Abstract
Abdominal and retroperitoneal masses in children and adolescents present the clinician with diagnostic and therapeutic challenges. Ultrasound is a valuable diagnostic and therapeutic tool that should become part of the surgeon’s repertoire. Ultrasound can often be used as the first diagnostic test for many intra-abdominal and retroperitoneal masses in children and neonates. Importantly, ultrasound can be used to determine the size, location, vascularity, and cystic versus solid nature of the mass. Using the sonographic characteristics of a mass, coupled with the age, sex, and history of the patient, often leads to a precise narrowing of the differential diagnosis. Here, we describe the sonographic findings of some of the most commonly seen cystic and solid intra-abdominal and retroperitoneal masses of infancy and childhood. Following diagnosis, ultrasound is often an important adjunct for bedside procedures as well as in the operating room. The chapter concludes with descriptions on how ultrasound is useful when performing biopsies, guided drainage procedures, and as an intraoperative guide for tumor resection.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Abdominal and retroperitoneal masses in children and adolescents present the clinician with diagnostic and therapeutic challenges. Because of the number of different structures in the abdomen, the differential diagnosis is quite broad. Further, the management of these lesions may involve biopsy, drainage, or resection of the mass. For all of these reasons, ultrasound may serve as a valuable diagnostic and therapeutic tool for the surgeon.
Diagnosis
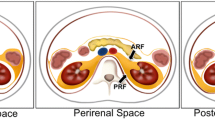
The most common entities in early childhood arise from the retroperitoneum. As children age, the lesions trend towards intra-abdominal. Ultrasound is often used as the initial study for pediatric abdominal masses and will, in most instances, at least narrow the differential diagnosis. Ultrasound is advantageous for this purpose as it is widely available, noninvasive, and provides information without the use of ionizing radiation. Important aspects of the ultrasound examination include identifying the location of the lesion—whether it is located in the abdomen, retroperitoneum, or the pelvis . This, along with the patient’s age, will guide the focus to the most likely organ of origin. Echogenicity and vascularity of the mass can further differentiate between solid and cystic masses. Also, continuity with adjacent abdominal organs or mass effect on adjacent vasculature may aid in determining the origin of the abdominal mass. Further information can be gained by examining for vascular invasion, adjacent solid organ involvement, lymphadenopathy, or vessel thrombosis.
After examining the sonographic characteristics of the mass and adding that information to the sex, age, and location of the mass, a narrow list of differential diagnoses can be made. We will now examine the imaging characteristics of cystic and solid abdominal and retroperitoneal masses , subcategorized by organ or origin and age at diagnosis to aid in the creation of a diagnostic algorithm.
Cystic Masses
Retroperitoneal
Kidney
Up to two third of abdominal masses in the neonate are renal in origin, with hydronephrosis and simple cysts accounting for most of the benign masses [4]. Common causes of hydronephrosis in the neonate are ureteropelvic obstruction, vesicoureteral reflux, posterior urethral valves, or ureterovesicular junction obstruction. A detailed discussion of these is beyond the scope of this chapter, but should be accounted for when evaluating cystic renal masses. Cystic masses in the neonate can also be caused by multicystic dysplastic kidney (MCDK), autosomal recessive polycystic kidney disease (ARPKD), and congenital mesoblastic nephroma (CMN), which we will discuss further.
Multicystic Dysplastic Kidney
Most renal cysts detected in childhood are secondary to congenital cystic diseases of the kidney. MCDK is the most likely cystic disease to present as a palpable abdominal mass in childhood [20]. Sonographic examination will show multiple, noncommunicating anechoic structures of varying sizes. In general, no ureter or collecting system will be seen in the involved kidney. In fact, no discernible normal renal parenchyma is typically visualized. Further evaluation with renal scintigraphy would show a nonfunctioning kidney. Continued follow-up ultrasound will show eventual involution of the involved kidney.
Autosomal Recessive Polycystic Kidney Disease
ARPKD usually presents with bilateral enlarged kidneys, detected on prenatal ultrasound. Renal enlargement is secondary to hyperplasia of the remaining collecting tubules. Sonographic appearance is variable, but typically demonstrates bilaterally enlarged, echogenic kidneys with multiple anechoic spaces and poor corticomedullary differentiation caused by dilated collecting ducts [21]. This pathology, i.e., numerous tiny cysts that are smaller than the sonographic resolution, results in multiple acoustic interfaces of the ultrasound beam, and hence, hyperechogenicity.
Abdominal
Liver
Mesenchymal Hamartoma
Mesenchymal hamartomas are benign hepatic tumors that typically present as a palpable abdominal mass between birth and 10 years of age, most often occurring between 15 and 20 months [7]. These tumors arise from the mesenchyme of the periportal tracts, and thus have cystic and stromal architecture. Sonography demonstrates an anechoic, cystic structure with interspersed solid, echogenic septations representing the stromal component.
Biliary/Gallbladder
Choledocal Cyst
Choledocal cyst (CC) refers to dilation of the common bile duct (CBD), the intrahepatic bile ducts, or both. It is believed to be secondary to an abnormal junction of the pancreatic duct with the CBD, resulting in reflux of pancreatic enzymes into the CBD followed by chemical cholangitis and dilation of the ducts [5]. Congenital CCs are classified based on the location and type of dilation. Most patients with CC present in the first decade of life, and the “classic” triad of episodic abdominal pain, jaundice, and right upper quadrant mass is present in only one fourth of patients. Ultrasound evaluation will show dilation of either the extrahepatic ducts, intrahepatic ducts, or both, depending on type of CC [17]. The diagnosis is made by the presence of a cystic structure near the porta hepatis. Visualization of multiple planes on ultrasound is necessary to confirm that the CC is in continuity with the CBD, a requirement for the diagnosis [10]. Further evaluation with magnetic resonance cholangiopancreatography (MRCP) is usually performed prior to surgical therapy.
Bowel
Duplication Cyst
Enteric duplication cysts are rare congenital cysts that may occur anywhere along the gastrointestinal (GI) tract, but are most common in the small intestine . They arise from the mesenteric side of the intestine and range from a few centimeters in length up to the size of the entire bowel [2]. The most common presenting signs and symptoms include a palpable abdominal mass, intestinal obstruction, or hemorrhage. Additionally, they may serve as a lead point for intussusception . Ultrasound examination will show a hypoechoic to anechoic cystic structure. The wall of the cyst may show an echogenic inner mucosal layer and a hypoechoic outer mucosal layer. Layering of debris within the cyst can often be seen. [23]
Lymphangioma
Abdominal lymphangiomas are benign mesenteric (Fig. 11.1) or omental cysts that occur secondary to congenital malformations of the abdominal and/or retroperitoneal lymphatic tissue (Fig. 11.2). They are most commonly found in the mesentery, followed in frequency by the omentum, mesocolon, and retroperitoneum [11]. Ultrasound will demonstrate a thin-walled, hypo- to anechoic structure with posterior acoustic enhancement. They may also have some internal echoes from debris, hemorrhage, or infection [13]. Usually, a computed tomography (CT) or magnetic resonance imaging (MRI) is necessary to determine involvement of adjacent structures prior to surgical resection [19].
Transabdominal ultrasound of cystic abdominal mass demonstrating an anechoic, irregularly shaped cystic lesion at midline located anterior to the SMA and SMV and inferior to the pancreas. Lesion measured 8 × 3 cm and was compressible (arrows). Surgery demonstrated this to be a mesenteric cyst. SMA superior mesenteric artery, SMV superior mesenteric vein
Pseudocyst
A meconium pseudocyst forms secondary to an intestinal perforation during fetal life. The inflammatory reaction from this chemical peritonitis causes the perforation to seal, and the meconium that was released into the peritoneal cavity is walled off into a pseudocyst. Ultrasound examination will demonstrate a cystic mass with heterogeneous echogenicity [3]. There may also be calcifications present, causing shadowing of the cyst, which can sometimes be seen on plain radiographs.
Urachal Cyst
Urachal cysts are most frequently seen in infants and young children. They arise when the urachus obliterates at the umbilicus and the bladder, but not in between. Most urachal cysts remain asymptomatic, but some may present as a palpable abdominal mass, an infection of the cyst, or as symptoms from compression of adjacent structures. Ultrasound demonstrates a hypoechoic, thick-walled cystic structure, often just superior to the bladder wall. [18]
Pelvis
Uterus/Ovaries
Ovarian Cysts
Ovarian cysts are common in the neonatal period, likely secondary to in utero hormone exposure [22]. They may be diagnosed on prenatal ultrasound, or present symptomatically with pain, abdominal distension, or fever—usually as a result of torsion or hemorrhage. Sonography of ovarian cysts (Fig. 11.3) usually demonstrates a simple cyst with no internal echoes, and a thin wall. If there has been torsion or hemorrhage, the inner part of the cyst will contain echogenic debris. Doppler ultrasound may differentiate a hemorrhagic cyst from other ovarian neoplasms, as the latter would demonstrate internal flow. Ovarian torsion may be demonstrated by the whirlpool sign , which represents the twisted pedicle of the ovary [14]. Doppler flow to the ovarian parenchyma may be absent (Fig. 11.4) but this absence should not be used to rule out torsion since some studies have demonstrated Doppler flow in up to 50 % of torsed ovaries. Simple cysts that are less than 4 cm and have no solid component may be monitored with serial ultrasound examinations [16]. Removal of cysts is generally reserved for large, symptomatic, or torsed cysts.
Transabdominal ultrasound of the pelvis demonstrating an enlarged left ovary with small peripherally displaced follicles and heterogenous stromal echogenicity. Ovary measure 3 × 2 × 4 cm. Color and spectral Doppler demonstrated no arterial or venous flow. Laparoscopic detorsion was performed immediately thereafter
Solid Masses
Retroperitoneal
Kidney
Wilms’ Tumor
Wilms’ tumor is the most common renal malignancy in childhood. The majority of patients are between 1 and 5 years of age, and present with an asymptomatic abdominal mass. The diagnosis of Wilms’ tumor is associated with various conditions, including Beckwith–Weidemann syndrome, sporadic aniridia, Drash syndrome, and hemihypertrophy [8]. In fact, it is recommended that patients with either Beckwith–Weidemann or hemihypertrophy should be screened with an abdominal ultrasound every few months due to their increased risk of Wilms’ tumor. Ultrasound examination of Wilms’ tumor will reveal an echogenic, solid mass within the kidney that may contain some cystic areas (Fig. 11.5). Increased tumor vascularity will be noted with Doppler sonography. Careful attention should be paid to the extent of tumor involvement in regard to the perinephric space, inferior vena cava (IVC) (Fig. 11.6), and rarely, the right atrium. Peritoneal lymphadenopathy may also be seen. Further staging via a CT scan is recommended following the diagnosis of Wilms’ tumor in order to determine tumor rupture, contralateral kidney involvement, and/or lung involvement.
Congenital Mesoblastic Nephroma
CMN is the most common renal neoplasm of infancy, with 85 % of CMNs diagnosed prior to 6 months of age [15]. Presentation is often with a palpable abdominal mass and, occasionally, with a paraneoplastic syndrome such as hypertension or hypercalcemia. Sonography demonstrates a large, solid renal mass with heterogeneous echogenicity. Color Doppler will demonstrate internal flow. Often, there is a central area of necrosis that is hypoechoic in nature. Though this tumor may extend beyond the renal capsule, involvement of the renal vein is uncommon. CMN may be similar in appearance to Wilms’ tumor, but is differentiated based on age of presentation given that Wilms’ tumor is rarely seen in neonates.
Adrenal Gland
Neuroblastoma
Neuroblastomas are tumors derived from neural crest cells, and have an incidence of 1:10,000 live births in the USA. Advances in prenatal ultrasound have increased the prenatal detection of neuroblastoma. Furthermore, screening ultrasound in early neonates may also reveal adrenal masses, such that 30 % of neuroblastomas may be diagnosed in the neonatal period [9]. It was unknown if some of the early detection of these lesions was merely a result of increased sensitivity of the screening ultrasound, and therefore not clinically significant. Indeed, ultrasound screening performed in Japan and Quebec has demonstrated that many of these small lesions will regress spontaneously [12]. Such screening has been discontinued as the lesions detected early were low-staged tumors and the program did not alter the overall survival in the entire cohort. Ultrasound findings of neuroblastoma tend to vary with the stage of the tumor. In lower-stage tumors, ultrasound reveals a homogeneous or slightly heterogeneous solid mass that replaces the adrenal gland . At more advanced stages, this mass tends to have a much more heterogeneous echotexture, increased vascularity, and multiple intralesional calcifications [1]. All patients with neuroblastoma should receive a staging CT and a metaiodobenzylguanidine (MIBG) scan to determine the extent of involvement. Treatment is based on tumor stage, and certain neuroblastomas (4S) may be followed with serial ultrasound or CT to determine regression and need for surgery.
Abdominal
Liver
Infantile Hepatic Hemangioma
Hemangioma is the most common benign liver mass in infants and children, with a peak presentation between 3 and 6 months of age [5]. Presenting signs and symptoms range from a palpable abdominal mass to congestive heart failure and thrombocytopenia as a result of Kasabach–Merritt syndrome. Sonography will demonstrate a complex, solid mass with heterogeneous echotexture (Fig. 11.7) and robust Doppler flow. Infantile hemangiomas typically increase in size until 9–10 months of age, and then slowly involute [6]. Medical therapies for those that do not involute spontaneously include the use of propranolol and corticosteroids. Embolization or surgical removal is reserved for those that do not involute with medical therapy, or for patients with severe complications.
Transabdominal ultrasound of infant with large right hepatic mass with cystic spaces and increased blood flow. Patient also had congestive heart failure. Image and presentation is typical of a large, symptomatic hepatic hemangioma. The child was started on oral propranolol and has had significant improvement in symptoms and resolution of the liver mass
Hepatoblastoma
Malignant tumors comprise the majority of hepatic masses in children, with the most common tumor being hepatoblastoma [5]. Hepatoblastoma typically presents in children between the ages of one and three as a palpable abdominal mass. Initial ultrasound evaluation typically shows a well-defined, heterogeneous tumor often with cystic areas caused by necrosis and calcifications. Use of a high-frequency (> 7 MHz) linear transducer will aid in the evaluation of portal and hepatic venous involvement. The tumor may invade the venous system, or cause the formation of an echogenic tumor thrombus within the lumen of the vessels. The intraluminal material may be examined with Doppler sonography, and if there is arterial flow within the intraluminal material, venous invasion by the tumor is likely.
Hepatocellular Carcinoma
Hepatocellular Carcinoma (HCC) is the second most common type of childhood liver tumor, and is more often found in older children (median 10–12 years of age) compared to hepatoblastoma [5]. Ultrasound examination of HCC will demonstrate a hyperechoic, solid mass with a thin, hypoechoic capsule that resembles a halo around the mass. As with hepatoblastoma, evaluation of invasion into portal structures is paramount when evaluating HCC. Unfortunately, only 18–36 % of HCCs in children are amenable to complete surgical resection. Often, chemotherapy, embolization, and/or radiofrequency ablation are used to shrink the tumor in hopes of subsequent resection, or as palliative therapy.
Bowel
Lymphoma
Non-Hodgkin’s Lymphoma (NHL) often presents in extranodal sites in children. The bowel is the most common extranodal site involved in NHL, up to one third of the time [4]. The presentation may be of a palpable abdominal mass , or the lymphoma may serve as a lead point for intussusception. Because of this, any intussusception in a child older than 5 years must be evaluated for intestinal lymphoma. Sonography will demonstrate a lobular, solid mass within and extending from the bowel wall. There may be circumferential involvement, and often there is internal vascularity on Doppler ultrasound. If intestinal NHL is suspected via ultrasound, a CT must be performed for initial staging.
Rhabdomyosarcoma
Rhabdomyosarcoma is the fourth most common solid tumor of childhood, and the genitourinary (GU) tract is the second most common site for rhabdomyosarcomas, behind the head and neck [9]. Median age at presentation, which is usually that of a palpable abdominal mass, is approximately 7 years. Ultrasound examination can help to identify the tumor as well as to evaluate the other pelvic and abdominal organs to determine the origin of the tumor. The sonographic appearance of rhabdomyosarcomas is variable, but most often is a solid mass with heterogeneous echogenicity. There are frequently hypoechoic areas within the tumor, signifying previous hemorrhage and necrosis.
Pelvic
Ovary
Germ Cell Tumors
Ovarian germ cell tumors account for up to two third of all pediatric ovarian tumors (Figs. 11.8 and 11.9). Similar to simple cysts, they may present as a palpable abdominal mass, or with signs of ovarian torsion [16]. Ultrasound findings will vary based on the type of germ cell tumor. Teratomas are formed from all three embryonic germ layers, and as such may have complex internal components, i.e., hair, mucus, or calcium deposits. Most commonly, there will be a cystic structure with echogenic foci and variable internal acoustic shadowing. Often, the dermoid mesh sign can be seen, which shows areas of linear hyperechogenicity. Doppler flow is used to determine the location of the involved ovary. Surgical removal is recommended for ovarian germ cell tumors based on the increased risk for ovarian torsion.
Transabdominal ultrasound demonstrating large soft tissue peritoneal implants in close contiguity to the right ovary. There is a large amount of ascites noted with multiple other peritoneal implants. Resection of these masses followed with histological assessment revealed papillary serous cystadenoma
Transabdominal ultrasound demonstrating a large, solid, heterogenous, hypervascular midline pelvic mass posterior to the uterus measuring 10.1 × 11.4 × 7.0 cm. There are multiple echogenic foci within the mass, and the tumor caused anterior displacement of the uterus and posterior wall of the bladder. Mass was resected and histologically determined to be a dysgerminoma of the ovary
Therapeutic
Masses that are either cystic or solid may require ultrasound to help perform drainage, sclerotherapy, or biopsy. Care must be taken to consider the whole picture and involve all interested care providers. Further, ultrasound may be used intraoperatively to help identify vascular structures to aid dissection and resection.
Percutaneous Drainage
Selected lesions, i.e., those that are either difficult to resect or infected and need drainage, will benefit from percutaneous ultrasound-guided drainage. The most common example of this would be perforated appendicitis with associated abscess, where drainage will allow at least partial treatment of the infectious process, and either obviate or alter an urgent need for an elective operation. Also, percutaneous drainage may be considered therapy for lymphatic malformation when used in conjunction with a sclerosant agent (Figs. 11.10 and 11.11).
Biopsy
In situations where it is deemed unwarranted for initial resection of a mass (due to large size, adjacent or involving other structures, or metastasis), a biopsy is often undertaken to obtain tissue for diagnostic purposes. In these scenarios, ultrasound guidance is often helpful whether it be by transabdominal, open, or laparoscopic means. Biopsy may be performed with a Tru-cut (core) biopsy needle, whereby the ultrasound is used to identify and then follow the passage of the needle (Fig. 11.12). Doppler may be useful in order to identify and avoid vascular structures to minimize bleeding from the biopsy procedure. Prior to biopsy, the clinical team must always consider a working diagnosis, as a biopsy is not recommended in all clinical situations and may result in an upstaging of the tumor (e.g., Wilms’ tumor).
Intraoperative Guide
Surgical resection requires the operator to be able to identify what should and should not be resected. While preoperative imaging is extremely helpful in most instances, the operator sometimes requires real-time imaging to guide the surgical resection. The added benefit of using ultrasound as a real-time imaging modality is clear: tools are commonplace, radiation is avoided, Doppler ultrasound can identify vessels, and the study can be easily repeated if needed. Examples of clinical scenarios in which ultrasound may be beneficial include:
-
Identification of vascular anatomy in liver resections—in situations in which the tumor is adjacent to hepatic or portal veins (Figs. 11.13 and 11.14), the use of ultrasound has been key to determining the extent of resection, often leading to the conversion of what might otherwise be an extensive resection into a smaller one. Alternatively, ultrasound may identify situations where a resection is not possible, and therefore hasten the conclusion of surgery.
Fig. 11.13 -
Identification of vascular and collecting system anatomy in partial renal resections—there are well-established clinical scenarios in which a partial nephrectomy is warranted (e.g., bilateral renal tumors to preserve nephrons; syndromic patients where future resections are likely; horseshoe kidney; renal cell carcinoma). In these situations, intraoperative ultrasound may provide valuable real-time assessment of whether a partial nephrectomy is feasible (Fig. 11.15).
Summary
Abdominal and retroperitoneal masses in children and adolescents present the clinician with diagnostic and therapeutic challenges. Ultrasound is a valuable diagnostic and therapeutic tool that should become part of the surgeon’s repertoire. Ultrasound can often be used as the first diagnostic test for many intra-abdominal and retroperitoneal masses in children and neonates. Importantly, ultrasound can be used to determine the size, location, vascularity, and cystic versus solid nature of the mass. Using the sonographic characteristics of a mass, coupled with the age, sex, and history of the patient, often leads to a precise narrowing of the differential diagnosis. In this chapter, we reviewed the sonographic findings of some of the most commonly seen cystic and solid intra-abdominal and retroperitoneal masses of infancy and childhood. Following diagnosis, ultrasound is often an important adjunct for bedside procedures as well as in the operating room. The chapter also discussed descriptions on how ultrasound is useful when performing biopsies, guided drainage procedures, and as an intraoperative guide for tumor resection.
References
Berdon WE, Ruzal-Shapiro C, Abramson SJ, Garvin J. The diagnosis of abdominal neuroblastoma: relative roles of ultrasonography, CT, and MRI. Urol Radiol. 1992;14(4):252–62.
Bliss DP, Coffin CM, Bower RJ, Stockmann PT, Ternberg JL. Mesenteric cysts in children. Surgery. 1994;115(5):571–7.
Carroll BA, Moskowitz PS. Sonographic diagnosis of neonatal meconium cyst. AJR Am J Roentgenol. 1981;137(6):1262–4. doi:10.2214/ajr.137.6.1262.
Crane GL, Hernanz-Schulman M. Current imaging assessment of congenital abdominal masses in pediatric patients. Semin Roentgenol. 2012;47(1):32–44. doi:10.1053/j.ro.2011.07.004.
Dezsöfi A, McLin V, Hadzic N. Hepatic neoplasms in children: a focus on differential diagnosis. Clin Res Hepatol Gastroenterol. 2014;38(4):399–402. doi:10.1016/j.clinre.2014.05.001.
Friedman AP, Slovis TL, Haller JO, Lebensart DP. The role of sonography in evaluating right upper quadrant disease in children. Clin Pediatr (Phila). 1980;19(9):591–6.
Haddad MC, Birjawi GA, Hemadeh MS, Melhem RE, Al-Kutoubi AM. The gamut of abdominal and pelvic cystic masses in children. Eur Radiol. 2001;11(1):148–66. doi:10.1007/s003300000487.
Kim S, Chung DH. Pediatric solid malignancies: neuroblastoma and Wilms’ tumor. Surg Clin North Am. 2006;86(2):469–87, xi. doi:10.1016/j.suc.2005.12.008.
Ladd AP, Grosfeld JL. Gastrointestinal tumors in children and adolescents. Semin Pediatr Surg. 2006;15(1):37–47. doi:10.1053/j.sempedsurg.2005.11.007.
Lee HC, Yeung CY, Chang PY, Sheu JC, Wang NL. Dilatation of the biliary tree in children: sonographic diagnosis and its clinical significance. J Ultrasound Med. 2000;19(3):177–82; quiz 183–4.
Luo CC, Huang CS, Chao HC, Chu SM, Hsueh C. Intra-abdominal cystic lymphangiomas in infancy and childhood. Chang Gung Med J. 2004;27(7):509–14.
Nuchtern JG. Perinatal neuroblastoma. Semin Pediatr Surg. 2006;15(1):10–6. doi:10.1053/j.sempedsurg.2005.11.003.
Okur H, Küçükaydin M, Ozokutan BH, Durak AC, Kazez A, Köse O. Mesenteric, omental, and retroperitoneal cysts in children. Eur J Surg. 1997;163(9):673–7.
Onur MR, Bakal U, Kocakoc E, Tartar T, Kazez A. Cystic abdominal masses in children: a pictorial essay. Clin Imaging. 2013;37(1):18–27. doi:10.1016/j.clinimag.2012.03.010.
Riccabona M. Imaging of renal tumours in infancy and childhood. Eur Radiol. 2003;13(Suppl 4):L116–29. doi:10.1007/s00330-003-2001-x.
Milla SS, Lee EY, Buonomo C, Bramson RT. Ultrasound evaluation of pediatric abdominal masses. Ultrasound Clin. 2007;2(3):541–59.
Sato M, Ishida H, Konno K, Naganuma H, Hamashima Y, Komatsuda T, Watanabe S. Liver tumors in children and young patients: sonographic and color Doppler findings. Abdom Imaging. 2000;25(6):596–601.
Ueno T, Hashimoto H, Yokoyama H, Ito M, Kouda K, Kanamaru H. Urachal anomalies: ultrasonography and management. J Pediatr Surg. 2003;38(8):1203–7.
Vargas-Serrano B, Alegre-Bernal N, Cortina-Moreno B, Rodriguez-Romero R, Sanchez-Ortega F. Abdominal cystic lymphangiomas: US and CT findings. Eur J Radiol. 1995;19(3):183–7.
White KS. Imaging of abdominal masses in children. Semin Pediatr Surg. 1992;1(4):269–76.
Wicks JD, Silver TM, Bree RL. Giant cystic abdominal masses in children and adolescents: ultrasonic differential diagnosis. AJR Am J Roentgenol. 1978;130(5):853–7. doi:10.2214/ajr.130.5.853.
Wootton-Gorges SL, Thomas KB, Harned RK, Wu SR, Stein-Wexler R, Strain JD. Giant cystic abdominal masses in children. Pediatr Radiol. 2005;35(12):1277–88. doi:10.1007/s00247-005-1559-7.
Yamaguchi M, Takeuchi S, Akiyama H, Sawaguchi S. Ultrasonic evaluation of abdominal masses in the pediatric patient. Tohoku J Exp Med. 1980;130(1):25–39.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Riggle, K., Gow, K. (2016). Intra-abdominal and Retroperitoneal Masses. In: Scholz, S., Jarboe, M. (eds) Diagnostic and Interventional Ultrasound in Pediatrics and Pediatric Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-21699-7_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-21699-7_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-21698-0
Online ISBN: 978-3-319-21699-7
eBook Packages: MedicineMedicine (R0)