Abstract
The patient was a 14-year-old right-hand dominant male who tripped on a tennis ball and landed on his outstretched left hand 1 week prior to presentation. He was evaluated by the emergency room and diagnosed with a scaphoid fracture. Initial treatment consisted of placing him in a removable thumb spica splint. He was then referred to a hand surgeon for additional evaluation and treatment. On presentation to the hand surgeon, he complained of mild-to-moderate intermittent pain. He denied any limitations in his activities of daily living. The patient was an elite tennis player and was eager to resume playing tennis as early as possible.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute pediatric scaphoid waist fractures
- Pediatric scaphoid waist fractures scaphoid waist fractures in pediatrics
- Carpal scaphoid fracture nonunion in children
- Percutaneous screw fixation in pediatric scaphoid fracture
- Screw fixation in pediatric scaphoid fracture
Case Presentation
The patient was a 14-year-old right-hand dominant male who tripped on a tennis ball and landed on his outstretched left hand 1 week prior to presentation . He was evaluated by the emergency room and diagnosed with a scaphoid fracture. Initial treatment consisted of placing him in a removable thumb spica splint. He was then referred to a hand surgeon for additional evaluation and treatment. On presentation to the hand surgeon, he complained of mild-to-moderate intermittent pain. He denied any limitations in his activities of daily living. The patient was an elite tennis player and was eager to resume playing tennis as early as possible.
Physical Assessment
The physical examination was remarkable for mild ecchymosis and swelling over the dorsal radial left wrist and tenderness to palpation over the anatomic snuffbox. He also had diffuse ligamentous laxity, and both patellas were dislocatable .
Diagnostic Studies and Diagnosis
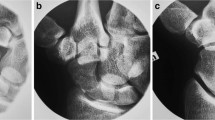
Left-wrist radiographs were significant for a nondisplaced scaphoid waist fracture and skeletal immaturity (Fig. 6.1) . The scaphoid was completely ossified.
Management Options
Most acute scaphoid fractures that are minimally displaced or nondisplaced can be successfully treated with cast immobilization in the pediatric population. This patient was adamant about returning to full activity as quickly as possible; his coach was concerned that even a short-arm thumb spica cast would interfere with his ability to serve a tennis ball. Treatment options were reviewed with the family, including casting versus percutaneous screw fixation. The family was informed of the potential risks of percutaneous screw fixation , including injury to branches of the superficial radial nerve, infection, scaphotrapezial and radiocarpal screw prominence, nonunion, malunion, and fracture displacement during percutaneous fixation requiring open reduction and fixation.
Management Chosen
The patient chose to pursue percutaneous fixation because it would allow him the best chance to resume tennis more quickly.
Surgical Technique
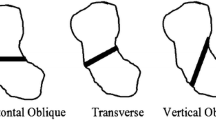
Volar percutaneous screw fixation was performed using a modified technique to optimize screw position [1] . Ten pounds of traction was placed on the thumb, thereby facilitating reduction and opening the scaphotrapezial joint. Using a mini fluoroscopy unit to visualize the distal pole of the scaphoid, freehand K-wires were used to draw intersecting lines on the skin overlying the scaphotrapezial joint. A small incision was then made at the base of the thenar eminence over the scaphotrapezial joint, and a 14-gauge angiocatheter needle was placed into the distal pole of the scaphoid, starting within the scaphotrapezial joint. The angiocatheter needle facilitates localizing the starting point, directs the guide wire toward the proximal pole, functions as a lever to translate the trapezium ulnarly, and serves as a soft tissue protector. Proper placement was confirmed using fluoroscopy, and the needle was then gently tapped into position using a mallet. The guide wire was advanced across the fracture so that the wire ended up in the center of the proximal pole . Finally, the bone tunnel was hand-drilled, and a Mini-Acutrak 2 (Hillsboro, OR) screw was placed, making sure that the screw was at least 4 mm shorter than the measured length. Traction was released after the screw crossed the fracture site to allow for compression. Successful compression of the fracture was achieved. Final fluoroscopic images were obtained before the guide wires were removed and after the traction was released (Fig. 6.2). A sterile dressing and short-arm thumb spica splint were then placed .
Clinical Course and Outcome
Two weeks after the surgery, the patient was fitted with an over-the-counter thumb spica splint and he began some gentle range of motion exercises. Seven weeks after the surgery, routine X-rays demonstrated fracture healing and he was released to full activities without restrictions. At final follow-up 3 months postoperative, he had full range of motion in his left wrist that was equal to the contralateral side, as well as grip strength that was equal to the right. He denied any deficits in his activities of daily living and was able to resume playing tennis at his previous level of competitiveness.
Clinical Pearls/Pitfalls
-
Failure to identify fracture on initial X-ray:
Standard X-rays in children with incomplete ossification can be difficult to interpret; Initial X-rays should include the standard posterioanterior, lateral, and scaphoid views, and obtaining similar images of the contralateral wrist is useful . Failure to visualize a fracture in the context of positive physical examination findings does not exclude a fracture. These children should be immobilized in a short-arm thumb spica cast for 1–2 weeks and then reimaged. If clinical suspicion for a fracture persists in light of normal X-rays, obtaining an MRI may be appropriate, given that occult fractures can take up to 7 weeks to be seen on plain films [2, 3]
-
Over-diagnosis of scapholunate dissociation:
It is possible to over-diagnose injuries in the immature skeleton; the scapholunate interval appears abnormally wide until the carpal bones fully ossify, and failure to recognize this can lead to incorrect diagnosis of scapholunate dissociation (“pseudo-Terry Thomas sign”) [4] .
-
Occult enchondroma:
Occasionally, a patient will present with wrist pain without a clear mechanism of injury or history of only minor trauma; standard workup for a scaphoid fracture is still indicated given case reports of scaphoid fractures as the initial presentation of occult scaphoid enchondromas [5] .
-
Combined distal radius and carpal bone fracture:
The clinician must remember that clinical presentation of a scaphoid fracture can be subtle. It is critical to evaluate the wrist in the presence of more proximal injuries, keeping in mind that while distal radius fractures are much more common than scaphoid fractures, there are case reports of combined injuries [6].
-
Bipartite scaphoid:
There is some controversy regarding the possibility of a bipartite scaphoid. Some authors attribute this to a failure of fusion of the distal and proximal poles and regard this as a normal variant, while others argue that it represents a nonunion from a previous injury [7]. If seen on X-ray, the clinician should obtain images of the contralateral wrist as this rare variant, if it truly exists, would often be bilateral .
Literature Review and Discussion
This case illustrates one option for treating nondisplaced or minimally displaced scaphoid waist fractures in the adolescent . Scaphoid fractures are relatively rare in young children, but their incidence increases as children approach and enter adolescence. Overall, they represent 3 % of fractures of the hand and wrist, but only 0.45 % of pediatric upper extremity fractures, and 0.39 % of all pediatric fractures [7]. The low incidence of scaphoid fractures in younger children may be attributable to the cartilage cushion that protects the ossific nucleus. The ossific nucleus appears midway through the first decade of life and takes about 9 years to completely ossify [8]. As this cartilage cushion is progressively replaced by bone, the incidence of scaphoid fractures increases. The scaphoid ossifies from distal to proximal, and fracture patterns follow this ossification process with distal pole fractures being the most common scaphoid fracture in children 13 years and younger. However, a recent study of scaphoid fractures in children and adolescents found an anatomic distribution of fracture patterns that more closely resembles to those found in adults, with 71 % of fractures in the waist, 23 % at the distal pole, and 6 % at the proximal pole. Causes implicated in these recent epidemiological changes include the higher incidence of fractures in males, high-energy mechanisms of injury, closed physes, and higher body mass index [9].
The vast majority of pediatric scaphoid fractures will heal with cast immobilization for 2–3 months. Union rates for nondisplaced scaphoid fractures that are identified in the acute period approach 90 % [9]. This includes scaphoid tubercle fractures, waist, and proximal pole fractures . Indications for surgical intervention include fractures displaced greater than 1 mm or angulated greater than 10°, as well as chronic scaphoid nonunions [10].
With the increased participation in competitive sports in adolescence, seemingly more and more adolescent athletes and their parents’ request return to full activity as soon as possible. In such cases, particularly when an early return to sports cannot be accommodated with a short-arm thumb spica cast, operative treatment may be offered and may minimize the time away from participation associated with the injury. However, surgical treatment does not necessarily guarantee a quicker return to full activity. For children with open physes, surgical fixation of acute fractures may not heal significantly faster than those treated with cast immobilization [9].
Since almost all acute nondisplaced scaphoid waist fractures will heal with cast immobilization, casting until radiological union is achieved is considered the standard of care for both the pediatric and adolescent patients. In addition, many scaphoid fractures in the immature skeleton will be distal pole fractures or monocortical fractures that are also suitable for casting [7]. The case described here presents a patient who is reaching skeletal maturity and who is an elite athlete. Absolute indications for operative treatment in the skeletally immature patient include acute displaced waist and proximal pole fractures that are not likely to heal with cast immobilization alone [9].
Union rates using the described technique equal or exceed those treated nonoperatively [1]. Morbidity of the operative procedure is low, but complications can include technical errors that lead to scaphotrapezial joint arthritis, radiocarpal joint arthritis, injury to the superficial radial nerve, injury to the volar branch of the radial artery, infection, need to convert a percutaneous approach to an open approach, or exacerbation of an unstable fracture leading to compromise of the vasculature of the proximal pole of the scaphoid.
In conclusion, scaphoid fractures represent only a small proportion of fractures in the pediatric population. Vigilance is required since the implications of missing such an injury could be devastating, and include wrist arthritis and collapse (Fig. 6.3). It behooves all physicians, including pediatricians, emergency room physicians, and hand surgeons to have a high index of suspicion for occult fractures. The standard of care includes short-term cast immobilization if initial X-rays are negative, with repeat imaging in 2 weeks. If X-rays continue to be negative and there is still clinical suspicion for a scaphoid fracture, MRI may be indicated to confirm or deny the presence of a fracture [10]. Most acute scaphoid fractures that are minimally displaced or nondisplaced can be successfully treated with cast immobilization, but patient-specific factors must be considered when discussing individual treatment options.
A 15-year-old girl with a nondisplaced scaphoid fracture that was missed both by the emergency department and their radiologist, as well as the initial treating orthopaedic surgeon. She was treated in a removable splint for 2 weeks with no further follow-up. She presented to the same orthopaedist 4 months later with continued pain and now evidence of delayed union and a cavitary defect in the scaphoid on anteroposterior (a) and lateral (b) radiographs. She was again treated expectantly and returned 4 months later with an established nonunion on the scaphoid view (c) and a humpback deformity with Dorsal Intercalary Segment Instability (DISI) carpal instability on sagittal MRI (d, e). (Published with kind permission of © Peter R. Letourneau and Dan A. Zlotolow, 2015. All rights reserved)
References
Zlotolow DA, Knutsen E, Yao J. Optimization of volar percutaneous screw fixation for scaphoid waist fractures using traction, positioning, imaging, and an angiocatheter guide. J Hand Surg. 2011;36(5):916–21.
Evenski AJ, Adamczyk MJ, Steiner RP, Morscher MA, Riley PM. Clinically suspected scaphoid fractures in children. J Pediatr Orthop. 2009;29(4):352–5.
Williams A, Lochner H. Pediatric hand and wrist injuries. Curr Rev Musculoskelet Med. 2013;6:18–25.
Light TR. Carpal injuries in children. Hand Clinics 2000;16(4):513–22.
Takka S, Poyraz A. Enchondroma of the scaphoid bone. Arch Ortho Trauma Surg. 2002;122:369–70.
Garcia-Mata S. Carpal scaphoid fracture nonunion in children. J Pediatr Orthop. 2002;22(4):448–51.
Christodoulou AG, Colton CL. Scaphoid fractures in children. J Pediatr Orthop. 1986;6(1):37–9.
Anz AW, Bushnell BD, Bynum, DK, Chloros GD, Wiesler ER. Pediatric scaphoid fractures. J Am Acad Orthop Surg. 2009;17(2):77–87.
Gholson JJ, Bae DS, Zurakowski D, Waters PM. Scaphoid fractures in children and adolescents: contemporary injury patterns and factors influencing time to union. J Bone Jt Surg (A). 2011;93(13):1210–9.
Huckstadt T, Klitscher D, Weltzien A, Müller LP, Rommens PM, Schier F. Pediatric fractures of the carpal scaphoid: a retrospective clinical and radiological study. J Pediatr Orthop. 2007;27(4):447–50.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Letourneau, P.R., Zlotolow, D.A. (2015). Treatment of Acute Pediatric Scaphoid Waist Fractures. In: Yao, J. (eds) Scaphoid Fractures and Nonunions. Springer, Cham. https://doi.org/10.1007/978-3-319-18977-2_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-18977-2_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-18976-5
Online ISBN: 978-3-319-18977-2
eBook Packages: MedicineMedicine (R0)