Abstract
The equity-efficiency trade-off in health care has received increasing attention in recent decades – the ‘equity’ component referring to the distribution of health care and incorporation of social value and the ‘efficiency’ component concerned with obtaining the ‘greatest health gain per amount spent’. Which dimensions of equity should be incorporated remains unresolved, while factors such as age, social class, and time lived with the condition have all been cited as possible criteria. In terms of efficiency, economic evaluation has emerged as a useful means to guide policy decisions as to which health-care interventions should be available to the public. The quality-adjusted life-year (QALY) is a composite measure of health benefit that incorporates both quantity (life-years gained) and quality (health-related quality of life) from treatment and enables comparisons of health-care programs with different types of outcomes from various domains. It is widely used as a measure of health benefit in economic evaluation alongside intervention cost.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 The Equity-Efficiency Trade-Off and the QALY
The equity-efficiency trade-off in health care has received increasing attention in recent decades – the ‘equity’ component referring to the distribution of health care and incorporation of social value and the ‘efficiency’ component concerned with obtaining the ‘greatest health gain per amount spent’. Which dimensions of equity should be incorporated remains unresolved, while factors such as age, social class, and time lived with the condition have all been cited as possible criteria (Dolan et al. 2008).Footnote 1 In terms of efficiency, economic evaluation has emerged as a useful means to guide policy decisions as to which health-care interventions should be available to the public (Simoens 2010). The quality-adjusted life-year (QALY) is a composite measure of health benefit that incorporates both quantity (life-years gained) and quality (health-related quality of life) from treatment and enables comparisons of health-care programs with different types of outcomes from various domains (McKie et al. 1996; Ubel et al. 2000). It is widely used as a measure of health benefit in economic evaluation alongside intervention cost.
1.1 QALY Maximization
… they presume to compare apples, oranges and pears on the grounds that they are all fruit. Light and Hughes (2001)
While the current modus operandi in many countries is to maximize health outcomes (e.g. in the form of QALY maximization), whether or not this is the most suitable form of distributing resources is widely debated. An underlying condition of QALY maximization – that ‘a QALY is a QALY is a QALY’ irrespective to whom it is being allocated – has been actively questioned as many argue that distributional concerns and considerations for equity have been overlooked in efforts to achieve efficiency.
A particular concern relates to the disadvantages incurred by those who have already experienced a misfortune (e.g. poor health) and thus are anticipated to accrue fewer posttreatment QALYs than an otherwise healthy individual. Suppose, for example, there are two individuals equal in all other aspects except that one individual is in relatively good health and the other individual is partially deaf. Consider the circumstance where both require a health intervention (unrelated to the latter individual’s deafness) and only one may receive treatment. Under QALY maximization, the individual who is partially deaf is less likely to be allocated scarce resources since their condition will preclude them from generating as many posttreatment QALYs as the individual in good health. This notion of ‘double injustice’ or ‘double jeopardy’ stipulates that ‘those who have already experienced significant misfortune should not have further tribulation imposed upon them because they are not good candidates (within the efficiency calculus) for the receipt of health care’ (Harris 1985; Williams 1997).
In response to the issue of double jeopardy and as an alternative to QALY maximization insofar as incorporating distributional concerns, Alan Williams derived his fair innings argument, which is founded in the notion that everyone is entitled to a particular quality-adjusted life expectancy. Williams’ (1997) argument built upon a proposal advanced by Harris (1985) that each individual was entitled to a particular life expectancy ‘a fair innings’ and that as one fulfills this ‘fair inning’, they receive relatively lower priority for available resources.
2 The Fair Innings Argument Defined: Two Versions
2.1 Harris’ Version
Harris’ (1985) version of the fair innings argument is grounded in an aversion to inequality in age of death, positing that everyone is entitled to some ‘normal’ span of years that constitutes a ‘fair inning’. An individual who has reached their fair innings, defined by Harris as a biblical ‘three score years and ten, seventy years’, might be considered to be living ‘a sort of bonus beyond that which could reasonably be hoped for’ (emphasis added) (Harris 1970). This means priority should be given to those that have not yet reached their fair innings since, as Harris (1985) comments, ‘it is sometimes said that it is a misfortune to grow old, but it is not nearly so great a misfortune as not to grow old’. He refers to the ‘greater injustice’ experienced in a younger person dying ‘too soon’ versus the individual who has lived a reasonable amount of years.
2.2 Williams’ Version
Treating Harris’ version as a first approximation, Williams (1997, 1999) sought to bypass prioritization based on age alone by merging concerns of health experiences with those of length of life. He commented that failing to include considerations of health experiences meant that those who have lived longer lives (and who possess ‘normal’ life expectancies) in poor health might not be prescribed appropriate consideration. Thus, Williams extended the fair innings argument to propose that lifetime health is the overarching concern and that in order for fairness to be achieved, we must consider two things: first, the amount of life-years and health an individual can expect to have over the course of their lifetime (quality-adjusted life expectancy, QALE) and, second, what constitutes a fair innings QALE. Each individual’s QALE is composed of the QALYs they have accrued up to now in addition to their (future) QALE (Williams defines the sum of past QALYs and future QALE as the individual’s expected lifetime experience of health). The individual’s expected lifetime experience of health (hereon referred to simply as their QALE, noting that both past and future health are included) is subsequently compared to the fair innings QALE that serves as a reference point from which equity weights can be calculated.Footnote 2 Ceteris paribus, individuals who can expect a QALE lower than the fair innings QALE are given priority over individuals who are expected to reach their fair innings. The priority setting calculus is such that QALY gains in individuals with lower QALEs should be weighted more heavily than those of individuals who are expected to reach their fair innings.
Williams (1997) provided a detailed example of the implications of varying QALEs according to social class. He estimated that, at birth, a fair QALE for males in the UK was 61. In separating social classes 1 and 2 (‘higher’ social classes) from social classes 4 and 5 (‘lower’ social classes), he noted that the former group had a QALE of 66 whereas the latter group a QALE of 57. Thus, in order for an equitable redistribution to occur among all social classes, QALYs would need to be allocated in such a manner that those in lower social classes would receive more weight.
Although Williams illustrated his argument in the context of social classes, the fair innings argument has been widely discussed in the context of age-based rationing. Williams (1999) explained that the fair innings argument does not discriminate based on age per se, but since achieving one’s fair innings (expected lifetime health) is inherently associated with age, priority will often be ‘in favour of the young’.Footnote 3 It follows that given the young are further away from reaching their fair innings (they have thus far accumulated fewer QALYs than the relatively old), they should therefore be prioritized over older individuals and their QALYs weighted more heavily.
3 Public Preferences
While the fair innings argument has featured prominently in philosophical debate, determining whether its propositions align with public preference is desirable if the argument is to be practically applied and supported in a policy setting. In attempts to incorporate considerations for fairness into value judgments, gauging the public’s support for various methods of prioritization has become an increasingly frequent exercise (Cooper et al. 1995; Hadorn 1996).Footnote 4 Batifoulier et al. (2013) comment that in the absence of a ‘definitive conception of equity, a significant empirical literature has developed which assumes that the answer to this theoretical impasse lies with the general public’. In the UK, for example, it is proposed that ‘advice from NICE to the NHS should embody values that are generally held by the population of the NHS’ (Rawlins and Culyer 2004).
Public preferences have been shown not to align with QALY maximization (or health benefit maximization) across a variety of contexts (Ubel and Loewenstein 1995) and considerations affecting these preferences often extend well beyond strict utilitarian concerns (McKie et al. 1996). In line with both Harris’ and Williams’ versions of the fair innings argument that both suggest that priority would be allocated to the young over the old, age has been shown to be among the most frequently cited variables affecting the public’s prioritization decisions (see Nord et al. (1999) and Dolan et al. (2005) for references).
3.1 Public Preferences: Harris’ Argument
A number of studies suggest that public preferences often align with Harris’ versionFootnote 5 of the argument whereby younger individuals are prioritized over older individuals on the basis of having lived fewer years (see Tsuchiya (1999) and Dolan et al. (2005) for comprehensive reviews), although there are some exceptions (Zweibel et al. 1993; Kuder and Roeder 1995; Mossialos and King 1999; Anand and Wailoo 2000). Olsen (2013), for example, provides a convincing test of Harris’ argument, showing that it fares better than the end-of-life argument (i.e. that QALYs should be given greater weight where individuals have short life expectancies in instances where capacity to benefit is deemed sufficient).
It should be noted that in some of these studies, however, it is difficult to disentangle whether respondents prioritize younger individuals due to the fair innings argument, other forms of ‘ageism’ – namely, reasons of productivityFootnote 6 (‘productivity ageism’) – or ‘utilitarian ageism’ (QALY maximization) (Nord et al. 1996; Tsuchiya 1999; Dolan et al. 2005). An exception is a study by Tsuchiya et al. (2003) who sought to separate productivity ageism considerations from those stipulated by the fair innings argument. They found that respondents prioritized on the basis of the fair innings argument (the young received priority) when patients were given the possibility of living out their normal life expectancy; however when the benefit was fixed to 5 years, the respondents prioritized more closely in line with reasons of productivity, ranking middle-age higher.
3.2 Public Preferences: Williams’ Argument
Relatively fewer studies of public preferences have evaluated the relevance of Williams’ version of the fair innings argument. Although there is some empirical evidence that respondent priorities are influenced by information about past health (e.g. Dolan et al. 2008 Footnote 7), Stolk et al. (2005) comment that the literature has tended to focus on future gains in life expectancy and/or health. In order to truly assess if Williams’ arguments are relevant in an empirical setting, the respondent should be asked to set priorities when they are presented with lifetime health profiles – i.e. the individual’s pretreatment, present, and posttreatment health states. Implementing lifetime health profiles as well as using a mixed method approach enables the researcher to gain better insight as to if (and to what degree) respondents balanced pretreatment considerations with posttreatment considerations, the two main tenets of the fair innings argument.Footnote 8
I focus here on a study by Oliver (2009) who conducted a mixed-methods investigation into whether the fair innings argument factored into public preferences for prioritization. A brief review of studies by Dolan and Tsuchiya (2005) and Stolk et al. (2005) follows. These studies also aimed at assessing Williams’ account of the fair innings argument although they adopted slightly different methodologies to that of Oliver (2009).
3.3 A Specific Test of the Fair Innings Argument
To date, the only study to have examined Williams’ version of the fair innings argument using equity-weighted lifetime health profiles is Oliver (2009) in his article ‘A Fair Test of the Fair Innings?’ in Medical Decision Making. Oliver developed a number of priority-setting questions whereby selecting one of the patients would attenuate differences in lifetime QALYs between the two patients (possibly consistent with the fair innings argument) and selecting the other patient would correspond to QALY maximization.
Before completing the prioritization questions, a convenience sample of 50 respondents were asked to value each health state using the time trade-off (TTO). The TTO is a commonly used choice-based method for eliciting health state values for implementation into QALY calculations. In its standard form, the TTO asks respondents to state the number of years they would be willing to give up from a certain fixed time period in a deteriorated health state in order to live in full health. In Oliver’s study, respondents were asked how many years they would be willing to forgo to live in full health as opposed to living in health state x for 50 years. The aim of carrying out the TTO task was to elicit QALY values (when TTO values are combined with life-years) that could be age-weighted.Footnote 9 Since the fair innings argument prescribes that QALYs accrued by relatively young respondents should receive greater weight since they are farther from achieving their fair innings, respondents’ raw QALY values were adjusted using age-weights from Williams’ (1997) estimations of fair QALE at birth in the UK for social classes 1 and 2.Footnote 10
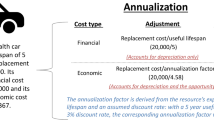
In the prioritization questions (following the same structure as that presented in Fig. 1), respondents were asked to serve as the decision-maker, and given that resources were limited, they were only able to treat one patient. The lifetime health profiles involved patients of different ages and different lifetime experiences of health. Three questions featured intragenerational trade-offs (i.e. untreated and treated life expectancies, respectively, were similar between patients), and two questions involved intergenerational trade-offs (i.e. the patients differed in their untreated and treated life expectancies).
An illustration of an intergenerational priority-setting questions in Oliver (2009) (Reprinted by permission of SAGE Publications)
Looking at the quantitative data, Oliver found that there was no discernable pattern in terms of respondents minimizing the difference in QALYs between patients or maximizing QALYs. This suggests that even when those with lower QALEs were compensated, respondents did not always elect to prioritize on the basis of the fair innings argument. Referring to the qualitative data, in three of the five priority-setting questions, some respondents (less than half the sample in each task) seemed to have made their selection on the basis of the fair innings argument. Overall, however, a wide range of context-dependent ‘decision rules’ emerged across the decision tasks that appeared to be dependent on the scenario presented. Respondents referenced reasons including maximizing QALYs,Footnote 11 maximizing life-years or posttreatment quality of life,Footnote 12 providing equal access to health care, maximizing health based on perceptions of adaptation, maximizing societal productivity (including familial roles, i.e. ‘productivity ageism’), minimizing suffering, minimizing costs, and distributing available resources equitably. As an illustration of its variability, he noted that 46 of the 50 respondents were inconsistent in their reasoning across the questions. Oliver commented that underlying values influence the respondents’ decisions, but if these values are context dependent, it becomes a challenge – if not impossible – to identify a preferred, overarching rule by which to distribute resources.
3.4 Other Studies of the Fair Innings Argument
Few other studies have implemented lifetime health profiles (including both longevity and health dimensions) in order to test whether the fair innings argument is relevant in empirical settings. Broadly, many of these studies support the results of Oliver (2009) in that the fair innings argument is but one of a host of different decision rules that are called upon.
Stolk et al. (2005) sought to evaluate whether public preferences aligned more closely with any of three equity concepts: severity of illness, fair innings, and proportional shortfall. The latter concept – proportional shortfall – refers to the ratio between the number of QALYs lost due to illness or disability and the number of QALYs expected based on age- and gender-specific norms (I return to this concept later). Respondents were provided with information about each patient’s age (ranging from 40 to 70 years old), time spent without disability, their time with health complaints, average quality of life loss, and life-years lost. It should be noted that although information in regard to past health was included, in order to simplify their analysis, all of the patients were described as having been in good health up to the point of intervention. Respondents were asked to prioritize between a series of paired lifetime health profiles and their rankings were then compared to the ranking predicted by the respective equity arguments (they assumed a fair innings QALE of 70 from which they could establish a ranking based on ‘fair innings foregone’). They found greatest support for fair innings, followed by proportional shortfall and then severity.
Dolan and Tsuchiya (2005) had respondents rank a number of health profiles that forced them to consider trade-offs between patients with short life expectancies and severe conditions across different ages. In the first set of questions respondents were asked to rank patients either of 40 or 60 years of age based on past health and future life expectancy without treatment. In the second set of questions, respondents were given the same information about past health and information about future health status without treatment over a fixed 10-year period across all respondents was provided (instead of information about future life expectancy). They found that respondents allocated priority based on past years (i.e. age) in favour of younger patients in both questions. The results were less clear in terms of past health. In the case where a health improvement was at stake (question 2), it was unclear whether the individuals’ past health influenced respondents’ prioritizations. On the other hand, past health did seem to have an influence on who was allocated the life-extending treatment (question 1).
3.5 Summary of Observations
While a relatively large body of literature provides support for Harris’ account of the fair innings argument through preferences for prioritizing the young over the old, a smaller number of investigations have assessed whether public preferences are consistent with Williams’ version of the argument. In these latter tests – that are focused on concerns of lifetime health – it appears that Williams’ argument does carry weight in respondents’ prioritizations and is a basis for their decisions in some circumstances. These findings support a similar ‘pluralistic position’ observed in some purely qualitative studies (Cookson and Dolan 1999; Wilmot and Ratcliffe 2002).
Although Williams set out with the intention of quantifying equity considerations by attaching fair innings-based weights to QALYs accrued by those with lower lifetime QALEs, empirical evidence – such as that presented above – suggests that these weights may be insufficient in accounting for context-dependent distributional concerns. A number of alternatives exist by which concerns for equity can be included in health-care decision-making, some of which may involve, for example, adopting components or variations on the fair innings argument.
4 Moving Forward: Empirical Findings, Priority Setting, and Potential Policy Implications
Given the empirical observations that respondents do not seem to rely upon a consistent decision rule that is independent of the prioritization context, some have suggested that deliberative judgments be used to incorporate equity considerations (e.g. Daniels 2008; Oliver 2009). This means that decision makers may call upon a host of different ‘rules’ to set priorities depending on the context.
When the patients are of similar ages, prioritization by severity may offer a morally justifiable solution, for example. In contrast, as the age discrepancy becomes greater between the two patients, there may be a point at which ‘the priority view’ (i.e. those who in the most dire conditions take precedence) no longer holds (Parfit 1997). Wilmot and Ratcliffe (2002) and Lewis and Charny (1989), for example, found that preferences for the young over the old are not constant in that prioritization by severity was more common when age differences were small and, on the other hand, consistent with fair innings arguments when the differences were greater.
In other instances, intragenerational debates could be informed by consideration of the ability to benefit, as implied by some empirical findings (e.g. if Oliver’s findings could be replicated insofar as respondents opting to ‘maximize’ QALYs in choosing between patients of similar ages and ‘minimizing’ QALY differences when an intergenerational choice is at hand) (e.g. QALY maximization). Whether this ‘decision rule’ is relevant, however, may be contingent on the severity of the condition of the patients involved.
Case by case deliberations might also be based on various interpretations of the fair innings argument. As presented in its original formulation by Harris, it might be desirable in some instances to establish thresholds (based on what Nord (2005) termed ‘sufficient innings’) rather than allocate priority weighting based on the degree to which one has fulfilled their fair innings. As a result, only in the case where the patient had surpassed a given threshold are they allocated relatively less priority. This is a somewhat more docile reflection of the cutoff age of 80 years Callahan (1987) proposed should be applied to life extending interventions.
In regard to possible practical implementations of such thresholds, perhaps it is helpful to ask ourselves – in what instances do we not want to prioritize someone who has ‘lived less’? There is some evidence that indicates that public preferences do not support giving priority in instances where the intervention has a poor prognosis (e.g. leaves the patient in poor health). Recently, Brazier et al. (2013) found that in attitudinal questions about end-of-life care, respondents provided preferences that indicated that the support for prioritization of end-of-life care was dependent on the level of posttreatment health the patient was able to achieve (see also Roberts et al. 1999). If older patients have poorer health outcomes as a result of certain interventions, this latter finding might imply that in these instances, they should receive lower priority or not be eligible for certain care. Importantly, Nord (2005) comments that it is one thing to restrict life-extending treatment to those who have reach a fair inning although a separate issue arises when considering the relief of suffering or pain (to a similar extent, Bowling (1996), Evans (1997), and Williams et al. (2011) propose that palliative care be exempt from prioritization and available equally to individuals of all ages regardless of QALY gainsFootnote 13). Therefore it may be that this ‘threshold’ interpretation of an individual’s fair innings is most suited for applications to only certain areas of high-cost intervention.
Developing a framework for deliberative judgement aligns with recent attempts in a number of countries to better involve the public in priority setting. For instance, in Canada and the USA, juries and panels have been used to help inform which criteria and ethical considerations are relevant for health technology assessment and cancer interventions (Menon and Stafinski 2008; Abelson et al. 2012). Similarly, NICE’s Citizens Council was initiated in order to provide insight from the public’s perspective on a number of issues to complement economic evaluation (Bognar and Hirose 2014).Footnote 14
Another option is the ‘complete lives’ system (or a version thereof) proposed by Persad et al. (2009), a framework that integrates several ethical principles into a single system. The complete lives system incorporates distributional principles (specifically youngest-first, prognosis, save the most lives, lottery, and instrumental value) so as to consider the individuals’ ‘entire lives rather than events or episodes’ on the basis that we are assigning value to human lives instead of experiences (Lockwood 1988; Rawls 1999). Notably, at its core, it is congruent with the fair innings argument insofar as prioritizing the young who have the greatest amount of ‘innings’ remaining and without intervention may fail to reach their fair innings. Further, although nascent in its development in terms of its applications to priority setting in health care, an additional alternative would be to look towards multicriteria decision analysis as a tool for concurrently balancing considerations of both equity and efficiency (Baltussen and Niessen 2006).
Alongside these attempts directed towards attaining distributive justice (determining one or a set of allocation ‘rules’ deemed justifiable as a whole), a more concentrated focus on ‘procedural justice’ and how existing methods of resource allocation are implemented has emerged. NICE specifically addresses this issue through their ‘accountability for reasonableness’ (AFR) process that encompasses the following criteria: publicity, relevance, challenge and revision, and regulation (see Daniels and Sabin 1997; NICE 2009; see chapter “Accountability for Reasonableness and Priority Setting in Health”). Publicity and relevance refer to the decision and decision process insofar as they must be publicly available (publicity) and align with those of a reasonable, ‘fair-minded’ individual (relevance). The challenge and revision criteria refer to the consideration of new evidence or further arguments in decisions and existing policy. Lastly, public or voluntary regulation should be in place to ensure the above criteria are met. Setting out policy guidelines a priori offers many advantages and will help in adherence to procedural justice while we learn more about how to appropriately incorporate social value judgments into prioritization decisions.
4.1 Existing Applications of the Fair Innings Argument
Two examples of where the fair innings argument has been translated into policy measures are in a protocol for allocating influenza vaccines in the event of a pandemic and in proposed organ allocation schemes. In the context of emergency medicine and disaster preparedness, the USA has elected to allocate greater priority to younger children than adults or older people in the instance of an influenza pandemic (Dept. of Health and Human Services 2007). Emanuel and Wertheimer (2006) comment that this sort of prioritization is consistent with a ‘life-cycle allocation principle’ that aligns with the value attached to enabling an individual to pass through ‘each life stage’.
In the context of organ allocation, the concept of survival matching under a scheme termed ‘20/80’, as explained in Hoffmaster and Hooker (2013), allocates the ‘20 percent of kidneys with the longest expected length of functioning to the 20 percent of candidates who have the longest expected length of life’ (KTC 2012). The remaining 80 % of kidneys are allocated to age-matched recipients on the basis of time spent on dialysis, a measure similar to wait time. Ross et al. (2012) proposed an alternative method of allocating kidneys termed Equal Opportunity Supplemented by Fair Innings (EOFI). The EOFI strategy operationalizes the fair innings argument by allocating the higher-quality kidneys to younger patients since they are deemed to be ‘worse off’ since they developed renal disease at a relatively earlier age and ‘consequently have had fewer years of healthy life’.
4.2 QALY Shortfall
Recent discussion across several countries has centred around how the notion of QALY shortfall – a ‘hybrid’ concept drawing on the fair innings argument and concerns for severity – might be incorporated into policy debates. QALY shortfall is manifested in two versions: absolute shortfall and proportional shortfall. Absolute shortfall relates to the total amount of QALYs lost due to a disease or condition. For example, ceteris paribus, there are two individuals: one who is perfectly healthy and can expect a future gain of 30 more QALYs and one who suffers from a condition and can expect a future QALY gain of 20 QALYs. The latter individual’s absolute shortfall is 10 QALYs (30–20). Alternatively, proportional shortfall is concerned with the ratio of QALYs lost over QALYs remaining assuming a normal life expectancy and health. Referring to the previous example, the individual in worse health has a proportional shortfall of 33 % ([(30–20)/30] × 100 = 0.33) (UK Department of Health 2011). Equalizing QALY shortfall from birth, as opposed to the time of treatment, could be interpreted as a version of the fair innings argument (Towse and Barnsley 2013).
Proportional shortfall has received support as a means of incorporating equity-based considerations in small-scale studies in the Netherlands (Stolk et al. 2005) where it seems likely to be used as a basis for equity weights in the near future (van de Wetering et al. 2013). In the UK, it has been suggested that either proportional or absolute shortfall be used to quantify burden of disease (Towse and Barnsley 2013).
Bognar and Hirose (2014) remark that the case for QALY shortfall is more intuitive compared to that for the fair innings argument given that standard cost-effectiveness is forward looking, in line with the future QALY losses considered in QALY shortfall. To this extent, it offers a simpler solution to incorporating equity claims than would the fair innings argument that would require the incorporation of past health into calculations and incur greater associated uncertainties with regard to disease trajectory, for example (Lindemark et al. 2014). This follows an earlier comment by Nord (2005) that current suffering is likely to induce a stronger reaction than past suffering, where the former may evoke strong feelings of the obligation to ‘rescue’ (see McKie and Richardson 2003) as well as align with Norwegian guidelines that recognize that helping the worst off should be a priority in the provision of health careFootnote 15 (Dolan et al 2005; Cookson et al. 2008).
An important contrasting perspective, however, is proposed by Lindemark et al. (2014) who posit that ‘the length and quality of life lived before time of intervention may be relevant in judgements about who are worse off’, referencing instances of early-onset conditions. Proportional shortfall does not encapsulate these types of considerations, and thus in some instances, it may be best to attempt to operationalize arguments that are more consistent with the fair innings argument.
4.3 Public Preferences: Important Considerations
Important decisions are to be made insofar as how we want to incorporate public preferences and to what degree. In addition, it is essential to ensure that these preferences are robust and are not artefacts of the conditions through which they are elicited (Shickle 1997; Lloyd 2003; Owen-Smith et al. 2009). It has been shown, for example, that decisions may change with better understanding or knowledge of trade-offs (e.g. of the patients’ health conditions or personal circumstances) (Ham 1993; McIver 1995), through deliberation (Dolan et al. 1999), and the decision frame (e.g. ‘lives saved’ versus ‘lives lost’ in Li et al. 2010). Schwappach (2002) comments that public preferences in support of age-based prioritization vary depending on whether the elicitation has been through public opinion surveys (limited support) or hypothetical decision or ranking tasks (where preferences have been observed to be stronger).
Congruent with the principle of ‘empirical ethics’ advanced by Richardson (2000), the evaluation of ethical principles should be undertaken through both quantitative and qualitative researches, whereby an understanding of the respondents’ perspectives is clarified and deliberated upon ‘until acceptable, stable (reliable and deliberative) ethical principles are identified (albeit unique to a particular context)’.
Whether there is a divide between the prioritization strategies that are evoked in empirical studies using patient scenarios and profiles and public support of their explicit use and the larger-scale implications of these strategies is deserving of greater attention. Cuadras-Morató et al. (2001) found that while respondents thought one method of prioritization was ‘theoretically’ superior given the circumstances presented in the questions, they prioritized on a different basis. Suppose, for example, preferences for prioritization were decided in the context of approval of political candidates’ platforms – would this different context increase our moral friction with these ideas when compared to person trade-off exercises? Kuder and Roeder (1995) demonstrated that the change in perspective affects preferences, reporting that in trade-off situations, respondents were willing to prioritize based on age, but when asked in qualitative terms about using age as a means to ration health-care resources, many disapproved (also see Zweibel et al. 1993).
It is important to determine the extent to which the ‘should’ component of prioritizing by age counterbalances society’s ‘comfort’ with the current utilitarian strategy of QALY maximization. That is, while greater distributional equity seems desirable in both empirical settings and common parlance, whether or not we can come to terms with the broader consequences of a ‘redistribution’ to the young and to the sick is another matter in itself.
5 Conclusions
While a wide range of prioritization schemes have been discussed within philosophical boundaries, a greater understanding of the degree to which they (and, more importantly, their implications) align with public preferences is necessary to move beyond philosophical arguments and towards measurable (i.e. quantifiable) policy frameworks. A substantial body of evidence indicates that the utilitarian approach of QALY maximization fails to adequately capture public preferences for a greater degree of equity into health-care distribution; however, how to go about incorporating these concerns remains unresolved.
Eliciting public preferences for various methods of distribution is one strategy that decision-makers can use to guide how equity is incorporated into policy; however, it remains open for debate as to how and the degree to which these preferences should inform priority setting (Robinson et al. 2012). The brief review of empirical evidence included in this chapter suggests that support for intergenerational equity through the fair innings principle is mixed and seems to be context dependent. Nonetheless, there are several methods by which the fair innings argument in its entirety or parts can start and have started to be implemented.
The extent to which the fair innings argument or similar principles that advocate for age-based prioritization can be translated into policy contexts will become an increasingly relevant debate as populations age, and new technologies enable health improvements and, importantly, potentially allow for increased longevity (van de Wetering et al. 2013). If this discussion is to be informed by public preferences and opinions, much work is to be done before we can assume that these preferences are robust and sustainable across empirical contexts and thus suitable for translation into policy.
Notes
- 1.
Norheim et al. (<CitationRef CitationID="CR63" >2014</Citation Ref>) recently summarized priority-setting criteria that might be considered alongside cost-effectiveness results.
- 2.
By definition, the ratio of expected QALE/fair innings QALE should be adjusted by an index of aversion to inequality r (which indicates the strength of aversion to inequality) such that (fair innings QALE/expected QALE)(1+r) (Williams <CitationRef CitationID="CR96" >1997</Citation Ref>; Oliver <CitationRef CitationID="CR65" >2009</Citation Ref>).
- 3.
To highlight an exception where the young would not be prioritized, Williams (<CitationRef CitationID="CR97" >1999</Citation Ref>) gives the example of an older individual with poor lifetime health and a somewhat younger individual with very good lifetime health.
- 4.
There are several qualitative (e.g. discussion groups) and/or quantitative (e.g. person trade-off tasks, discrete choice experiments, or contingent analysis) means through which empirical studies can gauge whether public preferences align with particular ethical principles (Green and Gerard <CitationRef CitationID="CR34" >2009</Citation Ref>). For a detailed discussion, see Hasman (<CitationRef CitationID="CR40" >2003</Citation Ref>).
- 5.
I have specified these studies as following Harris’ argument since they largely do not mention past health (and in some cases – such as life-saving scenarios – any descriptions of health at all).
- 6.
Reasons of productivity refer to the individual’s ability to contribute to society and care for others in middle age, widely referenced in the context of ‘disability-adjusted life-year’ (DALY) age-weights; see Murray and Lopez (<CitationRef CitationID="CR58" >1997</Citation Ref>).
- 7.
It is worthwhile noting that some recent studies have, in contrast, suggested that past health is not considered to be an adequate criterion on which prioritization can be based (Franken et al. <CitationRef CitationID="CR33" >2015</Citation Ref>; Nord and Johansen <CitationRef CitationID="CR60" >2014</Citation Ref>).
- 8.
The importance of the methodological approach in assessing support for various distributional arguments is highlighted by Tsuchiya et al. (<CitationRef CitationID="CR91" >2003</Citation Ref>) who remarked that, in their review of empirical evidence on age as a characteristic for priority setting, there was a dearth of studies that have incorporated qualitative components that would aid in clarifying respondents’ rationales for their decisions.
- 9.
Borrowing an example from Oliver and Sorenson (<CitationRef CitationID="CR67" >2009</Citation Ref>), suppose two individuals, P and Q, require treatment and that without this treatment they will both live for 5 more years during which P will be in full health (a health state-TTO-value of 1) and Q will be in a health state valued at 0.5 using the TTO. Together, they have an average of 3.75 expected QALYs (([5 × 1] + [5 × 0.5])/2 = 3.75). In this instance, P will have a QALY weight of 3.75/5 = 0.75, and Q will have a weight of 3.75/2.5 = 1.5. Consider that either P or Q takes a treatment that provides them with 5 additional years of life (in the same health state: P in 1 and Q in 0.5), the weighted QALY gains for both P and Q will be the same (5 × 1 × 0.75 = 3.75 for P and 5 × 0.5 × 1.5 = 3.75 for Q).
- 10.
Based on a fair innings QALE of 61 for UK males, Williams provided expected lifetime QALYs at ages 0, 20, 40, 60, and 80 of 65.8, 66.0, 66.5, 67.6, and 73.9, respectively. It follows, for example, that the age weight for a 40-year-old individual is 61/66.5 = 0.917. Thus, if the respondent provides a TTO value of 0.8 for a given health state, then the resulting weighted QALY value will be equal to 0.8 × 0.917 × the number of years spent in the health state.
- 11.
It is worthwhile noting that in some instances where respondents prioritize on the basis of QALY maximization, they may in fact have referred to the fair innings argument during their deliberative process since the fair innings argument encompasses concerns for both pre-intervention QALYS and post-intervention QALE (Oliver and Mossialos <CitationRef CitationID="CR66" >2004</Citation Ref>; Oliver <CitationRef CitationID="CR65" >2009</Citation Ref>). Whether or not the respondent maximizes QALYs when having considered the fair innings argument in their deliberation will depend on the degree to which they are averse to inequality.
- 12.
Oliver described this reason as the respondent ‘maximizing health after adjudicating for the possibility that different respondents may differentially “appreciate” a particular health state depending on the health state to which they are accustomed’.
- 13.
Johri et al. (<CitationRef CitationID="CR44" >2005</Citation Ref>) provide empirical support for this proposition.
- 14.
See Abelson et al. (<CitationRef CitationID="CR1" >2007</Citation Ref>) for additional examples of citizen engagement in policy decisions.
- 15.
It is worthwhile to note that the Norwegian Commission has combined their concern for severity with that of prognosis in order to form a multiprinciple system that more adequately controls for costs and intervention effectiveness (see Carlsson et al. <CitationRef CitationID="CR13" >2007</Citation Ref>; Sabik and Lie <CitationRef CitationID="CR80" >2008</Citation Ref>).
References
Abelson J, Giacomini M, Lehoux P, Gauvin FP (2007) Bringing ‘the public’ into health technology assessment and coverage policy decisions: from principles to practice. Health Policy 82(1):37–50
Abelson J, Wagner F, Levin L et al (2012) Consulting Ontario citizens to inform the evaluation of health technologies: the citizens’ reference panel on health technologies. Canadian Institutes of Health Research, Ottawa
Anand P, Wailoo A (2000) Utilities versus rights to publicly provided goods: arguments and evidence from health care rationing. Economica 67(268):543–577
Baltussen R, Niessen L (2006) Priority setting of health interventions: the need for multi-criteria decision analysis. Cost Effect Resour Alloc 4(1):1–9
Batifoulier P, Braddock L, Latsis J (2013) Priority setting in health care: from arbitrariness to societal values. J Institut Econ 9(01):61–80
Bognar G, Hirose I (2014) The ethics of health care rationing: an introduction. Routledge, Abingdon/New York
Bowling A (1996) Health care rationing: the public’s debate. BMJ 312(7032):670–674
Brazier J, Rowen D, Murkuria C, Whyte S et al (2013) Eliciting societal preferences for burden of illness, therapeutic improvement and end of life for value based pricing: a report of the main survey. University of York/University of Sheffield
Callahan D (1987) Setting limits: medical goals in an aging society. Simon & Schuster Children’s Publishing, New York
Carlsson P, Kärvinge C, Broqvist M, Eklund K, Hallin B, Jacobsson C et al (2007) National model for transparent vertical prioritisation in swedish health care. National Centre for Priority Setting in Health Care, Linköping
Cookson R, Dolan P (1999) Public views on health care rationing: a group discussion study. Health Policy 49(1–2):63–74
Cookson R, McCabe C, Tsuchiya A (2008) Public healthcare resource allocation and the rule of rescue. J Med Ethics 34(7):540–544
Cooper L, Coote A, Davies A (1995) Voices off: tackling the democratic deficit in health. Institute for Public Policy Research, London
Cuadras-Morató X, Pinto-Prades JL, Abellán-Perpiñán JM (2001) Equity considerations in health care: the relevance of claims. Health Econ 10(3):187–205
Daniels N (2008) Just health: meeting health needs fairly. Cambridge University Press, New York
Daniels N, Sabin J (1997) Limits to health care: fair procedures, democratic deliberation, and the legitimacy problem for insurers. Philos Public Aff 26(4):303–350
Department of Health U (2011) A new value-based approach to the pricing of branded medicines: Government response to consultation. Department of Health- Medicines, Pharmacy an Industry Group, London
Dolan P, Tsuchiya A (2005) Health priorities and public preferences: the relative importance of past health experience and future health prospects. J Health Econ 24(4):703–714
Dolan P, Cookson R, Ferguson B (1999) Effect of discussion and deliberation on the public’s views of priority setting in health care: focus group study. BMJ 318(7188):916–919
Dolan P, Shaw R, Tsuchiya A, Williams A (2005) QALY maximisation and people’s preferences: a methodological review of the literature. Health Econ 14(2):197–208
Dolan P, Edlin R, Tsuchiya A (2008) The relative societal value of health gains to different beneficiaries. London: National Institute for Health and Care Excellence
Emanuel EJ, Wertheimer A (2006) Public health. Who should get influenza vaccine when not all can? Science 312(5775):854–855
Evans JG (1997) The case against. BMJ; 314:822–825
Excellence NIfHaC (2009) Social value judgments: principles for the development of NICE guidance. NICE, London
Franken M, Stolk E, Scharringhausen T, de Boer A, Koopmanschap M (2015) A comparative study of the role of disease severity in drug reimbursement decision making in four European countries. Health Policy 119(2):195–202
Green C, Gerard K (2009) Exploring the social value of health-care interventions: a stated preference discrete choice experiment. Health Econ 18(8):951–976
Hadorn D (1996) The Oregon priority-setting exercise: cost-effectiveness and the rule of rescue, revisited. Med Decis Making 16(2):117–119
Ham C (1993) Priority setting in the NHS: reports from six districts. BMJ 307(6901):435
Harris J (1970) The value of life, an introduction to medical ethics. Routledge & Keegan Paul, London
Harris J (1985) The value of life. London: Routledge
Hasman A (2003) Eliciting reasons: empirical methods in priority setting. Health Care Anal 11(1):41–58
Hoffmaster B, Hooker C (2013) Tragic choices and moral compromise: the ethics of allocating kidneys for transplantation. Milbank Q 91(3):528–557
Johri M, Damschroder LJ, Zikmund-Fisher BJ, Ubel PA (2005) The importance of age in allocating health care resources: does intervention-type matter? Health Econ 14(7):669–678
Kuder LB, Roeder PW (1995) Attitudes toward age-based health care rationing. A qualitative assessment. J Aging Health 7(2):301–327
KTC (Kidney Transplantation Committee) Report to the Board of Directors, (2012). 12–13. Available at http://optn.transplant.hrsa.gov/CommitteeReports/board_main_KidneyTransplantationCommittee_11_14_2012_11_33.pdf (accessed December 6th, 2014).
Lewis PA, Charny M (1989) Which of two individuals do you treat when only their ages are different and you can’t treat both? J Med Ethics 15(1):28–34
Li M, Vietri J, Galvani AP, Chapman GB (2010) How do people value life? Psychol Sci 21(2):163–167
Light DW, Hughes D (2001) Introduction: a sociological perspective on rationing: power, rhetoric and situated practices. Sociol Health Illn 23(5):551–569
Lindemark F, Norheim O, Johansson K (2014) Making use of equity sensitive QALYs: a case study on identifying the worse off across diseases. Cost Effect Resour Alloc 12(1):1–9
Lloyd AJ (2003) Threats to the estimation of benefit: are preference elicitation methods accurate? Health Econ 12(5):393–402
Lockwood M (1988) Quality of life and resource allocation. R Inst Philos Suppl 23:33–55
McIver S (1995) Information for public choice. Br Med Bull 51(4):900–913
McKie J, Richardson J (2003) The rule of rescue. Soc Sci Med 56(12):2407–2419
McKie J, Kuhse H, Richardson J, Singer P (1996) Double jeopardy, the equal value of lives and the veil of ignorance: a rejoinder to Harris. J Med Ethics 22(4):204–208
Menon D, Stafinski T (2008) Engaging the public in priority-setting for health technology assessment: findings from a citizens’ jury. Health Expect 11(3):282–293
Mossialos E, King D (1999) Citizens and rationing: analysis of a European survey. Health Policy 49(1–2):75–135
Murray C, Lopez AD (1997) The utility of DALYs for public health policy and research: a reply. Bull World Health Organ 75(4):377
Nord E (2005) Concerns for the worse off: fair innings versus severity. Soc Sci Med 60(2):257–263
Nord E, Johansen R (2014) Concerns for severity in priority setting in health care: a review of trade-off data in preference studies and implications for societal willingness to pay for a QALY. Health Policy 116(2–3):281–288
Nord E, Street A, Richardson J, Kuhse H, Singer P (1996) The significance of age and duration of effect in social evaluation of health care. Health Care Anal 4(2):103–111
Nord E, Pinto JL, Richardson J, Menzel P, Ubel P (1999) Incorporating societal concerns for fairness in numerical valuations of health programmes. Health Econ 8(1):25–39
Norheim OF, Baltussen R, Johri M, Chisholm D, Nord E, Brock D et al (2014) Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost Effect Resour Alloc 12:18
Oliver A (2009) A fair test of the fair innings? Med Decis Making 29(4):491–499
Oliver A, Mossialos E (2004) Equity of access to health care: outlining the foundations for action. J Epidemiol Community Health 58(8):655–658
Oliver A, Sorenson C (2009) The limits and challenges to the economic evaluation of health technologies. In: Costa-i-Font J, Courbage C, McGuire A (eds) The economics of new health technologies: incentives, organization, and financing. Oxford University Press, Oxford, pp 205–218
Olsen JA (2013) Priority preferences: “end of life” does not matter, but total life does. Value Health 16(6):1063–1066
Owen-Smith A, Coast J, Donovan J (2009) “I can see where they’re coming from, but when you’re on the end of it … you just want to get the money and the drug”.: explaining reactions to explicit healthcare rationing. Soc Sci Med 68(11):1935–1942
Parfit D (1997) Equality and priority. Ratio 10(3):202–221
Persad G, Wertheimer A, Emanuel EJ (2009) Principles for allocation of scarce medical interventions. Lancet 373(9661):423–431
Rawlins MD, Culyer AJ (2004) National Institute for Clinical Excellence and its value judgments. BMJ 329(7459):224–227
Rawls J (1999) A theory of justice. Oxford University Press, Oxford
Richardson J (2000) Empirical ethics versus analytical orthodoxy: two constrasting bases for the reallocation of resources. In J Bridges (ed) Economics and Health: Proceedings of the twenty-second Australian Conference of Health Economists. University of New South Wales, School of Health Services Management: Sydney, 227–42.
Roberts T, Bryan S, Heginbotham C, McCallum A (1999) Public involvement in health care priority setting: an economic perspective. Health Expect 2(4):235–244
Robinson S, Williams I, Dickinson H, Freeman T, Rumbold B (2012) Priority-setting and rationing in healthcare: evidence from the English experience. Soc Sci Med 75(12):2386–2393
Ross LF, Parker W, Veatch RM, Gentry SE, Thistlethwaite JJR (2012) Equal opportunity supplemented by fair innings: equity and efficiency in allocating deceased donor kidneys. Am J Transplant 12(8):2115–2124
Sabik L, Lie R (2008) Priority setting in health care: lessons from the experiences of eight countries. Int J Equity Health 7(1):1–13
Schwappach DLB (2002) Resource allocation, social values and the QALY: a review of the debate and empirical evidence. Health Expect 5(3):210–222
Services DoHaH (2007) Draft guidance on allocating and targeting pandemic influenza vaccine. Services DoHaH, Washington, DC
Shickle D (1997) Public preferences for health care: prioritisation in the United Kingdom. Bioethics 11(3–4):277–290
Simoens S (2010) Health technology assessment and economic evaluation across jurisdictions. Value Health 13(6):857–859
Stolk EA, Pickee SJ, Ament AH, Busschbach JJ (2005) Equity in health care prioritisation: an empirical inquiry into social value. Health Policy 74(3):343–355
Towse A, Barnsley P (2013) Clarifying the meanings of absolute and proportional shortfall with examples. Office of Health Economics, London
Tsuchiya A (1999) Age-related preferences and age weighting health benefits. Soc Sci Med 48(2):267–276
Tsuchiya A, Dolan P, Shaw R (2003) Measuring people’s preferences regarding ageism in health: some methodological issues and some fresh evidence. Soc Sci Med 57(4):687–696
Ubel PA, Loewenstein G (1995) The efficacy and equity of retransplantation: an experimental survey of public attitudes. Health Policy 34(2):145–151
Ubel P, Nord E, Gold M, Menzel P, Prades J-LP, Richardson J (2000) Improving value measurement in cost-effectiveness analysis. Med Care 38(9):892–901
Van de Wetering E, Stolk E, Van Exel N, Brouwer WB (2013) Balancing equity and efficiency in the Dutch basic benefits package using the principle of proportional shortfall. Eur J Health Econ 14(1):107–115
Williams A (1997) Intergenerational equity: an exploration of the ‘fair innings’ argument. Health Econ 6(2):117–132
Williams A (1999) Inequalities in health and intergenerational equity. Ethical Theory Moral Pract 2(1):47–55
Williams I, Robinson S, Dickinson H (2011) Rationing in health care: the theory and practice of priority setting. Policy Press, Bristol
Wilmot S, Ratcliffe J (2002) Principles of distributive justice used by members of the general public in the allocation of donor liver grafts for transplantation: a qualitative study. Health Expect 5(3):199–209
Zweibel N, Cassel C, Karrison T (1993) Public attitudes about the use of chronological age as a criterion for allocating heath care resources. Gerontologist 33(1):74–80
Acknowledgements
I would like to thank Dr. Adam Oliver for his guidance and insightful comments.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Watters, S.M. (2016). Fair Innings as a Basis for Prioritization: An Empirical Perspective. In: Nagel, E., Lauerer, M. (eds) Prioritization in Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-21112-1_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-21112-1_14
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-21111-4
Online ISBN: 978-3-319-21112-1
eBook Packages: MedicineMedicine (R0)