Abstract
Professor Schwab presents a concise and excellent overview of biliary injuries and provides the reader with several important guiding principles for the early management. He emphasizes (a) Damage Control surgery and resuscitation, (b) use of simple maneuvers to provide control of bile drainage/leakage/repair, and (c) involvement of a hepatobiliary surgeon once physiologic recovery has been achieved.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Professor Schwab presents a concise and excellent overview of biliary injuries and provides the reader with several important guiding principles for the early management. He emphasizes (a) Damage Control surgery and resuscitation, (b) use of simple maneuvers to provide control of bile drainage/leakage/repair, and (c) involvement of a hepatobiliary surgeon once physiologic recovery has been achieved.
Injuries by external force to the extrahepatic biliary tree are uncommon in occurrence and in isolation. Penetrating injury, especially gunshot wounding, in our experience, is the more common mechanism. Any trajectory that crosses the RUQ (especially medially) regardless of entrance or exit sites, should raise suspicion for biliary tract injury. Most of these, along with the much less common high energy blunt force mechanisms, present with concomitant vascular and hepatic parenchymal disruption as a part of the injury complex; therefore they present in shock. Thus, the surgeon is initially focused on rapid reversal of shock and moving to the operating room, while assessing and prioritizing other extra-abdominal threatening injury.
The initial hour of any damage control laparotomy focuses on hemorrhage control and gross examination for vascular and visceral injury. Most surgeons are knowledgeable about the maneuvers for vessel, solid viscera bleeding, and bowel contamination control. These can be accomplished expeditiously and with the necessary accelerated efficiencies. In reality, these are cases of competing priorities and the recognition of the extrahepatic biliary injury will most likely occur late in the initial damage control laparotomy when the surgeon notes bile staining, tissue destruction, or the “sense” that it is present from the array of RUQ injuries. At this point, the surgeon should be comfortable, if conditions allow, with a period of slower and methodical inspection of the gallbladder, bile ducts, duodenum, and pancreas. Proper exposure and lighting is mandatory to evaluate the extent of all injuries and a period of reflection on how to control the source(s) of bile and other visceral leakage is necessary. As suggested, this may involve a few simple sutures for small and partial bile duct lacerations or more commonly, the placement of a small, soft catheter within the injured bile duct as an external drainage conduit. In addition, Dr. Schwab emphasized some form of “educated placement of closed suction drainage,” intraperitoneal packing and temporary open abdominal wall management with negative pressure dressing systems. I would add that this is preferred to a hurried and less than optimal attempt at a biliary repair. The damage control pathway provides the advantage of a second look when physiology and coagulation have returned to normal. In stable patients with complete transection, he recommends the time tested Roux-en-Y biliary-jejunostomy procedures for definitive repair and avoidance of more esoteric procedures. Again, I agree. I would further advise any surgeon who is not comfortable with small ductal-enteric anastomosis or in a patient with other critical injuries to provide external biliary drainage and safer solution, deferring biliary reconstruction to later.
A few additional comments :
-
1.
Hepatic disruption with deep parenchymal bleeding not amendable to direct control may benefit from perihepatic packing and immediate angio-embolization. In the RUQ packing cases, one may not be able to examine the extrahepatic ductal system as the packing obscures the infra-hepatic area. The objective here is to expedite the angiographic interrogation. As well, the angiography should delineate arterial anatomy with variants and address the status of the right hepatic artery to further inform the team as to repair options if a proximal ductal injury is subsequently found. In these cases, an early return to the OR with inspection of the extrahepatic biliary system, ductal drainage, and insertion of regional drains with repacking should be considered.
-
(a)
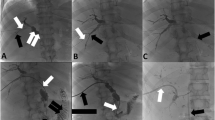
In some centers with capable hands, ERCP and investigation of the biliary anatomy can be accomplished in the interim period and temporary biliary stenting considered.
-
(a)
-
2.
In those cases with a transected hepatic or common bile duct, the placement of a soft, small drain into the proximal duct and brought out externally with minimum dissection to the bile duct is my preferred method of control along with regional dependent suction drains.
-
3.
In all cases of hepatic and biliary injury regardless of type, at the time of the take back surgery (damage control part III), I am a strong proponent and user of dependent closed suction drains away from the site of visceral injury. I have found that in most of the cases, there are several sites needing drainage (liver, pancreas, retroperitoneal, kidney, and biliary) and provision of multiple channels of egress affords better drainage than a single large stiff drain.
-
4.
Despite my own experience, I strongly support the principle of involving a surgical specialist as a consultant for uncommon and rare injuries whether biliary or otherwise. Almost all low grade injuries to the biliary system, liver, and pancreas can be managed with the established surgical principles and techniques. However, the more complex and extensive injuries to the RUQ, especially disruption of the biliary tree, are facilitated with the input of a hepatobiliary surgeon with an understanding of trauma management.
-
(a)
If necessary, transfer to a regional trauma center with such capability is in the best interest of the patient.
-
(a)
-
5.
Biliary reconstruction can and should be delayed if necessary because of other life- and limb-threatening injury and the physiologic consequences. Once adequate external biliary drainage is assured, there is no rush to enter into reconstruction until the patient is fully recovered. Thus, when appropriate, I counsel the patient that definitive surgery may take place months from discharge.
-
(a)
In these cases, as soon as visual inspection at the initial or subsequent damage control laparotomy is completed, a well-crafted anatomic picture and a few descriptive notes about the injuries are helpful for long-term records and conveying the pathology to subsequent consultants.
-
(a)
-
6.
Last, my approach to any surgeon referring one of these cases to our center has been to compliment them on saving a life, managing a very complex situation and setting the stage so we could help further in the recovery of the patient.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Schwab, B. (2015). Commentary: Traumatic Biliary Strictures—Comprehensive Management of Benign Biliary Stenosis and Injury. In: Dixon, E., Vollmer Jr., C., May, G. (eds) Management of Benign Biliary Stenosis and Injury. Springer, Cham. https://doi.org/10.1007/978-3-319-22273-8_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-22273-8_13
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22272-1
Online ISBN: 978-3-319-22273-8
eBook Packages: MedicineMedicine (R0)