Abstract
From his first conceptualisation of attachment theory, Bowlby recognised the relationship between attachment and pain, and described pain as one of the triggers of the attachment system. Over the last 10 years, attachment theory has been investigated in relation to acute and experimental pain, various painful conditions, and outcomes from pain treatment programs. It has been considered in relation to pain experienced by adults, adolescents, and children. Insecure attachment has also been conceptualised as a risk factor for the development of chronic pain in the face of acute pain experiences. Attachment theory provides a useful lens through which to view the assessment and treatment of pain, informs research, and opens the field to exciting new possibilities. In this chapter, the literature on the associations between pain and attachment will be reviewed in order to understand how an attachment framework informs our understanding, and management, of pain. Special emphasis will be given to the Attachment-Diathesis Model of Chronic Pain.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
From his first conceptualisation of attachment theory, Bowlby recognised the relationship between attachment and pain, and described pain as one of the triggers of the attachment system: ‘…a child’s attachment behavior is activated especially by pain, fatigue, and anything frightening…’ (Bowlby 1998, p. 3). Even earlier, Engel (1959), the founder of the biopsychosocial model (Engel 1977), had considered a link between chronic pain and both childhood neglect and abuse. Perhaps as a result of these precedents, the value of using an attachment theoretical framework to understand pain in clinical settings was one of the earliest applications of attachment theory to physical health (Kolb 1982).
Empirical evidence hasburgeoned, particularly over the last 10 years (see Meredith 2013; Meredith et al. 2008). During this time, attachment theory has been investigated in relation to acute and experimental pain (Andrews et al. 2011; Meredith et al. 2006b), various painful conditions (Costa-Martins et al. 2014; McWilliams et al. 2000; Meredith et al. 2006a, 2007), and outcomes from pain treatment programs (Andersen 2012; Kowal et al. 2015). Attachment has been considered in relation to pain experienced by adults (Meredith et al. 2008), adolescents (Laird et al. 2015; Tremblay and Sullivan 2010), and children (Esposito et al. 2013; Walsh et al. 2008; Williamson et al. 2002). Insecure attachment has also been conceptualised as a risk factor for the development of chronic pain in the face of acute pain experiences (Meredith et al. 2008).
Attachment theory provides a useful lens through which to view the assessment and treatment of pain, informs research, and opens the field to exciting new possibilities. In this chapter, the literature on the association between pain and attachment will be reviewed in order to understand how an attachment framework informs our understanding, and management, of pain. Special emphasis will be given to the Attachment-Diathesis Model of Chronic Pain (Meredith et al. 2008), which provides a heuristic of the complex interplay of psychosocial factors linking attachment theory and the pain experience.
1 What Is Pain?
According to a well-accepted definition, pain is ‘…an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’ (Merskey and Bogduk 1994, p. 210). Acute pain lasts for a short period of time, while chronic pain is considered to be present if the pain has persisted unabated for at least 3 months.
The experience of pain is a necessary and important part of human life. Pain serves to alert us to the threat of injury, raising levels of distress and providing us with a cue to take rapid action to address the painful stimulus. Effective responses to painful stimuli may remove the cause of the pain, halt the discomfort and distress, curtail the risk of long-term tissue damage, and even enable us to evade death. These actions have consequences for the prevention of disability or disease and for ongoing participation in life’s roles. Importantly, pain also triggers the attachment system, which serves these same functions. With both the pain and attachment systems conferring advantages for survival, it is perhaps not surprising that they are linked.
Unfortunately, however, a painful stimulus is not always an alert to imminent danger and our responses are not always effective in obtaining positive outcomes, such as relieving the pain. In some cases, pain may persist long after the trigger has abated and may even defy medical and therapeutic efforts to explain and manage it. While there may be physiological factors, such as central sensitisation (Baron et al. 2013) at play, in such cases the intractability of the pain and the unrelenting levels of distress add an additional layer of suffering, which challenge any individual’s coping repertoire.
Pain and coping are both uniquely individual experiences, known to be affected by a complex interplay of biological, psychological, behavioral, social, and historical factors. In fact, psychological characteristics, such as a tendency to catastrophise or one’s level of pain self-efficacy (the strength of one’s belief in one’s ability to respond effectively to pain), are known to be stronger predictors of pain outcomes than either medical diagnosis or pain intensity (Arnstein 2000). Individual tendencies to respond to pain in specific ways, known as ‘pain behaviors’, also affect pain outcomes. Although a wide range of explanatory models have been developed to portray the complex interrelationships among the many pain-related factors, these models have thus far failed to explain the developmental origins of these individual differences (see Meredith et al. 2008). Attachment theory may fill this gap, as it represents a compelling, evidence-based model for understanding the development of social and personality factors that may contribute to either resilience or vulnerability in the face of pain. Attachment theory further provides an explanatory model for understanding the individual’s social environment (both past and present), and for considering how people are likely to experience the therapeutic relationship.
2 Attachment and Pain
During a painful experience, or when anticipating pain, the attachment system is activated, initiating a series of unique internal and behavioral responses. From the youngest of ages, pain causes an expression of distress, in order that someone will either remove the cause of the pain or provide comfort in the face of the associated distress. Over time, based on the quality of experiences with caregivers, these responses to painful stimuli become imbedded and habitual. In the following sections, the literature that pertains to the associations between attachment and pain will be reviewed, beginning with studies of associations between attachment and different types of pain. With links between attachment and chronic pain representing the most extensively investigated type of pain, this literature will be considered in Sect. 5.3.
2.1 Labour Pain
The experience of delivering a newborn infant represents a unique circumstance of acute pain, overlaid with implications for the woman’s transition to parenthood (or memories of that transition from previousbirths), the activation of her caregiving system, and her developing relationship with her infant. Like other sources of pain, labour is likely to activate the mother’s attachment system, and different attachment behaviors will be elicited depending on her internal working model. In such circumstances, the response of others to those behaviors can affect the pain experience. To date, only one study has been published which has considered the implications of attachment for women’s experience of pain during labour. Costa-Martins et al. (2014) demonstrated, among a sample of 81 pregnant women, that those who were insecurely attached reported significantly more labour pain and analgesic consumption compared to those who were securely attached. Although the authors noted that administration of patient-controlled epidural anaesthesia was provided using the standard protocol, no other information was available about the nature of any support provided to the women during labour. This field provides a valuable avenue for future research, as it is likely that interventions providing attachment-informed support to these more vulnerable mothers during this time may provide benefit. For example, a woman with a preoccupied attachment pattern may benefit more from the support of a doula, while a dismissing mother may prefer minimal and instrumental support.
2.2 Headache
Research has demonstrated links between attachment style and headache-related pain and disability, although the associations are complex. For example, Savi et al. (2005) showed that people with headaches were more likely to report insecure attachment styles compared with a matched control group without headaches. Esposito et al. (2013) identified a higher prevalence of avoidant, and lower prevalence of secure attachment in a sample of 219 children (6–11 years) with headaches, compared with 381 healthy controls. McWilliams and Bailey (2010) found that both anxious and avoidant attachment were positively associated with reports of headache pain, and especially with pain due to frequent or severe headaches, although this association was mediated by a history of depression or anxiety disorders. Unfortunately, these authors were not able to make a distinction between those with diagnosed migraine and those who simply perceived their headaches as ‘frequent or severe’. Because neurophysiological differences between migraineurs and non-migraineurs have been highlighted in the literature (Harriott and Schwedt 2014), these groups would be usefully separated in future research.
In contrast, Berry and Drummond (2014) found no difference in avoidant or anxious attachment between a control group of people who rarely experienced headaches and people with either episodic migraine or tension-type headaches. Their sample size was small (only 22 controls), however, and no details of participant matching were provided. Using an experimental paradigm, these authors did show that preoccupied (anxious) attachment was associated with intensity of headache, pain-related distress, and forehead pain in response to mild electric shocks to the forehead (Berry and Drummond 2014), and these results were retained when controlling for neuroticism and the other five-factor personality variables.
Insecure attachment has also been associated with higher levels of migraine-related disability (Rossi et al. 2004). In this study, attachment insecurity was the most significant predictor of disability for patients with episodic migraine; however, attachment was not a predictor of chronic migraine-related disability.
2.3 Cancer Pain
Pain is a common symptom of cancer, and there is some evidence that attachment is associated with coping with cancer-related pain (Gauthier et al. 2012). More specifically, Gauthier and colleagues showed that attachment anxiety was associated with perceptions of more punishing responses from others, while attachment avoidance was associated with perceptions of less frequent solicitous and distracting responses. An interaction was observed between attachment style and the relational context in coping with cancer pain, in that attachment anxiety was associated with higher levels of dependency – ‘Higher pain catastrophizing was associated with less frequent punishing responses only among anxiously attached patients who identified their spouse/partner as their supportive other’ (Gauthier et al. 2012, p. 1264). These social aspects of pain coping are discussed in more detail below. In addition, insecure (particularly avoidant) attachment has been shown to be more prevalent for people with cancer (e.g. Tacon et al. 2001) and to be linked with poorer quality of life in breast cancer survivors (Fagundes et al. 2014) (see Chap. 6).
2.4 Acute or Experimental Pain
Several investigations of healthy, pain-free people have been conducted using various experimental or induced-pain techniques, including a cold pressor apparatus, finger pressure, contact heat, and an ischaemic pain task. Results of these studies, while diverse, reveal important findings. As seen in Box 5.1, a wide range of factors have been empirically linked with insecure adult attachment in experimental studies (see Meredith 2013, for a detailed review).
Box 5.1. Factors that are empirically linked to insecure adult attachment in experimental pain studies
Higher
-
Perceived pain intensity
-
Pain catastrophising
-
Depression
-
Anxiety
-
Perceived stress
-
Neuroticism
Lower
-
Pain tolerance
-
Pain threshold
-
Perceived control of pain
-
Perceived ability to self-manage acute pain
This body of evidence suggests that insecure attachment precedes and, thus, may contribute causally to a problematic adjustment to pain. If extended to pain experienced in the real world, insecurely attached people responding in these ways to painful stimuli might plausibly have an inadequate resolution of pain and even be at increased risk for developing chronic pain. Convincing longitudinal evidence of this proposition is yet to be provided.
3 Attachment and Chronic Pain
The term ‘chronic pain’ encompasses a wide range of conditions including arthritis, low back pain, and generalised pain conditions such as fibromyalgia. Consistent with the conceptualisation of insecure attachment as a risk factor in the development of chronic pain, it has repeatedly been demonstrated that attachment insecurity, particularly fearful and dismissing attachment, is overrepresented in chronic pain populations (Davies et al. 2009; Kowal et al. 2015; Meredith et al. 2005, 2006a; Schmidt et al. 2002). For example, while there is evidence that approximately 65 % of people in normative samples are securely attached and 35 % are insecurely attached (Mickelson et al. 1997), in pain samples these numbers are more likely to be reversed (Kowal et al. 2015; Meredith et al. 2005). Insecure attachment has also been associated with having more pain sites (Davies et al. 2009) when compared with people with a secure attachment style.
In this section, I address early theoretical associations between attachment and chronic pain, the mechanisms through which attachment-related predispositions impact on chronic pain, and clinical implications for managing and preventing chronic pain.
3.1 Historical Context of the Links between Attachment and Chronic Pain
The first documented discourse linking attachment theory and chronic pain emerged more than 30 years ago (Kolb 1982). At thattime, Kolb drew parallels between the pain behaviors of his patients and their efforts to meet their attachment needs. For example, he viewed pain complaints as solicitation of caretaking behavior. In turn, the practitioner’s response and efficacy of interventions served to either alleviate or magnify these attachment-focused pain behaviors. Kolb advised that people in pain be approached with ‘noncritical acceptance’ and an effort to understand the origins of the threats they perceived. Based on this perspective, he viewed pain-complaining behaviors (including anger) as separation anxiety. He suggested that,
…attachment theory offers a significant new understanding that can expand our capacity to maintain gains in those who have achieved some control of their pain complaints…[and] help us to accept chronic pain complainers and provide guidelines for primary physicians and others who care for [these] persons…. (1982, p. 413)
In 1982, categories of attachment in adulthood were less clearly defined, and only attachment security versus insecurity was discussed. Since then, adult attachment styles have been elucidated, permitting more specific theoretical and empirical consideration.
For instance, Mikail et al. (1994) described the anticipated responses of people in each of four attachment categories (secure, dismissing, preoccupied, and fearful) to the presence of chronic pain. These responses are summarised in Table 5.1. Understanding the tendencies of people with different attachment styles enables us to predict the ways in which they may try to manage their pain and the possible consequences of these strategies, which may then provide targets for therapy. Given this degree of detail, it is perhaps surprising that the evidence to support these responses in chronic pain samples (as discussed in the next section) is still relatively limited, and it is not yet clear how much clinical impact these suggestions have had.
At the same time, Anderson and Hines (1994) described insecure attachment patterns as relative failures of early attachment support mechanisms, which leave the individual vulnerable to later stressors, such as pain. While these authors did not investigate attachment styles specifically, they gathered information about history of physical, sexual, and/or emotional abuse/neglect, abandonment, and substance abuse in primary caregivers. They suggested that these factors disrupt the child’s capacity to develop consoling relationships, such that later experiences of pain reactivate (or exacerbate) latent distress states in a self-perpetuating hyperarousal pattern. In contrast, a secure base in childhood, and the associated secure attachment pattern, was suggested to support one’s ability to tolerate and accommodate pain.
Anderson and Hines (1994) emphasised the impact of attachment security on one’s capacity to be consoled when in pain. That is, while the majority of people have developed relationships and/or activities (e.g. work, athletics) that they find consoling, these strategies are likely to be disrupted by pain. According to these authors, the less secure the attachment, the less consolable the person and the lower the person’s ability to tolerate pain. In addition, unremitting pain can be debilitating, leading to an undesirable level of vulnerability and dependency. These effects are understood to be more pronounced and difficult to manage for the more insecurely attached person. Thus, pain, related distress, and insecure attachment interact in a self-sustaining manner, with potentially incapacitating consequences (Anderson and Hines 1994).
Attachment-related coping strategies, many of which are relevant to pain behaviors, have been described in detail by Cole and colleagues (Cole-Detke and Kobak 1996; Dozier and Kobak 1992; Kobak et al. 1993) as either secure or defensive. While secure strategies involve timely and adaptive responses to stressors, defensive coping strategies may be either hyperactivating or deactivating (for detailed discussions of these strategies, see Fraley and Shaver 1997, 2000; Fraley et al. 2000).
Hyperactivation of the attachment system is akin to Anderson and Hines’ hyperaroused state and would be characteristic of preoccupied attachment. It involves exaggerating behaviors designed to attract care and attention, minimising distance from others, and hypervigilance towards events perceived as potential stressors. Conversely, deactivation of the attachment system suggests denial of attachment needs, avoidance of behaviors designed to attract attachment security, and denial or minimisation of the emotions and cognitions associated with these needs, resulting in a compulsive self-reliance typical of dismissing attachment. Finally, individuals with fearful attachment patterns use strategies associated with both coping extremes, often indiscriminately (Dozier, Stovall, and Albus 1999; Simpson and Rholes 2002). These behaviors have consequences for the individual in pain and are also represented in Table 5.1.
Case: Dismissing Attachment
Frank is a truck driver. His hands are rough, his cheeks ruddy, and his smile ready. He is known as a hard worker, typically working 12–16 h days, 6 days a week. He has no problem with this; his father had been a dairy farmer so Frank knew what hard work was. Frank did not have time for medical appointments and generally felt healthy, so did not see the need. Even when he fell and broke two ribs and his collar bone, he went back to work the next day, despite the pain, which he described as ‘not too bad’.
It was not until Frank was involved in a workplace accident that this changed. He was closing up his trailer when his rig rolled backwards, pinning him between the factory wall and his truck. Frank sustained fractured vertebrae, spinal injuries, and nerve and soft tissue damage to his lower back, legs, and buttocks. His medical and rehabilitation program was intensive, and he regained most of his musculoskeletal functioning; however, nothing worked to control the pain. Morphine and other prescription medications only ever ‘took the edge off’ for a short while, and he was uncomfortable being dependent on drugs. Frank now found that he could sit for only 10 minutes at a time before the pain forced him to move. This affected not only his capacity to work but also to fish, which was his other main interest in life.
When seen in treatment, Frank admitted that all he wanted to do was to be able to climb into his boat and float off into the river where he had always found solace. If he could not do this again, he did not see that life was worth living. He was angry with the specialists who had treated him, and admitted he held little stock in what they told him. He also seemed to hold little hope that this referral would result in any positive outcomes. Frank just wanted to be fixed and to get on with his life.
4 Mechanisms Linking Chronic Pain and Attachment
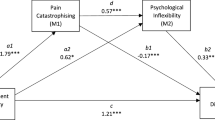
Meredith and colleagues (2008) have reviewed the available literature and proposed a heuristic pathway through which attachment insecurity could contribute to the development of chronic pain and to maladaptive outcomes when experiencing pain. According to this Attachment-Diathesis Model of Chronic Pain (Meredith et al. 2008; see Fig.5.1), attachment insecurity (column A) is likely to result in cognitive appraisals (column B) of:
The Attachment-Diathesis Model of Chronic Pain (From Meredith et al. 2008, used with permission from Elsevier Ltd.)
-
(a)
Pain as being more threatening and less manageable
-
(b)
The self as being less able to manage the pain and/or less deserving of support
-
(c)
Support as being less available and responsive
These appraisals are, in turn, theoretically associated with specific emotional responses (column C), including pain-related fear, depression, and anxiety, and less adaptive behavioral coping responses, including hypervigilance and pain catastrophising, delayed or inadequate help-seeking behavior, and limited pain coping strategies. As might be anticipated, these responses predispose insecurely attached individuals to more problematic pain experiences and poorer adjustment to pain (column D) compared with their more securely attached counterparts. Moreover, according to this model, attachment insecurity moderates the associations between appraisals/responses (B and C) and impact (D), as well as potentially impacting directly on the adjustment.
Until recently, evidence of these associations was only available in relation to experimental pain (see above). However, evidence is now available for a substantial number of relationships between attachment insecurity and aspects of chronic pain as follows:
Insecurity, in general, is related to:
-
(a)
Perceptions of diminished ability to control and decrease pain (Meredith et al. 2006a; Mikulincer and Florian 1998)
-
(b)
Appraisal of the pain as more intense (Kratz et al. 2012; MacDonald and Kingsbury 2006; McWilliams et al. 2000; Meredith et al. 2006a)
-
(c)
Appraisal of the pain as more threatening (Meredith et al. 2005; Mikulincer and Florian 1998)
-
(d)
Appraisal of the self as not being able to cope with the pain (Meredith et al. 2006a)
-
(e)
Reliance on more emotion-focussed and less problem-focussed coping strategies (Mikulincer and Florian 1998)
-
(f)
More emotional distress (Meredith et al. 2005) and depression (Ciechanowski et al. 2003; Meredith et al. 2007)
-
(g)
More pain-related disability (Davies et al. 2009; McWilliams et al. 2000)
Dismissing insecurity, specifically, is related to:
-
(a)
The tendency to cope by ignoring pain sensations and using coping self-statements (Meredith et al. 2006a)
-
(b)
More avoidant coping (Williamson et al. 2002)
Preoccupied insecurity is related to:
-
(c)
Less social coping (Kratz et al. 2012)
-
(d)
The tendency to catastrophise (Kratz et al. 2012; Meredith et al. 2006a)
In addition, Laird et al. (2015) recently tested predictions of the Attachment-Diathesis Model of Chronic Pain and found good model fit with their sample of 261 adolescents and young adults. These findings provide evidence for a range of mechanisms that explain the influence of attachment style on adjustment of people with chronic pain. In the following sections, additional mechanisms are considered through which attachment patterns may impact on the risk of developing chronic pain and on the pain experience, contributing to the overrepresentation of insecure attachment in chronic pain populations.
4.1 Help-Seeking and Treatment Adherence
Maunder and Hunter (2001) noted that insecure attachment is associated with altered help-seeking behavior (either under- or over-reliance on health services) and with lowered treatment adherence. If applied to pain, this suggests that insecurely attached people may engage in behaviors that diminish the opportunity for conditions to be diagnosed and treated in a timely manner, potentially resulting in more recalcitrant and painful conditions. Alternatively, they may visit the doctor more often, as a consequence of their incapacity to regulate the fear and distress caused by the pain, which may result in a range of unnecessary or inappropriate investigations and eventual disregard. Evidence supporting this was found in a sample of 111 people after treatment at a multidisciplinary pain treatment program, when associations between preoccupied attachment and high levels of pain-related healthcare visits over 12 months occurred (Ciechanowski et al. 2003). A similar finding emerged for people with fearful attachment, but only in the presence of catastrophising. As noted by Porter et al. (2007), these expectations deserve more attention in the field of chronic pain.
4.2 Attachment and Risk Taking
Taubman, Ben-Aria, and Mikulincer (2007) presented evidence, obtained from both community and clinical samples of adolescents and young adults, of links between insecure attachment and a range of risky behaviors. These included substance abuse (cigarettes, drugs, and alcohol), reckless driving, and unsafe sexual practices. Similar findings have been reported by Ahrens and colleagues (2012). These authors also demonstrated links between attachment anxiety and higher rates of unplanned pregnancy and increased risk of becoming HIV-positive. It is likely that these behaviors will predispose people to the development of painful conditions due to physical injury resulting from physical trauma, disease, or chronic conditions. Indeed, evidence suggests that insecure attachment is associated with a range of potentially painful and disabling health conditions. For example, preoccupied attachment has been linked with disorders of the cardiovascular system (stroke, heart attack), with reports of more physical symptoms (Ciechanowski et al. 2002; Feeney and Ryan 1994), and with impaired physical health (Maunder and Hunter 2008) (see Chap. 4).
4.3 Attachment and Pain-Related Activity Patterns
As noted earlier (Anderson and Hines 1994), people engage in activities that they find consoling. In pain-free samples, Hazan and Shaver (1990) have highlighted the use of work and other activities to self-regulate or avoid social demands. Some evidence from the chronic pain literature suggests that individuals may use activity avoidance or overutilisation to manage their pain. For example, high levels of engagement in productive tasks have been associated with overactivity when in pain (van Houdenhove 1986), which has, in turn, been linked to poorer emotional and physical functioning (Andrews et al. 2012). This makes activity levels primary targets in pain treatment programs, where participants are instructed in pacing techniques, in an attempt to support measured activity levels and avoid exacerbations of pain. However, there are attachment-related variations in the repertoire of activities that pain patients find consoling (Anderson and Hines 1994).
At present, only one study has investigated associations between attachment patterns and the activity patterns of people with chronic pain (Andrews et al. 2014). In a sample of 164 adults with chronic pain in a tertiary pain clinic, secure attachment was associated with less use of activity avoidance, preoccupied attachment was linked with higher levels of both avoidance and overactivity, and fearful attachment was associated with a combination of high levels of both overactivity and avoidance. Many of these associations were partly or wholly mediated by pain catastrophising. Thus, having insecure attachment may create vulnerability for the development of maladaptive activity levels for people in pain. Understanding the role of attachment insecurity in activity engagement may then optimise strategies taught in treatment (Andrews et al. 2015). This area represents a fertile vein for further research, with therapeutic implications for tailoring pacing instructions by type of attachment insecurity.
4.4 Attachment and Social Support
Social factors such as the presence, attentiveness, and solicitousness of others, social context, and non-verbal behaviors have long received attention in the pain field. Social support is an important part of the pain treatment milieu, and it is customary for pain management programs to provide information to family members of people in pain and to include them in aspects of treatment. In paediatric settings, family involvement is especially emphasised.
The role of partners, parents, and other attachment figures for the person in pain has been investigated, often with complex and even contradictory findings. This is likely due to the sheer number of factors that may moderate or mediate the associations between support and pain-related experiences. Two of these factors are the person’s attachment style and that of their partner. Individual differences exist in the nature of support that is sought and valued by people with different attachment styles, and the nature of support or caregiving that a person is comfortable providing. As a general rule, when in pain, the match between the available and the desired support is likely to have a considerable influence on perceptions of, and adaptation to, pain. When in pain, social cues from others can signal either safety or threat, resulting in heightened or diminished levels of stress (Kolb 1982). These perceptions can, in turn, affect the person’s expression of pain. For example, while a preoccupied person might be expected to magnify pain complaints, MacDonald (2008) found that preoccupied people who felt rejected were likely to report even lower pain thresholds than when they felt supported.
Other studies illustrate the complexity of this area. For example, Vervoort and colleagues (2010) found that when less securely attached children in pain catastrophised, they received negative responses from caregivers, but that more securely attached children catastrophising obtained positive responses. In contrast, Gauthier et al. (2012) found that preoccupied adults with cancer pain who catastrophised obtained more solicitous and distracting responses and less punishing responses. Partner or carer’s attachment styles influence their own adjustment, as well (Porter et al. 2007). For example, insecurely attached carers of children in pain have been shown to have higher levels of depression (Williamson et al. 2002).
Although convincing, the evidence linking attachment insecurity to mechanisms associated with negative outcomes in chronic pain remains largely correlational and little prospective data is available. It will be important for future research to consider longitudinal studies from normative samples to determine whether or not insecure attachment before the onset of pain predicts more problematic coping with acute pain over time, the development of chronic pain conditions, more difficulties managing these conditions, and more challenging long-term outcomes. Nevertheless, the amount of evidence accumulated does point to a role for attachment-informed approaches in the management of pain.
5 Implications of Attachment Theory for the Management of Pain
While it has long been known that a wide range of psychosocial factors are associated with pain coping, past efforts to identify these have often resulted in labels such as ‘hysterical’, which rarely contributed to helpful interventions (Anderson and Hines 1994). An attachment-informed approach in the management of pain has implications for what information we gather about people in pain, how we view the person with pain, the emphasis on the therapeutic relationship, and associated outcomes, as will be discussed below. An attachment perspective also has implications for the person’s own perception of their pain, their experience of their treatment, their self-management, and their willingness to adopt recommendations.
5.1 Information Gathering
An attachment perspective emphasises that a developmental history should be gathered before more intrusive investigations are considered. Without such a history, a pain presentation can be misunderstood. For example, dismissing individuals may minimise their pain and be undertreated, while preoccupied individuals might magnify their concerns and be overly investigated, exposed to intrusive interventions, and risk having future reports of pain ignored when no organic cause is identified. Use of an attachment perspective also highlights the need to inquire about the person’s relationships with significant others and their broader social network, in order to understand their available social support. Kolb (1982) noted that increased pain complaining may indicate that social attachments have been threatened, as illustrated by the case of Gina.
Case: Gina
Gina is a 67-year-old grandmother of four. She has been married for 51 years and has complained of severe pain throughout her body, with exacerbations in different parts of her body from moment to moment, for more than 10 years. She reports that she has sought assistance from a range of professionals, and while she initially finds some comfort, she quickly becomes disenchanted when progress slows or when she realises that the professional seems less attentive than they should be. Gina has had an extensive series of investigations, including blood tests, MRIs, and CT scans over the last 10 years, and was eventually diagnosed retrospectively as having had Ross River fever (a viral illness transmitted by mosquitoes) and as having osteoarthritis; however, no other abnormalities were found. She has been prescribed a range of medications including prednisone, diazepam, and fluoxetine. These treatments provided only limited pain relief.
Gina’s new GP collected a more detailed history and found that she hedged around questions about her marriage, implying that her husband has been abusive or at least neglectful of her needs and that life was inherently dissatisfying. Gina does not see her son or daughter as often as she would like and says they never make contact with her. She hinted that she wants more from her family than they are prepared to give. Over time Gina further disclosed that the reason she married young was that she was being sexually abused by her paternal grandfather.
This information highlighted Gina’s social isolation. It enabled the doctor to consider Gina’s pain presentation through a wider lens and to incorporate her emotional and social support needs into the treatment. In particular, the doctor’s office itself was experienced by Gina as a safe haven, where she could feel heard and supported.
5.2 The Therapeutic Relationship and Counter-transference
Kolb (1982) recognised that, for some people, the professionals involved in treating pain problems become ‘surrogate’ attachment figures. However, because of individual attachment-related differences, people in pain will prefer, or accept, different types of support from healthcare providers. If unrecognised, this seems likely to strain the therapeutic alliance and could be ameliorated if attachment style were taken into account. Consistent with this, Kowal (2015) suggested that the higher levels of insecure attachment identified in pain rehabilitation programs may be a result of negative healthcare relationships and consequent referral to tertiary level treatment programs. Within most pain clinics, however, there is a similar lack of consideration of attachment patterns or effort to tailor communication styles to suit the needs of individuals with different attachment styles.
In relation to spinal pain, Anderson and Hines (1994, p. 149) stated that, ‘It is our experience that the ability of the treatment team to form a consoling relationship with the patient is necessary for a successful outcome’, while Rossi et al. (2004, p. 567) noted ‘…that attachment style is a major variable in the regulation of the patient-physician relationship.’ Emphasising this point, Porter et al. (2007, p. 197) recently called for more research into ‘…the match between patient and caregiver attachment styles… [the] importance of provider sensitivity to attachment-related needs and motives, and tailoring caregiver interactions to patient attachment styles’. In fact, a person who does not feel that their attachment needs are met by their practitioner may engage in ‘attachment searching’ (Kolb 1982, p. 416) or seeking alternative sources of help. Kolb suggested some time ago that:
On the basis of attachment theory, it becomes clear that establishment of a trusting, expectant, and secure attachment base forms the fulcrum on which rests application of any indicated technical intervention to relieve painful distress…In so doing, the physician accepts the attachment behavior for what it is and without admonition. Contacts can be scheduled in such a way as to avoid or alleviate separation anxiety and arousal of attachment behaviors… by scheduling them to see the caretakers at regular intervals and on a fixed time schedule… It is extraordinarily important that the patient be greeted with interest, respect, and a willingness to accept the pain complaint as serious… Any unscheduled contact accepted without criticism increases the patient’s confidence…. (Kolb 1982, p. 416)
At the time that Kolb recognised this need, dismissing attachment was not recognised. Extending his insight to people with a dismissing style, however, who prefer to be self-sufficient, the clinician should guard against ‘taking them at face value’ and agreeing that they have no need of help. Inviting them back for further assessment conveys a willingness to listen and does not minimise or shame as previous attachment figures probably have. Simultaneously, one needs to avoid ‘crowding’ such an individual, or they will react by reducing contact, and the opportunity for effective intervention will be lost.
Regardless of the person’s attachment style, the clinician also needs to be aware of his or her own emotional and behavioral reactions, in order to optimally manage the interaction. The clinician’s reaction will, inevitably, be determined in part by his or her own attachment experiences, so it behoves us to appreciate our own attachment style and the manner in which it affects the development of the therapeutic alliance.
5.3 Outcomes from Pain Treatment Programs
Rossi et al. (2004, p. 567) recognised ‘…the influence of attachment style on … treatment response of patients with chronic pain syndromes’. A small amount of evidence suggests that insecure attachment may predict more limited responses to pain treatment programs. According to Andersen (2012), both secure and insecure groups demonstrated improved levels of anxiety and depression following cognitive behavioral intervention for chronic pain. However, the level of depression and anxiety for insecurely attached patients remained above the clinical level from pre- to post-treatment, while securely attached people scored below the clinical cutoff post-treatment. Similar results have also been found by Ciechanowski et al. (2003), Kowal et al. (2015), and Meredith et al. (2007). Proposed reasons for such findings included poorer therapeutic alliance, variations in treatment adherence and self-management, maladaptive coping strategies (more emotion-focussed or diverting strategies), lower levels of self-efficacy, and diminished emotional connection with the patient therapy group and participants. Interestingly, these reasons resemble the factors considered in the Attachment-Diathesis Model of Chronic Pain.
Andersen (2012) also found that insecurely attached people used significantly more opioids both before and after treatment compared to their securely attached counterparts. He suggested that the natural endogenous opioid system is not as easily activated by social interactions in insecurely attached people as it is in those who are securely attached, making them more vulnerable to opioid abuse.
Conclusion
Over a period of more than 30 years, the theoretical and empirical evidence of associations between attachment and pain has been accumulating. There is now greater awareness of the different mechanisms through which attachment may impact on pain and the ways in which understanding this association might improve the provision of services to people with, or at risk of developing, painful conditions. While many gaps still exist in this collective body of research, there are two pressing needs. The first is to obtain longitudinal evidence of the causal link between attachment insecurity and poor pain adjustment, and the second is to design and evaluate an attachment-informed treatment approach for people in pain.
References
Ahrens KR, Ciechanowski P, Katon W (2012) Associations between adult attachment style and health risk behaviors in an adult female primary care population. J Psychosom Res 72(5):364–370
Andersen TE (2012) Does attachment insecurity affect the outcomes of a multidisciplinary pain management program? The associations between the attachment insecurity, pain, disability, distress, and the use of opioids. Soc Sci Med 74:1461–1468
Anderson DJ, Hines RH (1994) In: Grzesiak RC, Ciccone DS (eds) Psychological vulnerability to chronic pain. Springer Publishing Company, New York
Andrews NE, Meredith PJ, Strong J (2011) Adult attachment, fear-avoidance and pain intensity in experimentally-induced pain. Eur J Pain 15:523–530
Andrews N, Meredith PJ, Strong J (2012) Activity pacing, avoidance, endurance, and associations with patient functioning in chronic pain: a systematic review and meta-analysis. Arch Phys Med Rehabil 93:2109–2121
Andrews N, Meredith PJ, Strong J, Donoghue G (2014) Adult attachment and approaches to activity in chronic pain. Pain Res Manag 19(6):317–327
Andrews N, Strong J, Meredith PJ, Gordon K, Bagraith K (2015) “It’s very hard to change yourself”: an exploration of overactivity in people with chronic pain using interpretative phenomenological analysis. Pain 156(7):1215–1231
Arnstein P (2000) The mediation of disability by self efficacy in different samples of chronic pain patients. Disabil Rehabil 22:794–801
Baron R, Hans G, Dickenson AH (2013) Peripheral input and its importance for central sensitization. Ann Neurol 74(5):630–636. doi:10.1002/ana.24017
Berry JKM, Drummond PD (2014) Does attachment anxiety increase vulnerability to headache? J Psychosom Res 76:113–120
Bowlby J (1998) A secure base: clinical applications of attachment theory. Routledge, London
Ciechanowski P, Walker EA, Katon WJ, Russo JE (2002) Attachment theory: a model for health care utilization and somatization. Psychosom Med 64:660–667
Ciechanowski P, Sullivan M, Jensen M, Romano J, Summers H (2003) The relationship of attachment style to depression, catastrophizing and health care utilization in patients with chronic pain. Pain 104:627–637
Cole-Detke H, Kobak R (1996) Attachment processes in eating disorder and depression. J Consult Clin Psychol 64(2):282–290
Costa-Martins JM, Pereira M, Martins H, Moura-Ramos M, Coelho R, Tavares J (2014) Attachment styles, pain, and the consumption of analgesics during labor: a prospective observational study. J Pain 15(3):304–311
Davies KA, Macfarlane GJ, McBeth J, Morriss R, Dickens C (2009) Insecure attachment style is associated with chronic widespread pain. Pain 143:200–205
Dozier M, Kobak RR (1992) Psychophysiology in attachment interviews: converging evidence for deactivating strategies. Child Dev 63(6):1473–1480
Dozier M, Stovall KC, Albus KE (1999) Attachment and psychopathology in adulthood. In: Cassidy J, Shaver PR (eds) Handbook of attachment: theory, research, and clinical applications. The Guildford Press, New York
Engel GL (1959) “Psychogenic” pain and the pain-prone patient. Am J Med 26:899–918
Engel GL (1977) The need for a new medical model: a challenge for biomedicine. Science 196:129–136
Esposito M, Parisi L, Gallai B, Di Dona A, Mavano SM, Rocella M, Carotenuto M (2013) Attachment styles in children affected by migraine without aura. Neuropsychiatr Dis Treat 9:1513–1519
Fagundes CP, Jaremka LM, Malarkey WB, Kiecolt-Glaser JK (2014) Attachment style and respiratory sinus arrhythmia predict post-treatment quality of life in breast cancer survivors. Psychooncology 23:820–826
Feeney JA, Ryan SM (1994) Attachment style and affect regulation: relationships with health behaviour and family experiences of illness in a student sample. Health Psychol 13(4):334–345
Fraley RC, Shaver PR (1997) Adult attachment and the suppression of unwanted thoughts. J Pers Soc Psychol 73(5):1080–1091
Fraley RC, Shaver PR (2000) Adult romantic attachment: theoretical developments, emerging controversies, and unanswered questions. Rev Gen Psychol 4(2):132–154
Fraley RC, Garner JP, Shaver PR (2000) Adult attachment and the defensive regulation of attention and memory: examining the role of preemptive and postemptive defensive processes. J Pers Soc Psychol 79(5):816–826
Gauthier LR, Rodin G, Zimmermann C, Warr D, Librach SL, Moore M, Shepherd FA, Gagliese L (2012) The communal coping model and cancer pain: the roles of catastrophizing and attachment style. J Pain 13(12):1258–1268
Harriott AM, Schwedt TJ (2014) Migraine is associated with altered processing of sensory stimuli. Curr Pain Headache Rep 18:458. doi:10.1007/s11916-014-1458-8
Hazan C, Shaver PR (1990) Love and work: an attachment-theoretical perspective. J Pers Soc Psychol 59:270–280
Kobak RR, Cole HE, Ferenz-Gillies R, Fleming WS, Gamble W (1993) Attachment and emotional regulation during mother-teen problem solving: a control theory analysis. Child Dev 64(1):231–245
Kolb LC (1982) Attachment behavior and pain complaints. Psychosomatics 23(4):413–425
Kowal J, McWilliams LA, Peloquin K, Wilson KG, Henderson PR, Fergusson DA (2015) Attachment insecurity predicts responses to an interdisciplinary chronic pain rehabilitation program. J Behav Med 38:518–526
Kratz AL, Davis MC, Zautra AJ (2012) Attachment predicts daily catastrophizing and social coping in women with pain. Health Psychol 31(3):278–285
Laird KT, Preacher KJ, Walker LS (2015) Attachment and adjustment in adolescents and young adults with a history of pediatric functional abdominal pain. Clin J Pain 31(2):152–158
MacDonald G (2008) Use of pain threshold reports to satisfy social needs. Pain Res Manag 13:309–319
MacDonald G, Kingsbury R (2006) Does physical pain augment anxious attachment? J Soc Pers Relat 23(2):291–305
Maunder RG, Hunter JJ (2001) Attachment and psychosomatic medicine: developmental contributions to stress and disease. Psychosom Med 63(4):556–567
Maunder RG, Hunter JJ (2008) Attachment relationships as determinants of physical health. J Am Acad Psychoanal Dyn Psychiatry 36:11–32
McWilliams LA, Bailey SJ (2010) Associations between adult attachment ratings and health conditions: evidence from the National Comorbidity Survey Replication. Health Psychol 29(4):446–453
McWilliams LA, Cox BJ, Enns MW (2000) Impact of adult attachment styles on pain and disability associated with arthritis in a nationally representative sample. Clin J Pain 16:360–364
Meredith PJ (2013) A review of the evidence regarding associations between attachment theory and experimentally-induced pain. Curr Pain Headache Rep 17(4):326
Meredith PJ, Strong J, Feeney JA (2005) Evidence of a relationship between adult attachment variables and appraisals of chronic pain. Pain Res Manag 10(4):191–200
Meredith PJ, Strong J, Feeney JA (2006a) Adult attachment, anxiety and pain self-efficacy as predictors of pain intensity and disability. Pain 123:146–154
Meredith PJ, Strong J, Feeney JA (2006b) The relationship of adult attachment to emotion, catastrophizing, control, threshold and tolerance in experimentally-induced pain. Pain 120(1–2):44–52
Meredith PJ, Strong J, Feeney JA (2007) Adult attachment variables predict depression before and after treatment for chronic pain. Eur J Pain 11(2):164–170
Meredith PJ, Ownsworth T, Strong J (2008) A review of the evidence linking adult attachment theory and chronic pain: presenting a conceptual model. Clin Psychol Rev 28(3):407–429
Merskey H, Bogduk N (eds) (1994) Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms, 2nd edn. IASP Press, Seattle
Mickelson KD, Kessler RC, Shaver PR (1997) Adult attachment in a nationally representative sample. J Pers Soc Psychol 73(5):1092–1106
Mikail SF, Henderson PR, Tasca GA (1994) An interpersonally based model of chronic pain: an application of attachment theory. Clin Psychol Rev 14(1):1–16
Mikulincer M, Florian V (1998) The relationship between adult attachment styles and emotional and cognitive reactions to stressful events. In: J. A. Simpson and W. S. Rholes (Eds.).Attachment Theory and Close Relationships. New York: Guilford Press, pp. 143–65
Porter LS, Davis D, Keefe FJ (2007) Attachment and pain: recent findings and future directions. Pain 128:195–198
Rossi P, Di Lorenzo G, Malpezzi MG, Di Lorenzo C, Cesarino F, Faroni J, Siracusano A, Troisi A (2004) Depressive symptoms and insecure attachment as predictors of disability in a clinical population of patients with episodic and chronic migraine. Headache 45:561–570
Savi L, Buccheri R, Tambornini A, De Martino P, Albasi C, Pinessi L (2005) Attachment styles and headache. J Headache Pain 6:254–257
Schmidt S, Nachtigall C, Wuethrich-Martone O, Strauss B (2002) Attachment and coping with chronic disease. J Psychosom Res 53:763–773
Simpson JA, Rholes WS (2002) Fearful-avoidance, disorganization, and multiple working models: some directions for future theory and research. Attach Hum Dev 4(2):223–229
Tacon AM, Caldera YM, Bell NJ (2001) Attachment style, emotional control, and breast cancer. Fam Syst Health 19(3):319–326
Taubman Ben-Aria O, Mikulincer M (2007) The effects of dispositional attachment orientations and contextual priming of attachment security on reckless driving. Transp Res F 10:123–138
Tremblay I, Sullivan MJL (2010) Attachment and pain outcomes in adolescents: the mediating role of pain catastrophizing and anxiety. J Pain 11(2):160–171
van Houdenhove B (1986) Prevalence and psychodynamic interpretation of premorbid hyperactivity in patients with chronic pain. Psychother Psychosom 45:195–200
Vervoort T, Goubert L, Crombez G (2010) Parental responses to pain in high catastrophizing children: the moderating effect of child attachment. J Pain 11(8):755–763
Walsh TM, McGrath PJ, Symons DK (2008) Attachment dimensions and young children’s response to pain. Pain Res Manag 13(1):33–40
Williamson GM, Walters AS, Shaffer DR (2002) Caregiver models of self and others, coping, and depression: predictors of depression in children with chronic pain. Health Psychol 21(4):405–410
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Meredith, P.J. (2016). Attachment Theory and Pain. In: Hunter, J., Maunder, R. (eds) Improving Patient Treatment with Attachment Theory. Springer, Cham. https://doi.org/10.1007/978-3-319-23300-0_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-23300-0_5
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-23299-7
Online ISBN: 978-3-319-23300-0
eBook Packages: MedicineMedicine (R0)