Abstract
Modern-day primary hyperparathyroidism (PHPT) usually presents as mild hypercalcemia and is often asymptomatic. Severe PHPT can present with pathologic fracture related to underlying associated bone disease (osteitis fibrosa cystica) that can often be mistaken for malignancy. Severe, long-standing hypocalcemia with a normal or increased parathyroid hormone (PTH) level, hungry bone syndrome, more commonly occurs after parathyroidectomy in the setting of severe, long-standing PHPT and in the presence of associated bone disease. Treatment with calcium and calcitriol may be required for months following surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Case Presentation
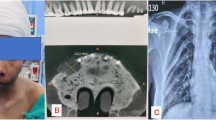
A 58-year-old female with a history of Hodgkin lymphoma treated with chemotherapy 20 years prior presented with left leg pain after a fall from standing height. Physical exam was notable for deformity of the left lower extremity and a large left-sided neck mass. Left hip x-ray confirmed a subtrochanteric femur fracture and a lytic lesion. Lucent lesions were noted on the left femoral shaft and patella (Fig. 2.1). Computed tomography (CT) scan of the chest, abdomen, and pelvis was notable for a 3.5 × 2.5 cm peritracheal nodule with local compression of the trachea. Widespread “metastatic” lytic lesions were noted diffusely throughout the axial and appendicular skeleton, and non-obstructing calyceal tip stones were also present. Laboratory results revealed a serum calcium of 15.6 mg/dL (8.9–10.2 mg/dL), alkaline phosphatase of 399 units/L (46–118 U/L), and a mild normocytic anemia.
Her hypercalcemia was treated with aggressive intravenous fluid administration, subcutaneous calcitonin, and zoledronic acid 4 mg. Her calcium level normalized. An ultrasound of the neck showed a solid mass encompassing the left lobe of the thyroid with sonographic features of malignancy. Parathyroid hormone (PTH) was 1510 pg/mL (15–65 pg/mL), and 25-hydroxyvitamin D was undetectable. The thyroid-stimulating hormone (TSH) level was 3.5 mIU/L (0.3–5.0 mIU/L). Fine-needle aspiration (FNA) of the neck mass was positive for neoplastic cells with Hürthle cell features.
Assessment and Diagnosis
The most likely diagnosis for a patient presenting with a pathologic fracture, lytic bone lesions, and severe hypercalcemia is widespread malignancy. The presence of a neck mass would also be consistent with a malignancy. The cytology of FNA does not prove or disprove malignancy. Although thyroid cancers such as follicular, medullary, or anaplastic thyroid carcinoma can metastasize to the bone, they are not generally associated with hypercalcemia. The profound elevation of PTH indicates a PTH-mediated hypercalcemia. The findings of severe hypercalcemia, significant elevation of PTH, and a neck mass are highly suspicious for parathyroid carcinoma [1–3]. Cytologic features alone on FNA cannot distinguish thyroid and parathyroid tissue nor parathyroid carcinoma from benign parathyroid tissue.
Lytic bone lesions are a common finding when widespread malignancy metastasizes to the bone and also in multiple myeloma which can also result in severe hypercalcemia. Osteitis fibrosa cystica is a skeletal disorder with lytic bone lesions related to hyperparathyroidism. Although rarely seen in the USA today, it occurs in severe long-standing primary hyperparathyroidism and parathyroid carcinoma. The proliferation and activity of osteoclasts in response to PTH leads to cystic defects that can produce pain and be locally aggressive, resulting in pathologic fractures. This is often initially mistaken for widespread malignancy [4]. However, the lesions are composed of numerous multinucleated giant cells admixed with fibroblasts and associated with interstitial hemorrhage marked by hemosiderin deposition, resulting in a brown appearance (“brown tumors”). The imaging and histology in isolation may not be diagnostic for osteitis fibrosa cystica due to overlapping features with other conditions but in addition to the biochemical and clinical picture, can lead to the correct diagnosis.
When parathyroid carcinoma is a concern, as in this setting, the surgical team should be alerted to this possibility so that the appropriate en bloc surgical resection can be performed (see Chap. 10). Also when parathyroid carcinoma is a concern, FNA is not diagnostic and has the potential for tumor seeding [5].
Management
The subtrochanteric femur fracture required resection and endoprosthetic replacement. The pathology from the operation revealed a brown tumor of hyperparathyroidism (Fig. 2.2). The patient then underwent neck surgery with excision of a 5.3 × 3.5 × 2.2 cm left superior parathyroid adenoma that was adherent to the left lobe of the thyroid but did not show invasion to suggest carcinoma. Postoperatively, hypocalcemia and hypophosphatemia developed, and she was treated with calcium, initially intravenous via central line, and calcitriol.
Hypocalcemia following parathyroidectomy is common but usually transient and not symptomatic. Hungry bone syndrome is the term used to describe prolonged, severe, symptomatic hypocalcemia, often with hypophosphatemia, accompanied by normal or elevated PTH levels [6]. This distinguishes it from postoperative hypoparathyroidism in which the PTH is low and the phosphorus is increased. Depending on the severity of hypercalcemia at the time of surgery, the development of hypocalcemia due to hypoparathyroidism may be delayed up to 48 h postoperatively. Postoperative hypoparathyroidism is often also accompanied by significant hypercalciuria, due to the loss of PTH-stimulated renal tubular reabsorption of calcium, and is not seen in hungry bone syndrome. The hypophosphatemia of hungry bone syndrome does not usually require replacement (unless <1.0 mg/dL), and intravenous phosphorus should be avoided due to the further lowering of calcium seen with it. In this case, hypocalcemia developed rapidly following parathyroidectomy, as her calcium was normalized preoperatively. Her coexistent vitamin D deficiency may also have contributed to hungry bone syndrome.
Reduction in bone resorption and increase in bone formation occur acutely after removal of the abnormal parathyroid tissue, resulting in the large influx of calcium into the bone. Although the incidence of hungry bone syndrome is not well defined, an older case series identified the volume of resected parathyroid adenoma, preoperative blood urea nitrogen, preoperative alkaline phosphatase, and older age as predictors of its development [7]. The presence of bone disease also is a risk factor [6]. The treatment of hungry bone syndrome requires calcium (sometimes intravenous) and calcitriol and may last for months. The use of bisphosphonates to lower bone remodeling and prevent the development of hungry bone syndrome has been reported in small series [8–10]. Our patient did receive preoperative zoledronic acid but still developed hungry bone syndrome. In contrast to bisphosphonates, preoperative cinacalcet therapy in secondary hyperparathyroidism may be a risk for lower calcium postoperatively [11, 12]. Prospective trials have not been performed to inform the optimal treatment or prevention of hungry bone syndrome.
Outcome
Over the 6 months following dismissal from the hospital, hypocalcemia resolved and calcitriol was discontinued. The bone lesions showed sclerosis consistent with interval healing.
Clinical Pearls/Pitfalls
-
Severe bone disease from PHPT (osteitis fibrosa cystica) can mimic metastatic malignancy.
-
Cytology on FNA cannot distinguish thyroid tissue from parathyroid tissue nor benign parathyroid tissue from parathyroid carcinoma.
-
A prior FNA can make histologic assessment of invasion difficult due to biopsy site changes and has a remote risk for tumor rupture or seeding tumor cells.
-
Postoperative hypocalcemia from hungry bone syndrome is more likely in patients with severe long-standing hyperparathyroidism and evidence of related bone disease.
References
Shane E. Clinical review 122: parathyroid carcinoma. J Clin Endocrinol Metab. 2001;86(2):485–93.
Wynne AG, et al. Parathyroid carcinoma: clinical and pathologic features in 43 patients. Medicine. 1992;71(4):197–205.
Robert JH, et al. Primary hyperparathyroidism: can parathyroid carcinoma be anticipated on clinical and biochemical grounds? Report of nine cases and review of the literature. Ann Surg Oncol. 2005;12(7):526–32.
Yang Q, et al. Skeletal lesions in primary hyperparathyroidism. Am J Med Sci. 2015;349(4):321–7.
Spinelli C, et al. Cutaneous spreading of parathyroid carcinoma after fine needle aspiration cytology. J Endocrinol Invest. 2000;23(4):255–7.
Witteveen JE, et al. Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: a systematic review of the literature. Eur J Endocrinol/Eur Fed Endocr Soc. 2013;168(3):R45–53.
Brasier AR, Nussbaum SR. Hungry bone syndrome: clinical and biochemical predictors of its occurrence after parathyroid surgery. Am J Med. 1988;84(4):654–60.
Lee IT, et al. Bisphosphonate pretreatment attenuates hungry bone syndrome postoperatively in subjects with primary hyperparathyroidism. J Bone Miner Metab. 2006;24(3):255–8.
Kumar A, Ralston SH. Bisphosphonates prevent the hungry bone syndrome. Nephron. 1996;74(4):729.
Davenport A, Stearns MP. Administration of pamidronate helps prevent immediate postparathyroidectomy hungry bone syndrome. Nephrology. 2007;12(4):386–90.
Wirowski D, et al. Cinacalcet effects on the perioperative course of patients with secondary hyperparathyroidism. Langenbeck’s Arch Surg/Deut Ges Chir. 2013;398(1):131–8.
Meyers MO, et al. Postoperative hypocalcemia after parathyroidectomy for renal hyperparathyroidism in the era of cinacalcet. Am Surg. 2009;75(9):843–7.
Conflict of Interest
All authors state that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Mayo Foundation for Medical Education and Research
About this chapter
Cite this chapter
Kearns, A.E. (2016). Severe Primary Hyperparathyroidism. In: Kearns, A., Wermers, R. (eds) Hyperparathyroidism. Springer, Cham. https://doi.org/10.1007/978-3-319-25880-5_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-25880-5_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-25878-2
Online ISBN: 978-3-319-25880-5
eBook Packages: MedicineMedicine (R0)