Abstract
Cardiovascular disease (CVD) is the biggest cause of death and disability worldwide and diet is well established in reducing the risk of CVD. In recent years the focus of dietary research has shifted from single nutrients and food items to overall diet quality, assessed by hypothesis driven, a priori, approaches which generate diet scores and indexes, and data-driven, a posteriori, approaches such as factor analysis and cluster analysis. This chapter has reviewed the current evidence from prospective cohort studies and randomized controlled trials (RCTs) on the associations between diet quality, measured using a priori and a posteriori approaches, and risk of CVD. Epidemiological evidence shows that high diet quality is associated with a reduced risk of CVD. Adherence to healthy dietary patterns, identified from either diet scores and indexes or factor and cluster analysis, has tended to show an inverse association with CVD risk but the magnitude of protective effects has varied across studies. Consistent evidence from prospective studies and RCTs has provided strong evidence for an inverse association between adherence to a Mediterranean diet or the Dietary Approaches to Stop Hypertension (DASH) diet and reduced CVD risk. Such dietary patterns may therefore be a relatively low cost tool for public health nutrition interventions for the prevention of CVD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cardiovascular disease
- Cluster analysis
- Dietary pattern
- Diet index
- Diet quality
- Diet score
- Factor analysis
-
In recent years the focus of dietary research has shifted from single nutrients and food items to overall diet quality and dietary patterns.
-
Two main approaches have been developed to assess diet quality: hypothesis-driven (a priori) approaches which generate diet scores and indexes and data-driven (a posteriori) approaches such as factor analysis and cluster analysis.
-
Epidemiological evidence shows that high diet quality (assessed using both diet scores/indexes and data-driven approaches) is associated with reduced cardiovascular risk.
-
Strong evidence from randomized controlled trials and prospective cohorts have found protective effects of adherence to healthy diet scores, including the Mediterranean diet and the Dietary Approaches to Stop Hypertension diet, on cardiovascular risk factors and incidence of cardiovascular disease.
-
Studies using data-driven dietary patterns have frequently identified Healthy/Prudent and Unhealthy/Western dietary patterns, with adherence to the former diet generally associated with reduced risk of cardiovascular disease.
1 Introduction
Cardiovascular disease (CVD) is the biggest cause of death and disability worldwide [1, 2]. CVD is largely preventable and much focus of prevention efforts has turned to promoting healthy lifestyle behaviors, including a healthy diet which is well established in reducing the risk of CVD [1, 3–5]. A recent American Heart Association statement identified a healthy varied diet as an essential behavior for ideal cardiovascular health [6]. Historically, studies investigating the associations between diet and CVD have focused on single foods items or specific dietary nutrients. However, this approach has several limitations ; it does not take into account the fact that foods are eaten in combination, interactions and synergies between nutrients are likely to exist, the effects of single nutrients may be too small to detect, and single nutrient analysis may be confounded by the effects of overall dietary patterns [7–9]. In recent years the focus of nutritional epidemiology has shifted towards examining overall dietary patterns to reflect the complex and multidimensional nature of diets consumed in the population, to examine the cumulative effects of the consumption of various foods/nutrients and to reflect real world dietary preferences.
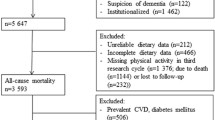
Two main approaches have been developed to assess diet quality: (1) Hypothesis-oriented or theoretically defined approaches which are a priori in nature, since they use available scientific evidence to generate predefined dietary scores or indexes based on dietary recommendations or guidelines and (2) Data-driven or exploratory approaches which are a posteriori in nature, since dietary patterns are derived from the available data based on factor analysis, such as principal component analysis , or cluster analysis (Fig. 13.1) [8, 10].
Methods to derive dietary patterns. Adapted from Schulze et al. [8]
This chapter will review the current evidence from prospective cohort studies and randomized controlled trials (RCTs) on the associations between diet quality, measured using a priori and a posteriori approaches, and the risk of CVD.
2 A Priori-Defined Dietary Patterns and CVD Prevention
A variety of diverse a priori-defined dietary scores and indexes have been developed to assess overall diet quality, based on adherence to healthy diet patterns or adherence to national or international dietary guidelines [4, 9, 11, 12]. Evidence of the relationship between some of the most commonly used scores and indexes and CVD will be presented here.
2.1 Mediterranean Diet Score
A ‘Mediterranean diet’ reflects the dietary patterns characteristic of several olive growing countries in the Mediterranean Basin in the early 1960s including Greece, southern Italy, and Spain [13]. It was first defined by Ancel Keys in the Seven Countries Study who observed lower incidence of CVD in some Mediterranean countries and hypothesized this was due to the dietary habits of these populations [14]. The traditional Mediterranean diet is characterized by an abundant consumption of olive oil as the main source of dietary lipids, a high consumption of fruit, vegetables, legumes, cereals, and nuts, a moderate to low consumption of fish, dairy, and wine (consumed with meals), and a low consumption of meat and meat products [13] (Fig. 13.2). The Mediterranean Diet Score (MDS) is one of the most commonly researched predefined dietary patterns and is based on adherence to a combination of food items characteristic of a Mediterranean-style diet. The MDS was first developed by Trichopoulou et al. in 1995 [15] and later revised to include fish intake [16]. The MDS ranges from 0 (minimal adherence) to 9 (maximal adherence). Further details of the components of the MDS and its scoring can be found in Table 13.1.
Mediterranean diet pyramid (Adapted from the Supreme Scientific Health Council, Ministry of Health and Welfare Greece [25])
Since the original MDS was defined, several modified versions have been used [17], but regardless of the slight variations in scores, the association with CVD has shown consistent beneficial results across studies. Numerous prospective cohort studies, based in European and North American adult populations, have shown consistent protective effects of adherence to a Mediterranean diet on the risk of CVD. A systematic review and meta-analysis carried out by Sofi et al. in 2010, which pooled data from 18 cohorts (including more than two million subjects and 50,000 deaths or incident cases), showed that a two-point increase in the MDS was associated with a 10 % reduction in CVD incidence and mortality [pooled relative risk (RR): 0.90, 95 % confidence interval (CI): 0.87–0.93] [18]. This was followed up by Martinez-Gonzalez et al. in 2014, which included seven more recent prospective studies, including separate estimates for both men and women, and showed highly consistent results. A two-point increase in the MDS was associated with a 13 % relative reduction in the incidence of CVD events (pooled RR: 0.87, 95 % CI: 0.85–0.90) [19]. There is also evidence that a Mediterranean-style diet is effective in reducing the risk of CVD in older adult populations. A recent review in elderly cohorts (aged 65 years or older) identified 20 studies assessing the relationship between the Mediterranean diet and cardiovascular disease, and found that such a diet had benefits on incidence of myocardial infarction (MI), cardiovascular mortality, and cardiovascular risk factors [20]. A recent systematic review assessed association between a Mediterranean diet and cardiovascular risk factors and suggested that possible causal mechanisms underlying the protective effects of a Mediterranean diet on CVD include improvements in blood lipid profile, and a reduction of blood pressure, insulin resistance, and inflammatory markers [21].
The strongest evidence of a causal association between adherence to a Mediterranean diet and the prevention of CVD comes from two RCTs. The Lyon Diet Heart Study, a randomized secondary prevention trial in over 600 French survivors of a first MI, compared an intervention of a Mediterranean diet to a control group receiving standard dietary advice [22]. Interim analysis after 27 months showed a 76 % reduction in major coronary events in the Mediterranean diet group [22] and this protective effect was maintained up to 4 years after the first MI [23]. In a large multicenter randomized primary prevention trial in Spain (PREDIMED), over 7000 individuals at high cardiovascular risk were allocated to one of three diets: a Mediterranean diet supplemented with mixed nuts, a Mediterranean diet supplemented with extra-virgin olive oil, and a control group receiving advice to reduce dietary fat [24]. The risk of major cardiovascular events was reduced by 30 % in the Mediterranean diet and olive oil group and by 28 % in the Mediterranean diet and nuts group at 4.8 years of follow-up, at which point the trial was stopped on the basis of these results. A recent review of the evidence of an association between adherence to a Mediterranean diet and the risk of CVD used meta-analysis to combine the results from these two aforementioned trials, showing a pooled CVD risk reduction of 38 % after intervention with a Mediterranean diet (RR: 0.62, 95 % CI 0.40–0.85) [19].
2.2 Dietary Approaches to Stop Hypertension
The Dietary Approaches to Stop Hypertension (DASH ) diet is well established in the prevention and control of hypertension. This dietary pattern is rich in fruits, vegetables, and low-fat dairy products, includes whole grains, legumes, fish, poultry, and nuts, and is limited in sugar-sweetened foods, red meat, and added fats. Further details of the components of DASH can be found in Table 13.2. RCTS have shown the DASH dietary pattern to lower systolic blood pressure (SBP) and diastolic blood pressure (DBP) by 5.5 and 3.0 mmHg, respectively [26]. As well as decreasing SBP and DBP, RCTs have also shown DASH improves other CVD risk factors. A meta-analysis of RCTs found that an intervention with the DASH diet resulted in significant reductions in total cholesterol (−0.20 mmol/L, 95 % CI: −0.31, −0.10) and low density lipoprotein cholesterol (−0.10 mmol/L, 95 % CI −0.20, −0.01) [27].
In addition to examining cardiovascular risk factors, many studies have also assessed the associations between adherence to the DASH dietary pattern and the incidence of CVD. A recent systematic review identified six such prospective cohort studies and pooled analysis showed that a DASH-style diet significantly reduced the risk of CVD, coronary heart disease (CHD), stroke, and heart failure by 20 %, 21 %, 19 %, and 29 %, respectively [28].
2.3 Healthy Eating Index
The Healthy Eating Index (HEI ) was originally proposed by the United States Department of Agriculture to measure adherence to Dietary Guidelines for Americans and the Food Guide Pyramid [30]. The HEI is a 10-component system made up of five food groups (grains, fruit, vegetable, milk, and meat), four nutrients [total fat, saturated fatty acids (SFA), cholesterol, and sodium], and a measure of diet variety, with a total possible 100-point score. McCullough et al. developed a modified version of this score, the Alternative Healthy Eating Index (AHEI) . The AHEI was designed to assess intake of food groups and macronutrient sources associated with reduced chronic disease risk, and compared to the HEI it distinguishes quality within food groups and acknowledges the health benefits of unsaturated oils [31]. The AHEI consists of nine components with a possible score from 2.5 to 87.5. Further details of the components of the AHEI and its scoring can be found in Table 13.3.
A study in two large American cohorts prospectively compared the two scores and found that AHEI was better at predicting CVD risk than the original HEI. Men from the Health Professionals’ Follow-up Study and women from the Nurses’ Health Study, with AHEI scores in the top compared to the bottom quintile had a 39 % and a 28 % reduction in CVD risk, respectively [32]. Similarly, in the Whitehall II study, British adults in the top compared to the bottom tertile of AHEI score showed a 42 % reduction in the risk of CVD mortality after controlling for potential confounders [33].
2.4 Healthy Diet Indicator
The Healthy Diet Indicator (HDI ) is another a priori-defined dietary score which was developed by Huijbregts et al. and is based on adherence to World Health Organization dietary guidelines for the intake of nutrients and food components [3, 34]. The HDI consists of nine components (SFA; polyunsaturated fatty acids [PUFA]; protein; complex carbohydrates; dietary fibre; fruit and vegetables; pulses, nuts, and seeds; monosaccharides and disaccharides; and cholesterol), each scoring one if the dietary guideline is met and zero otherwise, resulting in a total score range from 0 to 9. Further details of the components of the HDI and its scoring can be found in Table 13.4. The HDI has been shown to be inversely associated with cardiovascular mortality risk in older European men, with an 18 % risk reduction in the group with the highest HDI score [34]. Similarly, associations have also been found in Eastern European populations, with a 10 % reduction in CVD mortality risk and a 15 % reduction in CHD mortality risk per one standard deviation increase in HDI score [35].
However, associations of the HDI with CVD risk have been inconsistent across studies. Findings from elderly male cohorts in Sweden and Britain have shown no association between HDI and CVD mortality [36, 37] and in Dutch adults from the European Prospective Investigation into Cancer and Nutrition (EPIC-NL), no association was found between HDI and CVD incidence [38].
2.5 Other A Priori-Defined Dietary Patterns
In addition to some of the most commonly used scores and indexes mentioned above, there are other less widely used dietary scores which have been developed, and in some cases tailored for specific populations or countries or designed to evaluate prevention efforts for specific diseases [12].
It has been suggested that recall of usual dietary behaviors may be less prone to recall errors than specific types or amounts of food consumed and an alternative approach to assessing healthy dietary patterns is the dietary behavior score (DBS) . The DBS is based on the usual consumption related to recommended dietary behavior, including consumption of fruit, vegetables, whole grains, low-fat dairy, and low-fat meats. In the American Association of Retired Persons Diet and Health Study, participants in the highest quintile of the DBS, compared to the lowest had a 23–30 % lower risk of CHD mortality [39].
3 A Posteriori-Defined Dietary Patterns and CVD Prevention
Many studies have used data-driven or exploratory approaches to assess overall diet quality and the two predominant approaches are factor analysis, such as principal component analysis, and cluster analysis [4, 9, 40]. Factor analysis or principal component analysis identifies foods that are frequently consumed together and aggregates food items or groups on the basis of the degree of correlation with one another [8, 10]. Cluster analysis derives dietary patterns based on differences in dietary intakes between individuals who are separated into mutually exclusive groups [7, 10]. In factor analysis, individuals are scored based on their degree of adherence to each derived dietary pattern, whereas in cluster analysis individuals are assigned to one cluster only. Typical dietary patterns derived by such methods tend to include healthy or prudent and unhealthy or Western style patterns.
In the Nurses’ Health Study, factor analysis identified two major dietary patterns—prudent (characterized by higher intakes of fruits, vegetables, legumes, fish, poultry, and whole grains) and Western (characterized by higher intakes of red and processed meats, sweets and desserts, French fries, and refined grains) [41]. The prudent diet score was associated with a reduced risk of CHD (quintile 5 vs. quintile; 1 RR: 0.76, 95 % CI: 0.60–0.98) and the Western diet was associated with an increased risk of CHD (quintile 5 vs. quintile; 1 RR: 1.46, 95 % CI: 1.07–1.99). Similarly, the EPIC-NL study used principal component analysis to identify a prudent pattern (high intakes of fish, high-fibre products, raw vegetables, and wine) and a Western pattern (high consumption of French fries, fast food, low-fibre products, other alcoholic drinks and soft drinks with sugar) and found that the prudent pattern was associated with a reduced risk of CHD (hazard ratio (HR) for extreme quartiles: 0.87, 95 % CI: 0.75–1.00) and stroke (HR: 0.68, 95 % CI: 0.53–0.88), but found no association with the Western dietary pattern [42].
The PREDIMED RCT identified two major baseline dietary patterns using factor analysis based on 34 predefined food groups—a Western dietary pattern (rich in red and processed meats, alcohol, refined grains, and whole dairy products) and a Mediterranean-type dietary pattern (MDP ) [43]. Higher adherence to the MDP was associated with a lower CVD risk (adjusted HR for fourth vs. first quartile: 0.52, 95 % CI: 0.36–0.74) but the Western pattern was not significantly associated with CVD risk.
In the Whitehall II study, cluster analysis identified four dietary patterns at baseline: unhealthy (white bread, processed meat, fries, and full-cream milk), sweet (white bread, biscuits, cakes, processed meat, and high-fat dairy products), Mediterranean-like (fruit, vegetables, rice, pasta, and wine), and healthy (fruit, vegetables, whole-meal bread, low-fat dairy, and little alcohol) [44]. Compared with the unhealthy cluster, the healthy cluster was associated with a reduced risk of CHD mortality (HR: 0.71, 95 % CI: 0.51–0.98) after adjustment for confounders. However the other dietary patterns were not associated with CHD risk. Cluster analysis was also used in the EPIC-NL study, which identified a prudent dietary pattern and a Western pattern, similar to the patterns identified in this cohort using principal component analysis analysis mentioned above [42]. Individuals in the prudent cluster showed a reduced risk of CHD (HR: 0.91, 95 % CI: 0.82–1.00) and stroke (HR: 0.79, 95 % CI: 0.67–0.94) compared to those in the Western cluster [42].
4 Caveats of Dietary Pattern Analysis
It is important to take into account some general limitations of deriving dietary patterns to analyse the association of diet quality with health outcomes. Dietary patterns are population specific and likely to vary according to sex, ethnicity, culture, and socio-economic status, so it is difficult to make informative comparisons across studies [7]. Also, measurement error exists in the assessment of all dietary data, with problems surrounding recall bias, social desirability in reporting, and issues of under- or over-reporting of total energy intake [9, 45]. In addition, diet quality may strongly relate to other behavioral risk factors for disease that may not be fully accounted for in studies by adjustment for measured confounders.
In particular, there are some limitations of using a priori methods to assess diet quality in relation to CVD risk that should be taken into account [10]. Firstly diet quality scores or indexes may be culturally or regionally specific so may not be universally applicable. Scores may also be dependent on the selected underlying dietary guidelines, which are related to morbidity and mortality risk generally but not specifically to CVD risk. Adding together equally weighed dietary components implies that each component is equally important to CVD risk, which may not be the case. Also, scores which dichotomize components do not take into account the full range of consumed foods, so using scoring ranges may be preferable to simple cut-offs [11].
Using data-driven approaches to generate dietary patterns has the advantage of not making any prior assumptions but uses the existing data to characterize total diet, meaning that results can be meaningful, interpretable and can show some reproducibility across populations [10]. However, a posteriori methods of deriving dietary patterns, including factor analysis and cluster analysis, do have some considerations. Data are limited on the validity of these methods, and subjectivity may be introduced when grouping dietary variables, making analytic choices about statistical methods and in selecting final dietary patterns to use [7, 10, 40].
5 Conclusions
CVD is the biggest cause of death and disability worldwide and diet is well established in reducing the risk of CVD. In recent years the focus of dietary research has shifted from single nutrients and food items to overall diet quality, assessed by hypothesis-driven, a priori, approaches which generate diet scores and indexes, and data-driven, a posteriori, approaches such as factor analysis and cluster analysis. Epidemiological evidence shows that high diet quality is associated with reduced risk of CVD. Adherence to healthy dietary patterns, identified from either diet scores and indexes or factor and cluster analysis, has tended to show an inverse association with CVD risk but the magnitude of protective effects has varied across studies. Consistent evidence from prospective studies and RCTs has provided strong evidence for an inverse association between adherence to a Mediterranean diet or a DASH diet and reduced CVD risk. Such dietary patterns may therefore be a relatively low cost tool for public health nutrition interventions for the prevention of CVD.
References
World Health Organization. Global Atlas on cardiovascular disease prevention and control. Geneva: World Health Organization; 2011.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128.
World Health Organization. Diet, nutrition and the prevention of chronic disease. Joint WHO/FAO Expert Consultation. WHO Technical Report Series, No 916. Geneva: WHO; 2003.
Bhupathiraju SN, Tucker KL. Coronary heart disease prevention: nutrients, foods, and dietary patterns. Clin Chim Acta. 2011;412(17–18):1493–514.
Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659–69.
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13(1):3–9.
Schulze MB, Hoffmann K. Methodological approaches to study dietary patterns in relation to risk of coronary heart disease and stroke. Br J Nutr. 2006;95(5):860–9.
Kant AK. Dietary patterns and health outcomes. J Am Diet Assoc. 2004;104(4):615–35.
Moeller SM, Reedy J, Millen AE, Dixon LB, Newby PK, Tucker KL, et al. Dietary patterns: challenges and opportunities in dietary patterns research an Experimental Biology workshop, April 1, 2006. J Am Diet Assoc. 2007;107(7):1233–9.
Waijers PM, Feskens EJ, Ocke MC. A critical review of predefined diet quality scores. Br J Nutr. 2007;97(2):219–31.
Fransen HP, Ocke MC. Indices of diet quality. Curr Opin Clin Nutr Metab Care. 2008;11(5):559–65.
Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. 1995;61(6 Suppl):1402S–6.
Keys A, Menotti A, Karvonen MJ, Aravanis C, Blackburn H, Buzina R, et al. The diet and 15-year death rate in the seven countries study. Am J Epidemiol. 1986;124(6):903–15.
Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, et al. Diet and overall survival in elderly people. BMJ. 1995;311(7018):1457–60.
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–608.
Bach A, Serra-Majem L, Carrasco JL, Roman B, Ngo J, Bertomeu I, et al. The use of indexes evaluating the adherence to the Mediterranean diet in epidemiological studies: a review. Public Health Nutr. 2006;9(1A):132–46.
Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92(5):1189–96.
Martinez-Gonzalez MA, Bes-Rastrollo M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr Opin Lipidol. 2014;25(1):20–6.
Roman B, Carta L, Martinez-Gonzalez MA, Serra-Majem L. Effectiveness of the Mediterranean diet in the elderly. Clin Interv Aging. 2008;3(1):97–109.
Grosso G, Mistretta A, Frigiola A, Gruttadauria S, Biondi A, Basile F, et al. Mediterranean diet and cardiovascular risk factors: a systematic review. Crit Rev Food Sci Nutr. 2014;54(5):593–610.
de Lorgeril M, Salen P, Martin JL, Mamelle N, Monjaud I, Touboul P, et al. Effect of a Mediterranean type of diet on the rate of cardiovascular complications in patients with coronary artery disease. Insights into the cardioprotective effect of certain nutriments. J Am Coll Cardiol. 1996;28(5):1103–8.
de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–85.
Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–90.
Supreme Scientific Health Council. Ministry of Health and Welfare Greece. Arch Hell Med. 1999;16:516–24.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–24.
Siervo M, Lara J, Chowdhury S, Ashor A, Oggioni C, Mathers JC. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis. Br J Nutr. 2014;28:1–15.
Salehi-Abargouei A, Maghsoudi Z, Shirani F, Azadbakht L. Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases—incidence: a systematic review and meta-analysis on observational prospective studies. Nutrition. 2013;29(4):611–8.
Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114(1):82–96.
Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995;95(10):1103–8.
McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr. 2002;76(6):1261–71.
McCullough ML, Willett WC. Evaluating adherence to recommended diets in adults: the Alternate Healthy Eating Index. Public Health Nutr. 2006;9(1A):152–7.
Akbaraly TN, Ferrie JE, Berr C, Brunner EJ, Head J, Marmot MG, et al. Alternative Healthy Eating Index and mortality over 18 y of follow-up: results from the Whitehall II cohort. Am J Clin Nutr. 2011;94(1):247–53.
Huijbregts P, Feskens E, Rasanen L, Fidanza F, Nissinen A, Menotti A, et al. Dietary pattern and 20 year mortality in elderly men in Finland, Italy, and The Netherlands: longitudinal cohort study. BMJ. 1997;315(7099):13–7.
Stefler D, Pikhart H, Jankovic N, Kubinova R, Pajak A, Malyutina S, et al. Healthy diet indicator and mortality in Eastern European populations: prospective evidence from the HAPIEE cohort. Eur J Clin Nutr. 2014;68(12):1346–52.
Sjogren P, Becker W, Warensjo E, Olsson E, Byberg L, Gustafsson IB, et al. Mediterranean and carbohydrate-restricted diets and mortality among elderly men: a cohort study in Sweden. Am J Clin Nutr. 2010;92(4):967–74.
Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG. High diet quality is associated with a lower risk of cardiovascular disease and all-cause mortality in older men. J Nutr. 2014;144(5):673–80.
Struijk EA, May AM, Wezenbeek NL, Fransen HP, Soedamah-Muthu SS, Geelen A, et al. Adherence to dietary guidelines and cardiovascular disease risk in the EPIC-NL cohort. Int J Cardiol. 2014;176(2):354–9.
Kant AK, Leitzmann MF, Park Y, Hollenbeck A, Schatzkin A. Patterns of recommended dietary behaviors predict subsequent risk of mortality in a large cohort of men and women in the United States. J Nutr. 2009;139(7):1374–80.
Newby PK, Tucker KL. Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev. 2004;62(5):177–203.
Fung TT, Willett WC, Stampfer MJ, Manson JE, Hu FB. Dietary patterns and the risk of coronary heart disease in women. Arch Intern Med. 2001;161(15):1857–62.
Stricker MD, Onland-Moret NC, Boer JM, van der Schouw YT, Verschuren WM, May AM, et al. Dietary patterns derived from principal component- and k-means cluster analysis: long-term association with coronary heart disease and stroke. Nutr Metab Cardiovasc Dis. 2013;23(3):250–6.
Martinez-Gonzalez MA, Zazpe I, Razquin C, Sanchez-Tainta A, Corella D, Salas-Salvado J, et al. Empirically-derived food patterns and the risk of total mortality and cardiovascular events in the PREDIMED study. Clin Nutr. 2014.
Brunner EJ, Mosdol A, Witte DR, Martikainen P, Stafford M, Shipley MJ, et al. Dietary patterns and 15-y risks of major coronary events, diabetes, and mortality. Am J Clin Nutr. 2008;87(5):1414–21.
Willett W. Nutritional epidemiology. 2nd ed. New York: Oxford University Press; 1998.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Atkins, J.L., Wannamethee, S.G. (2015). Diet Quality and Cardiovascular Disease Prevention. In: Bendich, A., Deckelbaum, R. (eds) Preventive Nutrition. Nutrition and Health. Springer, Cham. https://doi.org/10.1007/978-3-319-22431-2_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-22431-2_13
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22430-5
Online ISBN: 978-3-319-22431-2
eBook Packages: MedicineMedicine (R0)