Abstract
The molecular characterization of recurrent chromosome aberrations in the early 1980s laid the foundation for gene fusion detection in cancer. This approach remained the unrivalled method to identify fusion genes for a quarter of a century and led to the detection of more than 700 neoplasia-associated fusion genes. The advancement of deep sequencing in the mid-2000s revolutionized the search for cytogenetically undetectable fusions, and such studies have dramatically changed the gene fusion landscape. A myriad of new gene fusions – more than 1,300 – the great majority involving previously unsuspected genes, have been identified by sequencing-based analyses during the past 10 years.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
One hundred years ago, Theodor Boveri in his famous book Zur Frage der Entstehung maligner Tumoren [1] proposed an idea that later became known as the somatic mutation theory of cancer, which essentially states that cancer originates in a single cell by a mitotic disturbance leading to chromosomal damage. The acquired genetic change is then propagated during subsequent mitoses to all descendants of the originally transformed cell. This concept is today the paradigmatic view of cancer pathogenesis, supported by a wealth of experimental evidence. It long remained a theoretical idea, however, which could not be examined critically until technical improvements in human cytogenetic analysis were made half a century later, culminating in the description of the normal human chromosome complement by Tjio and Levan in 1956 [2].
The discovery only 4 years later by Nowell and Hungerford [3] of an acquired characteristic marker chromosome consistently seen in patients with chronic myelogenous leukaemia (CML), later designated the Philadelphia chromosome (Ph) after the city where it had been found, immediately provided strong support for the idea that chromosome aberrations indeed may play a major role in the initiation of the carcinogenic process. It was reasonable to assume that the specific chromosomal abnormality – a perfect example of a somatic mutation in a haematopoietic stem cell – was the direct cause of the neoplastic state, i.e., the true verification of Boveri’s somatic mutation theory. The discovery of the Ph chromosome greatly stimulated interest in cancer cytogenetics in the 1960s. However, the results obtained over the next decade were disappointing. Chromosome aberrations were detected in most tumours but no specific change comparable to the Ph was found. The abnormalities varied within the same tumour types and among patients, and at the end of the 1960s most scientists agreed that chromosome aberrations were secondary epiphenomena – not the cause, but the consequence, of neoplasia. The Ph was the exception to the rule that chromosome changes did not play any important pathogenetic role in carcinogenesis.
2 Chromosome Banding
The situation changed dramatically in 1970 with the introduction of chromosome banding by Caspersson and co-workers [4]. Each chromosome, chromosome arm, and even chromosome region could now be precisely identified on the basis of its unique banding pattern, and hence aberrations that previously had not been possible to detect could now be visualized. The first characteristic cytogenetic changes in cancer cells discovered with the help of the new technique appeared in 1972 (see Mitelman and Heim [5] for a review of the early data): a 14q+ marker chromosome in Burkitt lymphoma (BL), a deletion of the long arm of a chromosome 20 in polycythemia vera, +8 in acute myeloid leukaemia (AML), and −22 in meningiomas. The first balanced rearrangements were reported shortly afterwards. In 1973, Rowley first identified a reciprocal translocation between chromosomes 8 and 21, i.e., t(8;21)(q22;q22), in the bone marrow cells of a patient with AML [6] and the very same year she showed that the Ph in CML originated through a t(9;22)(q34;q11), not a deletion of the long arm of chromosome 22 as previously thought [7]. A steadily increasing number of characteristic, specific, sometimes even pathognomonic balanced rearrangements, in particular translocations, were soon described in various haematologic disorders and malignant lymphomas, including t(8;14)(q24;q32), t(2;8)(p11;q24), and t(8;22)(q24;q11) in BL [8–11], t(15;17)(q22;q21) in acute promyelocytic leukaemia [12], t(4;11)(q21;q23) in acute lymphoblastic leukaemia [13], t(8;16)(p11;p13) in acute monocytic leukaemia [14], and t(14;18)(q32;q21) in follicular lymphoma [15]. The first specific translocations in experimental neoplasms and, as it turned out, the perfect equivalents of the characteristic rearrangements in human BL were identified by Ohno et al. [16] in mouse plasmacytomas (MPC) by the end of the 1970s.
The following decade saw a similar explosion of data emerging from studies of solid tumours, initially in particular among mesenchymal tumours. Several of the aberrations identified in the solid tumours were as specific as those previously found among haematologic malignancies, e.g., t(2;13)(q36;q14) in alveolar rhabdomyosarcoma [17], t(11;22)(q24;q12) in Ewing sarcoma [18, 19], and t(12;16)(q13;p11) in myxoid liposarcoma [20]. At this time, it also became clear that many benign tumours carried characteristic aberrations, including reciprocal translocations, e.g., t(3;8)(p21;q12) in salivary gland adenoma [21], t(3;12)(q27–28;q13–15) in lipoma [22, 23], and t(12;14)(q14;q24) in uterine leiomyoma [24–26]. All published abnormal karyotypes in neoplasia detected by banding analyses are presented in Mitelman et al. [27], and a comprehensive review of the presently known recurrent and specific chromosome aberrations may be found in Heim and Mitelman [28].
3 Recombinant DNA Technology
Technical developments in the late 1970s enabling the identification and characterization of genes in the breakpoints of chromosome rearrangements made it possible to elucidate the molecular consequences of the recurrent cancer-associated chromosome changes, and analyses in the early 1980s of the specific translocations in MPC, BL, and CML proved particularly pivotal for our understanding of how chromosome aberrations contribute to neoplastic transformation. When the different pieces of the puzzle were assembled, it became apparent that balanced rearrangements exert their effects by one of two mechanisms: Transcriptional up-regulation of an oncogene in one of the breakpoints through exchange of regulatory sequences in the other breakpoint, and the creation of a hybrid gene through fusion of parts of two genes, one in each breakpoint [29]. Deregulation of an oncogene by juxtaposition to a constitutively active gene region was predicted by Klein already in 1981 [30] and the principle was soon demonstrated in MPC and human BL. The breakpoints of the characteristic translocations in mice and humans were found to be located within or close to the MYC oncogene and one of the immunoglobulin heavy- or light-chain genes (IGH, IGK or IGL). As a consequence of the translocations, the entire coding part of MYC is juxtaposed to one of the immunoglobulin genes, resulting in deregulation of MYC because the gene is now driven by regulatory elements of the immunoglobulin genes. The alternative mechanism – the creation of a fusion gene – was documented at the same time in CML with the demonstration that the Ph chromosome, i.e., the der(22)t(9;22)(q34;q11), contains a fusion in which the 3′ part of the ABL1 oncogene from 9q34 has become juxtaposed with the 5′ part of a gene from 22q11 called the BCR gene, resulting in the creation of an in-frame BCR/ABL1 fusion transcript.
The first confirmation of the BL scenario in another B-cell neoplasm was the demonstration in 1984 that the t(14;18)(q32;q21) in follicular lymphoma results in overexpression of BCL2 [31] due to its juxtaposition to the IGH locus, and in 1986 an analogous situation was established in T-cell acute lymphoblastic leukaemia in which regulatory elements of the T-cell receptor alpha (TRA) gene were found to deregulate the expression of MYC [32–34]; other 3′ partner genes, e.g., LYL1, TAL1, LMO1,and LMO2, involved in translocations involving TRB and TRD loci were soon identified in T-cell leukaemias/lymphomas carrying various translocations [35–39]. The CML scenario, i.e., the creation of a chimeric fusion gene, was firmly established in both haematologic malignancies and solid tumours in the early 1990s: PML/RARA in acute promyelocytic leukaemia with t(15;17)(q22;q21) [40, 41], RET/CCDC6 in thyroid carcinomas with inv(10)(q11q21) [42], DEK/NUP214 in AML with t(6;9)(p22;q34) [43], RUNX1/RUNX1T1 in AML with t(8;21)(q22;q22) [44], and EWSR1/FLI1 in Ewing sarcoma with t(11;22)(q24;q12) [45].
The molecular insights into the pathogenetic mechanisms of cancer-specific chromosome aberrations sparked an enormous interest in cancer cytogenetics as a powerful tool to locate and identify genes important in tumourigenesis. Further technical improvements during the 1980s, in particular the development of fluorescence in situ hybridization (FISH), multi-colour FISH, and the widespread adoption of the polymerase chain reaction (PCR), added a further sophistication to the analysis, and radically increased the precision in identifying new gene fusions [28]. This course of action – the genomic characterization of the breakpoints in cytogenetically detected specific balanced aberrations – remained the unrivalled method to identify fusion genes in cancer for a quarter of a century and led to the detection of more than 700 fusion genes (Table 1.1) caused by acquired translocations, inversions, and insertions characterizing various tumour entities [27].
There was a major limitation of this remarkably successful approach, however. It was in principle restricted to haematological malignancies and mesenchymal tumours, which typically have simple abnormalities, often seen as a sole anomaly. Malignant epithelial tumours, representing the dominant cause of human cancer morbidity and mortality, which characteristically have complex karyotypes with numerous numerical and structural abnormalities, were consequently not amenable for analysis. As a consequence, very few fusion genes were detected in carcinomas. By 2005, only 29 fusion genes were known in carcinomas, all organs combined, as compared to 56 in mesenchymal neoplasms and 272 in haematological malignancies. These quantitative differences led to the generally held view that fusion genes are not an important mechanism in carcinoma pathogenesis. Indirect evidence that fusion genes actually may play the same fundamental role in epithelial carcinogenesis as they do for the initiation of haematologic and mesenchymal neoplasms was presented by Mitelman et al. [46], and direct evidence clearly substantiating this view was soon produced with the help of new powerful technologies developed during the last decade.
4 Next-Generation Sequencing
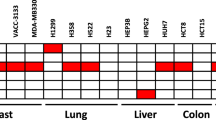
The breakthrough in the search for fusion genes by alternative methods to chromosome banding analysis followed by reverse transcriptase-PCR and Sanger sequencing was made by Chinnaiyan and coworkers in 2005 [47]. They took a bioinformatics approach to look for genes in prostate cancer that showed a very high expression in RNA microarray experiments, and demonstrated that two of the outlier genes – ERG and ETV1 – were frequently fused to the 5′ part of the prostate-specific androgen-regulated gene TMPRSS2. Subsequently other ETS family genes were found to be fused with TMPRSS2, and several other 5′ partner genes that activate ETS genes were also discovered [48]. The frequencies of the various fusions vary slightly in different patient series depending on the populations studied but altogether about 80 % of prostate cancers harbour one of the presently known fusion genes, the most common being TMPRSS2/ERG. Very soon afterwards, an EML4/ALK gene fusion was found in a subset of non-small cell lung cancer by screening a retroviral cDNA expression library from cancer samples [49]. The importance of these results in prostate and lung cancer cannot be overestimated. They showed, for the first time, that cytogenetically undetectable gene fusions may be a causative factor in a substantial fraction of common human cancers, and the findings underscored the need for high-resolution methods to be used in parallel with chromosome banding to characterize cancer genomes. The advancement of next-generation sequencing (NGS) at this time revolutionized the search for new fusion genes, enabling unprecedented opportunities to process thousands of tumours for systematic mutation and fusion gene discovery without any knowledge of the genetic constitution. The first report using the new sequencing technology to find fusion genes in cancer was presented by Stratton and co-workers in 2008 [50]. Numerous studies of common cancer types, such as carcinomas of the breast, lung, prostate, and uterus, quickly followed (e.g., [51–57]), and the results have dramatically changed the gene fusion landscape. A myriad of new gene fusions – more than 1,300 – the great majority involving previously unsuspected genes, have been identified with the help of NGS-based analysis [27]. Table 1.1 shows the dramatic increase of gene fusions detected since 2010, in particular among malignant epithelial tumours, and Table 1.2 presents the distribution of all presently reported fusions among major neoplasia subtypes.
As can be seen from Table 1.1, the total number of gene fusions now exceeds 2,000 and at least 65 % of these were identified by various sequencing technologies during the last 5 years. Clearly, the presently known gene fusions represent only the tip of an iceberg. Given the extraordinary rate at which The Cancer Genome Atlas (TCGA) project is generating cancer genomic data [58, 59], a huge number of new genomic rearrangements can be expected to be discovered within the next few years. It is important in this context to mention two notable differences between the fusion genes detected on the basis of cytogenetically identified aberrations and those so far identified by NGS. First, multiple NGS-detected fusion genes are generally found within the same tumour, e.g., more than 25 different fusions in one prostate cancer, and secondly, very few of the NGS-detected fusion genes have been found to be recurrent. A major challenge will be to verify by functional studies which of the alleged gene fusions are primary, pathogenetically important, and which are either secondary progressional changes or non-consequential “noise” abnormalities.
References
Boveri T (1914) Zur Frage der Entstehung maligner Tumoren. Gustav Fisher Verlag, Jena
Tjio JH, Levan A (1956) The chromosome number of man. Hereditas 42:1–6
Nowell PC, Hungerford DA (1960) A minute chromosome in human chronic granulocytic leukemia. Science 132:1497
Caspersson T, Zech L, Johansson C (1970) Differential binding of alkylating fluorochromes in human chromosomes. Exp Cell Res 60:315–319
Mitelman F, Heim S (2015) How it all began: cancer cytogenetics before sequencing. In: Heim S, Mitelman F (eds) Cancer cytogenetics, 4th edn. Wiley, New York
Rowley JD (1973) Identification of a translocation with quinacrine fluorescence in a patient with acute leukemia. Ann Genet 16:109–112
Rowley JD (1973) A new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature 243:290–293
Zech L, Haglund U, Nilsson K, Klein G (1976) Characteristic chromosomal abnormalities in biopsies and lymphoid-cell lines from patients with Burkitt and non-Burkitt lymphomas. Int J Cancer 17:47–56
Berger R, Bernheim A, Weh H-J, Flandrin G, Daniel MT et al (1979) A new translocation in Burkitt’s tumor cells. Hum Genet 53:111–112
Miyoshi I, Hiraki S, Kimura I, Miyamoto K, Sato J (1979) 2/8 translocation in a Japanese Burkitt’s lymphoma. Experientia 35:742–743
van den Berghe H, Parloir C, Gosseye S, Englebienne V, Cornu G et al (1979) Variant translocation in Burkitt lymphoma. Cancer Genet Cytogenet 1:9–14
Rowley JD, Golomb HM, Dougherty C (1977) 15/17 translocation, a consistent chromosomal change in acute promyelocytic leukaemia. Lancet 1:549–550
Oshimura M, Freeman AI, Sandberg AA (1977) Chromosomes and causation of human cancer and leukemia. XXVI. Banding studies in acute lymphoblastic leukemia (ALL). Cancer 40:1161–1172
Mitelman F, Brandt L, Nilsson PG (1978) Relation among occupational exposure to potential mutagenic/carcinogenic agents, clinical findings, and bone marrow chromosomes in acute nonlymphocytic leukemia. Blood 52:1229–1237
Fukuhara S, Rowley JD, Variakojis D, Golomb HM (1979) Chromosome abnormalities in poorly differentiated lymphocytic lymphoma. Cancer Res 39:3119–3128
Ohno S, Babonits M, Wiener F, Spira J, Klein G et al (1979) Nonrandom chromosome changes involving the Ig gene-carrying chromosomes 12 and 6 in pristane-induced mouse plasmacytomas. Cell 18:1001–1007
Seidal T, Mark J, Hagmar B, Angervall L (1982) Alveolar rhabdomyosarcoma: a cytogenetic and correlated cytological and histological study. APMIS 90:345–354
Aurias A, Rimbaut C, Buffe D, Dubousset J, Mazabraud A (1983) Chromosomal translocations in Ewing’s sarcoma. N Engl J Med 309:496–497
Turc-Carel C, Philip I, Berger M-P, Philip T, Lenoir GM (1983) Chromosomal translocations in Ewing’s sarcoma. N Engl J Med 309:497–498
Limon J, Turc-Carel C, Dal Cin P, Rao U, Sandberg AA (1986) Recurrent chromosome translocations in liposarcoma. Cancer Genet Cytogenet 22:93–94
Mark J, Dahlenfors R, Ekedahl C, Stenman G (1980) The mixed salivary gland tumor – a normally benign human neoplasm frequently showing specific chromosomal abnormalities. Cancer Genet Cytogenet 2:231–241
Heim S, Mandahl N, Kristoffersson U, Mitelman F, Rööser B et al (1986) Reciprocal translocation t(3;12)(q27;q13) in lipoma. Cancer Genet Cytogenet 23:301–304
Turc-Carel C, Dal Cin P, Rao U, Karakousis C, Sandberg AA (1986) Cytogenetic studies of adipose tissue tumors. I. A benign lipoma with reciprocal translocation t(3;12)(q28;q14). Cancer Genet Cytogenet 23:283–289
Heim S, Nilbert M, Vanni R, Floderus U-M, Mandahl N et al (1988) A specific translocation, t(12;14)(q14-15;q23-24), characterizes a subgroup of uterine leiomyomas. Cancer Genet Cytogenet 32:13–17
Mark J, Havel G, Grepp C, Dahlenfors R, Wedell B (1988) Cytogenetical observations in human benign uterine leiomyomas. Anticancer Res 8:621–626
Turc-Carel C, Dal Cin P, Boghosian L, Terk-Zakarian J, Sandberg AA (1988) Consistent breakpoints in region 14q22-q24 in uterine leiomyoma. Cancer Genet Cytogenet 32:25–31
Mitelman F, Johansson B, Mertens F (2014) Mitelman database of chromosome aberrations and gene fusions in cancer. http://cgap.nci.nih.gov/Chromosomes/Mitelman
Heim S, Mitelman F (eds) (2015) Cancer cytogenetics, 4th edn. Wiley, New York
Mitelman F, Johansson B, Mertens F (2007) The impact of translocations and gene fusions on cancer causation. Nat Rev Cancer 7:233–245
Klein G (1981) The role of gene dosage and genetic transpositions in carcinogenesis. Nature 294:313–318
Tsujimoto Y, Finger LR, Yunis J, Nowell PC, Croce CM (1984) Cloning of the chromosome breakpoint of neoplastic B cells with the t(14;18) chromosome translocation. Science 226:1097–1099
Erikson J, Finger L, Sun L, ar-Rushdi A, Nishikura K et al (1986) Deregulation of c-myc by translocation of the alfa-locus of the T-cell receptor in T-cell leukemias. Science 232:884–886
Mathieu-Mahul D, Sigaux F, Zhu C, Bernheim A, Mauchauffe M et al (1986) A t(8;14)(q24;q11) translocation in a T-cell leukemia (L1-ALL) with c-myc and TcR-alpha chain locus rearrangements. Int J Cancer 38:835–840
McKeithan TW, Shima EA, Le Beau MM, Minowada J, Rowley JD et al (1986) Molecular cloning of the breakpoint junction of a human chromosomal 8;14 translocation involving the T-cell receptor alpha-chain gene and sequences on the 3′ side of MYC. Proc Natl Acad Sci U S A 83:6636–6640
Boehm T, Baer R, Lavenir I, Forster A, Waters JJ et al (1988) The mechanism of chromosomal translocation t(11;14) involving the T-cell receptor Cdelta locus on human chromosome 14q11 and a transcribed region of chromosome 11p15. EMBO J 7:385–394
Mellentin JD, Smith SD, Cleary ML (1989) lyl-1, a novel gene altered by chromosomal translocation in T cell leukemia, codes for a protein with a helix-loop-helix DNA binding motif. Cell 58:77–83
Finger LR, Kagan J, Christopher G, Kurtzberg J, Hershfield MS et al (1989) Involvement of the TCL5 gene on human chromosome 1 in T-cell leukemia and melanoma. Proc Natl Acad Sci U S A 86:5039–5043
McGuire EA, Hockett RD, Pollock KM, Bartholdi MF, O’Brien SJ et al (1989) The t(11;14)(p15;q11) in a T-cell acute lymphoblastic leukemia cell line activates multiple transcripts, including Ttg-1, a gene encoding a potential zinc finger protein. Mol Cell Biol 9:2124–2132
Boehm T, Foroni L, Kaneko Y, Perutz MF, Rabbitts TH (1991) The rhombotin family of cysteine-rich LIM-domain oncogenes: distinct members are involved in T-cell translocations to human chromosomes 11p15 and 11p13. Proc Natl Acad Sci U S A 88:4367–4371
Lemons RS, Eilender D, Waldmann RA, Rebentisch M, Frej A-K et al (1990) Cloning and characterization of the t(15;17) translocation breakpoint region in acute promyelocytic leukemia. Gene Chromosome Cancer 2:79–87
de Thé H, Chomienne C, Lanotte M, Degos L, Dejean A (1990) The t(15;17) translocation of acute promyelocytic leukaemia fuses the retinoic acid receptor alpha gene to a novel transcribed locus. Nature 347:558–561
Pierotti MA, Santoro M, Jenkins RB, Sozzi G, Bongarzone I et al (1992) Characterization of an inversion on the long arm of chromosome 10 juxtaposing D10S170 and RET and creating the oncogenic sequence RET/PTC. Proc Natl Acad Sci U S A 89:1616–1620
von Lindern M, Fornerod M, van Baal S, Jaegle M, de Wit T et al (1992) The translocation (6;9), associated with a specific subtype of acute myeloid leukemia, results in the fusion of two genes, dek and can, and the expression of a chimeric, leukemia-specific dek-can mRNA. Mol Cell Biol 12:1687–1697
Erickson P, Gao J, Chang K-S, Look T, Whisenant E et al (1992) Identification of breakpoints in t(8;21) acute myelogenous leukemia and isolation of a fusion transcript, AML1/ETO, with similarity to Drosophila segmentation gene, runt. Blood 80:1825–1831
Delattre O, Zucman J, Plougastel B, Desmaze C, Melot T et al (1992) Gene fusion with an ETS DNA-binding domain caused by chromosome translocation in human tumours. Nature 359:162–165
Mitelman F, Johansson B, Mertens F (2004) Fusion genes and rearranged genes as a linear function of chromosome aberrations in cancer. Nat Genet 36:331–334
Tomlins SA, Rhodes DR, Perner S, Dhanasekaran SM, Mehra R et al (2005) Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science 310:644–648
Rubin MA, Maher CA, Chinnaiyan AM (2011) Common gene rearrangements in prostate cancer. J Clin Oncol 29:3659–3668
Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y et al (2007) Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 448:561–566
Campbell PJ, Stephens PJ, Pleasance ED, O’Meara S, Li H et al (2008) Identification of somatically acquired rearrangements in cancer using genome-wide massively parallel paired-end sequencing. Nat Genet 40:722–729
Maher CA, Kumar-Sinha C, Cao X, Kalyana-Sundaram S, Han B et al (2009) Transcriptome sequencing to detect gene fusions in cancer. Nature 458:97–101
Stephens PJ, McBride DJ, Lin M-L, Varela I, Pleasance ED et al (2009) Complex landscapes of somatic rearrangement in human breast cancer genomes. Nature 462:1005–1010
Robinson DR, Kalyana-Sundaram S, Wu Y-M, Shankar S, Cao X et al (2011) Functionally recurrent rearrangements of the MAST kinase and Notch gene families in breast cancer. Nat Med 17:1646–1651
Asmann YW, Necela BM, Kalari KR, Hossain A, Baker TR et al (2012) Detection of redundant fusion transcripts as biomarkers or disease-specific therapeutic targets in breast cancer. Cancer Res 72:1921–1928
Hammerman PS, Hayes DN, Wilkerson MD, Schultz N, Bose R et al (2012) Comprehensive genomic characterization of squamous cell lung cancers. Nature 489:519–525
Lapuk AV, Wu C, Wyatt AW, McPherson A, McConeghy BJ et al (2012) From sequence to molecular pathology, and a mechanism driving the neuroendocrine phenotype in prostate cancer. J Pathol 227:286–297
Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y et al (2013) Integrated genomic characterization of endometrial carcinoma. Nature 497:67–73
Kandoth C, McLellan MD, Vandin F, Ye K, Niu B et al (2013) Mutational landscape and significance across 12 major cancer types. Nature 402:333–341
Weinstein JN, Collisson EA, Mills GB, Mills Shaw KR, Ozenberger BA et al (2013) The cancer genome atlas pan-cancer analysis project. Nat Genet 45:1113–1120
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Mitelman, F. (2015). A Short History of Chromosome Rearrangements and Gene Fusions in Cancer. In: Rowley, J., Le Beau, M., Rabbitts, T. (eds) Chromosomal Translocations and Genome Rearrangements in Cancer. Springer, Cham. https://doi.org/10.1007/978-3-319-19983-2_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-19983-2_1
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-19982-5
Online ISBN: 978-3-319-19983-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)