Abstract
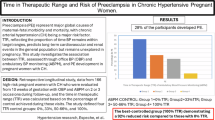
Gestational hypertension (GH) and preeclampsia (PE) are major causes of perinatal morbidity and mortality. The diagnosis of these conditions still relies on unreliable conventional clinic blood pressure (BP) measurements and inappropriate thresholds of ≥140/90 mmHg for systolic/diastolic BP. Noninvasive around-the-clock ambulatory BP monitoring (ABPM) investigations have documented predictable differences in the 24-h BP pattern between pregnant women who during the course of gestation will remain normotensive versus those who will develop GH or PE. In normotensive pregnancies, ambulatory BP steadily decreases until the middle of gestation and thereafter increases slightly until delivery. In contrast, women who will develop GH or PE exhibit stable BP during the first half of pregnancy and afterwards a continuous linear and significantly greater BP increase until delivery. An additional typically neglected factors, but of nonetheless of great clinical significance for making the diagnosis of GH and PE, is the reported sex difference in the 24-h BP pattern. The lower BP of nongravid women compared to men plus the second trimester decrease of BP in normotensive pregnancies have yet to be taken into consideration when establishing BP reference thresholds for the diagnosis of GH and PE. Prospective studies designed to take all these factors into consideration have consistently documented that ABPM during gestation, commencing preferably at the time of the first obstetric examination following positive confirmation of pregnancy, provides (1) sensitive and specific endpoints for early identification of PE and other complications in pregnancy, and (2) guidance of very low-cost and highly effective prophylactic and/or therapeutic intervention. Accordingly, ABPM is now recommended as the gold standard, thereby replacing unreliable clinic BP measurements, for the diagnosis of hypertension in pregnancy and the screening of pregnant women at high risk for other complications of gestation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Hypertensive complications in pregnancy are associated with increased risk of both adverse fetal/neonatal outcomes, including preterm birth, intrauterine growth retardation (IUGR), and perinatal death, as well as maternal outcomes, including acute renal or hepatic failure, antepartum and postpartum hemorrhage, and even death [1–3]. Hypertensive complications in pregnancy range from hypertension alone (gestational hypertension [GH]) through proteinuria and multiorgan dysfunction (preeclampsia [PE]) to seizures (eclampsia) [4]. Reported rates of GH and PE vary substantially, ranging from 4 to 15 % and 2 to 5 %, respectively [5–7]. However, these rates might well underestimate actual ones [8], since the rather large variation in reported prevalence is likely due to under-ascertainment and/or misclassification of GH and PE [8–10]. Furthermore, since the majority of cases of GH and PE are typically diagnosed at term, the increasing trend of early elective delivery contributes to additional underestimation of their prevalence [11].
Many of the physiologic changes of PE are essentially a reversal of those that accompany a healthy pregnancy, i.e., absence of normal increase in plasma volume, elevation of blood pressure (BP), increase of peripheral vascular resistance, and decrease (insufficiency) of aldosterone concentration [12]. Even though the exact cause of PE is unknown, several mechanisms have been suggested, including enhanced sensitivity to vasopressors, abnormal maternal immunologic reaction, and imbalance of vasoactive prostaglandin (thromboxane A2 and prostacyclin) concentrations, resulting in small arteries vasoconstriction, platelet activation, and uteroplacental insufficiency [12–15]. Maternal risk factors for GH and PE include nulliparity, advanced age, multiple births, diabetes, chronic hypertension, obesity, previous or family history of PE, different father and/or ≥10 years since last pregnancy, renal disease, and circulating antiphospholipid antibodies [3, 5, 6, 16–18]. Decreased risk of GH and PE has been associated with placenta previa, summer births, daily low-dose aspirin (particularly when ingested daily at bedtime and commencing early in pregnancy) and calcium supplementation, and BP-lowering and glucose-lowering medications to control, respectively, hypertension and diabetes [3, 16, 19–24].
Several clinical, biochemical, and biophysical tests have been applied to predict development of GH or PE later in pregnancy , but with inconsistent and usually rather low specificity and sensitivity [25]. Because an elevated BP after 20-week gestation is common to the definition of both GH and PE [4, 26], several studies [27–30] have assessed if these complications may be predicted on the basis of office cuff BP measured during conventional antenatal visits. Clinic BP values, however, have several shortcomings: they are representative of only a very small fraction of the 24-h BP profile, usually under circumstances that may have pressor effect, and the technique is fraught with potential errors, including instrument defects and poor examiner technique [31]. Not surprisingly, several investigators have found office BP measurements to be neither diagnostic nor sufficiently predictive of the development of hypertension in pregnancy [8, 9, 32–35], showing both disappointing sensitivity, as low as 9 % [36], and positive predictive value, as low as 8 % [29]. Nonetheless, the diagnosis of GH continues to rely on conventional clinic BP measurements that are interpreted relative to fix threshold values, i.e., 140/90 mmHg for systolic (SBP)/diastolic BP (DBP) after 20-week gestation [4, 26]. These reference thresholds for clinic BP measurements, the same one used to diagnose essential hypertension in nongravid women [37], are applied independently of gestational age at the time of BP measurement.
Ambulatory BP monitoring (ABPM ) has been suggested as a logical approach to overcoming many of the shortcomings and uncertainties associated with clinical BP measurement in pregnancy [8, 9, 33, 34, 38–40]. Indeed, multiple studies have evaluated the potential prognostic value of ABPM for the early detection of GH and PE [40–53]. However, many ABPM-based studies evidence the same kind of methodological deficiency as clinic BP-based ones: most investigators reporting on the potential prognostic value of ABPM failed to take into account gestational age at the time of measurement on their findings [41, 42, 45, 49, 50], thus disregarding the predictable changes in BP level that occur throughout gestation.
Predictable BP Trends during Gestation in Healthy and Complicated Pregnancies
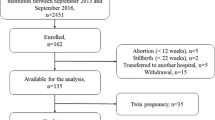
Noninvasive around-the-clock ABPM investigations have documented predictable differences in ambulatory BP between clinically healthy and hypertensive pregnant women during the course of gestation [38, 54, 55]. Hermida et al. [55] conducted a prospective ABPM study on 403 (207 nullipara) untreated Spanish pregnant women. Among them, 235 remained normotensive, 128 developed GH, and 40 developed PE. The SBP and DBP of each pregnant woman were automatically assessed every 20 min between 07:00 and 23:00 h and every 30 min during the night for 48 consecutive hours at the time of recruitment (usually within the first trimester of pregnancy), and thereafter every 4 weeks until delivery. A 48-h, instead of the most common 24-h, monitoring was chosen to improve reproducibility of results, as previously demonstrated both in nonpregnant [56] and pregnant women [57].
In normotensive pregnancies, ambulatory BP steadily decreases until the middle of gestation and then increases only slightly until delivery (Fig. 13.1, top). In contrast, women who develop GH or PE exhibit a stable SBP and DBP during the first half of pregnancy and thereafter a continuous linear and significantly greater increase until delivery (Fig. 13.1, bottom) [55]. According to these findings, the ABPM-derived 48-h SBP/DBP means during the first trimester of pregnancy already differ significantly between women who will remain normotensive throughout pregnancy and those who will later develop hypertensive complications. At the 14th week of gestation, the 48-h SBP/DBP means of women who developed GH or PE were significantly greater—115/67 mmHg—than of those who had a healthy normotensive pregnancy—103/60 mmHg. Differences in the 48-h SBP/DBP means between healthy and complicated pregnancies can be observed, therefore, quite before the actual clinical diagnosis of GH or PE is made, typically in the third trimester of pregnancy. The results of this study on women systematically sampled by 48-h ABPM throughout gestation not only confirm the predictable gestation-stage-dependent BP variation, but provide proper information to establish both around-the-clock and gestational-age-dependent reference limits for SBP and DBP [58], essential for the early identification of women at risk for developing hypertensive complications later in pregnancy [8, 9, 33, 34, 38, 59].
Variation of the 48-h SBP mean throughout gestation in normotensive pregnancies (top; 1408 ABPM profiles of 48-h duration obtained from 235 women) and women who developed either GH (bottom; 800 ABPM profiles from 128 women) or PE (bottom; 222 ABPM profiles from 40 women). Updated from [55]
Circadian BP Patterns in Normotensive and Hypertensive Pregnant Women
An important advantage of around-the-clock ABPM is thorough description and quantification of the mostly predictable 24-h BP variation that results from the interrelationship of various internal and external time-of-day influences: (1) rest/activity-associated changes in behavior (including activity routine and level, meal timings and content, mental stress, and posture); (2) day–night divergence in ambient temperature, humidity, and noise; and (3) circadian (~24 h) rhythms in neuroendocrine, endothelial, BP-modulating peptide, and hemodynamic parameters, e.g., plasma noradrenaline and adrenaline (autonomic nervous system), atrial natriuretic and calcitonin gene-related peptides, and renin, angiotensin, and aldosterone (renin-angiotensin-aldosterone system) [60–62]. Such 24-h BP variability also characterizes clinically healthy pregnant women and those who develop GH or PE [9, 36, 38, 63–66]. Many reports indicate alteration in the 24-h BP pattern during gestation can be used either to predict PE or to assess its severity [8, 9, 33, 34, 66]. However, few studies have reported on the normal 24-h BP pattern in uncomplicated pregnancies [47, 50, 67], most of them without comparison to complicated pregnancies, an issue only occasionally addressed [9, 36, 38, 49, 63–65]. By the use of ABPM, several authors have found reduced BP decline during sleep in women with PE [9, 38, 63–65], whereas others even reported a reversed circadian BP pattern towards higher sleep-time than awake-time mean BP associated with PE [66, 68, 69]. A major limitation of most of the latter studies is that they have usually been conducted during the last stages of pregnancy. Moreover, they were not specifically designed to assess if ABPM might, indeed, be used to predict GH and PE.
Normal 24-h BP values in pregnancy have been established by several ABPM trials, including one involving a primigravid population of 98 women sampled at five different gestational ages [47], and a second one involving 235 normotensive pregnant women systematically sampled every 4 weeks from early in the first trimester of pregnancy until delivery, as described in the previous section, and that also provided comparison with the 24-h BP pattern of complicated pregnancies [38, 58, 65]. Figure 13.2 presents the 24-h pattern of SBP (left) and DBP (right) assessed by 48-h ABPM per trimester of pregnancy for clinically healthy normotensive women and those who developed GH or PE. BP data were pooled over an idealized single 24-h span to simplify graphic presentations.
24-h pattern of SBP (left) and DBP (right) of normotensive pregnancies (continuous line) and women who developed GH or PE (dashed line) sampled by 48-h ABPM. Each graph shows hourly means and standard errors of data for each group of pregnant women. Dark shading along lower horizontal axis of graphs denotes the average hours of nighttime sleep across the sample. Panel A: Women evaluated during the first trimester of pregnancy (<14 weeks gestation). Panel B: Women evaluated during the second trimester of pregnancy (14–27 weeks gestation). Panel C: Women evaluated during the third trimester of pregnancy (≥27 weeks gestation). Updated from [65]
A statistically significant increased 48-h SBP/DBP mean was documented in pregnancies complicated with GH or PE compared to uncomplicated pregnancies in all three trimesters (p always <0.001). Differences in the hourly BP means between normotensive and hypertensive women were also statistically significant at all circadian times and in each trimester of gestation, even after correcting for multiple testing (Fig. 13.2). No differences (p > 0.108) were detected during the first trimester of pregnancy in the 48-h SBP/DBP means between women who later developed GH versus PE. The 48-h SBP/DBP means of normotensive pregnant women were statistically lower in the second as compared to the first trimester (p < 0.001) in keeping with the documented trends of BP variation with increasing gestational age (Fig. 13.1). In the second trimester, there was statistically significant difference in the 48-h SBP/DBP means (p = 0.002/0.038) between the two groups of women who subsequently developed GH and PE [65]. Panel C of Fig. 13.2, for women sampled by 48-h ABPM during their third trimester of pregnancy, shows larger between-groups differences than those documented for the first and second trimesters of pregnancy (panels A and B of Fig. 13.2, respectively). BP slightly increased from the second to the third trimester in normotensive pregnancies, up to values equivalent to those obtained in the first trimester for the same women. In women who developed GH or PE, BP increased greatly from the second to the third trimester, the increase in BP being greater for women who developed PE versus GH (Fig. 13.1). Accordingly, during the third trimester, the difference in 48-h SBP/DBP means between the GH and PE groups was statistically significant (p < 0.001).
The results depicted in Fig. 13.2 indicate statistically significant differences in ambulatory BP between healthy and complicated pregnancies that are detectable as early as the first trimester of pregnancy; nonetheless, at this stage of gestation, both SBP and DBP for women with a later diagnosis of GH and PE were still well within the currently accepted, but as discussed below, outdated, normal physiologic BP range [65]. Despite this available information, the diagnosis of hypertension in pregnancy based on ABPM [51] has frequently relied on the very same reference thresholds established for the diagnosis of essential hypertension, i.e., 130/80 mmHg for the 24-h SBP/DBP means [37]. These reference thresholds have several shortcomings for use in pregnancy, as documented in the following section.
24-h BP Patterns in Men, Nonpregnant Women, and Pregnant Women
Apart from the predictable changes in BP with gestational age (Fig. 13.1), epidemiologic studies report significant sex differences in BP and heart rate [59, 70–73]. Typically, men exhibit lower heart rate and higher BP than women, the differences being larger for SBP than DBP [39, 71]. These differences become apparent during adolescence and remain significant until 55–60 years of age [74]. Results from a recent large long-term prospective study on cardiovascular and cerebrovascular morbidity and mortality of subjects evaluated by periodic, at least annually, 48-h ABPM reveal the outcome-based 48 h SBP/DBP reference thresholds for the diagnosis of hypertension to be 10/5 mmHg lower for women than men [72].
The sex differences in BP regulation are illustrated in Fig. 13.3, which presents, first, the 24-h SBP pattern of 643 clinically healthy young-adult men and 504 nonpregnant normotensive women, 18–40 years of age [71]. Data of these 1147 normotensive subjects, matched by age, ethnicity, and, to the extent possible, body weight and height to the population of pregnant women that provided data for Figs. 13.1 and 13.2, were obtained using the same sampling scheme, i.e., ABPM performed every 20 min from 07:00 to 23:00 h and every 30 min during the night for 48 consecutive hours. Figure 13.3 also illustrates the 24-h BP pattern of normotensive pregnant women and those who developed GH or PE evaluated by 48-h ABPM during the second trimester of gestation. Figure 13.3 documents: (1) ambulatory SBP is significantly higher in young-adult normotensive men than similarly aged nonpregnant normotensive women (p < 0.001); (2) as previously demonstrated [65], ambulatory SBP during the second trimester of gestation is significantly diminished in women having normotensive pregnancies compared to ones later complicated with GH or PE (p < 0.001), although these differences between healthy and complicated pregnancies can already be observed during the first trimester of pregnancy (Fig. 13.2, panel A); (3) ambulatory SBP is significantly lower in normotensive pregnant women than in normotensive nonpregnant women (p < 0.001), as a consequence of the diminished BP during the second trimester of gestation in healthy pregnancies (Figs. 13.1 and 13.2); (4) ambulatory SBP is significantly higher in women who developed GH or PE evaluated during the second trimester of gestation than in normotensive women, either pregnant or nonpregnant (p < 0.001); and (5) ambulatory SBP is fully equivalent in clinically healthy normotensive men and in pregnant women who developed GH or PE when sampled during the second trimester of pregnancy (p = 0.187).
24-h SBP pattern of clinically healthy normotensive men (Group 1: 643 individuals) and normotensive nonpregnant women (Group 2: 504 individuals), normotensive pregnant women (Group 3: 546 ABPM profiles from 235 women), and women who developed GH or PE (Group 4: 412 ABPM profiles from 168 women) sampled by 48-h ABPM during the second trimester of pregnancy (14–27 weeks gestation). Each graph shows hourly means and standard errors of data for each group of subjects. Dark shading along lower horizontal axis of graphs denotes the average hours of nighttime sleep across the subject sample. Updated from [38]
Although Fig. 13.3, as an example, presents data from pregnant women sampled during their second trimester of gestation, the conclusions are similar for the same women sampled by 48-h ABPM before 14 weeks gestation, i.e., during the first trimester [36, 38, 64, 65]. These significant differences in ambulatory BP that are expressed several months before the diagnosis of GH or PE cannot be established by clinic BP measurements until very late in pregnancy, well within the third trimester. Of additional significant clinical relevance is the finding that the detected 48-h SBP/DBP means, which differ between healthy and complicated pregnancies by ~12/7 mmHg, still fall below the threshold limits currently accepted for the diagnosis of hypertension in pregnancy [4, 26]. Until recently [39], knowledge of the diminished BP of nongravid women as compared to men plus the decrease in BP during the second half of gestation in normotensive pregnant women was not taken into account when establishing reference BP thresholds for the diagnosis of hypertension in pregnancy, whether based either on unreliable clinic BP measurements [4, 26] or the more reproducible ambulatory ones [37]. The unfortunate consequence of reliance upon the currently accepted thresholds established for clinic BP and ABPM measurements is high risk of misdiagnosis, i.e., gestational normotension when, in actuality, it should be GH.
24-h BP Mean for Diagnosis of Hypertension in Pregnancy
In chronic essential hypertension , the correlation between BP level and target organ damage, cardiovascular disease risk, and long-term prognosis is greater for ABPM than clinic BP measurement [75–77]. Accordingl y, several investigators have attempted to extrapolate these advantages of ABPM to the diagnosis of hypertension in pregnancy and prediction of pregnancy outcome. As in essential hypertension, the most common approach for diagnosing hypertension in pregnancy has been reliance on the ABPM-derived 24-h BP mean. However, previous studies have reported inconsistent 24-h BP mean threshold reference values for the diagnosis of GH that only occasionally have been tested prospectively [42, 78]. Moreover, there is considerable controversy regarding the comparative prognostic value of the awake versus asleep BP means for the prediction of complications in pregnancy [43, 44, 47, 49].
A large number of studies have addressed the utility of the 24-h BP mean to predict GH and/or PE, often with significant deficiencies and limitations [38]. For example, Kyle et al. [49] investigated the usefulness of the second trimester 24-h BP mean as a screening test for predicting the development of hypertension later in pregnancy. They reported the awake SBP mean was elevated at 18 and 28 weeks gestation in women who subsequently developed “preeclampsia,” defined by them as women with an increase in clinic DBP of ≥25 mmHg during gestation or clinic DBP ≥90 mmHg, independent of SBP or proteinuria, which differs greatly from how it is currently defined [4, 26]. The first criterion—a fixed increase in clinic SBP/DBP throughout gestation—has been eliminated from the current definition of GH [26], and the second criterion, totally disregarding SBP and proteinuria for the proper definition of PE, is inaccurate and thus of very low prognostic value [8, 9, 33, 40, 51]. Despite the significant difference in BP detected between the compared groups, the best predictive BP parameter of the study by Kyle et al. [49] was mean arterial BP ≥85 mmHg at 28 weeks gestation, providing sensitivity of 65 %, specificity of 81 %, and positive predictive value of 31 % for the improperly defined “preeclampsia.” Daytime and nighttime BP means were of similar predictive value.
Penny et al. [51] used a threshold value of 135/85 mmHg for the 24-h SBP/DBP means to assess the ability of ABPM to predict development of severe hypertension (clinic SBP/DBP measurements ≥160/110 mmHg), proteinuria, birth weight < third percentile for gestational age, preterm delivery, and admission of the newborn to the neonatal intensive care unit. The authors justified their conceptual approach on the invalid claim that the 135/85 mmHg thresholds for the 24-h SBP/DBP means, greater than the ones of 130/80 mmHg currently used for non-pregnant women [37], are comparable to the 140/90 mmHg thresholds commonly used for clinic SBP/DBP. Moreover, as described above, such threshold values established independent of gestational age ignore the reported predictable BP changes that occur throughout pregnancy (Fig. 13.1). Despite all these major limitations, the authors concluded that a 24-h BP mean >135/85 mmHg in the second half of pregnancy is a significantly better predictor than conventional office BP values ≥140/90 mmHg for the development of cuff-substantiated severe hypertension.
Bellomo et al. [42] also evaluated the prognostic value of ABPM in pregnancy using reference thresholds of 125/74 mmHg, 128/78 mmHg, and 121/70 mmHg for the 24 h, awake, and asleep SBP/DBP means, respectively, in women sampled on just one occasion during their third trimester of pregnancy. These investigators reported that the 24-h BP mean is superior to clinic BP measurements obtained at the same time during the third trimester of gestation for prediction of pregnancy outcome.
Brown et al. [43] reported 70 % sensitivity to predict later detection of either GH or PE by clinic BP defined by the thresholds of ≥140/90 mmHg, when using a fixed non-varying by gestational age cutoff value of 62 mmHg for the asleep DBP mean obtained from ABPM done between 18- and 30-week gestation. They also suggested fixed threshold values of 115 mmHg for the 24-h SBP mean and 106 mmHg for the asleep SBP mean were predictive of later GH or PE, but again with relatively low sensitivities, 77 % and 54 %, respectively. In actuality, this research study describes the potential ability of the highly reproducible ABPM to predict the poorly reproducible clinic BP ≥140/90 mmHg threshold later in pregnancy.
Higgins et al. [48] applied the same questionable approach of investigating ABPM as a potential predictor of future clinic BP measurements in pregnancy. They studied 1048 women evaluated by 24-h ABPM at 18–24 weeks gestation. The best overall predictor for PE was the 24-h DBP mean, which when using a fixed cutoff threshold value of 71 mmHg provided a test with sensitivity of only 22 % and positive predictive value of only 15%.
The illustrative examples presented above highlight the limitation of relying solely on the ABPM-derived 24-h or even awake or asleep SBP/DBP means determined early in pregnancy to predict later development of GH or PE defined exclusively in terms of clinic BP and the thresholds of ≥140/90 mmHg. ABPM is unquestionably of higher prognostic value than conventional clinic BP measurements. However, due to poor results from the diagnostic test based only on the basis of the 24-h BP mean—namely the identification by ABPM of women who might or might not show elevated clinic BP later in pregnancy—the most extended, in our opinion wrong and unjustified, conclusion in the obstetric field so far is that ABPM is not a suitable tool for the early identification of GH or PE, and therefore should not be used in pregnancy [48].
The findings of studies entailing a different approach of utilizing ABPM-derived data by Hermida & Ayala [32], in contrast, clearly substantiate the ability of ABPM to predict early in pregnancy the risk of GH and PE. They performed a study on 113 pregnant women sampled for 48 h every 4 weeks from the first obstetric examination until delivery, thus providing 759 ABPM profiles in total, to assess the sensitivity and specificity of the 48-h BP mean per trimester of pregnancy in identifying hypertensive complications. This was accomplished by comparing distributions of the 48-h BP mean values of both healthy and complicated pregnancies, without assuming an a priori threshold for the diagnosis of GH based on mean BP [32]. Sensitivity ranged from 32 % for DBP in the second trimester to 84 % for SBP in the third trimester. Specificity, however, was as low as 7 % for the first trimester DBP. Results from this study revealed the threshold values for the 48-h SBP/DBP means that would eventually provide the highest combined sensitivity and specificity in the diagnosis of hypertension in pregnancy are: 111/66 mmHg in the first trimester of pregnancy, 110/65 mmHg in the second trimester, and 114/69 mmHg in the third trimester (Table 13.1). The corresponding threshold values in each of the three trimesters of pregnancy for the awake SBP/DBP means were 115/70, 115/69, and 118/72 mmHg; and 99/58, 98/56, and 104/60 mmHg for the asleep SBP/DBP means, respectively (Table 13.1 [32]). These apparently low values, reflecting the predictable changes in BP during gestation in normotensive pregnant women plus the expected diminished BP in pregnant as compared to nonpregnant women (Fig. 13.3), are fully equivalent to those proposed by other independent investigators to define normal ABPM values in pregnancy [47, 79].
In the attempt to validate prospectively these results, Hermida & Ayala calculated the sensitivity and specificity of the 48-h, awake, and asleep BP means for the early identification of hypertension in pregnancy using the reference threshold values provided above (and also in Table 13.1) when analyzing data described in Figs. 13.1 and 13.2 [78]. As an illustrative example, Fig. 13.4 represents the frequency histograms with the distributions of the 48-h (left), awake (center), and asleep SBP means (right) calculated from the 958 ABPM profiles of 48 h duration obtained from the participating pregnant women in their second trimester of pregnancy. Comparison of the histograms of the normotensive (top) and hypertensive pregnancies (bottom) does not reveal clear separation between the two populations for any of the three mean BP values investigated. However, testing prospectively the previously established second trimester thresholds (110, 115, and 98 mmHg for the 48-h, awake, and asleep SBP mean, respectively [32]) reveals relatively small overlap between healthy and complicated pregnant women. Only 40 out of the 546 (7.3 %) BP profiles representative of normotensive pregnant women in the second trimester of gestation have a 48-h SBP mean >110 mmHg, while 362 out of the 412 (87.9 %) profiles representative of those who later developed GH or PE show a 48-h SBP mean above this threshold. Results are similar for the awake SBP mean (Fig. 13.4, center), although the overlap between the distributions of values of normotensive and hypertensive women is slightly higher for the asleep SBP mean (Fig. 13.4, right). Results further indicate a slightly larger overlap of BP mean values between normotensive and hypertensive women during the first trimester, and a slightly smaller overlap of the data sampled during the third trimester. Thus, the sensitivity and specificity of the diagnosis of hypertension in pregnancy based on mean SBP values increase with gestational age. The sensitivity and specificity of the DBP means according to the threshold values listed in Table 13.1 are consistently lower than they are for the SBP means at all stages of pregnancy [78].
Frequency distribution of 48-h (left ), awake (center ), and asleep SBP mean (right ) from normotensive (top; 546 ABPM profiles from 235 women) and hypertensive pregnant women (bottom; 412 ABPM profiles from 168 women) sampled by 48-h ABPM during the second trimester of pregnancy (14–27 weeks gestation). The tested reference thresholds of 110, 115, and 98 mmHg for the 48-h, awake, and asleep SBP mean, respectively, are represented as thick vertical lines in each graph. Updated from [78]
These findings on the prospective evaluation per trimester of the prognostic value in pregnancy of the mean BP values derived from ABPM were additionally compared to those obtained from clinic BP measurements on the same women. For data obtained during the second trimester, the total overlap between normotensive and hypertensive pregnancies was 97.7 and 98.2 % for clinic SBP and DBP, respectively. Women who later developed GH or PE had during the second trimester of pregnancy clinic SBP values as low as 100 mmHg, with only 33 out of a total of 412 SBP values (8 %) actually ≥140 mmHg. These findings thus indicate very poor sensitivity at all stages of gestation, mainly for clinic DBP. Specificity, on the contrary, was very high, as just a very small proportion of women in this study, including those with PE, showed conventional clinic BP values ≥140/90 mmHg, even during most of their third trimester of pregnancy.
The results of this prospective trial [78] corroborate, first, the advantages of ABPM over clinic BP values for the early identification of hypertension in pregnancy. Relative to the 130/80 mmHg reference thresholds for 24-h SBP/DBP means proposed for the general population [37], the thresholds listed in Table 13.1 as a function of gestational age reflect the previously documented [71] expected lower BP in women as compared to men, the expected further decrease in BP in gravid as compared to nongravid women [36, 38, 64, 65], and the predictable changes in BP as a function of gestational age [38, 54, 55]. Results presented in Fig. 13.4 corroborate prospectively that the diagnosis of hypertension in pregnancy based on mean BP values derived from ABPM should be established from thresholds much lower than those currently used in clinical practice [39]. Although the sensitivity and specificity in the diagnosis of hypertension can still be improved by the use of other indexes derived from ABPM (for example, by the tolerance-hyperbaric test subsequently discussed) [8, 9, 33, 34, 38], the results of rigorously conducted studies indicate the 48-h, awake, and asleep BP means (Fig. 13.4) provide a diagnostic test markedly superior to clinic BP measurements, rendering ABPM a more useful tool for the clinical evaluation and early identification of complications in pregnancy.
Early Identification of Hypertension in Pregnancy with the Tolerance-Hyperbaric Test
The differing 24-h BP pattern between healthy and complicated pregnancies at all gestational ages, as shown in Fig. 13.2 [36, 38, 63–65], suggests the diagnosis of hypertension in pregnancy might be improved without reliance only on 24-h SBP/DBP mean values that disregard information on 24-h BP variability [32], and the use for diagnosis of a time-specified reference limit [38, 58]. Once the time-varying threshold, given for instance by the upper limit of a time-qualified tolerance interval derived per each hour of the activity and sleep spans [58], is available, the hyperbaric index (HBI), as a determinant of entire 24-h BP excess, can be calculated as the total area of any given subject’s BP above the threshold [8, 9, 33, 34, 59, 80]. The HBI as well as the duration of BP excess (percentage time of excess, defined as the percentage time during the 24 h when the BP of the test subject exceeds the upper limit of the tolerance interval) can then be used as nonparametric endpoints for assessing hypertension in pregnancy. This so-called tolerance-hyperbaric test, by which the diagnosis of hypertension is based on the HBI calculated with reference to a time-specified tolerance limit, has been shown to provide high sensitivity and specificity for the early identification of subsequent hypertension in pregnancy [33], thereby constituting a valuable approach for the prediction of pregnancy outcome [8, 9]. Because the conventional assessment of GH relies on office values ≥140/90 mmHg for SBP/DBP [4, 26], results based on the determination of BP excess have been usually expressed as a function of the maximum HBI, defined as the maximum of the three values of HBI determined for SBP, mean arterial BP, and DBP, respectively, for any given individual [9, 33, 34, 59, 80]. The prospective evaluation of the reproducibility of this ABPM-based test for early identification of complications in pregnancy was found to show a sensitivity of 93 % for women evaluated by ABPM during their first trimester of gestation [34]. Sensitivity improved with gestational age, as BP also increases steadily during the second half of gestation in women who develop hypertension in pregnancy (Fig. 13.1).
Beyond the studies summarized above, several other authors have reported consistent positive results when testing the ability of the HBI derived from ABPM to predict pregnancy outcome [81–84]. Benedetto et al. [81] performed 24-h ABPM at 8–16 and 20–25 weeks gestation in 104 women at risk of GH or PE. Best sensitivity and specificity were obtained between 20 and 25 weeks gestation with the 24-h mean and the HBI of SBP using as cut-off values 103 mmHg (sensitivity: 88 %; specificity: 75 %) and 10 mmHg × h (sensitivity: 70 %; specificity: 92 %), respectively. The authors concluded ABPM in pregnancy allows definition of objective cut-off values that can be particularly useful in routine clinical practice when the risk of developing GH or PE must be calculated for each individual woman. Shaginian [84] evaluated 34 apparently healthy pregnant women by 72-h ABPM finding elevated HBI for SBP in the first trimester of pregnancy for the 17 women who developed GH or PE during the second half of gestation compared to the 17 women who remained normotensive until delivery. On the contrary, Vollebregt et al. [85] reported limited accuracy of the HBI in predicting hypertension in pregnancy from a study of 101 women evaluated by 48-h ABPM only once in the first trimester of gestation. Their approach, which we feel is invalid for many reasons [38], utilized a (highly reproducible [34]) first trimester ABPM profile to predict elevated (highly variable and poorly reproducible) clinic BP later in pregnancy. This approach, far from novel, has been used in the past by many other obstetricians [43, 48], as briefly discussed above. When both clinic and ambulatory BP are available, ABPM, but not clinic BP, prevails for diagnosis. This is so because, by comparing clinic and ambulatory BP, one is able to distinguish groups of subjects with normotension, sustained hypertension, isolated clinic (white coat) hypertension, and masked hypertension, characterized by different cardiovascular risk [37, 39, 86]. The inappropriate approach of Vollebregt et al. [85] undoubtedly included women with masked hypertension in their reference population as well as in the comparative group they mistakenly called “normotensive women,” making invalid all conclusions drawn from their study. Most important in terms of clinical relevance, the Vollebregt et al. study found perinatal outcome to be more favorable for women with GH than for the ones with normotension, which is just the opposite of what the literature in the field leads anyone to expect.
Previous prospective studies have also documented the ability of the ABPM-derived HBI, but not clinic BP measurements, to differentiate as early as at 20-week gestation women who will develop PE from those who will just develop GH without proteinuria [8, 9]. Accordingly, GH was predicted on the basis of a maximum HBI value exceeding the relatively low specified threshold of 15 mmHg × h, while PE was predicted by the higher HBI threshold of 65 mmHg × h [8].
Clinic versus Ambulatory BP for Diagnosis of Complications in Pregnancy
Another prospective study [8, 9] compared the ABPM profiles and pregnancy outcome between three groups of pregnant women evaluated by 48-h ABPM at the time of recruitment (<16 weeks gestation), and then every 4 weeks thereafter until delivery, namely: (1) “detected” GH, defined as clinic BP ≥140/90 mmHg after 20-week gestation plus maximum HBI consistently above the threshold for diagnosing hypertension in pregnancy provided above (therefore classified as hypertensive by both independent criteria); (2) “undetected” GH (i.e., masked GH), defined as clinic BP <140/90 mmHg but HBI above the threshold for diagnosis in each and everyone of the monthly profiles of ABPM obtained after 20-week gestation (therefore considered “normotensive” according to current obstetric guidelines [4, 26], but in actuality considered to be hypertensive by the ABPM-derived HBI criterion); and (3) normotension, defined as clinic BP and maximum HBI both consistently below their respective diagnostic thresholds at all evaluations after 20-week gestation. The demographic and perinatal characteristics of the investigated women are summarized in Table 13.2.
Comparison of the 24-h BP characteristics of “detected” and “undetected” (masked) GH for women sampled during the first trimester of pregnancy revealed only a small and nonsignificant (p = 0.056) greater 24-h SBP mean by 2.6 mmHg in “detected” than “undetected” GH (Fig. 13.5, left pane l). Differences between groups in the 24-h DBP mean (not shown) only amounted to 0.2 mmHg (p = 0.682). The hourly means of SBP and DBP did not differ significantly between “detected” and “undetected” GH at any circadian time, as corroborated by t-tests adjusted for multiple testing. In the second trimester, comparisons between the groups of women with “detected” and “undetected” GH failed to reveal any significant differences in the 24-h SBP/DBP means (Fig. 13.5, central panel; p > 0.386). In the third trimester of pregnancy, differences in the 24-h SBP/DBP means between “detected” and “undetected” GH were even smaller (Fig. 13.5, right panel). Additionally, at all stages of pregnancy, ambulatory BP was highly significantly lower in normotensive pregnant women than in women with either “detected” or “undetected” GH (p < .001). Moreover, average newborn weight, gestational age at delivery, plus incidence of preterm delivery, IUGR, and delivery by cesarean section were similar between the two groups of women with “detected” and “undetected” GH (Table 13.2). There were, however, statistically significant differences in all those perinatal outcome variables between these two GH groups and normotensive pregnant women (Table 13.2). Results from this prospective study provide strong evidence to support ABPM as the proper “gold standard,” instead of unreliable clinic cuff BP measurements, for the early identification of true hypertension in pregnancy and associated maternal and perinatal complications [8, 9].
24-h SBP pattern of pregnant women sampled by 48-h ABPM at different stages of pregnancy. Women were divided for comparative purposes into three groups according to the values of clinic BP and maximum HBI at all evaluations after 20-week gestation: (1) normotensives (N = 234), with both clinic BP and maximum HBI below diagnostic thresholds; (2) “detected” GH (N = 62), with clinic BP ≥140/90 mmHg plus elevated HBI; “undetected” (masked) GH (N = 59), with clinic BP <140/90 mmHg but elevated HBI. Each graph shows hourly means and standard errors of data for each group of women. Dark shading along lower horizontal axis of graphs denotes the average hours of nighttime sleep across the sample. Updated from [9]
Discussion
Although PE has generally received more attention than just hypertension in the absence of any other symptom or complication in pregnancy, the long-term follow-up of women with complicated pregnancies has indicated that GH is associated with highest incidence of subsequent chronic hypertension [87]. Thus, although PE is a more severe obstetric complication, GH may have more important long-term implications. Accordingly, following the common standard applied in most of the cited references in this review, we focused on the identification of BP elevation in pregnancy, whether or not it could be later accompanied by proteinuria. As discussed earlier, clinical studies already substantiate the ability of the HBI to differentiate to some extent, at the end of the first half of pregnancy, women who will develop PE from those who will develop GH [8].
Common to the current definition of all hypertensive complications in pregnancy, independent of how PE might be defined, is the use of the fixed reference threshold of 140/90 mmHg for conventional clinic SBP/DBP measurements obtained at the physician’s office [4, 26, 37]. Previous results have consistently documented the poor prognostic value of clinic BP for the early identification of hypertension in pregnancy and prediction of pregnancy outcome [8, 9]. The ideal predictive or diagnostic test should be simple and easy to perform, reproducible, noninvasive, and with high sensitivity and positive predictive value. The tolerance-hyperbaric test described above is noninvasive since it relies on ABPM. Many results summarized in this review are based on ABPM assessed for 48 consecutive hours as opposed to the most common 24 h [40–53]. As a compromise with practicability, monitoring over at least 48 h has been shown to present advantages in the analysis of BP variability, diagnosis of hypertension, and evaluation of patient response to treatment [33]. Moreover, accuracy in the derivation of ABPM characteristics (including mean BP values and HBI) depends markedly on the duration of ABPM [56, 57]. Indeed, sampling requirements for the tolerance-hyperbaric test are not very demanding. While results summarized in this review were obtained with BP series sampled at 20- or 30-min intervals, the HBI can be well-estimated from data sampled at ~2-h intervals with just marginal loss in sensitivity or specificity [57]. Although 15-min sampling for ABPM evaluation in pregnancy has been unjustifiably advocated [40], a longer sampling interval increases compliance and patient acceptability [88]. Additionally, the number of reference subjects needed for estimating stable time-qualified tolerance SBP and DBP intervals is also quite small, as previously documented [58, 89]. Finally, the tolerance-hyperbaric test provides both high sensitivity and positive predictive value as early as in the first trimester of pregnancy [8, 9, 33, 34, 81–84].
Perceived limitations of ABPM stem from the fact that most ambulatory devices, although advanced, are still expensive and most have not been properly validated for specific application in pregnancy. Cost, however, should always be evaluated in relation to potential benefit. Results of the prospective ABPM evaluation studies summarized here indicate the cost–benefit relationship for ABPM is more favorable than clinic BP measurements in pregnancy, simply because ABPM allows proper identification of women at high risk of complications, while clinic BP does not [8, 9, 34]. Tolerability of ABPM has also been discussed as a possible limitation of its use in pregnancy. Although compliance is usually very high [9, 33, 34], reported patient acceptability tends to be lower [88]. Patient acceptability, a potential limitation also discussed when criticizing the utilization of ABPM in general practice [37], is in part related to the ability of the physician to provide useful and convincing information to the patient on the potential advantages of ABPM [39].
Unfortunately, despite the much higher prognostic value of ABPM than clinic BP measurements, the most extended conclusion so far, due to poor results from the diagnostic test when based on 24-h SBP/DBP means ≥130/80 mmHg irrespective of gestational stage, is that ABPM does not provide a proper approach for the early identification of GH or PE, and it should not be used in pregnancy [48]. Thus, from this perspective, it is not surprising that the current obstetric guidelines recommend reliance only upon clinic BP ≥140/90 mmHg after 20-week gestation to establish the diagnosis of GH [4, 26]. However, it must be recognized that these guidelines are obsolete because they have not been updated to acknowledge the consensus recommendations of the European Societies of Hypertension and Cardiology, which specifically state 24-h BP has been shown to be superior to conventional measurements in predicting proteinuria, risk of preterm delivery, infant weight at birth, and in general, outcome of pregnancy [37]. Studies summarized above claiming “poor results” of ABPM are based on the questionable approach to test the ability of the ABPM-derived 24-h mean to predict a diagnosis founded on unreliable clinic BP measurements obtained later in pregnancy. Most important, the significantly lower ambulatory BP of nongravid women as compared to men, the added decrease in ambulatory BP during the second half of gestation in normotensive but not in hypertensive pregnant women, and the 24-h pattern with large amplitude that characterizes BP of healthy and complicated pregnant women at all gestational ages (Fig. 13.3) were not taken into account in studies providing negative results on the use of ABPM in pregnancy. The establishment of proper reference thresholds for the 24-h BP mean derived by taking all those considerations into account has been shown prospectively to markedly increase the sensitivity and specificity of ABPM for the early identification of complications in pregnancy (Fig. 13.4 [78]). Sensitivity and specificity in the early identification of hypertension in pregnancy based on mean BP values can be even further improved by the use of other indexes also derived from ABPM [8, 9, 33, 34]. In particular, the tolerance-hyperbaric test represents a reproducible, noninvasive, and highly sensitive test for the early identification of subsequent hypertension in pregnancy, including PE.
ABPM during gestation, commencing preferably at the time of the first obstetric check-up following positive confirmation of pregnancy, thus provides sensitive endpoints for use in early risk assessment and as a guide for establishing prophylactic or therapeutic intervention [19–23]. Accordingly, ABPM-derived BP measurements have been recently recommended as substitute for the unreliable clinic ones as the “gold standard” for the diagnosis of hypertension in pregnancy and the screening of women at high risk for additional complications, including IUGR and preterm delivery [39].
References
Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009;33:130–7.
Roberts CL, Ford JB, Algert CS, et al. Population-based trends in pregnancy hypertension and pre-eclampsia: an international comparative study. BMJ Open. 2011;1, e000101. doi:10.1136/bmjopen-2011-000101.
Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376:631–44.
Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from The International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy. 2001;20:ix–xiv.
Hernández-Díaz S, Toh S, Cnattingius S. Risk of pre-eclampsia in first and subsequent pregnancies: prospective cohort study. BMJ. 2009;338:b2255.
Roberts CL, Algert CS, Morris JM, Ford JB, Henderson-Smart DJ. Hypertensive disorders in pregnancy: a population-based study. Med J Aust. 2005;182:332–5.
Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of pre-eclampsia, eclampsia, and gestational hypertension, United States, 1987–2004. Am J Hypertens. 2008;21:521–6.
Hermida RC, Ayala DE. Prognostic value of office and ambulatory blood pressure measurements in pregnancy. Hypertension. 2002;40:298–303.
Hermida RC, Ayala DE, Iglesias M. Circadian rhythm of blood pressure challengues office values as the “gold standard” in the diagnosis of gestational hypertension. Chronobiol Int. 2003;20:135–56.
Roberts CL, Bell JC, Ford JB, Hadfield RM, Algert CS, Morris JM. The accuracy of reporting of the hypertensive disorders of pregnancy in population health data. Hypertens Pregnancy. 2008;27:285–97.
Koopmans CM, Bijlenga D, Groen H, et al. Induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation (HYPITAT): a multicentre, open-label randomised controlled trial. Lancet. 2009;374:979–88.
Dekker GA, Sibai BM. Low-dose aspirin in the prevention of preeclampsia and fetal growth retardation: rationale, mechanisms, and clinical trials. Am J Obstet Gynecol. 1993;168:214–27.
Redman CWG, Sargent IL. Pre-eclampsia, the placenta and the maternal systemic inflammatory response—a review. Placenta. 2003;24:s21–7.
Sibai BM, Caritis S, Hauth J. What we have learned about preeclampsia. Semin Perinatol. 2003;27:239–46.
Walsh SW. Preeclampsia: an imbalance in placental prostacyclin and thromboxane production. Am J Obstet Gynecol. 1985;152:335–40.
Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ. 2005;330:565.
Saftlas AF, Levine RJ, Klebanoff MA, et al. Abortion, changed paternity, and risk of pre-eclampsia in nulliparous women. Am J Epidemiol. 2003;157:1108–14.
Skjaerven R, Wilcox AJ, Lie RT. The interval between pregnancies and the risk of pre-eclampsia. N Engl J Med. 2002;346:33–8.
Askie LM, Duley L, Henderson-Smart DJ, Stewart LA, Collaborative Group PARIS. Antiplatelet agents for prevention of pre-eclampsia: a meta-analysis of individual patient data. Lancet. 2007;369:1791–8.
Ayala DE, Ucieda R, Hermida RC. Chronotherapy with low-dose aspirin for prevention of complications in pregnancy. Chronobiol Int. 2013;30:260–79.
Hermida RC, Ayala DE, Iglesias M, et al. Time-dependent effects of low-dose aspirin administration on blood pressure in pregnant women. Hypertension. 1997;30:589–95.
Hermida RC, Ayala DE, Fernández JR, et al. Administration time-dependent effects of aspirin in women at differing risk for preeclampsia. Hypertension. 1999;34:1016–23.
Hermida RC, Ayala DE, Iglesias M. Administration-time dependent influence of aspirin on blood pressure in pregnant women. Hypertension. 2003;41:651–6.
Hofmeyr GJ, Atallah AN, Duley L. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev. 2006;3, CD001059.
Cnossen JS, ter Riet G, Mol BW, et al. Are tests for predicting pre-eclampsia good enough to make screening viable? A review of reviews and critical appraisal. Acta Obstet Gynecol Scand. 2009;88:758–65.
Lindheimer MD, Taler SJ, Cunningham FG. Hypertension in pregnancy. J Am Soc Hypertens. 2008;2:484–94.
Miller RS, Rudra CB, Williams MA. First-trimester mean arterial pressure and risk of preeclampsia. Am J Hypertens. 2007;20:573–8.
Nijdam ME, Janssen KJ, Moons KG, et al. Prediction model for hypertension in pregnancy in nulliparous women using information obtained at the first antenatal visit. J Hypertens. 2010;28:119–26.
Page EW, Christianson R. The impact of mean arterial pressure in the middle trimester upon the outcome of pregnancy. Am J Obstet Gynecol. 1976;125:740–6.
Villar MA, Sibai BM. Clinical significance of elevated mean arterial blood pressure in second trimester and threshold increase in systolic or diastolic blood pressure during the third trimester. Am J Obstet Gynecol. 1989;160:419–23.
Patterson HR. Sources of error in recording the blood pressure of patients with hypertension in general practice. BMJ. 1984;289:1661–4.
Hermida RC, Ayala DE. Diagnosing gestational hypertension and preeclampsia with the 24-hour mean of blood pressure. Hypertension. 1997;30:1531–7.
Hermida RC, Ayala DE, Mojón A, et al. Blood pressure excess for the early identification of gestational hypertension and preeclampsia. Hypertension. 1998;31:83–9.
Hermida RC, Ayala DE, Fernández JR, Mojón A, Iglesias M. Reproducibility of the tolerance-hyperbaric test for diagnosing hypertension in pregnancy. J Hypertens. 2004;22:565–72.
Peek M, Shennan A, Halligan A, Lambert PC, Taylor DJ, De Swiet M. Hypertension in pregnancy: which method of blood pressure measurement is most predictive of outcome? Obstet Gynecol. 1996;88:1030–3.
Ayala DE, Hermida RC, Mojón A, Fernández JR, Iglesias M. Circadian blood pressure variability in healthy and complicated pregnancies. Hypertension. 1997;30:603–10.
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Ayala DE, Hermida RC. Ambulatory blood pressure monitoring for the early identificaton of hypertension in pregnancy. Chronobiol Int. 2013;30:233–59.
Hermida RC, Smolensky MH, Ayala DE, et al. 2013 ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals. Joint recommendations from the International Society for Chronobiology (ISC), American Association of Medical Chronobiology and Chronotherapeutics (AAMCC), Spanish Society of Applied Chronobiology, Chronotherapy, and Vascular Risk (SECAC), Spanish Society of Atherosclerosis (SEA), and Romanian Society of Internal Medicine (RSIM). Chronobiol Int. 2013;30:355–410.
Shennan A, Halligan A. Ambulatory blood pressure monitoring in pregnancy. Fetal Maternal Med Rev. 1998;10:69–89.
Bellomo G, Rondoni F, Pastorelli G, Stangoni G, Narducci P, Angeli G. Twenty four-hour ambulatory blood pressure monitoring in women with pre-eclampsia. J Hum Hypertens. 1995;9:617–21.
Bellomo G, Narducci PL, Rondoni F, et al. Prognostic value of 24-hour blood pressure in pregnancy. JAMA. 1999;282:1447–52.
Brown MA, Bowyer L, McHugh L, Davis GK, Mangos GJ, Jones M. Twenty-four-hour automated blood pressure monitoring as a predictor of preeclampsia. Am J Obstet Gynecol. 2001;185:618–22.
Brown MA, Davis GK, McHugh L. The prevalence and clinical significance of nocturnal hypertension in pregnancy. J Hypertens. 2001;19:1437–44.
Churchill D, Perry IJ, Beevers DG. Ambulatory blood pressure in pregnancy and fetal growth. Lancet. 1997;349:7–10.
Cugini P, Di Palma L, Battisti P, et al. Describing and interpreting 24-hour blood pressure patterns in physiologic pregnancy. Am J Obstet Gynecol. 1992;166:54–60.
Halligan A, O’Brien E, O’Malley K, et al. Twenty-four-hour ambulatory blood pressure measurement in a primigravid population. J Hypertens. 1993;11:869–73.
Higgins JR, Walshe JJ, Halligan A, O’Brien E, Conroy R, Darling MRN. Can 24-hour ambulatory blood pressure measurement predict the development of hypertension in primigravidae? Br J Obstet Gynaecol. 1997;104:356–62.
Kyle PM, Clark SJ, Buckley D, et al. Second trimester ambulatory blood pressure in nulliparous pregnancy: a useful screening test for pre-eclampsia? Br J Obstet Gynaecol. 1993;100:914–9.
Margulies M, Voto LS, Fescina R, Lastra L, Lapidus AM, Schwarcz R. Arterial blood pressure standards during normal pregnancy and their relation with mother-fetus variables. Am J Obstet Gynecol. 1987;156:1105–9.
Penny JA, Halligan AWF, Shennan AH, et al. Automated, ambulatory, or conventional blood pressure measurement in pregnancy: which is the better predictor of severe hypertension? Am J Obstet Gynecol. 1998;178:521–6.
Tranquilli AL, Giannubilo SR, Dell’Uomo B, Corradetti A. Prediction of gestational hypertension or intrauterine fetal growth restriction by mid-trimester 24-h ambulatory blood pressure monitoring. Int J Gynaecol Obstet. 2004;85:126–31.
Waugh J, Perry IJ, Halligan AW, et al. Birth weight and 24-hour ambulatory blood pressure in nonproteinuric hypertensive pregnancy. Am J Obstet Gynecol. 2000;183:633–7.
Ayala DE, Hermida RC, Mojón A, et al. Blood pressure variability during gestation in healthy and complicated pregnancies. Hypertension. 1997;30:611–8.
Hermida RC, Ayala DE, Iglesias M. Predictable blood pressure variability in healthy and complicated pregnancies. Hypertension. 2001;38:736–41.
Hermida RC, Ayala DE, Fontao MJ, Mojón A, Fernández JR. Ambulatory blood pressure monitoring: importance of sampling rate and duration—48 versus 24 hours—on the accurate assessment of cardiovascular risk. Chronobiol Int. 2013;30:55–67.
Hermida RC, Ayala DE. Sampling requirements for ambulatory blood pressure monitoring in the diagnosis of hypertension in pregnancy. Hypertension. 2003;42:619–24.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Time-qualified reference values for ambulatory blood pressure monitoring in pregnancy. Hypertension. 2001;38:746–52.
Hermida RC, Mojón A, Fernández JR, Alonso I, Ayala DE. The tolerance-hyperbaric test: a chronobiologic approach for improved diagnosis of hypertension. Chronobiol Int. 2002;19:1183–211.
Fabbian F, Smolensky MH, Tiseo R, Pala M, Manfredini R, Portaluppi F. Dipper and non-dipper blood pressure 24-hour patterns: circadian rhythm-dependent physiologic and pathophysiologic mechanisms. Chronobiol Int. 2013;30:17–30.
Hermida RC, Ayala DE, Portaluppi F. Circadian variation of blood pressure: the basis for the chronotherapy of hypertension. Adv Drug Deliv Rev. 2007;59:904–22.
Portaluppi F, Tiseo R, Smolensky MH, Hermida RC, Ayala DE, Fabbian F. Circadian rhythms and cardiovascular health. Sleep Med Rev. 2012;16:151–66.
Benedetto C, Zonca M, Marozio L, Dolco C, Carandente F, Massobrio M. Blood pressure patterns in normal pregnancy and in pregnancy-induced hypertension, preeclampsia, and chronic hypertension. Obstet Gynecol. 1996;88:503–10.
Hermida RC, Ayala DE, Mojón A, et al. Blood pressure patterns in normal pregnancy, gestational hypertension and preeclampsia. Hypertension. 2000;36:149–58.
Hermida RC, Ayala DE, Mojón A, et al. Differences in circadian blood pressure variability during gestation between healthy and complicated pregnancies. Am J Hypertens. 2003;16:200–8.
Miyamoto S, Shimokawa H, Sumioki H, Touno A, Nakano H. Circadian rhythm of plasma atrial natriuretic peptide, aldosterone, and blood pressure during the third trimester in normal and preeclamptic pregnancy. Am J Obstet Gynecol. 1998;158:393–9.
Contard S, Chanudet X, Coisne D, et al. Ambulatory monitoring of blood pressure in normal pregnancy. Am J Hypertens. 1993;6:880–4.
Beilin LJ, Deacon J, Michael CA, et al. Circadian rhythms of blood pressure and pressor hormones in normal and hypertensive pregnancy. Clin Exp Pharmacol Physiol. 1982;9:321–6.
Redman C, Beilin LJ, Bonnar J. Reversed diurnal blood pressure rhythm in hypertensive pregnancies. Clin Sci Mol Med. 1976;51:687s–9.
Ben-Dov IZ, Mekler J, Bursztyn M. Sex differences in ambulatory blood pressure monitoring. Am J Med. 2008;121:509–14.
Hermida RC, Ayala DE, Fernández JR, Mojón A, Alonso I, Calvo C. Modeling the circadian variability of ambulatorily monitored blood pressure by multiple-component analysis. Chronobiol Int. 2002;19:461–81.
Hermida RC, Ayala DE, Mojón A, Fontao MJ, Chayán L, Fernández JR. Differences between men and women in ambulatory blood pressure thresholds for diagnosis of hypertension based on cardiovascular outcomes. Chronobiol Int. 2013;30:221–32.
Vriz O, Lu H, Visentin P, Nicolosi L, Mos L, Palatini P. Gender differences in the relationship between left ventricular size and ambulatory blood pressure in borderline hypertension. The HARVEST study. Eur Heart J. 1997;18:664–70.
Wang X, Poole JC, Treiber FA, Harshfield GA, Hanevold CD, Snieder H. Ethnic and gender differences in ambulatory blood pressure trajectories: results from a 15-year longitudinal study in youth and young adults. Circulation. 2006;114:2780–7.
Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348:2407–15.
Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–61.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk. J Am Coll Cardiol. 2011;58:1165–73.
Hermida RC, Ayala DE. Reference thresholds for 24-hour, diurnal, and nocturnal blood pressure mean values in pregnancy. Blood Press Monit. 2005;10:33–41.
O’Brien A, Asmar R, Beilin L, et al. European society of hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–48.
Hermida RC, Mojón A, Fernández JR, Ayala DE. Computer-based medical system for the computation of blood pressure excess in the diagnosis of hypertension. Biomed Instrum Technol. 1996;30:267–83.
Benedetto C, Marozio L, Giarola M, Chiarolini L, Maulà V, Massobrio M. Twenty-four hour blood pressure monitoring in early pregnancy: is it predictive of pregnancy-induced hypertension and preeclampsia? Acta Obstet Gynecol Scand. 1998;77:14–21.
Carandente F, Angeli A, Massobrio M, et al. Blood pressure and heart rate in pregnancy: comparison between health and pathologic conditions. Prog Clin Biol Res. 1990;341A:575–84.
Cornélissen G, Kopher R, Brat P, et al. Chronobiologic ambulatory cardiovascular monitoring during pregnancy in Group Health of Minnesota. In: Proceedings of the 2nd Annual IEEE Symposium on Computer-Based Medical Systems. Minneapolis, MN, June 26–27; 1989;226–237.
Shaginian MG. Blood pressure circadian rhythms during development of hypertension in healthy pregnant women. Georgian Med News. 2006;138:84–6.
Vollebregt KC, Gisolf J, Guelen I, Boer K, van Montfrans G, Wolf H. Limited accuracy of the hyperbaric index, ambulatory blood pressure and sphygmomanometry measurements in predicting gestational hypertension and preeclampsia. J Hypertens. 2010;28:127–34.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Sleep-time blood pressure and the prognostic value of isolated-office and masked hypertension. Am J Hypertens. 2012;25:297–305.
Marín R, Gorostidi M, Portal CG, Sánchez M, Sánchez E, Alvarez J. Long-term prognosis of hypertension in pregnancy. Hypertens Pregnancy. 2000;19:199–209.
Taylor RS, Freeman L, North RA. Evaluation of ambulatory and self-initiated blood pressure monitors by pregnant and postpartum women. Hypertens Pregnancy. 2001;20:25–33.
Hermida RC, Fernández JR. Computation of time-specified tolerance intervals for ambulatorily monitored blood pressure. Biomed Instrum Technol. 1996;30:257–66.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Hermida, R.C., Ayala, D.E. (2016). Ambulatory Blood Pressure Monitoring in Special Populations: During Pregnancy. In: White, W. (eds) Blood Pressure Monitoring in Cardiovascular Medicine and Therapeutics. Clinical Hypertension and Vascular Diseases. Humana Press, Cham. https://doi.org/10.1007/978-3-319-22771-9_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-22771-9_13
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-22770-2
Online ISBN: 978-3-319-22771-9
eBook Packages: MedicineMedicine (R0)