatic cancer cells through AKT and ERK dependent pathways. Pancreas 39:81–87
Shull GH (1948) What is “heterosis”? Genetics 33:439–446
Sleeman JP (2012) The metastatic niche and stromal progression. Cancer Metastasis Rev 31:429–440
Sleeman JP, Nazarenko I, Thiele W (2011) Do all roads lead to Rome? Routes to metastasis development. Int J Cancer 128:2511–2526
Sodi SA, Chakraborty AK, Platt JT, Kolesnikova N, Rosemblat S, Keh-Yen A, Bolognia JL et al (1998) Melanoma x macrophage fusion hybrids acquire increased melanogenesis and metastatic potential: altered N-glycosylation as an underlying mechanism. Pigment Cell Res 11:299–309
Stoecklein NH, Klein CA (2010) Genetic disparity between primary tumours, disseminated tumour cells, and manifest metastasis. Int J Cancer 126:589–598
Stoetzer OJ, Wittwer C, Lehner J, Fahmueller YN, Kohles N, Fersching DM, Leszinski G et al (2012) Circulating nucleosomes and biomarkers of immunogenic cell death as predictive and prognostic markers in cancer patients undergoing cytotoxic therapy. Expert Opin Biol Ther 12(suppl 1):S217–S224
Stylli et al. (2008). http://www.ncbi.nlm.nih.gov/pubmed/1118468901
Suetsugu S (2009) The direction of actin polymerization for vesicle fission suggested from membranes tubulated by the EFC/F-BAR domain protein FBP17. FEBS Lett 583:3401–3404
Suzuki A, Togasht K, Nokubi M, Koinuma K, Miyakura Y, Horie H, Lefor AT, Yasuda Y (2009) Evaluation of venous invasion by Elastica van Gieson stain and tumor budding predicts local and distant metastases in patients with T1 stage colorectal cancer. Am J Surg Pathol 33:1601–1607
Takahashi K, Suzuki K (2009) Membrane transport of WAVE2 and lamellipodia formation require Pak1 that mediates phosphorylation and recruitment of stathmin/Op18 to Pak1-WAVE2-kinesin complex. Cell Signal 21:695–703
Tarabichi M, Antoniou A, Saiselet M, Pita JM, Andry G, Dumont JE, Detours V, Maenhaut C (2013) Systems biology of cancer: entropy, disorder, and selection-drive evolution to independence, invasion and “swarm intelligence”. Cancer Metastasis Rev 32:403–421
Toyoda A, Kawana H, Azuhata K, Yu J, Omata A, Kishi H, Higashi M, Harigaya K (2009) Aberrant expression of human ortholog of mammalian enabled (hMena) in human colorectal carcinomas: implications for its role in tumor progression. Int J Oncol 34:53–60
Turchinovich A, Samatov TR, Tonevitsky AG, Burwinkel B (2013) Circulating miRNAs: cell-cell communication function ? Front Genet 4:119
Ulivi P, Silvestrini R (2013) Role of quantitative and qualitative characteristics of free circulating DNA in the management of patients with non-small cell lung cancer. Cell Oncol (Dordr) 36:439–448
Uzawa K, Baba T, Uchida F, Yamatoji M, Kasamatsu A, Sakamoto Y, Ogawara K et al (2012) Circulating tumor-derived mutant mitochondrial DNA: a predictive biomarker of clinical prognosis in human squamous cell carcinoma. Oncotarget 3:670–677
Valiunas V, Wang HZ, Li L, Gordon C, Valiuniene L, Cohen IS, Brink PR (2015) A comparison of two cellular delivery mechanisms for small interfering RNA. Physiol Rep 3, pii:e12286
van der Bij GJ, Oosterling SJ, Meijer S, Beelen RH, van Egmond M (2005) The role of macrophages in tumor development. Cell Oncol 27:203–213
Van Golen KL, Rison S, Staroselsky A, Berger D, Tainsky MA, Pathak S, Price JE (1996) Predominance of the metastatic phenotype in hybrids formed by fusion of mouse and human melanoma clones. Clin Exp Metastasis 14:95–106
van Kilsdonk JW, Wilting RH, Bergers M, van Muijen GN, Schalkwijk J, van Kempen LC et al (2008) Attenuation of melanoma invasion by a secreted variant of activated leukocyte cell adhesion molecule. Cancer Res 68:3671–3679
Vignery A (2005) Macrophage fusion: are somatic and cancer cells possible partners? Trends Cell Biol 15:188–193
Vignery A (2008) Macrophage fusion: molecular mechanisms. Methods Mol Biol 475:149–161
Vlassov VV, Laktionov PP, Rykova EY (2010) Circulating nucleic acids as a potential source for cancer biomarkers. Curr Mol Med 10:142–165
Wang LM, Kevans D, Mulcahy H, O’Sullivan J, Fennelly D, Hyland J, O’Donoghue D, Sheahan K (2009) Tumor budding is a strong and reproducible prognostic marker in T3N0 colorectal cancer. Am J Surg Pathol 33:134–141
Watanabe T (1984) Supermelanotic hybrids between mouse teratocarcinoma and mouse melanoma cells. Exp Cell Res 154:625–631
Wiener F, Fenyö EM, Klein G (1974a) Tumor-host cell hybrids in radio-chimeras. Proc Natl Acad Sci U S A 71:148–152
Wiener F, Klein G, Harris H (1974b) The analysis of maligancy by cell fusion. V Further evidence of the ability of normal diploid cells to suppress malignancy. J Cell Sci 15:177–183
Wittwer C, Boeck S, Heinemann V, Haas M, Stieber P, Nagel D, Holdenrieder S (2013) Circulating nucleosomes and immunigenic cell death markers HMGB1, sRAGE and DNAse in patients with advance pancreatic cancer undergoing chemotherapy. Int J Cancer 133:2619–2630
Yamaguchi H, Pixley F, Condeelis J (2006) Invadopodia and podosomes in tumor invasion. Eur J Cell Biol 85:213–218
Yamauchi H, Tigashi K, Kawamura YJ, Horie H, Sasaki J, Tsujinaka S, Yasuda Y, Konishi F (2008) Pathological predictors for lymph node metastasis in T1 colorectal cancer. Surg Today 38:905–910
Yu M (2012) Circulating cell-free mitochondrial DNA as a novel cancer biomarker: opportunities and challenges. Mitochondrial DNA 23:329–332
Yu L, Cecil J, Peng SB, Schrementi J, Kovacevic S, Paul D, Su EW, Wang J (2006) Identification and expression of novel isoforms of human stromal cell-derived factor 1. Gene 374:174–179
Zanutto S, Pizzamiglio S, Ghilotti M, Ravagnani F, Perrone F, Leo E, Pilotti S, Verderio P et al (2014) Circulating miR-378 in plasma: a reliable, haemolysis-independent biomarker for colorectal cancer. Br J Cancer 110:1001–1007
Zheng H, Liu JY, Song FJ, Chen KX (2013) Advances in circulating microRNAs as diagnostic and prognostic markers for ovarian cancer. Cancer Biol Med 10:123–130
Zimmermann A, Schaer JC, Schneider J, Molo P, Schindler R (1981) Dominant versus recessive behavior of a cold-and a heat-sensitive mammalian cell cycle variant in heterokaryons. Somatic Cell Genet 7:591–601
Zlobec I, Lugli A, Baker K, Roth S, Minoo P, Hayashi S, Terracciano L, Jass JR (2007) Role of APAF-1, E-cadherin and peritumoral lymphocytic infiltration in tumour budding in colorectal cancer. J Pathol 212:260–268
Zlobec I, Minoo P, Baumhoer D, Baker K, Terracciano L, Jass JR, Lugli A (2008) Multimarker phenotype predicts adverse survival in patients with lymph node-negative colorectal cancer. Cancer 112:495–502
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this entry
Cite this entry
Zimmermann, A. (2017). Pathogenic Features of Liver Metastasis: The Complex Cancer Cell–Cancer Cell, and Cancer Cell–Microenvironment Interactomes. In: Tumors and Tumor-Like Lesions of the Hepatobiliary Tract. Springer, Cham. https://doi.org/10.1007/978-3-319-26956-6_114
Download citation
DOI: https://doi.org/10.1007/978-3-319-26956-6_114
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26954-2
Online ISBN: 978-3-319-26956-6
eBook Packages: MedicineReference Module Medicine