Abstract
Background. This paper provides an overview of complex adaptive systems (CAS) theories and value in enabling change in an adaptive organisation. A CAS approach is interpreted here as a framework that assists thinking about the nature of quality improvement programmes with a focus on the people involved.
Objective. To identify key elements and characteristics of complex adaptive systems, drawing on examples from primary care informatics and clinical governance programmes.
Method. The research strategy is built on longitudinal case studies of the implementation of clinical governance arrangements in two United Kingdom (UK) Primary Care Organisations (PCOs) and includes a literature review to develop theoretical models relevant to the governance of quality improvement.
Results. The findings show that CAS theories are a valuable tool to help make sense of natural phenomena, which include human responses to problem solving. Approaches incorporate professional self-regulation that builds on the skills and strengths of the clinicians. There is considerable variation in the way in which consultation data is captured, recorded and organised, which includes free text, coded data and structured data collected using templates. An emphasis on incentivised information sharing led to local consensus on standard coding policies and models of data recording before any national contractual requirement. Informatics is acknowledged as a mechanism to link electronic health record outputs, quality improvement and resources. Investment in informatics, education and training is identified as development priorities in order to embed clinical governance principles in practice.
Conclusions. This study suggests that a CAS approach is useful in describing evolutionary change processes in semi-autonomous, networked PCOs. The adoption of new forms of governance does not necessarily neutralise previous models, but adds further dimensions to them. For instance, clinical governance models have moved from deterministic and “objective” factors, to incorporate cultural aspects and the exploitation of the potential offered by networks, interactions and feedback mechanisms enabled by developments in primary care informatics.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Change Enablers
- Primary Care Organisations (PCOs)
- Clinical Governance
- Quality Improvement Program
- Complex Adaptive Systems (CAS)
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
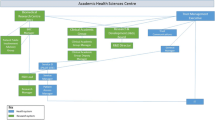
This paper stems from the researcher’s interest in the value of complex adaptive systems thinking to explain responses to the challenges faced when a systemFootnote 1 is perturbed, illustrated by the introduction of a quality improvement programme within the context of two United Kingdom (UK) National Health Service (NHS) Primary Care Organisations (PCOs) whose characteristics are shown in Fig. 18.1.
1 The Problem
Towards the end of the twentieth century, concerns about quality in the UK appeared to be widespread and increasing in frequency due to a number of high profile system failures that included The Shipman Inquiry [2]. The UK government argued that the NHS operated within an increasingly competitive world; it had become more demanding, less stable and the consequences of failure immediate. There was a perceived need for a more holistic approach because the NHS was providing variable quality of care to patients and resources were limited. Clinical governance, a quality improvement programme, was introduced described as:
“A framework through which the NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish.” [3]
The remit for clinical governance sat amongst other NHS reorganised structures and processes within an organisational maturity model that ranged from levels 1 to 4, (level 1 organisations providing advisory support to Health Authorities, to free standing Trusts at level 4). The “stepped” model designed to support an evolutionary approach at a pace that was to be agreed locally; justified in terms of reducing inequalities, inefficiencies and fragmentation in the quality of service provision, coupled with a need to maintain the NHS in financial balance. Networks were constructed as governance-linked structures forming Primary Care Organisations (PCOs) each serving populations ranging from 50,000 to over 250,000. Explicit within policy was a requirement to develop a “corporate culture” in which governance and quality improvement were to be seen as a shared enterprise “whereby initiatives would not be implemented in isolation” [4, p. 244]. In the light of proposals to develop PCOs, a “core” electronic patient record, integrated at the general practice level developed.
2 The Actors
Those initially involved in establishing clinical governance arrangements in the two studied PCOs included a board of 13 general practitioners, nurses, general managers and lay representatives in each organisation. Primary healthcare systems include multiple health professionals who often are dispersed across different physical locations.
3 The Argument
It is argued that a systems and complexity perspective has important implications to two complementary foci addressed in this paper. The first focus is on demonstrating the value of embedding technological innovation into existing complex adaptive systems such as primary care to support symmetry of information amongst stakeholders.
The second focus is to provide a framework for organisational change management that forms the basis for appropriate educational interventions across health care organisations [5, 6].
4 Research Strategy
Longitudinal case studies, based in two North of England NHS PCOs, conducted over 6 years in three phases between 2000 and 2006, traced responses to the implementation and development of clinical governance—a quality improvement programme. The first case study, Anytown, followed a relatively small PCO representing a population of approximately 70,000. The second followed Townend, representing a population of approximately 150,000. The PCOs consist of a mixture of urban, suburban and rural General Practices.
The decision to study the real world phenomenon of responses to governance, using a qualitative case study within a social constructionist ontological perspective, was based on the assumption that it was necessary to consider the meanings attributed to the experience of those involved in implementing and developing quality improvement programmes. In particular, the case study approach provides a “way of thinking about complex situations which takes the conditions into account” [7, p. 445]. The methodology includes a review of literature, survey, interviews, participant observer notes and documentation review.
Limitations of the case study methodology include a tendency to provide selected accounts. These are potentially biased and risk trivialising findings. Rooted in specific context, their generalisability to other contexts is limited by the extent to which contexts are similar. Reasonable attempts were made to minimise any bias. For example, multiple data gathering techniques were used that included a postal survey, face-to-face interviews, observation notes and document analysis, conducted within an overall qualitative case study. The diversity of data collection methods used in this study was an attempt to counterbalance the limitations highlighted in one method by strength from alternative techniques. For example, survey, as a method of data collection, allows a limited amount of information to be obtained at a given point in time; which was counterbalanced by the strength of in-depth, face-to-face interviews characterised as flexible, adaptable and associated with rich, illuminating data focused on human narratives, to obtain insight of phenomena and investigate underlying motives that self-administered surveys cannot.
5 Findings
5.1 Literature: An Overview of Complex Adaptive Systems
A CAS approach is interpreted as a framework that assists in thinking about the nature of primary care that allows consideration of its dynamic beyond the practice, the background of trend towards integrated organisations and federated models of practice [8]. A CAS perspective acknowledges primary care structures and moves towards semi-autonomous networked organisations. Key elements that characterise a CAS, based on the works of Reynolds [9], Kaufman [10] and Gell-Mann [11], include:
-
Multiple components, which interact with the environment, some may represent different world-views. Such systems are open systems that can be understood by observing, as a participant, and appreciating interrelated relationships, rich interaction, feedback and behaviour amongst components.
-
Self-organising networks: influence is exercised both by the system on the components and by the components on the system, termed mutual causation. The pervasive nature of non-linear, interlinked interactions can be observed in the patterning of behaviours that emerge in response to change, which cannot be predicted by studying the elements.
-
Co-evolution and adaptation of the system: there may be no central direction; small inputs may have large effects and vice versa.
-
Complex systems have a history which co-creates the present: non-linear interactions generate new properties, known as emergent behaviours of the system. Associated principles acknowledge that there is a need to respect ecologies by avoiding disturbance of natural systems with major change, and allowing time for properties to emerge.
Second-order systems based thinking moves away from simple objective observation to understand humans as participants in systems that allows for the flow of energy (motivation, information and innovation), networked interactions, continuous feedback and interdependencies.
Table 18.1 translates the CAS principles to primary care and emphasises its impact on understanding quality improvement programmes.
5.2 Clinical Governance
The components of clinical governance are presented in Table 18.2.
To function most effectively the system of managing performance depends on quality improvement, use of electronic health records and shared learning/education supported by informatics. This approach highlights the importance of lifelong learning, and the role of health informatics in actively managing individual performance in a primary care setting.
5.3 Electronic Health Records
Informatics is acknowledged as a mechanism to link electronic health record outputs, quality improvement and resources [12]. The use and access to electronic health records is essential in supporting the strategic drive for quality within the context of UK primary care, with its increased focus on multidisciplinary teams to deliver care. Information flows, feedback and co-evolution form the essence of processes in primary care systems; their iterative patterning co-creates coherent behaviours and outcomes. This establishes a service accountable to patients, open to the public and shaped by their perspectives. This has implications to primary care strategists in terms of the empowerment and responsibilities of local communities, which can be thought of as ecosystems that place an emphasis on a holistic “whole system” management perspective. Moreover, thinking from a CAS perspective suggests the benefit of considering both the linear and non-linear features of the system. Approaches incorporated professional self-regulation that built on the skills and strengths of the clinicians. There was considerable variation in the way in which consultation data was captured, recorded and organised, which included free text, coded data and structured data collected using templates. An emphasis on incentivised information sharing led to local consensus on standard coding policies and models of data recording well before it became a national contractual requirement [12]. Investment in informatics, education and training was identified as development priorities in order to embed clinical governance principles in practice, shown in Fig. 18.2.
Responses to the need for support of practices in developing aspects of quality improvement (Ellis and Herbert [6]). Reprinted with kind permission of copyright holder @2011 Primary Health Care Specialist Group, British Computer Society
5.4 Education: Through Shared Learning
Initial responses to the implementation of a quality improvement strategy focused on creating safe space, time for stakeholders to meet and bring about mutual adjustment, to support shared learning and establish partnerships, supported by informatics. These patient–public–professional partnerships show a willingness to exchange information about the quality of care. Those involved in this study reported the importance of creating an environment conducive to education and learning to develop this willingness, within a context of stakeholder and inter-professional working. This approach provides a wider perspective for learners, but also highlights the importance of inter-professional cooperation in the development, clinical management and monitoring of health information. Learning models that include “action learning” sets [13] and “learning organisation concepts” [14, 15] were adopted and manifest an understanding of the need for skills and knowledge to be embedded in experience, and allow reflection on that experience to create new meaning and enduring changes in behaviour. One explanation is that shared learning reflects a social world,
-
constructed by the perceptions and interests of those involved and the meaning they share, expressed as “I think it’s been quite, I think bringing professionals together is very powerful indeed and I think that’s (Clinical Education Society) been very, very good for achieving that and significant numbers turn up regularly.” (Chief Executive, lines 237... 238), and
-
supported by a perceived need to distribute responsibilities through team development “I don’t think I can fulfil my responsibilities for clinical governance by myself. I think that it [clinical governance] is something that is developed as part of a team and that it would be impossible to do really without that, and I am quite happy to be part of developing how a team is going to approach that and be part of delivering it in the practice.” (GP 4, lines 26... 29)
Figure 18.3 shows PCO characteristics and responses to system perturbation.
6 Themed Results
The findings reflect the following broad-based themes: mutual adjustment of a plurality of stakeholder perceptions, preferences and priorities; the development of networked information and communication systems, empowered by informatics; an emphasis on education and training to build capacity and capability. Participants reported a need to collaborate with a range of stakeholders that included multidisciplinary teams. This was found to lead to an evolving learning approach that contributed to the implementation and development of each PCO quality improvement programme, rapid increases in information exchanges and feedback. Preferred approaches incorporated professional self-regulation that built on the skills and strengths of the clinicians. Informatics was acknowledged as a mechanism to link electronic health record outputs, quality improvement and resources. Investment in informatics, education and training was identified as development priorities in order to embed quality improvement principles in practice.
7 Discussion
PCOs in this study behaved as CAS, reaching mutual agreement without the need to impose a particular world-view of the problem. The changes observed were achieved through collaborative approaches that incorporated multi-perspective world-views, local ownership and empowerment. Complex problem solving stimulated both a degree of reciprocity and earned autonomy between those involved. Each PCO community found novel local solutions to the problems brought about by the introduction of clinical governance policies, which led to the development of cooperation, open trusting relationships and understanding. Diversity amongst constituents needs to be protected to accommodate multifarious needs and priorities. This provides a degree of flexibility and resilience to problem solving capability within the whole system.
It is important that sufficient space is created, possibly facilitated through the provision of protected time, to allow collaboration and exchange of ideas. Managers need to focus on providing opportunities for regular social forums, such as team meetings, to develop a shared understanding and response to presenting problems. Top–down command and control management approaches are likely to obscure, or constrict, the novel behaviour that produced action and behavioural change found in working practices within the two PCOs.
The collection and distribution of expert knowledge was supported by an increased use of technology and informatics. For example, initial responses that reflected a strategic orientation towards demonstrating accountability translated into quality standards and conventions, which can be thought of as rules. These in turn led to the emergence of structures and sufficient order to establish a quality improvement programme supported by informatics. A move towards real-time recording of data during patient contact suggests that outputs from integrated electronic health records, such as NHS Quality and Outcomes Framework (QOF), facilitate management monitoring, authenticating and reporting of progress towards organisational objectives. This alleviates the need for external management to interfere with the operational and day-to-day activities at any one location in each PCO. The ongoing challenge is to embed health informatics into all clinical and non-clinical educational and training programmes as far as possible, to help health care staff manage information better in a world that is expecting more information empowered professionals, patients and public.
8 Conclusions
The application of the CAS framework provides insight into the emergent, socially constructed nature of the process of implementation where results are unpredictable. Clinical governance emerges from a set of complex interactions, rather than from rational planning. The theme suggests that the effectiveness of individuals may be related to their ability to acquire and learn specific skills and knowledge within available resources. Thinking from a CAS perspective has an important role to play in improving the public’s confidence in the delivery and quality of primary healthcare. Informatics complements this role based on the belief that the best decisions are based on the best information that flows throughout networked systems of healthcare to establish symmetry of information, the delivery of information technology enabled change and meet the future information requirements of patients, public and healthcare service.
9 Impact and Imperatives
This study has made a significant impact on the development and application of CAS models for technology implementation as well as the development of policy in relation to education and learning to manage health information technology [6, 12, 16]. Outcomes include the implementation of electronic records systems in the UK, supporting diversity in user support organisations, and the author’s work with the Royal College of General Practitioners resulting in improved patients’ online access to their electronic health records [17–19].
Twenty-first century primary health care systems will increasingly need to distribute responsibilities and encourage professional, patient public partnerships, supported by informatics. One problem for informatics that supports clinical practice is the tension between local specialism “the way we do things round here” and approaches that seek to standardise, recognising that outputs may be of interest to one or more stakeholders, and the need to reduce asymmetry of information. The use of informatics allows individuals and organisations to demonstrate how clinical teams can integrate the use of information and information systems within the broader context of continuous quality improvement. Practical tools such as training need analysis linked to competency frameworks [20] and quality methods are reported to improve system-wide performance (organisational learning), leading to improved patient care and economic benefit [16]. This approach integrates technology throughout care and business processes enabling continual learning through feedback. The motivation for change is explained as a need to facilitate access and delivery of effective quality health care within available resources through continuous feedback supported by electronic records, in response to the challenges brought about by social, economic, technical, political and organisational changes. It is envisaged that the development and use of open source software and “apps” on mobile devices by healthcare professionals, patients and the public will increase and impact on twenty-first century primary health care systems, ensuring flexible and agile solutions designed to meet the health, social and information needs of local, national and global populations. It is suggested that there is a need to increase the tolerance of diversity and failure, noting that levels of achievement can be variable, which will contribute to an environment conducive to innovation.
Notes
- 1.
The term “system” used throughout this paper follows the definition provided by Plesk [1]—the coming together of parts, their interaction and sense of purpose.
References
Plesk P. Re-designing healthcare with insights from the science of complex adaptive systems, crossing the quality chasm: a new health system for the 21st century. vol. 322. Washington, DC: National Academy of Sciences; 2000. p. 355. www.ihi.org/iomreport
The Shipman Inquiry. Presented to parliament by the Secretary of State for Health, September, 2000. Crown Copyright; 2000
Department of Health. Clinical Governance: quality in the new NHS, HSC (99) 065. London: Department of Health; 1999a
Jackson S. Exploring the possible reasons why the UK Government commended the EFQM excellence model as the framework for delivering governance in the new NHS. Int J Healthc Qual Assur. 1999;12(6–7):244–53
Ellis B. Managing governance programmes in primary care: lessons from case studies of the implementation of clinical governance in two primary care trusts [Ph.D.]. UCLan; 2008
Ellis B, Howard J. Clinical governance, education and learning to manage health information. Clin Gov: Int J. 2011; 16(4):337–52. Emerald Group Publishing Ltd. Available via: http://dx.doi.org/10.1108/14777271111175378
Keen J, Packwood T. Qualitative research: case study evaluation. Br Med J. 1995;311(7002):444–6
Ellis B. An overview of complexity theory: understanding primary care as a complex adaptive system. In: Sturmberg JP, Martin C, editors. Handbook on complexity in health. Chap. 29. NY: Springer Science and Business; 2013. ISBN: 978-1-4614-4997-3
Reynolds C W. Flocks, Herds and schools: a distributed behaviour model. In: SIGGRAPH ’87: Proceedings of the 14th Annual Conference on Computer Graphics and Interactive Techniques. 21(4); 1987. p. 25–34
Kaufman SA. Origins of order: self organisation and selection in evolution. Oxford: Oxford University Press; 1993
Gell-Mann M. The quark and the jaguar. New York: Freeman; 1994
Ellis B. Agreeing a PCG coding policy, BCS healthcare computing, 2001 (Conference Proceedings); 2001
Revans R. The origins and growth of action learning. Bromley: Chatwell-Bratt; 1982
Argyris C. On organizational learning. Reading: Addison-Wesley; 1999
Argyris C, Schön D. Organisational learning: a theory of action perspective. New York: McGraw Hill, 1978
Cowley C, Daws L, Ellis B. Health informatics and modernisation: bridging the gap. J Inform Prim Care. 2003;11(4):207–14
Royal College of General Practitioners. Patient online access to records roadmap; 2013. Available via http://www.rcgp.org.uk/~/media/Files/CIRC/POA/RCGP-Road-Map.ashx
de Lusignan S, Mold F, Sheikh A, Majeed A, Wyatt JC, Quinn T, Cavill M, Gronlund TA, Franco C, Chauhan U, Blakey H, Kataria N, Barker F, Ellis B, Koczan P, Arvanitis TN, McCarthy M, Jones S, Rafi I. Patients’ online access to their electronic health records and linked online services: a systematic interpretative review. Br Med J Open 2014;4: e006021. doi:10.1136/bmjopen-2014-006021
Mold F, de Lusignan S, Sheikh A, Majeed A, Wyatt JC, Quinn T, Cavill M, Gronlund TA, Franco C, Chauhan U, Blakey H, Kataria N, Barker F, Ellis B, Koczan P, Arvanitis TN, McCarthy M, Jones S, Rafi I. Patients’ online access to their electronic health records and linked online services: a systematic review. Br J Gen Pract. 2014. doi:10.3399/bjgp15X683941
Gillies A, Howard J. Managing change in process and people: combining a maturity model with a competency-based approach. Total Qual Manag Bus Excell. 2003; 14(7):779–87
Nicholls S, Cullen R, O’Neill S, Halligan A. Clinical governance: its origins and its foundations. Clin Perform Qual Health Care. 2000;8(3):172–8
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Ellis, B.S. (2016). The Value of Systems and Complexity Thinking to Enable Change in Adaptive Healthcare Organisations, Supported by Informatics. In: Sturmberg, J. (eds) The Value of Systems and Complexity Sciences for Healthcare. Springer, Cham. https://doi.org/10.1007/978-3-319-26221-5_18
Download citation
DOI: https://doi.org/10.1007/978-3-319-26221-5_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26219-2
Online ISBN: 978-3-319-26221-5
eBook Packages: MedicineMedicine (R0)