Abstract
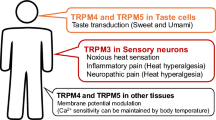
In the somatosensory system, cold thermoreceptor neurons and cold nociceptors are responsible for the detection of environmental low temperatures. The underlying machinery is far from simple; it is a result of the participation of several classes of transduction and voltage-gated ion channels that functionally coexist to give shape to the cold-induced receptor potential and subsequent action potential firing in response to cold stimulation. The cold-induced electrical responses begin in the free nerve endings of these sensory neurons, where a subgroup of thermosensitive Transient Receptor Potential channels (thermoTRPs) plays a critical role. These channels have evolved as molecular thermal sensors activated by a wide range of cold temperatures, and they have been proposed as key elements of the transduction machinery responsible for detection of environmental cold in primary somatosensory neurons. In this chapter, we summarize the most important functional properties of the primary sensory neurons involved in cutaneous cold detection, and the corresponding role of the thermoTRP channels TRPM8, TRPA1 and TRPC5 in cold transduction.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
9.1 Introduction
Primary sensory neurons of the peripheral somatosensory system are responsible for converting a wide range of environmental physical and chemical stimuli into electrical signals. Sensory signals begin at the nerve endings of these pseudounipolar neurons that innervate the skin and exposed mucosae, which home the molecular machinery necessary for the detection and transduction of these stimuli into a receptor potential (Fig. 9.1). The soma of primary somatosensory neurons is located in the dorsal root ganglia (DRG) and trigeminal ganglia (TG). These neurons project one axonal branch peripherally innervating the skin and mucosae, and the other branch centrally to dorsal horn neurons at the spinal cord and brain stem nuclei, where the information is transmitted towards the central integrative areas of the brain.
Sensory innervation of the skin. a. Simplified schematic representation of the different primary sensory neurons innervating the skin. b. In the dorsal root ganglion at right, the somas of the different subclasses of primary sensory neurons that project to dorsal horn are represented in different colors. The nerve ending of a cold thermoreceptor neuron (CTN) is shown in the left panel. The site of cold transduction (terminal) is depicted as separated from the site of action potential generation and propagation. In this scheme, TRPM8 is the most prominent channel, representing its contribution to cold sensing. Kv1.1-1.2 channels (the molecular counterpart of Ih break potassium current IKD), TREK-1/TRAAK and TASK-3 background potassium channels are also important components of the molecular machinery underlying cold temperature transduction. HCN1 and, to a lower extent, HCN2 channels (the molecular counterpart of Ih current) contribute to give shape to the net electrical response to temperature reductions in primary somatosensory neurons. The heat- and capsaicin-activated TRPV1 channel is also expressed in a large subpopulation of CTNs (~ 25 %); TRPA1 is only expressed in a small subpopulation of CTNs (~ 5 % of the TRPM8-expressing neurons). Although depicted, further studies are necessary to determine the role of TRPC5 in cold transduction. Among Nav channels, Nav1.8 channels are critical to allow impulse generation in primary sensory neurons at very low temperatures
TG and DRG comprise a variety of neurons responding to a wide range of mechanical stimuli, chemical agents of different nature, and temperature, and the activation of functional subpopulations of the primary sensory neurons evoke diverse sensations of touch , itch, irritation, cold, heat and pain . Thus, primary somatosensory receptors can be divided into cold and warm thermoreceptors, mechanoreceptors and nociceptors. Based on the intensity of the stimuli necessary to initiate a sensory signal, primary somatosensory neurons can be separated into low-threshold and high-threshold receptors. Under this general classification, low-threshold receptor neurons correspond to thermoreceptors (cold and warm) and low-threshold mechanoreceptors, whereas high-threshold receptors correspond to nociceptors, which include polymodal nociceptors and mechanonociceptors (Fig. 9.1a).
The wide diversity of cold sensations that arise from the exposure of the skin and mucosae to environmental temperature reductions varies from comfortable cold to intense pain, depending on the intensity of the thermal stimulus. The perception of cold as an innocuous temperature drop takes place when the surface of the skin is cooled by as little as 1 °C, or even less, and cold normally feels painful or noxious at temperatures below 15 °C. The detection of innocuous and noxious cold is mediated by cold thermoreceptors and nociceptors respectively, expressing a large variety of transduction and voltage-gated channels. These channels work concertedly in generating the cold-induced receptor potential and subsequent action potential firing in response to an environmental temperature decrease. In the last years, the identification of ion channels with a strong thermal sensitivity, including several cold- and heat-activated members of the superfamily of Transient Receptor Potential (TRP) (also called thermoTRP channels), has shed light on the molecular mechanisms underlying the diverse sensory modalities that emerge from the activation of distinct sets of peripheral receptors, including cold-sensitive neurons (Vriens et al. 2014).
9.2 Cold Thermoreceptor and Cold Nociceptor Neurons
In mammals, cold thermoreceptor neurons (CTNs) correspond to subpopulations of small diameter unmyelinated primary afferent C-fibers and medium diameter thinly myelinated Aδ-fibers, in a proportion that varies among different species and somatic territories (Hensel and Zotterman 1951b; Iriuchijima and Zotterman 1960; Hensel 1981; Heppelmann et al. 1990) . CTNs show a wide range of temperature thresholds, and can be separated into low-threshold and high-threshold cold-sensitive neurons, the latter having a role in the detection of cold discomfort under physiological conditions (Belmonte et al. 2009) . At a normal skin temperature of 33 °C, cold thermoreceptors detecting and encoding innocuous or moderate cold typically exhibit spontaneous electrical activity, mainly in a beating (regular) pattern of action potential firing. The firing of these exquisitely temperature-sensitive neurons increases in response to temperature reductions of less than 1 °C, and is reduced by heating. These cold afferents are sensitized by micromolar concentrations of the natural cold-mimetic compound menthol (Hensel and Zotterman 1951a; Brock et al. 2001) . Cold thermoreceptor neurons comprise about 8–15 % of the neuronal population in DRG and TG.
The functional properties of primary somatosensory neurons that respond to innocuous and moderate cold have been extensively characterized by Ca2+-imaging, patch-clamping and extracellular recordings in several somatic territories (Fig. 9.2). In culture, these neurons respond to cooling with a depolarizing inward current. The depolarization induces an increase in the action potential firing followed by a rise in intracellular Ca2+ concentration that depends on external Ca2+ . In CTNs, intracellular Ca2+ increases in response to cold stimulation are mainly due to the activation of voltage-gated Ca2 + channels during action potential firing. As a consequence, there is a tight correlation between temperature threshold for firing of action potentials and for [Ca2+] i elevations in each individual neuron (Viana et al. 2002; Madrid et al. 2006) (Fig. 9.3a). Canonical CTNs fire short duration action potentials (~ 1 ms at the half-amplitude of the depolarizing phase) (Fig. 9.3b) and are characterized by a low rheobase current and by the presence of a prominent hyperpolarization-activated current (Ih), mediated by HCN1 and, to a lower extent, HCN2 channels (Reid et al. 2002; Viana et al. 2002; Madrid et al. 2006, 2009, 2012; Orio et al. 2009) .
Calcium imaging and electrophysiological tools in the study of thermal responses in cold thermoreceptor neurons. a. Transmitted and pseudocolor ratiometric [Ca2+]i images cultured trigeminal neurons showing the effects of cold and menthol on its intracellular calcium concentration. Note that the same neurons are sensitive to both stimuli (Madrid and Viana, unpublished). Scale bar in left panel, 15 µm. b. Left, simultaneous recording of membrane current using patch clamp technique (top trace) and bath temperature (bottom trace) during a cooling ramp from 34 to 22 °C in a cold-sensitive trigeminal neuron (Vhold = − 60 mV). Right, simultaneous recording of membrane potential (top trace) and bath temperature during a cooling ramp in a cold-sensitive neuron recorded in current-clamp mode (Ihold = 0 pA) (González and Madrid, unpublished). c. Extracellular recording of nerve terminal impulses (NTI) activity in a corneal cold-sensitive neuron in response to cooling (González and Madrid, unpublished; Scheme at left modified from Parra et al. 2010)
The intracellular calcium increase in response to cold in cultured cold-sensitive neurons depends on the action potential firing. a. Left, simultaneous recording of [Ca2+]i signals (top trace), action currents (middle) and bath temperature (bottom) during a cooling ramp in a cold-sensitive neuron in culture, recorded in cell-attached condition. Right, scatter plot of thresholds for action potential firing and [Ca2+]i signals in response to cooling in 14 cold-sensitive neurons (each neuron has been color coded). The dotted line represents the unity line (González and Madrid, unpublished). b. Left, typical voltage responses (upper traces) to 500 ms hyperpolarizing and depolarizing current pulses (lower traces) of a trigeminal CTN. Note the fast repetitive discharge, the strong sag and the presence of rebound firing (in green). The first action potential of the train (orange arrow) is shown at right (González and Madrid, unpublished)
As mentioned before, the vast majority of cold thermoreceptor neurons are sensitive to menthol, a natural cyclic terpene alcohol that induces cold sensations (Hensel and Zotterman 1951a) . Menthol sensitivity in cold-sensitive fibers (and cold-sensitive cultured neurons) is manifested as an increase in the action potential firing frequency in response to this so-called cooling compound at 33 °C. Expressed differently, menthol shifts the temperature threshold of the cold-induced response to higher temperatures. This is not a trivial point, since high-threshold cold-sensitive neurons that do not respond to menthol at 33 °C could be erroneously classified as menthol-insensitive cells (Fig. 9.4).
Differential menthol sensitivity in low- and high-threshold cold thermoreceptor neurons. a. Simultaneous recordings of cold-induced [Ca2+]i and bath temperature in two cold-sensitive neurons with different temperature thresholds (low-threshold (LT-CS) and high-threshold (HT-CS)) during two consecutive cooling ramps, in control condition and in the presence of 100 μM menthol. Note that in the low-threshold CSN menthol evoked a robust [Ca2+]i rise at 34 °C, while in the HT-CS neurons menthol only shifted the threshold of cold induced response to higher temperatures. b. Dot plot summarizing the effect of 100 μM menthol on cold threshold in 86 trigeminal cold-sensitive neurons in culture. The neurons activated by 100 μM menthol at 34 °C are marked by a magenta star. The menthol-insensitive neurons are marked by a green triangle. (Modified from Madrid et al. 2009)
CTNs maintain an ongoing firing activity at normal skin temperature (33 °C), suggesting a tone of excitatory input of CTNs to the central cells where they synapse. This basal activity has been attributed to a temperature-dependent rhythmic oscillation of the membrane potential (Braun et al. 1980) (See also Chap. 10 by Orio and Olivares in this book). After the action potential firing frequency in response to a temperature drop reaches the peak (dynamic response), it slowly decreases to a lower sustained rate at the new temperature (static response) (Hensel and Iahn 1973) (see Fig. 10.3 in Chap. 10 of this book). The amplitude and rate of change of the cold-induced response is proportional to the rate and magnitude of the temperature decrease. The firing changes gradually from a beating to a bursting pattern at lower temperatures, and when the temperature is raised back, the electrical activity transiently silences with the rewarming process (Hensel and Iahn 1973; Darian-Smith et al. 1973) .
In contrast to cold thermoreceptor neurons, C- and Aδ-nociceptors responding to intense cold are silent at normal temperature of the skin, and fire only in response to temperatures below 15 °C. These neurons fire wide action potentials (> 2 ms at the half-amplitude) with an inflection (or hump) in the falling phase, and also respond to other modalities of noxious stimuli (Bessou and Perl 1969; Croze et al. 1976; LaMotte and Thalhammer 1982; Campero et al. 1996; Simone and Kajander 1996, 1997; Craig et al. 2001) . Interestingly, additional nociceptors are excited with larger temperature reductions. Moreover, almost all primary somatosensory neurons respond to cold temperatures below 0 °C, complicating the determination of the exact percentage of cold nociceptors in the peripheral somatosensory system (Simone and Kajander 1996, 1997; Campero et al. 2001) .
In primary somatosensory neurons, TTx-insensitive Nav1.8 sodium channels are critical for noxious cold response. Unlike the TTx-sensitive Na+ channels, whose slow inactivation is potentiated by cold, the inactivation of Nav1.8 is largely cold-insensitive. Thus, Nav1.8 channels allow the impulse generation of nociceptive neurons at very low temperatures (Zimmermann et al. 2007) . In addition, the increase in membrane resistance and the decrease in the activation threshold of the Na+ currents induced by cold augment the membrane potential change in response to a depolarizing stimulus.
9.3 TRPM8 Channels in Cold Transduction
9.3.1 Molecular Cloning of TRPM8 and Expression in Primary Sensory Neurons
TRPM8 is the 8th member of the Melastatin-related family of TRP channels . The encoding gene was originally identified by its expression in normal prostate epithelial cells and prostate carcinomas, and the full-length cDNA of human TRPM8 was formerly called trp-p8 (Tsavaler et al. 2001) . The transcript corresponds to a 1104 amino acid protein with a marked homology to some members of the TRP channels superfamily. The expression of this protein in primary somatosensory neurons was not reported until 2002, when TRPM8 was cloned by two groups independently, and characterized as a cold- and menthol-activated ion channel (McKemy et al. 2002; Peier et al. 2002) . In order to identify the putative cold and menthol receptor protein(s) responsible for cold and menthol sensitivity of CTNs, McKemy and coworkers constructed a cDNA expression library of trigeminal ganglia. They carried out a functional screening with this material, transfecting HEK293 cells with discrete cDNA pools obtained from this library. Using calcium imaging in isolated cells that exhibited intracellular calcium rises in response to menthol, they were able to identify a single cDNA sequence that conferred both menthol and cold sensitivity to these normally cold-insensitive cells, and classified it as a TRP channel (McKemy et al. 2002). Peier and colleagues, on the other hand, used a different strategy. Reasoning that the cold- and menthol-sensitive receptor could be a protein related to the recently cloned heat- and capsaicin-activated channel TRPV1 (Caterina et al. 1997) , they searched directly for TRP-like proteins in genomic DNA databases looking for putative exons with similarity to the S4 and S6 transmembrane domains of TRPV1. One of these sequences was used to design primers to amplify a fragment of a putative TRP channel from a DRG cDNA library, and by using a rapid amplification of cDNA ends-PCR (RACE-PCR) in combination with an exon-prediction software, they obtained the full length sequence of the protein (Peier et al. 2002) .
The TRPM8 channel is robustly expressed in trigeminal and dorsal root ganglia. TRPM8-positive neurons, corresponding to ~ 8–15 % of the neurons of these sensory ganglia, exhibit a relatively diverse neural and biochemical phenotype. These neurons show immunoreactivity to peripherin, a marker of C-fibers, and intermediate filament NF200, a marker of Aδ fibers. Furthermore, TRPM8 is co-expressed to a variable extent with nociceptive markers such as calcitonin gene-related peptide (CGRP), substance P, artemin receptor GFRα3 and the nociceptive channel TRPV1 (Viana et al. 2002; Babes et al. 2004; Okazawa et al. 2004; Xing et al. 2006; Takashima et al. 2007; Dhaka et al. 2008; Axelsson et al. 2009; Parra et al. 2010; Zimmermann et al. 2011; Lippoldt et al. 2013) . The NGF receptor TrkA is also expressed in a large subpopulation of TRPM8-positive neurons, and mediates the increase in cold-sensitivity of CTNs induced by this growth factor (Babes et al. 2004). A fraction of cold- and menthol-sensitive neurons also responds to proinflammatory mediators such as bradykinin, histamine and prostaglandin E2, with a reduction of its sensitivity to agonists (Linte et al. 2007; Zhang et al. 2012) . On the other hand, non-peptidergic primary sensory neurons that bind isolectin B4 do not show significant expression levels of TRPM8 (Takashima et al. 2007) .This neurochemical phenotype is in line with a sensory role of TRPM8 channels beyond innocuous cold thermosensation .
9.3.2 Functional Properties and Modulation of TRPM8 Channels
As mentioned before, TRPM8 is a nonselective cationic channel activated by cold, by natural and artificial cooling compounds such as menthol and icilin, and by voltage (for recent reviews, see (Babes et al. 2011; Latorre et al. 2011; McCoy et al. 2011; Yudin and Rohacs 2012; Almaraz et al. 2014; Madrid and Pertusa 2014) . Ion substitution experiments show a low discrimination of this channel among monovalent cations, but a significantly higher permeability for calcium ions (P Ca/P Na = 3.2; P K/P Na = 1.1; P Cs/P K = 1.2) (McKemy et al. 2002) . Both cold and menthol increase the open probability of the channel. Activation of TRPM8 by cooling-mimetic compounds such as menthol explains the refreshing sensation evoked by natural and artificial activators of this channel, widely used in many toiletries. Interestingly, higher concentrations of menthol can evoke sensations of irritation and burning pain, probably due to the activation of TRPA1 channels in nociceptors (Karashima et al. 2007) . TRPM8 shows a strong outward rectification at depolarized membrane potentials and an estimated single channel conductance of 60–90 pS depending on temperature. It is directly activated by cold, with a Q10 temperature coefficient as high as 25. Activation of the TRPM8 channel by low temperatures and by most of its natural and artificial agonists is related to a shift in its voltage-activation curve to more negative voltages. This shift results in an increase in the open probability of the channel at physiologically relevant membrane potentials in response to thermal and chemical stimulation (Brauchi et al. 2004; Voets et al. 2004, 2007b) .
TRPM8 is a homotetramer, where each subunit consists of six transmembrane domains with the N- and C- termini facing the cytosolic side of the plasma membrane (Fig. 9.5a). As in other members of the TRP channels family, the C-terminal domain of TRPM8 contains a TRP domain (Clapham 2003; Montell 2005) . This domain plays an important role in its modulation by phosphatidylinositol 4,5-bisphosphate (PI(4,5)P2) (Rohacs et al. 2005) (see below) . The coiled-coil motif located in the distal C-terminal domain plays an important role in the tetramerization and function of the channel (Erler et al. 2006; Tsuruda et al. 2006; Phelps and Gaudet 2007) . Several regions have recently been described in the N-terminal domain as relevant for both cold and menthol sensitivity and proper folding and assembly of the channel protein (Pedretti et al. 2009; Pertusa et al. 2014) . The pore module consists of the S5 and S6 domains and the interconnecting loop, where the selectivity filter is located. A unique N-glycosylation, at asparagine 934 facilitates the segregation of the channel to lipid rafts (Morenilla-Palao et al. 2009) . This N-glycosylation site is flanked by two cysteine residues that form a conserved double cysteine motif (C929 and C940), which is essential for channel function (Dragoni et al. 2006) . N-glycosylation of TRPM8 occurs in both native and recombinant channels, and it has a direct effect on their biophysical properties. The membrane potential for half-maximal activation (V1/2) of the channel carrying the single point mutation N934Q is 60 mV more positive than the wild type channel, shifting the mean temperature threshold of the cold response to lower temperatures (Pertusa et al. 2012) (see Chap. 3 by Pertusa and Madrid in this book) .
Schematic representation of a TRPM8, TRPA1 and TRPC5 channel subunit. Left, TRPM8. Middle, TRPA1. Right, TRPC5. Each subunit presents six transmembrane domains, and the N- and C-terminal tails are located in the intracellular side of the plasma membrane. The most conspicuous functional domains and residues are indicated. Temperature-activation ranges and typical chemical activators are also depicted
Mean cold thresholds over 30 °C can be found in corneal cold-sensitive nerve endings and cultured CTNs, as opposed to a mean value of 25 °C observed in transfected hippocampal neurons or HEK293 cells heterologously expressing TRPM8 (Reid et al. 2002; Viana et al. 2002; de la Peña et al. 2005; Madrid et al. 2006, 2009; Malkia et al. 2007) . At the same temperature, the V1/2 by equivalent cold stimulation is ~ 140 mV more negative in native TRPM8 than in recombinant channels. This results in a significantly lower thermal excitation threshold of CTNs compared to the heterologous expression systems such as HEK293 cells (Malkia et al. 2007) . Thus, the activation of TRPM8 at physiological membrane potentials results in larger inward currents in cold-sensitive neurons than in recombinant systems. Interestingly, it has been reported different temperature activation threshold and menthol sensitivity among TRPM8 orthologs, which is coincident with the mean body temperature in endothermic animals and tuned to the environmental temperature of its ecological niche in ectotherms (Myers et al. 2009) . Recently, Fujita and coworkers have also reported that warm ambient temperatures shift the cold threshold of TRPM8 to higher temperatures (Fujita et al. 2013) .
Charge-neutralizing mutations of positively charged residues in the S4 transmembrane segment and the S4-S5 linker of TRPM8 cause a decrease in its voltage dependence, suggesting that this region may be part of the voltage sensor (Voets et al. 2007a) . Nevertheless, despite the advances in the study of the voltage and temperature dependence of TRPM8, and in contrast to its activation by cooling compounds, both the precise location of the voltage sensor and the molecular determinants of the temperature sensitivity remain elusive.
Functional and biophysical properties of TRPM8 can be finely tuned by diverse mechanisms, including lipid-protein interactions, protein-protein interactions, activation of intracellular cascades of second messengers and post-translational modifications such as phosphorylation and N-glycosylation . These mechanisms can influence its contribution to cold sensing under physiological and physiopathological conditions (see (Almaraz et al. 2014; Madrid and Pertusa 2014) for recent reviews; see also Chap. 3 by Pertusa and Madrid in this Book). In fact, both cold and menthol responses of TRPM8 are reduced by its basal association with lipid rafts at the plasma membrane (Morenilla-Palao et al. 2009) . Although still unexplored, these results suggest that the association of TRPM8 with specific membrane microdomains may affect the targeting and trafficking dynamics of this channel in the nerve endings of cold-sensitive neurons. On the other hand, PI(4,5)P2 is a critical cofactor for TRPM8 activation, and the positions K995, R998 and R1008 within the TRP domain appear to mediate the interaction of this lipid with the channel (Rohacs et al. 2005) . PI(4,5)P2 is able to activate TRPM8 in the absence of other physical and chemical stimuli (Liu and Qin 2005; Rohacs et al. 2005) . Similarly to cold and cooling compounds, positive modulation of TRPM8 by PI(4,5)P2 seems to be related to a shift in the V1/2 value of voltage activation towards more negative membrane potentials (Daniels et al. 2009) .
Desensitization of TRPM8 to sustained cold and menthol stimulation strongly depends on extracellular Ca2 + (McKemy et al. 2002) . It has been suggested that this property is related to a depletion of PI(4,5)P2 of the plasma membrane. Calcium entry through TRPM8 activates Ca2+-dependent PLC, reducing the sensitivity of the channel to thermal and chemical stimulation by diminishing PI(4,5)P2 levels (Daniels et al. 2009) . Sarria and coworkers on the other hand have proposed that tachyphylaxis in response to repetitive stimulation of TRPM8 would be mediated by PLC-dependent hydrolysis of PI(4,5)P2 and the activation of a PKC/Protein Phosphatase 1 cascade, and that the desensitization by single sustained stimulation of the channel would depend on calmodulin activation and PI(4,5)P2 availability (Sarria et al. 2011) .
TRPM8 channel function can be also modulated by different protein kinases (see Chap. 3 by Pertusa and Madrid in this Book). These intracellular modulatory mechanisms could explain the desensitization of the channel induced by inflammatory mediators. Thus, it has been suggested that bradykinin reduces the cold and menthol responses of TRPM8 though the activation of Gq protein and PKC-dependent mechanisms, respectively (Premkumar et al. 2005; Linte et al. 2007) . Nevertheless, recently Zhang and coworkers proposed an alternative explanation, suggesting that the inhibition of TRPM8 activity is due to a direct interaction of the Gαq subunit with the channel, independent of the signaling pathway downstream of Gαq-coupled receptors (Zhang et al. 2012) .
9.3.3 TRPM8 as the Main Molecular Entity in Cold Transduction
In CTNs, the depolarizing inward cold-induced current (Icold) is the main responsible for the excitatory receptor potential in response to temperature reductions. Icold displays a biophysical and pharmacological profile consistent with a depolarizing current depending on the TRPM8 channel. This current exhibits outward rectification and can be fully suppressed by BCTC, a potent blocker of TRPM8 (Madrid et al. 2006) .
CTNs display a wide range of temperature thresholds. This differential thermal sensitivity is to a large extent determined by the functional counterbalance of two conductances with opposite effects on temperature-dependent excitability. Differential functional expression of TRPM8 (the main responsible for the excitatory cold-activated current) and Kv1.1-1.2 Shaker -like potassium channels (responsible for the excitability break current IKD) is intimately linked to the thermosensitive phenotype of individual CTNs. The fast-activating slow-inactivating outward IKD current dampens the effect of the cold-induced depolarizing TRPM8-dependent current, shifting the temperature threshold of the neuron to higher values, reducing the net response of the CTN to temperature reductions. Interestingly, pharmacological suppression of IKD induces cold-sensitivity in cold-insensitive neurons (Viana et al. 2002) . It is important to mention here that a fraction of cold-sensitive neurons does not express TRPM8, suggesting the presence of other mechanisms. Closure of thermosensitive background K + channels TREK-1 and TRAAK by temperature drops also contributes to increase the excitability of CTNs neurons under cold stimulation (Reid and Flonta 2001; Viana et al. 2002; Noel et al. 2009) . Recently, TASK-3 and Kv7.2-7.3 potassium channels have also been proposed as modulators of cold-sensitivity in TRPM8-expressing neurons (Vetter et al. 2013; Morenilla-Palao et al. 2014) .
The use of genetically modified mice has been critical to unveil the role of TRPM8 in sensing innocuous and noxious cold. Mice lacking functional expression of TRPM8 were developed by three groups independently (Bautista et al. 2007; Colburn et al. 2007; Dhaka et al. 2007) , and all three TRPM8 knockout strains presented a strongly impaired cold sensitivity. TRPM8 knockout mice failed to discriminate between cold and warm environments. These mice exhibited a clearly reduced avoidance to cold in two-temperature tests and in thermotaxis assays of temperature gradients, when compared to wild type animals (Bautista et al. 2007; Colburn et al. 2007; Dhaka et al. 2007) . Molecular ablation of the TRPM8 channel also reduced the behavioral responses to cooling agents and abolished their response to systemic stimulation with icilin, one of the strongest chemical agonists of TRPM8 (Dhaka et al. 2007). Using calcium imaging techniques in cultured primary sensory neurons, Bautista and coworkers additionally found that TRPM8 knockout animals showed a strong decrease in the incidence and magnitude of cold-induced responses (Bautista et al. 2007). Extracellular recordings of single sensory fibers revealed that both low- and high-threshold cold-sensitive primary afferents have impaired responses to temperature reductions. Cold-sensitive C-fibers from TRPM8 knockout mice also display lower basal action potential firing, but no effect on their general excitability (Bautista et al. 2007). Accordingly, basal firing of corneal CTNs and their responses to cold and menthol are virtually absent in TRPM8 knockout mice and proportionally reduced in heterozygous animals (Parra et al. 2010) . Thus, not only the static and dynamic responses to temperature drops, but also the ongoing spontaneous activity of CTNs is largely dependent of the functional expression level of the cold- and menthol-activated channel TRPM8.
More recently, Knowlton and coworkers demonstrated that selective ablation of TRPM8-expressing neurons yielded animals with an even higher cold insensitivity in both innocuous and noxious range than observed in TRPM8 knockout animals (Knowlton et al. 2013) . This result not only supports a critical role of TRPM8-expressing neurons in cold sensing, but also suggests the participation of other molecular mechanisms in cold-detection. Animals that lack TRPM8-expressing neurons have normal mechanical and heat sensitivity, suggesting that these neurons could be largely dispensable for other somatosensory modalities (Knowlton et al. 2013). Using a similar ablation strategy to eliminate TRPM8-expressing neurons but in adult mice, Pogorzala and coworkers demonstrated that this approach strongly reduced the responses of these animals to cold in a wide range of low temperatures (Pogorzala et al. 2013) .
Summarizing, molecular, cellular, biophysical and behavioral studies support a key role of TRPM8 in the molecular and neural machinery responsible for cold sensing in a wide range of low temperatures.
9.4 TRPA1 Channels in Cold Transduction
9.4.1 Molecular Cloning of TRPA1 and Expression in Primary Sensory Neurons
Transient Receptor Potential Ankiryn 1 channel (TRPA1) , first identified in human fibroblasts and liposarcoma cells (Jaquemar et al. 1999) , is the only member of the subfamily of TRPA channels found in mammals. A similar bioinformatic approach used in the molecular cloning of TRPM8 (Peier et al. 2002) was used by Patapoutian and his group to design primers for obtaining the full-length TRPA1 from mouse TG cDNA, encoding a 1115 amino acid protein (Story et al. 2003) . TRPA1 was originally described as an ion channel activated by intense cold (< 17 °C) (Story et al. 2003). TRPA1 works as a sensor of cell threat, responding to a plethora of structurally diverse pungent and noxious compounds, and nowadays it is seen as the main molecular entity in the somatosensory system responsible for the detection of irritant and potentially harmful substances. The TRPA1 channel also plays an important role as regulator of neuropeptide release and neurogenic inflammation, and is considered a promising molecular target for new analgesic and anti-inflammatory drugs (for reviews see (Bautista et al. 2006; Baraldi et al. 2010; Nilius et al. 2012; Zygmunt and Hogestatt 2014)) . Moreover, TRPA1 functions as a detector of potentially toxic compounds throughout the animal kingdom, implying that it emerged early in evolution (Kang et al. 2010; Macpherson and Patapoutian 2010) .
The proportion of sensory neurons expressing TRPA1 in sensory ganglia varies from one report to another, with observations ranging from 3.6 to 56.7 % (Story et al. 2003; Jordt et al. 2004; Kobayashi et al. 2005; Nagata et al. 2005) . TRPA1 can be found in both peptidergic (substance P- and CGRP-positive) and non-peptidergic (IB4-positive) primary sensory neurons (Hjerling-Leffler et al. 2007; Barabas et al. 2012) . The channel colocalizes with the heat-activated polymodal channel TRPV1 in a subpopulation of nociceptors, while its co-expression with TRPM8 channels in cold thermoreceptor neurons is very low, comprising about 5 % of TRPM8-expressing cells (Story et al. 2003; Jordt et al. 2004; Parra et al. 2010) .
The particularly high threshold for the activation of TRPA1 by cold temperatures, along with its expression in nociceptive neurons, makes it a strong candidate as the molecular entity responsible for transducing painful cold.
9.4.2 Functional Properties and Modulation of TRPA1 Channels
TRPA1 is most likely a homotetramer, with each subunit having a topology of six transmembrane segments (S1-S6), a putative pore loop and selectivity filter between S5 and S6, and large cytoplasmic N- and C- terminal domains (Fig. 9.5b). TRPA1 is highly permeable to Ca2+ , with a PCa/PNa of 5.8 and 17 % of the inward current carried by Ca2+ ions measured under physiological ionic conditions (Karashima et al. 2010) . TRPA1 is also activated by voltage, showing a shift in its voltage dependence in response to agonists toward more negative membrane potentials (Karashima et al. 2007; Zurborg et al. 2007) . In cell-attached patches, TRPA1 shows conductances of ~ 65 pS and ~ 110 pS in the inward and outward directions respectively under physiological conditions. In the absence of divalent cations, TRPA1 shows a linear I-V relationship with a slope conductance of ~ 120 pS (see (Nilius et al. 2011)) . In heterologously expressed TRPA1 channels, cold produces an exponential increase in the open probability, which is accompanied by an important decrease in single channel conductance and an increase in the mean open time (Sawada et al. 2007; Karashima et al. 2009) .
The molecular nature of TRPA1 agonists is remarkably diverse. The TRPA1 agonists include active ingredients in many natural compounds commonly used as spices in cooking: cinnamaldehyde present in cinnamon (Bandell et al. 2004) , isothiocyanates in mustard oil, wasabi, and horseradish (Bandell et al. 2004; Jordt et al. 2004), allicin and diallyldisulfide in garlic (Bautista et al. 2005; Macpherson et al. 2005) and methyl salicylate in winter green oil (Bandell et al. 2004) are some examples. Noxious compounds like acrolein (in smoke and tear gas) (Bautista et al. 2006), ∆9-tetrahydrocannabinol (in marijuana) (Jordt et al. 2004) , as well as irritant compounds generated endogenously during inflammatory, oxidative and nitrative stress responses, such as 4-hydroxynonenal, 15-deoxy-∆12,14-prostaglandin J2 and nitrooleic acid, have also been reported as activators of TRPA1 (Trevisani et al. 2007; Macpherson et al. 2007b; Taylor-Clark et al. 2008, 2009) , just to name a few. Many agonists of TRPA1 are electrophilic compounds that activate the channel through covalent modification of cysteine or lysine residues (Hinman et al. 2006; Macpherson et al. 2007a; Takahashi et al. 2008; Bang and Hwang 2009) . In contrast, non-electrophilic compounds that activate TRPA1 bind to the channel in a non-covalent manner (Karashima et al. 2007; Fajardo et al. 2008; Talavera et al. 2009; Nilius et al. 2012) .
Ca2 + ions modulate TRPA1 function. The N-terminal domain of this channel contains an EF-hand Ca2 + binding motif between Ankyrin Repeat Domain (ARD) 11 and 12, which has been related with Ca2 +-dependent modulation (Doerner et al. 2007; Zurborg et al. 2007) . Ca2+ ions in the micromolar range induce a concentration-dependent leftward shift in the V1/2 toward physiologically relevant membrane potentials, enhancing the channels’ chemical responses (Doerner et al. 2007; Zurborg et al. 2007) . However, later studies suggest that apparently EF-hand motif is not required for this phenomenon (Wang et al. 2008) .
Furthermore, it has been shown that activation and desensitization of TRPA1 channels in response to cold and chemical agonists are modulated by Ca2+ ions (Wang et al. 2008; Karashima et al. 2009) . Thus, when Ca2+ is present, the current elicited by addition of the potent TRPA1 agonist mustard-oil shows a rapid activation and further desensitization. In the absence of Ca2+, both processes are still present but with higher rise and decay time constants. An alternative Ca2+ binding site has been proposed within a cluster of acidic residues in the distal C-terminus of TRPA1, that has been found to be important for Ca2+-mediated modulation of the agonist-induced responses (Sura et al. 2012) .
9.4.3 TRPA1 as a Molecular Determinant in Noxious Cold Sensitivity
Cold-sensitivity of mammalian TRPA1 has been matter of intense debate. The seminal study of Story and co-workers described that mammalian cell lines and Xenopus oocytes expressing recombinant TRPA1 channels responded to intense cooling (Story et al. 2003) . However, these results were not corroborated by similar experiments carried out by Jordt and co-workers one year later (Jordt et al. 2004) . These authors studied thermal and chemical responses of cultured TG neurons, and they did not find a direct correlation between the cells responding to mustard oil and to noxious cold (Jordt et al. 2004). Later studies have argued either in favour (Bandell et al. 2004; Kwan et al. 2006; Sawada et al. 2007; Karashima et al. 2009) or against (Zurborg et al. 2007; Knowlton et al. 2010; Dunham et al. 2010) the cold sensitivity of TRPA1 and its contribution to cold sensing in vivo.
An alternative gating mechanism has been proposed, where the thermal sensitivity of TRPA1 would be an effect of cold-induced intracellular Ca2+-increases required for channel activation in HEK293 cells (Zurborg et al. 2007; Caspani and Heppenstall 2009) . Nevertheless, Karashima and co-workers found that heterologously expressed TRPA1 channels were able to respond to cold in a Ca2+-independent fashion (Karashima et al. 2009) . This cooling activation followed the same scheme of shifting V1/2 to more negative voltages, described as a general mechanism of thermal activation for other thermoTRP channels (Karashima et al. 2009) .
It has been recently reported that differences in cold-sensitivity of TRPA1 channels, which appears to be largely species-dependent since mouse and rat TRPA1 can be activated by cold in heterologous expression systems but not its orthologous of monkey and human, would be related to differences in a single residue within the S5 domain. Moreover, this residue (G878 in rodent and V875 in primate) also appears underlie the different effects of menthol on the channel observed across species (Chen et al. 2013) . Interestingly, Jabba and coworkers recently reported that three single point mutations (S250, M258 and D261) switch mouse TRPA1 channels from cold- to hot-sensitive without affecting its chemical sensitivity (Jabba et al. 2014) .
The contribution of TRPA1 to cold-sensing in vivo has been studied using genetically modified animals. Thermal sensitivity of two different lines of transgenic TRPA1 null mice has been evaluated. Bautista and coworkers developed a TRPA1-deficient mouse through deletion of the putative pore-loop domain of the channel (Bautista et al. 2006) . On the other hand, Kwan and coworkers, generated a TRPA1 null mouse deleting the exons downstream of the pore region, by insertion of an IRES cassette and polyadenylation sequences (Kwan et al. 2006) . Although disruption of the TRPA1 gene abolishes the behavioral responses to chemical activators of the channel, it has no mayor effects in the response or prevalence of cold-sensitive neurons (Bautista et al. 2006; Kwan et al. 2006) . Bautista and coworkers found that behavioral responses to noxious and innocuous cold stimuli between knockout and control mice were similar. In contrast, other studies using knockout mice show lower sensitivity to noxious and innocuous cold stimuli than wild type animals (Kwan et al. 2006; Gentry et al. 2010) . Using the TRPA1 knockout mice developed by David Corey and his group, Karashima and coworkers reported a decreased cold sensitivity of null mutant mice, supporting the idea that TRPA1 plays a role in noxious cold detection in vivo (Karashima et al. 2009) . A recent study on the TRPA1 knockout mice developed by Kwan and coworkers showed a considerable loss of nerve endings in the skin compared to wild type animals, which may account for the reduced responses to mechanical and cold stimuli of these mice in vivo (Andersson et al. 2013) .
On the other hand, it has also been suggested that TRPA1 is a mediator of hypersensitivity to cold under pathological conditions (del Camino et al. 2010; Chen et al. 2011) . It has also been reported that TRPA1 could play a role defining the thermal threshold in heat nociception (Hoffmann et al. 2013) . In cultured vagal sensory neurons, Fajardo and coworkers showed a clear overlap between cold sensitivity of these neurons and TRPA1 pharmacology, and a large reduction in the population of cold-sensitive neurons from nodose ganglia in TRPA1 knockout mice compared with wild-type animals (Fajardo et al. 2008) .
Thus, TRPA1 emerges as a critical component of the molecular machinery involved in the response to noxious agents in primary somatosensory neurons, with an important role in the release and detection of inflammatory mediators, and a species-dependent contribution to cutaneous thermal sensitivity under physiological conditions.
9.5 TRPC5 Channel in Cold Transduction
Transient Receptor Potential Canonical 5 (TRPC5) (Fig. 9.5c) is a Ca2+ -permeable nonselective cation channel predominantly expressed in central nervous system, but is also found in primary somatosensory neurons and other cells and tissues, including vascular smooth muscle cells, endothelial cells, T-lymphocytes, monocytes cardiac cells, adrenal medulla, mammary glands and yolk sac, among others (reviewed by (Jiang et al. 2011; Zholos 2014)) . This channel was cloned by Okada and colleagues in 1998 and formerly named TRP5 (Okada et al. 1998) . Its full length mRNA sequence was obtained from the screening of a Oligo(dT)-primed cDNA library constructed with poly(A) RNA from adult mouse brain. This channel shows a wide diversity of opening mechanisms and activators. TRPC5 is mainly activated through receptors coupled to Gq, PLC and/or Gi proteins, but can be directly activated by a large list of agonist of the most diverse nature. This channel may also open in a store-dependent manner that requires other partner proteins, including other TRP channels (see (Zholos 2014)) . It has been reported that TRPC5 also displays cold sensitivity in the mild to intense cold range (Zimmermann et al. 2011) . Heterologous expression of TRPC5 in HEK293 cells generates cold-sensitive cation currents at temperatures below 37 °C that can be potentiated by the PLC-Gq cascade activated by carbachol (Zimmermann et al. 2011) . In addition to its sensitivity to cold, the expression pattern of this thermoTRP channel in primary somatosensory neurons also pointed to a role in cold thermotransduction. Specifically, this channel is expressed in ~ 32 % of mouse DRG neurons of small and medium diameter, in the nerve endings, axons and soma of these neurons, and in the regions I/II/III of superficial laminae of the dorsal horn of the spinal cord (Zimmermann et al. 2011) .
A TRPC5 deficient mouse strain was developed by Riccio and co-workers in 2009, using a targeting construct that allows the deletion of the genomic region encoding amino acids 412–459 of the TRPC5 gene and the introduction of a frame shift and a stop codon (Riccio et al. 2009) . Calcium imaging experiments using cultured DRG neurons from TRPC5 knockout mice revealed a significant reduction in the percentage of cold-sensitive neurons, with a decrease in both the menthol-sensitive and the menthol-insensitive populations of cold-responding neurons (Zimmermann et al. 2011) . These results are in agreement with the reduction in the total population of TRPM8-possitive neurons detected by immunostaining. However, in several behavioral tests, TRPC5 knockout mice have no impairment in their responses to cold in a wide range of temperatures, suggesting that TRPC5 is not required for innocuous and noxious cold detection (Zimmermann et al. 2011) . The authors suggest that cold-sensitivity of TRPC5 could be involved in other adaptations, such as localized metabolic changes, vascular changes, retraction of neurites, or initiation of transcriptional programs, rather than cold thermotransduction.
9.6 Concluding Remarks
In summary, an increasing number of cellular, molecular, electrophysiological and behavioral studies support the idea that, among the thermoTRP channels activated by cold temperatures, TRPM8 is the main component of the molecular machinery responsible for cold sensitivity in primary somatosensory neurons. The uncontested involvement of TRPM8 in innocuous cold transduction is also being extended nowadays to noxious cold detection. TRPA1 appears to have a species-dependent contribution to cutaneous noxious-cold sensing under physiological conditions, and it is critical to the cold-sensitivity of visceral vagal afferents. On the other hand, further studies are necessary to determine if TRPC5 has a significant contribution to cold sensing. The molecular basis underlying cold-sensitivity of these thermoTRP channels is an exciting open question, and the whole picture of the role that these cold-activated thermoTRP channels play beyond thermosensation is still emerging.
References
Almaraz L, Manenschijn JA, de la Pena E, Viana F (2014) Trpm8. Handb Exp Pharmacol 222:547–579
Andersson DA, Gentry C, Light E, Vastani N, Vallortigara J, Bierhaus A, Fleming T, Bevan S (2013) Methylglyoxal evokes pain by stimulating TRPA1. PLoS One 8:e77986
Axelsson HE, Minde JK, Sonesson A, Toolanen G, Hogestatt ED, Zygmunt PM (2009) Transient receptor potential vanilloid 1, vanilloid 2 and melastatin 8 immunoreactive nerve fibers in human skin from individuals with and without Norrbottnian congenital insensitivity to pain. Neuroscience 162:1322–1332
Babes A, Zorzon D, Reid G (2004) Two populations of cold-sensitive neurons in rat dorsal root ganglia and their modulation by nerve growth factor. Eur J Neurosci 20:2276–2282
Babes A, Ciobanu AC, Neacsu C, Babes RM (2011) TRPM8, a sensor for mild cooling in mammalian sensory nerve endings. Curr Pharm Biotechnol 12:78–88
Bandell M, Story GM, Hwang SW, Viswanath V, Eid SR, Petrus MJ, Earley TJ, Patapoutian A (2004) Noxious cold ion channel TRPA1 is activated by pungent compounds and bradykinin. Neuron 41:849–857
Bang S, Hwang SW (2009) Polymodal ligand sensitivity of TRPA1 and its modes of interactions. J Gen Physiol 133:257–262
Barabas ME, Kossyreva EA, Stucky CL (2012) TRPA1 is functionally expressed primarily by IB4-binding, non-peptidergic mouse and rat sensory neurons. PLoS One 7:e47988
Baraldi PG, Preti D, Materazzi S, Geppetti P (2010) Transient receptor potential ankyrin 1 (TRPA1) channel as emerging target for novel analgesics and anti-inflammatory agents. J Med Chem 53:5085–5107
Bautista DM, Movahed P, Hinman A, Axelsson HE, Sterner O, Hogestatt ED, Julius D, Jordt SE, Zygmunt PM (2005) Pungent products from garlic activate the sensory ion channel TRPA1. Proc Natl Acad Sci U S A 102:12248–12252
Bautista DM, Jordt SE, Nikai T, Tsuruda PR, Read AJ, Poblete J, Yamoah EN, Basbaum AI, Julius D (2006) TRPA1 mediates the inflammatory actions of environmental irritants and proalgesic agents. Cell 124:1269–1282
Bautista DM, Siemens J, Glazer JM, Tsuruda PR, Basbaum AI, Stucky CL, Jordt SE, Julius D (2007) The menthol receptor TRPM8 is the principal detector of environmental cold. Nature 448:204–208
Belmonte C, Brock JA, Viana F (2009) Converting cold into pain. Exp Brain Res 196:13–30
Bessou P, Perl ER (1969) Response of cutaneous sensory units with unmyelinated fibers to noxious stimuli. J Neurophysiol 32:1025–1043
Brauchi S, Orio P, Latorre R (2004) Clues to understanding cold sensation: thermodynamics and electrophysiological analysis of the cold receptor TRPM8. Proc Natl Acad Sci U S A 101:15494–15499
Braun HA, Bade H, Hensel H (1980) Static and dynamic discharge patterns of bursting cold fibers related to hypothetical receptor mechanisms. Pflugers Arch 386:1–9
Brock JA, Pianova S, Belmonte C (2001) Differences between nerve terminal impulses of polymodal nociceptors and cold sensory receptors of the guinea-pig cornea. J Physiol 533:493–501
Campero M, Serra J, Ochoa JL (1996) C-polymodal nociceptors activated by noxious low temperature in human skin. J Physiol 497(Pt 2):565–572
Campero M, Serra J, Bostock H, Ochoa JL (2001) Slowly conducting afferents activated by innocuous low temperature in human skin. J Physiol 535:855–865
Caspani O, Heppenstall PA (2009) TRPA1 and cold transduction: an unresolved issue? J Gen Physiol 133:245–249
Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, Julius D (1997) The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 389:816–824
Chen J et al (2011) Selective blockade of TRPA1 channel attenuates pathological pain without altering noxious cold sensation or body temperature regulation. Pain 152:1165–1172
Chen J, Kang D, Xu J, Lake M, Hogan JO, Sun C, Walter K, Yao B, Kim D (2013) Species differences and molecular determinant of TRPA1 cold sensitivity. Nat Commun 4:2501
Clapham DE (2003) TRP channels as cellular sensors. Nature 426:517–524
Colburn RW, Lubin ML, Stone DJ, Jr, Wang Y, Lawrence D, D’Andrea MR, Brandt MR, Liu Y, Flores CM, Qin N (2007) Attenuated cold sensitivity in TRPM8 null mice. Neuron 54:379–386
Craig AD, Krout K, Andrew D (2001) Quantitative response characteristics of thermoreceptive and nociceptive lamina I spinothalamic neurons in the cat. J Neurophysiol 86:1459–1480
Croze S, Duclaux R, Kenshalo DR (1976) The thermal sensitivity of the polymodal nociceptors in the monkey. J Physiol 263:539–562
Daniels RL, Takashima Y, McKemy DD (2009) Activity of the neuronal cold sensor TRPM8 is regulated by phospholipase C via the phospholipid phosphoinositol 4,5-bisphosphate. J Biol Chem 284:1570–1582
Darian-Smith I, Johnson KO, Dykes R (1973) “Cold” fiber population innervating palmar and digital skin of the monkey: responses to cooling pulses. J Neurophysiol 36:325–346
de la Peña E, Malkia A, Cabedo H, Belmonte C, Viana F (2005) The contribution of TRPM8 channels to cold sensing in mammalian neurones. J Physiol 567:415–426
del Camino D, Murphy S, Heiry M, Barrett LB, Earley TJ, Cook CA, Petrus MJ, Zhao M, D’Amours M, Deering N, Brenner GJ, Costigan M, Hayward NJ, Chong JA, Fanger CM, Woolf CJ, Patapoutian A, Moran MM (2010) TRPA1 contributes to cold hypersensitivity. J Neurosci 30:15165–15174
Dhaka A, Murray AN, Mathur J, Earley TJ, Petrus MJ, Patapoutian A (2007) TRPM8 is required for cold sensation in mice. Neuron 54:371–378
Dhaka A, Earley TJ, Watson J, Patapoutian A (2008) Visualizing cold spots: TRPM8-expressing sensory neurons and their projections. J Neurosci 28:566–575
Doerner JF, Gisselmann G, Hatt H, Wetzel CH (2007) Transient receptor potential channel A1 is directly gated by calcium ions. J Biol Chem 282:13180–13189
Dragoni I, Guida E, McIntyre P (2006) The cold and menthol receptor TRPM8 contains a functionally important double cysteine motif. J Biol Chem 281:37353–37360
Dunham JP, Leith JL, Lumb BM, Donaldson LF (2010) Transient receptor potential channel A1 and noxious cold responses in rat cutaneous nociceptors. Neuroscience 165:1412–1419
Erler I, Al-Ansary DM, Wissenbach U, Wagner TF, Flockerzi V, Niemeyer BA (2006) Trafficking and assembly of the cold-sensitive TRPM8 channel. J Biol Chem 281:38396–38404
Fajardo O, Meseguer V, Belmonte C, Viana F (2008) TRPA1 channels mediate cold temperature sensing in mammalian vagal sensory neurons: pharmacological and genetic evidence. J Neurosci 28:7863–7875
Fujita F, Uchida K, Takaishi M, Sokabe T, Tominaga M (2013) Ambient temperature affects the temperature threshold for TRPM8 activation through interaction of phosphatidylinositol 4,5-bisphosphate. J Neurosci 33:6154–6159
Gentry C, Stoakley N, Andersson DA, Bevan S (2010) The roles of iPLA2, TRPM8 and TRPA1 in chemically induced cold hypersensitivity. Mol Pain 6:4
Hensel H (1981) Thermoreception and temperature regulation. Monogr Physiol Soc 38:1–321
Hensel H, Iahn M (1973) Cutaneous thermoreceptors. J Neurophysiol 14:377–385. (Handbook Sensory Physiology NY)
Hensel H, Zotterman Y (1951a) The effect of menthol on the thermoreceptors. Acta Physiol Scand 24:27–34
Hensel H, Zotterman Y (1951b) The response of the cold receptors to constant cooling. Acta Physiol Scand 22:96–105
Heppelmann B, Messlinger K, Neiss WF, Schmidt RF (1990) Ultrastructural three-dimensional reconstruction of group III and group IV sensory nerve endings (“free nerve endings”) in the knee joint capsule of the cat: evidence for multiple receptive sites. J Comp Neurol 292:103–116
Hinman A, Chuang HH, Bautista DM, Julius D (2006) TRP channel activation by reversible covalent modification. Proc Natl Acad Sci U S A 103:19564–19568
Hjerling-Leffler J, Alqatari M, Ernfors P, Koltzenburg M (2007) Emergence of functional sensory subtypes as defined by transient receptor potential channel expression. J Neurosci 27:2435–2443
Hoffmann T, Kistner K, Miermeister F, Winkelmann R, Wittmann J, Fischer MJ, Weidner C, Reeh PW (2013) TRPA1 and TRPV1 are differentially involved in heat nociception of mice. Eur J Pain 17:1472–1482
Iriuchijima J, Zotterman Y (1960) The specificity of afferent cutaneous C fibres in mammals. Acta Physiol Scand 49:267–278
Jabba S, Goyal R, Sosa-Pagan JO, Moldenhauer H, Wu J, Kalmeta B, Bandell M, Latorre R, Patapoutian A, Grandl J (2014) Directionality of temperature activation in mouse TRPA1 ion channel can be inverted by single-point mutations in ankyrin repeat six. Neuron 82:1017–1031
Jaquemar D, Schenker T, Trueb B (1999) An ankyrin-like protein with transmembrane domains is specifically lost after oncogenic transformation of human fibroblasts. J Biol Chem 274:7325–7333
Jiang LH, Gamper N, Beech DJ (2011) Properties and therapeutic potential of transient receptor potential channels with putative roles in adversity: focus on TRPC5, TRPM2 and TRPA1. Curr Drug Targets 12:724–736
Jordt SE, Bautista DM, Chuang HH, McKemy DD, Zygmunt PM, Hogestatt ED, Meng ID, Julius D (2004) Mustard oils and cannabinoids excite sensory nerve fibres through the TRP channel ANKTM1. Nature 427:260–265
Kang K, Pulver SR, Panzano VC, Chang EC, Griffith LC, Theobald DL, Garrity PA (2010) Analysis of Drosophila TRPA1 reveals an ancient origin for human chemical nociception. Nature 464:597–600
Karashima Y, Damann N, Prenen J, Talavera K, Segal A, Voets T, Nilius B (2007) Bimodal action of menthol on the transient receptor potential channel TRPA1. J Neurosci 27:9874–9884
Karashima Y, Talavera K, Everaerts W, Janssens A, Kwan KY, Vennekens R, Nilius B, Voets T (2009) TRPA1 acts as a cold sensor in vitro and in vivo. Proc Natl Acad Sci U S A 106:1273–1278
Karashima Y, Prenen J, Talavera K, Janssens A, Voets T, Nilius B (2010) Agonist-induced changes in Ca(2+ ) permeation through the nociceptor cation channel TRPA1. Biophys J 98:773–783
Knowlton WM, Bifolck-Fisher A, Bautista DM, McKemy DD (2010) TRPM8, but not TRPA1, is required for neural and behavioral responses to acute noxious cold temperatures and cold-mimetics in vivo. Pain 150:340–350
Knowlton WM, Palkar R, Lippoldt EK, McCoy DD, Baluch F, Chen J, McKemy DD (2013) A sensory-labeled line for cold: TRPM8-expressing sensory neurons define the cellular basis for cold, cold pain, and cooling-mediated analgesia. J Neurosci 33:2837–2848
Kobayashi K, Fukuoka T, Obata K, Yamanaka H, Dai Y, Tokunaga A, Noguchi K (2005) Distinct expression of TRPM8, TRPA1, and TRPV1 mRNAs in rat primary afferent neurons with adelta/c-fibers and colocalization with trk receptors. J Comp Neurol 493:596–606
Kwan KY, Allchorne AJ, Vollrath MA, Christensen AP, Zhang DS, Woolf CJ, Corey DP (2006) TRPA1 contributes to cold, mechanical, and chemical nociception but is not essential for hair-cell transduction. Neuron 50:277–289
LaMotte RH, Thalhammer JG (1982) Response properties of high-threshold cutaneous cold receptors in the primate. Brain Res 244:279–287
Latorre R, Brauchi S, Madrid R, Orio P (2011) A cool channel in cold transduction. Physiology (Bethesda) 26:273–285
Linte RM, Ciobanu C, Reid G, Babes A (2007) Desensitization of cold- and menthol-sensitive rat dorsal root ganglion neurones by inflammatory mediators. Exp Brain Res 178:89–98
Lippoldt EK, Elmes RR, McCoy DD, Knowlton WM, McKemy DD (2013) Artemin, a glial cell line-derived neurotrophic factor family member, induces TRPM8-dependent cold pain. J Neurosci 33:12543–12552
Liu B, Qin F (2005) Functional control of cold- and menthol-sensitive TRPM8 ion channels by phosphatidylinositol 4,5-bisphosphate. J Neurosci 25:1674–1681
Macpherson LJ, Patapoutian A (2010) Channels: flies feel your pain. Nat Chem Biol 6:252–253
Macpherson LJ, Geierstanger BH, Viswanath V, Bandell M, Eid SR, Hwang S, Patapoutian A (2005) The pungency of garlic: activation of TRPA1 and TRPV1 in response to allicin. Curr Biol 15:929–934
Macpherson LJ, Dubin AE, Evans MJ, Marr F, Schultz PG, Cravatt BF, Patapoutian A (2007a) Noxious compounds activate TRPA1 ion channels through covalent modification of cysteines. Nature 445:541–545
Macpherson LJ, Xiao B, Kwan KY, Petrus MJ, Dubin AE, Hwang S, Cravatt B, Corey DP, Patapoutian A (2007b) An ion channel essential for sensing chemical damage. J Neurosci 27:11412–11415
Madrid R, Pertusa M (2014) Intimacies and physiological role of the polymodal cold-sensitive ion channel TRPM8. Curr Top Membr 74:293–324
Madrid R, Donovan-Rodriguez T, Meseguer V, Acosta MC, Belmonte C, Viana F (2006) Contribution of TRPM8 channels to cold transduction in primary sensory neurons and peripheral nerve terminals. J Neurosci 26:12512–12525
Madrid R, de la Peña E, Donovan-Rodriguez T, Belmonte C, Viana F (2009) Variable threshold of trigeminal cold-thermosensitive neurons is determined by a balance between TRPM8 and Kv1 potassium channels. J Neurosci 29:3120–3131
Malkia A, Madrid R, Meseguer V, de la Peña E, Valero M, Belmonte C, Viana F (2007) Bidirectional shifts of TRPM8 channel gating by temperature and chemical agents modulate the cold sensitivity of mammalian thermoreceptors. J Physiol 581:155–174
McCoy DD, Knowlton WM, McKemy DD (2011) Scraping through the ice: uncovering the role of TRPM8 in cold transduction. Am J Physiol Regul Integr Comp Physiol 300:R1278–R1287
McKemy DD, Neuhausser WM, Julius D (2002) Identification of a cold receptor reveals a general role for TRP channels in thermosensation. Nature 416:52–58
Montell C (2005) The TRP superfamily of cation channels. Sci STKE 2005:re3
Morenilla-Palao C, Pertusa M, Meseguer V, Cabedo H, Viana F (2009) Lipid raft segregation modulates TRPM8 channel activity. J Biol Chem 284:9215–9224
Morenilla-Palao C, Luis E, Fernandez-Pena C, Quintero E, Weaver JL, Bayliss DA, Viana F (2014) Ion channel profile of TRPM8 cold receptors reveals a role of TASK-3 potassium channels in thermosensation. Cell Rep 8:1571–1582
Myers BR, Sigal YM, Julius D (2009) Evolution of thermal response properties in a cold-activated TRP channel. PLoS One 4:e5741
Nagata K, Duggan A, Kumar G, Garcia-Anoveros J (2005) Nociceptor and hair cell transducer properties of TRPA1, a channel for pain and hearing. J Neurosci 25:4052–4061
Nilius B, Prenen J, Owsianik G (2011) Irritating channels: the case of TRPA1. J Phys 589:1543–1549
Nilius B, Appendino G, Owsianik G (2012) The transient receptor potential channel TRPA1: from gene to pathophysiology. Pflugers Arch 464:425–458
Noel J, Zimmermann K, Busserolles J, Deval E, Alloui A, Diochot S, Guy N, Borsotto M, Reeh P, Eschalier A, Lazdunski M (2009) The mechano-activated K + channels TRAAK and TREK-1 control both warm and cold perception. EMBO J 28:1308–1318
Okada T, Shimizu S, Wakamori M, Maeda A, Kurosaki T, Takada N, Imoto K, Mori Y (1998) Molecular cloning and functional characterization of a novel receptor-activated TRP Ca2+ channel from mouse brain. J Biol Chem 273:10279–10287
Okazawa M, Inoue W, Hori A, Hosokawa H, Matsumura K, Kobayashi S (2004) Noxious heat receptors present in cold-sensory cells in rats. Neurosci Lett 359:33–36
Orio P, Madrid R, de la Peña E, Parra A, Meseguer V, Bayliss DA, Belmonte C, Viana F (2009) Characteristics and physiological role of hyperpolarization activated currents in mouse cold thermoreceptors. J Physiol 587:1961–1976
Orio P, Parra A, Madrid R, Gonzalez O, Belmonte C, Viana F (2012) Role of Ih in the firing pattern of mammalian cold thermoreceptor endings. J Neurophysiol 108:3009–3023
Parra A, Madrid R, Echevarria D, Del OS, Morenilla-Palao C, Acosta MC, Gallar J, Dhaka A, Viana F, Belmonte C (2010) Ocular surface wetness is regulated by TRPM8-dependent cold thermoreceptors of the cornea. Nat Med 16:1396–1399
Pedretti A, Marconi C, Bettinelli I, Vistoli G (2009) Comparative modeling of the quaternary structure for the human TRPM8 channel and analysis of its binding features. Biochim Biophys Acta 1788:973–982
Peier AM, Moqrich A, Hergarden AC, Reeve AJ, Andersson DA, Story GM, Earley TJ, Dragoni I, McIntyre P, Bevan S, Patapoutian A (2002) A TRP channel that senses cold stimuli and menthol. Cell 108:705–715
Pertusa M, Madrid R, Morenilla-Palao C, Belmonte C, Viana F (2012) N-Glycosylation of TRPM8 Ion Channels Modulates Temperature Sensitivity of Cold Thermoreceptor Neurons. J Biol Chem 287:18218–18229
Pertusa M, González A, Hardy P, Madrid R, Viana F (2014) Bidirectional modulation of thermal and chemical sensitivity of TRPM8 channels by the initial region of the N-terminal domain. J Biol Chem 289:21828–21843
Phelps CB, Gaudet R (2007) The role of the N terminus and transmembrane domain of TRPM8 in channel localization and tetramerization. J Biol Chem 282:36474–36480
Pogorzala LA, Mishra SK, Hoon MA (2013) The cellular code for mammalian thermosensation. J Neurosci 33:5533–5541
Premkumar LS, Raisinghani M, Pingle SC, Long C, Pimentel F (2005) Downregulation of transient receptor potential melastatin 8 by protein kinase C-mediated dephosphorylation. J Neurosci 25:11322–11329
Reid G, Flonta ML (2001) Physiology. Cold current in thermoreceptive neurons. Nature 413:480
Reid G, Babes A, Pluteanu F (2002) A cold- and menthol-activated current in rat dorsal root ganglion neurones: properties and role in cold transduction. J Physiol 545:595–614
Riccio A, Li Y, Moon J, Kim KS, Smith KS, Rudolph U, Gapon S, Yao GL, Tsvetkov E, Rodig SJ, Van’t Veer A, Meloni EG, Carlezon WA, Jr, Bolshakov VY, Clapham DE (2009) Essential role for TRPC5 in amygdala function and fear-related behavior. Cell 137:761–772
Rohacs T, Lopes CM, Michailidis I, Logothetis DE (2005) PI(4,5)P2 regulates the activation and desensitization of TRPM8 channels through the TRP domain. Nat Neurosci 8:626–634
Sarria I, Ling J, Zhu MX, Gu JG (2011) TRPM8 acute desensitization is mediated by calmodulin and requires PIP(2): distinction from tachyphylaxis. J Neurophysiol 106:3056–3066
Sawada Y, Hosokawa H, Hori A, Matsumura K, Kobayashi S (2007) Cold sensitivity of recombinant TRPA1 channels. Brain Res 1160:39–46
Simone DA, Kajander KC (1996) Excitation of rat cutaneous nociceptors by noxious cold. Neurosci Lett 213:53–56
Simone DA, Kajander KC (1997) Responses of cutaneous A-fiber nociceptors to noxious cold. J Neurophysiol 77:2049–2060
Story GM, Peier AM, Reeve AJ, Eid SR, Mosbacher J, Hricik TR, Earley TJ, Hergarden AC, Andersson DA, Hwang SW, McIntyre P, Jegla T, Bevan S, Patapoutian A (2003) ANKTM1, a TRP-like channel expressed in nociceptive neurons, is activated by cold temperatures. Cell 112:819–829
Sura L, Zima V, Marsakova L, Hynkova A, Barvik I, Vlachova V (2012) C-terminal acidic cluster is involved in Ca2+ -induced regulation of human transient receptor potential ankyrin 1 channel. J Biol Chem 287:18067–18077
Takahashi N, Mizuno Y, Kozai D, Yamamoto S, Kiyonaka S, Shibata T, Uchida K, Mori Y (2008) Molecular characterization of TRPA1 channel activation by cysteine-reactive inflammatory mediators. Channels (Austin) 2:287–298
Takashima Y, Daniels RL, Knowlton W, Teng J, Liman ER, McKemy DD (2007) Diversity in the neural circuitry of cold sensing revealed by genetic axonal labeling of transient receptor potential melastatin 8 neurons. J Neurosci 27:14147–14157
Talavera K, Gees M, Karashima Y, Meseguer VM, Vanoirbeek JA, Damann N, Everaerts W, Benoit M, Janssens A, Vennekens R, Viana F, Nemery B, Nilius B, Voets T (2009) Nicotine activates the chemosensory cation channel TRPA1. Nat Neurosci 12:1293–1299
Taylor-Clark TE, Undem BJ, Macglashan DW, Jr, Ghatta S, Carr MJ, McAlexander MA (2008) Prostaglandin-induced activation of nociceptive neurons via direct interaction with transient receptor potential A1 (TRPA1). Mol Pharmacol 73:274–281
Taylor-Clark TE, Ghatta S, Bettner W, Undem BJ (2009) Nitrooleic acid, an endogenous product of nitrative stress, activates nociceptive sensory nerves via the direct activation of TRPA1. Mol Pharmacol 75:820–829
Trevisani M, Siemens J, Materazzi S, Bautista DM, Nassini R, Campi B, Imamachi N, Andre E, Patacchini R, Cottrell GS, Gatti R, Basbaum AI, Bunnett NW, Julius D, Geppetti P (2007) 4-Hydroxynonenal, an endogenous aldehyde, causes pain and neurogenic inflammation through activation of the irritant receptor TRPA1. Proc Natl Acad Sci U S A 104:13519–13524
Tsavaler L, Shapero MH, Morkowski S, Laus R (2001) Trp-p8, a novel prostate-specific gene, is up-regulated in prostate cancer and other malignancies and shares high homology with transient receptor potential calcium channel proteins. Cancer Res 61:3760–3769
Tsuruda PR, Julius D, Minor DL, Jr (2006) Coiled coils direct assembly of a cold-activated TRP channel. Neuron 51:201–212
Vetter I, Hein A, Sattler S, Hessler S, Touska F, Bressan E, Parra A, Hager U, Leffler A, Boukalova S, Nissen M, Lewis RJ, Belmonte C, Alzheimer C, Huth T, Vlachova V, Reeh PW, Zimmermann K (2013) Amplified cold transduction in native nociceptors by M-channel inhibition. J Neurosci 33:16627–16641
Viana F, de la Peña E, Belmonte C (2002) Specificity of cold thermotransduction is determined by differential ionic channel expression. Nat Neurosci 5:254–260
Voets T, Droogmans G, Wissenbach U, Janssens A, Flockerzi V, Nilius B (2004) The principle of temperature-dependent gating in cold- and heat-sensitive TRP channels. Nature 430:748–754
Voets T, Owsianik G, Janssens A, Talavera K, Nilius B (2007a) TRPM8 voltage sensor mutants reveal a mechanism for integrating thermal and chemical stimuli. Nat Chem Biol 3:174–182
Voets T, Owsianik G, Nilius B (2007b) TRPM8. Handb Exp Pharmacol 179:329–344
Vriens J, Nilius B, Voets T (2014) Peripheral thermosensation in mammals. Nat Rev Neurosci 15:573–589.
Wang YY, Chang RB, Waters HN, McKemy DD, Liman ER (2008) The nociceptor ion channel TRPA1 is potentiated and inactivated by permeating calcium ions. J Biol Chem 283:32691–32703
Xing H, Ling J, Chen M, Gu JG (2006) Chemical and cold sensitivity of two distinct populations of TRPM8-expressing somatosensory neurons. J Neurophysiol 95:1221–1230
Yudin Y, Rohacs T (2012) Regulation of TRPM8 channel activity. Mol Cell Endocrinol 353:68–74
Zhang X, Mak S, Li L, Parra A, Denlinger B, Belmonte C, McNaughton PA (2012) Direct inhibition of the cold-activated TRPM8 ion channel by Galphaq. Nat Cell Biol 14:851–858
Zholos AV (2014) TRPC5. Handb Exp Pharmacol 222:129–156
Zimmermann K, Leffler A, Babes A, Cendan CM, Carr RW, Kobayashi J, Nau C, Wood JN, Reeh PW (2007) Sensory neuron sodium channel Nav1.8 is essential for pain at low temperatures. Nature 447:855–858
Zimmermann K, Lennerz JK, Hein A, Link AS, Kaczmarek JS, Delling M, Uysal S, Pfeifer JD, Riccio A, Clapham DE (2011) Transient receptor potential cation channel, subfamily C, member 5 (TRPC5) is a cold-transducer in the peripheral nervous system. Proc Natl Acad Sci U S A 108:18114–18119
Zurborg S, Yurgionas B, Jira JA, Caspani O, Heppenstall PA (2007) Direct activation of the ion channel TRPA1 by Ca2+. Nat Neurosci 10:277–279
Zygmunt PM, Hogestatt ED (2014) TRPA1. Handb Exp Pharmacol 222:583–630
Acknowledgements
Supported by Grants CONICYT Anillo ACT-1113 (RM, MP, GU), FONDECYT 1131064 (RM), FONDECYT 11130144 (MP) and FONDECYT 3150431 (AG). We thank Dr. Carlos Belmonte and Dr. Annika Mälkiä for comments to the manuscript. We apologise for omission of relevant work due to space constraints. RP hold a PhD fellowship from CONICYT. We thank the support of VRIDEI-USACH.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
González, A., Ugarte, G., Piña, R., Pertusa, M., Madrid, R. (2015). TRP Channels in Cold Transduction. In: Madrid, R., Bacigalupo, J. (eds) TRP Channels in Sensory Transduction. Springer, Cham. https://doi.org/10.1007/978-3-319-18705-1_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-18705-1_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-18704-4
Online ISBN: 978-3-319-18705-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)