Abstract
The rising demand for medical implants for ageing populations and ongoing advancements in medical technology continue to drive the use of implantable devices. Higher implant usage has a consequent increased incidence of implant-related infections, and associated prolonged patient care, pain and loss of limb and other organ function. Numerous antibacterial surfaces have been designed that prevent the onset of biofilm formation, thus reducing or preventing implant-associated infections through inhibiting bacterial adhesion or by killing the organisms that successfully attach to the surface of the implant. Other surfaces have been designed to stimulate a local immune response, promoting the natural clearing of the invading pathogen. The desired antibacterial effects are typically achieved by modulating the surface chemistry and morphology of the implant material, by means of the controlled release of pharmacological agents and bioactive compounds from the surface of the material, or by a combination of both processes. An important issue for any type of antibacterial surface modification lies in balancing the non-fouling, bacteriostatic or bactericidal effects against local and systemic biocompatibility. In this chapter, we will first describe the concept of biocompatibility and its evolution, from devices that do not evoke a negative host response to those that actively drive host regeneration. We will then review the challenges associated with merging the need for an implant material to withstand a bacterial load with those associated with supporting function restoration and tissue healing.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Bacteriostatic
- Bactericidal
- Systemic biocompatibility
- Cytotoxicity
- Inflammation
- Host regeneration
- Tissue healing
7.1 Introduction
Any surgical intervention carries a risk of infectio n. Whenever the skin, a natural barrier to infection, is perforated or incised, a significant opportunity is created for infective agents to enter the body. The likelihood of developing an infection is dependent on a multitude of procedure- and patient-related factors (Phillips et al. 2014). These include the type, invasiveness, duration and complexity of the surgery (Olsen et al. 2008; Neumayer et al. 2007). Minimally invasive surgery techniques have been found to notably reduce post-operative wound infections by as much as tenfold in the case of minimally invasive versus open spinal surgery (O’Toole et al. 2009).
The skill of the operating team, the cleanness of the surgical environment and the use of pre- and post-surgery antibiotics have also shown to vastly reduce, if not fully eliminate the patient’s risk of being infected (Ridgeway et al. 2005; Sharaf et al. 2011). Indeed, it is very difficult to create a perfectly bacteria-free operating theatre and thus avoid at least low-cell-load bacterial contamination of the wound space. Whilst strategies can be used to lower the incidence of surgical wound infections that may occur though one process, this same strategy may inadvertently increase the risk of infection through another pathway. For example, intraoperative warming has been shown to reduce postoperative infections in patients undergoing major orthopedic, general, or urologic surgery by maintaining a cutaneous blood flow, increasing tissue viability and reducing the incidence of pressure sores. When intraoperative warming has been performed using forced-air devices, however, the moving air may act as a vector for the transfer of infectious agents, causing unwanted airflow disturbances (Weissman and Murray 2013; Augustine 2014).
Interestingly, in a large proportion of surgical site infections, the pathogens responsible are not exogenous, but emerge from the normal endogenous flora of the patient. Staphylococcus aureus, coagulase-negative staphylococci, Pseudomonas aeruginosa, Enterococcus spp. and Escherichia coli are among most commonly implicated pathogens (Owens and Stoessel 2008). The act of surgery facilitates the transport of these microorganisms from their habitat, e.g. skin or gastrointestinal tract, to the sterile sites of the body, such as spinal cord or muscle tissue (Thakkar et al. 2014). An infection elsewhere in the body, whether being a pre-existing condition or having been acquired post-surgery, can also serve as an internal source of infection (Claridge et al. 2014).
An individual’s risk of developing an infection depends greatly on the patient’s state of health, and particularly their ability to resist infection. Immunocompromised patients, such as the elderly, pregnant women, those suffering from chronic illnesses, those undergoing cancer treatment, recovering from a recent illness or invasive intervention, or having certain genetic disorders, may succumb to significantly lower bacterial loads or develop infections caused by opportunistic bacteria (Neumayer et al. 2007; Ridgeway et al. 2005). For example, patients suffering from hypoalbuminemia prior to gastrointestinal surgery are more likely to develop deeper surgical site infections and recover more slowly compared to patients whose pre-operative albumin levels were higher (Hennessey et al. 2010). According to a review study published by Pittet et al., patients being treated for breast cancer and undergoing a mastectomy experienced an increased risk of surgical site infection from an average rate of 2.5 % up to 53 %. This increase can be attributed to postoperative tissue ischemia and delayed wound healing (Pittet et al. 2005).
7.1.1 Biomaterial-Associated Infections and Inflammation
The introduction of an implant into the body further predisposes the host to infection and inflammation. For one, tissue that has already been injured by the surgical intervention is subjected to further physical damage from implant insertion and positioning. Subsequent to the insertion, the implant may continue to inflict physical damage to the adjacent tissues, putting excessive pressure on the surrounding tissues, rubbing against the tissues or by breaching epithelial or mucosal barriers. This breach may provide a means for bacteria to enter host tissues, whereas the subsequent physical trauma may impair the ability of the tissue to recover and to resist bacterial invasion (Chandorkar et al. 2015).
A persistent sterile inflammatory response, in itself, presents a significant issue for all medical implants, irrespective of their type and method of implantation. For example, a chronic foreign body response to devices implanted into brain tissue a ffects the electrophysiological and neurobiological activity of nearby neurons and the neural circuitry by a variety of neuro-inflammatory mechanisms, including disruption of the blood brain barrier, demyelination and reduction in density of local nerve fibers and neuronal cell bodies, and changes in the local ionic milieu (Skousen et al. 2015). Continuing physical damage and chronic infection can lead to tissue necrosis and permanent changes in the tissue surrounding the implant.
The surface of the implant may serve as a vector for the introduction of the microorganisms into the body. Although in developed countries, this issue is rarely observed due to highly controlled sterilization practices, the sterilization compliance remains an issue in countries with limited-resources (Rosenthal 2008). It is important to note that implant sterilization does not automatically render it free from agents that can induce a pro-inflammatory response, namely the endotoxins and micro- and nano-sized particles. Endotoxins are the lipopolysaccharides in the cell membrane of Gram-negative bacteria (Vetten et al. 2014). Residual endotoxin contaminations can vary significantly, depending on the method used for sterilizing the biomaterial.
For example, microelectrodes sterilized by autoclave, dry heat, or ethylene oxide gas, retained residual endotoxins of 0.55 EU per mL, 0.22 EU per mL, and 0.11 EU per mL, respectively (Ravikumar et al. 2014). At early stages of implantation into neural tissue, the extent of microglia/macrophage activation is directly related to the level of endotoxins present on the implant surface , whereas the degree of astrogliosis, neuronal loss, and blood-brain barrier dysfunction exhibit a threshold-dependent response. The effect of endotoxin levels diminishes with longer implantation periods, suggesting that the endotoxin contributes to the initial, but not chronic neuro-inflammation.
Just as initially sterile implant surfaces can induce a foreign body response, the abiotic surface of the implant provides excellent grounds fo r secondary colonization of the implant surface via the hematogenous dissemination from a remote focus of the infection. Indeed, conventional (non-antibacterial) biomaterials are not able to prevent bacteria from permanently attaching to their surfaces and forming a biofilm , nor activating a host immune response. Once colonized, the im plant surface can not only lead to peri-implant infection but also serve as a reservoir from which bacteria can spread to other parts of the body (Claridge et al. 2014).
Implant-associated infections are difficult to treat with antibiotics alone and often necessitate the removal of the implant. The protective nature of a biofilm significantly reduces the efficacy of both pharmacological therapies and host defense mechanisms (Lisanti et al. 2015; Khan et al. 2014). In addition, as most biomaterials do not react to being colonized, the infection is often detected only after the biofilm has been formed and the pathogen activity begins to impact on the surrounding tissues. Although some progress has been made in the development of strategies for dissolution of biofilms that have already been established, targeting of the bio film matrix for degradation, interference with the biofilm regulation (Hogan et al. 2015) and removal of biofilm-residing bacteria remains a challenge.
7.1.2 Resistance and Persistence of Pathogenic Bacteria
When resident in a biofilm, certain species of bacteria, such as staphylococci, exhibit increased mutation ability and enhanced ability to acquire/disseminate plasmid-borne antibiotic resistance determinants by horizontal gene transfer (Savage et al. 2013; Ryder et al. 2012). Compared to planktonic cultures, the mutation ability of S. aureus and S. epidermidis biofilm cultures increased up to 60-fold and 4-fold, respectively. Such enhanced spontaneous mutation accelerates the emergence of heritable antibiotic resistance and horizontal gene transfer ensures that this resistance spreads throughout the biofilm community. Mixed-species biofilms can also be more resilient to the action of antibiotics due to phenomenon known as indirect pathogenicity, where an antibiotic-resistant microorganism of low intrinsic virulence shields an antibiotic-sensitive pathogen from eradication (O’Connell et al. 2006). For example, antibiotics such as penicillins and cephalosporins can be inactivated via hydrolysis of the cyclic amide bond by beta-lactamase-producing bacteria, thereby preventing these antimicrobials from acting upon susceptible microorganisms. With an increasing prevalence of multidrug resistant bacteria, identifying antibiotic agents that would be able to overcome multidrug resistance in biofilm-dwelling bacteria is very challenging.
In addition to enzymes, antibiotic-sensitive strains can also benefit from the action of multifunctional extracellular polymers produced by other bacteria within the community. For example, P. aeruginosa produces Psl polysaccharide, which acts as molecular glue to enable bacterial attachment, self-organization of the attached cells into micro-colonies, and commu nal biofilm organization (Zhao et al. 2013a). As such, Psl provides a generic first line of defense against antibiotics with diverse biochemical properties during the initial stages of biofilm development. In mixed-species biofilms, Psl mediated matrix protection is extended to non-Psl-producing antibiotic-sensitive E. coli and S. aureus cells (Billings et al. 2013). Reducing surface adhesion and the production of bacterial adhesins are often a strategy of choice to prevent biofilm formation and implant-related infections.
Even in a population of genetically identical antibiotic-sensitive bacterial cells, not all cells will die as a result of an antibiotic treatment, even at a sufficiently high antimicrobial dose; the killing efficacy of penicillin depends on the physiological state of the cell, with rapidly growing bacteria being killed most efficiently, followed by slowly growing cells, whereas dormant (non-growing) bacteria are generally not affected by the drug (Tuomanen et al. 1986; Gerdes and Maisonneuve 2012). Even in an actively growing population, however, not all cells will succumb to penicillin treatment. While most of the population will be killed, a fraction of this genetically homogeneous microbial population may persist. In contrast to resistant mutants, persistent microorganisms do not acquire resistance to the said antibiotic (Balaban et al. 2004), which confirms that persistence is a phenotypic and not genotypic effect.
Persistence stems from inherent phenotypic heterogeneity within a microbial population, where distinct subpopulations with different growth rates co-exist: normal cells and persister (slow-growing) cells. Normal cells ensure population survival under normal conditions, whereas persisters provide fitness benefit under stressed conditions, e.g. antibiotic load (Patra and Klumpp 2013). The phenotype switching is reversible, with the population regrown from the persister cells possessing both normal and persister cells. Peptidoglycan plasticity is a key factor in drug sensing and signaling to mitigate antibiotic exposure, where peptidoglycan remodeling enzymes are intimately involved in dormancy and resuscitation phenomena (Cava and de Pedro 2014; Amoroso et al. 2012; Courvalin 2006). In a dormant organism, the presence of specific peptidoglycan fragments can trigger the resuscitation pathway directly; peptidoglycan can also function as a substrate for the endogenous resuscitation-promoting factors, whereby it is hydrolyzed to liberate stimulatory fragments of different size (Nikitushkin et al. 2013). In addition to diversifying the growt h rate to ensure population survival, bacteria can gain survival advantages from differentiation into different shapes (i.e. from bacillary to coccoid morphology) and into a filamentous morphology (Justice et al. 2014; Friedlander et al. 2013).
At present, the molecular mechanisms underlying bacterial persistence remain undiscovered (Maisonneuve et al. 2011), however it is believed that gene pairs encoding cognate toxin-antitoxins present in virtually all bacteria control reversible bacterial growth arrest (Holden 2015; Germain et al.). Equally, little is understood about the relationship between the recurring use of antibiotics, persistence and development of antibiotic resistance . In the future, the persistence-enabling toxin-antitoxin and associated signaling mechanisms may be targeted to either prevent persisters from arising or to transition them into a normal and thus antibiotic-susceptible state (Holden 2015).
7.1.3 Preventing Implant-Associated Infections via Implant Modification
It is evident that antibiotic prophylaxis and tightly controlled operating environment does not prevent an implant-associated infection from occurring. Furthermore, once established on the surface of the implant, a biofilm is difficult to eradicate with systemic antibiotics alone. The efficacy of these antibiotics is also diminishing, with antibiotic resistance spreading faster than the rate at which new antimicrobial compounds, such as teixobactin, can be discovered, evaluated and clinically introduced (Ling et al. 2015). Besides, persistent cells may remain on the surface of the implant, giving rise to chronic infections, and therefore the most logical step would be to localize the antibacterial activity to the surface of the implantable material itself.
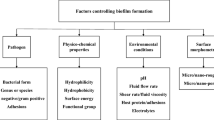
Over the years, numerous strategies have been devised to prevent implant-associated infections by targeting different stages of biofilm formation and molecular and cellular mechanisms of bacterial pathogenesis (Grainger et al. 2013). These include various specific and non-specific anti-adhesive surfaces, and controlled systemic or localized drug delivery to interrupt cell-cell communication, inhibit bacterial aggregation and biofilm formation, or eliminate bacteria directly.
There are several important aspects that need to be considered when imparting antibacterial properties, whether they are physical or chemical features, onto the surface of the implant. An obvious factor is that the bacteria-repelling, bacteriostatic or bactericidal property should be maintained for the intended period of time under in vivo conditions, considering that in vivo environment may vary significantly over time and between patients. For example, if the anti-infective effect is due to the specific surface topograph ical features of the implants, these features should remain available and not be masked by protein fouling or cell debris.
The selected processing methodology should be compatible with the type of the implant material/s and not undermine the physico-chemical and mechanical integrity of the modified device. Neither should this modification destabilize the interactions between the individual components and/or different materials that may constitute a device or be a part of the fixative system, e.g. the adhesion of cement to the metallic component of the bone implant should be maintained. The modification itself should be mechanically robust to withstand normal pre-, intra-, and post-operative handling and operation. For example, an antibacterial coating on a load-bearing implant will experience a wide range of mechanical stresses and strains.
Critically, the modified implant should remain biocompatible and retain its ability to perform its intended function with an appropriate host response. Host response is triggered by the trauma of the surgical and implantation process, and then maintaine d by the physical, chemical, biological and mechanical interactions between the resident implant and the surrounding tissues. Depending on the nature of the implant and the stage of implantation, host response will include inflammatory and wound healing responses, foreign body reactions, or fibrous encapsulation (Anderson 2001).
7.1.4 Host Response and Implant Biocompatibility
Initiated by the action of implantation of a foreign body into a host, the tissue response continuum comprises a diverse ensemble of biological responses, including early events, such as injury, blood-implant interactions, provisional matrix formation, and acute inflammation, and later events, e.g. chronic inflammation, tissue granulation, foreign body reaction and fibrosis (Anderson 2001; Karlsson et al. 2014).
The extent of implantation injury is associated with the placement of the implant, its dimensions, weight and configuration, as well as its mechanical (e.g. flexible vs rigid) and surface (e.g. low-friction vs. abrasive) properties. Most implant-related anti-infective strategies are confined to the surface of the material, potentially altering the surface properties and three-dimensional configuration of the implant.
The injury incites a wound healing cascade, beginning with initial platelet adhesion to the injury site, followed by platelet activation and aggregation. In turn, this initiates a coagulation cascade, leading to clot formation as a measure to manage blood loss and minimise the risk of microbial infection. Clot formation is followed by highly mobile neutrophil granulocytes infiltrating the injury site as part of innate immune responses. Phagocytosis ensues clearing the de bris of damaged tissues and pathogens that may have been introduced into the peri-implant space. Concurrently, phagocytic cells release growth factors to stimulate tissue regeneration, promoting the formation of granulation tissue.
Where an injury results in only exudative inflammation, inflammation resolution and restoration of the original tissue structure proceeds relatively quickly. On the other hand, dominance of pro-inflammatory over generative-type macrophages at the injury sites with significant tissue necrosis and/or loss of basement membrane structures may lead granulation tissue to grow into the inflammatory exudate. As a result, instead of restoration of original tissue structure, organisation and development of fibrous tissue takes place. It is important that even in the case of tissue restoration, re-grown cells may differ in their growth and differentiation behaviour from the original (pre-surgery) tissue. Regenerated cells can differ in their type, size, number, and function level; their ability to produce intra- an extra-cellular polymers can also change.
In addition to the nature of the injury (e.g. skill of the surgeon) and the health status of the host (e.g. suppressed proliferative capacity of cells), the nature of the implant may significantly affect the hemostasis, inflammation, repair, and remodeling processes, and thus directly influence the tissue healing outcomes. For example, copper-based coatings have been shown to effectively reduce infections on the surfaces of titanium implants. Implantation of copper-modified titanium implants has been associated with increased total and tissue macrophages and MHC-class-II-positive cells i n a murine model (Andreas et al. 2013). As the tissue reactions persisted beyond the Cu release, it was concluded that surface-bound Cu may have also contributed to the increased local inflammatory response. In Cu/Ti coatings, an increasing Cu fraction led to an increase in the degree of hemolysis, limited break down of platelets and reduction in platelet adhesion (Liu et al. 2012a). At Cu concentrations above 10 wt.%, significant inhibition of endothelial cell adhesion and proliferation was observed. Given the important role of chemical factors released by plasma and cells in mediating the inflammatory response, implant-released chemicals may interfere with correct tissue regeneration (Yu et al. 2013). Furthermore, the lysosomal proteases and reactive oxygen species abundant at the site of inflammation may promote degradation of the implant material, thus further exacerbating the release of the active compounds.
The importance of the provisional matrix formation on tissue integration should not be underestimated (Anitua et al. 2014; Abrahamsson et al. 2004). The matrix is composed of many components; fibronectin, collagen and thrombospondin bind to fibrin and the platelet granule components of the initial clot. A major constituent of the matrix, fibrin induces neovascularization, promotes cell attachment (Thomson et al. 2013), and provides a scaffold for cell migration and tissue formation. The matrix also releases a wide array of mitogens, chemoattractants, cytokines, and growth factors that regulates cellular proliferation. The formation of the provisional matrix may be considerably altered by the surface properties of the materials (Tejero et al. 2014; Lang et al. 2011), and thus needs to be considered when developing anti-infective coatings.
Importantly, the inflammatory resp onse to the surface properties of the biomaterial needs to be considered in all of its complexity. Specifically, it is important to look beyond the cellular and tissue morphology of the peri-implant region to consider the densities, activities and functions of other cells which may be impacted by endogenous and autacoid mediators (Anderson 2001; Anderson and Miller 1984). Moreover, while the histopathological consequences of acute inflammation are relatively uniform, the same cannot be said for chronic inflammation, where multiple factors can alter the histological appearance of the process. Enduring stimulations, e.g. those by a controlled-released antimicrobial agent, chemical or morphological surface features of the implant, may contribute to the establishment of chronic inflammation. The foreign body response is also influenced by the surface topography , configuration and the surface-to-volume ratio of the implant, with smoother implants having been associated with low levels of macrophages and foreign body giant cells in the peri-implant milieu and a tendency to develop a fibrous capsule. Rough, porous and fabric-like surfaces, on the other hand, have more macrophages and foreign body giant cells in the proximity to the implant, and are less likely to become encapsulated.
7.1.5 Evaluating Biocompatibility
Application of any type of physical or chemical modification to the surface of the implant will directly affect the dynamics of the above described host-implant relationships (Triantafillopoulos and Papaioannou 2014). It is therefore essential to determine whether or not the modified implant is still sufficiently biocompatible for the intended application. This can be done by assessing a series of biological responses, and then comparing the magnitude and duration of the adverse changes in homeostatic mechanisms of the host against those for the unmodified implant.
Consideration needs to be given to the nature and duration of the implant-tissue contact. For example, for medical devices that come into direct contact with blood, good hemocompatibility is paramount. Silver is an element with well-known antibacterial properties that has many promising applications, however, contradictory reports exist about the ability of silver nanoparticles to induce platelet aggregation and procoagulant activation, potentially leading to increased risk of cardiovascular events (Jun et al. 2011; Smock et al. 2014; Shrivastava et al. 2009; AshaRani et al. 2009). The effect of the implant on the mechanisms of thrombosis, coagulation, platelet activation, and production of blood and its components, i.e. blood cells, hemoglobin, blood proteins, will depend on the surface physico-chemical properties of the implant, as well as its geometry, contact conditions, and flow dynamics.
The contact duration is regarded as limited for contact time of less than 24 h, prolonged when implant-tissue contact is maintained for over 24 h to 1 month and permanent thereafter. The location of the implant and the types of tissues and bodily fluids that will be in direct contact with the implant are also considered.
For anti-infective modifications that involve biodegradation and controlled release of particles and/or chemical substances into the peri-implant milieu, the transport, accumulation, degradation and metabolism of these release by-products by other tissues may be of significance. Even very small amounts of metal ions, antimicrobials, biomolecules, nano- and micro-particles can give rise to allergic or sensitization reactions, with the severity of the reaction dependent on the properties of the leachable agent and the sensitivity of the host.
In cases where these biom aterials are implanted into susceptible individuals or are present in higher amounts, leachable agents can induce systemic toxicity , directly affecting the immune, hematologic, central nervous and cardiovascular systems, amongst others. In addition to leachable agents, any structural components of bacteria, yeasts, and molds, organic and inorganic dusts, nanoparticles , and diesel exhaust particles that may remain on the surface of the implant post-sterilization may provoke an inflammatory (innate) response and be fever-producing (pyrogenic) (Mazzotti et al. 2007).
Given that many modern antimicrobial and tissue regeneration strategies are based on the controlled release of biologically active molecules, including growth factors, cytokines, antimicrobial factors and proteins, stem cell stimulating factors, complement proteins, and chemotactic factors, it is important to consider the immunotoxic and immunogenic potential of these reactive agents (Maeda et al. 2007; Bielecki et al. 2007; Chandorkar et al. 2015). Once released inside the host, these molecules, their fragments or their degradation by-products can be recognized by the adaptive immunity, triggering the humoral and cellular response. As such, exposure to these substances can lead to immunosuppression, immunostimulation, or autoimmunity, manifested as histopathological changes, host tissue autoimmune damage, and compromised ability of the host to protect itself from foreign agents. For example, an inorganic compound, protein or lipid component in the drug delivery system may perform as an adjuvant, stimulating autoimmune response; similarly, a foreign biomolecule may induce antibodies that will react with host molecules, leading undesirable t issue damage via complement pathway (Anderson 2001).
Systemic toxicity is typically evaluated as a function of exposure time, with relevant adverse reactions being observed within 24 h after first contact (acute), after 14–28 days of repeat exposure (sub-acute), and up to 90 days of exposure (sub-chronic). Chronic toxicity arises from long term exposure, and is characterized by persistent or progressively deteriorating dysfunction of cells, organs or multiple organ systems. Unlike other types of toxicity, it is difficult to evaluate and predict the chronic toxicity potential of the modified implant, due to the obvious difficulty in maintaining the experimental conditions, such as nutrition, health, and lifestyle parity between test groups.
Implant-related physical, chemical and biological agents may lead to genotoxicity. For example, particles and ions leached from the surface of metallic bone implants have been shown to increase DNA damage, gene mutations, and chromosome aberrations in the adjacent bone marrow and chromosome translocations and aneuploidy in the peripheral blood (Gajski et al. 2014; Karahalil et al. 2014). Such mutations, mistimed event activation, and direct DNA damage may lead to the development of cancer, although the risk of implant-leached products inducing systemic cancers is regarded as very low (Christian et al. 2014; Moalli et al. 2014). The carcinogenicity of the compound is patient-specific in that it depends on the ability of the individual to activate or detoxify genotoxic substances, and to repair deletions, breaks and/or rearrangements within DNA. Interestingly, biomaterial-associated tumor development in animals has been demonstrated to be associated with the physical configuration, not the chemical composition of the implant (Moalli et al. 2014). Implants with a smooth surface and large surface area, such as thin sheets and discs, are more carcinogenic than biomaterials with irregular surface morphologies, such as meshes and porous solids.
Implant-derived particles and reactive chemical species may affect reproductive toxicity . For instance, the reproductive potential of male mice injected with CoCr nanoparticles (to simulate leaching of particles and ions from CoCr alloy implants) was lower than that of the control group, with reduced epididymal sperm motility, viability and concentration, and higher abnormal sperm rate (Wang et al. 2013). Popular anti-microbial agents, silver and titanium dioxide nanoparticles were also found to be cytotoxic and cytostatic for primary testicular cells, causing apoptosis, necrosis and decreased proliferation (Asare et al. 2012). Oxidative stress is the likely driver for the testicular damage and pathological changes. Indeed, the production of reactive oxygen species and DNA damage are regarded as the underlying mechanism of nanoparticle cytotoxicity (Taylor et al. 2012). Compared to bulk materials, nanoparticles have heightened chemical and biological reactivity due to much higher surface-to-volume ratio, which means that even inert biocompatible materials, e.g. gold (Zhao et al. 2013b), can become toxic. Specific toxicity is highly dependent on the size, shape, polarization and surface functionalization of the particle.
Nanoparticles may induce teratogenicity, halting the development or leading to congenital malformation of the fetus, and negatively affecting post-natal development of the offspring. For example, graphene oxide is a promising antimicrobial material (Liu et al. 2011; Podila et al. 2013), which, when modified with silver nanoparticles , becomes even more strongly antibacterial towards pathogens such as E. coli (Ma et al. 2011). When maternal mice were exposed to graphene oxide during lactation, the filial mice developed significantly slower, gaining less body weight and length compared to control group (Fu et al. 2015). The intest inal villus of the filial mice was found to be notably shorter in the offspring mice in the treatment group, indicating a possible mechanism of toxicity .
A critical determinant of toxicity is the dose to which the host is exposed. Biodegradable and drug-release antimicrobial coatings are designed to release tightly controlled quantities of biochemically active substances into the peri-implant milieu. The release rate balances microbial efficacy against host toxicity. Premature biodegradation in vivo, i.e. excessive elimination of the therapeutic compound, may tip that balance. In addition to toxicity, distorted degradation kinetics may result in the premature exhaustion of the anti-bacterial agent. The suboptimal levels of the released agent may not be sufficient to effectively kill bacteria, potentially acting as a positively driver for the development of antibiotic resistivity.
In addition to the active ingredient, toxicity can arise from other seemingly benign degradation products, including very low amounts of impurities, additives and chemicals used in the synthesis and processing of a biomaterial. The chemical and morphological properties of the released agents will be affected by the biodegradation mechanism and on the health status of the host (Baran et al. 2014). Medically compromising systemic conditions, e.g. diabetes, and inflammatory diseases may increase the rate of biomaterial degradation (Alani and Bishop 2014). Higher blood glucose levels and lower pH levels, for instance, has been shown to the rate of electrochemical corrosion of titanium dental implants (Tamam and Turkyilmaz 2014). It is challenging to predict all the potential interactions among the degradation products, and also between these products and other biochemical agents used for the treatment of the patient. One of the issues is associated with the difficulty in identifying appropriate biomarkers for detection of premature degradation onset and progression (Sumner et al. 2014; Grainger et al. 2013).
7.2 Modern Strategies to Minimize Implant-Associated Infections
There exists a wide spectrum of substances and technological methodologies that can be used to fabricate biomaterials with anti-infective features (Jadalannagari et al. 2014), including those based on bio-inspired and biomimetic surface topograph ies (discussed in Chap. 2), electroactive and mechano-responsive surfaces (Chaps. 4 and 8), and natural antimicrobial agents (Chap. 2). Broadly, anti-infective approaches can be divided into two categories: antifouling, i.e. those that repel microbes; and antimicrobial, those that prevent cell proliferation (bacteriostatic ) and/or kill bacteria (bactericidal ). In the following sections, we will discuss several examples of the modern strategies to minimize implant-associated infections, focusing on the challenges in merging the need to withstand bacterial load with that to support fun ction restoration and tissue healing .
7.2.1 Anti-adhesive Surfaces
Device related infections take place when bacteria coat the surface or infiltrate the lumen of an implant. The peri-implant milieu is abundant in nutrients, providing suitable growth conditions for bacterial growth and replication. On the surfaces of implants, bacteria can be present in both planktonic and biofilm forms, the former affording mobility whereas the latter providing means of protection, selective transport of biomolecules, environmental regulation and communication for resident cells. The presence of biofilm markedly increases the likelihood of bacteria evading host defense mechanisms, antimicrobial agents and extended periods of unfavorable environmental conditions. The release of extracellular polymeric substances, e.g. polysaccharides, amyloid fibrils, lipids and nucleic acid (Claessen et al. 2014), is critical to establishment, development and functioning of any biofilm. For example, adhesins enable cell attachment to living tissue or an abiotic substrate and act as receptors for adhesins on other bacteria. A detailed overview of the process of bacterial attachment and biofilm formation can be found in Chap. 1.
Since adherence is a critical first step in pathogenesis, many strategies have been developed to control bacterial and protein adhesion via steric repulsion, low surface energy and electrostatic repulsion. This can be achieved by modifying the surface to be hydrophilic, negatively charged, and/or with low surface free energy (Yu et al. 2011). In the case of hydrophilic polymers, water is attracted to the surface, encapsulating it in a thin repellent layer that is associated with the polymer via hydrogen bonds. This layer creates steric barrier for the biomolecules and cells, preventing their attachment.
The appropriate chemistry is typically obtai ned by surface functionalization, e.g. plasma treatment (Bazaka et al. 2011, 2012; Jacobs et al. 2012), or application of coatings and polymer brushes (Knetsch and Koole 2011; Hook et al. 2012; Chauhan et al. 2014). Hydrophilicity of the material may also be altered by controlling surface morphology (Zheng et al. 2010). For example, metallic surfaces can be made superhydrophobic using chemical etching or laser ablation (Fadeeva et al. 2011). Amongst polymer brushes, amphiphilic copolymers (Liu et al. 2012b; Zhou et al. 2014), zwitterionic polymers (Cheng et al. 2008) and patterned polymers are common. Polymer chemistries based on polyethylene glycol (PEG) or its derivatives are common (Ye and Zhou 2015; Yang et al. 2014), as they are non-immunogenic and effectively resist protein fouling and thrombosis (Chen et al. 2011). The efficacy of PEG modification is strongly dependent on the molecular weight, branching and surface chemistry of the coating (Beloin et al. 2014). In addition to PEG, hydrophilic polymers based on hyaluronic acid (Liu et al. 2014) such as poly-N-vinylpyrrolidone (Liu et al. 2013a), poly(dimethylaminoethyl methacrylate) (Lih et al.; Tu et al. 2013), have also been used.
There are many possible configurations in which polymer brushes can be assembled, and enumerate chemistries that can be used to fine tune their properties for a desired application or to enhance the antifouling property of the surface. Broadly, polymer can be attached in the form of a homopolymer, as mixed polymer or block co-polymer brushes, assembled from functional particles or as layer-by-layer films, incorporating nano- an micro-sized particles, in a form of cross-linked polymer matrixes, and so on (Lih et al.; Wang et al. 2014). For example, the antifouling efficacy of fluorinated amphiphilic copolymers composed of 2-perfluorooctylethyl methacrylate and 2-hydroxyethyl methacrylate was greater than that of their constituent homopolymers, suggesting a synergistic mechanism of fouling inhibition (Zhao et al. 2013c). The stability of the polymer layer is depen dent on the method of immobilization, with physically absorbed (self-assembled) brushes being less chemically stable than covalently linked molecules, e.g. grafted-to or grafted-from polymer chains.
Improved anti-infective outcomes can be achieved by synergistically merging antifouling and antibacterial chemistries, e.g. by coating the implant surface with brush-like polycarbonates containing pendent adhesive dopamine, antifouling PEG , and antibacterial cations (Yang et al. 2014). Such a surface can ensure that bacterial cells able to overcome antifouling chemistry and attach to the implant surface are prevented from multiplying and forming a biofilm (Yang et al. 2014). In another example, antifouling poly(sulfobetaine methacrylate) and bactericidal polymer, N-[(2-hydroxy-3-trimethylammonium)propyl] chitosan chloride polymers are integrated to achieved a similar result (Wang et al. 2015). Heparin and other biomolecules can be loaded into such a coating to enhance surface hemocompatibility and improve host cell attachment (Almodóvar et al. 2013; Zhu et al. 2013). Coating the surface of the implant with heparin and heparin-like molecules has been demonstrated to reduce bacterial attachment and biofilm formation. Presence of heparin or albumin results in a negatively charged surface that reduces bacterial adhesion (as cells bear a net negative charge on their surface under normal pH conditions) and the deposition of fibronectins (Francolini and Donelli 2010).
From a biocompatibility point of view, most anti-fouling surfaces are non-toxic, as the effect is typically achieved by surface chemistry rather tha n a release of antimicrobial agents. At the same time, the antifouling action is generally non-specific, i.e. it may alter the attachment of host biomolecules and cells. While this may be desired for urinary or vascular catheter applications or wound dressings, it may impede the establishment of a tissue-implant interface where integration is desired. To circumvent this problem, antifouling polymer brushes can be functionalized or loaded with biomolecules that promote host cell adhesion, tissue formation and spreading. For example, improved tissue compatibility was obtained by functionalizing brushes of the block copolymer Pluronic F-127 with contact-killing antimicrobial peptides and host cell adhesion promoting arginine-glycine-aspartate (Muszanska et al. 2014) (Figs. 7.1 and 7.2).
Interactions between host cells and anti-adhesive surfaces (Reproduced with a permission (Lih et al.))
Effect of various concentrations of antibiotics on osteogenic cell viability and activity. The mean % decreases in osteoblast cell number (a) and ALP activity (b) are classified as <25 %, 26–50, 51–74, and >75 % of control after incubation with 0, 10, 100, 200, 500, 1000, 2000, and 5000 μg/mL of each antibiotic for 10 and 14 days (n = 5–6 per dose after data are pooled). Not determined: ALP activity and/or cell number was untestable for some of the antibiotics due to precipitation or incompatibility with the test assays used. Decreases in osteoblast cell number and ALP activity >25 % were significant, p < 0.05, with exceptions indicated by (*) where the value at that dose was not different from control (Reproduced with permission (Rathbone et al. 2011))
Higher control over host cell adhesion can be obtained by specifically targeting bacterial adhesion, by using strategies that hinder biogenesis of fimbrial adhesins (Lo et al. 2013; Nait Chabane et al. 2014; Shamir et al. 2010). Production of functional extracellular amyloid fibers by uropathogenic E. coli and other Enterobacteriaceae can be effectively hindered in vitro and in vivo by using ring-fused 2-pyridones, such as FN075 and BibC6 (Cegelski et al. 2009). Pyridone-based pilicides inhibit the assembly of type 1 pili and thus interfere with pathogenesis and formation of curli-dependent and type 1-dependent biofilms. Another target is the FimH, an adhesion located at the tip of type 1 fimbriae and responsible for binding to mannosylated glycoproteins on human cells (Totsika et al. 2013). Here, small molecule mannosides can be used to bind FimH thus making it unavailable for binding to eukaryotic receptors (Guiton et al. 2012). Glycoclusters based on a cyclic oligo-(1→6)-β-D-glucosamine core can be employed to inhibit bacterial lectin LecA of P. aeruginosa (Gening et al. 2013), interfering with the colonization abil ity of the pathogen. Furthermore, the biofilm-forming ability of P. aeruginosa can be compromised by targeting several specific functions of the pathogen. For example, maltose derivatives with bulky hydro-carbon groups inhibit the swarming motility and cell adhesion of P. aeruginosa, demonstrating biofilm inhibition and dispersion (Shetye et al. 2014).
Another potential target is small messenger molecules that enable pathogen cell-to-cell communication within a colony. Being a co-operative process, biofilm formation is inherently dependent on information being effectively transported from cell to cell. Quorum sensing is responsible for synchronization of gene expression, co-ordinated switch between planktonic and sessile states, biofilm formation, maturation and disassembly (Solano et al. 2014; Singh et al. 2000). By targeting the major signaling pathways of cells, bacterial communication and thus biofilm formation can be compromised. Sulfathiazole and azathioprine has been shown to inhibit diguanylate cyclases (Sambanthamoorthy et al. 2012, 2013; Antoniani et al. 2010, 2013). This enzyme is responsible for production of c-di-GMP, a small messenger molecule responsible for switching from planktonic to biofilm modality.
Nitric oxide is another molecule that can interfere with biofilm formation and induce dispersal of P. aeruginosa (Barraud et al. 2009). Nitric oxide increases cell motility by decreasing the levels of the secondary messenger cyclic di-GMP and decreasing production of adhesins, making these cells more susceptible to antibiotic agents (Li et al. 2013). Nitric-oxide producing compounds can be easily immobilized on the surfaces of implants, releasing NO under specific in vivo conditions (Li et al. 2013; Duong et al. 2014). A controlled release of low levels of NO may also enhance the biocompatibility of the surfaces by reducing platelet activation and adhesion, and inhibiting thrombus formation. NO has a complex role in tissue inflammation (Laroux et al. 2001), where under normal physiological conditions, NO has an anti-inflammatory effect. At the same time, overproduction of NO can promote inflammation, with large amounts of NO being released by cytokine-activated macrophages, contributing to pathogenesis of inflammatory disorders, vasoconstriction, and tissue damage (Sharma et al. 2007).
7.2.2 Antibacterial Surfaces
Most strategies aimed at reducing biofilm-associated infections combine an antifouling property with antimicrobial activity (Francolini et al. 2015; Salwiczek et al. 2014), either through eluti on of antimicrobial agent or a surface killing. Antimicrobial agents range from conventional (systemic) antibiotics (Gao et al. 2011), e.g. nafcillin, levofloxacin, daptomycin, gentamycin, vancomycin (Bastari et al. 2014; Beenken et al. 2014; Ordikhani et al. 2014; Wu et al. 2014; Cashman et al. 2013), to metallic ions such as silver (Wong and Liu 2010; Chernousova and Epple 2013; Perez et al. 2014; Jo et al. 2014) and copper (Kalaivani et al. 2014; Ye et al. 2014; Chen et al. 2014), nitrofurazone (Kottur et al. 2015; Johnson et al. 2012), chlorhexidine (Jamal et al. 2014), quaternary ammonium compounds (Asri et al. 2014; Shalev et al. 2012; Cheng et al. 2012; Bakhshi et al. 2013), antibacterial peptides (Muszanska et al. 2014; Cleophas et al. 2014; Rapsch et al. 2013; Etayash et al. 2013) and anionic nanoporous hydrogels (Li et al. 2011; Hook et al. 2012). These agents are highly diverse in their modes of action. For example, an antimicrobial polycationic hydrogel based on dimethyldecylammonium chitosan-graft-PEG methacrylate and PEG diacrylate attracts sections of the anionic membrane of the pathogen into the internal nanopores of the hydrogel (Li et al. 2011). This process leads to bacterial membrane disruption and subsequent death. Synthetic macromolecular antimicrobials are being researched for their potential to physically destroy cell membranes of the pathogens thus preventing them from developing drug-resistance. Examples of this type of antibacterial s include biodegradable cationic polycarbonates containing propyl and hexyl side chains quaternized with various nitrogen-containing heterocycles, such as imidazoles and pyridines (Ng et al. 2014). Although not based on a particular chemistry, surface capable of contact killing using morphological features are also being investigated (Ivanova et al. 2012, 2013).
7.2.2.1 Systemic Antibiotics
Conventional antibiotics have the advantage of having been thoroughly investigated, with well-defined host toxicity profiles and hist ories of clinical use that might detail potential long-term side effects. Since the doses of antibiotic released from the surface of implant are typically notably smaller than those used systemically, the toxicity of drug-eluting coatings is considered to be low. Indeed, one of the key advantages of drug-release coatings is the ability to locally deliver relatively high doses of antibiotic without inducing systemic toxicity. Nonetheless, the effects of antibiotics on cell viability and tissue regeneration should be considered. Osteoblasts treated with 21 different antibiotics over 0–5000 μg/mL concentrations for up to 14 days showed significantly lower cell number and osteogenic activity when exposed to rifampin, minocycline, doxycycline, nafcillin, penicillin, ciprofloxacin, colistin methanesulfonate, and gentamicin (Rathbone et al. 2011). On the other hand, osteoblast deoxyribonucleic acid content and alkaline phosphatase activity were least affected by amikacin, tobramycin, and vancomycin (Rathbone et al. 2011). Nevertheless, the majority of the antibiotics tested, a ≥50 % decrease in osteoblast cell number and/or osteogenic activity was observed. The decrease in the metabolic activity and thus the osteogenic potential of surviving cells may undermine bone repair.
7.2.2.2 Metals Salts
Metallic salts, such as those of silver, copper, zinc and mercury have been used to prevent and treat infections in wounds and burns for thousands of years. Long before the invention of polymer sutures, silver threads were also used to clo se wounds (Muffly et al. 2011), while silver-based solutions and creams (e.g. silver nitrate, silver sulfadiazine) were used as washes and ointments. Silver-based compounds precipitate cellular proteins and interfere with respiration of both aerobic and anaerobic bacteria, however the exact mechanism is yet to be fully elucidated (Chernousova and Epple 2013). Silver can also be used as part of combination therapy, where its ability to damage bacterial cells is used to potentiate antibiotic activity of conventional antibiotics (Morones-Ramirez et al. 2013) and thus target persister cells.
Current uses of silver primarily focus on a nano-sized particulate form of the metal (Rai et al. 2009; Wong and Liu 2010; Taheri et al. 2014). The nanoparticle form is characterized by high surface -to-volume ratio, which makes the particulate form of silver significantly more active with regard to its physicochemical and biological properties. It is believed that large surface area of nanoparticles allows them to establish good contact with the surfaces of target cell, whereas small size may facilitate particle penetration inside the pathogen. Larger surface area also enables more efficient release of silver ions, which can then interact with sulfur- and phosphorous-containing biomolecules in the bacterial membrane and DNA, respectively. Enhanced chemical reactivity of silver nanoparticles leads to the generation of a large number of reactive oxygen species, which inflict further damage to the cells.
From a biocompatibility and cytotoxicity point of view, the major issue with the use of metallic ions is that their biological interactions are non-specific. Indeed, silver nanoparticles can easily breach host tissue and cell barriers, and interact with host biomolecules, e.g. enzymes, altering cell signalling and metabolic pathways (Gérard et al. 2010; Taylor 1985; Mouriño et al. 2012). Composition, dimensions, configuration and functionalization will affect the transport of chemical reactivity, and as such, the antibacterial efficacy and the potential toxicity of the nanoparticles (Li et al. 2012; Rai et al. 2009). For example, when human bone marrow mesenchymal stem cells and human hepatoma carcinoma cells were incubated in the presence of gold nanoparticles of different size, survival was 80 % in the case of 15 and 30 nm cells and less than 60 % for 5 nm particles (Fan et al. 2009). The increased levels of cell necrosis and altered osteogenic and adipogenic capabilities were attributed to the increase in the level of reactive oxygen species.
Anti-proliferative activity of silver nanoparticles was demonstrated in human lung fibroblasts (IMR-90) and glioblastoma cells, with treated cells ex hibiting chromosome instability and mitotic arrest (AshaRani et al. 2009). Exposure to silver nanoparticles induced apoptosis in NIH3T3 fibroblast cells, inducing the release of cytochrome c into the cytosol and translocation of Bax to mitochondria through ROS and JNK (Hsin et al. 2008). Cellular apoptosis was also induced in RAW264.7 macrophage cells cultured in the presence of ~70 nm silver nanoparticles (Park et al. 2010). These particles were found to lower the intracellular glutathione level, increase NO secretion and TNF-α in protein and gene levels, and increase the gene expression of matrix metalloproteinases. It was demonstrated that intracellular oxidative stress due to the presence of agglomerated nanoparticles rather than ion damage was responsible for apoptosis in human hepatoma HepG2 cells (Kim et al. 2009). DNA damage may have also played a role, as hepatoma cells cultured with low dose silver nanoparticles showed an upregulation of DNA repair-associated genes (Kawata et al. 2009).
Oxidative stress was determined to be the cause of HeLa cell death, where oxidative stress-related genes, ho-1 and mt-2A, were expressed (Miura and Shinohara 2009). Coated silver nanoparticles also induced oxidative stress-type damage onto N27 rat dopaminergic neurons, where the size of the particle and type of coating determined the dominant pathway (Chorley et al. 2014). Poly(vinyl pyrrolidone)-coated particles were found to be more bioactive than citrate-coated particles, increasing intra-neuronal nitrite levels and inducing mitochondrial dysfunction (75 nm particles) and NRF2 oxidative stress pathway (10 nm particles) (Veronesi et al. 2014).
In the case of copper particles, the physical form of the particle is important, with dissolved Cu2+ ions contributing <50 % to cytotoxicity (Wang et al. 2012). A comparison between cell-particle interactions of nano-sized CuO and Ag showed that in the case of CuO, the particle was subject to rapid uptake by endocytosis, releasing copious amounts of co pper ionic species within the cells (Cronholm et al. 2013). Even though silver particles were readily taken up by the cells, the intracellular release of silver ions and hence the toxicity of the particles was low. The mechanism of toxicity also differed between different types of copper, where nanoparticles of copper and Cu-Zn alloy inflicted substantial damage onto cell membranes, whereas this behavior was not observed in the case of CuO nanoparticles and the micron-sized Cu metal particles (Karlsson et al. 2013). Protein fouling in the presence of serum albumin inhibited cell toxicity of silver nanoparticles (Gnanadhas et al. 2013).
The systemic toxicity of medically-relevant metallic nanoparticles is not well studied (Alenius et al. 2014). Once eluted from the surface of the implant, the particles should theoretically be able to quickly and easily cross the blood barrier, being transported to other tissues in the body. There, these nanoparticles can potentially accumulate and degrade (Wong and Liu 2010). With regard to the cardiovascular system, sufficiently high doses of nanoparticles can alter the microcirculation, and promote thrombus formation and pro-inflammatory responses (Wong and Liu 2010), whilst in the central nervous system metallic nanoparticles may generate oxygen reactive species and damage the brain cells (Alenius et al. 2014). An iron- and oxygen-binding protein found in the muscle tissue, myoglobin can be affected by the presence of silver nanoparticles, where ~10 nm particles were shown to significantly augment its electron-transfer reactivity and catalytic ability toward hydrogen peroxide (Gan et al. 2004). They may also affect the reproduc tive ability of the host, as silver nanoparticles showed concentration dependent cytotoxicity towards mouse spermatogonial stem cells (Braydich-Stolle et al. 2005).
7.2.2.3 Chlorhexidine and Quaternary Ammonium Compounds
Chlorhexidine, a bisbiguanide, is an effective hospital disinfectant often used in surgery skin preparation and as an antimicrobial agent in medical devices (Opstrup et al. 2014; Silvestri and McEnery-Stonelake 2013) where they are employed to reduce extraluminal contamination, particularly in patients who require long-term vascular access (Khoo and Oziemski 2011). Recently, concerns have been raised about potentially significant allergic reactions to chlorhexidine-impregnated medical devices (Guleri et al. 2012). Severe allergic reactions, including anaphylactic shock have been reported for patients during the placement of a chlorhexidine impregnated central venous catheters (Khoo and Oziemski 2011; Faber et al. 2012; Bae et al. 2008), urological and rectal procedures (Jayathillake et al.; Bae et al. 2008). Approximately 10 % of patients with suspected perioperative allergic reactions were diagnosed with chlorhexidine (Opstrup et al. 2014). Wide e xposure to chlorhexidine in hospital and non-medical environments may potentially sensitize some patients, leading to adverse reactions during surgery.
Quaternary ammonium compounds (QACs) are potent cationic antimicrobials active against a wide range of pathogens (Hegstad et al. 2010). QACs kill bacteria by interfering with cell membranes, primarily the cytoplasmic membrane, leading to membrane damage and loss of cellular content (Martín et al. 2014). QACs block potassium channels that are responsible for the passive movement of potassium ions across the cell membrane and control the membrane potential in both eukaryotic and prokaryotic cells (Lenaeus et al. 2014). QACs may disrupt and denature structural proteins and enzymes. In anti-infective device applications, QACs can be loaded into coatings or surface immobilize for contact killing (Asri et al. 2014). As with other non-specific antimicrobial compounds, quaternary ammonium compounds display concentration-dependent eukaryotic cell toxicity with all types of exposure, namely inhalation, ingestion, and dermal application and irrigation of body cavities (Xue et al. 2004, 2012; Świercz et al. 2013; Dutot et al. 2008a, b). In susceptible individuals, contact with QACs may result in allergies that can range from mild localised irritation to anaphylactic reaction (Bello et al. 2009) and contact tissue damage (Kilic et al.). Mucosal contact with QACs may produce sensitization.
7.2.2.4 Antimicrobial Peptides
Produced by a large number of microorganisms, plants, invertebrates and animal species, antimicrobial peptides fulfil a broad range of roles in producing an innate immune response, specifically they hinder the growth and colonisation by infectious agents (Zasloff 2002; Bals et al. 1999). For example, resident epithelial cells (e.g. keratinocytes) produce a number of antimicrobial peptides and also signal the recruitment of circulating immune cells (e.g. neutrophils); once summoned, neutrophils also produce antimicrobial peptides, such as cathelicidin and β-defensins to fight the infection (Braff et al. 2005; Nizet et al. 2001). When adsorbed onto surfaces, nisin, an antimicrobial peptide, inhibits the attachment and biofilm formation capability of Gram-positive bacteria (Bower et al. 2002), whereas covalently-bound to the surface cathelin LL37 effectively kills E. coli on contact (Zaiou et al. 2003).
In Gram-positive and Gram-negative organisms, the antibacterial mechanism of the antimicrobial peptides is biophysical rather than biochemical in nature, destabilizing and disorganizing the structure of the membrane (Fitzgerald-Hughes et al. 2012). The cationic nature and amphipathic structure of antimicrobial peptides allows them to electrostatically attach to the negatively charged microbial surfaces (Powers and Hancock 2003; Forbes et al. 2013; Zasloff 2002). Subsequently, some peptides induce pore formation in the phospholipid bilayer, with death being a consequence of osmolysis (Augustyniak et al. 2012). A compromised cytoplasmic membrane also enables the translocated peptides to interact with intracellular biomolecules of the pathogen, inhibiting protein synthesis and conformation, interfering with DNA and metabolic activit y, and suppressing cell multiplication (Brogden 2005). For example, the antibacterial action of nisin involves bacterial membrane permeation and disruption of the ability for the cell wall to undergo synthesis and regeneration (Hale and Hancock 2007).
Given that antimicrobial peptides typically combine several mechanisms of action, they are less likely to prompt de novo resistance (Yeung et al. 2011). The killing efficacy, and potentially the antibacterial mechanism itself varies with peptide structure and the target organism (Augustyniak et al. 2012; Veiga et al. 2012; Salick et al. 2007, 2009; Liu et al. 2013b; Zhou et al. 2011); however, there is only a limited understanding of all the mechanisms involved, which limits the optimization and clinical use of these peptides (Sahl et al. 2005). Further hindrance comes from the in vivo instability of these antimicrobial agents, whereby they are easily degraded by host enzymes, in addition to being affected by pH and osmotic conditions (Brogden and Brogden 2011). Various structural modifications have been proposed to improve peptide resistance to enzymatic proteolysis without compromising its killing efficacy (Zasloff 2002; Hamuro et al. 1999; Porter et al. 2000).
Being a foreign protein, host defense peptides can potentially be immunogenic. Host defense peptides are considered to be weakly immunogenic, owing to their small size and linear structure (Fitzgerald-Hughes et al. 2012). Nevertheless, antibodies were produced to human neutrophil defensins (Panyutich et al. 1991), bovine lactoferricin(R) (Shimazaki et al. 1996) and hCAP-18 (Sørensen et al. 1997). Furthermore, it is unclear whether the use of foreign peptides will lead to the development of peptide resistance in pathogenic ba cteria, and thus compromise the natural ability of the host to fight infection (Fitzgerald-Hughes et al. 2012). The effect of synthetic human defense peptide-like molecules on the natural innate response has yet to be studied.
With regard to selectivity and cytotoxicity of antimicrobial peptides (Hancock and Sahl 2006), the comparative absence of negatively charged lipids on the surfaces of eukaryotic cells and their weak membrane potential gradient may afford some protection to host cells (Fitzgerald-Hughes et al. 2012). Some host defense peptides, e.g. magainin 2 and human cathelicidin LL-37, can translocate into the cytosol of mammalian cells, e.g. HeLa, TM12 and Chinese hamster ovary (CHO)-K1 cells (Imura et al. 2008; Takeshima et al. 2003). At higher concentrations of the magainin 2 peptide, cell toxicity was observed. The translocation across host cell is possible owing to a dual role of peptides such as LL-37, i.e. bacterial targeting and delivery of nucleic acids into the host cells (Zhang et al. 2010). Even though LL-37 is not haemolytic at antibacterial-relevant concentrations, in vitro cytotoxicit y has been observed. Toxicity towards eukaryotic cells of orangutan, rhesus macaque and leaf eater monkey orthologues of LL-37 varied with the physical characteristics, with the leaf eater monkey peptide being most toxic (Tomasinsig et al. 2009). Cytotoxicit y also depended on the nature and metabolic state of the target cells. At the same time, haemolytic activity was fou nd to be similar among the tested peptides.
The preferential activity against Gram-positive and/or Gram-negative bacteria membranes over eukaryotic cells can be enhanced by controlling the ratio of D- to L-amino acids (Fernandez-Lopez et al. 2001; Oren and Shai 2000; Yin et al. 2012). Structural modifications, e.g. truncation or rearrangement, can be used to enhance membranolytic efficiency (Shimizu et al. 1998). If it is done while disregarding other relevant targets, however, the increased non-specific membranolytic activity can undermine surface bio-compatibility to the extent that this modification will have limited in vivo use. Target-specific antimicrobial peptides, where a Pseudomonas-specific targeting moiety is appended to a generally killing peptide novispirin G10, can both improve the speed and efficiency of bactericidal action (Eckert et al. 2006).
7.3 Conclusion
The host response to the act of implantation initiates a highly complex and multi-dimensional cascade of events, that start with an injury and proceeds to include blood-surface interactions, provisional matrix formation, acute and chronic inflammation, foreign body reaction, development of granulated tissue, healing and fibrous capsule formation. The exact events taking place will depend on a multitude of different parameters, including those pertinent to the host, those associated with the quality of the surgical procedure, and those that result from interactions between living host tissues and the surface and bulk characteristics of the biomaterial. Not surprisingly, predicting or even describing the biocompatibility of an implant is not trivial. The task becomes even more challenging when bio degradable and eluting surfaces are considered. It is these surfaces, however, that hold the greatest promise in mitigating biomaterial-associated infections. Indeed, where antifouling surfaces may succeed in some short term applications, long-term and permanent devices require a reliable means to ensure pathogen-free surfaces. Surface modification that synergistically combines multiple complementary lines of defense may provide the most effective and durable solution. Nevertheless, balancing the biocompatibility of an implant against the ability of their surfaces to be efficient over a range of bacterial loads is a difficult task. With the rise of alternative antimicrobial agents or configurations, more information is needed regarding their compatibility, toxicity and immunogenicity towards relevant host cells. In order to attain a more comprehensive picture, it is important to approximate the conditions under which implants will operate and the quantities of active agents that can potentially be leached out into the peri-implant milieu. A standardized experimental procedure with a focus on both the anti-infective efficacy and biocompatibility should provide for a better comparison between different antimicrobial strategies. It should also provide valuable information on which material and process optimization can be based to ensure appropriate cell integration; after all, for many applications, th e ultimate aim is to achieve an adequate tissue integration and a functional implant.
References
Abrahamsson I, Berglundh T, Linder E, Lang NP, Lindhe J (2004) Early bone formation adjacent to rough and turned endosseous implant surfaces. Frühe Knochenbildung bei rauen und gedrehten enossalen Implantatoberflächen Eine experimentelle Studie an Hunden. Clin Oral Implants Res 15(4):381–392. doi:10.1111/j.1600-0501.2004.01082.x
Alani A, Bishop K (2014) Peri-implantitis. Part 2: Prevention and maintenance of peri-implant health. Br Dent J 217(6):289–297. doi:10.1038/sj.bdj.2014.809
Alenius H, Catalán J, Lindberg H, Norppa H, Palomäki J, Savolainen K (2014) Chapter 3 – Nanomaterials and human health. In: Berges UVSWTB (ed) Handbook of nanosafety. Academic, San Diego, pp 59–133. http://dx.doi.org/10.1016/B978-0-12-416604-2.00003-2
Almodóvar J, Mower J, Banerjee A, Sarkar AK, Ehrhart NP, Kipper MJ (2013) Chitosan-heparin polyelectrolyte multilayers on cortical bone: periosteum-mimetic, cytophilic, antibacterial coatings. Biotechnol Bioeng 110(2):609–618. doi:10.1002/bit.24710
Amoroso A, Boudet J, Berzigotti S, Duval V, Teller N, Mengin-Lecreulx D, Luxen A, Simorre J-P, Joris B (2012) A peptidoglycan fragment triggers β-lactam resistance in <italic>Bacillus licheniformis</italic> PLoS Pathog 8(3):e1002571. doi:10.1371/journal.ppat.1002571
Anderson JM (2001) Biological responses to materials. Annu Rev Mater Res 31(1):81–110. doi:10.1146/annurev.matsci.31.1.81
Anderson JM, Miller KM (1984) Biomaterial biocompatibility and the macrophage. Biomaterials 5(1):5–10. http://dx.doi.org/10.1016/0142-9612(84)90060-7
Andreas H, Cornelia P, Uwe W, Silke L, Maciej P, Lutz W, Hans-Georg N, Michael S (2013) In vivo evaluation of copper release and acute local tissue reactions after implantation of copper-coated titanium implants in rats. Biomed Mater 8(3):035009
Anitua E, Prado R, Orive G, Tejero R (2014) Effects of calcium-modified titanium implant surfaces on platelet activation, clot formation, and osseointegration. J Biomed Mater Res A. doi:10.1002/jbm.a.35240
Antoniani D, Bocci P, Maciąg A, Raffaelli N, Landini P (2010) Monitoring of diguanylate cyclase activity and of cyclic-di-GMP biosynthesis by whole-cell assays suitable for high-throughput screening of biofilm inhibitors. Appl Microbiol Biotechnol 85(4):1095–1104. doi:10.1007/s00253-009-2199-x
Antoniani D, Rossi E, Rinaldo S, Bocci P, Lolicato M, Paiardini A, Raffaelli N, Cutruzzolà F, Landini P (2013) The immunosuppressive drug azathioprine inhibits biosynthesis of the bacterial signal molecule cyclic-di-GMP by interfering with intracellular nucleotide pool availability. Appl Microbiol Biotechnol 97(16):7325–7336. doi:10.1007/s00253-013-4875-0
Asare N, Instanes C, Sandberg WJ, Refsnes M, Schwarze P, Kruszewski M, Brunborg G (2012) Cytotoxic and genotoxic effects of silver nanoparticles in testicular cells. Toxicology 291(1–3):65–72. http://dx.doi.org/10.1016/j.tox.2011.10.022
Asharani P, Hande MP, Valiyaveettil S (2009) Anti-proliferative activity of silver nanoparticles. BMC Cell Biol 10(1):65
Asri LATW, Crismaru M, Roest S, Chen Y, Ivashenko O, Rudolf P, Tiller JC, van der Mei HC, Loontjens TJA, Busscher HJ (2014) A shape-adaptive, antibacterial-coating of immobilized quaternary-ammonium compounds tethered on hyperbranched polyurea and its mechanism of action. Adv Funct Mater 24(3):346–355. doi:10.1002/adfm.201301686
Augustine S (2014) All surgical site infections are not equal. Anesth Analg 118(4):883 810.1213/ANE.0000000000000104
Augustyniak D, Nowak JT, Lundy F (2012) Direct and indirect antimicrobial activities of neuropeptides and their therapeutic potential. Curr Protein Pept Sci 13(8):723–738. doi:10.2174/138920312804871139
Bae Y-J, Park CS, Lee JK, Jeong E, Kim T-B, Cho YS, Moon H-B (2008) A case of anaphylaxis to chlorhexidine during digital rectal examination. J Korean Med Sci 23(3):526–528
Bakhshi H, Yeganeh H, Mehdipour-Ataei S, Shokrgozar MA, Yari A, Saeedi-Eslami SN (2013) Synthesis and characterization of antibacterial polyurethane coatings from quaternary ammonium salts functionalized soybean oil based polyols. Mater Sci Eng C 33(1):153–164. http://dx.doi.org/10.1016/j.msec.2012.08.023
Balaban NQ, Merrin J, Chait R, Kowalik L, Leibler S (2004) Bacterial persistence as a phenotypic switch. Science 305(5690):1622–1625. doi:10.1126/science.1099390
Bals R, Weiner DJ, Moscioni AD, Meegalla RL, Wilson JM (1999) Augmentation of innate host defense by expression of a cathelicidin antimicrobial peptide. Infect Immun 67(11):6084–6089
Baran G, Kiani M, Samuel S (2014) Properties of the host (the human body). In: Healthcare and biomedical technology in the 21st century. Springer, New York, pp 183–202. doi:10.1007/978-1-4614-8541-4_6
Barraud N, Schleheck D, Klebensberger J, Webb JS, Hassett DJ, Rice SA, Kjelleberg S (2009) Nitric oxide signaling in Pseudomonas aeruginosa biofilms mediates phosphodiesterase activity, decreased cyclic Di-GMP levels, and enhanced dispersal. J Bacteriol 191(23):7333–7342. doi:10.1128/jb.00975-09
Bastari K, Arshath M, Ng Z, Chia J, Yow Z, Sana B, Tan M, Lim S, Loo S (2014) A controlled release of antibiotics from calcium phosphate-coated poly(lactic-co-glycolic acid) particles and their in vitro efficacy against Staphylococcus aureus biofilm. J Mater Sci Mater Med 25(3):747–757. doi:10.1007/s10856-013-5125-9
Bazaka K, Jacob MV, Crawford RJ, Ivanova EP (2011) Plasma-assisted surface modification of organic biopolymers to prevent bacterial attachment. Acta Biomater 7(5):2015–2028. http://dx.doi.org/10.1016/j.actbio.2010.12.024
Bazaka K, Jacob M, Crawford R, Ivanova E (2012) Efficient surface modification of biomaterial to prevent biofilm formation and the attachment of microorganisms. Appl Microbiol Biotechnol 95(2):299–311. doi:10.1007/s00253-012-4144-7
Beenken KE, Smith JK, Skinner RA, McLaren SG, Bellamy W, Gruenwald MJ, Spencer HJ, Jennings JA, Haggard WO, Smeltzer MS (2014) Chitosan coating to enhance the therapeutic efficacy of calcium sulfate-based antibiotic therapy in the treatment of chronic osteomyelitis. J Biomater Appl. doi:10.1177/0885328214535452
Bello A, Quinn M, Perry M, Milton D (2009) Characterization of occupational exposures to cleaning products used for common cleaning tasks-a pilot study of hospital cleaners. Environ Heal 8(1):11
Beloin C, Renard S, Ghigo J-M, Lebeaux D (2014) Novel approaches to combat bacterial biofilms. Curr Opin Pharmacol 18:61–68. http://dx.doi.org/10.1016/j.coph.2014.09.005
Bielecki TM, Gazdzik TS, Arendt J, Szczepanski T, Król W, Wielkoszynski T (2007) Antibacterial effect of autologous platelet gel enriched with growth factors and other active substances: an in vitro study. J Bone Joint Surg Br 89-B(3):417–420. doi:10.1302/0301-620x.89b3.18491
Billings N, Ramirez Millan M, Caldara M, Rusconi R, Tarasova Y, Stocker R, Ribbeck K (2013) The extracellular matrix component Psl provides fast-acting antibiotic defense in <italic>Pseudomonas aeruginosa</italic> iofilms. PLoS Pathog 9(8):e1003526. doi:10.1371/journal.ppat.1003526
Bower CK, Parker JE, Higgins AZ, Oest ME, Wilson JT, Valentine BA, Bothwell MK, McGuire J (2002) Protein antimicrobial barriers to bacterial adhesion: in vitro and in vivo evaluation of nisin-treated implantable materials. Colloids Surf B: Biointerfaces 25(1):81–90. http://dx.doi.org/10.1016/S0927-7765(01)00318-6
Braff MH, Zaiou M, Fierer J, Nizet V, Gallo RL (2005) Keratinocyte production of cathelicidin provides direct activity against bacterial skin pathogens. Infect Immun 73(10):6771–6781. doi:10.1128/iai.73.10.6771-6781.2005
Braydich-Stolle L, Hussain S, Schlager JJ, Hofmann M-C (2005) In vitro cytotoxicity of nanoparticles in mammalian germline stem cells. Toxicol Sci 88(2):412–419. doi:10.1093/toxsci/kfi256
Brogden KA (2005) Antimicrobial peptides: pore formers or metabolic inhibitors in bacteria? Nat Rev Microbiol 3(3):238–250. doi:10.1038/nrmicro1098
Brogden NK, Brogden KA (2011) Will new generations of modified antimicrobial peptides improve their potential as pharmaceuticals? Int J Antimicrob Agents 38(3):217–225. http://dx.doi.org/10.1016/j.ijantimicag.2011.05.004
Cashman J, Jackson J, Mugabe C, Gilchrist S, Ball K, Tredwell S, Burt H (2013) The use of tissue sealants to deliver antibiotics to an orthopaedic surgical site with a titanium implant. J Orthop Sci 18(1):165–174. doi:10.1007/s00776-012-0325-6
Cava F, de Pedro MA (2014) Peptidoglycan plasticity in bacteria: emerging variability of the murein sacculus and their associated biological functions. Curr Opin Microbiol 18:46–53. http://dx.doi.org/10.1016/j.mib.2014.01.004
Cegelski L, Pinkner JS, Hammer ND, Cusumano CK, Hung CS, Chorell E, Åberg V, Walker JN, Seed PC, Almqvist F, Chapman MR, Hultgren SJ (2009) Small-molecule inhibitors target Escherichia coli amyloid biogenesis and biofilm formation. Nat Chem Biol 5(12):913–919. doi:10.1038/nchembio.242
Chandorkar Y, Bhaskar N, Madras G, Basu B (2015) Long term, sustained release of salicylic acid from crosslinked. Biodegradable polyesters induces reduced foreign body response in mice. Biomacromolecules. doi:10.1021/bm5017282
Chauhan A, Bernardin A, Mussard W, Kriegel I, Estève M, Ghigo J-M, Beloin C, Semetey V (2014) Preventing biofilm formation and associated occlusion by biomimetic glycocalyx-like polymer in central venous catheters. J Infect Dis. doi:10.1093/infdis/jiu249
Chen X, Su Y, Shen F, Wan Y (2011) Antifouling ultrafiltration membranes made from PAN-b-PEG copolymers: effect of copolymer composition and PEG chain length. J Membr Sci 384(1–2):44–51. http://dx.doi.org/10.1016/j.memsci.2011.09.002
Chen N-H, Chung C-J, Chiang C-C, Chen K-C, He J-L (2014) Antimicrobial copper-containing titanium nitride coatings Co-deposited by arc ion plating/magnetron sputtering for protective and decorative purposes. Surf Coat Technol 253:83–88. http://dx.doi.org/10.1016/j.surfcoat.2014.05.017
Cheng G, Xue H, Zhang Z, Chen S, Jiang S (2008) A switchable biocompatible polymer surface with self-sterilizing and nonfouling capabilities. Angew Chem Int Ed 47(46):8831–8834. doi:10.1002/anie.200803570
Cheng L, Weir MD, Xu HHK, Antonucci JM, Kraigsley AM, Lin NJ, Lin-Gibson S, Zhou X (2012) Antibacterial amorphous calcium phosphate nanocomposites with a quaternary ammonium dimethacrylate and silver nanoparticles. Dent Mater 28(5):561–572. http://dx.doi.org/10.1016/j.dental.2012.01.005
Chernousova S, Epple M (2013) Silver as antibacterial agent: ion, nanoparticle, and metal. Angew Chem Int Ed 52(6):1636–1653. doi:10.1002/anie.201205923
Chorley B, Ward W, Simmons SO, Vallanat B, Veronesi B (2014) The cellular and genomic response of rat dopaminergic neurons (N27) to coated nanosilver. NeuroToxicology 45:12–21. http://dx.doi.org/10.1016/j.neuro.2014.08.010
Christian WV, Oliver LD, Paustenbach DJ, Kreider ML, Finley BL (2014) Toxicology-based cancer causation analysis of CoCr-containing hip implants: a quantitative assessment of genotoxicity and tumorigenicity studies. J Appl Toxicol 34(9):939–967. doi:10.1002/jat.3039
Claessen D, Rozen DE, Kuipers OP, Sogaard-Andersen L, van Wezel GP (2014) Bacterial solutions to multicellularity: a tale of biofilms, filaments and fruiting bodies. Nat Rev Microbiol 12(2):115–124. doi:10.1038/nrmicro3178
Claridge JA, Banerjee A, Kelly KB, Leukhardt WH, Carter JW, Haridas M, Malangoni MA (2014) Bacterial species-specific hospital mortality rate for intra-abdominal infections. Surg Infect 15(3):194–199. doi:10.1089/sur.2011.039
Cleophas RTC, Riool M, Quarles Van Ufford HC, Zaat SAJ, Kruijtzer JAW, Liskamp RMJ (2014) Convenient preparation of bactericidal hydrogels by covalent attachment of stabilized antimicrobial peptides using thiol–ene click chemistry. ACS Macro Lett 3(5):477–480. doi:10.1021/mz5001465
Courvalin P (2006) Vancomycin resistance in gram-positive cocci. Clin Infect Dis 42(Supplement 1):S25–S34. doi:10.1086/491711
Cronholm P, Karlsson HL, Hedberg J, Lowe TA, Winnberg L, Elihn K, Wallinder IO, Möller L (2013) Intracellular uptake and toxicity of Ag and CuO nanoparticles: a comparison between nanoparticles and their corresponding metal ions. Small 9(7):970–982. doi:10.1002/smll.201201069
Duong HTT, Jung K, Kutty SK, Agustina S, Adnan NNM, Basuki JS, Kumar N, Davis TP, Barraud N, Boyer C (2014) Nanoparticle (star polymer) delivery of nitric oxide effectively negates Pseudomonas aeruginosa biofilm formation. Biomacromolecules 15(7):2583–2589. doi:10.1021/bm500422v
Dutot M, Liang H, Pauloin T, Brignole-Baudouin F, Baudouin C, Warnet J-M, Rat P (2008a) Effects of toxic cellular stresses and divalent cations on the human P2X7 cell death receptor. Mol Vis 14:889–897
Dutot M, Warnet J-M, Baudouin C, Rat P (2008b) Cytotoxicity of contact lens multipurpose solutions: role of oxidative stress, mitochondrial activity and P2X7 cell death receptor activation. Eur J Pharm Sci 33(2):138–145. http://dx.doi.org/10.1016/j.ejps.2007.10.006
Eckert R, Qi F, Yarbrough DK, He J, Anderson MH, Shi W (2006) Adding selectivity to antimicrobial peptides: rational design of a multidomain peptide against Pseudomonas spp. Antimicrob Agents Chemother 50(4):1480–1488. doi:10.1128/aac.50.4.1480-1488.2006
Etayash H, Norman L, Thundat T, Stiles M, Kaur K (2013) Surface-conjugated antimicrobial peptide leucocin a displays high binding to pathogenic gram-positive bacteria. ACS Appl Mater Interfaces 6(2):1131–1138. doi:10.1021/am404729c
Faber M, Leysen J, Bridts C, Sabato V, De Clerck LS, Ebo DG (2012) Allergy to chlorhexidine: beware of the central venous catheter. Acta Anaesthesiol Belg 63(4):191–194
Fadeeva E, Truong VK, Stiesch M, Chichkov BN, Crawford RJ, Wang J, Ivanova EP (2011) Bacterial retention on superhydrophobic titanium surfaces fabricated by femtosecond laser ablation. Langmuir 27(6):3012–3019. doi:10.1021/la104607g
Fan JH, Hung WI, Li WT, Yeh JM (2009) Biocompatibility study of gold nanoparticles to human cells. In: Lim C, Goh JH (eds) 13th international conference on biomedical engineering, vol 23. IFMBE proceedings. Springer, Berlin, pp 870–873. doi:10.1007/978-3-540-92841-6_214
Fernandez-Lopez S, Kim H-S, Choi EC, Delgado M, Granja JR, Khasanov A, Kraehenbuehl K, Long G, Weinberger DA, Wilcoxen KM, Ghadiri MR (2001) Antibacterial agents based on the cyclic d, l-[alpha]-peptide architecture. Nature 412(6845):452–455
Fitzgerald-Hughes D, Devocelle M, Humphreys H (2012) Beyond conventional antibiotics for the future treatment of methicillin-resistant Staphylococcus aureus infections: two novel alternatives. FEMS Immunol Med Microbiol 65(3):399–412. doi:10.1111/j.1574-695X.2012.00954.x
Forbes S, McBain AJ, Felton-Smith S, Jowitt TA, Birchenough HL, Dobson CB (2013) Comparative surface antimicrobial properties of synthetic biocides and novel human apolipoprotein E derived antimicrobial peptides. Biomaterials 34(22):5453–5464. http://dx.doi.org/10.1016/j.biomaterials.2013.03.087
Francolini I, Donelli G (2010) Prevention and control of biofilm-based medical-device-related infections. FEMS Immunol Med Microbiol 59(3):227–238. doi:10.1111/j.1574-695X.2010.00665.x
Francolini I, Donelli G, Crisante F, Taresco V, Piozzi A (2015) Antimicrobial polymers for anti-biofilm medical devices: state-of-art and perspectives. In: Donelli G (ed) Biofilm-based healthcare-associated infections. Advances in experimental medicine and biology, vol 831. Springer International Publishing, Switzerland, pp 93–117. doi:10.1007/978-3-319-09782-4_7
Friedlander RS, Vlamakis H, Kim P, Khan M, Kolter R, Aizenberg J (2013) Bacterial flagella explore microscale hummocks and hollows to increase adhesion. Proc Natl Acad Sci 110(14):5624–5629. doi:10.1073/pnas.1219662110
Fu C, Liu T, Li L, Liu H, Liang Q, Meng X (2015) Effects of graphene oxide on the development of offspring mice in lactation period. Biomaterials 40:23–31. http://dx.doi.org/10.1016/j.biomaterials.2014.11.014
Gajski G, Jelčić Ž, Oreščanin V, Gerić M, Kollar R, Garaj-Vrhovac V (2014) Physico-chemical characterization and the in vitro genotoxicity of medical implants metal alloy (TiAlV and CoCrMo) and polyethylene particles in human lymphocytes. Biochim Biophys Acta Gen Subj 1840(1):565–576. http://dx.doi.org/10.1016/j.bbagen.2013.10.015
Gan X, Liu T, Zhong J, Liu X, Li G (2004) Effect of silver nanoparticles on the electron transfer reactivity and the catalytic activity of myoglobin. ChemBioChem 5(12):1686–1691. doi:10.1002/cbic.200400080
Gao P, Nie X, Zou M, Shi Y, Cheng G (2011) Recent advances in materials for extended-release antibiotic delivery system. J Antibiot 64(9):625–634
Gening ML, Titov DV, Cecioni S, Audfray A, Gerbst AG, Tsvetkov YE, Krylov VB, Imberty A, Nifantiev NE, Vidal S (2013) Synthesis of multivalent carbohydrate-centered glycoclusters as nanomolar ligands of the bacterial lectin LecA from Pseudomonas aeruginosa. Chem Eur J 19(28):9272–9285. doi:10.1002/chem.201300135
Gérard C, Bordeleau L-J, Barralet J, Doillon CJ (2010) The stimulation of angiogenesis and collagen deposition by copper. Biomaterials 31(5):824–831. http://dx.doi.org/10.1016/j.biomaterials.2009.10.009
Gerdes K, Maisonneuve E (2012) Bacterial persistence and toxin-antitoxin loci. Annu Rev Microbiol 66(1):103–123. doi:10.1146/annurev-micro-092611-150159
Germain E, Castro-Roa D, Zenkin N, Gerdes K (2013) Molecular mechanism of bacterial persistence by HipA. Mol Cell 52(2):248–254. doi:10.1016/j.molcel.2013.08.045
Gnanadhas DP, Ben Thomas M, Thomas R, Raichur AM, Chakravortty D (2013) Interaction of silver nanoparticles with serum proteins affects their antimicrobial activity in vivo. Antimicrob Agents Chemother 57(10):4945–4955. doi:10.1128/aac.00152-13
Grainger DW, van der Mei HC, Jutte PC, van den Dungen JJAM, Schultz MJ, van der Laan BFAM, Zaat SAJ, Busscher HJ (2013) Critical factors in the translation of improved antimicrobial strategies for medical implants and devices. Biomaterials 34(37):9237–9243. http://dx.doi.org/10.1016/j.biomaterials.2013.08.043
Guiton PS, Cusumano CK, Kline KA, Dodson KW, Han Z, Janetka JW, Henderson JP, Caparon MG, Hultgren SJ (2012) Combinatorial small-molecule therapy prevents uropathogenic Escherichia coli catheter-associated urinary tract infections in mice. Antimicrob Agents Chemother 56(9):4738–4745. doi:10.1128/aac.00447-12
Guleri A, Kumar A, Morgan RJM, Hartley M, Roberts DH (2012) Anaphylaxis to chlorhexidine-coated central venous catheters: a case series and review of the literature. Surg Infect 13(3):171–174. doi:10.1089/sur.2011.011
Hale JDF, Hancock REW (2007) Alternative mechanisms of action of cationic antimicrobial peptides on bacteria. Expert Rev Anti-Infect Ther 5(6):951–959. doi:10.1586/14787210.5.6.951
Hamuro Y, Schneider JP, Degrado WF (1999) De novo design of antibacterial β-peptides. J Am Chem Soc 121(51):12200–12201. doi:10.1021/ja992728p
Hancock REW, Sahl H-G (2006) Antimicrobial and host-defense peptides as new anti-infective therapeutic strategies. Nat Biotech 24(12):1551–1557
Hegstad K, Langsrud S, Lunestad BT, Scheie AA, Sunde M, Yazdankhah SP (2010) Does the wide use of quaternary ammonium compounds enhance the selection and spread of antimicrobial resistance and thus threaten our health? Microb Drug Resist 16:91+
Hennessey DB, Burke JP, Ni-Dhonochu T, Shields C, Winter DC, Mealy K (2010) Preoperative hypoalbuminemia is an independent risk factor for the development of surgical site infection following gastrointestinal surgery: a multi-institutional study. Ann Surg 252(2):325–329 310.1097/SLA.1090b1013e3181e9819a
Hogan S, Stevens NT, Humphreys H, O’Gara JP, O’Neill E (2015) Current and future approaches to the prevention and treatment of staphylococcal medical device-related infections. Curr Pharm Des 21(1):100–113
Holden DW (2015) Persisters unmasked. Science 347(6217):30–32. doi:10.1126/science.1262033
Hook AL, Chang C-Y, Yang J, Luckett J, Cockayne A, Atkinson S, Mei Y, Bayston R, Irvine DJ, Langer R, Anderson DG, Williams P, Davies MC, Alexander MR (2012) Combinatorial discovery of polymers resistant to bacterial attachment. Nat Biotechnol 30(9):868–875. doi:10.1038/nbt.2316. http://www.nature.com/nbt/journal/v30/n9/abs/nbt.2316.html#supplementary-information
Hsin Y-H, Chen C-F, Huang S, Shih T-S, Lai P-S, Chueh PJ (2008) The apoptotic effect of nanosilver is mediated by a ROS- and JNK-dependent mechanism involving the mitochondrial pathway in NIH3T3 cells. Toxicol Lett 179(3):130–139. http://dx.doi.org/10.1016/j.toxlet.2008.04.015
Imura Y, Choda N, Matsuzaki K (2008) Magainin 2 in action: distinct modes of membrane permeabilization in living bacterial and mammalian cells. Biophys J 95(12):5757–5765. http://dx.doi.org/10.1529/biophysj.108.133488
Ivanova EP, Hasan J, Webb HK, Truong VK, Watson GS, Watson JA, Baulin VA, Pogodin S, Wang JY, Tobin MJ, Löbbe C, Crawford RJ (2012) Natural bactericidal surfaces: mechanical rupture of Pseudomonas aeruginosa cells by cicada wings. Small 8(16):2489–2494. doi:10.1002/smll.201200528
Ivanova EP, Hasan J, Webb HK, Gervinskas G, Juodkazis S, Truong VK, Wu AHF, Lamb RN, Baulin VA, Watson GS, Watson JA, Mainwaring DE, Crawford RJ (2013) Bactericidal activity of black silicon. Nat Commun 4. doi:10.1038/ncomms3838
Jacobs T, Morent R, De Geyter N, Dubruel P, Leys C (2012) Plasma surface modification of biomedical polymers: influence on cell-material interaction. Plasma Chem Plasma Process 32(5):1039–1073. doi:10.1007/s11090-012-9394-8
Jadalannagari S, Deshmukh K, Ramanan S, Kowshik M (2014) Antimicrobial activity of hemocompatible silver doped hydroxyapatite nanoparticles synthesized by modified sol–gel technique. Appl Nanosci 4(2):133–141. doi:10.1007/s13204-013-0197-x
Jamal MA, Rosenblatt JS, Hachem RY, Ying J, Pravinkumar E, Nates JL, Chaftari A-MP, Raad II (2014) Prevention of biofilm colonization by Gram-negative bacteria on minocycline-rifampin-impregnated catheters sequentially coated with chlorhexidine. Antimicrob Agents Chemother 58(2):1179–1182. doi:10.1128/aac.01959-13
Jayathillake A, Mason DF, Broome K (2003) Allergy to chlorhexidine gluconate in urethral gel: report of four cases and review of the literature. Urology 61(4):837. doi:10.1016/S0090-4295(02)02432-9
Jo YK, Seo JH, Choi B-H, Kim BJ, Shin HH, Hwang BH, Cha HJ (2014) Surface-independent antibacterial coating using silver nanoparticle-generating engineered mussel glue. ACS Appl Mater Interfaces 6(22):20242–20253. doi:10.1021/am505784k
Johnson JR, Johnston B, Kuskowski MA (2012) In vitro comparison of nitrofurazone- and silver alloy-coated foley catheters for contact-dependent and diffusible inhibition of urinary tract infection-associated microorganisms. Antimicrob Agents Chemother 56(9):4969–4972. doi:10.1128/aac.00733-12
Jun E-A, Lim K-M, Kim K, Bae O-N, Noh J-Y, Chung K-H, Chung J-H (2011) Silver nanoparticles enhance thrombus formation through increased platelet aggregation and procoagulant activity. Nanotoxicology 5(2):157–167. doi:10.3109/17435390.2010.506250
Justice SS, Harrison A, Becknell B, Mason KM (2014) Bacterial differentiation, development, and disease: mechanisms for survival. FEMS Microbiol Lett 360(1):1–8. doi:10.1111/1574-6968.12602
Kalaivani S, Singh RK, Ganesan V, Kannan S (2014) Effect of copper (Cu2+) inclusion on the bioactivity and antibacterial behavior of calcium silicate coatings on titanium metal. J Mater Chem B 2(7):846–858. doi:10.1039/C3TB21522A
Karahalil B, Kadioglu E, Tuzuner-Oncul AM, Cimen E, Emerce E, Kisnisci RS (2014) Micronucleus assay assessment of possible genotoxic effects in patients treated with titanium alloy endosseous implants or miniplates. Mutat Res/Genet Toxicol Environ Mutagen 760:70–72. http://dx.doi.org/10.1016/j.mrgentox.2013.10.005
Karlsson HL, Cronholm P, Hedberg Y, Tornberg M, De Battice L, Svedhem S, Wallinder IO (2013) Cell membrane damage and protein interaction induced by copper containing nanoparticles—Importance of the metal release process. Toxicology 313(1):59–69. http://dx.doi.org/10.1016/j.tox.2013.07.012
Karlsson J, Sundell G, Thuvander M, Andersson M (2014) Atomically resolved tissue integration. Nano Lett 14(8):4220–4223. doi:10.1021/nl501564f
Kawata K, Osawa M, Okabe S (2009) In vitro toxicity of silver nanoparticles at noncytotoxic doses to HepG2 human hepatoma cells. Environ Sci Technol 43(15):6046–6051. doi:10.1021/es900754q
Khan W, Challa V, Pawar R, Nyska M, Brin Y, Domb A (2014) Antibiotics delivery for treating bone infections. In: Domb AJ, Khan W (eds) Focal controlled drug delivery. Advances in delivery science and technology. Springer, New York, pp 459–472. doi:10.1007/978-1-4614-9434-8_21
Khoo A, Oziemski P (2011) Chlorhexidine impregnated central venous catheter inducing an anaphylactic shock in the intensive care unit. Heart Lung Circ 20(10):669–670. http://dx.doi.org/10.1016/j.hlc.2010.10.001
Kilic E, Er N, Alkan A, Ferahbas A (2011) Accidental benzalkonium chloride (zephiran) injection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112(6):e103–e105. doi:10.1016/j.tripleo.2011.06.004
Kim S, Choi JE, Choi J, Chung K-H, Park K, Yi J, Ryu D-Y (2009) Oxidative stress-dependent toxicity of silver nanoparticles in human hepatoma cells. Toxicol in Vitro 23(6):1076–1084. http://dx.doi.org/10.1016/j.tiv.2009.06.001
Knetsch MLW, Koole LH (2011) New strategies in the development of antimicrobial coatings: the example of increasing usage of silver and silver nanoparticles. Polymers 3(1):340–366
Kottur J, Sharma A, Gore Kiran R, Narayanan N, Samanta B, Pradeepkumar PI, Nair Deepak T (2015) Unique structural features in DNA polymerase IV enable efficient bypass of the N2 adduct induced by the nitrofurazone antibiotic. Structure 23(1):56–67. http://dx.doi.org/10.1016/j.str.2014.10.019
Lang NP, Salvi GE, Huynh-Ba G, Ivanovski S, Donos N, Bosshardt DD (2011) Early osseointegration to hydrophilic and hydrophobic implant surfaces in humans. Clin Oral Implants Res 22(4):349–356. doi:10.1111/j.1600-0501.2011.02172.x
Laroux FS, Pavlick KP, Hines IN, Kawachi S, Harada H, Bharwani S, Hoffman JM, Grisham MB (2001) Role of nitric oxide in inflammation. Acta Physiol Scand 173(1):113–118. doi:10.1046/j.1365-201X.2001.00891.x
Lenaeus MJ, Burdette D, Wagner T, Focia PJ, Gross A (2014) Structures of KcsA in complex with symmetrical quaternary ammonium compounds reveal a hydrophobic binding site. Biochemistry 53(32):5365–5373. doi:10.1021/bi500525s
Li P, Poon YF, Li W, Zhu H-Y, Yeap SH, Cao Y, Qi X, Zhou C, Lamrani M, Beuerman RW, Kang E-T, Mu Y, Li CM, Chang MW, Jan Leong SS, Chan-Park MB (2011) A polycationic antimicrobial and biocompatible hydrogel with microbe membrane suctioning ability. Nat Mater 10(2):149–156. http://www.nature.com/nmat/journal/v10/n2/abs/nmat2915.html#supplementary-information
Li X, Wang L, Fan Y, Feng Q, Cui F-z (2012) Biocompatibility and toxicity of nanoparticles and nanotubes. J Nanomater 2012:19. doi:10.1155/2012/548389
Li Y, Heine S, Entian M, Sauer K, Frankenberg-Dinkel N (2013) NO-induced biofilm dispersion in Pseudomonas aeruginosa is mediated by an MHYT domain-coupled phosphodiesterase. J Bacteriol 195(16):3531–3542. doi:10.1128/jb.01156-12
Lih E, Oh SH, Joung YK, Lee JH, Han DK (2015) Polymers for cell/tissue anti-adhesion. Progress in Polymer Science. http://dx.doi.org/10.1016/j.progpolymsci.2014.10.004
Ling LL, Schneider T, Peoples AJ, Spoering AL, Engels I, Conlon BP, Mueller A, Schaberle TF, Hughes DE, Epstein S, Jones M, Lazarides L, Steadman VA, Cohen DR, Felix CR, Fetterman KA, Millett WP, Nitti AG, Zullo AM, Chen C, Lewis K (2015) A new antibiotic kills pathogens without detectable resistance. Nat Adv Online Publ. doi:10.1038/nature14098. http://www.nature.com/nature/journal/vaop/ncurrent/abs/nature14098.html#supplementary-information
Lisanti M, Piolanti N, Tagliaferri E, Andreani L, Parchi P, Menichetti F (2015) The fight against the slime: can we ever win? In: Baldini A, Caldora P (eds) Perioperative medical management for total joint arthroplasty. Springer International Publishing, Switzerland, pp 253–267. doi:10.1007/978-3-319-07203-6_21
Liu S, Zeng TH, Hofmann M, Burcombe E, Wei J, Jiang R, Kong J, Chen Y (2011) Antibacterial activity of graphite, graphite oxide, graphene oxide, and reduced graphene oxide: membrane and oxidative stress. ACS Nano 5(9):6971–6980. doi:10.1021/nn202451x
Liu H, Zhang D, Shen F, Zhang G, Song S (2012a) Hemocompatibility and anti-endothelialization of copper–titanium coating for vena cava filters. Surf Coat Technol 206(16):3501–3507. http://dx.doi.org/10.1016/j.surfcoat.2012.02.025
Liu W-d, Zhang Y-h, Fang L-f, Zhu B-k, Zhu L-p (2012b) Antifouling properties of poly(vinyl chloride) membranes modified by amphiphilic copolymers P(MMA-b-MAA). Chin J Polym Sci 30(4):568–577. doi:10.1007/s10118-012-1153-z
Liu X, Xu Y, Wu Z, Chen H (2013a) Poly(N-vinylpyrrolidone)-modified surfaces for biomedical applications. Macromol Biosci 13(2):147–154. doi:10.1002/mabi.201200269
Liu Y, Yang Y, Wang C, Zhao X (2013b) Stimuli-responsive self-assembling peptides made from antibacterial peptides. Nanoscale 5(14):6413–6421. doi:10.1039/c3nr00225j
Liu X, Huang R, Su R, Qi W, Wang L, He Z (2014) Grafting hyaluronic acid onto gold surface to achieve low protein fouling in surface plasmon resonance biosensors. ACS Appl Mater Interfaces 6(15):13034–13042. doi:10.1021/am502921z
Lo AWH, Van de Water K, Gane PJ, Chan AWE, Steadman D, Stevens K, Selwood DL, Waksman G, Remaut H (2013) Suppression of type 1 pilus assembly in uropathogenic Escherichia coli by chemical inhibition of subunit polymerization. J Antimicrob Chemother. doi:10.1093/jac/dkt467
Ma J, Zhang J, Xiong Z, Yong Y, Zhao XS (2011) Preparation, characterization and antibacterial properties of silver-modified graphene oxide. J Mater Chem 21(10):3350–3352. doi:10.1039/C0JM02806A
Maeda H, Uehara A, Saito T, Mayanagi H, Nagaoka I, Takada H (2007) An antibacterial protein CAP18/LL-37 enhanced production of hepatocyte growth factor in human gingival fibroblast cultures. In: Watanabe M, Okuno O, Sasaki K, Takahashi N, Suzuki O, Takada H (eds) Interface oral health science 2007. Springer, Tokyo, Japan, pp 283–284. doi:10.1007/978-4-431-76690-2_55
Maisonneuve E, Shakespeare LJ, Jørgensen MG, Gerdes K (2011) Bacterial persistence by RNA endonucleases. Proc Natl Acad Sci 108(32):13206–13211. doi:10.1073/pnas.1100186108
Martín VI, de la Haba RR, Ventosa A, Congiu E, Ortega-Calvo JJ, Moyá ML (2014) Colloidal and biological properties of cationic single-chain and dimeric surfactants. Colloids Surf B: Biointerfaces 114:247–254. http://dx.doi.org/10.1016/j.colsurfb.2013.10.017
Mazzotti F, Beuttler J, Zeller R, Fink U, Schindler S, Wendel A, Hartung T, von Aulock S (2007) In vitro pyrogen test—a new test method for solid medical devices. J Biomed Mater Res A 80A(2):276–282. doi:10.1002/jbm.a.30922
Miura N, Shinohara Y (2009) Cytotoxic effect and apoptosis induction by silver nanoparticles in HeLa cells. Biochem Biophys Res Commun 390(3):733–737. http://dx.doi.org/10.1016/j.bbrc.2009.10.039
Moalli P, Brown B, Reitman MF, Nager C (2014) Polypropylene mesh: evidence for lack of carcinogenicity. Int Urogynecol J 25(5):573–576. doi:10.1007/s00192-014-2343-8
Morones-Ramirez JR, Winkler JA, Spina CS, Collins JJ (2013) Silver enhances antibiotic activity against Gram-negative bacteria. Sci Transl Med 5(190):190ra181. doi:10.1126/scitranslmed.3006276
Mouriño V, Cattalini JP, Boccaccini AR (2012) Metallic ions as therapeutic agents in tissue engineering scaffolds: an overview of their biological applications and strategies for new developments. J R Soc Interface 9(68):401–419
Muffly TM, Tizzano AP, Walters MD (2011) The history and evolution of sutures in pelvic surgery. J R Soc Med 104(3):107–112. doi:10.1258/jrsm.2010.100243
Muszanska AK, Rochford ETJ, Gruszka A, Bastian AA, Busscher HJ, Norde W, van der Mei HC, Herrmann A (2014) Antiadhesive polymer brush coating functionalized with antimicrobial and RGD peptides to reduce biofilm formation and enhance tissue integration. Biomacromolecules 15(6):2019–2026. doi:10.1021/bm500168s
Nait Chabane Y, Mlouka M, Alexandre S, Nicol M, Marti S, Pestel-Caron M, Vila J, Jouenne T, De E (2014) Virstatin inhibits biofilm formation and motility of Acinetobacter baumannii. BMC Microbiol 14(1):62
Neumayer L, Hosokawa P, Itani K, El-Tamer M, Henderson WG, Khuri SF (2007) Multivariable predictors of postoperative surgical site infection after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg 204(6):1178–1187. http://dx.doi.org/10.1016/j.jamcollsurg.2007.03.022
Ng VWL, Tan JPK, Leong J, Voo ZX, Hedrick JL, Yang YY (2014) Antimicrobial polycarbonates: investigating the impact of nitrogen-containing heterocycles as quaternizing agents. Macromolecules 47(4):1285–1291. doi:10.1021/ma402641p
Nikitushkin V, Demina G, Shleeva M, Kaprelyants A (2013) Peptidoglycan fragments stimulate resuscitation of “non-culturable” mycobacteria. Antonie Van Leeuwenhoek 103(1):37–46. doi:10.1007/s10482-012-9784-1
Nizet V, Ohtake T, Lauth X, Trowbridge J, Rudisill J, Dorschner RA, Pestonjamasp V, Piraino J, Huttner K, Gallo RL (2001) Innate antimicrobial peptide protects the skin from invasive bacterial infection. Nature 414(6862):454–457
O’Connell HA, Kottkamp GS, Eppelbaum JL, Stubblefield BA, Gilbert SE, Gilbert ES (2006) Influences of biofilm structure and antibiotic resistance mechanisms on indirect pathogenicity in a model polymicrobial biofilm. Appl Environ Microbiol 72(7):5013–5019. doi:10.1128/aem.02474-05
O’Toole JE, Eichholz KM, Fessler RG (2009) Surgical site infection rates after minimally invasive spinal surgery. J Neurosurg Spine 11(4):471–476. doi:10.3171/2009.5.SPINE08633
Olsen MA, Nepple JJ, Riew KD, Lenke LG, Bridwell KH, Mayfield J, Fraser VJ (2008) Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg 90(1):62–69
Opstrup MS, Malling HJ, Krøigaard M, Mosbech H, Skov PS, Poulsen LK, Garvey LH (2014) Standardized testing with chlorhexidine in perioperative allergy – a large single-centre evaluation. Allergy 69(10):1390–1396. doi:10.1111/all.12466
Ordikhani F, Tamjid E, Simchi A (2014) Characterization and antibacterial performance of electrodeposited chitosan–vancomycin composite coatings for prevention of implant-associated infections. Mater Sci Eng C 41:240–248. http://dx.doi.org/10.1016/j.msec.2014.04.036
Oren Z, Shai Y (2000) Cyclization of a cytolytic amphipathic α-helical peptide and its diastereomer: effect on structure, interaction with model membranes, and biological function†. Biochemistry 39(20):6103–6114. doi:10.1021/bi992408i
Owens CD, Stoessel K (2008) Surgical site infections: epidemiology, microbiology and prevention. J Hosp Infect 70(Supplement 2):3–10. http://dx.doi.org/10.1016/S0195-6701(08)60017-1
Panyutich AV, Voitenok NN, Lehrer RI, Ganz T (1991) An enzyme immunoassay for human defensins. J Immunol Methods 141(2):149–155. http://dx.doi.org/10.1016/0022-1759(91)90141-2
Park E-J, Yi J, Kim Y, Choi K, Park K (2010) Silver nanoparticles induce cytotoxicity by a Trojan-horse type mechanism. Toxicol in Vitro 24(3):872–878. http://dx.doi.org/10.1016/j.tiv.2009.12.001
Patra P, Klumpp S (2013) Population dynamics of bacterial persistence. PLoS ONE 8(5):e62814. doi:10.1371/journal.pone.0062814
Perez E, Williams M, Jacob JT, Reyes MD, Chernetsky Tejedor S, Steinberg JP, Rowe L, Ganakammal SR, Changayil S, Weil MR, Donlan RM (2014) Microbial biofilms on needleless connectors for central venous catheters: comparison of standard and silver-coated devices collected from patients in an acute care hospital. J Clin Microbiol 52(3):823–831. doi:10.1128/jcm.02220-13
Phillips J, O’Grady H, Baker E (2014) Prevention of surgical site infections. Surgery (Oxford) 32(9):468–471. http://dx.doi.org/10.1016/j.mpsur.2014.06.011
Pittet B, Montandon D, Pittet D (2005) Infection in breast implants. Lancet Infect Dis 5(2):94–106. http://dx.doi.org/10.1016/S1473-3099(05)01281-8
Podila R, Moore T, Alexis F, Rao AM (2013) Graphene coatings for enhanced hemo-compatibility of nitinol stents. RSC Adv 3(6):1660–1665. doi:10.1039/C2RA23073A
Porter EA, Wang X, Lee H-S, Weisblum B, Gellman SH (2000) Antibiotics: non-haemolytic [beta]-amino-acid oligomers. Nature 404(6778):565–565
Powers J-PS, Hancock REW (2003) The relationship between peptide structure and antibacterial activity. Peptides 24(11):1681–1691. http://dx.doi.org/10.1016/j.peptides.2003.08.023
Rai M, Yadav A, Gade A (2009) Silver nanoparticles as a new generation of antimicrobials. Biotechnol Adv 27(1):76–83. http://dx.doi.org/10.1016/j.biotechadv.2008.09.002
Rapsch K, Bier FF, Tadros M, von Nickisch-Rosenegk M (2013) Identification of antimicrobial peptides and immobilization strategy suitable for a covalent surface coating with biocompatible properties. Bioconjug Chem 25(2):308–319. doi:10.1021/bc4004469
Rathbone CR, Cross JD, Brown KV, Murray CK, Wenke JC (2011) Effect of various concentrations of antibiotics on osteogenic cell viability and activity. J Orthop Res 29(7):1070–1074. doi:10.1002/jor.21343
Ravikumar M, Hageman DJ, Tomaszewski WH, Chandra GM, Skousen JL, Capadona JR (2014) The effect of residual endotoxin contamination on the neuroinflammatory response to sterilized intracortical microelectrodes. J Mater Chem B 2(17):2517–2529. doi:10.1039/C3TB21453B
Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R (2005) Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br Vol 87-B(6):844–850. doi:10.1302/0301-620x.87b6.15121
Rosenthal VD (2008) Device-associated nosocomial infections in limited-resources countries: findings of the International Nosocomial Infection Control Consortium (INICC). Am J Infect Control 36(10):S171.e177–S171.e112. http://dx.doi.org/10.1016/j.ajic.2008.10.009
Ryder VJ, Chopra I, O’Neill AJ (2012) Increased mutability of Staphylococci in biofilms as a consequence of oxidative stress. PLoS ONE 7(10):e47695. doi:10.1371/journal.pone.0047695
Sahl H-G, Pag U, Bonness S, Wagner S, Antcheva N, Tossi A (2005) Mammalian defensins: structures and mechanism of antibiotic activity. J Leukoc Biol 77(4):466–475. doi:10.1189/jlb.0804452
Salick DA, Kretsinger JK, Pochan DJ, Schneider JP (2007) Inherent antibacterial activity of a peptide-based β-hairpin hydrogel. J Am Chem Soc 129(47):14793–14799. doi:10.1021/ja076300z
Salick DA, Pochan DJ, Schneider JP (2009) Design of an injectable β-hairpin peptide hydrogel that kills methicillin-resistant Staphylococcus aureus. Adv Mater 21(41):4120–4123. doi:10.1002/adma.200900189
Salwiczek M, Qu Y, Gardiner J, Strugnell RA, Lithgow T, Mclean KM, Thissen H (2014) Emerging rules for effective antimicrobial coatings. Trends Biotechnol 32(2):82–90. http://dx.doi.org/10.1016/j.tibtech.2013.09.008
Sambanthamoorthy K, Sloup RE, Parashar V, Smith JM, Kim EE, Semmelhack MF, Neiditch MB, Waters CM (2012) Identification of small molecules that antagonize diguanylate cyclase enzymes to inhibit biofilm formation. Antimicrob Agents Chemother 56(10):5202–5211. doi:10.1128/aac.01396-12
Sambanthamoorthy K, Luo C, Pattabiraman N, Feng X, Koestler B, Waters CM, Palys TJ (2013) Identification of small molecules inhibiting diguanylate cyclases to control bacterial biofilm development. Biofouling 30(1):17–28. doi:10.1080/08927014.2013.832224
Savage VJ, Chopra I, O’Neill AJ (2013) Staphylococcus aureus biofilms promote horizontal transfer of antibiotic resistance. Antimicrob Agents Chemother 57(4):1968–1970. doi:10.1128/aac.02008-12
Shalev T, Gopin A, Bauer M, Stark RW, Rahimipour S (2012) Non-leaching antimicrobial surfaces through polydopamine bio-inspired coating of quaternary ammonium salts or an ultrashort antimicrobial lipopeptide. J Mater Chem 22(5):2026–2032. doi:10.1039/C1JM13994K
Shamir ER, Warthan M, Brown SP, Nataro JP, Guerrant RL, Hoffman PS (2010) Nitazoxanide inhibits biofilm production and hemagglutination by enteroaggregative Escherichia coli strains by blocking assembly of AafA fimbriae. Antimicrob Agents Chemother 54(4):1526–1533. doi:10.1128/aac.01279-09
Sharaf B, Jandali-Rifai M, Susarla SM, Dodson TB (2011) Do perioperative antibiotics decrease implant failure? J Oral Maxillofac Surg 69(9):2345–2350. http://dx.doi.org/10.1016/j.joms.2011.02.095
Sharma JN, Al-Omran A, Parvathy SS (2007) Role of nitric oxide in inflammatory diseases. Inflammopharmacology 15(6):252–259. doi:10.1007/s10787-007-0013-x
Shetye GS, Singh N, Jia C, Nguyen CDK, Wang G, Luk Y-Y (2014) Specific maltose derivatives modulate the swarming motility of nonswarming mutant and inhibit bacterial adhesion and biofilm formation by Pseudomonas aeruginosa. ChemBioChem 15(10):1514–1523. doi:10.1002/cbic.201402093
Shimazaki K-i, Nam MS, Harakawa S, Tanaka T, Omata Y, Saito A, Kumura H, Mikawa K, Igarashi I, Suzuki N (1996) Monoclonal antibody against bovine lactoferricin(R) and its epitopic site. J Vet Med Sci 58(12):1227–1229. doi:10.1292/jvms.58.12_1227
Shimizu M, Shigeri Y, Tatsu Y, Yoshikawa S, Yumoto N (1998) Enhancement of antimicrobial activity of neuropeptide Y by N-terminal truncation. Antimicrob Agents Chemother 42(10):2745–2746
Shrivastava S, Bera T, Singh SK, Singh G, Ramachandrarao P, Dash D (2009) Characterization of antiplatelet properties of silver nanoparticles. ACS Nano 3(6):1357–1364. doi:10.1021/nn900277t
Silvestri DL, Mcenery-Stonelake M (2013) Chlorhexidine: uses and adverse reactions. Dermatitis 24(3):112–118 110.1097/DER.1090b1013e3182905561
Singh PK, Schaefer AL, Parsek MR, Moninger TO, Welsh MJ, Greenberg EP (2000) Quorum-sensing signals indicate that cystic fibrosis lungs are infected with bacterial biofilms. Nature 407(6805):762–764
Skousen JL, Bridge MJ, Tresco PA (2015) A strategy to passively reduce neuroinflammation surrounding devices implanted chronically in brain tissue by manipulating device surface permeability. Biomaterials 36:33–43. http://dx.doi.org/10.1016/j.biomaterials.2014.08.039
Smock KJ, Schmidt RL, Hadlock G, Stoddard G, Grainger DW, Munger MA (2014) Assessment of orally dosed commercial silver nanoparticles on human ex vivo platelet aggregation. Nanotoxicology 8(3):328–333. doi:10.3109/17435390.2013.788749
Solano C, Echeverz M, Lasa I (2014) Biofilm dispersion and quorum sensing. Curr Opin Microbiol 18:96–104. http://dx.doi.org/10.1016/j.mib.2014.02.008
Sørensen O, Cowland JB, Askaa J, Borregaard N (1997) An ELISA for hCAP-18, the cathelicidin present in human neutrophils and plasma. J Immunol Methods 206(1–2):53–59. http://dx.doi.org/10.1016/S0022-1759(97)00084-7
Sumner DR, Ross R, Purdue E (2014) Are there biological markers for wear or corrosion? A systematic review. Clin Orthop Relat Res 472(12):3728–3739. doi:10.1007/s11999-014-3580-3
Świercz R, Hałatek T, Stetkiewicz J, Wąsowicz W, Kur B, Grzelińska Z, Majcherek W (2013) Toxic effect in the lungs of rats after inhalation exposure to benzalkonium chloride. IJOMEH 26(4):647–656. doi:10.2478/s13382-013-0137-8
Taheri S, Cavallaro A, Christo SN, Smith LE, Majewski P, Barton M, Hayball JD, Vasilev K (2014) Substrate independent silver nanoparticle based antibacterial coatings. Biomaterials 35(16):4601–4609. http://dx.doi.org/10.1016/j.biomaterials.2014.02.033
Takeshima K, Chikushi A, Lee K-K, Yonehara S, Matsuzaki K (2003) Translocation of analogues of the antimicrobial peptides magainin and buforin across human cell membranes. J Biol Chem 278(2):1310–1315. doi:10.1074/jbc.M208762200
Tamam E, Turkyilmaz I (2014) Effects of pH and elevated glucose levels on the electrochemical behavior of dental implants. J Oral Implantol 40(2):153–159. doi:10.1563/AAID-JOI-D-11-00083
Taylor A (1985) Therapeutic uses of trace elements. Clin Endocrinol Metab 14(3):703–724. http://dx.doi.org/10.1016/S0300-595X(85)80013-X
Taylor U, Barchanski A, Garrels W, Klein S, Kues W, Barcikowski S, Rath D (2012) Toxicity of gold nanoparticles on somatic and reproductive cells. In: Zahavy E, Ordentlich A, Yitzhaki S, Shafferman A (eds) Nano-biotechnology for biomedical and diagnostic research. Advances in experimental medicine and biology, vol 733. Springer, Dordrecht, pp 125–133. doi:10.1007/978-94-007-2555-3_12
Tejero R, Anitua E, Orive G (2014) Toward the biomimetic implant surface: biopolymers on titanium-based implants for bone regeneration. Prog Polym Sci 39(7):1406–1447. http://dx.doi.org/10.1016/j.progpolymsci.2014.01.001
Thakkar V, Ghobrial GM, Maulucci CM, Singhal S, Prasad SK, Harrop JS, Vaccaro AR, Behrend C, Sharan AD, Jallo J (2014) Nasal MRSA colonization: impact on surgical site infection following spine surgery. Clin Neurol Neurosurg 125:94–97. http://dx.doi.org/10.1016/j.clineuro.2014.07.018
Thomson KS, Korte FS, Giachelli CM, Ratner BD, Regnier M, Scatena M (2013) Prevascularized microtemplated fibrin scaffolds for cardiac tissue engineering applications. Tissue Eng A 19(7-8):967–977. doi:10.1089/ten.tea.2012.0286
Tomasinsig L, Morgera F, Antcheva N, Pacor S, Skerlavaj B, Zanetti M, Tossi A (2009) Structure dependence of biological activities for primate cathelicidins. J Pept Sci 15(9):576–582. doi:10.1002/psc.1143
Totsika M, Kostakioti M, Hannan TJ, Upton M, Beatson SA, Janetka JW, Hultgren SJ, Schembri MA (2013) A FimH inhibitor prevents acute bladder infection and treats chronic cystitis caused by multidrug-resistant uropathogenic Escherichia coli ST131. J Infect Dis 208(6):921–928. doi:10.1093/infdis/jit245
Triantafillopoulos I, Papaioannou N (2014) The effect of pharmacological agents on the bone-implant interface. In: Karachalios T (ed) Bone-implant interface in orthopedic surgery. Springer, London, pp 221–237. doi:10.1007/978-1-4471-5409-9_16
Tu Q, Wang J-C, Liu R, He J, Zhang Y, Shen S, Xu J, Liu J, Yuan M-S, Wang J (2013) Antifouling properties of poly(dimethylsiloxane) surfaces modified with quaternized poly(dimethylaminoethyl methacrylate). Colloids Surf B: Biointerfaces 102:361–370. http://dx.doi.org/10.1016/j.colsurfb.2012.08.033
Tuomanen E, Cozens R, Tosch W, Zak O, Tomasz A (1986) The rate of killing of Escherichia coli byβ-lactam antibiotics is strictly proportional to the rate of bacterial growth. J Gen Microbiol 132(5):1297–1304. doi:10.1099/00221287-132-5-1297
Veiga AS, Sinthuvanich C, Gaspar D, Franquelim HG, Castanho MARB, Schneider JP (2012) Arginine-rich self-assembling peptides as potent antibacterial gels. Biomaterials 33(35):8907–8916. http://dx.doi.org/10.1016/j.biomaterials.2012.08.046
Veronesi B, Chorley B, Ward W, Simmons SO, Tennant A, Vallanat B (2014) The physicochemistry of capped nanosilver predicts its biological activity in rat brain endothelial cells (RBEC4). ACS Sustain Chem Eng 2(7):1566–1573. doi:10.1021/sc5000896
Vetten MA, Yah CS, Singh T, Gulumian M (2014) Challenges facing sterilization and depyrogenation of nanoparticles: effects on structural stability and biomedical applications. Nanomed Nanotechnol Biol Med 10(7):1391–1399. http://dx.doi.org/10.1016/j.nano.2014.03.017
Wang Z, Li N, Zhao J, White JC, Qu P, Xing B (2012) CuO nanoparticle interaction with human epithelial cells: cellular uptake, location, export, and genotoxicity. Chem Res Toxicol 25(7):1512–1521. doi:10.1021/tx3002093
Wang Z, Chen Z, Zuo Q, Song F, Wu D, Cheng W, Fan W (2013) Reproductive toxicity in adult male rats following intra-articular injection of cobalt–chromium nanoparticles. J Orthop Sci 18(6):1020–1026. doi:10.1007/s00776-013-0458-2
Wang L, Su B, Cheng C, Ma L, Li S, Nie S, Zhao C-S (2014) Layer by Layer assembly of sulfonic poly(ether sulfone) as heparin-mimicking coatings: scalable fabrication of super-hemocompatible and antibacterial membranes. J Mater Chem B. doi:10.1039/C4TB01865F
Wang R, Neoh KG, Kang E-T (2015) Integration of antifouling and bactericidal moieties for optimizing the efficacy of antibacterial coatings. J Colloid Interface Sci 438:138–148. http://dx.doi.org/10.1016/j.jcis.2014.09.070
Weissman C, Murray WB (2013) It’s not just another room…. Anesth Analg 117(2):287–289 210.1213/ANE.1210b1013e3182991c3182990e
Wong KKY, Liu X (2010) Silver nanoparticles-the real “silver bullet” in clinical medicine? MedChemComm 1(2):125–131. doi:10.1039/C0MD00069H
Wu F, Meng G, He J, Wu Y, Wu F, Gu Z (2014) Antibiotic-loaded chitosan hydrogel with superior dual functions: antibacterial efficacy and osteoblastic cell responses. ACS Appl Mater Interfaces 6(13):10005–10013. doi:10.1021/am502537k
Xue Y, Hieda Y, Kimura K, Takayama K, Fujihara J, Tsujino Y (2004) Kinetic characteristics and toxic effects of benzalkonium chloride following intravascular and oral administration in rats. J Chromatogr B 811(1):53–58. http://dx.doi.org/10.1016/j.jchromb.2004.03.075
Xue Y, Zhang S, Tang M, Zhang T, Wang Y, Hieda Y, Takeshita H (2012) Comparative study on toxic effects induced by oral or intravascular administration of commonly used disinfectants and surfactants in rats. J Appl Toxicol 32(7):480–487. doi:10.1002/jat.1662
Yang C, Ding X, Ono RJ, Lee H, Hsu LY, Tong YW, Hedrick J, Yang YY (2014) Brush-like polycarbonates containing dopamine, cations, and PEG providing a broad-spectrum, antibacterial, and antifouling surface via one-step coating. Adv Mater 26(43):7346–7351. doi:10.1002/adma.201402059
Ye Q, Zhou F (2015) Antifouling surfaces based on polymer brushes. In: Zhou F (ed) Antifouling surfaces and materials. Springer, Berlin, pp 55–81. doi:10.1007/978-3-662-45204-2_3
Ye J, He J, Wang C, Yao K, Gou Z (2014) Copper-containing mesoporous bioactive glass coatings on orbital implants for improving drug delivery capacity and antibacterial activity. Biotechnol Lett 36(5):961–968. doi:10.1007/s10529-014-1465-x
Yeung AY, Gellatly S, Hancock RW (2011) Multifunctional cationic host defence peptides and their clinical applications. Cell Mol Life Sci 68(13):2161–2176. doi:10.1007/s00018-011-0710-x
Yin LM, Edwards MA, Li J, Yip CM, Deber CM (2012) Roles of hydrophobicity and charge distribution of cationic antimicrobial peptides in peptide-membrane interactions. J Biol Chem 287(10):7738–7745. doi:10.1074/jbc.M111.303602
Yu Q, Zhang Y, Wang H, Brash J, Chen H (2011) Anti-fouling bioactive surfaces. Acta Biomater 7(4):1550–1557. http://dx.doi.org/10.1016/j.actbio.2010.12.021
Yu X, Ning Z, Hua M, Wang C, Cui F (2013) Mechanical and biomedical properties of copper-containing diamond-like carbon films on magnesium alloys. J Mater Chem B 1(37):4773–4780. doi:10.1039/C3TB20570C
Zaiou M, Nizet V, Gallo RL (2003) Antimicrobial and protease inhibitory functions of the human cathelicidin (hCAP18/LL-37) prosequence. J Investig Dermatol 120(5):810–816
Zasloff M (2002) Antimicrobial peptides of multicellular organisms. Nature 415(6870):389–395
Zhang X, Oglęcka K, Sandgren S, Belting M, Esbjörner EK, Nordén B, Gräslund A (2010) Dual functions of the human antimicrobial peptide LL-37—target membrane perturbation and host cell cargo delivery. Biochim Biophys Acta Biomembr 1798(12):2201–2208. http://dx.doi.org/10.1016/j.bbamem.2009.12.011
Zhao K, Tseng BS, Beckerman B, Jin F, Gibiansky ML, Harrison JJ, Luijten E, Parsek MR, Wong GCL (2013a) Psl trails guide exploration and microcolony formation in Pseudomonas aeruginosa biofilms. Nature 497(7449):388–391. doi:10.1038/nature12155. http://www.nature.com/nature/journal/v497/n7449/abs/nature12155.html#supplementary-information
Zhao Y, Chen Z, Chen Y, Xu J, Li J, Jiang X (2013b) Synergy of non-antibiotic drugs and pyrimidinethiol on gold nanoparticles against superbugs. J Am Chem Soc 135(35):12940–12943. doi:10.1021/ja4058635
Zhao Z, Ni H, Han Z, Jiang T, Xu Y, Lu X, Ye P (2013c) Effect of surface compositional heterogeneities and microphase segregation of fluorinated amphiphilic copolymers on antifouling performance. ACS Appl Mater Interfaces 5(16):7808–7818. doi:10.1021/am401568b
Zheng J, Song W, Huang H, Chen H (2010) Protein adsorption and cell adhesion on polyurethane/Pluronic® surface with lotus leaf-like topography. Colloids Surf B: Biointerfaces 77(2):234–239. http://dx.doi.org/10.1016/j.colsurfb.2010.01.032
Zhou C, Li P, Qi X, Sharif ARM, Poon YF, Cao Y, Chang MW, Leong SSJ, Chan-Park MB (2011) A photopolymerized antimicrobial hydrogel coating derived from epsilon-poly-l-lysine. Biomaterials 32(11):2704–2712. http://dx.doi.org/10.1016/j.biomaterials.2010.12.040
Zhou Z, Calabrese DR, Taylor W, Finlay JA, Callow ME, Callow JA, Fischer D, Kramer EJ, Ober CK (2014) Amphiphilic triblock copolymers with PEGylated hydrocarbon structures as environmentally friendly marine antifouling and fouling-release coatings. Biofouling 30(5):589–604. doi:10.1080/08927014.2014.897335
Zhu L-J, Zhu L-P, Yi Z, Jiang J-H, Zhu B-K, Xu Y-Y (2013) Hemocompatible and antibacterial porous membranes with heparinized copper hydroxide nanofibers as separation layer. Colloids Surf B: Biointerfaces 110:36–44. http://dx.doi.org/10.1016/j.colsurfb.2013.04.020
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bazaka, O., Bazaka, K. (2015). Cytotoxic Effects and Biocompatibility of Antimicrobial Materials. In: Ivanova, E., Crawford, R. (eds) Antibacterial Surfaces. Springer, Cham. https://doi.org/10.1007/978-3-319-18594-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-18594-1_7
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-18593-4
Online ISBN: 978-3-319-18594-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)